Abstract
The D620N variant in Vacuolar Protein Sorting 35 (VPS35) causes autosomal-dominant, late-onset Parkinson’s disease. VPS35 is a core subunit of the retromer complex that canonically recycles transmembrane cargo from sorting endosomes. Although retromer cargoes include many synaptic proteins, VPS35’s neuronal functions are poorly understood. To investigate the consequences of the Parkinson’s mutation, striatal neurotransmission was assessed in 1- to 6-month-old VPS35 D620N knock-in (VKI) mice. Spontaneous and optogenetically-evoked corticostriatal glutamate transmission was increased in VKI spiny projection neurons by 6 months and was unaffected by acute leucine-rich repeat kinase 2 (LRRK2) inhibition. Total striatal glutamate release by iGluSnFR imaging was similar to wild-type. dLight imaging revealed robust increases in VKI striatal dopamine release by 6 months, which were reversed with acute LRRK2 kinase inhibition. We conclude that increased striatal neurotransmission in VKI mice progressively emerges in young-adulthood, and that dopamine dysfunction is likely the result of sustained, rapidly-reversible, LRRK2 hyperactivity.
Similar content being viewed by others
Introduction
A simplified definition of Parkinson’s disease (PD) is that of a movement disorder, resulting from the death of dopamine neurons in the substantia nigra pars compacta (SNpc). Within ~4 years of clinical presentation, there is an almost complete loss of nigrostriatal dopamine axon markers. Whereas, the loss of nigral neurons is less severe (30–60%) and remains fairly stable thereafter1. The resilience of a population of nigral neurons1, and the restorative effect of dopamine replacement therapy (e.g., L-DOPA) against motor symptoms2 offer hope that at least some function can be restored in remaining neurons after disease onset.
Unfortunately, no available PD treatment has been shown to slow or prevent disease progression. Furthermore, several disturbances that precede motor dysfunction by many years, e.g., rapid eye movement (REM) sleep behaviour disorder, anosmia, constipation, mood changes, and cognitive decline; are unresponsive to L-DOPA3,4,5. Many neuronal populations in addition to nigral dopamine neurons degenerate in PD; notably in the pedunculopontine nucleus and locus coeruleus containing cholinergic and noradrenergic neurons, as well as glutamatergic nuclei in the cortex and thalamus6,7,8. Thus, multiple neurotransmitter systems are implicated in both early symptom manifestation and disease progression.
A point of convergence of multiple neurotransmitter systems implicated are the spiny projection neurons (SPNs) of the dorsolateral striatum9,10,11. SPNs integrate extensive cortical and thalamic glutamate input with modulation by nigrostriatal dopamine to direct behavioural action selection via downstream basal ganglia nuclei12. Too much extracellular striatal glutamate and dopamine transmission may be toxic13,14,15,16,17,18,19, and could act as the initial pathophysiological stress that causes retrograde degeneration and selective loss of SNpc dopaminergic inputs8,20.
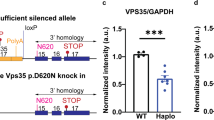
PD is thought to emerge from the combination of genetic predisposition and environmental stress, especially age21. To investigate how these factors precipitate a Parkinsonian state, we developed VKI mice expressing the VPS35 D620N variant linked to clinically-typical PD22,23,24,25,26. Heterozygote VKI mice (which model the autosomal dominant presentation in humans) develop tau pathology and nigral loss at >16 months27,28. Thus, VKI mice model human PD pathology at advanced ages and are appropriate for the study of early pathophysiological mechanisms.
We previously reported increased glutamate transmission in VKI cortical cultures and increased dopamine release in brain slices of young VKI mice22,23. These changes correlated with hyperphosphorylation of leucine-rich repeat kinase 2 (LRRK2) substrates, the kinase believed to be hyperactive in LRRK2-familial and idiopathic PD21,22,23,29. In cultures, despite reversal of LRRK2 substrate hyperphosphorylation, glutamate alterations were resistant to LRRK2 inhibition23. Contrastingly, 1-week in vivo LRRK2 kinase inhibition rescued decreased dopamine transporter (DAT) protein levels, and normalized dopamine release in VKI brain slices24.
Here we sought to define the emergence of synaptic glutamate and dopamine dysfunction as young VKI mice mature, and test whether acute LRRK2 kinase inhibition modifies release. We found that glutamate and dopamine transmission become elevated by 6 months of age. Elevated dopamine, but not glutamate, release was rapidly reversed by acute (≥1.5 h) LRRK2 kinase inhibition of slices, without evidence of changes to DAT function. We conclude that striatal glutamate and dopamine transmission is progressively increased in VKI mice throughout young adulthood, and that augmented dopamine release is a function of LRRK2 kinase hyperactivity. The data support the argument that LRRK2 inhibition is likely beneficial against synaptic dysfunction in PD and provide a model framework in which to test the neuroprotective potential of LRRK2 inhibitors.
Results
VKI SPNs show progressive increase in spontaneous activity by 6 months
We compared spontaneous excitatory postsynaptic currents (sEPSCs) by whole-cell patch-clamp as before30 in VKI and WT SPNs from 1-, 3-, and 6-month-old mice (Fig. 1A). Although similar at 1 month, we found that VKI sEPSCs begin to diverge from WT at 3 months with larger amplitudes. VKIs exhibit robustly elevated amplitude and frequency (ie. reduced inter-event interval) by 6 months (Fig. 1B–D). The decay of sEPSCs was faster in VKI SPNs at 3 months but normalized to WT levels at 6 months. An age-dependent decrease in WT sEPSC amplitude and frequency was absent in VKI SPNs (Supplementary Table 2).
A i) Schematic depicting whole-cell patch-clamp recording of spiny projection neurons (SPNs) in the dorsolateral striatum (STR) from acute coronal brain sections also containing cortex (CTX). ii) Representative trace of voltage-clamp recording of spontaneous excitatory post-synaptic current (sEPSC) from dorsolateral striatal SPNs. Representations of amplitude, inter-event interval, and decay tau measurements annotated in red. B At 1 month, i) cumulative probability distributions of sEPSC amplitude are not significantly different between VKI and WT SPNs (2-way ANOVA Interaction p > 0.99, genotype p = 0.22). ii) Cumulative probability distributions of inter-event intervals are not significantly different between VKI and WT SPNs (2-way ANOVA interaction p = 0.99, genotype p = 0.93). iii) sEPSC decay tau is not significantly different between VKI and WT SPNs (Unpaired t-test p = 0.43). C At 3 months, i) cumulative probability distributions show VKI SPNs have more, larger amplitude sEPSC than WT SPNs (2-way ANOVA interaction p = 0.02, genotype p = 0.21). ii) sEPSC inter-event intervals are not significantly different between genotypes (2-way ANOVA interaction p = 0.10, genotype p = 0.95). iii) Average sEPSC decay tau is significantly faster in VKI vs WT neurons (Mann-Whitney U-test p = 0.01). D At 6 months, i) cumulative distributions show a significantly higher number of larger-amplitude sEPSCs in VKI neurons (2-way ANOVA interaction p < 0.0001, genotype p = 0.02). ii) Cumulative distributions of sEPSC inter-event intervals indicate VKI neurons have shorter inter-event intervals than WT neurons (2-way ANOVA interaction p < 0.0001, genotype p = 0.06). iii) Average sEPSC decay taus are not significantly different in VKI vs WT neurons (Mann-Whitney U-test p = 0.65). Asterisks denote pairwise comparisons; * 0.05>p > 0.01, ** 0.01>p > 0.001, *** 0.001>p > 0.0001, **** p > 0.0001. 2-way ANOVA comparisons listed if p < 0.10.
We also observed early reductions in membrane tau of 1-month-old VKI SPNs, that normalized to WT levels by 3 months (Supplementary Fig. 1A, B, C iii). VKI SPNs also trend towards increased membrane capacitance at 3- and 6-months, but not at 1 month (Supplementary Fig. 1A, B, C i). Membrane resistance was reduced by 6 months in VKI SPNs (Supplementary Fig. 1A, B, C, ii). As with sEPSC properties, membrane capacitance and resistance measures were altered with age within WT SPNs, but not in VKI neurons (Supplementary Table 2). Together, age-dependent changes to passive membrane properties, and a progressive (relative) increase in the amplitude, frequency, and decay of spontaneous glutamate transmission is observed in VKI SPNs.
Corticostriatal glutamate transmission is progressively increased in VKI mice by 6 months
To determine whether increased frequency and amplitude of sEPSCs are due to changes in corticostriatal inputs, optogenetic stimulation of glutamate release onto patched SPNs was conducted at 3 and 6 months (Fig. 2A i). Light stimulation of local cortical terminals generated ChR2-induced post-synaptic currents (ChR2-PSCs). Glutamatergic currents through AMPA and NMDA receptors were isolated by membrane gating properties (ie. holding potential) and by pharmacology with the NMDAR blocker, D-AP5 (Fig. 2A ii). At 3 months, we found no change to VKI AMPAR- or NMDAR-mediated current amplitude. The ratio of NMDA:AMPA current and AMPAR-rectification indices were likewise similar (Fig. 2B). In contrast, we found AMPAR and NMDAR currents were both equally elevated in 6-month-old VKIs (Fig. 2C i-ii). There was no change in NMDA:AMPA ratio, or AMPA rectification index at this age (Fig. 2C iii-iv).
