Abstract
The study aims to tackle the seed and soil microbiome and mechanisms that contribute to the effect of synbiotics in enhancing immunogenicity after SARS-CoV-2 vaccination in elderly and diabetic patients. Among 369 subjects who received 3 months of SIM01, a gut microbiota-derived synbiotic formula of three Bifidobacterium strains (B. adolescentis, B. bididum, and B. longum) or a placebo after the SARS-CoV-2 vaccines (mRNA vaccine BNT162b2 (Pfizer-BioNTech) or the inactivated vaccine Sinovac-CoronaVac), we performed metagenomic sequencing in stool samples of 280 vaccinees collected at baseline and 3-month postvaccination and metabonomic sequencing in 276 vaccinees collected at baseline and 1-month postvaccination. The open niche of autochthonous gut microbiota (lower levels of Bifidobacterium and decreased functional potential for carbohydrate metabolism) was associated with enhancing SIM01-contained species. The enrichment of three bifidobacterial species after 3 months of SIM01 intervention (BABBBL_fc) was positively correlated with the level of neutralizing antibodies to the BNT162b2 vaccine at 6-month postvaccination. The fold change of benzoic acid was positively correlated with BABBBL_fc in the BNT162b2 vaccinees, which was also implicated with SARS-CoV-2 surrogate virus neutralization test (sVNT)% levels at 1-month postvaccination. Importantly, SIM01 strain engraftment assessed by StrainPhlAn (A metagenomic strain-level population genomics tool) was associated with a higher fold change of three bifidobacterial species and could be predicted based on the baseline gut microbiome. Therefore, the resident gut microbiome affected the SIM01 engraftment, which was associated with the immunogenicity of SARS-CoV-2 BNT162b2 vaccines.
Similar content being viewed by others
Introduction
Vaccines for SARS-CoV-2 have demonstrated efficacy in preventing infection and mitigating disease severity; however, the determinants influencing their immunogenicity and duration of protection are not yet fully understood. The elderly and individuals with diabetes mellitus were at an increased risk of more severe manifestations and higher mortality rates from COVID-191,2,3,4,5,6. Also, the antibody responses following COVID-19 vaccination in diabetes patients and the elderly were diminished7,8,9,10. Aging is associated with declining innate and adaptive immune system functionality11. In diabetic patients, immune responses are compromised due to the negative impacts of insulin deficiency and hyperglycemia on cellular immunity12. Hence, exploring strategies that enhance postvaccination immunogenicity in these vulnerable groups is imperative.
The gut microbiota is crucial for maintaining the host’s health by performing key functions, including nutrient provision, vitamin synthesis, facilitation of metabolic processes, and modulation of the immune system13. Our prior observation studies of the gut microbiota in recipients of COVID-19 vaccines demonstrated that postvaccination immune response enhancement or sustainability is associated with certain microbial markers or metabolites14,15. In addition, our previous study suggested that SIM01 hastened antibody formation against SARS-CoV-2, reduced nasopharyngeal viral load, reduced pro-inflammatory immune markers, and restored gut dysbiosis in hospitalized COVID-19 patients16, and also alleviated multiple symptoms of Post-acute COVID-19 syndrome (PACS)17. These previous findings suggest using interventions such as gut microbial derivatives to modulate post-vaccine immune responses. However, it remains to be determined whether microbiome modulation with SIM01 could serve as an effective intervention to optimize immune responses following vaccination.
Probiotics are known to modulate the immune system through various mechanisms18,19. However, probiotic engraftment has various challenges, with successful, long-lasting engraftment being intricately associated with the host’s autochthonous gut microbiota. There is nutritional competition between probiotics and the autochthonous gut microbiota, such as competition for carbon sources following niche overlap20. An investigation on one probiotic strain, Bifidobacterium longum AH1206, demonstrated that gut microbiota composition and the absence of specific functional capabilities—particularly the deficiency in genes of carbohydrate utilization—are principal determinants for the probiotic long-term colonization21. There is a lack of extensive prospective investigation specifically targeting high-risk populations to examine the rehabilitation of intestinal microbial ecology with multiple probiotic strains and what determines probiotic colonization.
Based on the Immune Microbiome Product Against COVID infecTion (IMPACT) study, we conducted a post hoc analysis of IMPACT to investigate (1) the impact of the SIM01 probiotic formulation on the gut microbiota and metabolites and how key elements that contribute to the probiotics engraftment, (2) how gut microbiome and metabolites modulated the immunogenicity of COVID-19 vaccines after SIM01 intake in elderly recipients and those with type 2 diabetes. This research aimed to enhance our understanding of how to optimize the immunogenicity in vulnerable populations following vaccination based on the resident microbiome22.
Results
The gut microbiome of subjects receiving SIM01 was more likely to transition towards Bifidobacterium enriched-cluster II
From April 2021 to March 2022, a total of 369 SARS-CoV-2 vaccinees (51.49% females; median age: 67.00 years old) received either SIM01 (189 participants) or placebo (180 participants), and available stool samples were included in this study. There was no significant difference in baseline characteristics between the placebo and SIM01 groups among BNT162b2 vaccinees or CoronaVac vaccinees (Table S1). Study visits were arranged at 1 month, 3 months, and 6 months after completion of the second dose of the COVID-19 vaccine. Shotgun metagenomic sequencing was performed to assess gut microbiota composition in stool samples at baseline and 3 months after the second vaccine dose (postvaccination). Blood samples at 1-month or 6-month postvaccination were subjected to the SARS-CoV-2 surrogate virus neutralization test (sVNT) and spike receptor-binding domain (RBD) IgG ELISA testing. Metabonomic sequencing was performed to assess the gut metabolite profile in fresh stool samples at baseline and 1-month postvaccination (Fig. 1A).
A Study design. Eligible subjects received a gut microbiota-derived synbiotic formula (SIM01) or placebo for 3 months in all subjects aged ≥65 years or with type 2 diabetes mellitus (T2DM). All subjects received the COVID-19 vaccine, including either the mRNA vaccine BNT162b2 (Pfizer-BioNTech) or the inactivated vaccine Sinovac-CoronaVac, within 1 week of intervention. Study visits were arranged at 1-month, 3-month, and 6-month after completion of the second dose of the COVID-19 vaccine. B The Sanky diagram shows the transition of three gut community clusters between baseline and 3-month postvaccination (p.v.) following a 3-months SIM01 intervention in both placebo and SIM01 groups. The width of each flow corresponds to the number of subjects undergoing an intra- or inter-cluster transition. The height of each bar is proportional to the number of subjects in each group. p values were given by the Chi-square test. The first line of p values indicated the overall comparison (transition in three clusters before and after treatment). The second line of p values indicates the subgroup comparison transition between cluster 2 and other clusters (combined C1 and C3). C cluster. C The relative abundance of the Bifidobacterium genus in the samples with distinct gut community clusters. p values were given by the Wilcoxon test (two-sided). D, E The gut microbiome Shannon diversity (D) and the richness of observed species (E) in the samples with distinct gut community clusters. p values were given by the Wilcoxon test (two-sided). Elements on boxplots: center line, median; box limits, upper and lower quartiles; whiskers, 1.5×IQR; points, samples. IQR interquartile range. * indicated p < 0.05, ** indicated p < 0.01, *** indicated p < 0.001, **** indicated p < 0.0001 after adjustment for multiple comparisons.
