Abstract
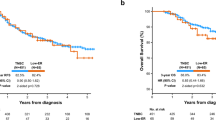
Pathological complete response (pCR) after neoadjuvant chemoimmunotherapy (NACi) is associated with improved patient outcomes in early triple-negative breast cancer (TNBC). This study aimed to identify factors associated with pCR after NACi. This cohort included all patients with stage II-III TNBC treated with NACi who underwent surgery at Institut Curie hospitals between 08/2021-06/2023. Among 208 patients, the overall pCR rate was 70% and was similar in ER < 1% (69%) and ER-low TNBC (73%, p = 0.6). In a multivariate model, Ki-67 ≥ 30% (OR 5.19 [1.73–17.3]), centralized TILs ≥ 30% (OR = 3.08 [1.42–7.04]), absence of DCIS at initial biopsy (OR = 2.56 [1.08–6.25]) and germline mutations in homologous recombination genes (OR = 9.50 [2.37–67.7]) remained strong independent predictors of pCR. These findings may guide treatment decisions in patients with TNBC undergoing NACi. Almost all patients with germline mutations in HR genes achieved pCR, supporting de-escalation trials. We suggest that ER-low tumors should be managed as TNBC tumors.
Similar content being viewed by others
Introduction
Triple-negative breast cancer (TNBC) is a highly heterogeneous disease comprised of breast tumors with no or minimal expression of estrogen receptor (ER), progesterone receptor (PR), and no amplification or overexpression of human epidermal growth factor receptor 2 (HER-2)1. Histopathological definition of TNBC varies across countries: while ER/PR negativity is defined as strictly less than 1% in immunohistochemistry (IHC) by the ASCO/CAP guidelines2, the ESMO guidelines include tumors with an expression of ER/PR up to 10%3. Accounting for approximately 15% of all breast cancers4, TNBC is characterized by an aggressive phenotype and embodies the breast cancer subtype with the worst prognosis, including early relapse and poor overall survival5. Despite recent advances in the insight of molecular heterogeneity of TNBC, few implications have translated into clinical practice, and cytotoxic chemotherapy remains the cornerstone of treatment.
While pre- and postoperative chemotherapies based on anthracycline and taxane regimens were shown to be equivalent in efficacy6,7, neoadjuvant chemotherapy (NAC) is the unanimously preferred treatment approach for stage II or III TNBC. NAC may enable tumor downstaging and more limited breast and axillary nodal surgery, but it also provides precious information as the tumor response is used for prognostication and indication of tailored postoperative therapies. Pathological complete response (pCR) to NAC is a validated surrogate marker indicating a significantly reduced risk of systemic recurrence. The residual cancer burden (RCB) score, based on the degree of response after NAC, is used to identify patients with a high risk of recurrence8. Over a 10-year span, only 10% of RCB 0 (pCR) TNBC patients treated with NAC are expected to suffer distant recurrence, compared to 19% in the RCB I group, 33% in the RCB II and 54% in the RCB III group9. Since pCR was shown to be strongly associated with improved long-term survival outcomes, especially in TNBC10,11, escalation of neoadjuvant treatment has been the focus in the past few years, and the addition of carboplatin to NAC regimens has improved pCR rates12,13. Recently, a paradigm shift was achieved, introducing neoadjuvant chemo-immunotherapy (NACi) as the new standard of care for high-risk early-stage TNBCs. Pembrolizumab, an immune checkpoint inhibitor (ICI) that blocks PD-1, administered in addition to taxane, carboplatin and anthracycline, improved both pCR rates (64.8%)14 and long-term outcomes: event-free survival (EFS, 5-year EFS rate 81.3%, 95% CI [78.4–83.9])15 and overall survival (OS, 5-year OS rate 86.6%, 95% CI [84–88.8%])16. The high rate of potentially fatal or permanent toxicities observed with NACi (34.1% G3-4 adverse events and 33.5% of immune-related adverse events, among which 12.9% of G3 or higher)17 lead to treatment discontinuation in a non-negligible proportion of patients (27.7%)18. Therefore, identifying the TNBC subgroup of patients with the highest likelihood of benefit from NACi prior to treatment initiation is critical for therapeutic decision-making.
However, no universally approved biomarker is currently approved to predict response to NACi. Results from Keynote-522 showed that PD-L1 expression cannot be used as an optimal tool for patient selection. On the other hand, TILs are both a prognostic and a predictive marker of pCR to NAC in TNBC19,20, but their ability to predict pCR to NACi remains unclear. There is promising research on emerging biomarkers such as tumor mutational burden, immune gene expression profiles, mRNA-based signatures, or circulating-tumor DNA21,22 but they lack significant clinical evidence, and their utility must be further evaluated in prospective studies.
In this study, we aimed to determine whether clinical or pathological pre-treatment biomarkers could predict pCR after NACi in a prospective real-life cohort of patients treated at Institut Curie Hospitals.
Methods
Patients
This study was a population-based prospective cohort study, which included every patient who received NACi (according to the pivotal KEYNOTE-522 trial regimen) and underwent surgery for high-risk early-stage II-III TNBC at Institut Curie hospitals, France (Paris and Saint-Cloud) between August 2021 and June 2023. This study was approved by the Ethical Review Board of Institut Curie (DATA220277) and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants prior to enrollment.
