Abstract
The influence of young age at diagnosis on prognosis of patients with metastatic breast cancer (MBC) remains unclear. We examined overall survival (OS) within a single-institution prospective study of patients with de novo or recurrent MBC. Kaplan-Meier curves assessed OS by age (≤35 or ≤40 years as the youngest category) and inferred metastatic tumor subtype. Multivariable Cox regression models estimated hazard ratios (HRs) and 95% CIs for OS by age adjusting for clinical factors. Of 4189 women <75 years, 571 were ≤40 years at MBC diagnosis, of whom 260 were ≤35 years. Over half (52%) died during follow-up (median = 5.3 years, IQR = 2.1–9.8 years). Compared to patients 45–55 years, those ≤35 years at diagnosis experienced worse OS (HR = 1.22, 95%CI 1.00–1.48, p = 0.05). This association was driven by HER2-negative/luminal B-like and hormone receptor-positive/HER2-positive tumors. These findings highlight the need to develop more effective therapies for young patients with this metastatic subtype.
Similar content being viewed by others
Introduction
The majority of breast cancer (BC)-related deaths are due to metastatic disease1. In the U.S., de novo metastatic BC (MBC) accounts for approximately 3–6% of incident BC cases2 and roughly 30% of all patients with early-stage BC will develop recurrent MBC3, with rates dependent on primary BC subtypes and treatments4,5. The high mortality rates of patients with MBC6,7, especially for those with recurrent MBC8,9,10, indicate the need for further exploration of predictors of overall survival (OS) in MBC.
Studies of patients with early-stage BC have demonstrated prognostic differences by age at diagnosis, with recent studies indicating worse BC-specific survival among young patients (≤40 years) compared to those older at diagnosis11,12, dependent on molecular subtype12,13. While younger women are more likely to be diagnosed with de novo MBC and have approximately double the risk for recurrent metastasis compared to their older counterparts5,14, the association between age at MBC diagnosis and OS is unclear. Studies report both better15,16,17, and worse OS5,18 for young patients with MBC, which may be attributed to heterogeneity between the represented patient cohorts, differences in the definition of young age (including <50 years,15 <40 years,17 ≤35 years18, and continuous age16), and inconsistent sets of adjustment factors used in multivariable models.
Studies of registry-based data rarely capture recurrence, leaving the largest studies on OS of MBC generalizable to the minority of patients who present with de novo MBC. Tumor molecular subtype is a known prognostic factor19,20 that differs in frequency and in association with OS by age at diagnosis12,21,22. However, most studies adjust for subtype by using hormone receptor and human epidermal growth factor receptor 2 (HER2) receptor status alone15,16,17, lacking the important distinction between luminal A and luminal B subtypes. In addition, most studies examining OS in patients with MBC have relied on primary as opposed to metastatic tumor subtype, misclassifying those individuals who will develop a metastasis with a different (often more aggressive) subtype than their primary tumor23, and limiting interpretation given that clinical recommendations emphasize treatment-based decision-making by metastatic tumor characteristics24. Here we evaluated whether and to what extent age influences survival following MBC diagnosis, accounting for clinicopathologic features of metastatic tumors.
Results
Patient characteristics
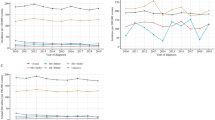
After excluding 31 women with unknown vital status and 178 women ≥75 years at metastatic diagnosis, the analytic cohort included 4189 patients, enrolled between 2009–2023, with diagnosis of MBC ranging from 1983–2023 and follow-up ending in May 2024. Median age at MBC diagnosis was 54 years (interquartile ranges [IQR] = 45–62 years, range = 18–75 years), with 571 ≤40 years, 1693 41–55 years, and 1925 >55- <75 years (Table 1, Table S1). Targeted germline genetic testing results were known for 2,610 participants (N = 62%), though numbers differed by gene tested. Among those with testing performed, a pathogenic variant (PV) in BRCA2 was slightly more common in individuals aged 40-55 years compared to those >55–75 years (3% v. 2%, p = 0.05), and BRCA1 PVs were numerically more frequent in the youngest age groups, though this was not statistically significant (2% in ≤40 years and 2% in ≤35 years v.1% in >55- < 75 years, p for ≤40 years vs. >55–75 years = 0.06). A high proportion of patients presented with stage 3 (25%) or stage 4 de novo (24%) disease. Compared to older patients, those ≤40 years at diagnosis were more likely to present with de novo disease ( ≤ 40 years: 36% v. >40–55 years: 23% v. >55-75 years: 21%, p < 0.001). The most common primary tumor histology was invasive ductal, though younger patients were significantly less likely to have lobular histology ( > 55 years: 18% v. ≤40 years: 5%, p = 0.001). Younger patients were more likely to receive radiation in the metastatic setting compared to older counterparts. Brain metastases were significantly more common in the younger patients (13%) compared to those ages 40–55 years (10%, p = 0.04) and those >55–75 years (p = 0.001).