The enterotypes (clusters) are useful for describing the gut microbial community structure and are linked to health and disease23. Therefore, to investigate the impact of SIM01 on the gut microbiome composition, we checked the gut microbiome cluster at baseline and 3-month postvaccination. The microbial community cluster at the genus-level was performed using the partitioning around medoid (PAM) method, including all samples from the SIM01 and placebo groups. Three clusters were identified, including cluster I dominated by the Bacteroides genus, cluster II enriched by Eubecterium and Bifidobacterium genus, and cluster III dominated by the Prevotella genus (Fig. 1B and Fig. S1A, B), which aligns with the existing enterotype classification23. Overall, SIM01 affected the gut microbiome cluster change before and after treatment (Chi-squared test, p = 0.0419, Fig. 1B), but Placebo did not (Chi-squared test, p = 0.07541). Further, we sub-grouped all samples into cluster 2 and other clusters (combined clusters 1 and 3). Indeed, subjects receiving SIM01 were more likely to transition to cluster II (Chi-squared test, p = 0.0175, Fig. 1B), which was characterized by a higher relative abundance of Bifidobacterium (Fig. 1C) and higher gut microbiome diversity and richness (Fig. 1D, E). Of note, the T2DM subjects had lower gut two Bifidobacterium species (B. longum and B. pseudocatenulatum) at baseline (Fig. S1C), while they had significantly higher B.bifidum after 3 months of SIM01 intervention after adjusting for age and sex (Fig. S1D).
The autochthonous gut microbiota affects the enhancement of SIM01-contained species
Then, we were interested in whether baseline features could affect the enhancement of SIM01-contained species within the SIM01 arm. Interestingly, subjects from cluster I/III at baseline had a significantly enriched SIM01 species at 3-month postvaccination compared to control, but not subjects from cluster II at baseline (Fig. S2A). This result was also confirmed in three individual Bifidobacterium species (Fig. S2B, C, D).
Further, we grouped the subjects within the SIM01 arm according to the fold change of relative abundance of SIM01 species (Increase group: fold change >0, Non-increase group: fold change ≤0, see method details). In particular, the increased group had a lower B. adolescentis at baseline than the non-increase group (Fig. 2A, B), and the increased group did have a higher relative abundance of SIM01 species collectively or separately at 3-month postvaccination (Fig. 2A, B and Fig. S2E, F). Besides, the depletion of baseline bacteria from the Actinomyces genus of the Actinobacteria phylum and the Coprobacillus genus was linked to the enrichment of species contained in SIM01 (Fig. 2C). Moreover, we checked the overlap number between the KEGG Orthology (KO) detected in the baseline samples and the KO encoded by SIM01 strains. Correlation results indicated that the overlap KO number is negatively associated with the fold change of SIM01 species (Fig. 2D, R = −0.18, p = 0.027), which indicates that the functional overlap may play a role in the baseline ecological effect on the SIM01 enhancement, but it is still affected by the incompleteness of the current microbiome function database. This result was also repeated in three individual species (Fig. S2G). Further, we compared the BABBBL_fc between baseline samples with or without specific KO. Specifically, the lack of 26 KOs (out of 857) at baseline was associated with the enhancement of SIM01-contained species (Fig. 2E and Table S2, FDR <0.05), especially KOs of metabolism class (carbohydrate metabolism, glycan biosynthesis and metabolism, amino acid metabolism). In summary, when the allochthonous species colonize a new community, their colonization outcome can vary depending on the resident gut microbiome.
A, B The changes in the sum relative abundance of three Bifidobacterium (A) or B. adolescentis (B) between baseline and 3-month postvaccination (p.v.) after subgrouping based on the increase or non-increase of SIM01-contained species within the SIM01 arm. Non-Increase, N = 34 each time point. Increase, N = 110 at each time point. C The depleted species at baseline in the gut of subjects who were characterized by an increase in SIM01-contained species after 3 months of treatment. Maaslin2 was used for identification after adjusting the gender, age, and T2D status. p < 0.05, FDR <0.25. D Correlation between fold change of SIM01 species and the overlap number of the KO-encoded in SIM01 strains in the baseline samples. Coefficients and p values of the correlations were given by Spearman’s correlation tests. E The heatmap showed the presence and absence of baseline KOs that were associated with the enhancement of SIM01-related species after 3 months of SIM01 intervention. Each row represents the baseline sample of each subject.
The enhancement of the SIM01 species is associated with SARS-CoV-2 vaccine immunogenicity
Next, we would like to test our hypothesis on whether the enhancement of the SIM01 species could enhance SARS-CoV-2 vaccine immunogenicity. Considering that the immune response varies among different types of vaccines24, the following analysis will subgroup according to vaccine type (Table S3). Interestingly, the fold change of SIM01 species was positively correlated with the anti-spike RBD IgG titer at 1-month postvaccination BNT162b2 in the SIM01 arm (R = 0.27, p = 0.019, Fig. 3A) and positively correlated with sVNT% level at 1-month postvaccination BNT162b2 in the SIM01 arm, but not statistically significant (R = 0.23, p = 0.055, Fig. 3B).
A, B The correlation between the fold change of three Bifidobacterium in the gut after 3 months of SIM01 treatment and the anti-spike receptor-binding domain (RBD) (A) or the neutralizing antibody sVNT (%) (B) at 1 month after the second dose of BioNTech was examined using Spearman’s correlation test. C The correlation between the fold change of three Bifidobacterium in the gut after 3 months of SIM01 treatment and the neutralizing antibody sVNT (%) at 6 months after the second dose of BioNTech was examined using Spearman’s correlation test. N = 75. D The correlation between the anti-spike receptor-binding domain (RBD) at 1 month after the second dose of BioNTech and the neutralizing antibody sVNT (%) at 6 months after the second dose of BioNTech was examined using Spearman’s correlation test. Regression lines with 95% CI (orange area) were shown on scatter plots. E Logistic regression based on fold change of individual Bifidobacterium species or a combined model based on fold change of all three Bifidobacterium species adjusting age, gender, and T2D status was used to calculate the odds ratio (OR, 95% Confidence interval) values for the for high (≥60%, n = 32) vs. low sVNT levels (<60%, n = 43) responders among BioNTech (BNT162b2) vaccines at 6 month after second dose within SIM01 arm. Each OR was presented as a dot with a bar showing the 95% CI. p < 0.05 was presented as an orange dot. OR, odds ratio; T2D, type 2 diabetes mellitus; fc fold change. F AUROC (95% CI) values of models based on combined fold change of three species contained in SIM01 for high (≥60%) vs. low sVNT levels (<60%) at 6-month postvaccination adjusting age, gender, and T2D status. p.v., postvaccination. G The volcano plot shows the differential pathway between two groups of subjects with the non-increase or increase SIM01 species in the gut after 3 months of treatment within the SIM01 arm. Maaslin2 was used for identification after adjusting the gender, age, and T2D status. p < 0.05, FDR < 0.25. H Correlations between the fold change of the relative abundance of SIM01-contained three species and the fold change of differential metabolites between baseline and 1-month postvaccination in BioNTech vaccinees. The label within each frame: · indicated p < 0.1, * indicated p < 0.05, ** indicated p < 0.01 based on Spearman correlation analysis. The color indicates the correlation Rho value. I AUROC (95% CI) values of models based on the combined fold change of three species contained in SIM01 and the fold change of three metabolites between baseline and 1-month postvaccination for high (≥60%) vs. low sVNT levels (<60%) at 6-month postvaccination, adjusting age, gender, and T2D status. p.v. postvaccination, T2D type 2 diabetes mellitus.