Treatment
NACi consisted of the pivotal KEYNOTE-522 trial treatment schedule14. Patients were planned to receive pembrolizumab 200 mg Q3W in addition to four cycles of carboplatin and weekly paclitaxel followed by four cycles of doxorubicin/cyclophosphamide. Dose-dense AC regimen was not used, and a growth factor prescription was left to the investigator’s discretion. After neoadjuvant treatment, all patients underwent breast-conservative surgery or total mastectomy with axillary staging according to local practice.
Clinical and pathological data
Electronic medical records were used to obtain detailed information regarding clinical and pathological data. Clinical Tumor (T) and node (N) stages were determined according to the 8th edition of the American Joint Committee on Cancer (AJCC) Staging Manual23. If clinical or radiological nodal involvement was suspected, a fine-needle aspiration was performed.
Pathologists confirmed pre-treatment pathological tumor characteristics from biopsy samples performed in our institute. Protein expression determined in IHC was used for tumor subtyping. According to ESMO guidelines, TNBC was defined as ER/PR expressed in <10% of tumor cells and HER2 negative (score 0, 1+, 2+ not amplified)3. Other histopathological variables of interest were the histological type and grade, the presence of ductal carcinoma in situ (DCIS), expression of androgen-receptor (AR), and Ki-67 index ≥ 30% (International Ki67 in Breast Cancer Working Group24). We reported two measures for tumor-infiltrating lymphocytes (TILs): “non-centralized TILs”, collected from medical files and referring to the original pathological reports from the local institution or outside reports (performed by various pathologists); and “centralized-TILs”, which consisted of a centrally reviewed TILs assessment of each H&E slide according to the recommendations of the TILs working group25,26, by two expert breast pathologists pre-trained using the TILs training tool available on www.tilsinbreastcancer.org. The FDA-approved antibody clone 22C3 was used for PD-L1 protein detection in FFPE pre-treatment biopsy samples to determine CPS27. PD-L1 testing was not routinely performed outside our institution, and tissue samples were not available for PD-L1 testing in all patients. Apocrine carcinoma was defined by apocrine morphology and AR positivity (≥10%)28.
Pathological response was confirmed by microscopic assessment of each resected specimen using the RCB index8. pCR (RCB 0) was defined as the absence of invasive cancer in the breast and axillary nodes, irrespective of the presence of residual ductal carcinoma in situ (ypT0/isN0)9.
According to local guidelines, patients who were diagnosed before the age of 61 or in case of familial history of breast cancer underwent genetic testing including germline deleterious mutation in homologous recombination (HR) genes: BRCA1, BRCA2, PALB2, RAD51C, and RAD51D, as well as TP53, CDH1, PTEN, MLH1, MSH2, MSH6, PMS2, and EPCAM29. When germline testing was not performed, we used a targeted NGS panel test to identify somatic mutations in the HR pathway. The absence of a germline mutation was defined as either the absence of a germline mutation in the HR pathway or the absence of somatic mutations in the HR pathway when germline testing was not performed.
Endpoint
We investigated the association between pre-treatment clinical and pathological biomarkers with the achievement of pCR after NACi. Patients who had a tumor progression before surgery were considered as non-pCR/RCB III. pCR rate was analyzed in all patients except for those who were lost to follow-up before surgery (Fig. 1).
Statistical analysis
We reported binary and categorical variables as frequencies (percentages), and continuous variables as medians (interquartile). Patient characteristics were reported using descriptive analyses and compared using the χ2 test, Fisher’s exact test, or the Wilcoxon rank sum test. For correlation, the Pearson correlation coefficient was used.
A logistic regression analysis was conducted for multivariate analysis, including only the significant variables identified in the univariate analysis. Considering the rate of missing data, PDL1 CPS was not included in the multivariate model. Lobular and apocrine carcinomas were rare and not included in the model.
The threshold for statistical significance was set at p < 0.05. R software version 4.2.2 was used for statistical analyses, and the gtsummary package for the analysis30.
Results
Baseline characteristics of patients
Between August 2021 and June 2023, 214 patients with TNBC followed at Institut Curie Hospitals were treated with NACi and 208 were included in this study (four patients declined consent, two patients had their surgery performed elsewhere and were lost to follow-up) (Fig. 1). Carboplatin was mainly planned every-3 week (q3w) (97%), while 3% of patients received it on a weekly schedule. Table 1 summarizes the demographic and clinical baseline characteristics of the 208 patients included in this study. All patients included in this cohort were women. Median age was 49 years (IQR, 41–56 years) and 149 (72%) had clinical stage II. In terms of histological subtype, 92% (n = 191/208) of patients had an invasive carcinoma of no special type (NST), 2% (n = 4/208) had an apocrine carcinoma, and less than 2% had an invasive lobular carcinoma (n = 3/208). Fourteen percent (n = 30/208) of the tumors expressed between 1 and 9% ER, and 15% (n = 32/208) of the patients harbored one germline mutation in homologous recombination (HR) genes. More specifically, we identified mutations in BRCA1 (n = 23/32, 72%), BRCA 2 (n = 5/32, 16%), PALB2 (n = 1/32, 3%), and RAD51C (n = 3/32, 9%). The rate of germline mutations in the HR pathway was similar between ER-low tumors (15.8%) and ER-negative tumors (13.8%).
