Abstract
Motor abnormalities, including psychomotor slowing, are prevalent in a large proportion of individuals with schizophrenia. While postural control deficits have been observed in this population, the impact of motor abnormalities on postural stability remains unclear. This study aimed to objectively evaluate postural stability in patients with and without psychomotor slowing and healthy controls. Seventy-three schizophrenia patients with psychomotor slowing (PS; Salpêtrière Retardation Rating Scale (SRRS) ≥ 15), 25 schizophrenia patients without psychomotor slowing (non-PS; SRRS < 15), and 27 healthy controls (HC) performed four conditions on the Kistler force plate: eyes open (EO), eyes closed (EC), head reclined with eyes open (EOHR), and head reclined with eyes closed (ECHR). Larger sway areas and higher Root Mean Square (RMS) values indicate lower postural stability, while a lower Complexity Index (CI) reflects reduced adaptability, flexibility, and dynamic functioning of postural control. PS exhibited larger sway areas and higher RMS compared to the other groups. Both PS and non-PS showed reduced complexity in postural control compared to healthy controls, without differences between the two patient groups. Reduced postural stability and complexity were associated with greater expert-rated motor abnormalities, as well as more severe negative symptoms. Additionally, lower complexity was linked to reduced physical activity levels. These findings suggest that psychomotor slowing is associated with lower postural stability, potentially reflecting impaired cerebellar function. Furthermore, the loss of complexity in postural control highlights reduced flexibility, adaptability, and efficiency in the postural control network of individuals with schizophrenia.
Similar content being viewed by others
Introduction
Schizophrenia is a severely disabling mental disorder that usually has its onset in adolescence1,2. Common features of schizophrenia are positive (e.g., hallucinations) or negative (e.g., anhedonia and social withdrawal) symptoms, cognitive impairments (e.g., poor working memory), and motor abnormalities (e.g., psychomotor slowing, catatonia, parkinsonism, and neurological soft signs (NSS))3,4,5,6. Motor abnormalities are associated with a more sedentary lifestyle7, poorer long-term psychosocial functioning8, and predict a more severe course of disease9. Abnormal psychomotor behaviour including aberrant balance and postural control are found even in antipsychotic naïve schizophrenia patients10,11 as well as in individuals at ultra-high risk12,13.
Psychomotor slowing refers to generalised hypokinesia. It affects spontaneous fine and gross motor tasks, and it is linked to poorer non-verbal social perception and gestures14,15,16,17,18. Fine motor behaviour is evaluated through writing or complex finger manipulations such as coin rotations, whereas gross motor behaviour is assessed using walking tasks, postural stability, or actigraphy to measure overall physical activity.
Neuroimaging studies linked psychomotor slowing to aberrant functional and structural connectivity between the supplementary motor area (SMA), primary motor cortex (M1), basal ganglia, thalamus, and cerebellum19,20,21,22,23. Also, it has been shown that functional connectivity at rest between the primary motor cortex, the anterior cingulate cortex and the cerebellum increases with stronger cortical inhibition in patients with schizophrenia and psychomotor slowing24. This may indicate that postural stability might be impaired in patients with psychomotor slowing.
One convenient property of motor abnormalities is their physical nature, making them available to instrumental quantification. Traditional expert-rating scales rely on the information disclosed by the patient or on behaviours observed in interaction, which can be confounded by suspiciousness, amotivation, and observer bias5. The use of sensitive instruments (e.g., Posturography System and Wii Balance Board) and relevant variables is more reliable than patients’ self-reports or visual assessment by clinicians25,26.
Dynamics of quiet, upright stance are complex, involving visual, vestibular, proprioceptive, and somatosensory feedback loops, multiple brain areas, and the musculoskeletal system27. As the cerebellum integrates and processes postural information, postural stability could be considered as an easy to implement behavioural marker of cerebellar dysfunction28,29. The cerebellum is not exclusively involved in motor function, but also in cognition and emotion30. For instance, the cerebellum has also been implicated in neurological soft signs (NSS) and negative symptoms31,32,33. Still, other brain areas such as the basal ganglia, brain stem, and motor cortex are also strongly involved in movements and should be considered when studying postural control.
Previous studies demonstrated impaired postural stability in patients with schizophrenia compared to controls34,35,36,37,38. However, they rarely considered motor abnormalities when examining postural function in patients with schizophrenia34,35. The most commonly chosen parameters are the sway path or the sway area, that inform on the total path length of a person’s sway and the total area that it covers34,39,40.
In order for an organism to function and adapt to demands of everyday life, a wide repertoire of behaviour is crucial. The integration of multiple feedback loops, control systems, and regulatory processes is a prerequisite for appropriate reactions to changing environments. This flexibility and variability of a system or organism can be quantified using a measure of complexity41,42, such as complexity index (CI) measured by multiscale entropy43. A healthy person (with a highly flexible network of neuromuscular connections) exhibits more complex dynamics in postural control and hence shows high postural control. Aging or illnesses (e.g., multiple sclerosis, scoliosis, and bipolar disorder) can compromise feedback loops, leading to reduced physiological complexity and increased swaying41,43,44,45,46.
This study aimed to explore cerebellar function, using postural stability markers, in schizophrenia with psychomotor slowing and to explore associations between cerebellar dysfunction and motor abnormalities. We included a natural stance condition, as well as conditions with manipulated visual (i.e., eyes closed), vestibular (i.e., head reclined), and proprioceptive (i.e., tandem stance) information. We hypothesised that patients with psychomotor slowing (PS) would show less postural control and less complexity compared to patients without psychomotor slowing (non-PS) and healthy controls (HC). We expected the deficit in postural control to increase from natural and ecological conditions (e.g., eyes open) to challenging conditions (e.g., eyes closed, head reclined, and tandem stance). In addition, we hypothesised that within patients, postural sway parameters would be associated with expert ratings of several hypokinetic motor abnormalities and negative symptoms.
Material and methods
Participants
We included baseline data of 98 patients fulfilling the criteria for schizophrenia spectrum disorders according to the Structured Clinical Interview for DSM-5® (SCID-5) and taking part in the recently completed prospective randomised, double-blind, placebo-controlled OCoPS-P study (Overcoming Psychomotor Slowing in Psychosis; ClinicalTrials.gov Identifier: NCT03921450)47. Using a cut-off score of 15 points on the Salpêtrière Retardation Rating Scale48 (SRRS), patients were categorised into a group with psychomotor slowing (PS, SRRS ≥ 15, N = 73) and without (non-PS, SRRS < 15, N = 25). We additionally included 27 age- and sex-matched healthy controls (HC) who neither had a history of psychiatric disorder nor any first-degree relative with schizophrenia spectrum disorder. General exclusion criteria included age <18 and >60 years, active substance abuse or dependence (except nicotine), past or current neurological disorders impacting motor behaviours, seizures, or hearing problems. All patients were recruited at the in- and out-patient departments of the University Hospital of Psychiatry and Psychotherapy in Bern, Switzerland. All except 3 patients were taking antipsychotics at the time of baseline assessments. Controls were contacted using flyers, online announcements, or word of mouth. All participants signed written informed consent prior to study participation. The study protocol adhered to the Declaration of Helsinki and was approved by the local ethics committee (2018-02164).
