Abstract
Meningiomas arise from arachnoid cells in the meninges surrounding the brain and spinal cord and are attributed to NF2 pathogenic variants in, approximately 60% of cases. Using exome sequencing, we found heterozygous germline variants in nine potential novel meningioma genes across four families and four sporadic cases. We then screened for germline and somatic variants in these genes and 11 known meningioma genes in 76 sporadic meningiomas blood/tumor pairs. We identified 18 germline and 58 somatic variants in 18 of the 20 genes, including seven of our newly proposed meningioma genes: CSMD3, EXTL3, FAT3, RAB44, RARA, RECQL4, and TNRC6A. Chromosomal abnormalities were identified in 39 of 49 tumors that also carried germline or somatic variants, with 71.8% encompassing NF2. This study provides potential novel genetic risk factors of meningiomas appropriate for further exploration from the greater scientific community and pathways to consider in the design of future therapeutic approaches.
Similar content being viewed by others
Introduction
Meningiomas are common primary intracranial tumors representing over 35% of all brain tumors1. Autopsy studies and incidental findings on brain imaging find subclinical meningiomas in over 3% of the population2. Most meningiomas are benign, but 20% can exhibit a malignant behavior with a recurrence or progressive course3. Multiple meningiomas occur in less than 10% of cases and 1–5% are familial4,5.
Variants in the neurofibromatosis type 2 gene (NF2; NM_000268) are the most prevalent cause of meningiomas and germline NF2 pathogenic variants are associated with multiple meningiomas6,7. While more than twenty genes have now been reported to have somatic variants in meningiomas, germline variants in small families and sporadic cases have only been observed in NF2, SUFU, SMARCE1 and SMARCB14,8. Recurrent somatic variants have also been observed in AKT1, TRAF7, TERT, SMO, KLF4, POLR2A, TP53, PTEN, which suggests that the dysregulation of several signaling pathways can contribute to the development of meningiomas9,10. Cases with variants in these genes often also have chromosomal abnormalities (CA), defined as large-scale insertions, deletions, inversions, or translocations of genomic material11. The most frequent is 22/del(22q) monosomy (NF2 locus) occurring in 50–70% of sporadic cases6,12; although, additional abnormalities, including losses, gains, or complex karyotypes, can occur.
Here, we aimed to identify novel germline variation that segregated in individuals with meningiomas by applying exome sequencing to four families, in addition to four sporadic cases with recurrent or multiple meningiomas, all of whom were negative for variants in NF2. We aimed to replicate our novel findings by screening 76 blood/tumor pairs from individuals with sporadic meningioma for germline and somatic variants with targeted sequencing. We also explored the landscape of CA across 144 tumors from individuals with meningiomas, including the 76 from the blood/tumor pairs.
Results
Candidate gene discovery
We performed germline whole exome sequencing on 20 individuals (13 affected and seven unaffected) from four families presenting with meningiomas. Family A presented with cranial and spinal meningiomas (World Health Organization [WHO] grade I), while families B, C and D presented with multiple cranial meningiomas (WHO grade I). Clinical details are listed in Supplementary Table 1.
Variants were filtered to identify those considered rare in the general population (minor allele frequency [MAF] < 0.001; The 1000 Genomes Project, NHLBI GO Exome Sequencing Project, Exome Aggregation Consortium (ExAC), Genome Aggregation Database (GnomAD) v2.1.1 non-cancer, gnomAD v3.1.2 non-cancer, and an in-house database of variation from ~5500 exomes and genomes) and those more likely to be pathogenic based on consensus of in silico pathogenicity prediciton and conservation tools (Supplementary Table 2). We also prioritized variants within genes involved in meningioma or cancer pathways or with proto-oncogenic or tumor suppressor function. We identified six genes with heterozygous germline variants segregating in the four families (Fig.1 and Supplementary Table 3). In family A, the four affected members (II-3, II-5, III-3, and III-5) were found to carry a heterozygous missense variant (c.26 C > T: p.P9L) in retinoic acid receptor α (RARA; NM_000964.4), which was not carried by the five unaffected family members. In family B, the three affected members (II-1, II-3, and II-4) were found to carry both a heterozygous missense variant (c.1255 A > G: p.K419E) in bone morphogenetic protein receptor 1 A (BMPR1A; NM_004329.3) and a heterozygous missense variant (c.224 C > T: p.S75F) in fibronectin type III domain containing 3B (FNDC3B; NM_022763.4). No unaffected family members were sequenced in family B. In family C, the three affected members (II-1, II-4, and II-5) were found to carry a heterozygous missense variant (c. 11546 G > A, p.R3849Q) in FAT atypical cadherin 3 tumor suppressor homolog (FAT3; NM_001367949.2). The variant was not identified in three members not affected with meningiomas (II-7, III-1, III-3) but was identified in two members not affected with meningiomas (II-8 and III-2), including one that presented with breast cancer (II-8). Finally, in family D, one affected member (IV-2) was found to carry both a heterozygous missense variant (c.31 G > A: p.D11N) in trinucleotide repeat containing 6 A (TNRC6A; NM_014494.4) and a heterozygous missense variant (c.1979G>A: p.R660Q) in exostosin like glycosyltransferase 3 (EXTL3; NM_001440.4), neither of which were carried by the unaffected family member that was sequenced.
