Abstract
More people are traveling to space for longer durations than ever before. Many long-duration flyers exhibit signs of Spaceflight Associated Neuro-ocular Syndrome (SANS). A greater understanding of the mechanisms and predictors of SANS may lead to new, more individually tailored countermeasures. Our objective here was to determine whether brain and ocular changes with spaceflight are related to each other and/or to crewmember demographic factors, including sex, age, body mass index, and prior spaceflight experience. We assessed brain change and ocular change associations and predictive models of changes in a cohort study. Our samples included 30 crewmembers with brain MRI but not ocular metrics, 37 with ocular but not brain MRI, and 22 with both sets of data. Approximately 25% of participants in each of these samples were female. Females showed greater free water reduction around the vertex of the brain from pre- to postflight than males. While not statistically significant, the odds ratio of males developing signs of SANS was approximately three times higher than for females. Unlike in past smaller studies, we found no association between brain changes and the development of signs of SANS. Interpretation of these findings should be tempered by the fact that our sample included a relatively small number of females.
Similar content being viewed by others
Introduction
Understanding spaceflight’s effects on the central nervous system is critical in light of plans to return to the moon, for the first human missions to Mars, and the burgeoning space tourism industry. Spaceflight has been shown to induce structural brain changes1,2,3,4,5,6,7,8,9,10,11,12,13 and, in approximately 70% of astronauts, a constellation of neuro-ocular structural abnormalities collectively known as Spaceflight Associated Neuro-ocular Syndrome (SANS)14,15,16. Signs of SANS include optic disc edema, choroidal folds, globe flattening, and refractive error shift16. It is important to identify whether and how demographic variables are risk factors for brain and ocular changes with spaceflight.
There are known age- and sex-differences in brain structure17,18,19,20 and the brain’s neuroplastic response to experiences such as training18 and stress20. Sex differences in brain changes with spaceflight are largely unexplored, and only one study has examined the effects of age4. Studies have begun examining associations between brain and ocular changes with spaceflight6,11, with a couple of studies showing associations between SANS and ventricular volume changes. Marshall-Goebel et al. found that spaceflight-associated changes in total retinal thickness were correlated with increases in ventricular volume11, but not with total brain white matter volume. In contrast, another study observed larger changes in ventricular volumes in crewmembers who did not show signs of SANS4.
Most SANS cases have been reported among male crewmembers21,22, raising the possibility that females are protected against SANS. However, more recent reports indicate SANS occurrence in both sexes23,24. Previous proposals of sex differences in SANS occurrence may have been driven by the underrepresentation of female crewmembers in samples and/or confounded by sex differences in body weight, which has been linked to SANS development22. In contrast, though, Pardon et al. reported that crewmember age, sex, body weight, and prior flight experience were not associated with the extent of optic disc edema developed during long-duration spaceflight24. It remains unclear whether crewmember demographic factors are associated with other signs of SANS25.
It is evident that we have little understanding of whether or how spaceflight-induced ocular and brain changes differ based on crewmember age, sex, and SANS status, and whether these changes relate to each other. Here, we investigated this issue by examining voxel-wise pre- to post-flight changes in brain structure and intracranial fluid shifts in a relatively large astronaut sample. We additionally performed follow-up analyses testing whether crewmember demographic factors are associated with brain changes and increased risk of SANS development.
Results
Study samples
Participants were astronauts who completed short- (weeks) or long- (months) duration missions onboard the International Space Station (ISS). In total, data from 37 astronauts were included in the analyses. These astronauts were separated into 3 samples based on the availability of MRI and/or ocular data (see Table 1). Participants overlapped across samples. Sample 1 (MRI only) consisted of 30 crewmembers for whom both T1-weighted and diffusion-weighted MRI (dMRI) scans were acquired pre- and post-flight. Within Sample 1, data from 15 crewmembers were prospectively collected26, and data from 15 were acquired retrospectively and accessed via the NASA Lifetime Surveillance of Astronaut Health Repository. Sample 2 (MRI and Ocular) was a subset of Sample 1, consisting of 22 crewmembers who consented to share their ocular exam data (described below). Sample 3 (Ocular only) consisted of data from 37 crewmembers for whom ocular exam results were available, and the crewmembers consented to data sharing.