A i) Schematic depicting ChR2 viral injection into motor cortex 4–6 weeks prior to preparation of acute coronal slices containing CTX and STR. Whole-cell patch-clamp recordings were obtained from dorsolateral striatal SPNs +/- NMDAR inhibitor, APV. ii) Representative ChR2-PSC traces in response to single pulses of light. SPNs that were held at membrane potentials of -70 mV or +40 mV (in black), and +40 mV in the presence of AP5 (in cyan). B At 3 months, i) the peak amplitude of AMPAR-mediated currents at -70 mV are not significantly different between WT and VKI SPNs (Unpaired t-test p = 0.46). ii) Amplitude of NMDAR-mediated currents are not significantly different between genotypes at +40 mV (Unpaired t-test p = 0.87). iii) Ratios of +40 mV NMDAR current to -70 mV AMPAR current are not significantly different between WT and VKI SPNs (Unpaired t-test p = 0.60). iv) Rectification Index of AMPA current is not significantly different between WT and VKI SPNs (Unpaired t-test p = 0.45). C At 6 months, i) VKI SPNs show larger currents than WT SPNs, in peak amplitude of both AMPAR-mediated current (Mann-Whitney U-test p = 0.01) and ii) NMDAR-mediated current (Unpaired t-test p = 0.0005). iii) Ratio of NMDA:AMPA currents are not significantly different between genotypes (Unpaired t-test p = 0.90). iv) AMPA Rectification Index is not significantly different between WT and VKI SPNs (Unpaired t-test p = 0.67). D i) Representative ChR2-PSCs with 4 pulses of ChR2 stimulation (in red), 100 ms inter-pulse interval. ii) At 3 months, the paired pulse ratio (PPR) of 4 responses to ChR2 stimulation, normalized to the first response, is not significantly different between VKI and WT SPNs (2-way ANOVA interaction p = 0.34, genotype p = 0.22). iii) At 6 months, the paired pulse ratio is significantly reduced in VKI vs WT SPNs (2-way ANOVA interaction p = 0.001, genotype p = 0.04).
To assess presynaptic probability of release, we quantified paired pulse ratios (PPRs) at 100 ms intervals (Fig. 2D). There was no significant difference to PPRs in VKI neurons at 3 months, but a significant reduction in PPR was observed in 6-month-old VKI SPNs, indicative of elevated probability of presynaptic release (Pr). Taken together, the data show corticostriatal glutamate transmission becomes elevated in VKI SPNs, relative to WT littermates, and that this correlates with an equivalent increase in both AMPAR and NMDAR transmission.
Spontaneous and corticostriatal glutamate transmission in SPNs is not altered with acute LRRK2 kinase inhibition
Previously, we showed that in young VKIs, LRRK2 kinase activity was elevated and could be reversed with acute inhibition using MLi-223. At 6-months-old, we found that VKIs remain elevated in Rab12 phosphorylation and that this hyperphosphorylation can be reduced to WT levels with >1.5 h bath incubation with MLi-2 (Supplementary Fig. 2A and B). Next, we tested whether a similar treatment paradigm could reduce elevated glutamate transmission in 6-month-old VKI SPNs (Fig. 3). We found that MLi-2 treatment did not alter spontaneous amplitude, frequency, or decay in either WT or VKI SPNs relative to vehicle (Fig. 3A–C). Further, it did not alter ChR2-evoked PPRs at corticostriatal synapses (Fig. 3D). Therefore, glutamatergic transmission onto SPNs are not affected by acute LRRK2 kinase inhibition in either WT or VKI mice.
A sEPSC cumulative probability distributions were analyzed together and displayed by genotype. Statistics were performed using 2-way ANOVA on WT veh vs VKI veh vs WT MLi-2 vs VKI MLi-2 with relevant post-hoc comparisons. i) WT sEPSC amplitude is not differentially distributed with acute MLi-2 treatment when compared to vehicle (veh) control (2-way ANOVA interaction p = 0.72, genotype p = 0.86, Šídák’s multiple comparisons test p=ns). ii) MLi-2 treatment does not alter cumulative probability distributions of inter-event intervals in WT SPNs (2-way ANOVA interaction p = 0 > 0.99, genotype p = 0.65, Šídák’s multiple comparisons test p=ns). B i) VKI sEPSC amplitudes are not altered in cumulative probability distributions with MLi-2 treatment when compared to vehicle control (Šídák’s multiple comparisons test p=ns). ii) MLi-2 treatment does not alter cumulative probability distributions of inter-event intervals in VKI SPNs Šídák’s multiple comparisons test p = ns). C sEPSC decay is not altered by MLi-2 treatment in either WT or VKI SPNs (Kruskal-Wallis test p = 0.62). D PPRs of ChR2 responses were analyzed together and displayed by genotype. Statistics were performed using 2-way ANOVA on WT veh vs VKI veh vs WT MLi-2 vs VKI MLi-2 with relevant post-hoc comparisons. i) PPRs of WT SPN responses to ChR2 stimulation were not altered by MLi-2 treatment when compared to vehicle treatment (2-way ANOVA interaction p = 0.41, genotype p = 0.80, Šídák’s multiple comparisons test p=ns). ii) PPRs of VKI SPN responses to ChR2 stimulation were not altered by MLi-2 treatment when compared to vehicle treatment (Šídák’s multiple comparisons test p=ns).
Total striatal glutamate release appears reduced in 3-month-old VKIs and normalizes to WT levels by 6 months
In addition to changes in presynaptic release, glutamate currents recorded in SPNs are modulated by regulation of postsynaptic responsiveness, thalamic glutamate, midbrain dopamine, and GABAergic interneuron activity31,32,33,34,35,36,37,38. To directly assess presynaptic release, extracellular glutamate transients were quantified with the intensity-based glutamate-sensing reporter, iGluSnFR1 (Fig. 4A) in response to fixed intensity pulse-trains (10 x 10 Hz) delivered by local striatal electrical stimulation. The amplitude of iGluSnFR responses was markedly reduced in 3-month-old VKI striata, and there was a significant interaction between the normalized peak and pulse number (Fig. 4B i-ii and Supplementary Table 1). The recovery capacity of iGluSnFR responses following the pulse train was similar at 3 months, as was the decay of the pulse train response (Fig. 4B iii-iv). At 6 months, iGluSnFR responses were similar to WT responses across all measures (Fig. 4C). Interestingly, a significant age-dependent reduction in the amplitude of iGluSnFR transients was only observed for WT and not VKI responses (Supplementary Table 2). No age-dependent changes were observed in other parameters except for the decay of iGluSnFR responses in VKI striata between 3 and 6 months, which appear significantly increased with age. In summary, total striatal glutamate release is reduced in VKI mice at 3 months, but similar to WT at 6 months, suggesting that total presynaptic glutamate release is relatively increased in the VKI striatum with age.
A i) Graphic depicting viral injection of iGluSnFR in dorsolateral striatum 4–6 weeks prior to acute slice preparation. ii) Area of iGluSnFR expression in coronal slices containing CTX and STR depicted in green along with stimulus electrode (Stim) placed in dorsolateral STR. iii) Visualization of intensity-based glutamate-sensing fluorescent reporter (iGluSnFR) change in fluorescence relative to baseline (ΔF/F) in dorsolateral STR in response to local electrical stimulation (Stim). Low to high ΔF/F as a ratio of 0 to 1 represented as a gradient from purple to white, respectively. Boundaries of the corpus callosum (CC) separate CTX and STR in a coronal brain slice. Dashed circle represents region of interest (ROI) of 20 pixels used for iGluSnFR analysis. ii) Representative iGluSnFR response corresponding to trains of 10x10Hz pulses of electrical stimulation followed by 11th pulse at increasing interval with each of 4 repetitions. Black trace represents 1st of 4 stimulations with subsequent stimulations overlayed in maroon. B At 3 months, i) VKI vs WT iGluSnFR response size (ΔF/F) is significantly smaller in VKI brain slices (2-way ANOVA interaction p < 0.0001, genotype p = 0.007). ii) When normalized to 1st pulse (Norm. P1), VKI iGluSnFR responses are significantly different from WT (2-way ANOVA interaction p = 0.006, genotype p > 0.99). iii) VKI and WT recovery after 10x10Hz stimulation, normalized to 1st pulse, are similar (2-way ANOVA interaction p = 0.84, genotype p = 0.50). iv) Decay of the last response in pulse train (P10) is similar between VKI and WT iGluSnFR responses (Unpaired t-test p = 0.17). C At 6 months, i) VKI vs WT iGluSnFR response size is similar in VKI and WT brain slices (2-way ANOVA interaction p = 0.90, genotype p = 0.40). ii) Normalized VKI iGluSnFR responses are not significantly different from WT (2-way ANOVA interaction p = 0.77, genotype p = 0.87). iii) VKI recovery capacity after 10 x 10 Hz stimulation is similar to WT capacity (2-way ANOVA interaction p = 0.63, genotype p = 0.12). iv) Decay of the last response to 10x10Hz stimulation is not different between VKI and WT iGluSnFR responses (Mann-Whitney U-test p = 0.33).