Considering the SARS-CoV-2 infectious and booster dose of vaccine will affect the immune response24, the subjects infected by SARS-CoV-2 after 3-month postvaccination and before 6-month postvaccination were excluded from the following analysis (n = 19), and whether subjects received a booster dose at 6-month postvaccination was taken into consideration. Notably, the enhancement of SIM01-contained species was positively correlated with sVNT% level at 6-month postvaccination of the second dose of BNT162b2 in the SIM01 arm (Fig. 3C), as well as subjects who received the third dose of BNT162b2 vaccination 6-month postvaccination (Fig. S3A). After subgrouping according to the elderly and type 2 diabetes population, a similar correlation was found in elderly subjects after the second dose of BNT162b2 vaccination, but not in the subjects who received the 3rd dose of BNT162b2 vaccination, which may be related to the limited sample size after subgrouping (Fig. S3B). Besides, the spike in RBD IgG titer at 1-month postvaccination was also positively associated with sVNT% 6-month postvaccination BNT162b2 in the SIM01 arm (Fig. 3D). Importantly, enhancement of SIM01 species could predict sVNT% levels at 6-month postvaccination (>60% or not, which corresponded to twice 50% protection titer25) after the second dose of BNT162b2 vaccination within the SIM01 arm, together with age, sex, and T2DM (p = 0.0378, Fig. 3E). Together with age, sex, and T2DM, enhancement of SIM01 species could predict sVNT% levels at 6-month postvaccination after the second dose of BNT162b2 vaccination within the SIM01 arm with an AUC = 0.802 (p < 0.001, Fig. 3F). Further, we compared the gut microbial functional pathway at 3-month postvaccination between Increase and Non-increase groups based on fold change of relative abundance of SIM01 species within the SIM01 group that received BNT162b2, and four pathways enriched in the SIM01-contained species-increase group, namely Bifidobacterium shunt (P124-PWY), formaldehyde assimilation III dihydroxyacetone cycle (P185-PWY), super pathway of pyrimidine ribonucleosides degradation (PWY-7209), and starch biosynthesis (PWY-622) (Fig. 3G). However, the above patterns were not found in the CoronaVac group (Table S3), which may be due to the limited sample size in the CoronaVac group and the different mechanisms of action of inactivated and mRNA vaccines. Also, similar results were not found in the placebo arm that received BNT162b2 (Table S3), which indicated that the enhancement of SIM01-contained species after intervention correlated with the SARS-CoV-2 vaccine immunogenicity, but not endogenous enrichment of three Bifidobacterium species.
The metabolite change induced by the SIM01 treatment improves the prediction for SARS-CoV-2 vaccine immunogenicity
We further detected the metabolites of available fresh stool samples collected at baseline (n = 276) and 1-month postvaccination (n = 276). A total of 338 metabolites were detected, and 290 metabolites with prevalence >25% were applied for further analysis. First, we separately identified the differential metabolites between baseline and 1-month postvaccination after adjusting for vaccine types within the two arms. There were 24 metabolites that were significantly changed from baseline to 1-month postvaccination after the SIM01 treatment (Table S4), with six overlapping with the placebo group (Fig. S3C and Table S5).
To identify the gut metabolites related to the SIM01 intervention, we further checked the correlation between the fold change of 18 unique metabolites in the SIM01 group (Fig. S3C) and the fold change of the relative abundance of SIM01-contained three species (BABBBL_fc). For CoronaVac vaccinees, one metabolite (Taurocyamine) was identified as positively correlated, and four metabolites (Myo-inositol, L-sorbose, pyridoxal, and ricinoleic acid) were identified as negatively correlated with the BABBBL_fc or fold change of the relative abundance of any SIM01-contained species (Table S6). Notably, three metabolites (N-formylmethionine, benzoic acid, myo-inositol) were identified as positively correlated with the BABBBL_fc or fold change of the relative abundance of any SIM01-contained species in the BNT162b2 vaccinee (Fig. 3H and Table S6). Among them, the fold change of Benzoic acid between baseline and 1-month postvaccination is positively correlated with sVNT% levels at 1-month postvaccination (R = 0.2274, p value = 0.048, Table S7). Although the fold change of these three metabolites between baseline and 1-month postvaccination is not significantly correlated with sVNT% levels at 6-month postvaccination, adding the fold change of these three metabolites in the prediction model could improve the AUC = 0.825 of predicted sVNT% levels at 6-month postvaccination (>60% or not, which corresponded to twice 50% protection titer25) after the second dose of BNT162b2 vaccination within the SIM01 arm (p < 0.001, Fig. 3I). Specifically, benzoic acid ranked in the top 1 among these three metabolites in the prediction model, and a previous study also showed that several Bifidobacteria species were able to convert albiflorin to benzoic acid in vitro26.
The engraftment of the SIM01 strain could be predicted by the baseline gut microbiome
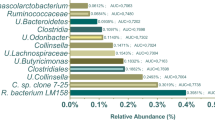
Colonization is key for probiotics to exert sufficient host interaction to confer health benefits. We used StrainPhlAn to evaluate whether the SIM01 strain became dominant after 3 months of intervention based on the pairwise genetic distance (Fig. S4A, see Methods for details). B. adolescentis had the highest engraftment rate (28/144 subjects (19.44%), Fig. 4A, B), followed by B. longum (12/144 subjects (8.33%)) and B. bifidum (7/144 subjects (4.86%), Fig. S4B, C), which echoed the abundance of Bifidobacterium species in the adult gut reported previously27. The subjects with any SIM01 strain that successfully became the dominant strain were consistently characterized by significantly higher fold change of three SIM01-contained species (p < 0.01, Fig. 4C). Also, the benzoic acid was significantly higher in BNT162b2 vaccinees with any SIM01 strain than those with non-SIM01 bifidobacteria species (Fig. S5A).
A Phylogenetic tree of dominant haplotypes of B. adolescentis per sample. B Subset of the phylogenetic tree of dominant haplotypes of B. adolescentis of the samples with SIM01 B. adolescentis strain as the dominant strain after 3 months of treatment. Orange circles and text represent the reference genomes of the SIM01 B. adolescentis strain. C The fold change of relative abundance of SIM01-contained three species in three groups of subjects (None: without any Bifidobacterium species contained in SIM01 that involved in the StrainPhlAn construction, None SIM01 strain: with Bifidobacterium species involved in the StrainPhlAn construction but not the same as the SIM01 strain, Any SIM01 strain: with at least one Bifidobacterium strain contained in SIM01 that involved in the StrainPhlAn construction). p values were given by the Wilcoxon test (two-sided). Points, samples. Elements on boxplots: center line, median; box limits, upper and lower quartiles; whiskers, 1.5×IQR. D AUROC (95% CI) values of models about SIM01 strain engraftment based on baseline differential gut microbial species. E The variable importance of features in the prediction model. F Correlation between the relative abundance of baseline SIM01-contained three Bifidobacterium species with the relative abundance of Anaerostipes hadrus. Coefficients and p values of the correlations were given by Spearman’s correlation tests.