Clinical outcomes and univariable associations of age and clinical factors with OS
Over a median follow up of 5.3 years (IQR = 2.1–9.8 years), 2190 (52%) of patients died. Among those who died, median time between metastatic diagnosis and death was 2.6 years (IQR = 1.3–4.6 years). In univariable models, age ≤35 years was associated with shorter OS compared to those >35-55 years (hazard ratio [HR] [95% CI] = 1.20 [1.01–1.43], p = 0.04) (Table 2), though age ≤40 years was not statistically significantly associated with OS. When comparing 10-year age groups, the difference in survival appeared most prominent between those ≤35 years v. those >35–45 years or >55–65 years (Table 2). OS was shorter among those with recurrent MBC compared to those with de novo MBC (HR [95% CI] = 1.51 [1.36–1.67], p < 0.001) and the reduction in OS time was stronger among those with shorter disease-free interval (DFI) (HR [95% CI]: 0–2 years v. de novo = 2.84 [2.50–3.24] v. ≥2 years v. de novo = 1.27 [1.14–1.42], p < 0.001) (Table 2). The strongest associations with OS were for metastatic tumor subtype and sites of metastases. Compared to luminal A-like tumors, HER2−, luminal B-like tumors were associated with approximately 2-times the hazard of death (HR = 1.85, p < 0.001), while HR−/HER2− tumors were associated with 4 times the hazard of death (HR = 4.22, p < 0.001). In addition, the hazard of death among those with brain or liver metastases was approximately 2-times that of individuals without these metastases.
Multivariable associations of age and clinical factors with OS
Age ≤35 years was associated with 1.2-times the hazard of death compared to age 45–55 years (p = 0.05) after adjustment for DFI, primary tumor grade, metastatic tumor subtype, and sites of disease (number and type) (Table 3). Older age (65–75 years) at diagnosis was also associated with shorter OS (HR [95% CI] v. 45–55 y = 1.15 [1.00–1.33], p = 0.05) (Table 3). All clinical factors significantly associated with OS in univariable associations remained significant in multivariable models. When using broader age categories and applying age ≤40 years as the cutoff for young diagnosis, multivariable models showed suggestive, but non-statistically significant associations between age ≤40 years at MBC and OS (HR [95% CI] v. 40–55 years = 1.13 [0.98–1.30], p = 0.08) (Table S2).
Association of age and OS by molecular subtype
In multivariable models stratified by metastatic molecular subtype, compared to older patients, OS was significantly shorter for younger patients (defined as both ≤35 years and ≤40 years at MBC diagnosis) with HER2-, luminal-B like tumors (N = 1213, deaths = 682) (Table 4). Age ≤35 years was associated with shorter OS for patients with hormone receptor-positive (HR + )/HER2+ tumors. Young age was not associated with OS in the other tumor subtypes.
Excluding individuals without direct metastatic tumor subtyping
In a sensitivity analysis excluding individuals without direct metastatic tumor subtyping and adjusting for receptor subtype only (HR + /HER2−, HR + /HER2 + , HR−/HER2−, HR−/HER2−), younger and older age were both associated with shorter OS (HR [95% CI] ≤35 years v. 45–55 years: 1.30 [1.03–1.65], p = 0.03; HR [95% CI]) >65- < 75 years v. 45−55 years: 1.21 [1.03−1.41], p = 0.02) (Table S3).
Inclusion of individuals ≥ 75 years at MBC diagnosis
The association between young age and OS remained similar and statistically significant when including all individuals in the Ending Metastatic Breast Cancer for Everyone (EMBRACE) program regardless of age (range age 18–95 years) at MBC diagnosis (HR [95% CI] <=35 years v. 45–55 years: 1.21 [1.00–1.47], p = 0.05) (Table S4). As expected, the negative impact of older age (>65 years v. 45–55 years) on OS was strengthened when including patients 75 years and older. Other covariates in the multivariable Cox model had similar effect estimates compared with the main analysis.
One-year OS
Out of 2190 deaths, 405 occurred within the first year after MBC diagnosis (≤40 years at MBC diagnosis: N = 305, 40–55 years: N = 914, >55– < 75 years: N = 971). In univariable models, younger age was associated with shorter one-year survival (HR [95% CI] ≤40 years v. >40–55 years=1.34 [1.02–1.76], p = 0.04) (Table S5), though this association disappeared after adjusting for clinical factors (HR [95% CI] ≤40 years v. >40–55 years=1.16 [0.87–1.53], p = 0.32) (Table S6). We were unable to assess the contribution of age ≤35 years on one-year survival in adjusted models given the limited number of events (N = 37 deaths in one year). Metastatic tumor subtype and DFI had an even greater impact on one-year survival compared to overall survival (Table S6 v. Table S2). Compared to patients with de novo disease, having a recurrent MBC diagnosed within 2 years of primary tumor diagnosis was associated with 3.7-times hazard of death (HR [95% CI] = 3.71 [2.64–5.22], p < 0.001). After adjusting for other clinical factors, compared to luminal A-like subtypes, both HER2−, luminal B-like MBC and HR−/HER2− disease were associated with higher hazard of death in one-year (HR [95% CI] luminal B-like= 2.06 [1.26–3.36], p = 0.004; HR−/HER2− = 6.27 [3.85–10.2], p < 0.001) (Table S6).