Association of clinicopathological characteristics with pCR
We observed pCR (RCB 0) in 70% 95% CI [63-76%] of patients (n = 145), and RCB I, II, and III in 7% (n = 15), 19% (n = 40) and 4% (n = 8) of patients respectively. The association between baseline clinicopathological characteristics and pathological complete response after NACi is provided in Table 1.
In univariate analysis, we observed a statistically significant association between pCR and clinical stage: in our study, patients with stage III TNBC achieved pCR less often than stage II patients (respectively 58% vs 74%, OR = 0.47 [0.25–0.88]). This effect appeared to be primarily driven by tumor size (cT1–T2 vs cT3–4 OR = 2.94 [1.53, 5.65]), as we did not observe a statistically positive association of pCR and regional lymph node metastasis (positive vs negative OR = 0.72 [0.38–1.32]). None of the few patients with ILC (n = 3) or apocrine carcinoma (n = 4) achieved a pCR. Of note, 72% of patients with AR-positive ≥ 10% tumors achieved pCR (n = 34/47), compared to 71% of patients with AR < 10% (n = 77/109), OR = 1.09 [0.52–2.38]. Apocrine carcinomas had a lower Ki67 rate than others, 25% IQR [24, 25] vs 70% IQR [50, 80], p = 0.002), and tended to have a lower grade (grade II in n = 2/4, 50% vs n = 24/204, 12%, p = 0.08). HER2 status was not associated with pCR (69% pCR in HER2-low tumors vs 71% in HER2 0 tumors, p = 0.8. Patients achieving pCR had a statistically higher tumor proliferation rate (Ki-67; OR = 1.03 [1.01–1.04]; Table 1 and Fig. 2A).
Patients with a germline mutation in HR genes were more likely to reach pCR (n = 30/32, 94% vs n = 114/175, 65% for patients with no germline mutations, OR = 8.03 [2.32–50.7]). Nearly all of the patients with a germline mutation in the HR pathway achieved pCR, with the exception of two patients harboring BRCA1 mutations.
Interestingly, 73% (n = 22/30) of patients with an expression of ER between 1% and 9% achieved pCR in our study, which was similar for patients with ER < 1% who achieved pCR in 69% (123/178, OR = 1.23 [0.53–3.10]).
We evaluated DCIS at two different time points: before receiving NACi (on tumor biopsy) and after receiving NACi (on surgical specimen). We observed that patients without DCIS on tumor biopsy before receiving any treatment were more likely to achieve pCR than those with DCIS (n = 119/158, 75% DCIS before NACi vs n = 18/34, 53% no DCIS before NACi, OR = 2.71 [1.26–5.85]). In addition, we observed that patients without DCIS on surgical specimens after receiving NACi achieved pCR more frequently than patients with residual DCIS (n = 137/176, 78% without residual DCIS vs n = 8/30, 27% with residual DCIS, OR = 9.66 [4.14–24.7]).
We observed in univariate analysis the same clinicopathological factors associated with RCB (Supplementary Table 1). Given the worse outcome of RCB II and RCB III patients, we also evaluated factors associated with the combined RCB II and III groups vs RCB 0 and I groups (Supplementary Table 2). Overall, the results were similar.
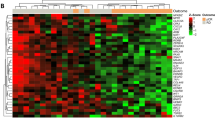
Impact of immunologic features on pCR
Regarding the association between clinicopathological characteristics, centralized TILs and CPS were moderately correlated (R = 0.52, p < 0.001, Pearson) (Fig. 2B). Interestingly, we found that the correlation between TILs assessments by pathologists and the centralized assessment was not strong (R = 0.79, p < 2.2e-16, Pearson).
In univariate analysis, CPS was associated with pCR (OR = 1.03 [1.01–1.06], Table 1 and Fig. 2C), as well as centralized TILs (OR = 1.04 [1.02–1.06], Table 1 and Fig. 2D), but not TILs assessed by various pathologists (OR = 1.00 [0.99–1.02]).
Multivariate analysis
In a multivariate model (Table 2), Ki-67 ≥ 30% (HR 5.19 [1.73–17.3]), centralized TILs ≥ 30% (OR = 3.08 [1.42–7.04]), absence of DCIS on the initial biopsy (OR = 2.56 [1.08–6.25]) and germline mutations in HR genes (OR = 9.50 [2.37–67.7]) remained strong independent predictors of pCR after NACi. Tumor grade was not an independent factor in the multivariate analysis (OR = 1.18 [0.40–3.30]).
Discussion
To our knowledge, in this study we reported for the first time that germline mutations in HR genes, Ki-67, TILs, histological subtype, and absence of DCIS on pre-treatment biopsy were associated with pCR in stage II-III TNBC undergoing NACi, and that TNBC with ER-low had a similar pCR rate to TNBC with ER < 1%.