We have previously published the pre to postflight brain changes for sample 127. Similar to our past work8,9,10, we found decreasing free water (FW) and increasing gray matter volume (GMv) around the vertex of the brain, increasing FM and decreasing GMv around the lower portions of the brain, and ventricular expansion. Here, we focus on whether and how demographic factors interact with brain and ocular changes, and whether brain and ocular changes are related to each other across the three samples.
Associations with age
Our voxel-wise brain analyses revealed no statistically significant associations between crewmember age and pre- to post-flight brain changes. Ventricular volume changes were also not related to crewmember age (see Table 2).
Sex differences
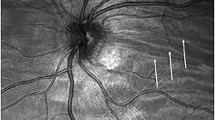
Our tests for sex differences in spaceflight-induced brain changes yielded a statistically significant result with respect to pre- to post-flight changes in FW fractional volume in clusters within the medial superior parietal and paracentral lobules and within the right postcentral gyrus (Fig. 1). While both males and females showed FW volume decreases within these regions from pre- to post-flight, the extent of the FW decrease was greater for female crewmembers. We observed no statistically significant results for sex differences with respect to the other brain structural changes examined.
The rendered brains on the left show clusters for which male and female crewmembers exhibited differential changes in FW volume from pre- to post-flight. The plot on the right shows the average FW volume across all significant clusters for male (light blue markers) and female (dark blue markers) crewmembers pre- and post-flight. Sample sizes of the subgroups are indicated in gray. Error bars represent standard error. Results are family-wise error corrected at p < 0.05, two-tailed. R indicates the right hemisphere.
SANS Status
Approximately 56.7% of Sample 3 (i.e., 21 of 37) developed SANS during their mission. Upon analysis of Sample 2 (a subset of 22 of those 37 crewmembers from whom both MRI and ocular measures were acquired), we observed no statistically significant differences in pre- to post-flight brain changes between the SANS and NoSANS subgroups.
SANS demographics analyses
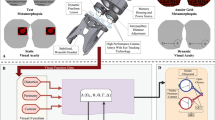
For qualitative purposes, Fig. 2 shows SANS frequency within Sample 3 (n = 37) as a function of demographic, anthropometric and spaceflight experience factors. Qualitatively, SANS prevalence was lower in astronauts who are female (Fig. 2A), younger (Fig. 2B), or with a lower body mass index (BMI) (Fig. 2C). In terms of current and previous spaceflight experience, SANS frequency was higher for 1 year-long missions (Fig. 2D; though this datapoint is based only on 4 crewmembers) and was comparable between novice and experienced crewmembers (Fig. 2E).
Frequency of SANS development as a function of A crewmember sex, B age (to protect anonymity, crewmembers have been divided into quartiles (Q1-Q4) based on their age at launch), C body mass index (divided into quartiles (Q1-Q4) based on their body mass index at launch), D mission duration (2 weeks (2 W), 6 months (6 M), or 1 year (1YR)), and E prior flight experience. Novice refers to crewmembers with no prior spaceflight experience. Experienced refers to crewmembers who have completed one or more previous missions. Actual counts are indicated within each bar; white numbers in the colored portion refer to those with SANS, black numbers within the gray portion refer to those without SANS. SANS, Spaceflight-Associated Neuro-Ocular Syndrome.
The binomial logistic regression model testing the effects of crewmember age, sex, and mission duration on the likelihood of SANS development was not statistically reliable (\(\chi\)2(3) = 4.82, p = 0.185). Table 3 shows model predictor coefficients and odd ratios. Notably, though non-significant, this model indicated that male crewmembers in this sample were over 3 times more likely to develop SANS during flight compared to female crewmembers.
Additional models that also included pre-flight BMI or body weight were also not statistically significant (\(\chi\)2(4) = 4.48, p = 0.34 and \(\chi\)2(4) = 4.54, p = 0.33, respectively). Table 4 shows the predictor coefficients and odd ratios of the model including pre-flight BMI. As in the model results above, male crewmembers were over 2.8 times more likely to develop SANS during spaceflight compared to female crewmembers. Results of the models, including pre-flight BMI and weight, were highly similar.