Procedures and measures
Clinical and motor scales
We measured general psychopathology with the Positive And Negative Symptom Scale (PANSS)49 and negative symptoms with the Brief Negative Symptom Scale (BNSS)50. Psychomotor slowing was assessed using the Salpêtrière Retardation Rating Scale (SRRS)48. Focusing on the motor components of psychomotor slowing, the first five items plus the last one (gait, movements of limbs/trunk, movements of head/neck, verbal flow, modulation of voice, and general appreciation) were summarised in the subscore mSRRS17,51,52. We also assessed other motor abnormalities, such as parkinsonism (Unified Parkinson’s Disease Rating Scale—Part III, UPDRS)53, Catatonia (Bush-Francis Catatonia Rating Scale, BFCRS)54, and neurological soft signs (Neurological Evaluation Scale, NES)55.
To objectively measure participants’ gross movements in a day, subjects wore a tri-axial-accelerometer Move4 (movisens GmbH, Karlsruhe, Germany) continuously for 24 h on their non-dominant arm7,21,52,56,57,58,59,60. Sleeping hours (including naps) were removed before calculating the activity level per hour (AL/h) with the Movisens DataAnalyzer Software. Current antipsychotic medication was converted into olanzapine equivalents (OLZ eq.) according to Leucht61.
Measurement of postural stability
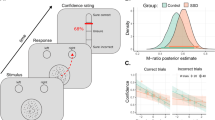
The participant’s balance was assessed using a 40 cm × 60 cm Kistler force plate (Type 9286A, Kistler Instrumente AG, Winterthur Schweiz). Participants were instructed to keep still, to relax their arms at their side, and to stand comfortably (e.g., feet approximately hip-width apart). We then manipulated visual (eyes open vs. closed), vestibular (head in natural upright position vs. head reclined), and proprioceptive inputs (feet hip-width apart vs. tandem stance). With a combination of these manipulations the origin of a deficit in postural control of patients might be identifiable.
If participants lost their balance, they could quickly hold on to a bar in front of them if necessary and/or quickly open their eyes in the eyes-closed tasks. Any occurrence of these safety behaviours (touching the bar or opening the eyes) was noted.
The centre of pressure (CoP) was recorded along the antero-posterior and medio-lateral axes (Fig. 1) with a sampling rate of 40 Hz using NeuroPlatform262. Each participant performed the conditions for 30 s in the following order: (i) eyes open in a natural stance (i.e., upright head position, feet hip-width apart) (EO); (ii) eyes closed in a natural stance (EC); (iii) eyes open and head reclined (EOHR); iv) eyes closed and head reclined (ECHR); (v) eyes open and tandem stance (i.e., one foot directly in front of the other in a straight line, with toes of one foot touching the heel of the other foot) (EOTS); (vi) eyes closed and tandem stance (ECTS).
The conditions EOTS and ECTS were exceptionally difficult for all participants due to the altered proprioceptive input (tandem stance instead of feet hip-width apart). In the tandem stance, the physical basis for postural control is heavily compromised, and neither visual, vestibular, nor proprioceptive inputs can fully compensate. Hence, the disproportionally high variance in EOTS and ECTS made these conditions incomparable to the first four conditions, which is why they were analysed separately (Tables S19 and S20, Fig. S7). Sample sizes vary between conditions, as some participants were unable to correctly perform them (e.g., falling off the platform without continuous use of safety behaviours and assistance).
We used six parameters to analyse postural stability: the root mean square (RMS) of CoP displacement in medio-lateral (RMSml) and antero-posterior (RMSap) direction and total (RMStotal), the sway area, and the Complexity Index (CI) in the medio-lateral (CIml) and antero-posterior (CIap) direction. For one participant the raw data was missing. Extreme outliers were defined as three interquartile ranges above the third or below the first quantile and removed for each parameter and each condition separately prior to analyses.
Root mean square
The RMS defines the displacement of all individual CoP measurements around the mean CoP for the whole measurement63. The RMS displays the average distance deviation from the mean of the recorded data points \(\bar{({\boldsymbol{x}})}\) in mm64. Higher RMS indicates worse balance65. We used PosturographicExplorer2 (version 2.0.77.2011, 2011, Dr. Sergei Novoshilov, Dr. Siegbert Krafczyk; Formula 1 + 2)66,67 to convert the raw CoP data into the three RMS measures (RMSml, RMSap, RMStotal). We removed 10 participants (6 PS, 2 non-PS, 2 HC) who were extreme outliers in at least one RMS measure in at least one condition. If a participant was an outlier in one RMS value, all RMS values were removed for that condition.
Formula 1 + 2.
Note. N = total number of measurement points over time; \(\,{x}_{{i}}\) = individual measured values in medio-lateral or antero-posterior direction; \(\bar{x}\) = mean of the measured data points
Sway area
The sway area represents the area that encloses the CoP data points (mm2). A large sway area results from more body swaying, i.e., worse balance68. The sway area was calculated from the raw CoP data in Matlab (MATLAB Version: 9.13.0.2166757 (R2022b) Update 4) using the convex hull method (Fig. 2, Figs. S1 and S2)69. We excluded the sway area of 12 participants (7 PS, 3 non-PS, 2 HC) as extreme outliers. Only the extreme condition was removed, while the other conditions of that participant were included.
Note. Same x- and y-scale is used for all plots to increase comparability (mm). Other conditions are presented in the supplements (S-Figs. 1 and 2). Top: Sway path and border defining the sway area of three individuals that best represent the median of their group during EO condition. Red PS, yellow non-PS, blue HC. Middle: scatterplot of all CoP measuring points of all individuals of the three groups together during EO condition. Bottom: Density plot illustrating the dispersion and height of the scatterplot above. Colour scale ranges from yellow (highest density of CoP data points) to dark purple (no or almost no CoP data points).
Complexity index
Complexity in postural sway reflects the adaptability and flexibility of the postural control system42,43. Higher complexity indicates a more dynamic and responsive system, capable of making varied and timely corrections to maintain balance, it should result in less overall sway. In contrast, reduced complexity indicates a less responsive postural system, associated with more predictable and larger sway patterns (Tables S14 and S15, Fig. S5).