Changes in tumor molecular subtype and OS
Among patients with recurrent MBC, those who experienced a change in tumor subtype from primary to first metastatic site (N = 392, 18%) were less likely to have primary lobular histology (7% vs. 13%, p < 0.001), more likely to have a higher primary grade (grade 3: 56% vs. 47%, p < 0.001), less likely to have received CDK4 inhibitors (26% vs. 56%, p < 0.001) and more likely to have received chemotherapy (99% vs. 95%, p < 0.001) in the metastatic setting compared to those who had a consistent subtype from primary to metastatic diagnosis. The most common subtype change in this cohort was from HR + /HER2− to hormone receptor-negative (HR−)/HER2− (7.3%) (Table S7). When testing subtype changes individually in a multivariable model adjusted for age at MBC diagnosis, DFI, primary tumor grade, and number and type of metastatic disease, the change from HR + /HER2− to HR−/HER2− disease was associated with shorter OS (HR [95% CI] vs. no change=1.71 [1.37-2.14], p < 0.001) (Table S8). The negative impact of hormone receptor change from positive to negative was not seen among individuals who maintained HER2+ status (HR [95% CI] for HR + /HER2+ to HR−/HER2+ vs. no change = 0.58 [0.38–0.88], p = 0.01). A change from HR + /HER2− to HR + /HER2+ subtype was also associated with improved OS (HR = 0.59 [0.35–0.99], p = 0.05).
Discussion
In this study of over 4000 patients with de novo and recurrent MBC, age ≤35 years at MBC diagnosis was associated with worse OS after adjustment for clinicopathological prognostic features, compared to middle-age (45–55 years at diagnosis). The relationship between young age and OS appeared to be dependent on tumor molecular subtype, with significant associations observed among individuals with HER2−, luminal B-like metastatic tumors. Ultimately, this study illustrates the existence of a complex relationship between age and survival among patients with MBC that requires further investigation of the potential biologic and treatment/access to care mechanisms at play.
Studies have consistently shown that younger patients with de novo MBC fare better than their older counterparts15,16,25. This finding should not be conflated with patients with recurrent MBC, given that de novo MBC is more common among younger patients (accounting for 7.9% of incident BC cases among those aged 15–39 years compared to 5.5% among those 40–75 years)26, and evidence that among young women ( <40 years at primary diagnosis), those with de novo disease fare much better than those with recurrent MBC27. While several studies to date investigating age-survival relationships in patients with MBC have incorporated recurrent patients, either alone or alongside de novo patients, our ability to compare and draw conclusions from these studies is limited by key differences in patient populations, age-groups compared, and variations in adjustment factors of survival models.
First, the majority of studies include elderly patients ( >75 years), who often have a population-based average life-expectancy that is less than the follow-up time of the study, which may bias results. In addition, decisions on how to model age within survival models heavily influence study conclusions. A handful of studies incorporating patients with recurrent MBC have reported better OS among young age groups in multivariable analyses adjusting for demographic and clinicopathological factors9,28,29,30, seemingly conflicting with our findings; however, the use of dichotomized age ( < 50 v. ≥50 years,28 <65 v. ≥65 years30, <70 v. ≥70 years9), or continuous age31 likely masks true patterns of survival among younger patient groups.
Among studies that have assessed the association between finer age groups and survival following MBC diagnosis, most suggest a similar survival experience for younger patients compared to those in middle-age, conflicting with our results. However, these differences may be explained by differences in age group comparisons (with varied definitions of “young age”) and adjustment variables between studies. A large study among 14,403 women diagnosed with MBC at French cancer centers (ESME cohort) between 2008–2014 reported better OS for younger compared to older and middle-aged patients after adjusting for DFI, number and type of metastatic sites, and primary or metastatic tumor subtype17. However, this study compared age groups of <40 years v. 40-60 years v. >60 years. Given that we found ≤35 years as the group with increased risk for poor OS, assessing very young age may be of higher importance. Median survival between younger and middle-aged patients in the ESME study was very similar ( <40 years: 38.8 months v. 40-60 years = 38.4 months), matching our findings. Other studies reporting no association between young age and OS following MBC did not look at very young age ( ≤35 years)10,32, and/or lacked key adjustment factors10,31. For instance, though a SEER study of patients with recurrent MBC31 found no association between continuous age and OS, the model lacked adjustment for two key factors that are consistently strongly associated with survival: HER2 status and site of metastatic disease. These factors were also not incorporated in an analysis of 3447 patients enrolled in the ECOG trials who were diagnosed with BC between 1978–2002, where age <40 years at recurrent MBC diagnosis was not significantly associated with survival compared to other groups (40–49, 50–59, 60–69, >69 years)10. Overall, given the differences in existing studies and lack of assessment of very young individuals ( ≤35 years), it is plausible that our findings, though seemingly in conflict with the current literature, represent a true association between very young age and survival among patients with MBC.