Figure 3 shows the frequency of each sign of SANS within the SANS subgroup (n = 21/37 in sample 3). Notably, all SANS cases included change in globe flattening (though globe flattening data were unavailable for 3 crewmembers). In 61.9% of SANS cases (i.e., 13 of 21), change in globe flattening was the only sign of SANS present.
Figure 4 shows a breakdown of SANS signs occurrence according to crewmember demographics, anthropometric characteristics, and spaceflight experience. All 4 signs of SANS occurred in the male crewmembers, but only refractive error shift and change in globe flattening occurred in female crewmembers with SANS (Fig. 4A). When our sample was stratified according to crewmember age (Fig. 4B), the occurrence of SANS signs was qualitatively similar across crewmember age quartiles. When stratified according to pre-flight BMI (Fig. 3C), those crewmembers in the lowest BMI quartile (Q1) did not develop optic disc edema, choroidal shifts, or refractive error shift during spaceflight. With respect to current mission duration, none of the crewmembers developed optic disc edema or refractive error shifts following a short duration spaceflight (Fig. 2D). Frequency of SANS signs development was qualitatively similar between those crewmembers who were first-time flyers (Novice) and those with prior spaceflight experience (having completed one or more prior missions, Experienced) (Fig. 2E).
A Frequency of each sign of SANS among male (n = 18) and female (n = 3) crewmembers. Actual counts are indicated in white within each bar. B Frequency of each sign with each age quartile (Q). C Frequency of each sign with body mass index quartile (Q). D Frequency of each sign of SANS following 2-week (2 W, n = 5), 6-month (6 M; n = 13), and 1-year (1YR; n = 3) missions. E Frequency of each sign of SANS for novice (n = 8) and experienced (n = 13) crewmembers. Change in globe flattening data was unavailable for 3 crewmembers. BMI data were unavailable for 3 crewmembers. SANS Spaceflight Associated Neuro-ocular Syndrome.
Discussion
Several studies have previously reported ventricular expansion and brain fluid and GMv changes with spaceflight2,4,5,6,8,9,10. Data from the current sample that we published previously shows the same pattern, with fluid decreases and GMv increases seen around the vertex and the opposite pattern around the lower portions of the brain27. Here, we examined demographic interactions with these brain changes and ocular changes occurring with spaceflight. We found that spaceflight-induced regional structural brain changes do not differ based on crewmember age or SANS status, a novel finding with our sample, which is larger than in past studies. We identified sex differences in FW regional changes following spaceflight, but the incidence of SANS was not related to this measure. Sex differences have been identified in cardiovascular changes with spaceflight, with women being more prone to post-flight orthostatic intolerance than men28,29. Post-flight orthostatic intolerance is related to fluid shifts that occur in microgravity and then reverse upon return to Earth. However, given that SANS status was unrelated to FW change, the functional implications of the greater FW change in females remain unclear.
Although the model was not statistically significant, males showed a three times greater odds ratio for SANS incidence than females in our sample. Wostyn and De Deyn proposed that greater optic nerve sheath compliance may allow for better compensation for cerebrospinal fluid build-up behind the eye, decreasing SANS incidence30. Optic nerve sheath stiffness is less in women than men, which may contribute to the higher incidence of SANS in men31. Additional studies are needed to better understand sex differences in SANS incidence with spaceflight, as reports have included very few female crewmembers. More women have been traveling to space recently, which should allow for greater focus on this issue. In fact, a recent case study reported some of the largest SANS effects in a female crewmember; these changes then reversed course inflight. It is not clear whether the improvements were associated with the B vitamin supplementation that was given or a concurrent decrease in CO2 that occurred on station at the same time32.
We observed no associations between crewmember age and any of the brain structural changes examined. Roberts et al. have previously reported that older crewmembers showed smaller ventricular volume increases with spaceflight compared to younger crewmembers4. It may be that this reported age difference reflects reduced tissue compliance with advancing age, but we did not replicate this effect. Our demographic analysis further found that age was also not a predictor of SANS development, with the pattern of SANS signs being qualitatively similar across quartiles spanning the 20-year age range of our sample. Moreover, similar to what was previously reported for optic disc edema24, we did not find a significant association between body mass index and signs of SANS.