Sample entropy quantifies the irregularity of temporal patterns in a given signal. Multiscale sample entropy extends the traditional sample entropy by assessing the entropy of a signal at various levels of temporal resolution (i.e., coarse-graining the data to different timescales), thereby capturing both short-term and long-term dynamics43,70. The complexity index reflects the area under the curve of sample entropy versus timescale (τ)41,43,70. For more in-depth explanation on the calculation refer to the Supplements.
We calculated the complexity index (CI) separately for the raw medio-lateral and antero-posterior CoP data using Matlab, using τ = 6 timescales, a similarity threshold (r) of 15% and a sequence length (m) of 2, as recommended in the literature43,70,71.
The complexity index showed no outliers; however, one participant, who was an outlier in both RMS and sway area across both conditions with the head reclined, was excluded from the complexity analysis for these conditions.
Statistical analyses
All analyses were done using R (4.3.0) and RStudio (2023.06.0 + 421). We calculated the extreme outliers (three interquartile ranges above the third or below the first quantile) for each parameter and each condition separately. Sample sizes vary slightly between analyses. Also, some data is not available for some participants (e.g., refusal of actigraphy). A p-value < 0.05 was considered to be significant. We used false discovery rate (FDR) to account for multiple comparisons (pcorr). Demographic and clinical characteristics were compared with Mann–Whitney U tests, ANOVAs, and chi-square tests (Table 1). We used a repeated-measures ANOVA for each postural parameter including 3 groups (Table 2, Fig. 3, Table S1) and 4 conditions (Table S2). P-values of 12 main effects and 6 interactions are corrected for multiple comparisons using FDR (pcorr).
Note. Points show individual measurements, violin the approximate distribution, boxplot the quartiles (1st, median, 3rd), black cross indicates the mean. Red PS, yellow non-PS, blue HC, EO eyes open, natural upright head position, and feet hip-width apart, EC eyes closed natural upright head position, and feet hip-width apart, EOHR eyes open, head reclined, and feet hip-width apart, ECHR eyes closed, head reclined, and feet hip-width apart, PS patients with psychomotor slowing, non-PS patients without psychomotor slowing, HC healthy controls, RMSml Root Mean Square medio-lateral, RMSap Root Mean Square antero-posterior, RMStotal Root Mean Square for total deviation, Clml Complexity Index medio-lateral, Clap Complexity Index antero-posterior. * pcorr < 0.05.
Further, we correlated the six postural parameters with clinical rating scales (mSRRS, UPDRS, BFCRS, NES total and subscores, BNSS total and subscores), as well as activity level using Kendall’s Tau for the EO condition across all patients (PS and non-PS) (Table 3, Figs. 4 and S3). All p-values are corrected using FDR (pcorr). In the Supplements we included these associations separated for PS and non-PS in EO (Table S9), the associations across patients for the other conditions (Tables S10–S12), and across all participants for activity level (Table S13, Fig. S4).
Note. Scatterplots show the association between selected postural parameters and clinical rating scales. Datapoints: red circles PS, yellow triangles non-PS. Regression lines: red PS, yellow non-PS, black correlation within total sample. RMSml Root Mean Square medio-lateral, Clml Complexity Index medio-lateral, UPDRS Unified Parkinson’s Disease Rating Scale part III, NES Neurological Evaluation Scale.
Sensitivity analyses demonstrated the robustness of our findings in the light of potential confounders such as, age, sex, BMI, safety behaviours, outliers, and medication (Tables S3–S5, S16–S18, Fig. S6). Furthermore, several additional analyses such as the two-way and three-way ANOVAs with factors “vision” and “vestibular” across conditions (Tables S6–S8), associations of swaying and complexity (Tables S14 and S15, Fig. S5), analyses for the tandem stance conditions (Tables S19 and S20, Fig. S7), sway path (Table S23), and sway velocity (Table S24) are reported in the Supplements.
Results
Demographics and clinical data
Groups did not differ in age, BMI, or sex distribution. PS had higher PANSS total scores, more negative symptoms (e.g., BNSS total), and motor abnormalities (e.g., mSRRS, UPDRS, BFCRS, and NES total) than non-PS. Additionally, PS had lower activity levels than non-PS and controls according to actigraphy (Table 1).
Group differences
For every postural parameter we found a main effect of group, with inferior performance of PS vs. controls. Except in CIml and Clap there was also a main effect of condition (Fig. 3, Table 2, Table S1). In most postural parameters and conditions, non-PS presented a mean value in-between the PS and controls. No group by condition interactions were present.
Root mean square
Post-hoc pairwise comparisons revealed a higher RMS in PS compared to the controls when manipulating either visual or vestibular input or both. Group differences appear to be bigger in the medio-lateral than in the antero-posterior direction, as in the medio-lateral direction there are also group differences between PS and non-PS.
Sway area
PS show a larger sway area compared to controls when eyes are closed and/or the head is reclined. PS and non-PS solely differ when only the visual input was omitted (EC).
Complexity index
In CIml, we noted lower complexity in PS compared to controls when the visual or vestibular system is challenged but found no difference during EO. In contrast, in PS the CIap is already reduced compared to controls in the most ecological condition (EO). Notably, only in the complexity we see differences between non-PS and controls.
Correlations
The severity of psychomotor slowing, parkinsonism, catatonia, and NSS is associated with a higher RMS and a lower CI (Table 3, Fig. 4, Fig. S3) in EO. Parkinsonism and NSS also correlate with sway area. RMSml and CIml are consistently associated with all BNSS subscores, except Asocial. The subscore Affect shows a correlation with all postural parameters except RMSap. Furthermore, more activity is associated with higher complexity in antero-posterior direction across patients; the association in ml-direction was no longer significant after FDR-correction.
Sensitivity analyses
Results of all further analyses are in the Supplements (Tables S6–S15, S21–S24, Fig. S4, S5, and S8). Potential confounders did not change the results considerably (Tables S3–S5, S16–S18, Fig. S6).
In EOTS, groups showed similar differences as the presented conditions. ECTS was very difficult for all groups, which is visible in the sway area in ECTS that is around 8 times larger than in EOTS and around 20 times larger than in EO (Tables S19 and S20, Fig. S7).
Discussion
This study aimed to explore cerebellar function in schizophrenia patients with psychomotor slowing (PS). We measured postural stability in schizophrenia patients with and without psychomotor slowing (PS and non-PS) and healthy controls (HC) using a Kistler platform in four conditions. In line with our first hypothesis, PS are less stable compared to controls, especially in the medio-lateral direction. Also, patients with schizophrenia (PS and non-PS) showed lower complexity in their postural stability compared to controls in both swaying directions. In line with our second hypothesis, we found associations between postural parameters and expert-rated motor abnormalities, negative symptoms, and activity level.