Increased striatal dopamine release appears in 6-month-old VKI mice
We measured extracellular dopamine transients in the dorsolateral striatum using the dLight fluorescence reporter, evoked by electrical stimulation in slices from 3- and 6-month-old mice (Fig. 5A i-iii). We did not observe any changes to dLight amplitudes (Fig. 5A iv-vi), or responses to pulse-train stimulation in 3-month-old VKI striata (Fig. 5B); however, recovery capacity following pulse train stimulation was significantly reduced in VKIs (Fig. 5B iv).
A i) Graphic depicting stereotaxic injection of AAVs encoding for dLight in dorsolateral STR 4-6 weeks prior to acute slice preparation. Area of dLight expression in coronal slices containing CTX and STR depicted in blue with Stim placed in dorsolateral STR. ii) Visualization of dLight change in fluorescence from baseline (ΔF/F) in response to local electrical stimulation (ΔF/F values of 0 to 1 represented as a gradient from purple to white, respectively). Boundaries of the CC separate CTX and STR in a coronal brain slice. Dashed circle represents ROI of 40 pixels used for dLight analysis. iii) Representative dLight response in dorsolateral striatum corresponding to 2 pulses delivered with 4 s inter-pulse interval. At 3 months iv) Increasing stimulus intensity did not alter size of dLight responses in VKI vs WT STR (2-way ANOVA interaction p = 0.69, genotype p = 0.83). v) Decay of the 1st response peak (P1) is similar between VKI and WT brain slices (Unpaired t-test p = 0.57). vi) PPR at 4 s (P2 Peak/P1 Peak) is similar between VKI and WT brain slices (Unpaired t-test p = 0.21). B i) Representative dLight response in dorsolateral STR corresponding to 4x stimulation with 10 x 10 Hz pulse train and subsequent recovery stimulation. At 3 months ii) dLight responses were not significantly different in size between VKI and WT brain slices (2-way ANOVA interaction p = 0.99, genotype p = 0.85). iii) dLight responses relative to 1st pulse (P1) were not different between VKIs and WTs (2-way ANOVA interaction p = 0.69, genotype p = 0.45). iv) Recovery capacity following 10x10Hz stimulation are lower in VKI brain slices (2-way ANOVA interaction p = 0.81, genotype p = 0.06). v) Decay of the pulse train response is not significantly different in VKI vs WT brain slices (Unpaired t-test p = 0.28).
At 6 months, dLight response peaks were significantly increased in VKI brain slices, without any change in decay tau, or PPR at 4 s intervals (Fig. 6B i and Supplementary Table 1). Pulse train response peaks in VKIs were accordingly increased, without changes in pulse-train response pattern (Fig. 7B and E). However, recovery following train stimulation was reduced at smaller intervals and increased at larger intervals (Fig. 7B iv). WT responses show amplitude reductions between 3 and 6 months, which are absent in VKI responses (Supplementary Table 2). There is also a significant change to the pattern of normalized responses to pulse train stimulation with age in VKI striata, but not WT. Decay of responses were not significantly different in either WTs or VKIs when comparing 3- to 6-month-old mice. Therefore, the data indicate dopamine release is progressively increased in VKIs, relative to WT, by 6 months old.
A i) Graphic depicting stereotaxic injection of AAVs encoding for dLight into the dorsolateral striatum 4-6 weeks prior to acute slice preparation. Coronal slices containing CTX and STR were subsequently incubated ≥1.5 h with either vehicle Captisol® or 500 nM MLi-2 prior to recording. dLight expression is depicted in blue with Stim in dorsolateral STR. ii) Representative 2-pulse stimulation with 4 s inter-pulse interval with accompanying dLight response. B dLight responses were analyzed together (WT veh vs VKI veh vs WT MLi-2 vs VKI MLi-2) and graphed separately. i) VKI responses are increased across increasing stimulus intensities compared to WT responses (2-way ANOVA interaction p = 0.0003, genotype p = 0.0001, Šídák’s multiple comparisons test @50 µA p=ns, 100–400 µA p > 0.05). ii) MLi-2 treatment does not alter WT dLight responses (Šídák’s multiple comparisons test p=ns). iii) MLi-2 treatment reduces elevated dLight responses in VKI brain slices (Šídák’s multiple comparisons test @50 µA p = 0.07, @100-400 µA p < 0.05). iv) Decay of 1st response is not different between VKI and WT brain slices and is not sensitive to MLi-2 treatment (Kruskal-Wallis p = 0.66). v) PPR at 4 s interval is not different between VKI and WT brain slices and is not sensitive to MLi-2 treatment (Kruskal-Wallis p = 0.69).
A i) Graphic depicting stereotaxic injection of AAVs encoding for dLight into the dorsolateral STR 4-6 weeks prior to acute slice preparation. Coronal slices containing CTX and STR were subsequently incubated >1.5 h with either vehicle Captisol® or 500 nM MLi-2 prior to recording. dLight expression is depicted in blue with Stim in dorsolateral STR. ii) Representative response to pulse train stimulation (10x10Hz with repeated 4x with increasing 11th recovery pulse interval). B-D dLight response parameters are shown separated by genotype in vehicle treatment and within genotypes by treatment condition. Statistics were performed using 2-way ANOVA on WT veh vs VKI veh vs WT MLi-2 vs VKI MLi-2 with relevant post-hoc comparisons. B i) dLight response size is significantly higher in VKI vs WT vehicle-treated brain slices (2-way ANOVA interaction p < 0.0001, genotype p = 0.003, Šídák’s multiple comparisons test @P1-P4 p < 0.05, P5 p = 0.06, P6-P10 p=ns). ii) dLight responses, when normalized to the first peak, are similar between VKI and WT vehicle-treated brain slices (2-way ANOVA interaction p < 0.0001, genotype p = 0.2393, Šídák’s multiple comparisons test @P1-P10 p=ns). iii) Recovery capacity following high frequency stimulation is significantly altered in VKI vs WT vehicle-treated brain slices (2-way ANOVA interaction p = 0.02, genotype p = 0.19, Šídák’s multiple comparisons test @500 ms p = 0.04, 1000–5000 ms p=ns). C i) dLight response peaks in WT brain slices are not altered with acute MLi-2 treatment (Šídák’s multiple comparisons test p=ns). ii) dLight responses normalized to the first peak are not altered with MLi-2 treament (Šídák’s multiple comparisons test p=ns). iii) Recovery after train stimulation is not altered with MLi-2 in WT brain slices (Šídák’s multiple comparisons test p=ns). D i) dLight response peaks in VKI brain slices are significantly reduced with MLi-2 treatment (Šídák’s multiple comparisons test @P1-P10 p < 0.05). ii) Normalized dLight responses in VKI brain slices are not altered with MLi-2 treatment (Šídák’s multiple comparisons test p=ns). iii) Recovery after train stimulation is not altered with MLi-2 treatment in VKI brain slices (Šídák’s multiple comparisons test p=ns). E Decay of pulse train response is not significantly different between VKI vs WT brain slices with vehicle or MLi-2 treatment (1-way ANOVA p = 0.21).
Increased dopamine release in VKI striata is reversed with acute LRRK2 kinase inhibition
We investigated whether the robustly elevated dopamine release in 6-month-old VKI striata could be targeted with acute LRRK2 kinase inhibition. Slices prepared for dLight recordings were incubated either in vehicle Captisol® or in 500 nM of LRRK2 kinase inhibitor, MLi-2, for ≥1.5 h (Fig. 6A). Elevated VKI dLight responses were reversed by LRRK2 inhibition, without altering decay constants, or 4 s interval PPRs (Fig. 6B iii-v and Supplementary Table 1). Although increased amplitudes were similarly reversed in pulse-train experiments, there were no significant effect of MLi-2 on the pattern of responses to stimulation trains (Fig. 7D and E). Further, MLi-2 had no effect on WT dLight responses (Fig. 6B ii, iv, v, and 7C and E). In conclusion, acute LRRK2 kinase inhibition with MLi-2 reversed the elevated dopamine release in VKI striata at 6 months, without altering dopamine release in WT.
Discussion
Previously, we found elevated glutamate transmission in 3- to 4-week-old VKI mouse cortical cultures23 and elevated striatal dopamine transmission in slices from VKI mice aged 3 months22,24. Here, we find corticostriatal glutamatergic transmission onto SPNs is normal at 1 month, but progressively increases to >50% over WT by 6 months, and is not sensitive to acute LRRK2 kinase inhibition. Intriguingly, total striatal glutamate release measured by iGluSnFR was reduced at 3 months and increased to match WT levels by 6 months. In contrast, striatal dopamine release in VKI striata measured by dLight was unaltered at 3 months, but markedly elevated by 6 months, and reversed by acute LRRK2 kinase inhibition. These findings were restricted to observations in male mice, to compare with previously published data from male VKI and GKI (LRRK2 G2019S Knock-in) mice. However, this limitation should be addressed in future studies, as there are sex differences in both the presentation and symptomology of PD, and in striatal neurotransmission39,40,41,42.
SPNs of the dorsolateral striatum are the initial point of convergence for control of behavioural action selection, habit formation, and movement initiation9,12,43. These functions are all altered in PD, and PD pathology is clearest first in nigrostriatal axons1. Our data suggest SPNs in VKI mice develop changes to passive membrane properties throughout young-adulthood, which could reflect functional and/or anatomical differences. Membrane capacitance is proportional to membrane area, whereas membrane resistance inversely correlates to process diameter (and usually correlates with capacitance). These properties were bidirectionally altered in 6-month-old VKI SPNs, indicative of a larger soma, neurites, and/or processes, and increased leak channel conductance44,45.