The etiology of SANS is unknown, but a leading hypothesis posits that SANS is caused by impaired cerebrospinal fluid outflow and/or cerebral venous congestion resulting from microgravity-induced headward fluid shifts33. Noninvasive measures of intracranial pressure are not elevated in microgravity, but they also do not vary with body position throughout the day as they do on Earth34. We found no associations between SANS development and pre- to post-flight changes in either ventricular volume or free water volume. Roberts et al. have shown that crewmembers who developed SANS (indicated by optic disc edema and/or choroidal folds) exhibited smaller post-flight ventricular enlargement and had evidence of enlargement of dural venous sinuses compared to crewmembers who did not4,6,35. Another study reported no association of SANS with changes in either whole-brain white matter volume or intracranial volume11. Our findings are consistent with those of Marshall-Goebel and colleagues11, suggesting that in-flight intracranial fluid changes may not mechanistically lead to SANS. Fluid alterations may occur outside of the cranium for instance, via impeded flow through the jugular veins and vertebral venous plexuses35. Furthermore, many other factors have been proposed to contribute to SANS, including hypercapnia, high salt diets, resistive exercises, and dysfunction in 1-carbon metabolism pathways36.
Approximately 57% of crewmembers in our sample developed SANS, and, in over half of those cases, a change in globe flattening was the sole sign of SANS present. This finding has important implications for interpreting previous studies in which SANS status was based only on the presence of optic disc edema4,6,11,21 and/or choroidal folds4,6,21. Omitting the change in globe flattening has likely resulted in false negatives in SANS classification. This may be especially true for female crewmembers with SANS, who here showed a qualitatively different profile of SANS signs compared to males. Females with SANS did not present with either optic disc edema or choroidal folds, instead showing a combination of changes in globe flattening and/or refractive error shift. We interpret this finding with caution as it is based on a subsample of only three crewmembers, but these preliminary results suggest that sex differences in SANS presentation may be an important consideration in future studies of SANS.
As in many spaceflight studies, our sample size is small, particularly in terms of female crewmembers (n = 3). Moreover, in some cases, MRI scan parameters varied across participants or over time. Some of the data here came from our prospective NASA study26, while other samples were acquired through the NASA Life Sciences Data Archive; thus, data acquisition parameters were beyond our control. We also had missing data for a few participants. Despite this, the data presented here are unique and reflect a large sample in comparison to much of the literature on this topic.
We also did not consider ocular changes on a continuous scale to factor in subclinical changes. Post-flight optic disc edema requires between 30–90 days to return to near baseline levels23, while globe flattening shows only partial recovery 1 year post-flight37. As such, some of the experienced crewmembers may have also had residual subclinical ocular changes from a previous flight.
In sum, we show for the first time that spaceflight-induced brain changes, characterized by FW shifts, ventricular volume changes, and GMv changes, are not associated with crewmember age or SANS status. Females showed greater free water decreases near the brain vertex than males. We found that all SANS cases in these samples included a change in globe flattening, and in 62% of cases, this was the only sign. This finding underscores the importance of this metric when evaluating SANS. We found that males were approximately three times more likely than females to show signs of SANS, but this effect was not statistically significant.
Methods
All astronauts provided written informed consent to participate in procedures approved by Institutional Review Boards at the University of Michigan, the University of Florida, and NASA Johnson Space Center.
SANS Definition
We obtained ocular exam results from the NASA Lifetime Surveillance of Astronaut Health Repository. A crewmember was deemed to have SANS if any of the following signs were present in either eye post-flight (but not pre-flight): optic disc edema, choroidal folds, hyperopic refractive error shifts >0.75 diopters, or change in globe flattening (mild to severe)16. All instances of optic disc edema were rated as Frisén Grade 1. Globe flattening data were unavailable for 3 crewmembers who were otherwise deemed to have SANS.
Image acquisition
All neuroimaging data were acquired using the same 3 T Siemens Magnetom Verio MRI scanner located at the University of Texas Medical Branch at Victory Lake in Houston, TX. T1-weighted anatomical images were collected using a magnetization-prepared rapid gradient-echo (MPRAGE) sequence with the following parameters: TR = 1900 ms, TE = 2.32 ms, flip angle = 9°, FOV = 250 × 250 mm, 176 sagittal slices of 0.9 mm thickness, matrix = 512 × 512, voxel size = 0.488 × 0.488 × 0.9 mm.