To precisely predict the SIM01 colonization based on the baseline microbial community, we first used Maaslin2 to identify the species associated with the engraftment of any SIM01 strain (Table S8). Based on the 22 species identified, the random forest was employed for the classification prediction model with an AUC = 0.873 (Fig. 4D). The variable importance is shown in Fig. 4E, with the baseline B. adolescentis ranked fifth with a negative impact on the SIM01 strain colonization. The top one species that negatively impacted the SIM01 strain colonization is Anaerostipes hadrus, which indicated the availability of Bifidobacterium species at baseline (Fig. 4F). Anaerostipes spp., butyrate-producers, could be cross-fed by the metabolites of Bifidobacterium spp in the infant's gut28. High relative abundance of baseline gut Clostridium bolteae, Clostridium bolteae CAG 59, and Clostridium symbiosum was associated with any SIM01 strain colonization. Therefore, the colonization potential of probiotics has been attributed to strain properties and is more permissive to certain individuals, which is implicated with the baseline microbial community.
Discussion
This research investigated the impact of the SIM01, a gut microbiota-derived synbiotic formula, on the gut microbiota and metabolites, as well as its correlation with the immunogenicity of COVID-19 vaccines in elderly recipients and those with type 2 diabetes. The study identified a correlation between baseline levels of specific gut bacterial species and the engraftment of SIM01-contained strains, implying that the intrinsic characteristics of the host’s autochthonous gut microbiota could influence the colonization efficacy of SIM01. Furthermore, the research suggested the augmentation of vaccine immunogenicity predicated on the gut microbial community profile and metabolites, offering novel insights for personalized vaccine adjuvant selection and the optimization of vaccine efficacy in vulnerable populations.
The influence of the autochthonous gut microbiota on the colonization of introduced bacterial strains is evidenced by (1) the subjects with baseline gut microbiome cluster II (high relative abundance Bifidobacterium genus) were implicated with lower enhancement of SIM01-contained species, (2) the association between lower levels of B. adolescentis and less carbohydrate metabolism function in the resident microbiome and enrichment of SIM01 species, (3) the predictable engraftment of SIM01 strain based on baseline gut microbiome. Specifically, Anaerostipes spp., butyrate-producers and could be cross-fed by the metabolites of Bifidobacterium spp. in infants’ gut28, were positively correlated with the resident Bifidobacterium spp., which might indicate an occupied niche (resource requirement overlap between allochthonous probiotic and autochthonous microbiota is high)29. This finding aligns with a previous study where lower pretreatment levels of Bifidobacterium longum in the gut microbiota were predictive of the B. longum AH1206 persistence21. Gut-resident bacteria adapt to specific niches by engaging in intricate competitive or cooperative interactions with other microbes30,31. These interactions regulate microbial community structure and restrict colonization by alien microbes32. For instance, sequential administration of identical bacterial strains to germ-free mice results in the first strain occupying the niche exclusively, while the subsequent strain cannot establish itself33. As stated in “The Origin of Species“34, it posits that introduced species have a greater likelihood of thriving in environments devoid of their close phylogenetic relatives. Besides, the association between high relative abundance of gut baseline Clostridium bolteae, C. symbiosum, and SIM01 later colonization may reflect metabolic synergy, as these species produce acetate35 and modulate bile acids36, which may facilitate engraftment. However, as C. bolteae is also implicated in dysbiosis, its role may depend on the ecological context and might reflect the vulnerability of the population37. Taken together, the diversity of the autochthonous gut microbiota (resident gut microbiome) can predict the colonization success of the allochthonous probiotic strain, which helps us better understand the relative niche and fitness difference.
The sVNT% level is a parameter commonly employed to assess the efficacy of vaccine-induced immune response. This study utilized the fold change of baseline and 3-month postvaccination SIM01 species to predict the sVNT level at 6-month postvaccination, which indicates the potential adjuvant effect of synbiotics on immune responses. Consistently, previous studies showed that Bifidobacterium species can influence postvaccination immune responses. In elderly individuals with a mean age of 86.7 years, Bifidobacterium longum BB536 appears to augment innate immunity, as its continuous intake before and after influenza vaccination correlated with reduced fever and influenza rates postvaccination38. In infants, Bifidobacterium longum subspecies infantis has been associated with improved humoral and T cell responses to Bacillus Calmette–Guérin, polio, and tetanus vaccines39. Animal models also indicate that Bifidobacterium animalis ssp. lactis (BB-12) boosts immune responses following seasonal influenza vaccination40.
Compared to the placebo group, subjects receiving SIM01 were more likely to transition to cluster II from baseline to 3-month postvaccination. Notably, in the placebo group, the endogenous enrichment of three Bifidobacterium species induced by the placebo did not correlate with the sVNT level at 6-month postvaccination, suggesting that the host had developed immune tolerance to the Bifidobacterium species. In contrast, the allochthonous enrichment of three Bifidobacterium species included by SIM01 was more effective in subjects who were not characterized by cluster II (which displays a high relative abundance of the Bifidobacterium genus) at baseline, and thus, the immune response facilitated the immunogenicity after elderly and diabetes patients received BNT162b2 vaccination.
Compared with the gut microbial pathways of the Non-increase group based on the fold change of relative abundance of SIM01 species at 3-month postvaccination, starch biosynthesis (PWY-622) was enriched in the SIM01 species-increase group, which may benefit other probiotics’ growth. According to an in vitro study, B. adolescentis 22 L has cross-feeding relationships with B. bifidum PRL2010, which promotes the growth and survival rate of the latter, possibly through sugars released from starch degradation41. In addition, B. bifidum PRL2010 specifically works for the extracellular breakdown of host-glycans that will again support the growth of other members of the Bifidobacterium bacterial community through simple sugars42. These may indicate that SIM01 partially plays a role that relies on interactions between bacterial species. Gut microbiota could exert diverse effects on immune function through direct interaction with immune cells in the gut and indirect mechanisms such as secreting metabolites and regulating the systemic availability of critical metabolites43. Notably, we identified that the fold change of benzoic acid (positively correlated with the fold change of SIM01-contained species) between baseline and 1-month postvaccination is also positively correlated with the sVNT% levels at 1-month postvaccination. Several Bifidobacteria species were able to convert albiflorin to benzoic acid in vitro based on a previous report26. And gut bacteria-derived benzoic acid can be absorbed into the bloodstream from the gut44. A previous study showed that benzoic acid enhances the intestinal expression of the polymeric immunoglobulin receptor, B-cell activating factor from the TNF family, and activation-induced cytidine deaminase (AID), thereby enhancing IgA production by B-cells in chickens45. Benzoic acid derivatives have been reported to possess anti-influenza virus activities and immune-modulatory effects46. The evidence underscores the potential of benzoic acid to bolster immune functions and partially explains why it is relevant to vaccine immune response. Therefore, the SIM01 may modulate the immune response through direct interaction with the gut community and indirect mechanisms such as secreting metabolites.
There are several strengths in our study. First, this study highlights the unique SARS-CoV-2 vaccinee characteristics of the population in Hong Kong, China. It examines participants who received either inactivated vaccines or mRNA-based SARS-CoV-2 vaccines, while mainland China’s predominant use of inactivated SARS-CoV-2 vaccines47. Secondly, the randomized controlled trial setting facilitates understanding of the enhancement of endogenous and allochthonous Bifidobacterium species. Thirdly, the whole-genome sequencing of three SIM01 Strains and the metagenomic sequence of stool samples collected from the subjects who received SIM01 for 3 months allowed us to check the engraftment of probiotics with multiple strains.