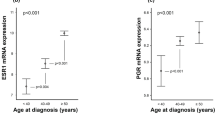
Tumor molecular subtype consistently appears as a significant factor in projecting OS for patients with MBC in the clinical setting. As demonstrated within the EMBRACE cohort and supported by previous studies, the association between age and OS following metastatic diagnosis also varies by molecular subtypes. Age has less impact on OS among individuals with triple-negative breast cancer (TNBC), seen in our study and in prior literature. Two studies of patients with TNBC diagnosed after 2000, found no differences in OS for patients aged <75 years and ≥75 years33, and patients aged >50 years v. ≤50 years29. It is known that patients with de novo metastatic TNBC do worse than other subtypes34, and high distant recurrence rates within the first five years of primary diagnosis (estimated as high as 12% in one Dutch study) contribute to decreased survival in this patient group4. While previous studies have shown better survival for younger vs. older patients with HER2+ disease29,35, we found shorter OS among patients ≤35 years at diagnosis with HER2+ tumors. Longer OS among young patients with HER2+ tumors is expected due to their ability to take advantage of advances in HER2 therapy over the past 2 decades that extend survival compared to other subtypes36. However, our finding suggests that factors aside from treatment differences influence OS differences in MBC patients by tumor subtype.
Categorization of HR + /HER2− tumors into luminal A-like v. luminal B-like revealed further differences in OS by age. Compared to luminal A tumors, luminal B tumors are characterized by a higher expression of genes associated with tumor cell proliferation37, and are associated with worse prognosis overall38. In the context of early BC, luminal B tumors may indicate higher likelihood of recurrence, providing one theory for this observed worse prognosis39. Interestingly, in this study young age was consistently associated with poorer overall survival among patients with HER2− luminal B-like tumors even after adjustment for DFI (which captures de novo v. recurrent status). Thus, the difference in survival among HER2− luminal B-like patients cannot be fully explained by a higher number of recurrent luminal B v. luminal A tumors. In general, our finding of strong associations between metastatic tumor subtype and OS makes the case for incorporating such metastatic tumor data into prognostic models, especially given that our study was able to assess subtype in metastatic tumors samples for the majority (76%) of patients, while most studies have relied on primary tumor subtyping.
Our finding of consistently worse OS with greater number and particular sites of disease at diagnosis of MBC has been reported elsewhere10,17. Before and after adjustment for other clinical factors, the presence of brain or liver metastases portended considerably worse OS, also consistent with existing literature showing up to 4x increased risk for those with liver metastases and up to 15x increased risk for those with brain metastases28.
Subtype switching between primary and metastatic tumor estrogen receptor (ER), progesterone receptor (PR), and HER2 status has been reported elsewhere. One review article combining data from many studies estimated average rates of discordance to be 14% (ER), 21% (PR), and 10% (HER2)40, though there is wide variation in estimates between studies. Overall, subtype switches resulting in loss of positivity are most common40,41,42, which was confirmed in EMBRACE. Our finding that women who had a primary HR+ tumor that switched to an HR− MBC tumor had worse OS aligns with findings from other studies41,43,44,45,46; the reduction in survival may be attributed to historically fewer therapeutic options for patients with HR− tumors or an associated increase in the biologic aggressiveness of the HR- disease. Overall, conclusions based on subtype switches indicate a need to re-assess the phenotype of the metastatic tumor at diagnosis of MBC at a minimum in order to provide proper treatment for patients of all ages.