Achieving pCR is a major goal of the neoadjuvant treatment approach as it was shown to be associated with significantly improved EFS and OS in TNBC9. A recent exploratory analysis from the KEYNOTE-522 trial also confirmed that the addition of pembrolizumab to chemotherapy improves EFS in patients who do not have a pCR: fewer EFS events were observed in the RCB 0, I/II categories, with the greatest benefit in RCB-II31. In our cohort, 70% of patients had a pCR, in line with the rates observed in KEYNOTE-52214. Identifying patients before treatment initiation who are more likely to achieve pCR could lead to treatment de-escalation, avoiding unnecessary toxicities of either the chemotherapy backbone, such as anthracyclines, or the ICI. Conversely, investigational therapeutic alternatives could be offered to those less likely to achieve pCR.
Approximately 10 to 15% of TNBC patients carry BRCA1 or BRCA2 germline mutations32 and conflicting data have been reported concerning pCR rates in these patients. A study reported that patients with BRCA mutations achieved higher pCR rates than patients without BRCA mutations after receiving NAC33, while Bonadio et al. did not observe such association34. In a cohort of patients treated at our institution before 2012 without carboplatin, the pCR rate among patients with TNBC was 48% in those with BRCA germline mutations, compared to 43% in those without35. Moreover, a group of sporadic cancers called “BRCA-like”, comprised of tumors with a homologous recombination deficiency (HRD) but without BRCA 1/2 germline mutations, has also been associated with higher pCR rates after receiving NAC36. One study revealed that the mutational status of 10 DNA repair genes involved in HR could predict response to NAC: tumors with a positive mutation status for such genes would achieve pCR more often37. Here, we also observed a statistically positive association between germline mutations in HR-related genes and pCR after NACi. This suggests that HRD may sensitize the tumor to chemotherapy and ICI. In addition, the predictive value of HRD for response to ICI in the chemotherapy-free regimens warrants further investigation. In our study, almost every patient with a germline BRCA1/2 mutation achieved pCR, meaning that only a few patients who did not achieve pCR would receive PARP inhibitors in the adjuvant setting38. These patients with germline BRCA1/2 mutations may benefit from a de-escalation strategy with the use of PARP inhibitors +/− ICI in the neoadjuvant setting39,40, and consideration of salvage chemotherapy in the absence of pCR.
TNBC is a highly proliferative breast cancer subtype, usually associated with high Ki-67 expression41. Although controversial data exist on the independent prognostic value of Ki-67, its use as a predictive marker of response to chemotherapy has been widely investigated. A high level of Ki-67 was shown to be a good predictor of response to chemotherapy, including in the neoadjuvant setting42. Consistent with these findings, we also observed statistically higher pCR rates among patients with high Ki-67 expression in our cohort. As Ki-67 correlates with tumor SUVmax in [18F]FDG-PET imaging, our observation here resonates with the conclusions drawn from our previous work, in a smaller cohort, exploring the predictive value of pre-treatment [18F]FDG-PET imaging, in which we concluded that high tumor metabolism (SUVmax) and low metabolic tumor volume (TMTV) could accurately predict pCR43.
Apocrine carcinoma, defined by apocrine morphology and AR positivity, accounts for approximately 1% of all breast cancers44 and has been shown to be associated with a better prognosis, despite a poorer response to NAC45. Several studies have described that apocrine carcinomas tend to show a lower proliferation rate and a rather chemo-resistant profile46,47, with a decreased probability of achieving pCR after NAC. It has also been suggested that AR expression would be associated with tumor cell immune evasion48. Consistent with these findings, we also observed that apocrine carcinomas had a lower pCR rate after NACi in univariate analysis. This observation should be taken carefully, since apocrine carcinomas represent a rare subset of TNBC, and therefore only a very small number were included in our cohort, as well as the absence of pCR observed in TNBC with ILC. However, we did not observe an association between AR expression/positivity and pCR.
TILs, lymphocytes infiltrating the tumor and its invasive margins49, are a major component of the tumor microenvironment, mediating adaptive, anti-tumor immune responses. Because of higher levels of TILs commonly reported, along with higher TMB and enhanced PD-L1 expression (measured by the CPS score), TNBC is considered the most immunogenic subtype of breast cancer50. TILs have been reported to be a strong prognostic marker in TNBC: a high abundance of TILs has robustly been associated with a greater likelihood of achieving pCR after NAC51,52, but their ability to predict responses to immunotherapy (IO) agents has not been fully defined in early-stage TNBC. A large body of data has emerged from early/advanced settings, in which a correlation between baseline TILs, CPS score, and tumor response has been reported53,54,55. Several studies then reported an independent correlation between the abundance of TILs in residual disease after NAC and long-term survival outcomes, leading to a 21% relative reduction in the risk of metastasis and death for each 10% TIL increment20,56. Similarly to other studies57,58, TILs were statistically associated with pCR after NACi in our cohort, with a positive association between tumors exhibiting higher TIL infiltration achieving higher pCR rates. CPS, a well-recognized predictive biomarker of response to pembrolizumab in advanced breast cancer55, was also associated with pCR in our cohort. Notably, similar to other studies59, we observed a significant disparity in TIL assessments between the evaluations by untrained pathologists vs the centralized review by trained experts, with only the centralized assessment being associated with pCR. Therefore, we emphasize that TIL evaluation should be performed by a well-trained breast pathologist, especially as several clinical trials rely on TIL measurements for treatment escalation or de-escalation (NCT06078384 and NCT06067061).