However, there are also some limitations. First, COVID-19 infection along the subject’s follow-up makes it hard to track long-term vaccine-induced-sVNT, which restricts the understanding of the prolonged effects of SIM01. As we know, vaccine antibody levels decline over time. Admittedly, during the COVID-19 pandemic, achieving perfect synchronization between gut microbiome sampling (stool collection) and immune profiling (blood sampling) was challenging. In our study, our results showed that the fold change of SIM01 species was positively correlated with both the immune index at 1-month postvaccination BNT162b2 and 6-month postvaccination of the 2nd dose of BNT162b2, which covered the time point when the gut metagenomic sequence was performed. Secondly, due to the deficiency of fresh stool at 3-month postvaccination, we can only detect the gut metabolites at 1-month postvaccination as a proxy to reflect the metabolism profile change induced by SIM01 treatment, but still, we found some metabolites change corresponding to Bifidobacterium species that with biological meaning. Besides, it would be hard to conclude that probiotic colonization depends on functional redundancy in the autochthonous gut microbiota based on a bioinformatic analysis only, since the complexities of microbiome functionality and the current limitations in existing pathway databases48. It is worthwhile to test out specific strains in vitro, ex vivo, and vivo in further studies, such as using co-culture systems to assess how different strains of probiotics interact with existing gut microbiota under controlled conditions (with or without strain utilized the specific carbohydrates e.g. oligosaccharides)49 and conducting studies using animal models to evaluate how the existing microbiota affect colonize of different probiotic strains50. In addition, previous studies showed that Bifidobacteria intervention could improve other types of vaccine immune response, such as the Bacillus Calmette–Guérin vaccine51 and 13-valent pneumococcal conjugate vaccine52. Therefore, further animal experimental and in vitro studies are necessary to establish causality and the mechanism between the Bifidobacteria or metabolites and enhanced COVID-19 vaccine immunogenicity. Last but not least, the lack of different population generalizations is another limitation; to address this, it would be beneficial to establish multiple testing sites across various regions, enabling the observation of microbial variations in a diverse racial demographic. Such an approach would enhance the generalizability of the findings and support further validation.
In summary, compared to the endogenous enrichment of three Bifidobacterium species induced by the placebo, the allochthonous enrichment of three Bifidobacterium species included by the 3 months treatment of SIM01 was associated with elevated gut benzoic acid levels and the immunogenicity of SARS-CoV-2 BNT162b2 vaccines. Besides, SIM01 engraftment was influenced by baseline gut microbiota. These findings underscore the importance of probiotics as personalized vaccine adjuvant selection and the optimization of vaccine efficacy in vulnerable populations.
Methods
Study design, participants
This study was part of a randomized clinical trial53, where the primary outcome was a composite of adverse health outcomes. Eligible subjects received a gut microbiota-derived synbiotic formula (SIM01) or placebo for 3 months in all subjects aged ≥65 years or with type 2 diabetes mellitus (T2DM). Subjects were randomized at the time of COVID-19 vaccination to reduce the confounding effects of vaccination on health outcomes. All subjects received the COVID-19 vaccine, including either the mRNA vaccine BNT162b2 (Pfizer-BioNTech) or the inactivated vaccine Sinovac-CoronaVac, within one week of intervention. Study visits were arranged at 1-month, 3-month, and 6-month after completion of the second dose of the COVID-19 vaccine (Fig. 1A). SIM01 is an oral microencapsulated formulation of three lyophilized Bifidobacteria at a dose of 20 billion colony-forming units (CFU) per day and 3 prebiotics, including galactooligosaccharides, xylooligosaccharide, and resistant dextrin, as derived from our previous study54,55. The three Bifidobacterium strains (B. adolescentis; B. bididum, and B. longum) are commercially available from Chambio Co., Ltd. and WECARE-PROBIOTICS. SIM01 has been approved by health authorities and is a patent-protected formula.
Further, a total of 376 subjects with available stool samples were screened out. Based on the inclusion criteria (e.g., without COVID-19 infection before 3-month postvaccination, received SARS-CoV-2 vaccine), 369 participants (SIM01, N = 189, Placebo, N = 180) were finally included in the study. Among them, 280 participants (SIM01, N = 144, Placebo, N = 136) with 560 stool samples with stool nucleic acid preservatives (Norgen, Cat#28330) were collected at both baseline and 3-month post the second dose of vaccine were applied for the metagenomic sequence. Besides, 276 participants (SIM01, N = 144, Placebo, N = 132) with 552 fresh stool samples collected at both baseline and 1-month post the second dose of vaccine were applied for the metabonomic sequence. This study was performed in the general population of Hong Kong from April 2021 to March 2022. The study was approved by the Clinical Research Ethics Committee of the Chinese University of Hong Kong on 19 April 2021 (Ref. No. 2021.186). It was registered on ClinicalTrials.gov (NCT04884776). This study was conducted according to the Declaration of Helsinki and ICH-GCP principles. All subjects provided informed consent.
Stool metagenomic sequencing and taxonomy, and function profile
Fecal samples were collected at baseline and 3-month postvaccination. We performed metagenomic profiling on fecal samples as previously described.15,53 Briefly, fecal DNA was extracted using Maxwell® RSC PureFood GMO and Authentication Kit (Promega, Madison, Wisconsin) following the manufacturer’s instructions. Sequencing libraries were prepared from extracted DNA using the Illumina DNA Prep kit, and sequenced with a paired-end 150 bp sequencing strategy by Illumina NovaSeq 6000 System. The raw sequence data generated 5.945 Gb [5.312-6.946] (median [IQR]) sequence depth per sample. Further, raw sequence reads were filtered and quality-trimmed using Trimmomatic v0.39 and decontaminated against the human genome (Reference: hg37dec_v0) by Kneaddata (V. 0.10.0, https://bitbucket.org/biobakery/kneaddata/wiki/Home). MetaPhlAn3 (v 3.0.13) was used to generate a species-level abundance table. To annotate the function of gut microbiome genes, we applied HUMAnN3 (3.0.0) to all metagenomic samples after filtering out reads mapping to the human reference. Moreover, the UniRef gene families that were detected by HUMAnN3 were mapped to KEGG Orthogroups (KOs) using the humann_regroup_table function, and the abundances of KOs were normalized using the humann_renorm_table function.
Stool metabolomic sequencing
Fresh stool metabolomes were profiled by liquid chromatography-tandem mass spectrometry (LC-MS/MS) using Waters UPLC I-Class Plus (Waters, USA) equipped with QTRAP 6500 Plus (SCIEX, USA). A high-throughput targeted quantification for a metabolites panel (HM700 Metabolome) can realize the absolute quantification of more than 700 metabolite small molecules, including amino acids, organic acids, fatty acids, sugars, bile acids, carnitine, phenyl or benzyl derivatives, indoles, etc.
Partitioning around the medoid for the microbial cluster
The microbial community cluster at the genus-level was performed according to a published protocol (https://enterotype.embl.de/enterotypes.html) with the partitioning around medoid (PAM) method, including samples from SIM01 and placebo groups. The optimal number of clusters was chosen based on the Calinski–Harabasz (CH) Index, which shows the performance in recovering the number of clusters.