Diffusion-weighted MRI (dMRI) scans were acquired using a 2D single-shot spin-echo prepared echo-planar imaging sequence. Prospective dMRI scans used the following parameters: TR = 11300 ms, TE = 95 ms, flip angle = 90°, FOV = 250 × 250 mm, matrix size = 128 × 128, 40 axial slices of 2 mm thickness (no gap), voxel size = 1.95 × 1.95 × 2 mm. One b = 0 s/mm2 and thirty non-collinear gradient directions with diffusion weighting of b = 1000 s/mm2 were sampled twice. Retrospective dMRI scans were collected using the following parameters: TR = 5800 ms, TE = 95 ms, flip angle = 90°, FOV = 250 × 250 mm, matrix size = 128 × 128, 40 axial slices of 3.9 mm thickness (no gap), voxel size = 1.95 × 1.95 × 3.9 mm. One b = 0 s/mm2 and twenty non-collinear gradient directions with diffusion weighting of b = 1000 s/mm2 were sampled three times. For 9 retrospective crewmembers, voxel dimensions were altered to 1.8 × 1.8 × 3.9 mm for 9 pre-flight and 1 post-flight scans. For 4 retrospective crewmembers, repetition times were also altered for 4 pre-flight scans (TR = 5846, 5500, 5900, 5600 ms) and 1 post-flight scan (TR = 5302 ms).
Image preprocessing
MRI data were included in analyses with samples 1 and 2. MRI processing methods are detailed below.
T1-weighted images were preprocessed using the Computational Anatomy Toolbox38 (CAT12.6 v.1450) for Statistical Parametric Mapping39 version 12 (SPM12 v.7219) and MATLAB R2016a, version 9.0. T1 images were skull stripped and segmented in CAT12, yielding gray matter segments, which were used in gray matter volume (GMv) analyses (see below). CAT12 provided estimates of the native space intracranial volume and the volumes of the left lateral, right lateral, third, and fourth ventricles.
Our dMRI preprocessing and free water (FW) estimation procedure has been previously detailed9,40. FW refers to extracellular water molecules that do not experience flow and whose diffusion is not restricted by their surroundings41. Preprocessing entailed visual inspection, eddy current correction, and motion correction using the FMRIB Software Library (FSL) version 6.0.142, then removal of outlier volumes (>1 mm inter-volume root mean square displacement) or volumes with visually evident artifacts.
We estimated FW and FW-corrected diffusion indices using a custom FW algorithm41 implemented in MATLAB R2018b. This algorithm fits a two-compartment model to each voxel. The FW compartment models freely-diffusing water molecules as isotropic diffusion with a diffusion coefficient of water at body temperature (3 × 10−3 mm2/s). The FW compartment fit yields FW maps reflecting per-voxel FW fractional volume with values ranging between 0 and 1, where 1 indicates a voxel is filled with freely-diffusing water molecules. The tissue compartment uses a diffusion tensor to model the remaining diffusion of hindered or restricted water molecules within white matter41 to estimate FW-corrected measures of fractional anisotropy (FAT), axial diffusivity (ADT), and radial diffusivity (RDT). The subscript T signifies that a diffusion index is based on the tissue compartment.
To improve within-subject image registration, we used a multi-step process in which native space images were normalized to standard space via subject-specific templates. This process used Advanced normalization tools (ANTs) version 1.9.1743,44 and has been previously described8,10,27,40. Briefly, native space images were registered to a subject-specific template, which was then registered to an MNI standard space template. Transformations used for individual registration steps were concatenated into flow fields and then applied individually to each native space preprocessed image (T1, FW, and FW-corrected diffusion maps).
We quantified voxel-wise GM changes from pre- to post-flight as in our previous work9,10. Flow fields generated during the T1 normalization procedure above were inputted to ANTs’ CreateJacobianDeterminantImage.sh function to create a Jacobian determinant image, which encodes voxelwise expansion and shrinkage. Each Jacobian determinant image was multiplied by its corresponding MNI-normalized GM segment. This yielded modulated GM segments that quantify local GM apparent expansion and shrinkage while preserving the amount of GM present in the original T1 image.