Postural stability
PS are less stable compared to controls in multiple postural conditions, specifically in the medio-lateral direction. In the most natural condition EO, PS can compensate for potential deficits, which is no longer possible when visual or vestibular input is limited, leading to greater group differences in difficult conditions (EC, EOHR, and ECHR). Non-PS generally show an intermediate position.
Irrespective of motor abnormalities, patients with schizophrenia had demonstrated impaired balance compared to controls34,35,36,38,72. Our results extend previous reports, as motor abnormalities greatly influence postural sway, surpassing the impact of a schizophrenia diagnosis. Data of non-PS were closer to controls than PS. We found no interaction between groups and conditions, although non-PS seem to be closer to controls during natural tasks and closer to PS in difficult tasks. Importantly, PS were impaired in all conditions, pointing to specific dysfunctions in PS, for example in the cerebellar circuits. Postural stability is an ideal behavioural marker for the functioning of the cerebellum, as the cerebellum is strongly involved in the maintenance of balance by integrating visual, proprioceptive, and vestibular sensory inputs, fine-tuning the timing, and correcting motor responses35,73. There are consistent reports of cerebellar dysfunctions in schizophrenia from eye-blink conditioning74, finger-tapping tasks75,76, and neuroimaging studies20,24,40,77,78,79,80. Cerebellar dysfunctions are thought to contribute to the cognitive dysmetria hypothesis in schizophrenia via the cortico-cerebellar-thalamic-cortical circuit (CCTCC), leading to problems in prioritising, processing, coordinating, and appropriately responding to information77,81,82.
In addition to the cerebellum, other brain structures are also involved in integrating sensory, visual, or proprioceptive information for postural control13. For example, the basal ganglia or the vestibular system play an important role in postural control and have also been shown to be compromised in schizophrenia36,83,84,85,86. Therefore, future research should focus on clarifying the simultaneous involvement of multiple brain regions.
Methods in prior studies led to equivocal findings34,72. Here, we demonstrate that all participants sway more in antero-posterior direction than in medio-lateral direction, which is due to biomechanical properties of the ankle joint and the foot placement87. Interestingly, we find stronger group differences in medio-lateral direction than in antero-posterior direction, possibly due to our highly motorically impaired sample.
Our results showed that there is no difference in the postural stability of controls and PS if all sensory inputs are unrestricted (EO). There are previous studies that support our finding that balance in schizophrenia patients is impaired in the absence of visual input34,36, while others do not35,72.
Structural and functional alterations are frequently found in the motor system of patients with schizophrenia, which are associated with motor abnormalities20,79,82,88,89,90,91. Alterations in the motor system in schizophrenia span cerebral blood flow22,92, white matter integrity21,93, resting-state and task fMRI24,78,90, and effective connectivity76. Also, patients with schizophrenia exhibit reduced cerebellar volumes compared to controls94,95, and lower cerebellar grey matter density24. Two meta-analyses observed reduced cerebellar grey matter volumes already in first-episode patients with schizophrenia and in people at clinical high risk of psychosis90,91. Also, the cerebellum shows altered connectivity to the motor cortices, the thalamus, and the basal ganglia during resting-state functional connectivity88,96,97,98,99,100. Importantly, this dysconnectivity is already present in subjects at clinical high risk of psychosis40 and there might even be longitudinal associations between aberrant CCTCC connectivity and conversion to psychosis and/or positive symptom progression98,101.
We speculate that these alterations in the cerebellum could be a distinct neural substrate for postural impairments in schizophrenia and might explain the deficits we found in this study. Bernard et al. demonstrated that individuals at ultra-high risk have increased postural sway and reduced resting-state functional connectivity between the cerebellum and the cortex across multiple networks compared to controls and an association between postural sway and resting-state functional connectivity40. This points to a potential deficit in sensory integration already at high risk for schizophrenia and supports the cognitive dysmetria hypothesis.
In summary, there is compelling evidence of structural and functional alterations in the cerebellum and its involvement in schizophrenia and in postural deficits. Nevertheless, the implications of these findings remain largely unclear.
Complexity
Patients with schizophrenia showed lower complexity in their postural stability compared to controls in both swaying directions. Unexpectedly, we found no effect of psychomotor slowing, although PS consistently had slightly lower complexity in medio-lateral direction than non-PS. Still, complexity in postural stability seems to be affected in schizophrenia in general and is not substantially reduced by psychomotor slowing.
Non-linear analyses such as complexity have been used in the last 30 years to investigate various data in ageing and disease27,34,42,44. Despite compelling and growing evidence of its relevancy, still, complexity remains an emerging field and functional implications are largely unknown27. The complexity in CoP dynamics in postural control is affected by ageing and disease. Neuropsychiatric disorders may affect postural control and reduce complexity44,46.
This is the first study to investigate complexity in postural control in schizophrenia using multiscale sample entropy as a measure of complexity. Kent et al. have investigated postural control deficits in schizophrenia using detrended fluctuation analysis, which itself is not a measure of complexity, but can be related to signal complexity34. Moreover, we are the first to focus on motor abnormalities in schizophrenia in the context of postural stability and complexity.
Likewise, Kent et al. found lower complexity in both medio-lateral and antero-posterior direction in patients with schizophrenia compared to controls at trend level. Furthermore, they detected a main effect of condition (eyes open vs. closed and feet together vs. shoulder-width apart) in both directions. They concluded that schizophrenia might be associated with inefficient adaptation when deprived of visual information during postural control. Instead, our complexity analysis suggests that patients with schizophrenia are inefficient in maintaining postural control regardless of the condition, as there is no main effect of condition in our data. Patients with schizophrenia show reduced complexity already in EO condition, and the complexity does not change much between conditions regardless of varying visual or vestibular input. Concurrently, PS had greater impaired postural stability measured with RMS and sway area in the complex conditions with sensory deprivation.
Associations
In line with our second hypothesis, we found associations between postural parameters and expert-rated motor abnormalities and negative symptoms in the EO condition. Parkinsonism (UPDRS), as well as the motor coordination subscore of the NES, were most strongly associated with postural stability. The subscore Affect of the BNSS was associated with all postural parameters except RMSap. Also, the CIml was associated with BNSS subscores. Interestingly, we also found a positive correlation between activity level and CI, as has previously been proposed by Busa et al. 44.