The KEGG ortholog (KO) annotation of the SIM01 strain
The whole-genome sequencing (WGS) of three SIM01 strains was performed. Bacterial genomes were assembled using MEGAHIT (v1.2.9)56. Prodigal (V2.6.3) was used to predict reliable protein-coding genes57. Further, the protein profiling was searched against the curated KOs database using KOfamscan58.
Blood samples sVNT and measurements
Blood samples at baseline, 1-month postvaccination or 6-month postvaccination were subjected to a SARS-CoV-2 surrogate virus neutralization test (sVNT) (GenScript, NJ, USA, Catalog No. L00847-A). Spike receptor-binding domain (RBD) IgG ELISA was used to assess antibody levels in plasma collected at baseline and 1-month postvaccination and carried out as previously described59,60. sVNT data was expressed as percentage inhibition (%).
Strain engagement check use StrainPhlAn
The SIM01 strain engagement check was based on StrainPhlAn and followed the instructions (https://github.com/biobakery/MetaPhlAn/wiki/Strain-Sharing-Inference). Briefly, the genomes of three SIM01 strains obtained via whole-genome sequencing and metagenomic samples of the SIM01 arm were employed for the StrainPhlAn phylogenetic tree construction and strain-level profiling. The pairwise phylogenetic normalized genetic distance (nGD) distribution of the same or different individuals was checked. Youden’s index was used to set the species-specific strain identity thresholds. The nGD between the SIM01 strain and the metagenomic samples at 3-month postvaccination within each species was compared with the corresponding thresholds to decide whether it was a successful engraftment in the gut microbiome. The “tree_subset” was used to subset a tree by the node of the SIM01 strain and return all related nodes within a selected number of levels.
Statistical analysis
Continuous variables were expressed in median (±interquartile range, IQR), while categorical variables were presented as percentages. Changes in continuous variables, including the quantities of bacteria, were compared by the Wilcoxon rank-sum test, whereas changes in categorical variables were compared using the Chi-square test or Fisher’s exact test. A two-sided p value of <5% was considered statistically significant. Alpha microbial diversity was studied using the observer species richness index and the Shannon diversity index based on the species-level profile for each sample. Maaslin2 was used to identify the baseline species associated with T2DM, age, and sex. The significance threshold for these analyses was a false discovery rate (FDR)-corrected p value (q value) of 0.25.
The fold change of the relative abundance of SIM01-contained three species was calculated based on the sum fold change of the relative abundance of SIM01-contained three individual species.
Fold change = Log10 (Relative abundance of one species at 3-month postvaccination/Relative abundance of one species at baseline)
Fold change of SIM01 species = Fold change (Bifidobacterium adolescentis) + Fold change (Bifidobacterium bifidum) + Fold change (Bifidobacterium longum)
Maaslin2 was used to identify the baseline features or 3-month postvaccination functional pathway associated with the fold change of SIM01 species (Increase group: fold change >0, Non-increase group: fold change ≤0). The correlations were analysed using Spearman’s correlation tests. In the analysis of the metabolites, only metabolites present in more than 25% of samples were included. Maaslin2 was used to identify the differential metabolites between baseline and 1-month postvaccination after adjusting the vaccine type within the two arms, separately. The fold change of metabolites between baselines and 1-month postvaccination was calculated similarly to the fold change of the relative abundance of SIM01-contained three individual species. The logistic regression was used to predict whether the fold change of SIM01 species (or add the fold change of identified metabolites) could classify sVNT(%) at 6-month postvaccination second dose of BNT162b2 > 60% or not with generalized linear regression modeling (GLM) together with age, sex, and T2DM. The area under the ROC Curve (AUC) was obtained via pROC.
Random forest was employed to classify any engraftment of the SIM01 strain. Each data frame was separated into a 70% testing set and a 30% training set. And performed five times cross-validation and repeated ten times in the random forest model. The default parameters of “mtry” were adopted, and the number of trees was 500. The “set.seed” was 100 to ensure reproducibility of results. The area under the receiver operating characteristic curve (AUROC) was calculated to check the model’s performance. The top important variables were defined based on the beta-IncNodepurity from the random forest model (v.4.7-1.1). False discovery rate (FDR) correction was applied for multiple tests. Analyses where FDR correction was not applicable included binary analysis of demographics, GLM, correlations between fold change of SIM01 species (or fold change of metabolites) and immune markers, and Wilcoxon’s tests of features' relative abundance. FDR correction was not applicable because these analyses did not include multiple testing, were based on a priori hypotheses, or had several metrics (multivariable and univariable tests) for marker identification.
All microbiome-related statistical tests were performed with R Statistics version 4.1.3 with the following packages: phyloseq, vegan, tidyverse, dplyr, ggplot2, Maaslin2, random Forest, pROC, and ggpubr.
Data availability
Quality-controlled and human DNA-removed sequence data have been deposited into the NCBI Sequence Read Archive database under BioProjects PRJNA1181778. According to our institutional data sharing policy, requests for data sharing can be submitted with a written proposal as a part of a collaboration effort. The proposal should detail the intended use of the data. The data management team composed of scientists and clinicians will review these requests based on scientific merit and ethical considerations, including patient consent, to avoid any misuse or misinterpretation. Data sharing will be undertaken if the proposed projects have a sound scientific rationale or potential patient benefit. Data recipients are required to enter formal data sharing agreement, which describes the conditions for release and requirements for data transfer, storage, archiving, publication, and intellectual property. Since the data management meeting is held monthly, please anticipate a response within two working months.
Code availability
This paper does not generate new code.
References
Dallavalasa, S. et al. COVID-19: diabetes perspective-pathophysiology and management. Pathogens 12, 184 (2023).
Hartmann-Boyce, J. et al. Risks of and from SARS-CoV-2 infection and COVID-19 in people with diabetes: a systematic review of reviews. Diabetes Care 44, 2790–2811 (2021).
Martín-Sánchez, F. J. et al. Clinical presentation and outcome across age categories among patients with COVID-19 admitted to a Spanish Emergency Department. Eur. Geriatr. Med. 11, 829–841 (2020).
Singh, A. K. & Khunti, K. Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: a narrative review. Diabetes Res. Clin. Pr. 165, 108266 (2020).
Chawla, U., Kashyap, M. K. & Husain, A. Aging and diabetes drive the COVID-19 forwards; unveiling nature and existing therapies for the treatment. Mol. Cell Biochem. 476, 3911–3922 (2021).
Farshbafnadi, M., Kamali Zonouzi, S., Sabahi, M., Dolatshahi, M. & Aarabi, M. H. Aging & COVID-19 susceptibility, disease severity, and clinical outcomes: the role of entangled risk factors. Exp. Gerontol. 154, 111507 (2021).
Shim, H. W. et al. Analysis of factors affecting neutralizing antibody production after COVID-19 vaccination using newly developed rapid point-of-care test. Diagnostics12, 1924 (2022).
Rangsrisaeneepitak, V., Porntharukchareon, T., Dechates, B., Sirisreetreerux, S. & Tawinprai, K. Antibody levels in people with diabetes after one dose of the ChAdOx1 nCoV-19 (AZD1222) vaccine. Diabetol. Int. 13, 637–643 (2022).