For each astronaut, we calculated pre- to post-flight difference images for each image type, which were then concatenated across subjects and submitted to randomise (FSL’s GLM-based tool for nonparametric permutation-based inference45, detailed below). Analyses were performed within a whole-brain mask. DTI analyses were performed within a white matter mask created by thresholding MNI normalized FA maps at 0.2 and retaining voxels in which white matter was present in more than half of the sample8. MNI-normalized FW maps and FW-corrected diffusion indices were smoothed using a 5 mm full width at half maximum (FWHM) Gaussian kernel. Modulated GM segments were smoothed using an 8 mm FWHM Gaussian kernel.
Statistical analyses
We performed separate voxel-wise statistical analyses on GMv, FW, FAT, RDT, and ADT difference images using randomise45. For each statistical test (below) we performed 15,000 random permutations with threshold-free cluster enhancement46 and familywise error correction at p < 0.05 (two-tailed). Our three models tested for post-flight brain changes that 1) were associated with crewmember age, 2) differed based on crewmember sex, and 3) differed between crewmembers who did versus did not develop SANS. Age-based and sex-based MRI analyses were performed using Sample 1 (MRI, n = 30). SANS-related MRI analyses were performed using Sample 2 (MRI and ocular, n = 22). All Models included covariates to adjust for individual differences in current mission duration (in days), the number of days between landing and the post-flight MRI scan, age at the time of launch, and sex (except where age or sex was the predictor of interest). GMv analyses also adjusted for pre-flight total intracranial volume.
We also assessed pre- to post-flight changes in ventricular volume for each of the 4 ventricles separately. These analyses used the native space ventricle volume estimates outputted by CAT12. Analyses were conducted using linear mixed models implemented in R version 4.1.2 using the nlme package47. Models used random intercepts, random slopes, and restricted maximum likelihood. The Benjamini-Hochberg procedure was used to maintain the false discovery rate at 0.0548. The same covariates were used as above, along with pre-flight total intracranial volume to account for differences in head size.
We performed follow-up analyses testing whether development of SANS could be predicted based on crewmember demographics such as age, sex, or current mission duration. SANS demographic analyses were performed on Sample 3 (Ocular, n = 37). We conducted binomial logistic regressions in R version 4.1.2. SANS status was used as a dependent variable. Predictor variables included age at launch, sex, and mission duration. The significance level was set at p < 0.05. Since higher pre-flight body weight has previously been associated with SANS development22, we ran two additional models including either pre-flight weight or pre-flight body mass index (BMI) as predictors. Weight and BMI data were unavailable for 3 crewmembers; thus, these models were carried out on sample sizes of 34.
Data availability
The data presented here are available upon request to the NASA Life Sciences Data Archives, https://nlsp.nasa.gov/explore/lsdahome.
Code availability
N/A.
References
Van Ombergen, A. et al. Brain Tissue-volume changes in cosmonauts. N. Engl. J. Med. 379, 1678–1680 (2018).
Van Ombergen, A. et al. Brain venticular volume changes induced by long-duration spaceflight. PNAS 116, 10531–10536 (2019).
Jillings, S. et al. Macro- and microstructural changes in cosmonauts’ brains after long-duration spaceflight.Sci. Adv 6, 1–12 (2020).
Roberts, D. et al. Prolonged microgravity affects human brain structure and function. AJNR Am. J. Neuroradiol. 40, 1878–1885 (2019).
Roberts, D. et al. Effects of spaceflight on astronaut brain structure as indicated on MRI. N. Engl. J. Med. 377, 1746–1753 (2017).
Roberts, D. R. et al. Longitudinal change in ventricular volume is accelerated in astronauts undergoing long-duration spaceflight. Aging Brain 3, 1–8 (2021).
Kramer, L. A. et al. Intracranial effects of microgravity: A prospective longitudinal MRI study. Radiology 295, 640–648 (2020).
Lee, J. et al. Spaceflight-associated brain white matter microstrucural changes and intracranial fluid redistribution. JAMA Neurol. 76, 412–419 (2019).