Pedigrees of four families with meningiomas and variants segregating in each family. Family A: Four affected members of a German family with spinal and cranial meningiomas were hererozygous for missense variant p.Pro9Leu (rs762408148) in RARA. Family B: Two heterezygous missenses variants p.Lys419Glu and p.Ser75Phe in BMPR1A and FNDC3B, respectively, segregated in three affected members of a French family. Family C: In a family with Ashkenazi jewish origin, three affected members with multiple meningiomas and one unaffected member with breast cancer were heterozygous for the missense variant p.Arg3849Gln (rs375687974) in FAT3. Family D: Two heterozygous variants, p.Asp11Asn and p.Arg660Gln in TNRC6A and EXTL3, segregated in one affected member in a Moroccan family.
We also performed germline whole exome sequencing on four sporadic cases with recurrent or multiple meningiomas (WHO grade I and II; Supplementary Table 1). Following the variant filtration and prioritization described above, three sporadic cases (SP1, SP2, and SP4) were found to each carry one of three heterozygous variants: (1) a missense variant (c.2899 G > C: p.E967Q) in member RAS oncogene family (RAB44; NM_001257357.2), (2) a frameshift variant resulting in an early truncation (c.2980_2986del: p.N994Sfs*10) in CUB and sushi multiple domains 3 (CSMD3; NM_198123.2), and (3) a missense variant (c.C3227A: p.A1076D) in recQ like helicase 4 (RECQL4; NM_004260.4).
All genes in which variants of interest were identified in the analyzed families and sporadic cases have not previously been associated with meningiomas.
Meningioma gene replication
In an effort to replicate our newly identified meningioma genes, we used targeted sequencing to screen the nine genes described above, as well as 11 genes previously reported to carry variants in meningiomas (AKT1, CDKN2A, KLF4, NF2, SMARCB1, SMARCE1, SMO, SUFU, TRAF7, TERT, and TP53) in blood/tumor pairs from 76 sporadic meningioma cases. Again, variants were filtered and prioritized to identify those considered rare in the general population and more likely to be pathogenic based on consensus of in silico pathogenicity prediction and conservation tools. However, following the assumption that sporadic meningiomas are more frequent than familial, we applied a MAF filter of <0.005. We identified 76 variants across 18 of the 20 sequenced genes: AKT1, CDKN2A, CSMD3, EXTL3, FAT3, KLF4, NF2, RAB44, RARA, RECQL4, SMARCB1, SMARCE1, SMO, SUFU, TERT, TNRC6A, TP53, and TRAF7 (Supplementary Data 1). The 76 variants were identified in 49 of the 76 blood/tumor pairs (64.5%). Twenty-nine of the 76 variants (38.2%) were in seven of the nine proposed newly identified genes (CSMD3, EXTL3, FAT3, RAB44, RARA, RECQL4, and TNRC6A). Of these, 17 variants (58.6%) were in the germline and 12 (41.4%) were somatic events. The remaining 47 variants (61.8%) were identified in the previously reported meningioma genes in 38 of the 76 pairs (50.0%) (Fig. 2). Of these, 1 variant (2.1%) was in the germline and 46 (97.9%) were somatic events. No variants of interest were found in 27 of the 76 blood/tumor pairs (35.5%).
Distribution of 76 variants identified in 76 matched blood/tumor pairs. The variants were identified by targeted sequencing with an average coverage of 805X. Variants were rare (minor allele frequency <0.005) and predicted to be damaging or probably damaging and/or conserved by a consensus of in silico prediction tools. Figure generated using the R statistical software v4.1.1 ggplot2 package in RStudio v1.4.1717.
Chromosomal abnormality screening
We also aimed to determine the landscape of CA in meningiomas. In addition to the 76 blood/tumor pairs described above, we obtained 68 tumor samples from additional meningioma cases. All 144 sporadic cases had previously screened negative for NF2 variants using microsatellites for monosomy of chromosome 22 and Sanger sequencing of the NF2 gene in the blood/tumor pairs.
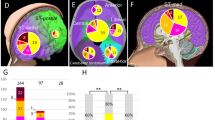
We used a high-density single-nucleotide polymorphism (SNP) array (CytoScanHD, Affymetrix) and calculated a cytogenetic abnormality score (CAS)13 for each of 141 meningiomas (three sample failures). The array identified 749 CA (Supplementary Data 2 and Supplementary Fig. 1). Complete or segmental deletion, duplication, or loss of heterozygosity (LOH) were observed at least once on all chromosomes and in 111 of all tumors examined (78.7%). Of the cases with CA, 54 had a CAS of 1–3 (48.6%), 22 had a CAS of 4–7 (19.8%), and 35 had a CAS > 7 (31.5%) (Fig. 3). Within the last category, 90% of the CA detected were abnormalities in chromosome 22 and encompassed either NF2 or SMARCB1 (Supplementary Fig. 1 and Table 1), and co-occurrences of CA encompassing NF2 and CA encompassing another gene within the same tumor were common (Supplementary Fig. 2). NF2 was also the gene with the most sequencing variants within our cases (26.3%) (Fig. 2). Yet, CA encompassing the sequenced genes were more common than sequence variants in all assessed genes except FAT3 and TRAF7 (Supplementary Fig. 3).