We observed a subtle increase in amplitude and reduced decay time of spontaneous glutamate events in 3-month-old VKI SPNs, but no changes to optogenetically-evoked corticostriatal AMPAR or NMDAR currents. This suggests any modestly increased response to quantal release in a proportion of synapses is not sufficient to be detected in large currents generated by activity-dependent release. In light of relatively unchanged corticostriatal transmission in SPNs, it was surprising to see that iGluSnFR measures of total glutamate release were markedly reduced in VKI mice at 3 months. This could be explained by an increased number of active synapses, with lower individual release probabilities, or increased postsynaptic responsiveness in the face of less release. Since we previously found no change to glutamate synapse number in VKI mice at 3 months22, it may be that increased postsynaptic responsiveness exists as an attempt to compensate for reduced release (or vice versa), thereby keeping transmission onto SPNs within a homeostatic range. Alternatively, glutamate release onto SPNs may be unaltered while being reduced at other non-SPN synapses (e.g., excitatory inputs to cholinergic interneurons32,34), inviting future interrogation by cell-type.
By 6 months, clear increases in SPN spontaneous event amplitude were accompanied by increased event frequency (i.e., decreased inter-event intervals). At this age, VKI SPN corticostriatal AMPAR- and NMDAR-current amplitudes were also increased ~50% over WT. More frequent spontaneous activity and higher PPRs, which we also observed in corticostriatal evoked responses, are usually interpreted as increased probability of presynaptic release. However, larger AMPAR and NMDAR currents could also be a result of higher postsynaptic receptor numbers. We and others have reported increased GluA1-containing AMPAR receptor surface expression in VPS35 D620N and LRRK2 G2019S knock-in23,46; but increases to both NMDAR and AMPAR expression would have to be equal to explain the lack of difference in NMDAR:AMPAR current ratios observed here. Thus, the parsimonious explanation is that of increased probability of release, as we found in vitro23. Direct measures of total striatal presynaptic release with iGluSnFR found no difference between VKI and WT striata, suggesting that corticostriatal transmission onto SPNs must be selectively increased in VKIs. Alternatively, local electrical stimulation and resultant dopamine release would be expected to reduce glutamate release, via negative tuning of corticostriatal synapses via presynaptic D2 receptors47. This would be apparent in total striatal glutamate release assayed by iGluSnFR imaging, but might be occluded by release driven by direct activation of corticostriatal release with ChR2. Together, the data reveal an emergent increase in cortical glutamate transmission onto VKI SPNs by 6 months, perhaps to compensate for a reduction in total glutamate release observed at 3 months, or the loss of a compensatory mechanism at 6 months which kept release lower at 3 months.
While not required for diagnosis, changes to glutamate transmission are observed in PD, and likely impact many non-motor and motor features of the disease5,20,48. Elevated glutamate transmission is seen early in PD-relevant mice carrying LRRK2 G2019S knock-in mutations, and those overexpressing synuclein19,30,49,50,51. Therefore, the progressive dysregulation of glutamate in young adult VKI mice is consistent with other models of PD and may represent a direct contribution to (or compensation against) pathophysiological progression to degeneration.
We have previously reported that cortical glutamatergic transmission in VKIs is altered in vitro, and is not sensitive to acute treatment with LRRK2 kinase inhibitor, MLi-2, despite the reversal of elevated phosphorylation of Rab1023. Here, we applied a similar acute treatment paradigm to assess whether elevated VKI striatal glutamatergic transmission at 6 months can be reduced with MLi-2 treatment. We found no change in spontaneous or evoked cortico-striatal glutamate activity with acute MLi-2 treatment in either WT or VKI SPNs despite this treatment being sufficient to reduce phosphorylation of Rab12. Further investigation is required to determine if chronic inhibition with MLi-2 could rescue VKI changes in glutamatergic transmission, as a week-long administration of MLi-2 does rescue augmented striatal dopamine release in VKIs24. Our data therefore suggest that elevated striatal glutamate transmission occurs independent of ongoing LRRK2 kinase activity over short time periods.
Previously, we found dopamine release was elevated in VKI mice at 3 months by fast-scan cyclic voltammetry (FSCV)22,24. This was accompanied by slower decay constants, indicative of reduced DAT activity, and a reduction of DAT protein expression22,24. Increased dopamine release in 3-month-old VKI slices was rescued by chronic 1-week in vivo administration of LRRK2 kinase inhibitor, MLi-224. LRRK2 kinase inhibition also normalized the reduced DAT levels, which we concluded was causal to the rescue24. Here, we aimed to determine whether a rescue of dopamine dysfunction can be observed with the short-term LRRK2 inhibition (≥1.5 h) typical for successful reversal of mutation-induced increases to LRRK2 substrate phosphorylation. A positive result would indicate that dysregulation of dopamine release machinery is directly LRRK2 kinase-dependent, and that the inhibitor rescue is not due to systemic effects chronic LRRK2 kinase inhibition. As FSCV offers low temporal (10 Hz) and spatial resolution (limited by the carbon fiber electrode surface area), we employed dLight1.3b to assay dopamine release across the entire dorsolateral striatum at 20x higher temporal resolution.
Considering our published data, we were surprised that dLight recordings showed no difference between VKI and WT dopamine release at 3 months, other than a reduction in the speed of recovery from train stimulation. In contrast, 6-month-old VKI mice displayed a robust elevation in the amplitude of dLight responses, while decay constants were unaltered. The capacity to re-release dopamine after train stimulation was biphasically altered at this age, with shorter time intervals showing a reduced recovery capacity, and longer time intervals showing an increased recovery capacity. Together, this suggests dopamine release is robustly elevated in VKI by 6 months old, and that dopamine axons repolarise, repackage, and re-release dopamine more readily at intervals >1 s. Decay constants, and short-term depression (which would be observed as depletion of PPRs during high-frequency trains) are both indicators of DAT function52,53,54,55. As we saw no difference in these measures, we posit that increased dopamine release is independent of DAT function, as in LRRK2 G2019S knock-in mice30.
Differences between our published 3-month VKI voltammetry22,24 and dLight data here may be explained by biological and/or technical differences. Three data sets on mice from the same founding colony now show elevated dopamine release, albeit at slightly different ages22,24. While institutional housing conditions may modify phenotype progression, technical differences between slice treatment might also explain the discrepancy. Here, unlike for previous voltammetry data, slices were bathed in NMDG recovery solution to increase slice viability. Recordings were performed in the vehicle for MLi2, Captisol®, a biopolymer that has the potential to increase neurotransmitter release56,57,58,59,60,61, potentially masking differences between genotypes at 3 months. Disparities in the recording modality might also change the interpretation of results at 3 months. Direct comparison of FSCV and dLight shows both techniques report the expected increase in dopamine release duration and decay with nomifensine or cocaine (blocking DAT); however, peak changes are only observed with FSCV, and not dLight52. FSCV relies on the area of a carbon fiber electrode onto which dopamine can diffuse, which will increase under conditions of DAT inhibition, and translate to an increase in the peak of FSCV transients52. If the spread of extracellular dopamine is increased in VKI at 3 months, this would translate to peak changes in voltammetry, but not dLight. Further investigation of the spread of dLight fluorescence may reveal whether diffusion is altered at ages preceding clear increases in dLight peaks in VKI mice. Despite these caveats, repeated assessment of dLight across ages in VKI mice reveals increased dopamine release in young-adulthood, which is sensitive to acute LRRK2 kinase inhibition.
Elevated dopamine release in 6-month VKI was returned to WT levels by ≥1.5 h slice treatment with LRRK2 inhibitor MLi-2, relative to vehicle-treated slices from the same brain. This occurred without changes to parameters dictated by DAT or D2 receptors (decay rate/pulse train PPR, and 4 s PPR53,62). Therefore, we conclude LRRK2 kinase hyperactivity and inhibition can alter dopamine release independent of canonical DAT and D2 receptor activity. Both DAT and D2 receptors appear to be VPS35 cargoes, as is the dopamine vesicular monoamine transporter (VMAT)23,63,64. It may be that aberrant LRRK2 kinase activity increases vesicular packing of dopamine via VMAT, as VMAT2 levels are elevated in VKI striatal tissue22,24. This aligns with our observation that dopamine release is elevated during pulse-trains without significantly altering release probability (P2/P1 PPR, 100 ms intervals). Circuit-level effects may also contribute, as in dLight experiments local electrical stimulation might implicate extra-dopaminergic regulation of dopamine release. Further investigation of the specific effects of MLi-2 on glutamatergic, cholinergic, and GABAergic regulation of dopamine release, is required to elucidate the MLi-2 effects on dopamine release observed here. That said, as isolated (ChR2-driven) cortico-striatal glutamate release was unaffected by MLi-2, dopamine release normalization in VKIs by MLi-2 would seem unlikely to result from changes to concurrent cortico-striatal glutamate release.