The strengths of this study include the large sample size and robust data collection with detailed information on patient tumor subtypes, treatment regimens, and outcomes. However, several study limitations must be considered when interpreting our findings. First, we did not include specific treatment regimens in our models given the vast diversity of regimens used in treating patients with MBC and the fact that many MBC treatments are decided based on patient response to primary treatments. Second, though we used metastatic tumor subtype as the main adjustment factor here, we were unable to obtain metastatic tumor subtype on 924 (24%) of patients and instead relied on primary subtype for these patients. However, when we restricted analysis to only those patients with direct metastatic tumor subtyping available, associations between age at diagnosis and OS remained similar. Because we did not have direct gene expression profiling available for MBC or primary tumors, nor did we have Ki67 status on the vast majority of patients, we used inferred molecular subtype based on clinicopathologic characteristics (tumor grade and PR positivity). While this captures some of the variation in HER2− luminal A v. luminal B tumor subtypes, and immunohistochemistry (IHC)-based criteria have been used across the literature in place of genetic profiling39, this remains an imperfect surrogate. In addition, inferred subtypes were by necessity defined in part by primary tumor grade, which may have resulted in misclassification of subtypes. Thus, further studies with direct molecular subtyping for metastatic tumors are needed to confirm our results.
In this large observational study, patients with MBC diagnosed at a very young age ( ≤35 years) experienced shorter OS compared to those diagnosed in middle-age, especially when comparing individuals with HER2−, luminal B-like metastatic tumors. The mechanisms behind this association are unclear. Our findings, which reflect observational data, should not impact current consensus guidelines that young age should not be a reason to treat MBC with more aggressive therapy47,48,49. Moreover, our study emphasizes that tumor subtype remains the most important predictor of OS alongside initial metastatic disease site(s). While promising advances have been made to decrease BC mortality in the U.S., with a 58% reduction in mortality reported between 1975 and 2019, the majority of this decline is due to treatment for early-stage BC or screening, as opposed to MBC treatment50, highlighting the importance of continuing to study this patient subgroup and find biologic as well as clinical explanations for survival advantages to identify avenues to improve survival.
Methods
Cohort
We used data from a prospectively maintained institutional database (EMBRACE), that includes women treated for MBC at Dana-Farber Cancer Institute who consented and enrolled to one of the following Dana-Farber/Harvard Cancer Center protocols: 09-204,05-246, 93-085, 11-104 and/or 17-000. Data collected includes patient demographics, clinicopathological characteristics, biopsy type, details on surgery and metastatic treatment regimens, sites of disease, and patient outcomes. Survival follow-up is collected via medical record review and via linkage to the National Death Index. For this analysis, eligible patients included those enrolled from January 2009 to December 2023 (N = 4397), who were <75 years at MBC diagnosis, with follow-up through 2024. Patients ≥75 years were excluded from the primary analysis due to the shorter projected lifespan of this group from comorbidities and competing causes of death. All protocols were approved by the Dana-Farber/Harvard Cancer Center institutional review board.
Tumor molecular subtype
Primary and metastatic tumor molecular subtype were determined by review of pathology reports, and classified based on ER, PR, and HER2 staining. Tumors were considered HR+ if ≥1% staining for ER or PR. HER2 status was assigned according to ASCO/CAP guidelines (HER2+ defined as 3+ by IHC, HER2 copy number ≥6, or HER2/CEP17 ratio ≥ 2.0)51. Where metastatic tumor molecular subtype was not available (i.e., the initial site of metastatic disease was not biopsied or biopsy was too small to assess subtype), subtype was assumed to be the same as that of the primary tumor. HR + /HER2− metastatic tumors were further characterized by inferring luminal A-like or luminal B-like subtype. Tumors were classified as HER2− luminal B-like if the tumor was grade 3 and/or PR staining was <10% (considered “PR low”). Due to difficulties in grading metastatic tumors, primary tumor grade was used for this classification. PR was directly measured in metastatic tumors in most cases; where this was not possible, PR staining in the primary tumor was used to designate luminal A and B-like subtypes.
Statistical analysis
Characteristics of cohort participants were described with medians and IQR or frequency (%). OS was examined from the time of MBC diagnosis, using Kaplan-Meier curves, stratified by age group at MBC diagnosis ([1] ≤40 years, 41–55 years, >55- < 75 years, [2] ≤35, 36–40, 41–45, 46–55, >55–65, >65- < 75 years), and inferred metastatic tumor molecular subtype. Two definitions were chosen for age group at diagnosis to enable direct comparison of our results with prior studies (most often using ≤40 years as the young cutoff), while also providing novel information on the youngest group of patients. Univariable Cox regression models estimated HRs and 95% CIs for OS by clinical features: including germline mutation status, primary tumor stage and grade, metastatic tumor subtype, DFI, number and type of metastatic sites developed during follow-up (yes/no for bone, brain, liver, lung, other), number of metastatic treatment regimens, and receipt of endocrine therapy (ET), cyclin-dependent kinase 4/6 (CDK4/6) inhibitor therapy, chemotherapy and/or radiation at any time during metastatic treatment. The association between age group at MBC diagnosis and OS was tested in a multivariable Cox model, after adjusting for tumor factors: metastatic tumor molecular subtype (inferred), primary tumor grade (0/1, 2, 3), DFI (defined as: de novo, >0–2 y, ≥2 years), and number and type of metastatic sites at the time of MBC diagnosis. Because inferred metastatic tumor molecular subtype was defined in part using primary tumor grade, we tested the correlation between these variables (all <0.15, considered acceptably low to avoid collinearity). Multivariable models assessing the association between age and OS were also stratified by metastatic tumor subtype. In addition to OS, we tested all models using one-year survival as the outcome of interest.