We estimated the CAS in each tumor by considering the abnormality in each chromosomal arm13. Gain and loss in the same arm or chromosome was considered as one CA. Segmental gain or segmental loss in more than one region in the same arm was considered as one chromosomal abnormality. Figure generated using the R statistical software v4.1.1 ggplot2 package in RStudio v1.4.1717.
Of the blood/tumor pairs encompassed within the replication cohort assessed for germline and somatic variation, 72 had usable CytoScanHD results to identify CA. Interestingly, of the 49 blood/tumor pairs from the replication cohort found to carry germline or somatic variants in the 20 assessed genes, 39 were found to also have at least one CA (79.6%) and 27 had CA encompassing NF2 (57.1%) (Fig. 4). Of these tumors with LOH or loss of NF2 and SMARCB1, 48.1% also carried a germline or somatic variant in one of the newly proposed meningioma genes and 77.8% carried a germline or somatic variant in a known meningioma gene, with 70.4% carrying a variant in NF2 (Supplementary Fig. 4). Greater chromosomal instability was also oberved in the tumors that had CA encompassing NF2 and SMARCB1 in addition to CA encompassing at least one of the newly proposed meningioma genes (n = 13), as demonstrated by 92.3% of these tumors having CAS > 5 (Supplementary Fig. 5). All tumors negative for LOH or loss of NF2 were also negative for germline or somatic NF2 variants in the sequencing analysis.
CA were identified using CytoHD in samples from 144 meningioma tumors and sequencing variants were identified in blood/tumor pairs from 76 meningioma cases using a targeted sequencing panel that included 11 genes previously associated with meningioma and nine meningioma genes discovered herein. Tumors were classified by World Health Organization (WHO) grades of meningiomas. Figure generated using the R statistical software v4.1.1 ggplot2 package in RStudio v1.4.1717.
Discussion
Previously, only four genes have been identified as harboring germline mutations in meningiomas: NF2, SUFU, SMARCE1 and SMARCB14,8,14. Here, we report nine new genes with germline variants in familial and sporadic cases of multiple or recurrent meningiomas and the replication of germline and somatic variants in seven of these genes in a secondary cohort of 76 blood/tumor pairs from individuals with meningiomas.
In the discovery phase of our analysis, we performed exome sequencing followed by variant filtration and prioritization to identify possibly pathogenic variants segregating with the phenotype in four families. Within family A, we identified a variant in the gene RARA that segregated within all four affected family members and was not identified in the five unaffected family members assessed. Upon validation, two germline missense variants of interest in RARA were found in one case from the replication cohort, who presented with a recurrent parietal meningioma (WHO grade II). The tumor of this patient had 8 CA, including segmental loss of 22q, as well as a somatic NF2 variant and a 17q segmental duplication where RARA is located. RARA has been associated acute promyelocytic leukemia (APL) through a PML-RARA fusion gene, and somatic variants of RARA were also observed in therapy-resistant PML and breast fibroepithelial neoplasms15. In contrast, a variant in each of the genes BMPR1A and FNDC3B was identified in the three affected members of family B, but there were no individuals with meningioma identified in the replication cohort with variants of interest in either of these genes. In recognition of the lack of replication of rare germline or somatic variants in these two genes in individuals with meningiomas, their implications for meningioma risk remain unclear.
FAT3 was identified as a potential new meningioma gene in Family C. While the variant was identified in two family members who have not presented with meningiomas, no brain imaging had been performed on these individuals to confirm that they did not have meningiomas, and it is unknown whether they may develop meningiomas in the future. Notably, up to 3% of the general population may have subclinical meningiomas that are unknown2,16. Upon replication analysis, FAT3 was the second most frequently altered gene, after NF2, with germline (n = 6 cases) or somatic variants (n = 4 cases) in 14% of the cohort. Interestingly, all variants identified were missense, allowing for their assessment with recently developed in silico prediction tools specific to amino acid substitutions. Of the ten variants, three had Rare Exome Variant Ensemble Learner (REVEL) or AlphaMissense scores suggesting potential for pathogenicity (Supplementary Data 1), and although five of the variants were observed in the Catalog of Somatic Mutations in Cancer (COSMIC) database, none of the variants are reported in meningiomas. All cases with FAT3 variants only had CAS of (0–1) and were tumors of WHO Grade I. Half of the cases had variants in the 19 remaining genes sequenced. Both NF2 and FAT3 encode tumor suppressors involved in the Hippo signaling pathway regulating cellular proliferation and apoptosis17, and dysregulation of this pathway is linked to several cancer events17, suggesting that FAT3 and NF2 pathogenic variants could have similar mechanisms and disrupt the Hippo signaling pathway at an early stage of tumorigenesis. FAT3 also belongs to a family of genes that are human orthologues of the Drosophila FAT genes family, which encode cadherin repeats, EGF-like domains, and a laminin G-like domain18. A missense variant within the cadherin domain of FAT2 was previously reported in spinal meningiomas19. Additionally, somatic variants in FAT1, FAT2, and FAT3 have previously been reported in various cancers (e.g., lung, esophageal squamous cell carcinoma, glioblastoma, breast, ovarian cancer, endometrial cancer, and early T-cell precursor acute lymphoblastic leukemia)20,21,22,23, most commonly affecting the cadherin repeats21,22. Cadherins are involved in cellular adhesion, and they are also upstream regulators of the Hippo pathway24. Eight of the ten FAT3 variants we identified were within the cadherin domains. RAB44 is another gene involved in the Hippo pathway that was found to harbor a variant in one of the individuals with sporadic meningiomas analyzed using exome sequencing, and it had mutations in 3.9% (3/76) of the blood/tumor pairs. The gene is a member of the RAB GTPase family has been associated with neurological disorders and cancer25,26. Nine cases with either FAT3 or RAB44 variants had normal to low CAS (1–3), thus suggesting FAT3 and RAB44 variants may be early tumorigenesis events.