Negative symptoms are a key predictor of unfavourable functional outcome in patients with schizophrenia102. Few studies tested the association of negative symptoms with metrics of postural stability or complexity and yielded conflicting results34,36,40,72. We found RMSml and CIml to be associated with negative symptoms, although with a small effect.
The CCTCC might be part of the neural underpinnings for negative symptoms in schizophrenia32,33,103. Compromised cerebellar-(subcortical-)prefrontal connectivity was implicated with negative symptom severity in patients with schizophrenia32,33,104. In fact, cerebellar transcranial magnetic stimulation (TMS) rescued the cerebello-(subcortical-)cortical connectivity33,104, ameliorating negative symptoms in a RCT by Brady et al. 33, but no clinical effect was seen in another RCT by Basavaraju et al. 104. In sum, there is some empirical support for a causal relationship between cerebellar-(subcortical-)prefrontal dysfunctional connectivity and psychopathology which appears even in prodromal states of psychosis40,105.
Neurological soft signs (NSS) are minor neurological abnormalities with deficits in sensory integration, motor coordination, and sequencing of motor tasks, often associated with negative symptom severity and poor outcome32,106,107. We found postural deficits to be associated with stronger NSS, especially in the motor coordination subscore.
Our study is the first linking NSS with postural stability in patients with schizophrenia. Marvel et al. found no association between tardive dyskinesia and postural stability, but did not include additional motor abnormalities, such as parkinsonism and NSS35. Conceptually, postural stability is tied to NSS5,108. Difficulties in the motor coordination domain of NSS manifest as abnormalities in general coordination, balance, and gait108, while the NES assesses tandem walk, rapid alternating movements, finger-thumb opposition, and finger-nose pointing. Postural stability is critical to perform the tandem walk, explaining the associations we found.
Cerebellar (network) alterations might be able to explain our result of an association between NSS and postural stability. The cerebellum, SMA, and the basal ganglia form a complex integrated network, thought to contribute to NSS24,31,109,110,111,112. If the CCTCC-network shows aberrant activity, this could lead to aberrant motor coordination, execution, and planning113. Indeed, Lefebvre et al. reported an association between lower cortical inhibition in the primary motor cortex and more motor coordination deficits24. Following this, psychomotor slowing in psychosis might also be linked to cortical inhibitory dysfunction and more neural noise in the motor system24.
Our results show that there are postural stability deficits in schizophrenia, but even more so with motor abnormalities such as psychomotor slowing. Regardless of the postural condition, PS show a deficit in postural stability compared to controls. In addition, the complexity in the CoP is reduced in patients versus controls, suggesting reduced variability, flexibility, and physiological function in postural control in schizophrenia. Our results further corroborate the role of the cerebellum in abnormal psychomotor behaviour, specifically NSS, as well as in negative symptoms. Thus, NSS and negative symptoms might share neural mechanisms in schizophrenia, and postural stability might be an easily accessible screening tool and could be used for monitoring of treatment progress. Nevertheless, there are still many inconsistencies in the existing literature and a lack of research on longitudinal neural changes.
Limitations
This study has several limitations. Firstly, we recorded daily medications but lack information on total antipsychotic exposure. However, including current medication (OLZ eq.) as a covariate in the group comparison did not affect the results. Also, no correlation has been found between antipsychotic dosage and the amount of sway35 and postural stability seems equally affected in unmedicated patients with schizophrenia and individuals at ultra-high risk38,39,40. Secondly, the literature is full of heterogeneity in assessing postural sway, potentially leading to inconsistent findings and hindering comparisons across studies114. Thirdly, no imaging data was included in this analysis to support the speculation of the cerebellum being affected, which suggest for future studies. Fourthly, this paper has placed a strong emphasis on the cerebellum due to the growing body of research linking schizophrenia, postural control, and neuroimaging findings that highlight its role. However, other brain regions, such as the basal ganglia and brainstem, also contribute to postural regulation and motor control. Future work should aim to clarify the simultaneous involvement of these regions alongside the cerebellum, offering a more comprehensive understanding of the neural mechanisms underlying postural instability in schizophrenia. Finally, postural stability and psychiatric symptoms seem to be associated cross-sectionally, while we lack information on the longitudinal development.
Conclusion
Independent of the postural condition, patients with schizophrenia and psychomotor slowing (PS) show a deficit in postural stability and complexity compared to controls, with patients without psychomotor slowing (non-PS) in an intermediate position. Psychomotor slowing impairs postural stability, leading to differences between PS and the other groups. Complexity is reduced in schizophrenia in general, without differences between patient groups. Postural sway is related to motor abnormalities and negative symptoms, possibly due to the involvement of the cerebellum. The postural sway task might be an easily accessible clinical tool to screen and monitor treatment outcomes.
Data availability
Participants have not provided consent to broad data sharing of their health-related data.
References
Jauhar, S., Johnstone, M. & McKenna, P. J. Schizophrenia. Lancet 399, 473–486 (2022).
McCutcheon, R. A., Reis Marques, T. & Howes, O. D. Schizophrenia—an overview. JAMA Psychiatry 77, 201–210 (2020).
Tandon, R., Nasrallah, H. A. & Keshavan, M. S. Schizophrenia, “just the facts” 4. Clinical features and conceptualization. Schizophr. Res. 110, 1–23 (2009).
Tandon, R. et al. Definition and description of schizophrenia in the DSM-5. Schizophr. Res. 150, 3–10 (2013).
van Harten, P. N., Walther, S., Kent, J. S., Sponheim, S. R. & Mittal, V. A. The clinical and prognostic value of motor abnormalities in psychosis, and the importance of instrumental assessment. Neurosci. Biobehav. Rev. 80, 476–487 (2017).
Walther, S. & Strik, W. Motor symptoms and schizophrenia. Neuropsychobiology 66, 77–92 (2012).
Walther, S. et al. Low physical activity is associated with two hypokinetic motor abnormalities in psychosis. J. Psychiatr. Res. 146, 258–263 (2022).
Cuesta, M. J. et al. Motor abnormalities in first-episode psychosis patients and long-term psychosocial functioning. Schizophr. Res. 200, 97–103 (2018).
Ferruccio, N. P. et al. Neurological signs at the first psychotic episode as correlates of long-term outcome: results from the AESOP-10 study. Schizophr. Bull. 47, 118–127 (2021).
Peralta, V., Campos, M. S., De Jalón, E. G. & Cuesta, M. J. Motor behavior abnormalities in drug-naïve patients with schizophrenia spectrum disorders. Mov. Disord. 25, 1068–1076 (2010).
Pappa, S. & Dazzan, P. Spontaneous movement disorders in antipsychotic-naive patients with first-episode psychoses: a systematic review. Psychol. Med. 39, 1065–1076 (2009).