Importantly, 73% of patients with an expression of ER between 1% and 9% achieved pCR in our study, indicating a pCR rate at least as high as the pCR rate observed in the KEYNOTE-522 trial (64.8%)14, in which only patients with ER expression < 1% were included. KEYNOTE 756, conducted in patients with ER ≥ 1%, reported that the addition of pembrolizumab leads to a higher pCR, especially in the ER-low (1–9%) subgroup60. Our data support the observation that patients with an ER expression between 1% and 9% have a very high pCR rate, similar to those with ER < 1%, and should therefore be treated as TNBC and receive chemo-immunotherapy with the addition of carboplatin, by opposition to the KEYNOTE 756 trial. This was also observed with a drug regimen without anthracycline49.
Also, the absence of DCIS on pre-treatment biopsy and on the resected specimen were both strongly associated with pCR, including in the multivariate model, while the presence of DCIS was not generally found to be a prognostic/predictive factor of pCR61. The presence of an in situ component (DCIS) is often associated with the invasive component in breast carcinoma62. In TNBC, DCIS is less frequently observed as compared to luminal or HER2-positive tumors. We hypothesize that this may be linked to distinctive biological features of TNBC such as a specific molecular subtype, intra-tumoral heterogeneity, and a distinct tumor microenvironment, all of which could contribute to the observed treatment resistance. Furthermore, there is conflicting literature regarding the predictive value of DCIS to NAC response: Van Bockstal et al. found no association between a DCIS component and pCR in a cohort of TNBC patients63, as well as a retrospective cohort from our institution61. By contrast, according to Von Minckwitz et al., the presence of DCIS is an independent negative predictor of pCR after NAC in HER2-positive BC64. Literature on the predictive value of DCIS to NACi in TNBC is scarcer. Nearly every tumor that achieved pCR was ypT0N0 (i.e., without residual DCIS). Therefore, pCR after NACi is rarely associated with residual in situ disease, suggesting that both in situ and infiltrative disease tend to regress in parallel. The biological significance of this result is currently unknown, and further studies are needed to examine specific characteristics of TNBC with in situ disease vs other TNBCs, and to compare biological features of the in situ and infiltrating components within the same tumor.
The main limitation of our study is the absence of a validation cohort and the fact that all patients were treated at the Institut Curie Hospitals. Other limitations include the absence of a blinded independent central review for TNBC diagnosis, the absence of systematic PD-L1 testing (due to the low tumor tissue availability), and the lack of information on chemo-immunotherapy compliance. Furthermore, results regarding apocrine and lobular carcinomas are derived from a very limited sample size, which affects the generalizability of our findings. Larger cohorts are needed to validate our observations.
In conclusion, we showed that germline mutation in genes involved in homologous recombination, TILs, Ki-67 expression, histological subtype, and absence of DCIS, could help to predict pathological complete response after neoadjuvant chemo-immunotherapy in triple-negative breast cancer. Moreover, patients with TNBC with ER-low tumors had a similar pCR to TNBC with ER <1%. To our knowledge, this is the first study to report such an association in a large real-life cohort of TNBC treated with the KEYNOTE-522 regimen.
Data availability
Data are available upon reasonable request at the discretion of the corresponding authors. Access to datasets used in this study should be requested directly from the corresponding authors.
References
Foulkes, W. D., Smith, I. E. & Reis-Filho, J. S. Triple-negative breast cancer. N. Engl. J. Med. 363, 1938–1948 (2010).
Hammond, M. E. H. et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version). Arch. Pathol. Lab. Med. 134, e48–e72 (2010).
Loibl, S. et al. Early breast cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up☆. Ann. Oncol. 35, 159–182 (2024).
Waks, A. G. & Winer, E. P. Breast cancer treatment: a review. JAMA 321, 288–300 (2019).
Dent, R. et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin. Cancer Res. 13, 4429–4434 (2007).
Wolmark, N., Wang, J., Mamounas, E., Bryant, J. & Fisher, B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J. Natl. Cancer Inst. Monogr. https://doi.org/10.1093/oxfordjournals.jncimonographs.a003469 (2001).
Mamounas, E. P. NSABP protocol B-27. Preoperative doxorubicin plus cyclophosphamide followed by preoperative or postoperative docetaxel. Oncol. Williston Park N. 11, 37–40 (1997).
Symmans, W. F. et al. Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J. Clin. Oncol. 25, 4414–4422 (2007).
Yau, C. et al. Residual cancer burden after neoadjuvant chemotherapy and long-term survival outcomes in breast cancer: a multicentre pooled analysis of 5161 patients. Lancet Oncol. 23, 149–160 (2022).
Cortazar, P. et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet Lond. Engl. 384, 164–172 (2014).
von Minckwitz, G. et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J. Clin. Oncol. 30, 1796–1804 (2012).
Shepherd, J. H. et al. CALGB 40603 (Alliance): long-term outcomes and genomic correlates of response and survival after neoadjuvant chemotherapy with or without carboplatin and bevacizumab in triple-negative breast cancer. J. Clin. Oncol. 40, 1323–1334 (2022).
Loibl, S. et al. Addition of the PARP inhibitor veliparib plus carboplatin or carboplatin alone to standard neoadjuvant chemotherapy in triple-negative breast cancer (BrighTNess): a randomised, phase 3 trial. Lancet Oncol. 19, 497–509 (2018).