Finally, rare variants of interest were identified in a single affected individual in family D in the genes TNRC6A and EXTL3, as well as in two individuals with sporadic meningiomas included in the discovery cohort in the genes CSMD3 and RECQL4. Variants within these genes were all replicated in the validation cohort, although with low variant frequency. TRAF7 and CSMD3 were tied as the third most frequently mutated genes. Of the replication cases, 9.2% (7/76) carried either germline or somatic variants in CSMD3. Germline missense variants of CSMD3 were previously reported in familial colorectal cancer and somatic missense variants in atypical fibroxanthoma and oral squamous cell carcinoma, breast cancer, and aggressive ovarian cancers27,28,29,30. Cases with variants in only CSMD3 had a low CAS (1–3). However, when these CSMD3 variants were carried along with loss of a wild-type copy of SUFU, RECQL4, or/and NF2, or with TP53 germline variants, CAS were higher (5–14). Although these variants may be driving the chromosomal instability that is resulting in the greater CAS, it remains possible that, in combination with these genomic events, the variants in CSMD3 might be contributing to the chromosomal instability with an oligogenic effect. TNRC6A and EXTL2 were also mutated at germline and somatic levels in the replication cohort, but at lower frequencies, limiting our understanding of their potential role in meningiomas. Somatic variants and loss of expression of TNRC6A have also been observed in gastric and colorectal cancers31,32, and its protein product’s inhibition impairs RNAi and microRNA-induced gene silencing, two pathways previously linked to the development of cancers31,32. Additionally, RECQL4 encodes a DNA unwinding helicase essential for DNA replication and repair33 that is thought to act as a tumor suppressor33. Deleterious RECQL4 germline variants cause type II Rothmund-Thomson syndrome (RTS), a recessive disorder characterised by premature aging and predisposition to cancer33, and an RTS patient has previously been reported to have atypical meningiomas (WHO grade II)34. However, it is important to note that RECQL4 variants were only identified in two replication cases, and both variants were identified in the germline. Further, RECQL4 has a higher-than-expected number of missense variants in population datasets, as demonstrated by its low missense constraint metric in gnomAD v4.1.0 (Z = −6.28), limiting the likelihood of the gene’s potential pathogenicity for meningiomas.
Four of our newly identified genes, RARA, TNRC6A, BMPR1A, and FNDC3B, were located within the same chromosomal region or are adjacent genes of known meningioma genes, including SMARCE1 and RARA in 17q21.2, TNRC6A and TRAF7 in 16p12.1-13.3, BMPR1A and SUFU in 10q23.2-10q24.32, and FNDC3B and PIK3CA in 3q26.31-26.32 (Table 1). Previous findings about gene neighborhoods suggest the proximity of the gene pairs may increase the likelihood of being involved in the same biological pathways35, and in many cancers, the disruption of chromosome neighborhoods induces proto-oncogenic activation36. Whether the proximity of these genes influences the pathological mechanisms of their potential roles in meningiomas warrants further exploration.
We were also able to identify variants of interest in known meningioma genes in our replication cohort using the targeted panel. Previously, CDKN2A pathogenic mutations described in meningiomas have only been somatic37, yet we identified a germline variant in CDKN2A. Conversely, meningioma germline mutations have been previously described in NF2, SMARCB1, SMARCE1, SUFU, and TP534,8,38,39,40,41. While we did identify one germline variant in each of SMARCB1 and SUFU and four germline variants in TP53, we also identified 36 somatic variants within these genes — 33 in NF2, five in TP53, and one in each of SMARCB1, SMARCE1, and SUFU. We also replicated the previously reported somatic meningioma genes AKT1, KLF4, SMO, TERT, and, TRAF79,10,42 with the identification of 41 somatic variants in the genes, contributing additional evidence to their role in tumorigenesis of meningiomas.