LRRK2 variants convey the highest genetic risk for PD, with several pathogenic variants linked to clinically-typical familial parkinsonism21. Brain scans of LRRK2 PD patients show impaired presynaptic dopamine function65, but asymptomatic LRRK2 mutation carriers exhibit higher dopamine turnover, indicating increased release66. Dopamine release measured by FSCV is also elevated in 3-month-old LRRK2 G2019S knock-in mice30, consistent with our results in VKI mice22,24. Early increases in dopamine release decline in LRRK2 knock-in mice30, and a similar pattern is observed in α-synuclein overexpressing PD mice67. Together, evidence from VKI, LRRK2, and synuclein mouse models are consistent with early elevations in dopamine release in humans66.
LRRK2 and VPS35 canonically function in endolysosomal regulation and trafficking, and synaptic vesicles (SVs) are highly specialised, neuronal-specific, endosomes68. As with other membranes, the SV cycle is orchestrated by Rabs, several of which are phosphorylated by LRRK2. This includes the canonically synaptic-vesicle associated Rab3&569,70 and classically-endolysosomal Rab10&12, that have recently been shown to be as enriched as Rab3&5 on SVs71. Both VPS35 and LRRK2 can alter synaptic vesicle docking and size72, although how remains speculative. Conceptually, LRRK2 phosphorylation of Rab3 might be expected to increase SV availability by facilitating biogenesis, trafficking, and priming of vesicles at the active zone. Rab3 tethering to Rab-Interacting Molecule (RIM)73 regulates vesicle fusion, without which DA release is blocked74. Other than Rab3, the role of Rabs at SVs is somewhat unclear, and effects of LRRK2-Rab phosphorylation almost entirely unknown. Finally, while Rabs have recently taken centre stage, several SV proteins were previously implicated as LRRK2 substrates; including, auxillin, endophilinA, dynamin, & synapsin51, and we show here that LRRK2 kinase inhibition can have rapid effects on dopamine release. Further investigation of VPS35 mutant, and LRRK2 inhibitor effects or lack thereof on dopamine and glutamate vesicle cycles seems justified.
Given the ubiquitous expression of VPS35 and LRRK2, a potential mechanism of onset of PD-like dysfunction and degeneration is likely due to an accumulation of low-level cellular insults over years in mice, or decades in humans. Sustained elevations in striatal neurotransmission, or even compensatory action towards it, may increase cellular stress. This in turn, could lead to the accumulation of excitotoxic damage which may not be effectively cleared in the presence of the VPS35 (or LRRK2) mutation75. The increased energy demands and calcium buffering required by increased synaptic activity may also contribute to mitochondrial dysfunction observed in many PD scenarios, including VPS35 patient-derived neurons76. These may eventually lead to axon degeneration in more vulnerable neuronal populations, such as nigrostriatal dopamine neurons.
In summary, we present evidence of progressively elevated neurotransmission in young-adult mice with VPS35 D620N mutations, which we propose could become neurotoxic if sustained. However, acute inhibition of LRRK2 kinase rapidly reverses the increased dopamine release, offering hope as a viable neuroprotective strategy. Targeting early neuronal hyperactivity may be the optimal timepoint for disease-modifying PD treatments, especially for individuals known to carry PD-causal gene variants.
Methods
Animals
VPS35 D620N knock-in (VKI) were generated as previously described in ref. 22 and maintained on a C57Bl6/J wild-type (WT) background. Mice were housed and bred in accordance with the Canadian Council on Animal Care regulations (Animal Use Protocol 2017-7888B). All procedures were approved by and governed in accordance with the Neuro Centre of Neurological Disease Models (Animal Use Protocol 2017-7888B) and Memorial University Animal Care Committee (Animal Use Protocol 18-01-MP). 1-, 3-, and 6-month-old male heterozygous VKI and WT mice were used for all measures of spontaneous glutamate transmission. 3- and 6- month male heterozygous VKI and WT mice were used for all experiments requiring stereotaxic injections as these surgeries were performed >4 weeks in advance of experiments.
Genotyping
Genotyping of all mice was conducted on tail samples at weaning and on post-mortem ear tissue. Samples were digested in 100 µL 10% Chelex (Bio-Rad 142–1253; 20 min 95 °C, 2x vortex) and centrifuged (2 minutes 12,000 RPM) before DNA-containing supernatant (2 µL) was added to PCR master mix (18 µL, Qiagen 201203: taq polymerase, DNAse and RNAse-free water, 10X buffer, 10 mM dNTPs, and custom DNA oligo primers [ThermoFisher: Forward-TGGTAGTCACATTGCCTCTG, Reverse-ATGAACCAACCATCAATAGGAACAC]). DNA was amplified by PCR (program cycle available upon request) and combined with fluorescent DNA intercalating dye (ZmTech LB-001G) prior to iontophoresis. 10 µL of PCR product was run in 4% agarose gel and visualized (BioRad UV gel imager) for the presence of 1 or 2 bands to determine WT vs VKI genotype, respectively.
Surgery
Channelrhodopsin-2 (ChR2), intensity-based glutamate-sensing fluorescent reporters (iGluSnFR), and D1 dopamine receptor-based fluorescent reporters (dLight1.3b) were delivered by stereotaxic injection of AAV constructs. 4–6 weeks prior to slice preparation, mice were subcutaneously injected with carprofen (2-4 mg/mL, 20 mg/kg, 0.9% NaCl), left to rest for ≥15 minutes, then anaesthetized with isoflurane (5% induction, 1-2% maintenance) and secured in a stereotaxic head frame (Kopf Instruments). The local analgesic, Marcaine, was injected subcutaneously below the site of incision and hair was removed chemically (Nair) or mechanically (Wahl clippers). An incision was made and skull, leveled using Bregma and Lambda as points of reference. A 0.5 mm craniotomy was then created (micro-burr dentistry drill) over the site of injection. A 10 µL syringe (Nanofil), attached to a microinjector (Harvard Apparatus Pump11 Elite) was lowered, with coordinates zeroed to the brain surface. Following AAV injection (details below), a 5-minute settling period was allowed before removing the needle. The scalp was then rehydrated with Marcaine, sutured (4-0 silk; Ethicon 683 G) and reinforced (Vetbond 3 M 1469SB), prior to subcutaneous 0.9% NaCl injection to replace fluids (0.2–0.5 mL/10 mg). Mice were monitored for pain and discomfort after regaining consciousness and returned to home cage in ~1 h. Post-operative monitoring (3 days) included daily subcutaneous carprofen injection.
Construct-specific injection details
For ChR2 optogenetic stimulation, AAV9-CAG-ChR2-mCherry (Neurophotonics Centre, Université Laval, lot #834 = 4 × 1012 GC/mL) was injected unilaterally (650nL, 1nL/sec) into primary motor cortex (1.5 mm anterior, 1.0 mm lateral, 0.8 mm ventral to Bregma). For optogenetic recording of glutamate release, AAV1.hSyn.iGluSnFr.WPRE.SV40 (Addgene 98929-AAV1, 2.8 × 1013 GC/mL) was injected bilaterally (1 uL, 2 nL/sec) into the dorsolateral striatum (coordinates: 2.0 mm anterior, 1.0 lateral, 3.2 ventral to Bregma). For optogenetic recording of dopamine release, AAV5-CAG-dLight1.3b (Addgene 125560-AAV5, 1.5 × 1013 GC/mL) was injected bilaterally (300 nL, 1nL/sec) into the dorsolateral striatum.
Preparation of acute brain slices
300 µm acute coronal brain slices were prepared from restrained mice which were swiftly decapitated. Brains were quickly transferred to ice-cold recovery solution (1 min; in mM: 93 NMDG, 93 HCl, 2.5 KCl, 1.2 NaH2PO4, 30 NaHCO3, 20 HEPES, 25 glucose, 5 sodium ascorbate, 3 sodium pyruvate, 10 MgSO4·7H2O, 0.5 CaCl2·2H2O, pH 7.3-7.4, 290-310 mOsm; carbogen-infused). Following this, extra-striatal rostral and caudal brain regions were removed by coronal sectioning, and the remaining block was mounted onto a vibrating-blade microtome platform with sodium acrylate (Leica Microsystems VT 1200S). After hemisectioning at the midline, coronal sections were cut, and slices were then transferred to warm recovery solution (35°C, 15 min). A final transfer of slices into holding chambers containing room-temperature artificial cerebrospinal fluid (aCSF; in mM: 125 NaCl, 3 KCl, 25 NaHCO3, 1.25 NaH2PO4, 2 MgCl2, 2 CaCl2, 10 glucose, pH 7.2-7.4, 300–310 mOsm, 22–25 °C, carbogen-infused) was followed by ≥45 min settling period before recording in aCSF began.