Hupfeld, K. E. & et al. RD; Alzheimer’s Disease Neuroimaging Initiative., The impact of 6 and 12 months in space on human brain structure and intracranial fluid shifts. Cereb. Cortex Commun 1, tgaa023 (2020).
Koppelmans, V., Bloomberg, J., Mulavara, A. P., Seidler, R. D., Brain structural plasticity with spaceflight. npj Microgravity. 2: p. https://doi.org/10.1038/s41526-016-0001-9 (2016).
Marshall-Goebel, K. et al. Assocation of structural changes in the brain and retina after long-duration spaceflight. JAMA Ophthalmol. 139, 781–784 (2021).
Alperin, N., Bagci, A. M., Lee, S. H., Spaceflight-induced changes in white matter hyperintensity burden in astronauts. Neurology. https://doi.org/10.1212/WNL.0000000000004475 (2017).
Riascos, R. F. et al. Longitudinal analysis of quantitative brain MRI in astronauts following microgravity exposure. J. Neuroimaging 29, 323–330 (2019).
Wostyn, P., Gibson, C. R. & Mader, T. H. The odyssey of the ocular and cerebrospinal fluids during a mission to Mars: the “ocular glymphatic system” under pressure. Eye 36, 686–691 (2022).
Mader, T. et al. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology 118, 2058–2069 (2011).
Lee, A. G. et al. Spaceflight associated neuro-ocular syndrome (SANS) and the neuro-ophthalmologic effects of microgravity: a review and update. npj Microgravity 6, 7 (2020).
Seidler, R. D. et al. Motor control and aging: Links to age-related brain structural, functional, and biochemical effects. Neurosci. Biobehav. Rev. 34, 721–733 (2010).
Wenger, E. et al. Cortical thickness changes following spatial navigation training in adulthood and aging. Neuroimage 59, 3389–3397 (2012).
Persson, J. et al. Sex differences in volume and structural covariance of the anterior and posterior hippocampus. Neuroimage 99, 215–225 (2014).
Cahill, L. Why sex matters for neuroscience. Nat. Rev. Neurosci. 7, 477–484 (2006).
Wahlin, A. et al. Optic nerve length before and after spaceflight. Ophthalmology 128, 309–316 (2021).
Buckey, J. C. et al. Mcrogravity-induced ocular changes are related to body weight. Am. J. Physiol. 315, R496–R499 (2018).
Macias, B. R. et al. Association of long-duration spaceflight with anterior and posterior ocular structure changes in astronauts and their recovery. JAMA Ophthalmol. 138, 553–559 (2020).
Pardon, L. P. et al. Identification of factors associated with the development of optic disc edema during spaceflight. JAMA Ophthalmol. 140, 1193–1200 (2022).
Seidler, R. D. et al. Future research directions to identify risks and mitigation strategies for neurostructural, ocular, and behavioral changes induced by human spaceflight: a NASA-ESA expert group consensus report. Front. Neural Circuits 16, 876789 (2022).
Koppelmans, V. et al. RD, Study protocol to examine the effects of spaceflight and a spaceflight analog on neurocognitive performance: extent, longevity and neural bases. BMC Neurol. 13, 205 (2013).
Mcgregor, H. R. et al. Impacts of spaceflight experience on human brain structure. Sci. Rep. 13, 7878 (2023).
Waters, W. W., Ziegler, M. G. & Meck, J. V. Postspaceflight orthostatic hypotension occurs mostly in women and is predicted by low vascular resistance. J. Appl. Physiol. 92, 586–594 (2002).
Harm, D. L. et al. Invited review: gender issues related to spaceflight: a NASA perspective. J. Appl. Physiol. 91, 2374–2383 (2001).
Wostyn, P., De & Deyn, P. P. The “Ocular Glymphatic System”: An important missing piece in the puzzle of optic disc edema in astronauts?. Invest. Ophthalmol. Vis. Sci. 59, 2090–2091 (2018).
Lee, C. et al. In vivo estimation of optic nerve sheath stiffness using noninvasive MRI measurements and finite element modeling. J. Mech. Behav. Biomed. Mater. 110, 103924 (2020).