Although the replication cohort had been previously screened for LOH of chromosome 22 using microsatellites and NF2 variants using Sanger sequencing and were considered NF2 negative, abnormalities affecting the NF2 locus were detected in 50% of our expanded replication cohort upon CA analysis (71/141). Therefore, we propose that the frequency of CA involving chromosome 22q may be higher than the current estimates of 50–70%; the sensitivity of the method used appears to be critical6,43. Of the 71 CA involving NF2, a complete loss or LOH of 22q was seen in 71.8% (51/71) of cases, and segmental loss or LOH in 22.1% (15/71) of cases, suggesting that the previous microsatellite genotyping had missed many events. When we analyzed the CA identified in the blood/tumor pairs sequenced for somatic and germline variants, we found that of those carrying both a germline or somatic variant in one of the sequenced genes and a LOH or loss of NF2 and SMARCB1, 77.8% carried a variant in NF2, supporting the previously described two-hit hypothesis of NF2 inactivation in cancer development44. Furthermore, 48.1% (n = 13) of individuals carried a germline or somatic variant in one of our newly proposed meningioma genes along with a LOH or loss of NF2 and SMARCB1, including eight individuals who also carried a variant in a known meningioma gene and five individuals that did not also have a variant in a known meningioma gene. In combination with the high CAS observed in these individuals, representative of high chromosomal instability, the finding suggests that our newly proposed genes may also be contributing to the development of meningiomas through increased genomic instability.
While we were able to replicate many of our novel findings in a secondary cohort, we recognize the limitations of our analyses. For the discovery analysis within the four families and four sporadic meningioma cases, we only assessed germline variation using exome sequencing. Therefore, we could not identify somatic variation that could be of interest in meningioma cases and may have missed additional novel meningioma candidate genes. We also did not perform microarray analysis on these samples, preventing the identification of CA that may have been relevant to the individuals’ phenotypes. Further, we did not observe the recurrence of variants of interest in the same genes across the assessed families in the discovery cohort. This remained unsurprising as the families all had differing ancestral backgrounds, including German, French, Ashkenazi Jewish, and North African, and the individuals with meningiomas within the families presented with distinct meningioma localization, recurrence, and subtypes, all of which may have contributed to the lack of gene recurrence between them. Finally, while we were able to validate the presence of variants of interest in seven of the nine novel meningioma candidate genes in a secondary cohort, we cannot confirm that the variants we identified are pathogenic and have yet to fully understand how variants in these genes may be contributing to the phenotype. Rather than suggesting that these genes are definitively associated with meningiomas, we present them to the greater scientific community as candidates for further replication across families and within case-control cohorts. Additional functional analyses will be required to elucidate the pathophysiology of the potential gene-disease associations.
In conclusion, we identified and replicated the presence of variants in seven newly identified potential genes for familial and sporadic meningioma — CSMD3, EXTL3, FAT3, RAB44, RARA, RECQL4, and TNRC6A. While the known meningioma gene, NF2, was found to have the greatest frequency of variants in our replication cohort, our novel gene, FAT3 had the second highest variant frequency in the sporadic meningioma cases. Within our replication cohort, we also identified somatic or germline variants of interest in ten additional known meningioma genes — CDKN2A, AKT1, KLF4, NF2, SMARCB1, SMARCE1, SMO, SUFU, TRAF7, TERT, and TP53 — and investigated the landscape of CA in meningiomas. Interestingly, we found that ~50% of the replication cohort carried CA affecting NF2, even though they had been pre-screened for these events, suggesting that CA detection in meningiomas may require a more sensitive methodology than is commonly used. In sum, our report of seven newly identified genes and replication of previously associated genes validates and may expand the genetic landscape of meningiomas that could be explored for the development of new therapies.
Methods
Ethics statement
Informed consent were obtained from all individuals involved. The study was conducted according to the ethical standards of the Declaration of Helsinki and was approved by the Research Ethics Board of the McGill University Health Center, Montréal, Quebec (IRB00010120).
Discovery phase specimens and exome capture
Genomic DNA was extracted from peripheral blood lymphoblasts and saliva using standard protocols from 26 individuals; 11 affected and 11 unaffected, from 4 families (A, B, C and D) and 4 sporadic cases (Fig. 1). 3–5 µg of blood DNA from 24 individuals (A.II.1, A.II.3, A.II.5, A.III.1, A.III.3, A.III.5, A.III.7, A.III.8, A.III.9, B.II.1, B.II.3, B.II.4, C.II.1, C.II.4, C.II.5, C.II.7, C.II.8, C.III.1, C.III.2, C.III.3, SP1, SP2, SP3 and SP4) and saliva DNA from two individuals (D.IV.2, D.IV.4) were used. To prepare libraries, Agilent SureSelect® Human All Exon V4 (Agilent Technologies, Santa Clara, CA) kits were used for eight samples (C.II.1, C.II.4, C.II.5, C.II.7, C.II.8, C.III.1, C.III.2, and C.III.3), Nextera® XT DNA Sample Preparation Kit (Illumina, San Diego, CA) were used for nine samples (A.II.1, A.II.3, A.II.5, A.III.1, A.III.3, A.III.5, A.III.7, A.III.8 and A.III.9) and NimbleGen SeqCap EZ® Exome v3 kits (Roche, Basel, Switzerland) were used for nine samples (B.II.1, B.II.3, B.II.4, D.IV.2, D.IV.4, SP1, SP2, SP3 and SP4) according to the manufacturer’s instructions.