Schmid, P. et al. Pembrolizumab for early triple-negative breast cancer. N. Engl. J. Med. 382, 810–821 (2020).
Schmid, P. et al. Event-free survival with pembrolizumab in early triple-negative breast cancer. N. Engl. J. Med. 386, 556–567 (2022).
Schmid, P. et al. Overall survival with pembrolizumab in early-stage triple-negative breast cancer. N. Engl. J. Med. 391, 1981–1991 (2024).
Johnson, D. B., Nebhan, C. A., Moslehi, J. J. & Balko, J. M. Immune-checkpoint inhibitors: long-term implications of toxicity. Nat. Rev. Clin. Oncol. 19, 254–267 (2022).
Rizzo, A. et al. Discontinuation rate and serious adverse events of chemoimmunotherapy as neoadjuvant treatment for triple-negative breast cancer: a systematic review and meta-analysis. ESMO Open 8, 102198 (2023).
El Bairi, K. et al. The tale of TILs in breast cancer: a report from the International Immuno-Oncology Biomarker Working Group. NPJ Breast Cancer 7, 150 (2021).
Loi, S. et al. Tumor-infiltrating lymphocytes and prognosis: a pooled individual patient analysis of early-stage triple-negative breast cancers. J. Clin. Oncol. 37, 559–569 (2019).
Karn, T. et al. Tumor mutational burden and immune infiltration as independent predictors of response to neoadjuvant immune checkpoint inhibition in early TNBC in GeparNuevo. Ann. Oncol. 31, 1216–1222 (2020).
Emens, L. A. et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immunotherapy for the treatment of breast cancer. J. Immunother. Cancer 9, e002597 (2021).
Amin, M. B. et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more ‘personalized’ approach to cancer staging. Ca. Cancer J. Clin. 67, 93–99 (2017).
Nielsen, T. O. et al. Assessment of Ki67 in breast cancer: updated recommendations from the International Ki67 in Breast Cancer Working Group. JNCI J. Natl. Cancer Inst. 113, 808–819 (2021).
Salgado, R. et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann. Oncol. 26, 259–271 (2015).
Hendry, S. et al. Assessing tumor-infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the International Immuno-Oncology Biomarkers Working Group: Part 2: TILs in melanoma, gastrointestinal tract carcinomas, non-small cell lung carcinoma and mesothelioma, endometrial and ovarian carcinomas, squamous cell carcinoma of the head and neck, genitourinary carcinomas, and primary brain tumors. Adv. Anat. Pathol. 24, 311–335 (2017).
Guo, H. et al. Comparison of three scoring methods using the FDA-approved 22C3 immunohistochemistry assay to evaluate PD-L1 expression in breast cancer and their association with clinicopathologic factors. Breast Cancer Res. BCR 22, 69 (2020).
Tan, P. H. et al. The 2019 World Health Organization classification of tumours of the breast. Histopathology 77, 181–185 (2020).
Moretta, J. et al. [The French Genetic and Cancer Consortium guidelines for multigene panel analysis in hereditary breast and ovarian cancer predisposition]. Bull. Cancer 105, 907–917 (2018).
Sjoberg, D. D., Whiting, K., Curry, M., Lavery, J. A. & Larmarange, J. Reproducible summary tables with the gtsummary package. R J. 13, 570–580 (2021).
Pusztai, L. et al. Event-free survival by residual cancer burden with pembrolizumab in early-stage TNBC: exploratory analysis from KEYNOTE-522. Ann. Oncol. 35, 429–436 (2024).
Hartman, A.-R. et al. Prevalence of BRCA mutations in an unselected population of triple-negative breast cancer. Cancer 118, 2787–2795 (2012).
Wang, C. et al. Prevalence of BRCA1 mutations and responses to neoadjuvant chemotherapy among BRCA1 carriers and non-carriers with triple-negative breast cancer. Ann. Oncol. 26, 523–528 (2015).
Bonadio, R. C. et al. Dose dense versus 3 weekly AC during neoadjuvant chemoimmunotherapy for triple negative breast cancer. NPJ Breast Cancer 10, 73 (2024).
Grandal, B. et al. Impact of BRCA mutation status on tumor infiltrating lymphocytes (TILs), response to treatment, and prognosis in breast cancer patients treated with neoadjuvant chemotherapy. Cancers 12, 3681 (2020).
Paluch-Shimon, S. et al. Neo-adjuvant doxorubicin and cyclophosphamide followed by paclitaxel in triple-negative breast cancer among BRCA1 mutation carriers and non-carriers. Breast Cancer Res. Treat. 157, 157–165 (2016).
Huang, L. et al. A predictor of pathological complete response to neoadjuvant chemotherapy in triple-negative breast cancer patients with the DNA repair genes. Ann. Transl. Med. 9, 301 (2021).
Geyer, C. E. et al. Overall survival in the OlympiA phase III trial of adjuvant olaparib in patients with germline pathogenic variants in BRCA1/2 and high-risk, early breast cancer. Ann. Oncol. 33, 1250–1268 (2022).