We conducted several sensitivity analyses. First, to assess the influence of excluding older MBC patients, we repeated analyses without restricting to <75 years at diagnosis. Second, we repeated analyses excluding individuals without tumor subtyping directly available from a metastatic sample. We then assessed differences in clinical and patient characteristics between individuals with recurrent MBC who experienced a change in molecular subtype from primary to metastatic tumor compared to those who did not experience a change, and calculated frequencies of specific tumor subtype changes. The association between specific subtype changes and OS were tested in multivariable Cox models, adjusting for age at MBC diagnosis.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity (e.g., inclusion of indirect patient identifiers such as age, sex, ethnicity, and treatment location) but are available from the corresponding author upon reasonable request and completion of a data use agreement. Data are located in controlled access data storage as part of the IRB-approved, Breast Cancer Data Warehouse at Dana-Farber Cancer Institute. Code availability statement: All coding was done using standard procedures in STATA version 18.0. Coding is specific to the dataset and is available from the corresponding author upon reasonable request.
Code availability
All coding was done using standard procedures in STATA version 18.0. Coding is specific to the dataset and is available from the corresponding author upon reasonable request.
References
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 72, 7–33 (2022).
Daily, K., Douglas, E., Romitti, P. A. & Thomas, A. Epidemiology of de novo metastatic breast cancer. Clin. Breast Cancer 21, 302–308 (2021).
O’Shaughnessy, J. Extending survival with chemotherapy in metastatic breast cancer. Oncologist 10, 20–29 (2005).
van Roozendaal, L. M. et al. Risk of regional recurrence in triple-negative breast cancer patients: a Dutch cohort study. Breast Cancer Res. Treat. 156, 465–472 (2016).
Pan, H. et al. 20-year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N. Engl. J. Med. 377, 1836–1846 (2017).
Cronin, K. A. et al. Annual report to the nation on the status of cancer, part 1: National cancer statistics. Cancer 128, 4251–4284 (2022).
Valachis, A. et al. Overall survival of patients with metastatic breast cancer in Sweden: a nationwide study. Br. J. Cancer 127, 720–725 (2022).
Hölzel, D. et al. Survival of de novo stage IV breast cancer patients over three decades. J. Cancer Res. Clin. Oncol. 143, 509–519 (2017).
Malmgren, J. A., Mayer, M., Atwood, M. K. & Kaplan, H. G. Differential presentation and survival of de novo and recurrent metastatic breast cancer over time: 1990-2010. Breast Cancer Res. Treat. 167, 579–590 (2018).
Tevaarwerk, A. J. et al. Survival in patients with metastatic recurrent breast cancer after adjuvant chemotherapy: little evidence of improvement over the past 30 years. Cancer 119, 1140–1148 (2013).
Chen, H. L., Zhou, M. Q., Tian, W., Meng, K. X. & He, H. F. Effect of age on breast cancer patient prognoses: a population-based study using the SEER 18 database. PLoS One 11, e0165409 (2016).
Kim, H. J., Kim, S., Freedman, R. A. & Partridge, A. H. The impact of young age at diagnosis (age <40 years) on prognosis varies by breast cancer subtype: a U.S. SEER database analysis. Breast 61, 77–83 (2022).
Partridge, A. H. et al. Subtype-dependent relationship between young age at diagnosis and breast cancer survival. J. Clin. Oncol. 34, 3308–3314 (2016).
Gonzalez-Angulo, A. M. et al. Factors predictive of distant metastases in patients with breast cancer who have a pathologic complete response after neoadjuvant chemotherapy. J. Clin. Oncol. 23, 7098–7104 (2005).
Chen, M. T. et al. Comparison of patterns and prognosis among distant metastatic breast cancer patients by age groups: a SEER population-based analysis. Sci. Rep. 7, 9254 (2017).
Wang, R. et al. The Clinicopathological features and survival outcomes of patients with different metastatic sites in stage IV breast cancer. BMC Cancer 19, 1091 (2019).
Frank, S. et al. Impact of age at diagnosis of metastatic breast cancer on overall survival in the real-life ESME metastatic breast cancer cohort. Breast 52, 50–57 (2020).
Adami, H. O., Malker, B., Holmberg, L., Persson, I. & Stone, B. The relation between survival and age at diagnosis in breast cancer. N. Engl. J. Med. 315, 559–563 (1986).
Houssami, N., Macaskill, P., von Minckwitz, G., Marinovich, M. L. & Mamounas, E. Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur. J. Cancer 48, 3342–3354 (2012).
Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature 490, 61–70 (2012).
Roy, M., Fowler, A. M., Ulaner, G. A. & Mahajan, A. Molecular classification of breast cancer. PET Clin. 18, 441–458 (2023).
Todorovic-Rakovic, N. & Neskovic-Konstantinovic, Z. Age related influence of triple receptor status on metastatic breast cancer post relapse survival. J. Buon. 18, 851–858 (2013).
Jørgensen, C. L. T. et al. PAM50 intrinsic subtype profiles in primary and metastatic breast cancer show a significant shift toward more aggressive subtypes with prognostic implications. Cancers (Basel). 13, 1592 (2021).
Cardoso, F. et al. 4th ESO-ESMO International Consensus guidelines for advanced breast cancer (ABC 4). Ann. Oncol. 29, 1634–1657 (2018).
Xiao, Q. et al. Patterns of de novo metastasis and survival outcomes by age in breast cancer patients: a SEER population-based study. Front Endocrinol. (Lausanne). 14, 1184895 (2023).
Surveillance Research Program, National Cancer Institute. SEER*Explorer: An interactive website for SEER cancer statistics. November 19, 2023. Available from: https://seer.cancer.gov/statistics-network/explorer/.
McKenzie, H. S. et al. Survival and disease characteristics of de novo versus recurrent metastatic breast cancer in a cohort of young patients. Br. J. Cancer 122, 1618–1629 (2020).
Largillier, R. et al. Prognostic factors in 1,038 women with metastatic breast cancer. Ann. Oncol. 19, 2012–2019 (2008).
den Brok, W. D. et al. Survival with metastatic breast cancer based on initial presentation, de novo versus relapsed. Breast Cancer Res. Treat. 161, 549–556 (2017).
Leone, J. P. et al. Clinical behavior of recurrent hormone receptor-positive breast cancer by adjuvant endocrine therapy within the Breast International Group 1-98 clinical trial. Cancer 127, 700–708 (2021).
Chang, E., Mougalian, S. S., Adelson, K. B., Young, M. R. & Yu, J. B. Association between prolonged metastatic free interval and recurrent metastatic breast cancer survival: findings from the SEER database. Breast Cancer Res. Treat. 173, 209–216 (2019).
Xie, Y. et al. Association between age at initial diagnosis and post-metastasis mortality among women with recurrent metastatic breast cancer in China. BMC Cancer 22, 385 (2022).
Tzikas, A. K., Nemes, S. & Linderholm, B. K. A comparison between young and old patients with triple-negative breast cancer: biology, survival and metastatic patterns. Breast Cancer Res. Treat. 182, 643–654 (2020).
Li, X. et al. Triple-negative breast cancer has worse overall survival and cause-specific survival than non-triple-negative breast cancer. Breast Cancer Res. Treat. 161, 279–287 (2017).
Murthy, P. et al. Clinical predictors of long-term survival in HER2-positive metastatic breast cancer. Breast Cancer Res. Treat. 155, 589–595 (2016).
Kikuchi, M. et al. Characteristics of patients with metastatic breast cancer who survived more than 10 years. Anticancer Res. 43, 217–221 (2023).
Hu, Z. et al. The molecular portraits of breast tumors are conserved across microarray platforms. BMC Genom. 7, 96 (2006).
Parker, J. S. et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J. Clin. Oncol. 27, 1160–1167 (2009).
Cheang, M. C. U. et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J. Natl. Cancer Inst. 101, 736–750 (2009).
Yeung, C. et al. Estrogen, progesterone, and HER2/neu receptor discordance between primary and metastatic breast tumours-a review. Cancer Metastasis Rev. 35, 427–437 (2016).
Yao, Z. X. et al. Discordance and clinical significance of ER, PR, and HER2 status between primary breast cancer and synchronous axillary lymph node metastasis. Med Oncol. 31, 798 (2014).
Berghuis, A. M. S. et al. Real-world data on discordance between estrogen, progesterone, and HER2 receptor expression on diagnostic tumor biopsy versus tumor resection material. Breast Cancer Res. Treat. 175, 451–458 (2019).
Meng, X. et al. Receptor conversion in metastatic breast cancer: a prognosticator of survival. Oncotarget 7, 71887–71903 (2016).
Chen, R., Qarmali, M., Siegal, G. P. & Wei, S. Receptor conversion in metastatic breast cancer: analysis of 390 cases from a single institution. Mod. Pathol. 33, 2499–2506 (2020).
Shen, J. et al. Prognostic value and influence of receptor conversion on treatment regimen in metastatic breast cancer at the first time of recurrence. Oncol. Res. Treat. 43, 620–627 (2020).
Dieci, M. V. et al. Discordance in receptor status between primary and recurrent breast cancer has a prognostic impact: a single-institution analysis. Ann. Oncol. 24, 101–108 (2013).