Whole-cell patch-clamp electrophysiology
Whole-cell patch-clamp electrophysiology was used to obtain recordings of spontaneous and ChR2-evoked glutamate transmission in SPNs of the dorsolateral striatum (caudate/putamen), as previously30. Slices were transferred to a recording chamber perfused with aCSF (22–25 °C) containing 100 µM picrotoxin (Tocris 1128) at a flow rate of ~1.5 mL/min. Slices were visualized on an Olympus BX51 microscope (40x magnification, 2x digital zoom, IR-DIC and Q-Imaging Electro camera). SPNs were identified within the dorsolateral striatum based on somatic size (8–20 µM) and distinct morphology, 50–150 µM below the surface of the slice. Borosilicate glass capillary tubes (Harvard Apparatus 640805) were pulled using a Sutter P-1000 micropipette puller to form 1 µm tip recording pipettes (filled resistance 4–8 MOhms; in mM: 130 Cs methanesulfonate, 5 CsCl, 4 NaCl, 1 MgCl2, 5 EGTA, 10 HEPES, 5 QX-314, 0.5 GTP, 10 Na2 phosphocreatine, 5 MgATP, and 0.1 spermine, pH 7.2, 290 mOsm). A motorized micromanipulator (Sutter Instrument MP-285) was used to patch onto identified SPNs, with signals obtained by MultiClamp 700B amplifier in voltage-clamp configuration, filtered at 2 kHz and digitized at 10 kHz (Molecular Devices Axon Digidata 1440 A). Membrane properties were determined with the membrane-test function while holding at -70 mV. Synaptic recordings were initiated after a 2 min settling period, with access resistance tolerance set to 27 MΩ and recordings discarded if Δ≥10% over the elapsed period. Spontaneous excitatory postsynaptic currents (sEPSCs) were recorded over a minimum 2 min period at -70 mV (gain 20) and analyzed in Clampfit10 (Molecular Devices; 5pA peak event threshold, confirmed manually). Non-unitary events were retained for inter-event interval analysis, but only unitary events were used for amplitude and decay constants. Cumulative distributions were used to evaluate amplitude and inter-event intervals in each recorded SPN. Unitary events in each recording were averaged and decay tau measured by 1-term exponential fit.
ChR2-evoked post-synaptic currents (ChR2-PSCs) were stimulated by wide-field illumination with blue light (473 nm, XCite Series 120Q) transmitted through the 40x immersion objective generating 2.7 mW. 5 ms pulses were controlled by a Lambda SC Smart Shutter Controller (Sutter Instruments) administered in trains of 4 pulses with 100 ms inter-pulse intervals. Trains were repeated every 30 s, 5–10 times and averaged for analysis. Recordings of ChR2-PSCs mediated by α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors (AMPARs) were taken at -70mV (gain 2) averaged across 5 repetitions. AMPAR and N-methyl-D-aspartate receptor (NMDAR) currents were generated by single 5 ms pulse stimulations repeated 5x every 30 s at -70 mV then +40 mV to assess AMPAR + NMDAR-mediated ChR2-PSCs, respectively. Peak NMDAR current was estimated at +40 mV, 40 ms post AMPA peak, and AMPAR currents were then isolated at +40 mV by bath application of 10 µM D-APV (NMDAR blocker, Tocris 0106). AMPA rectification indices were calculated as a ratio of isolated AMPAR ChR2-PSC peak at +40 mV : -70 mV.
iGluSnFR and dLight imaging
Imaging of iGluSnFR and dLight recordings were obtained using a 2X objective focused on dorsolateral STR. Slices were wide-field illuminated with blue light (473 nm, CoolLED pE-340fura), with the shutter, EM-CCD camera (Andor iXon Ultra 897), and stimulus isolator (WPI A365) triggered by Clampex & Digidata 1550B). The stimulus isolator was connected to a monopolar tungsten stimulating electrode (A-M Systems 574000) lowered into dorsolateral striatum 50–100 µM beneath the surface of the tissue. Recordings were captured using Andor Solis software using 4 × 4 binning at 205 Hz. For these experiments, spontaneous iGluSnFR & dLight transients were excluded from analysis of responses to electrical stimulation. For iGluSnFR recordings, a stimulation train was delivered at fixed stimulation intensity (150uA train of 10 × 0.2 ms pulses with 100 ms inter-pulse intervals). No-stimulation (for background & bleach subtraction) and stimulation trials were alternated at 1-minute intervals, repeated every 2 min, until 5 no-stimulation trials were recorded. An 11th pulse was delivered with each repetition of the stimulation trial, with increasing inter-pulse intervals between 500–5000 ms. The same protocol was used to obtain pulse train dLight recordings after 2-pulse dLight stimulation with 4 s inter-pulse intervals, delivered at 50–400 uA, every 2 min to generate stimulus response curves. Responses were then assessed to determine the stimulus intensity corresponding to 50-70% maximum response (FIJI software) for subsequent pulse train dLight experiments. iGluSnFR and dLight videos were converted to the change in fluorescence intensity over time (ΔF/F; FIJI software) with peak and decay analyzed in Clampfit (decays measured by the 1-term exponential function of each trace). Absolute and normalized peak and decay of pulse train responses were derived from the average of 4 responses.
Acute LRRK2 kinase inhibition
For assessment of glutamate transmission, 6-month-old mice were injected intraperitoneally with LRRK2 kinase inhibitor, MLi-2 (500 nM, Tocris 5756, 45% Captisol® in PBS) or vehicle-control (45% Captisol® in PBS 377.6 µL/L aCSF), 1.5 h prior to slice preparation, as before23. Slices were incubated and perfused with aCSF containing MLi-2 or vehicle throughout. For dLight experiments, slices from 6-month-old mice were pre-incubated ≥1.5 h and then bath-perfused during dLight recording MLi-2 or vehicle. Captisol® vehicle was also present in all 3-month-old dLight recordings to be able to compare dLight recordings across age.
Western blot for assessing LRRK2 target engagement
Western blots were performed on striatal brain slices from 6-month-old mice which were flash frozen after recording for dopamine release and stored at −80 °C. For cohort A, slices were first homogenized by trituration in ice-cold tris-buffered saline (TBS; 1% Triton X-100; pH 7.4), containing a cocktail of protease inhibitor (Roche 11697498001) and phosphatase inhibitor (Sigma 4906845001). Samples were then probe sonicated for 15 s at 20 kHz, then rotated at 4 °C for 30 min, and centrifuged for 10 min at 7000 RPM. The supernatant was used for protein quantification by Pierce BCA assay (ThermoFisher 23255) and samples were standardized to equivalent concentrations in lysis buffer before denaturation. 40 µg protein of each sample was added to 4x NuPage LDS sample buffer (Invitrogen NP0008) with a final concentration of 5% β-mercaptoethanol, for a total loading volume ranging from 10–24 µL. Samples were denatured at 95 °C for 5 min, then loaded onto 10% Bis-Tris gels. The gel was run in a Mini-PROTEAN Tetra vertical electrophoresis cell (Bio-Rad) for 30 min at 70 V, then 1 h at 110 V. Proteins were then transferred to a methanol-activated Immobilon-P PVDF membrane (Millipore IPVH00010) for 90 min at 25 V and held at 4 °C overnight. The membrane was blocked with 5% BSA in TBS-T for 1 h at room temperature. Primary antibodies (Rab12 pS106 (MJF-R25-9), Abcam ab256487; or Rab12, Proteintech 18843-1-AP) were added to membranes, shaking for 1 h at room temperature or overnight at 4 °C, then washed 4x in TBS-T (TBS, 0.05% Tween-20). HRP-conjugated secondary antibodies were added to membrane in TBS-T with 5% milk and shaken for 30 min at room temperature. Chemiluminescence of membranes was detected using the Pierce ECL (ThermonFisher32209) and the Chemi-Doc imaging system (Cell-Bio). Imaged membranes were background-subtracted and band intensity was analyzed with ImageJ software.
For Cohort B, slices were quickly thawed into 120uL of ice-cold lysis buffer (50 mM Tris–HCl, 1% Triton X-100, pH 7.5, 1 mM EGTA, 1 mM sodium orthovanadate, 50 mM NaF, 10 mM 2-glycerophosphate, 5 mM sodium pyrophosphate, 0.1 µg/ml microcystin-LR (Enzo Life Sciences), 270 mM sucrose, complete EDTA-free protease inhibitor cocktail (Sigma–Aldrich 11836170001), and Phostop phosphatase inhibitor (Millipore-Sigma 4906845001)), then homogenised using a Precellys homogeniser (Bertin Technologies) in 0.5 mL tubes with glass beads (3 x 30 s on at 6500 rpm, 10 s off, 4 °C). Samples were stored on ice until centrifugated at maximum speed for 30 min at 4 °C. Protein concentrations were then determined by BCA assay and standardized across samples by mixing with NuPAGE LDS Sample Buffer (Life Technologies) and 1% β-mercaptoethanol, then boiled for 10 min at 95 °C. 10-20 µg of samples were added to NuPAGE 4–12% Bis-Tris Midi Gels (Thermo Fisher Scientific WG1403) and run at 130 V using NuPAGE MOPS SDS running buffer (Thermo Fisher Scientific NP0001-02). Next, proteins were transferred onto Amersham Protran supported 0.45 µm nitrocellulose membranes (GE Healthcare) at 100 V for 90 min on ice in transfer buffer (48 mM Tris-HCl and 39 mM glycine). Nitrocellulose membranes were then blocked with 5% milk powder in TBS-T at room temperature for 30 min, then incubated overnight at 4 °C in TBS-T containing 5% BSA and primary antibodies for pRab12 or Rab12. Membranes were washed with TBS-T, then incubated at room temperature for 1 h with near-infrared fluorescent IRDye antibodies (LI-COR 925-68070 and 925-32211), diluted 1:10,000 in TBS-T. Membranes were thoroughly washed with TBS-T again before imaging using the LI-COR Odyssey CLx Western Blot imaging system (LI-COR). Signals were quantified using Image Studio software.