Brunstetter, T. J. et al. Severe spaceflight-associated neuro-ocular Syndrome in an Astronaut with 2 predisposing factors. JAMA Ophthalmol. 142, 808–817 (2024).
Ong, J. et al. Spaceflight associated neuro-ocular syndrome: proposed pathogenesis, terrestrial analogues, and emerging countermeasures. Br. J. Ophthalmol. 107, 895–900 (2023).
Jasien, J. V. et al. Noninvasive indicators of intracranial pressure before, during, and after long-duration spaceflight. J. Appl Physiol. 133, 721–731 (2022).
Rosenberg, M. J. et al. Comparison of dural venous sinus volumes before and after flight in astronauts with and without spaceflight-associated neuro-ocular syndrome. JAMA Netw. Open 4, e2131465 (2021).
Patel, Z. S. et al. Red risks for a journey to the red planet: The highest priority human health risks for a mission to Mars. npj Microgravity 6, 33 (2020).
Sater, S. H. et al. Automated MRI-based quantification of posterior ocular globe flattening and recovery after long-duration spaceflight. Eye35, 1869–1878 (2021).
Gaser C, Dahnke R, Thompson PM, Kurth F, Luders E, The Alzheimer's Disease Neuroimaging Initiative. CAT: a computational anatomy toolbox for the analysis of structural MRI data. Gigascience. 2024 Jan 2;13:giae049. https://doi.org/10.1093/gigascience/giae049. PMID: 39102518; PMCID: PMC11299546.
Penny, W. D., Friston, K. J., Ashburner, J. T., Kiebel, S. J., Nichols, T. E., Statistical parametric mapping: the analysis of functional brain images. Elsevier. (2011).
McGregor, H. R. et al. Case report: No evience of intracranial fluid shifts in an astronaut following an aborted Launch.Front. Neurol 12, 774805 (2021).
Pasternak, O., Sochen, N., Gur, Y., Intrator, N. & Assaf, Y. Free water elimination and mapping from diffusion MRI. Magn. Reson. Med. 62, 717–730 (2009).
Jenkinson, M., Beckmann, C. F., Behrens, T. E., Woolrich, M. W. & Smith, S. M. Fsl. Neuroimage 62, 782–790 (2012).
Avants, B. et al. A reproducible evalutation of ANTs similarity metric performance in brain image registration. Neuroimage 45, 2033–2044 (2011).
Avants, B. B. et al. The optimal template effect in hippocampus studies of diseased populations. Neuroimage 49, 2457–2466 (2010).
Winkler, A. M., Ridgway, G. R., Webster, M. A., Smith, S. M. & Nichols, T. E. Permutation inference for the general linear model. Neuroimage 92, 381–397 (2014).
Smith, S. M. & Nichols, T. E. Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage 44, 83–98 (2009).
Ezzet, F., Pinheiro, J. C. Linear, generalized linear, and nonlinear mixed effects models. Wiley. (2006).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc.: Ser. B (Methodol.) 57, 289–300 (1995).
Acknowledgements
This study was supported by NASA grant #NNX11AR02G awarded to RDS, SJW, PARL, and JJB. HRM was supported by an NSERC postdoctoral fellowship, a Translational Research Institute for Space Health Postdoctoral Fellowship, and a NASA Human Research Program augmentation grant. KEH was supported by National Institute on Aging fellowships F99AG068440 and K00AG068440.
Author information
Authors and Affiliations
Contributions
H.R.M. preprocessed the diffusion MRI scans, performed image normalization, and all statistical analyses. K.E.H. preprocessed the gray matter and ventricular volume data. N.E.B. and Y.E.D. collected data. O.P. designed the free water analysis pipeline and consulted on interpretation. H.R.M., R.D.S., J.J.B., S.J.W., P.A.R.L., designed the experiment and secured funding. H.R.M. drafted the manuscript and created all of the figures and tables. H.R.M., K.E.H., O.P., S.J.W., J.J.B., R.D.S. edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
N.E.B. and Y.E.D. are employed by KBR. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
McGregor, H.R., Hupfeld, K.E., Pasternak, O. et al. Crewmember demographic factors and their association with brain and ocular changes following spaceflight. npj Microgravity 11, 59 (2025). https://doi.org/10.1038/s41526-025-00505-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41526-025-00505-9