Validation phase specimens and MIPs capture
144 tumors were obtained from unrelated patients undergoing surgical excision of meningiomas non irradiated, with 76 having blood/tumor pairs available. They all had no Loss of Heterozygozity (LOH) of chromosome 22 (loss of the NF2 gene) using microsatellites and no known, pathogenic NF2 mutations using Sanger Sequencing. DNA was extracted from fresh tissues and blood using standard protocols. A total of 100 ng of DNA was used for molecular inverted probes (MIPs) to capture the coding and adjacent regions (+20 bp) of 20 genes, with 1,439 MIPs spanning 330 exons designed using scripts developed in Dr. Jay Shendure’s laboratory (http://krishna.gs.washington.edu/mip_pipeline). In addition to the nine genes identified within the discovery phase of our analysis, 11 known meningioma associated genes were assessed, including only those with replicated evdience of an association, such as those previously reported within COSMIC as accounting for >3% of somatic meningioma cases, and excluding genes only associated with meningiomas through only genome wide association analyses (GWAS). Primers are detailed in Supplementary Data 3.
Sequencing and bioinformatics analysis
Exome DNA captures were sequenced with Illumina HiSeq 2000 platform and MIPs captures were sequenced with Illumina HiSeq 4000, at the “McGill University and Génome Québec Innovation Center” and Pharmacogenomics Center, Université de Montreal. Sequence reads generated by exome sequencing or MIPs were mapped and aligned to Human Reference Genome GRCh37 using the Burrows-Wheeler Aligner (BWA) (v0.7.5). GATK tools and ANNOVAR were used to call and to annotate single nucleotide variants and indels.
Prioritization of variants
Discovery phase
The exome sequencing of all individuals with meningioma included in the discovery phase of the analysis was first assessed for likely pathogenic or pathogenic variants in known meningioma-associated genes and were found to be variant negative. The exome sequencing data were then filtered to identify nonsynonymous, frameshift, stop gain, and splice-site variants with MAF <0.001 in The 1000 Genomes Project, NHLBI GO Exome Sequencing Project, ExAC, GnomAD v2.1.1 non-cancer, GnomAD v3.1.2 non-cancer, and an in-house database of variation from ~5500 exomes and genomes. Additional filters were also used, including prediction of consequences of the variants on the proteins, conservations and involvement in tumor pathways. Details of filtering process are reported in Supplementary Table 2. We used prediction and conservation tools, Sorting Intolerant From Tolerant (SIFT), Likelihood Ratio Test (LTR), PolyPhen 2, MutationTaster, and Functional Analysis through Hidden Markov Models (FATHMM) to predict the pathogenicity, and PhyloP, Phastcons, and Genomic Evolutionary Rate Profiling (GERP)++ to evaluate the conservation of the variants. We considered variants predicted to be damaging or probably damaging by at least three prediction tools and highly conserved by at least two conservation tools. Finally, we used a Residual Variation Intolerance Score (RVIS) filter to select only variants within genes intolerant to mutations, specifically with a score below 20%. Following variant filtration, we prioritized variants within genes involved in meningioma or cancer pathways or connected to genes involved in meningioma using STRING Functional Protein Association Networks (https://string-db.org/). Variants within genes with proto-oncogenic or tumor suppressor function were also considered, even if not involved in the aforementioned pathways. We focused on variants co-segregating with the disease in an autosomal dominant manner in familial and sporadic cases. In family D, because of the consanguinity of the parents, the autosomal recessive model was also considered.
Sanger sequencing
To validate the variants identified and confirm co-segregation with the disease, we performed PCR using available DNA from affected and unaffected family members and nine pairs of primers detailed in (Supplementary Table 4). PCR amplification was conducted in a total of 15 μl reaction, containing 5 ng of genomic DNA, 1X buffer, 1.5 mM final concentration of MgCl2, 2 μl of Q-Solution (Qiagen, Valencia, CA), 0.5 mM dNTP, 0.5 mM of each primer, and 0.12 U Qiagen Taq DNA Polymerase (QIAGEN, Valencia, CA). Following initial denaturation at 96 °C for 10 min, PCR was carried out in 35 cycles of 96 °C for 30 s, 61 °C for 30 s, and 72 °C for 30 s. A final elongation was at 72 °C for 7 min. The PCR fragments were detected by gel electrophoresis analysis and sequenced by Sanger sequencing (Applied Biosystem’s 3730xl DNA Analyzer technology). We used Mutation surveyor’s V.4.0 to confirm the variants.
Validation phase
The average coverage of the MIPs for the 20 assessed genes was 805X in the 76 blood/tumor pairs (details by sample in Supplementary Data 4). A total of 554 variants were identified. We focused on nonsynonymous, frame-shift, stop gain, and splice-site variants with 99 genotype quality and >10% of variant allele frequency. Variants were considered germline if identified in both the blood and tumor. Assuming that sporadic is more frequent than familial meningioma, we filtered for variants with MAF <0.005 in The 1000 Genomes Project, NHLBI GO Exome Sequencing Project, ExAC, GnomAD v2.1.1 non-cancer, GnomAD v3.1.2 non-cancer, and an in-house database of variation from ~5500 exomes and genomes. Variants were retained that were predicted to be damaging or probably damaging by at least three of five prediction tools (SIFT, LTR, PolyPhen 2, MutationTaster, and FATHMM) and highly conserved by at least two of three conservation tools (PhyloP, Phastcons and GERP++).