Abraham, J. E. et al. The PARTNER trial of neoadjuvant olaparib with chemotherapy in triple-negative breast cancer. Nature 629, 1142–1148 (2024).
Buhrer, E. et al. 351TiP EORTC BCG 1984—NOBLE: noeoadjuvant olaparib and durvalumab for patients with BRCA-associated triple-negative breast cancer. Ann. Oncol. 34, S322 (2023).
Oshi, M. et al. ITPKC as a prognostic and predictive biomarker of neoadjuvant chemotherapy for triple negative breast cancer. Cancers 12, 2758 (2020).
Yerushalmi, R., Woods, R., Ravdin, P. M., Hayes, M. M. & Gelmon, K. A. Ki67 in breast cancer: prognostic and predictive potential. Lancet Oncol 11, 174–183 (2010).
Seban, R.-D. et al. [18F]FDG PET/CT for predicting triple-negative breast cancer outcomes after neoadjuvant chemotherapy with or without pembrolizumab. Eur. J. Nucl. Med. Mol. Imaging 50, 4024–4035 (2023).
Dellapasqua, S. et al. Immunohistochemically defined subtypes and outcome of apocrine breast cancer. Clin. Breast Cancer 13, 95–102 (2013).
Hu, T. et al. Triple-negative apocrine breast carcinoma has better prognosis despite poor response to neoadjuvant chemotherapy. J. Clin. Med. 11, 1607 (2022).
Thompson, K. J. et al. Luminal androgen receptor breast cancer subtype and investigation of the microenvironment and neoadjuvant chemotherapy response. NAR Cancer 4, zcac018 (2022).
Thomas, A., Reis-Filho, J. S., Geyer, C. E. & Wen, H. Y. Rare subtypes of triple negative breast cancer: Current understanding and future directions. NPJ Breast Cancer 9, 55 (2023).
Wang, Y. et al. An enhancer-based analysis revealed a new function of androgen receptor in tumor cell immune evasion. Front. Genet. 11, 595550 (2020).
Sharma, P. et al. Clinical and biomarker findings of neoadjuvant pembrolizumab and carboplatin plus docetaxel in triple-negative breast cancer: NeoPACT phase 2 clinical trial. JAMA Oncol 10, 227–235 (2024).
Barroso-Sousa, R. et al. Prevalence and mutational determinants of high tumor mutation burden in breast cancer. Ann. Oncol. 31, 387–394 (2020).
Denkert, C. et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol 19, 40–50 (2018).
Ochi, T. et al. Predictive and prognostic value of stromal tumour-infiltrating lymphocytes before and after neoadjuvant therapy in triple negative and HER2-positive breast cancer. Eur. J. Cancer Oxf. Engl. 1990 118, 41–48 (2019).
Schmid, P. et al. Pembrolizumab plus chemotherapy as neoadjuvant treatment of high-risk, early-stage triple-negative breast cancer: results from the phase 1b open-label, multicohort KEYNOTE-173 study. Ann. Oncol. 31, 569–581 (2020).
Loi, S. et al. Association between biomarkers and clinical outcomes of pembrolizumab monotherapy in patients with metastatic triple-negative breast cancer: KEYNOTE-086 exploratory analysis. JCO Precis. Oncol. 7, e2200317 (2023).
Cortes, J. et al. Pembrolizumab plus chemotherapy in advanced triple-negative breast cancer. N. Engl. J. Med. 387, 217–226 (2022).
Dieci, M. V. et al. Update on tumor-infiltrating lymphocytes (TILs) in breast cancer, including recommendations to assess TILs in residual disease after neoadjuvant therapy and in carcinoma in situ: a report of the International Immuno-Oncology Biomarker Working Group on Breast Cancer. Semin. Cancer Biol. 52, 16–25 (2018).
Wood, S. J. et al. High tumor infiltrating lymphocytes are significantly associated with pathological complete response in triple negative breast cancer treated with neoadjuvant KEYNOTE-522 chemoimmunotherapy. Breast Cancer Res. Treat. https://doi.org/10.1007/s10549-023-07233-2 (2024).
Marhold, M. et al. Emergence of immune-related adverse events correlates with pathological complete response in patients receiving pembrolizumab for early triple-negative breast cancer. Oncoimmunology 12, 2275846 (2023).
Van Bockstal, M. R. et al. Interobserver variability in the assessment of stromal tumor-infiltrating lymphocytes (sTILs) in triple-negative invasive breast carcinoma influences the association with pathological complete response: the IVITA study. Mod. Pathol. 34, 2130–2140 (2021).
Cardoso, F. et al. KEYNOTE-756: a randomized, double-blind, phase III study of pembrolizumab or placebo with neoadjuvant chemotherapy and adjuvant endocrine therapy for high-risk, early-stage, ER+/HER2−breast cancer. Ann. Oncol. 30, ix7–ix8 (2019).
Labrosse, J. et al. The Presence of an in situ component on pre-treatment biopsy is not associated with response to neoadjuvant chemotherapy for breast cancer. Cancers 13, 235 (2021).
Dieterich, M. et al. Accompanying DCIS in breast cancer patients with invasive ductal carcinoma is predictive of improved local recurrence-free survival. Breast 23, 346–351 (2014).