Kindler, J. et al. Abnormal involuntary movements are linked to psychosis-risk in children and adolescents: Results of a population-based study. Schizophr. Res. 174, 58–64 (2016).
Mittal, V. A., Neumann, C., Saczawa, M. & Walker, E. F. Longitudinal progression of movement abnormalities in relation to psychotic symptoms in adolescents at high risk of schizophrenia. Arch. Gen. Psychiatry 65, 165–171 (2008).
Docx, L. et al. Parsing the components of the psychomotor syndrome in schizophrenia. Acta Psychiatr. Scand. 126, 256–265 (2012).
Docx, L., Sabbe, B., Provinciael, P., Merckx, N. & Morrens, M. Quantitative psychomotor dysfunction in schizophrenia: a loss of drive, impaired movement execution or both? Neuropsychobiology 68, 221–227 (2013).
Putzhammer, A. et al. Spatial and temporal parameters of gait disturbances in schizophrenic patients. Schizophr. Res. 69, 159–166 (2004).
Nuoffer, M. G. et al. Psychomotor slowing alters gait velocity, cadence, and stride length and indicates negative symptom severity in psychosis. Schizophrenia 8, 116 (2022).
Walther, S. et al. Nonverbal social communication and gesture control in schizophrenia. Schizophr. Bull. 41, 338–345 (2015).
Viher, P. V. et al. Aberrant fronto-striatal connectivity and fine motor function in schizophrenia. Psychiatry Res. Neuroimaging 288, 44–50 (2019).
Walther, S. et al. Aberrant hyperconnectivity in the motor system at rest is linked to motor abnormalities in schizophrenia spectrum disorders. Schizophr. Bull. 43, 982–992 (2017).
Walther, S. et al. Alterations of white matter integrity related to motor activity in schizophrenia. Neurobiol. Dis. 42, 276–283 (2011).
Walther, S. et al. Resting state cerebral blood flow and objective motor activity reveal basal ganglia dysfunction in schizophrenia. Psychiatry Res. 192, 117–124 (2011).
Bracht, T. et al. Altered cortico-basal ganglia motor pathways reflect reduced volitional motor activity in schizophrenia. Schizophr. Res. 143, 269–276 (2013).
Lefebvre, S. et al. The pathobiology of psychomotor slowing in psychosis: altered cortical excitability and connectivity. Brain 147, 1423–1435 (2024).
Paillard, T. & Noe, F. Techniques and methods for testing the postural function in healthy and pathological subjects. Biomed. Res. Int. 2015, 891390 (2015).
Huang, C. C., Hung, H. H., Jaw, F. S. & Young, Y. H. Comparison of the Wii balance board system and foam posturography system in assessing postural balance. Ear Hear 43, 1800–1806 (2022).
Manor, B. et al. Physiological complexity and system adaptability: evidence from postural control dynamics of older adults. J. Appl Physiol. (1985) 109, 1786–1791 (2010).
Diener, H. C., Dichgans, J., Guschlbauer, B., Bacher, M. & Langenbach, P. Disturbances of motor preparation in basal ganglia and cerebellar disorders. Prog. Brain Res. 80, 481–488 (1989). discussion 479–480.
Pasma, J. H. et al. Impaired standing balance: the clinical need for closing the loop. Neuroscience 267, 157–165 (2014).
Schmahmann, J. D. The cerebellum and cognition. Neurosci. Lett. 688, 62–75 (2019).
Zhao, Q. et al. Neurological soft signs are not “soft” in brain structure and functional networks: evidence from ALE meta-analysis. Schizophr. Bull. 40, 626–641 (2014).
Cai, X. L. et al. Neurological soft signs are associated with altered cerebellar-cerebral functional connectivity in schizophrenia. Schizophr. Bull. 47, 1452–1462 (2021).
Brady, R. O. Jr. et al. Cerebellar-prefrontal network connectivity and negative symptoms in schizophrenia. Am. J. Psychiatry 176, 512–520 (2019).
Kent, J. S. et al. Motor deficits in schizophrenia quantified by nonlinear analysis of postural sway. PLoS ONE 7, e41808 (2012).
Marvel, C. L., Schwartz, B. L. & Rosse, R. B. A quantitative measure of postural sway deficits in schizophrenia. Schizophr. Res. 68, 363–372 (2004).
Teng, Y. L. et al. Postural stability of patients with schizophrenia during challenging sensory conditions: implication of sensory integration for postural control. PLoS ONE 11, e0158219 (2016).
Kim, D. J. et al. Cerebellar-cortical dysconnectivity in resting-state associated with sensorimotor tasks in schizophrenia. Hum. Brain Mapp. 41, 3119–3132 (2020).
Apthorp, D., Bolbecker, A. R., Bartolomeo, L. A., O’Donnell, B. F. & Hetrick, W. P. Postural sway abnormalities in schizotypal personality disorder. Schizophr. Bull. 45, 512–521 (2019).
Bolbecker, A. R., Apthorp, D., Bartolomeo, L. A., O’Donnell, B. F. & Hetrick, W. P. Postural sway in first-degree relatives of individuals with schizophrenia. Schizophr. Res. 228, 319–321 (2021).
Bernard, J. A. et al. Cerebellar networks in individuals at ultra high-risk of psychosis: impact on postural sway and symptom severity. Hum. Brain Mapp. 35, 4064–4078 (2014).
Gow, B. J., Peng, C.-K., Wayne, P. M. & Ahn, A. C. Multiscale entropy analysis of center-of-pressure dynamics in human postural control: methodological considerations. Entropy 17, 7926–7947 (2015).
Lipsitz, L. A. & Goldberger, A. L. Loss of ‘complexity’ and aging. Potential applications of fractals and chaos theory to senescence. J. Am. Med. Assoc. 267, 1806–1809 (1992).
Busa, M. A. & van Emmerik, R. E. A. Multiscale entropy: a tool for understanding the complexity of postural control. J. Sport Health Sci. 5, 44–51 (2016).
Busa, M. A., Jones, S. L., Hamill, J. & van Emmerik, R. E. Multiscale entropy identifies differences in complexity in postural control in women with multiple sclerosis. Gait Posture 45, 7–11 (2016).
Gruber, A. H. et al. Time-to-contact and multiscale entropy identify differences in postural control in adolescent idiopathic scoliosis. Gait Posture 34, 13–18 (2011).
Bolbecker, A. R. et al. Postural control in bipolar disorder: increased sway area and decreased dynamical complexity. PLoS ONE 6, e19824 (2011).
Walther, S. et al. Psychomotor slowing in psychosis and inhibitory repetitive transcranial magnetic stimulation: a randomized clinical trial. JAMA Psychiatry 81, 563–571 (2024).