Paluch-Shimon, S. et al. ESO-ESMO 3rd international consensus guidelines for breast cancer in young women (BCY3). Breast 35, 203–217 (2017).
Al Sukhun, S., Koczwara, B., Temin, S. & Arun, B. K. Systemic Treatment of Patients With Metastatic Breast Cancer: ASCO Resource-Stratified Guideline Q and A. JCO Glob Oncol 10, e2300411 (2024).
Cardoso, F. et al. 6th and 7th International consensus guidelines for the management of advanced breast cancer (ABC guidelines 6 and 7). Breast 76, 103756 (2024).
Caswell-Jin, J. L. et al. Analysis of breast cancer mortality in the US-1975 to 2019. JAMA 331, 233–241 (2024).
Wolff, A. C. et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology–College of American Pathologists guideline update. Arch. Pathol. Lab. Med. 147, 993–1000 (2023).
Acknowledgements
The authors would like to thank all participants of EMBRACE. This study was supported by: NCCN/Pfizer Independent Grants for Learning & Change, Elaine and Eduardo Saverin Foundation, and the Pan-Mass Challenge (Team Duncan) (NUL); Susan G. Komen, and the Breast Cancer Research Foundation (AHP); and the National Cancer Institute (T32 CA009001) (KDB).
Author information
Authors and Affiliations
Contributions
Conceptualization – K.D.B. and N.U.L. Data curation – G.J.K., M.E.H., G.S., O.M.C., S.R., C.S. Formal analysis – K.D.B. Funding acquisition – N.U.L. and A.H.P. Investigation – K.D.B. and G.J.K. Methodology – K.D.B., M.E.H., N.U.L. Project administration – M.E.H, N.U.L. Resources – G.J.K., M.E.H. Software – G.J.K. Supervision – N.U.L., A.H.P. Validation – K.D.B. Visualization – K.D.B. Writing – original draft: K.D.B. Writing – review & editing: K.D.B., G.J.K., M.E.H., L.V., G.S., O.M.C., S.R., C.S., S.M.T., S.S., A.H.P., and N.U.L.
Corresponding author
Ethics declarations
Competing interests
S.M.T. reports consulting or advisory role for Novartis, Pfizer/SeaGen, Merck, Eli Lilly, AstraZeneca, Genentech/Roche, Eisai, Bristol Myers Squibb/Systimmune, Daiichi Sankyo, Gilead, Blueprint Medicines, Reveal Genomics, Sumitovant Biopharma, Artios Pharma, Menarini/Stemline, Aadi Bio, Bayer, Jazz Pharmaceuticals, Natera, Tango Therapeutics, eFFECTOR, Hengrui USA, Cullinan Oncology, Circle Pharma, Arvinas, BioNTech, Launch Therapeutics, Zuellig Pharma, Johnson&Johnson/Ambrx, Bicycle Therapeutics, BeiGene Therapeutics, Mersana, Summitt Therapeutics, Avenzo Therapeutics, Aktis Oncology, Celcuity, Boehringer Ingelheim, Samsung Bioepis, Olema Pharmaceuticals; research funding from Genentech/Roche, Merck, Exelixis, Pfizer, Lilly, Novartis, Bristol Myers Squibb, AstraZeneca, NanoString Technologies, Gilead, SeaGen, OncoPep, Daiichi Sankyo, Menarini/Stemline, Jazz Pharmaceuticals; travel support from Lilly, Gilead, Jazz Pharmaceuticals, Pfizer, Arvinas, Roche. S.S. reports institutional research funding from Daichi Sankyo, Relay Therapeutics, SEAGEN and Sermonix; and consulting/advisory fees from Astra Zeneca, Daichi Sankyo, Gilead, Eli Lilly, Incyclix, Pfizer, Sermonix, SEAGEN, and Novartis. N.U.L. reports institutional research support from Genentech, Pfizer, Merck, Seattle Genetics, Zion Pharmaceuticals, Olema Pharmaceuticals, AstraZeneca; consulting honoraria from Seattle Genetics, Daichii-Sankyo, AstraZeneca, Olema Pharmaceuticals, Janssen, Blueprint Medicines, Stemline/Menarini, Artera Inc., Eisai, Shorla Oncology; royalties from Up to date (book); and travel support from Olema, AstraZeneca, DSI. The remaining authors report no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brantley, K.D., Kirkner, G.J., Hughes, M.E. et al. The association between young age at metastatic breast cancer diagnosis and overall survival in the EMBRACE study. npj Breast Cancer 11, 96 (2025). https://doi.org/10.1038/s41523-025-00822-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41523-025-00822-y
This article is cited by
-
Navigating Breast Cancer in Young Adults: Diagnostic and Therapeutic Considerations
Current Breast Cancer Reports (2025)