Chromosomal abnormality analysis
We analysed 144 meningioma tumors (including the 76 tumors analyzed by deep sequencing) using Affymetrix CytoScanHD microarrays. Genotyping was performed at The Center for Applied Genomics of The Hospital for Sick Children, Toronto, according to the manufacturer’s instructions (Santa Clara, CA, U.S.A). We used the Chromosome Analysis Suite (ChAS) 3.3.0 software package (Santa Clara, CA, U.S.A.) to detect CA. The threshold of CA detection was set at >5000 kb and >200 markers. In the chromosomal regions of the known meningioma genes and our newly identified genes, the threshold was >1000 kb and >100 markers. We excluded all CA seen in the Database of Genomic Variants (DGV; http://projects.tcag.ca/variation/). Four tumors were not analyzed because of low-quality DNA and were not processed.
Data availability
Raw data were generated at “McGill University and Génome Québec Innovation Center”. Derived data supporting the findings of this study are available from the corresponding author (GAR) on request. All variants identified in the study have been deposited into the ClinVar database (ClinVar Accession Numbers: SCV005902277–SCV005902303).
References
Wiemels, J., Wrensch, M. & Claus, E. B. Epidemiology and etiology of meningioma. J. Neuro-Oncol. 99, 307–314 (2010).
Vernooij, M. W. et al. Incidental findings on brain MRI in the general population. N. Engl. J. Med. 357, 1821–1828 (2007).
Preusser, M., Brastianos, P. K. & Mawrin, C. Advances in meningioma genetics: novel therapeutic opportunities. Nat. Rev. Neurol. https://doi.org/10.1038/nrneurol.2017.168
Aavikko, M. et al. Loss of SUFU function in familial multiple meningioma. Am. J. Hum. Genet. 91, 520–526 (2012).
Nahser, H. C., Grote, W., Lohr, E. & Gerhard, L. Multiple meningiomas. Clinical and computer tomographic observations. Neuroradiology 21, 259–263 (1981).
Rouleau, G. A. et al. Genetic linkage of bilateral acoustic neurofibromatosis to a DNA marker on chromosome 22. Nature 329, 246–248 (1987).
Rouleau, G. A. et al. Alteration in a new gene encoding a putative membrane-organizing protein causes neuro-fibromatosis type 2. Nature 363, 515–521 (1993).
Christiaans, I. et al. Germline SMARCB1 mutation and somatic NF2 mutations in familial multiple meningiomas. J. Med. Genet. 48, 93–97 (2011).
Clark, V. E. et al. Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO. Science 339, 1077–1080 (2013).
Clark, V. E. et al. Recurrent somatic mutations in POLR2A define a distinct subset of meningiomas. Nat. Genet. 48, 1253–1259 (2016).
Domingues, P. et al. Genetic/molecular alterations of meningiomas and the signaling pathways targeted. Oncotarget 6, 10671–10688 (2015).
Ruttledge, M. H. et al. Evidence for the complete inactivation of the NF2 gene in the majority of sporadic meningiomas. Nat. Genet. 6, 180–184 (1994).
Aizer, A. A. et al. A prognostic cytogenetic scoring system to guide the adjuvant management of patients with atypical meningioma. Neuro-Oncol. 18, 269–274 (2016).
Smith, M. J. et al. Loss-of-function mutations in SMARCE1 cause an inherited disorder of multiple spinal meningiomas. Nat. Genet. 45, 295–298 (2013).
Tan, J. et al. Genomic landscapes of breast fibroepithelial tumors. Nat. Genet. 47, 1341–1345 (2015).
Krampla, W. et al. Frequency and risk factors for meningioma in clinically healthy 75-year-old patients: results of the Transdanube Ageing Study (VITA). Cancer 100, 1208–1212 (2004).
Baia, G. S., Caballero, O. L. & Riggins, G. J. The Hippo signaling pathway and translational opportunities for brain cancers. CNS Oncol. 1, 113–115 (2012).
Katoh, M. Function and cancer genomics of FAT family genes (review). Int. J. Oncol. 41, 1913–1918 (2012).
Tate, G., Kishimoto, K. & Mitsuya, T. A novel mutation of the FAT2 gene in spinal meningioma. Oncol. Lett. 12, 3393–3396 (2016).
Longacre, M. et al. A comparative analysis of genetic and epigenetic events of breast and ovarian cancer related to Tumorigenesis. Int. J. Mol. Sci. 17 https://doi.org/10.3390/ijms17050759
Lin, D. C. et al. Genomic and molecular characterization of esophageal squamous cell carcinoma. Nat. Genet. 46, 467–473 (2014).
Furukawa, T. et al. Whole exome sequencing reveals recurrent mutations in BRCA2 and FAT genes in acinar cell carcinomas of the pancreas. Sci. Rep. 5, 8829 (2015).