Dantchev, N. & Widlöcher, D. J. The measurement of retardation in depression. J. Clin. Psychiatry 59(Suppl 14), 19–25 (1998).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
Kirkpatrick, B. et al. The brief negative symptom scale: psychometric properties. Schizophr. Bull. 37, 300–305 (2011).
Nadesalingam, N. et al. Motor abnormalities are associated with poor social and functional outcomes in schizophrenia. Compr. Psychiatry 115, 152307 (2022).
Nadesalingam, N. et al. The behavioral mapping of psychomotor slowing in psychosis demonstrates heterogeneity among patients suggesting distinct pathobiology. Schizophr. Bull. 49, 507–517 (2022).
Fahn S. & Elton R. L. Unified Parkinson’s disease rating scale. In: (eds Fahn S, Marsden CD, Goldstein M, Calne DB). Recent Developments in Parkinson’s Disease. pp. 153–164 (Macmillan Healthcare Information, Florham Park, NJ, 1987).
Bush, G., Fink, M., Petrides, G., Dowling, F. & Francis, A. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr. Scand. 93, 129–136 (1996).
Buchanan, R. W. & Heinrichs, D. W. The Neurological Evaluation Scale (NES): a structured instrument for the assessment of neurological signs in schizophrenia. Psychiatry Res. 27, 335–350 (1989).
von Känel, S. et al. Measuring catatonia motor behavior with objective instrumentation. Front. Psychiatry 13, 880747 (2022).
Walther, S. et al. Quantitative motor activity differentiates schizophrenia subtypes. Neuropsychobiology 60, 80–86 (2009).
Walther, S., Koschorke, P., Horn, H. & Strik, W. Objectively measured motor activity in schizophrenia challenges the validity of expert ratings. Psychiatry Res. 169, 187–190 (2009).
Walther, S., Ramseyer, F., Horn, H., Strik, W. & Tschacher, W. Less structured movement patterns predict severity of positive syndrome, excitement, and disorganization. Schizophr. Bull. 40, 585–591 (2014).
Walther, S. et al. The longitudinal course of gross motor activity in schizophrenia—within and between episodes. Front. Psychiatry 6, 1–10 (2015).
Leucht, S. et al. Dose equivalents for second-generation antipsychotic drugs: the classical mean dose method. Schizophr. Bull. 41, 1397–1402 (2015).
NeuroPlatform [computer program]. Version 2 Krafczyk S and Nowoshilow S.
Şimşek T. T., & Şimşek, İ. E. Balance and postural control. In: (ed Angin SS, Ibrahim) Comparative Kinesiology of the Human Body: Normal and Pathological Conditions pp. 467–475 (2020).
Neville, C., Ludlow, C. & Rieger, B. Measuring postural stability with an inertial sensor: validity and sensitivity. Med. Devices (Auckl.) 8, 447–455 (2015).
Brandt, T., Krafczyk, S. & Malsbenden, I. Postural imbalance with head extension: improvement by training as a model for ataxia therapy. Ann. N. Y. Acad. Sci. 374, 636–649 (1981).
Krafczyk, S., Tietze, S., Swoboda, W., Valkovic, P. & Brandt, T. Artificial neural network: a new diagnostic posturographic tool for disorders of stance. Clin. Neurophysiol. 117, 1692–1698 (2006).
Brandt, T., Strupp, M., Novozhilov, S. & Krafczyk, S. Artificial neural network posturography detects the transition of vestibular neuritis to phobic postural vertigo. J. Neurol. 259, 182–184 (2012).
Cherng, R. J., Hsu, Y. W., Chen, Y. J. & Chen, J. Y. Standing balance of children with developmental coordination disorder under altered sensory conditions. Hum. Mov. Sci. 26, 913–926 (2007).
Wollseifen, T. Different methods of calculating body sway area. Pharm. Program. 4, 91–106 (2011).
Kosciessa, J. Q., Kloosterman, N. A. & Garrett, D. D. Standard multiscale entropy reflects neural dynamics at mismatched temporal scales: what’s signal irregularity got to do with it? PLoS Comput. Biol. 16, e1007885 (2020).
Multiscale Sample Entropy [computer program]. MATLAB Central File Exchange (2023).
Matsuura, Y. et al. Standing postural instability in patients with schizophrenia: relationships with psychiatric symptoms, anxiety, and the use of neuroleptic medications. Gait Posture 41, 847–851 (2015).
Manzoni, D. The cerebellum may implement the appropriate coupling of sensory inputs and motor responses: evidence from vestibular physiology. Cerebellum 4, 178–188 (2005).
Bolbecker, A. R. et al. Exploration of cerebellar-dependent associative learning in schizophrenia: effects of varying and shifting interstimulus interval on eyeblink conditioning. Behav. Neurosci. 125, 687–698 (2011).
Carroll, C. A., O’Donnell, B. F., Shekhar, A. & Hetrick, W. P. Timing dysfunctions in schizophrenia as measured by a repetitive finger tapping task. Brain Cogn. 71, 345–353 (2009).
Moussa-Tooks, A. B. et al. Impaired effective connectivity during a cerebellar-mediated sensorimotor synchronization task in schizophrenia. Schizophr. Bull. 45, 531–541 (2019).
Rasser, P. E. et al. Cerebellar grey matter deficits in first-episode schizophrenia mapped using cortical pattern matching. Neuroimage 53, 1175–1180 (2010).
Bernard, J. A. & Mittal, V. A. Dysfunctional activation of the cerebellum in schizophrenia: a functional neuroimaging meta-analysis. Clin. Psychol. Sci. 3, 545–566 (2015).
Voineskos, A. N. et al. Functional magnetic resonance imaging in schizophrenia: current evidence, methodological advances, limitations and future directions. World Psychiatry 23, 26–51 (2024).
Moussa-Tooks, A. B. et al. Isolation of distinct networks driving action and cognition in psychomotor processes. Biol. Psychiatry 96, 390–400 (2024).
Andreasen, N. C., Paradiso, S. & O’Leary, D. S. “Cognitive dysmetria” as an integrative theory of schizophrenia: a dysfunction in cortical-subcortical-cerebellar circuitry? Schizophr. Bull. 24, 203–218 (1998).
Moberget, T. & Ivry, R. B. Prediction, psychosis, and the cerebellum. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 4, 820–831 (2019).
Konczak, J. et al. Proprioception and motor control in Parkinson’s disease. J. Mot. Behav. 41, 543–552 (2009).
Mittal, V. A. et al. Striatal volumes and dyskinetic movements in youth at high-risk for psychosis. Schizophr. Res 123, 68–70 (2010).