Lustig, Y. et al. BNT162b2 COVID-19 vaccine and correlates of humoral immune responses and dynamics: a prospective, single-centre, longitudinal cohort study in health-care workers. Lancet Respir. Med. 9, 999–1009 (2021).
Karamese, M. & Tutuncu, E. E. The effectiveness of inactivated SARS-CoV-2 vaccine (CoronaVac) on antibody response in participants aged 65 years and older. J. Med. Virol. 94, 173–177 (2022).
Duraisingham, S. S. et al. Systems biology of vaccination in the elderly. Curr. Top. Microbiol. Immunol. 363, 117–142 (2013).
Atwah, B. et al. Susceptibility of diabetic patients to COVID-19 infections: clinico-hematological and complications analysis. Vaccines11, 561 (2023).
Bull, M. J. & Plummer, N. T. Part 1: The human gut microbiome in health and disease. Integr. Med.13, 17–22 (2014).
Peng, Y. et al. Baseline gut microbiota and metabolome predict durable immunogenicity to SARS-CoV-2 vaccines. Signal Transduct. Target Ther. 8, 373 (2023).
Ng, S. C. et al. Gut microbiota composition is associated with SARS-CoV-2 vaccine immunogenicity and adverse events. Gut 71, 1106–1116 (2022).
Zhang, L. et al. Gut microbiota-derived synbiotic formula (SIM01) as a novel adjuvant therapy for COVID-19: an open-label pilot study. J. Gastroenterol. Hepatol. 37, 823–831 (2022).
Lau, R. I. et al. A synbiotic preparation (SIM01) for post-acute COVID-19 syndrome in Hong Kong (RECOVERY): a randomised, double-blind, placebo-controlled trial. Lancet Infect. Dis. 24, 256–265 (2024).
Garcia-Gutierrez, E., Mayer, M. J., Cotter, P. D. & Narbad, A. Gut microbiota as a source of novel antimicrobials. Gut Microbes 10, 1–21 (2019).
Lambring, C. B. et al. Impact of the microbiome on the immune system. Crit. Rev. Immunol. 39, 313–328 (2019).
Ma, C. et al. Probiotic consumption influences universal adaptive mutations in indigenous human and mouse gut microbiota. Commun. Biol. 4, 1198 (2021).
Maldonado-Gomez, M. X. et al. Stable engraftment of Bifidobacterium longum AH1206 in the human gut depends on individualized features of the resident microbiome. Cell Host Microbe 20, 515–526 (2016).
Wu, Z. et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy adults aged 60 years and older: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 21, 803–812 (2021).
Costea, P. I. et al. Enterotypes in the landscape of gut microbial community composition. Nat. Microbiol. 3, 8–16 (2018).
Fong, C. H. et al. Effect of vaccine booster, vaccine type, and hybrid immunity on humoral and cellular immunity against SARS-CoV-2 ancestral strain and Omicron variant sublineages BA.2 and BA.5 among older adults with comorbidities: a cross sectional study. EBioMedicine 88, 104446 (2023).
Lau, E. H. et al. Long-term persistence of SARS-CoV-2 neutralizing antibody responses after infection and estimates of the duration of protection. EClinicalMedicine 41, 101174 (2021).
Peng, R. et al. Esterases from Bifidobacteria exhibit the conversion of albiflorin in gut microbiota. Front. Microbiol. 13, 880118 (2022).
Lu, J. et al. Population-level variation in gut bifidobacterial composition and association with geography, age, ethnicity, and staple food. NPJ Biofilms Microbiomes 9, 98 (2023).
Chia, L. W. et al. Cross-feeding between Bifidobacterium infantis and Anaerostipes caccae on lactose and human milk oligosaccharides. Benef. Microbes 12, 69–83 (2021).
Ojima, M. N. et al. Ecological and molecular perspectives on responders and non-responders to probiotics and prebiotics. Curr. Opin. Biotechnol. 73, 108–120 (2022).
Kamada, N., Chen, G. Y., Inohara, N. & Nunez, G. Control of pathogens and pathobionts by the gut microbiota. Nat. Immunol. 14, 685–690 (2013).
Caballero-Flores, G., Pickard, J. M. & Nunez, G. Microbiota-mediated colonization resistance: mechanisms and regulation. Nat. Rev. Microbiol. 21, 347–360 (2023).
Clemente, J. C., Ursell, L. K., Parfrey, L. W. & Knight, R. The impact of the gut microbiota on human health: an integrative view. Cell 148, 1258–1270 (2012).
Lee, S. M. et al. Bacterial colonization factors control specificity and stability of the gut microbiota. Nature 501, 426–429 (2013).
Darwin, C. D. in The Life and Letters of Charles Darwin, Including an Autobiographical Chapter (ed. Darwin, F.) (John Murray, 1888).
Song, Y. et al. Clostridium bolteae sp. nov., isolated from human sources. Syst. Appl Microbiol. 26, 84–89 (2003).
Liu, H. et al. Gut microbiota from coronary artery disease patients contributes to vascular dysfunction in mice by regulating bile acid metabolism and immune activation. J. Transl. Med. 18, 382 (2020).
Pandit, L. et al. Clostridium bolteae is elevated in neuromyelitis optica spectrum disorder in India and shares sequence similarity with AQP4. Neurol. Neuroimmunol. Neuroinflamm. 8, e907 (2021).
Namba, K., Hatano, M., Yaeshima, T., Takase, M. & Suzuki, K. Effects of Bifidobacterium longum BB536 administration on influenza infection, influenza vaccine antibody titer, and cell-mediated immunity in the elderly. Biosci. Biotechnol. Biochem. 74, 939–945 (2010).
Huda, M. N. et al. Stool microbiota and vaccine responses of infants. Pediatrics 134, e362–e372 (2014).
Rizzardini, G. et al. Evaluation of the immune benefits of two probiotic strains Bifidobacterium animalis ssp. lactis, BB-12(R) and Lactobacillus paracasei ssp. paracasei, L. casei 431(R) in an influenza vaccination model: a randomised, double-blind, placebo-controlled study. Br. J. Nutr. 107, 876–884 (2012).
Turroni, F. et al. Glycan cross-feeding activities between bifidobacteria under in vitro conditions. Front. Microbiol. 6, 1030 (2015).
Turroni, F. et al. Deciphering bifidobacterial-mediated metabolic interactions and their impact on gut microbiota by a multi-omics approach. ISME J. 10, 1656–1668 (2016).
de Jong, S. E., Olin, A. & Pulendran, B. The impact of the microbiome on immunity to vaccination in humans. Cell Host Microbe 28, 169–179 (2020).
Yu, J. B. et al. Gut microbiota-based pharmacokinetics and the antidepressant mechanism of paeoniflorin. Front. Pharm. 10, 268 (2019).
Jia, J., Liu, R., Tang, R., Lin, J. & Yang, Q. Benzoic acid potentiates intestinal IgA response in broiler chickens against Salmonella enterica Serovar Typhimurium infection. Poult. Sci. 103, 104505 (2024).
Guo, M. et al. Antiviral activity of benzoic acid derivative NC-5 against influenza A virus and its neuraminidase inhibition. Int. J. Mol. Sci. 20, 6261 (2019).
Mallapaty, S. China’s COVID vaccines have been crucial - now immunity is waning. Nature 598, 398–399 (2021).