Cancer Genome Atlas Research, N. Integrated genomic analyses of ovarian carcinoma. Nature 474, 609–615 (2011).
Kourtidis, A., Lu, R., Pence, L. J. & Anastasiadis, P. Z. A central role for cadherin signaling in cancer. Exp. Cell Res. 358, 78–85 (2017).
Ioannou, M. S. & McPherson, P. S. Regulation of Cancer Cell Behavior by the Small GTPase Rab13. J. Biol. Chem. 291, 9929–9937 (2016).
Moya, I. M. & Halder, G. Discovering the Hippo pathway protein-protein interactome. Cell Res. 24, 137–138 (2014).
Maru, Y. et al. Identification of novel mutations in Japanese ovarian clear cell carcinoma patients using optimized targeted NGS for clinical diagnosis. Gynecol. Oncol. 144, 377–383 (2017).
Gylfe, A. E. et al. Somatic mutations and germline sequence variants in patients with familial colorectal cancer. Int. J. cancer 127, 2974–2980 (2010).
Lai, K. et al. Genomic analysis of atypical fibroxanthoma. PloS One 12, e0188272 (2017).
Al-Hebshi, N. N. et al. Exome sequencing of oral squamous cell carcinoma in users of Arabian snuff reveals novel candidates for driver genes. Int. J. Cancer 139, 363–372 (2016).
Kim, M. S. et al. Somatic mutations and losses of expression of microRNA regulation-related genes AGO2 and TNRC6A in gastric and colorectal cancers. J. Pathol. 221, 139–146 (2010).
Hafner, M. et al. Transcriptome-wide identification of RNA-binding protein and microRNA target sites by PAR-CLIP. Cell 141, 129–141 (2010).
Arora, A. et al. RECQL4 helicase has oncogenic potential in sporadic breast cancers. J. Pathol. 238, 495–501 (2016).
Pencovich, N., Margalit, N. & Constantini, S. Atypical meningioma as a solitary malignancy in a patient with Rothmund-Thompson syndrome. Surg. Neurol. Int. 3, 148 (2012).
Thevenin, A., Ein-Dor, L., Ozery-Flato, M. & Shamir, R. Functional gene groups are concentrated within chromosomes, among chromosomes and in the nuclear space of the human genome. Nucleic Acids Res. 42, 9854–9861 (2014).
Hnisz, D. et al. Activation of proto-oncogenes by disruption of chromosome neighborhoods. Science 351, 1454–1458 (2016).
Hayward, N. K. Genetics of melanoma predisposition. Oncogene 22, 3053–3062 (2003).
Sanson, M. et al. Germline deletion in a neurofibromatosis type 2 kindred inactivates the NF2 gene and a candidate meningioma locus. Hum. Mol. Genet. 2, 1215–1220 (1993).
Ammerlaan, A. C. et al. Long-term survival and transmission of INI1-mutation via nonpenetrant males in a family with rhabdoid tumour predisposition syndrome. Br. J. Cancer 98, 474–479 (2008).
Smith, M. J. et al. Germline SMARCE1 mutations predispose to both spinal and cranial clear cell meningiomas. J. Pathol. 234, 436–440 (2014).
Hong, C. S., Erson-Omay, E. Z. & Moliterno, J. Multiple meningiomas arising within the same hemisphere associated with Li-Fraumeni syndrome. Surg. Neurol. Int. 12, 99 (2021).
Wang, J. L. et al. Detection of TP53 gene mutation in human meningiomas: a study using immunohistochemistry, polymerase chain reaction/single-strand conformation polymorphism and DNA sequencing techniques on paraffin-embedded samples. Int. J. Cancer 64, 223–228 (1995).
Galani, V. et al. Genetic and epigenetic alterations in meningiomas. Clin. Neurol. Neurosurg. 158, 119–125 (2017).
Cheng, J. Q. et al. Frequent mutations of NF2 and allelic loss from chromosome band 22q12 in malignant mesothelioma: evidence for a two-hit mechanism of NF2 inactivation. Genes Chromosomes Cancer 24, 238–242 (1999).
Acknowledgements
We thank the families and patients for their participation. This study was funded by the Canadian Institutes for Health Research (CIHR). We thank Cathy Mirarchi and Sam Dougaparsad for their assistance.
Author information
Authors and Affiliations
Contributions
Conception and design of the work (B.O.A., J.G.), Data collection (G.A.R., J.L., R.L.M., J.P.S., S.-M.P.), Data analysis and interpretation (B.O.A., A.A.D., S.B.L., A.A., D.S., A.D.P., J.L.), Drafting the article (B.O.A.), Critical revision of the article (A.A.D., G.A.R., S.-M.P., S.M.K.F., P.A.D.).
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41525_2025_494_MOESM2_ESM.xlsx
Supplementary Data 1: Variants identified by targeted sequencing of 20 new and known meningioma genes in 76 blood/tumor pairs
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bencheikh, B.O.A., Dilliott, A.A., Gauthier, J. et al. Novel germline and somatic variants in familial and sporadic meningioma genes. npj Genom. Med. 10, 41 (2025). https://doi.org/10.1038/s41525-025-00494-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41525-025-00494-4