Morton, S. M. & Bastian, A. J. Cerebellar control of balance and locomotion. Neuroscientist 10, 247–259 (2004).
Dijkstra, B. W. et al. Functional neuroimaging of human postural control: a systematic review with meta-analysis. Neurosci. Biobehav. Rev. 115, 351–362 (2020).
Chen, F. C. et al. Postural control of anteroposterior and mediolateral sway in children with probable developmental coordination disorder. Pediatr. Phys. Ther. 27, 328–335 (2015).
Walther, S. Psychomotor symptoms of schizophrenia map on the cerebral motor circuit. Psychiatry Res. 233, 293–298 (2015).
Walther, S. et al. Resting-state hyperperfusion of the supplementary motor area in catatonia. Schizophr. Bull. 43, 972–981 (2017).
Ding, Y. et al. Cerebellar structural and functional abnormalities in first-episode and drug-naive patients with schizophrenia: a meta-analysis. Psychiatry Res. Neuroimaging 283, 24–33 (2019).
Luna, L. P. et al. A systematic review and meta-analysis of structural and functional brain alterations in individuals with genetic and clinical high-risk for psychosis and bipolar disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry 117, 110540 (2022).
Kindler, J. et al. Increased striatal and reduced prefrontal cerebral blood flow in clinical high risk for psychosis. Schizophr. Bull. 44, 182–192 (2018).
Viher, P. V. et al. Altered diffusion in motor white matter tracts in psychosis patients with catatonia. Schizophr. Res. 220, 210–217 (2020).
Bottmer, C. et al. Reduced cerebellar volume and neurological soft signs in first-episode schizophrenia. Psychiatry Res. 140, 239–250 (2005).
Moussa-Tooks, A. B. et al. Cerebellar structure and cognitive ability in psychosis. Biol. Psychiatry 92, 385–395 (2022).
Woodward, N. D. & Heckers, S. Mapping thalamocortical functional connectivity in chronic and early stages of psychotic disorders. Biol. Psychiatry 79, 1016–1025 (2016).
Ferri, J. et al. Resting-state thalamic dysconnectivity in schizophrenia and relationships with symptoms. Psychol. Med. 48, 2492–2499 (2018).
Cao, H. et al. Cerebello-thalamo-cortical hyperconnectivity as a state-independent functional neural signature for psychosis prediction and characterization. Nat. Commun. 9, 3836 (2018).
Zhuo, C. et al. Altered resting-state functional connectivity of the cerebellum in schizophrenia. Brain Imaging Behav. 12, 383–389 (2018).
Bernard, J. A., Goen, J. R. M. & Maldonado, T. A case for motor network contributions to schizophrenia symptoms: evidence from resting-state connectivity. Hum. Brain Mapp. 38, 4535–4545 (2017).
Bernard, J. A., Orr, J. M. & Mittal, V. A. Cerebello-thalamo-cortical networks predict positive symptom progression in individuals at ultra-high risk for psychosis. Neuroimage Clin. 14, 622–628 (2017).
Milev, P., Ho, B. C., Arndt, S. & Andreasen, N. C. Predictive values of neurocognition and negative symptoms on functional outcome in schizophrenia: a longitudinal first-episode study with 7-year follow-up. Am. J. Psychiatry 162, 495–506 (2005).
Gao, J. et al. Aberrant cerebellar neural activity and cerebro-cerebellar functional connectivity involving executive dysfunction in schizophrenia with primary negative symptoms. Brain Imaging Behav. 14, 869–880 (2020).
Basavaraju, R. et al. Intermittent theta burst stimulation of cerebellar vermis enhances fronto-cerebellar resting state functional connectivity in schizophrenia with predominant negative symptoms: a randomized controlled trial. Schizophr. Res. 238, 108–120 (2021).
Vanes, L. D. et al. Neural correlates of positive and negative symptoms through the illness course: an fMRI study in early psychosis and chronic schizophrenia. Sci. Rep. 9, 14444 (2019).
Heinrichs, D. W. & Buchanan, R. W. Significance and meaning of neurological signs in schizophrenia. Am. J. Psychiatry 145, 11–18 (1988).
Peralta, V. et al. Neuromotor dysfunction as a major outcome domain of psychotic disorders: a 21-year follow-up study. Schizophr. Res. 263, 229–236 (2024).
Rathod, B. et al. Neurological soft signs and brain abnormalities in schizophrenia: a literature review. Cureus 12, e11050 (2020).
Bostan, A. C. & Strick, P. L. The cerebellum and basal ganglia are interconnected. Neuropsychol. Rev. 20, 261–270 (2010).
Bostan, A. C. & Strick, P. L. The basal ganglia and the cerebellum: nodes in an integrated network. Nat. Rev. Neurosci. 19, 338–350 (2018).
Mittal, V. A., Bernard, J. A. & Northoff, G. What can different motor circuits tell us about psychosis? An RDoC perspective. Schizophr. Bull. 43, 949–955 (2017).
Mittal, V. A. et al. Neurological soft signs predict abnormal cerebellar-thalamic tract development and negative symptoms in adolescents at high risk for psychosis: a longitudinal perspective. Schizophr. Bull. 40, 1204–1215 (2014).
Hirjak, D., Kubera, K. M., Thomann, P. A. & Wolf, R. C. Motor dysfunction as an intermediate phenotype across schizophrenia and other psychotic disorders: progress and perspectives. Schizophr. Res. 200, 26–34 (2018).
Fujino, H. & Imura, O. Postural sway and clinical characteristics in patients with psychotic disorders: a review. Psychiatr. Q. 86, 603–614 (2015).
Acknowledgements
We would like to thank all the participants of the study and the clinical personnel of the wards for their help and support. This study was funded by the Swiss National Science Foundation (grant 182469 to SW) and intramural funding from SW.
Author information
Authors and Affiliations
Contributions
A.S. and M.G.N. performed the analyses and wrote the first draft of the paper. H.K. and R.K. set up postural assessments. M.G.N., N.N., and F.W. performed postural assessment. M.G.N. and N.N. recruited patients and acquired data. F.W. and A.K. performed clinical assessments. S.L. and J.B. supervised data analysis and manuscript writing. S.W. acquired funding, wrote the protocol, and supervised data acquisition, data analysis, and paper writing. All authors edited and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
Prof. Sebastian Walther reported having received honoraria from Lundbeck, Mepha, and Neurolite. The remaining authors declare no competing interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nuoffer, M.G., Schindel, A., Lefebvre, S. et al. Psychomotor slowing in schizophrenia is associated with aberrant postural control. Schizophr 10, 118 (2024). https://doi.org/10.1038/s41537-024-00534-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-024-00534-5