Statistical analysis
All data presentation and statistics were conducted in GraphPad Prism10. Data were tested against ROUT outlier analysis with a liberal maximum false discovery rate Q = 1%. Rarely, identified outliers were suppressed from the dataset prior to parametric or non-parametric distributions testing (D’Agostino and Pearson). Unpaired t-test/1-way ANOVA (if parametric) or Mann-Whitney U-test/Kruskal-Wallis testing (if non-parametric) were used to analyse data. Post-hoc analysis was performed if ANOVA p < 0.05 by Tukey’s (parametric) or Dunn’s (non-parametric) multiple comparisons tests as appropriate. Post-hoc pair-wise analysis was performed with Fisher’s LSD test. All 2-way ANOVA comparisons used Šídák post-hoc analyses. Asterisks represent p < 0.05 from pair-wise comparisons. All statistical analyses are described in figure legends, and post-hoc analyses are reported in Supplementary Tables 1 & 2. Trends are defined as 0.10 > p > 0.05. Data are presented as n=observations from (n) animals (e.g., WT = 6(3) is 6 observations from 3 WT animals).
Data availability
The VKI mouse strain has been deposited in Jackson Labs and openly distributed with the support of the Michael J. Fox Foundation (www.jax.org; Vps35 knock-in: B6(Cg)-Vps35tm1.1Mjff/J; Stock No: 023409; floxΔneo Vps35; B6.Cg Vps35tm1.2Mjff/J; Stock No: 021807). The datasets generated during and/or analysed during the current study are available from the corresponding authors on reasonable request.
References
Kordower, J. H. et al. Disease duration and the integrity of the nigrostriatal system in Parkinson’s disease. Brain 136, 2419–2431 (2013).
Kim, H. J., Jeon, B. S. & Jenner, P. Hallmarks of Treatment Aspects: Parkinson’s Disease Throughout Centuries Including l -Dopa. in International Review of Neurobiology vol. 132 295–343 (Elsevier, 2017).
Fereshtehnejad, S.-M. et al. Evolution of prodromal Parkinson’s disease and dementia with Lewy bodies: a prospective study. Brain 142, 2051–2067 (2019).
Kalia, L. V. & Lang, A. E. Parkinson’s disease. Lancet 386, 896–912 (2015).
Goldman, J. G. & Postuma, R. Premotor and nonmotor features of Parkinson’s disease. Curr. Opin. Neurol. 27, 434–441 (2014).
Henderson, J. M., Carpenter, K., Cartwright, H. & Halliday, G. M. Loss of thalamic intralaminar nuclei in progressive supranuclear palsy and Parkinson’s disease: clinical and therapeutic implications. Brain 123, 1410–1421 (2000).
MacDonald, V. & Halliday, G. M. Selective loss of pyramidal neurons in the pre-supplementary motor cortex in Parkinson’s disease. Mov. Disord. 17, 1166–1173 (2002).
Giguère, N., Burke Nanni, S. & Trudeau, L.-E. On Cell Loss and Selective Vulnerability of Neuronal Populations in Parkinson’s Disease. Front. Neurol. 9, 455 (2018).
Kreitzer, A. C. & Malenka, R. C. Striatal plasticity and basal ganglia circuit function. Neuron 60, 543–554 (2008).
Haber, S. N. Corticostriatal circuitry. Dialogues Clin. Neurosci. 18, 7–21 (2016).
Burke, D. A., Rotstein, H. G. & Alvarez, V. A. Striatal Local Circuitry: A New Framework for Lateral Inhibition. Neuron 96, 267–284 (2017).
Redgrave, P., Prescott, T. & Gurney, K. Selection and the Basal Ganglia. in The Basal Ganglia VI (eds. Graybiel, A. M., Delong, M. R. & Kitai, S. T.) 257–266 (Springer US, Boston, MA, 2003). https://doi.org/10.1007/978-1-4615-0179-4_26.
Milnerwood, A. J. et al. Early increase in extrasynaptic NMDA receptor signaling and expression contributes to phenotype onset in Huntington’s disease mice. Neuron 65, 178–190 (2010).
Milnerwood, A. J. & Raymond, L. A. Early synaptic pathophysiology in neurodegeneration: insights from Huntington’s disease. Trends Neurosci. 33, 513–523 (2010).
Masato, A., Bubacco, L. & Greggio, E. Too much for your own good: Excessive dopamine damages neurons and contributes to Parkinson’s disease: An Editorial Highlight for “Enhanced tyrosine hydroxylase activity induces oxidative stress, causes accumulation of autotoxic catecholamine metabolites, and augments amphetamine effects in vivo”. J. Neurochem. 158, 833–836 (2021).
Vecchio, L. M. et al. Enhanced tyrosine hydroxylase activity induces oxidative stress, causes accumulation of autotoxic catecholamine metabolites, and augments amphetamine effects in vivo. J. Neurochem.158, 960–979 (2021).
Masato, A., Plotegher, N., Boassa, D. & Bubacco, L. Impaired dopamine metabolism in Parkinson’s disease pathogenesis. Mol. Neurodegeneration 14, 35 (2019).
Vidyadhara, D. J. et al. Dopamine transporter and synaptic vesicle sorting defects underlie auxilin-associated Parkinson’s disease. Cell Rep. 42, 112231 (2023).
Matikainen-Ankney, B. A. et al. Altered Development of Synapse Structure and Function in Striatum Caused by Parkinson’s Disease-Linked LRRK2–G2019S Mutation. J. Neurosci. 36, 7128–7141 (2016).
Foffani, G. & Obeso, J. A. A Cortical Pathogenic Theory of Parkinson’s Disease. Neuron 99, 1116–1128 (2018).
Volta, M., Milnerwood, A. J. & Farrer, M. J. Insights from late-onset familial parkinsonism on the pathogenesis of idiopathic Parkinson’s disease. Lancet Neurol. 14, 1054–1064 (2015).
Cataldi, S. et al. Altered dopamine release and monoamine transporters in Vps35 p.D620N knock-in mice. npj Parkinson’s Dis. 4, 1–11 (2018).
Kadgien, C. A., Kamesh, A. & Milnerwood, A. J. Endosomal traffic and glutamate synapse activity are increased in VPS35 D620N mutant knock-in mouse neurons, and resistant to LRRK2 kinase inhibition. Mol. Brain 14, 1–20 (2021).
Bu, M. et al. Inhibition of LRRK2 kinase activity rescues deficits in striatal dopamine physiology in VPS35 p.D620N knock-in mice. npj Parkinsons Dis. 9, 1–12 (2023).
Munsie, L. N. et al. Retromer-dependent neurotransmitter receptor trafficking to synapses is altered by the Parkinson’s disease VPS35 mutation p.D620. N. Hum. Mol. Genet. 24, 1691–1703 (2015).
Vilariño-Güell, C. et al. DNAJC13 mutations in Parkinson disease. Hum. Mol. Genet. 23, 1794–1801 (2014).
Chen, X. et al. Parkinson’s disease-linked D620N VPS35 knockin mice manifest tau neuropathology and dopaminergic neurodegeneration. PNAS 116, 5765–5774 (2019).
Niu, M. et al. VPS35 D620N knockin mice recapitulate cardinal features of Parkinson’s disease. Aging Cell e13347 (2021) https://doi.org/10.1111/acel.13347.
Di Maio, R. et al. LRRK2 activation in idiopathic Parkinson’s disease. Sci. Transl. Med. 10, (2018).
Volta, M. et al. Initial elevations in glutamate and dopamine neurotransmission decline with age, as does exploratory behavior, in LRRK2 G2019S knock-in mice. Elife 6, (2017).
Köfalvi, A. et al. Control of glutamate release by complexes of adenosine and cannabinoid receptors. BMC Biol. 18, 9 (2020).
Kosillo, P., Zhang, Y.-F., Threlfell, S. & Cragg, S. J. Cortical Control of Striatal Dopamine Transmission via Striatal Cholinergic Interneurons. Cereb. Cortex 26, 4160–4169 (2016).
Ding, J., Peterson, J. D. & Surmeier, D. J. Corticostriatal and Thalamostriatal Synapses Have Distinctive Properties. J. Neurosci. 28, 6483–6492 (2008).
Ding, J. B., Guzman, J. N., Peterson, J. D., Goldberg, J. A. & Surmeier, D. J. Thalamic Gating of Corticostriatal Signaling by Cholinergic Interneurons. Neuron 67, 294–307 (2010).
Surmeier, D. J., Ding, J., Day, M., Wang, Z. & Shen, W. D1 and D2 dopamine-receptor modulation of striatal glutamatergic signaling in striatal medium spiny neurons. Trends Neurosci. 30, 228–235 (2007).
Momiyama, T. & Nishijo, T. Dopamine and Serotonin-Induced Modulation of GABAergic and Glutamatergic Transmission in the Striatum and Basal Forebrain. Front. Neuroanat. 11, 42 (2017).
Calabresi, P., Maj, R., Pisani, A., Mercuri, N. B. & Bernardi, G. Long-term synaptic depression in the striatum: physiological and pharmacological characterization. J. Neurosci. 12, 4224–4233 (1992).
Calabresi, P. et al. Abnormal synaptic plasticity in the striatum of mice lacking dopamine D2 receptors. J. Neurosci. 17, 4536–4544 (1997).
Gillies, G. E., Pienaar, I. S., Vohra, S. & Qamhawi, Z. Sex differences in Parkinson’s disease. Front. Neuroendocrinol. 35, 370–384 (2014).