Van Bockstal, M. R. et al. Predictive markers for pathological complete response after neo-adjuvant chemotherapy in triple-negative breast cancer. Ann. Diagn. Pathol. 49, 151634 (2020).
von Minckwitz, G. et al. Responsiveness of adjacent ductal carcinoma in situ and changes in HER2 status after neoadjuvant chemotherapy/trastuzumab treatment in early breast cancer–results from the GeparQuattro study (GBG 40). Breast Cancer Res. Treat. 132, 863–870 (2012).
Acknowledgements
On behalf of the Women’s Cancer Institute breast cancer group, Institut Curie discloses support for the research of this work. This work benefitted from a National grant from the National Research Agency within the France 2030 plan framework—ANR-23-IAHU-0006. We thank the patients who volunteered to participate in this study and the investigators and staff members who cared for them.
Author information
Authors and Affiliations
Contributions
L.C. conceptualized and designed the study. All authors contributed to the acquisition, analysis, or interpretation of the data. C.H., L.D., and L.C. drafted the manuscript, and all authors critically reviewed it for important intellectual content. M.C. and L.C. conducted the statistical analysis. L.C. supervised the study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Helal, Dr. Djerroudi, Dr. Ramtohul, Dr. Seban, Dr. Carton, Pr. Bieche, Dr. Maxime Jin, Dr. Enora Laas, Dr. Claire Bonneau, and Dr. Luc Cabel do not declare a conflict of interest. Pr Anne Vincent-Salomon reported lectures honorarium: AstraZeneca, Daiichi Sankyo, Ibex, MSD, PRIMAA, Roche, Gilead; Advisory Board: AstraZeneca, Daiichi Sankyo, Ibex, PRIMAA, Roche; Research Funding: AstraZeneca, Ibex, MSD, MSD Avenir, Owkin; Stock option: Ibex. Dr Bello-Roufai reported Board from MSD, AstraZeneca, Lilly, Eisai, and travel fees: MSD, AstraZeneca, Eisai. Pr Bidard reported Research fundings: GE Healthcare, Pfizer, Prolynx, Menarini Silicon Biosystems, Merck KGaA, MSD, Novartis, Personalis, Pfizer, Roche, SAGA Diagnostics, and Tempus. Advisory boards for AstraZeneca, Daiichi-Sankyo, Exact Sciences, GE Healthcare, Gilead, Inatherys, Lilly, Menarini/Stemline, Novartis, Pfizer, Roche, SAGA Diagnostics; Speaker for AstraZeneca, Daiichi-Sankyo, Lilly, Menarini/Stemline, and Pfizer. Travel support from AstraZeneca, Daiichi-Sankyo, Pfizer, Novartis. Pr Cottu reported Honoraria: Pfizer, Roche, Lilly, Daiichi Sankyo, AstraZeneca, Gilead Sciences, Novartis, and NanoString Technologies. Consulting or Advisory Role: Pfizer, Lilly. Research funding: Pfizer. Travel, accommodations, and expenses: Roche, Pfizer, and Lilly. Dr Loirat reported Honoraria: AstraZeneca, Gilead Sciences Inc, Eli Lilly and Company, and MSD. Consulting or advisory fees: 4D Pharma, AstraZeneca, Gilead Sciences Inc., Immunomedics, Eli Lilly and Company, MSD Oncology, Novartis AG, Pfizer Inc., and Roche. Funding for travel, accommodations, and expenses: AstraZeneca, Gilead Sciences Inc., MSD, Pfizer Inc., and Roche. Dr. Lerebours reported Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events: AstraZeneca, Eisai, Gilead, Daiichi Sankyo, Lilly, Menarini, Novartis, Roche, and Seagen. Support for attending meetings and/or travel: Daiichi Sankyo, Gilead, Lilly, MSD, Novartis, Pfizer, and Seagen. Dr Kiavue reported a Travel Grant from Seagen. Dr. Romano reported Grants and other support from AstraZeneca, Replimune, Bristol Myers Squibb, and Fonds Amgen France pour la Science et l’Humain outside the submitted work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Helal, C., Djerroudi, L., Ramtohul, T. et al. Clinico-pathological factors predicting pathological response in early triple-negative breast cancer. npj Breast Cancer 11, 15 (2025). https://doi.org/10.1038/s41523-025-00729-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41523-025-00729-8
This article is cited by
-
Enhanced Multi-Layer Graphene-Metal Terahertz Biosensor with Machine Learning Optimization for Early-Stage Breast Cancer Detection
Journal of Electronic Materials (2026)
-
Immunotherapy for triple-negative breast cancer: current trends and future prospects
Journal of the Egyptian National Cancer Institute (2025)
-
Neoadjuvant dose-dense anthracycline and cyclophosphamide in combination with carboplatin, paclitaxel, and pembrolizumab for triple-negative breast cancer: a systematic review and meta-analysis
Breast Cancer Research and Treatment (2025)
-
Ki-67 expression stratifies PD-L1-high NSCLC for immune checkpoint inhibitor plus chemotherapy: a real-world biomarker validation
Cancer Immunology, Immunotherapy (2025)
-
Pathological response to pembrolizumab-based neoadjuvant therapy in ER-low vs. ER-zero breast cancer: a Swedish population-based cohort study
Breast Cancer Research (2025)