Walker, A. W. & Hoyles, L. Human microbiome myths and misconceptions. Nat. Microbiol. 8, 1392–1396 (2023).
Ojima, M. N. et al. Priority effects shape the structure of infant-type Bifidobacterium communities on human milk oligosaccharides. ISME J. 16, 2265–2279 (2022).
Xiao, Y., Zhao, J., Zhang, H., Zhai, Q. & Chen, W. Mining Lactobacillus and Bifidobacterium for organisms with long-term gut colonization potential. Clin. Nutr. 39, 1315–1323 (2020).
Nyangahu, D. D. et al. Bifidobacterium infantis associates with T cell immunity in human infants and is sufficient to enhance antigen-specific T cells in mice. Sci. Adv. 9, eade1370 (2023).
Ryan, F. J. et al. Bifidobacteria support optimal infant vaccine responses. Nature 641, 456–464 (2025).
Wong, M. C. S. et al. Effects of gut microbiome modulation on reducing adverse health outcomes among elderly and diabetes patients during the COVID-19 pandemic: a randomised, double-blind, placebo-controlled trial (IMPACT Study). Nutrients 15, 1982 (2023).
Zuo, T. et al. Alterations in gut microbiota of patients with COVID-19 during time of hospitalization. Gastroenterology 159, 944–955 (2020). e948.
Yeoh, Y. K. et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut 70, 698–706 (2021).
Li, D. et al. MEGAHIT v1.0: A fast and scalable metagenome assembler driven by advanced methodologies and community practices. Methods 102, 3–11 (2016).
Hyatt, D. et al. Prodigal: prokaryotic gene recognition and translation initiation site identification. BMC Bioinformatics 11, 119 (2010).
Aramaki, T. et al. KofamKOALA: KEGG ortholog assignment based on profile HMM and adaptive score threshold. Bioinformatics 36, 2251–2252 (2020).
Perera, R. A. et al. Serological assays for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), March 2020. Euro Surveill 25, 2000421 (2020).
Perera, R. et al. Evaluation of a SARS-CoV-2 surrogate virus neutralization test for detection of antibody in human, canine, cat, and hamster sera. J. Clin. Microbiol 59, e02504-20 (2021).
Acknowledgements
This study was supported by the Health Bureau, the Government of the Hong Kong Special Administrative Region (M.C.S.W., Funding number: Ref.: COVID19F07). We would like to acknowledge InnoHK (F.K.L.C. and S.C.N.), the Government of Hong Kong, Special Administrative Region of the People’s Republic of China, The D. H. Chen Foundation (F.K.L.C. and S.C.N.), the New Cornerstone Science Foundation (grant no. NCI202346) through the New Cornerstone Investigator Program (S.C.N.), the Croucher Senior Medical Research Fellowship (S.C.N.). We would like to thank all the study participants for providing samples and devoting their time to our study, the CUHK Prince of Wales Hospital nursing staff, CU-Med Biobank, and Clinical Research Support Office and Department of Health, The Government of the Hong Kong Special Administrative Region, China. We would like to thank Dr. Yingzhi Liu for the statistics review. We would like to thank Lok Cheung Alan Chu, Yat Kwong Ranger Ng, Sophie Maria Dixon, Hoi Ting Krystal Lee, Pang Hoi Victor Man from the Central Biobank Team members for samples handling, processing, and quality control, Yee Ching Crystal Wong for metagenomic sequencing. Authors affiliated with MagIC are partially supported by InnoHK, the Government of Hong Kong, Special Administrative Region of the People’s Republic of China. This research has been conducted using the CU-Med Biobank Resource under request ID R20241047, ‘R20211003’, ‘R20221006’ and ‘R20221010’.
Author information
Authors and Affiliations
Contributions
S.C.N., F.K.L.C., L.Z., and S.W. conceived and designed the study. M.C.S.W., J.W.Y.M., O.L.C., and Y.T.F. were responsible for patient recruitment and acquired clinical data. J.Y.L.C. and P.K.C. executed clinical protocols. S.W. carried out the metagenomic and metabonomic analysis as well as statistical analyses. S.W., L.Z., and B.H. wrote the manuscript with input from all coauthors. All authors critically reviewed and approved the final version. All authors had full access to all the data in the study and accept the responsibility to submit it for publication. J.Y.L.C. and P.K.C. monitored the data while M.C.S.W., J.H., O.L.C., and Y.T.F. accessed and verified the data. C.C. supervised biobanking, and S.Y. performed metagenomic sequencing. F.K.L.C. and S.C.N. had final responsibility for the decision to submit for publication and are the guarantors of the study. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
F.K.L.C serves as the Principal Investigator for the Faecal Microbiota Transplantation Service under the Hospital Authority (HA). He is a Board Director of EHealth Plus Digital Technology Ltd., an HA-owned subsidiary driving the eHealth+ programme to transform the Electronic Health Record Sharing System into a comprehensive digital healthcare platform and advance other IT initiatives within the eHealth ecosystem. Additionally, he is a Board Director of CUHK Medical Services Limited. F.K.L.C is a shareholder of GenieBiome Holdings Limited and the co-founder, non-executive Board Chairman, and non-executive Scientific Advisor of its wholly owned subsidiary, GenieBiome Ltd. Similarly, he is a shareholder of MicroSigX Diagnostic Holding Limited and the co-founder, non-executive Board Chairman, and non-executive Scientific Advisor of its wholly owned subsidiary, MicroSigX Biotech Diagnostic Limited. He also serves as a Director of the Hong Kong Investment Corporation Limited and a member of the Steering Committee for the RAISe+ Scheme under the Innovation and Technology Commission. Furthermore, he is the Co-Director of the Microbiota I-Center (MagIC) Ltd. F.K.L.C receives advisory fees and speaker honoraria from AstraZeneca and Comvita New Zealand Limited, as well as patent royalties through affiliated institutions for microbiome-related applications. S.C.N. has served as an advisory board member for Pfizer, Ferring, Janssen, and Abbvie and received honoraria as a speaker for Ferring, Tillotts, Menarini, Janssen, Abbvie, and Takeda. She has received research grants through her affiliated institutions from Olympus, Ferring, and AbbVie, and is a founder member of GenieBiome Ltd, is a shareholder of GenieBiome Holdings Limited; GenieBiome Limited is wholly owned by GenieBiome Holdings Limited; is a non-executive Board director and non-executive scientific advisor of GenieBiome Ltd and its holding company which is non-remunerative; is a founder member of MicroSigX Biotech Diagnostic Limited; is a shareholder of MicroSigX Diagnostic Holdings Limited; GenieBiome Limited is wholly owned by GenieBiome Holdings Limited; is a non-executive Board director and non-executive scientific advisor of MicroSigX Biotech Diagnostic Limited and its holding company which is non-remunerative; and receives patent royalties through her affiliated institutions. F.K.L.C., S.C.N., and L.Z. are named inventors of patent applications held by the CUHK and MagIC that cover the therapeutic and diagnostic use of the microbiome. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, L., Wang, S., Wong, M.C.S. et al. The resident gut microbiome modulates the effect of synbiotics on the immunogenicity after SARS-COV-2 vaccination in elderly and diabetes patients. npj Biofilms Microbiomes 11, 171 (2025). https://doi.org/10.1038/s41522-025-00804-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41522-025-00804-9