Yoest, K. E., Cummings, J. A. & Becker, J. B. Oestradiol influences on dopamine release from the nucleus accumbens shell: sex differences and the role of selective oestradiol receptor subtypes. Br. J. Pharm. 176, 4136–4148 (2019).
Dluzen, D. E. & McDermott, J. L. Sex differences in dopamine- and vesicular monoamine-transporter functions. Ann. N. Y Acad. Sci. 1139, 140–150 (2008).
Van Zandt, M., Flanagan, D. & Pittenger, C. Sex differences in the distribution and density of regulatory interneurons in the striatum. Front. Cell Neurosci. 18, 1415015 (2024).
Kreitzer, A. C. Physiology and Pharmacology of Striatal Neurons. Annu. Rev. Neurosci. 32, 127–147 (2009).
Rall, W. Core Conductor Theory and Cable Properties of Neurons. in Comprehensive Physiology (ed. Terjung, R.) 39–97 (Wiley, 1977). https://doi.org/10.1002/cphy.cp010103.
Kandel, E. R. Membrane Potential and the Passive Electrical Properties of the Neuron. in Principles of Neural Science 126–147 (McGraw-Hill, New York, 2013).
Gupta, S., Tielemans, A., Guevara, C. A., Huntley, G. W. & Benson, D. L. Parkinson’s-linked LRRK2-G2019S derails AMPAR trafficking, mobility, and composition in striatum with cell-type and subunit specificity. Proc. Natl. Acad. Sci. USA 121, e2317833121 (2024).
Bamford, N. S. et al. Dopamine Modulates Release from Corticostriatal Terminals. J. Neurosci. 24, 9541–9552 (2004).
Carrillo-Mora, P., Silva-Adaya, D. & Villaseñor-Aguayo, K. Glutamate in Parkinson’s disease: Role of antiglutamatergic drugs. Basal Ganglia 3, 147–157 (2013).
Beccano-Kelly, D. A. et al. Synaptic function is modulated by LRRK2 and glutamate release is increased in cortical neurons of G2019S LRRK2 knock-in mice. Front. Cell Neurosci. 8, (2014).
Creed, R. B., Roberts, R. C., Farmer, C. B., McMahon, L. L. & Goldberg, M. S. Increased glutamate transmission onto dorsal striatum spiny projection neurons in Pink1 knockout rats. Neurobiol. Dis. 150, 105246 (2021).
Kuhlmann, N. & Milnerwood, A. J. A Critical LRRK at the Synapse? The Neurobiological Function and Pathophysiological Dysfunction of LRRK2. Front Mol. Neurosci. 13, 153 (2020).
Salinas, A. G. et al. Distinct sub-second dopamine signaling in dorsolateral striatum measured by a genetically-encoded fluorescent sensor. Nat. Commun. 14, 5915 (2023).
Condon, M. D. et al. Plasticity in striatal dopamine release is governed by release-independent depression and the dopamine transporter. Nat. Commun. 10, 1–15 (2019).
Formisano, R., Rosikon, K. D., Singh, A. & Dhillon, H. S. The dopamine membrane transporter plays an active modulatory role in synaptic dopamine homeostasis. J. Neurosci. Res. 100, 1551–1559 (2022).
Brimblecombe, K. R. et al. Calbindin-D28K Limits Dopamine Release in Ventral but Not Dorsal Striatum by Regulating Ca 2+ Availability and Dopamine Transporter Function. ACS Chem. Neurosci. 10, 3419–3426 (2019).
Pardeshi, C. V. et al. Sulfobutylether-β-cyclodextrin: A functional biopolymer for drug delivery applications. Carbohydr. Polym. 301, 120347 (2023).
Stella, V. J. & Rajewski, R. A. Sulfobutylether-β-cyclodextrin. Int. J. Pharmaceutics 583, 119396 (2020).
Choi, T.-Y. et al. Low levels of methyl β-cyclodextrin disrupt GluA1-dependent synaptic potentiation but not synaptic depression. J. Neurochem. 132, 276–285 (2015).
Frech, M. J., Rabenstein, M., Bovensiepen, K., Rost, S. & Rolfs, A. Cyclodextrin Alters GABAergic Input to CA1 Pyramidal Cells in Wild-Type But Not in NPC1-Deficient Mice. BioResearch Open Access 4, 358–362 (2015).
Geda, O., Tábi, T., Lakatos, P. P. & Szökő, É Differential Ganglioside and Cholesterol Depletion by Various Cyclodextrin Derivatives and Their Effect on Synaptosomal Glutamate Release. IJMS 23, 9460 (2022).
Ormerod, K. G., Rogasevskaia, T. P., Coorssen, J. R. & Mercier, A. J. Cholesterol-Independent Effects of Methyl-β-Cyclodextrin on Chemical Synapses. PLoS ONE 7, e36395 (2012).
Rice, M. E. & Cragg, S. J. Dopamine spillover after quantal release: Rethinking dopamine transmission in the nigrostriatal pathway. Brain Res. Rev. 58, 303–313 (2008).
Wu, S. et al. The Dopamine Transporter Recycles via a Retromer-Dependent Postendocytic Mechanism: Tracking Studies Using a Novel Fluorophore-Coupling Approach. J. Neurosci. 37, 9438–9452 (2017).
Wu, Q. et al. Retrograde trafficking of VMAT2 and its role in protein stability in non-neuronal cells. J. Biomed. Res. 30, 502–509 (2016).
Adams, J. R. et al. PET in LRRK2 mutations: comparison to sporadic Parkinson’s disease and evidence for presymptomatic compensation. Brain 128, 2777–2785 (2005).
Sossi, V. et al. Dopamine turnover increases in asymptomatic LRRK2 mutations carriers. Mov. Disord. 25, 2717–2723 (2010).
Lam, H. A. et al. Elevated tonic extracellular dopamine concentration and altered dopamine modulation of synaptic activity precede dopamine loss in the striatum of mice overexpressing human α-synuclein. J. Neurosci. Res. 89, 1091–1102 (2011).
Ivanova, D. & Cousin, M. A. Synaptic Vesicle Recycling and the Endolysosomal System: A Reappraisal of Form and Function. Front. Synaptic Neurosci. 14, 826098 (2022).
Komori, T. & Kuwahara, T. An Update on the Interplay between LRRK2, Rab GTPases and Parkinson’s Disease. Biomolecules 13, 1645 (2023).
Steger, M. et al. Phosphoproteomics reveals that Parkinson’s disease kinase LRRK2 regulates a subset of Rab GTPases. Elife 5, (2016).
Taoufiq, Z., et al. Hidden proteome of synaptic vesicles in the mammalian brain. Proc. Natl. Acad. Sci. USA 117, 33586–33596 (2020).
Inoshita, T. et al. Vps35 in cooperation with LRRK2 regulates synaptic vesicle endocytosis through the endosomal pathway in Drosophila. Hum. Mol. Genet. 26, 2933–2948 (2017).
Wang, X. et al. Rab3 and synaptotagmin proteins in the regulation of vesicle fusion and neurotransmitter release. Life Sci. 309, 120995 (2022).
Robinson, B. G. et al. RIM is essential for stimulated but not spontaneous somatodendritic dopamine release in the midbrain. eLife 8, e47972 (2019).
Tang, F.-L. et al. VPS35 in Dopamine Neurons Is Required for Endosome-to-Golgi Retrieval of Lamp2a, a Receptor of Chaperone-Mediated Autophagy That Is Critical for α-Synuclein Degradation and Prevention of Pathogenesis of Parkinson’s Disease. J. Neurosci. 35, 10613–10628 (2015).
Hanss, Z. et al. Mitochondrial and Clearance Impairment in p.D620N VPS35 Patient-Derived Neurons. Mov. Disord. 36, 704–715 (2021).
Acknowledgements
The authors thank Dr. Esther Sammler of The Medical Research Council Protein Phosphorylation and Ubiquitylation Unit, School of Life Sciences, University of Dundee, Dundee, UK for her expertise and collaboration in the independent biochemical assessment of LRRK2 target engagement by A.J.S.
Author information
Authors and Affiliations
Contributions
A.Ka. performed most animal surgeries and experiments, contributed to the experimental design and curation, performed data analysis, and co-wrote the manuscript with A.J.M. C.A.K. contributed intellectually to the interpretation of findings and training of A.Ka. N.K. performed initial animal surgeries and contributed to the training of A.Ka. S.C. collected a subset of iGluSnFR recordings A.P., Y.C., A.Kh. and A.J.S performed training and western blots for LRRK2 target engagement E.H. prepared slices and collected recordings for a subset of iGluSnFR experiments J.C.B. performed animal surgery for a subset of iGluSnFR experiments M.P.P. contributed to the experimental design and analysis of iGluSnFR experiments and to the training of A.Ka. A.J.M. contributed experimental analytical design and curation, supervision & training of A.Ka., C.A.K., N.K., S.C., A.P., Y.C., A.Kh. and co-wrote the manuscript with A.Ka.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kamesh, A., Kadgien, C.A., Kuhlmann, N. et al. Emergent glutamate & dopamine dysfunction in VPS35(D620N) knock-in mice and rapid reversal by LRRK2 inhibition. npj Parkinsons Dis. 11, 106 (2025). https://doi.org/10.1038/s41531-025-00948-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-00948-7