Abstract
Schizophrenia (SCZ) is a severe psychotic disorder characterized by a disruption in glutamatergic NMDA receptor (NMDAR)-mediated neurotransmission. Compelling evidence has revealed that NMDAR activation is not limited to L-glutamate, L-aspartate, and glycine since other free amino acids (AAs) in the atypical D-configuration, such as D-aspartate and D-serine, also modulate this class of glutamatergic receptors. Although dysregulation of AAs modulating NMDARs has been previously reported in SCZ, it remains unclear whether distinct variations of these biomolecules occur during illness progression from at-risk premorbid to clinically manifest stage. To probe this issue, we used High-Performance Liquid Chromatography (HPLC) to measure serum levels of D- and L-AAs that stimulate NMDARs across four groups of individuals diagnosed with (a) At-Risk Mental State (ARMS) for psychosis, (b) First Episode of Psychosis (FEP), (c) full-blown SCZ and (d) Healthy Donors (HD). We examined how diagnosis, demographic features, and antipsychotic treatment influence the variation of AA levels throughout psychosis progression. Finally, we explored the potential association between AA blood concentrations and clinical and cognitive measures related to psychosis. Our findings identified inter-group differences in serum AA composition, highlighting that the upregulation of D-serine/total serine and D-aspartate/total aspartate ratios represent a peculiar blood biochemical signature of early stages of psychosis progression, while increased L-glutamate, L-aspartate and glycine associate with chronic SCZ diagnosis. The present findings provide direct evidence for early dysregulation of D-AA metabolism and have potential implications for the identification of biomarkers for the early detection and staging of psychosis.
Similar content being viewed by others
Introduction
Schizophrenia (SCZ) is a severe psychotic disorder affecting about 20 million people worldwide1, significantly impacting patients’ quality of life. The symptoms of this illness include positive (delusion and hallucination) and negative (blunted affect, social withdrawal) symptoms, along with cognitive deficits2,3.
Compelling studies have indicated the involvement of an NMDA glutamate receptor (NMDAR) hypofunction in the pathophysiology of SCZ4. Accordingly, genetics studies have ascertained that variations in single genes associated with glutamatergic neurotransmission are related to phenotypes of SCZ5,6, and a recent Genome-Wide Association Study (GWAS) on SCZ7 has found that variants associated with this illness mainly occur in genes modulating NMDAR structure, expression and signaling.
Besides the endogenous agonists, L-glutamate (L-Glu) and L-aspartate (L-Asp), and the co-agonist glycine (Gly), two atypical amino acids in D-configuration, D-aspartate (D-Asp) and D-serine (D-Ser), modulate glutamatergic NMDAR neurotransmission. D-Ser binds to the co-agonist glycine site on GluN1, while D-Asp binds to the agonist glutamate site on GluN2 subunit of NMDARs8,9,10. In addition, D-Asp has been shown to stimulate metabotropic Glu5 receptors (mGluR5) in neonatal rat brain slices, thus extending its functional role to metabotropic receptor signaling during early postnatal life11.
Consistent with a critical role of NMDAR signaling dysfunction in SCZ, multiple studies have reported abnormally lower levels of D-Ser or D-Ser/total Ser ratio in cerebrospinal fluid (CSF) and serum12,13,14,15,16,17,18,19,20,21,22,23 of patients. Moreover, reduced D-Asp levels or a low D-Asp/total Asp ratio have been reported in the serum and post-mortem prefrontal cortex of patients with SCZ24,25,26,27. Specifically, the variation of D-Asp levels in SCZ brain has been associated with increased gene expression24 or abnormal overactivity of the D-aspartate-oxidase (DDO) enzyme, which degrades D-Asp25. Similarly, genes encoding D-amino acid oxidase (DAO), which degrades D-Ser, as well as the DAO activator (DAOA)/G72 have been associated with SCZ28,29. Finally, a variant of the gene encoding serine racemase (SR), which synthesizes D-Ser from L-Ser, has shown significant associations with SCZ in genome-wide studies30.
Consistent with these biochemical and genetic findings highlighting a prominent role of D-Ser metabolism in SCZ pathophysiology, clinical trials indicated that D-Ser add-on to antipsychotics (APs) can improve negative symptoms31,32 and deficits in auditory learning associated with SCZ33. In keeping with this, the NMDAR partial agonist at the GluN1 site, D-cycloserine, has demonstrated benefits for negative and cognitive symptoms34 of SCZ when used alongside APs35. Furthermore, AP add-on with sodium benzoate, a D-Ser catabolism inhibitor, showed beneficial effects in SCZ36,37.
Further indicating a remarkable influence of the GluN1 subunit of NMDARs in the pathophysiology of this mental illness, changes in Gly metabolism have been found in patients at their First Episode of Psychosis (FEP)38 and with full-blown SCZ39. Additionally, as reported for D-Ser, clinical investigations indicated the use of Gly as an adjunctive treatment to ameliorate SCZ cognitive deficits40.
Analogous results have been documented for asparagine (Asn), whose plasma levels were reported to be increased in FEP patients compared to healthy controls and remained high after starting AP treatment41. Similarly, Gln/Glu ratio was found to be increased in CSF of FEP patients42 and plasma of individuals with recent onset SCZ43, and reduced in FEP patients after AP treatment beginning41.
Altogether, this evidence highlights the potential impact of AAs acting at NMDAR as a putative determinant for the development of early psychosis and its progression toward SCZ. However, it remains obscure whether specific AA variation occurs as the illness progresses from at-risk premorbid to clinically manifest stages.
To clarify this issue, by using High-Performance Liquid Chromatography (HPLC), we measured the blood levels of L- and D-Asp, L- and D-Ser, L-Glu, L-Gln, Gly, L-Asn, along with the L-Gln/L-Glu, D-Ser/total Ser and D-Asp/total Asp ratios in a cohort of 73 subjects in an early stage of disease44, including 48 At-Risk Mental State (ARMS) and 25 FEP individuals, 82 patients with full-blown SCZ and 115 Healthy Donors (HD). Furthermore, we investigated the association of serum AA levels and psychosis symptom severity and performance of Working Memory (WM), a prototypical measure of cognitive impairment in psychosis45.
Materials and methods
Sample demographic and clinical characteristics
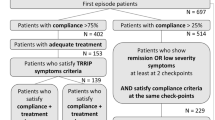
A total of 270 individuals entered the study and were classified as Healthy Donors (HD, n = 115, 43%), At-Risk Mental State (ARMS, n = 48, 18%), First Episode Psychosis (FEP, n = 25, 9%) and affected by schizophrenia (SCZ, n = 82, 30%). Demographic and clinical characteristics of participants are reported in Table 1. Subject enrollment was carried out at the Psychiatric Unit of the “Azienda Ospedaliera Universitaria Consorziale Policlinico di Bari”, Bari - Italy. Recruitment procedures were carried out in accordance with “The Code of Ethics of the World Medical Association” (Declaration of Helsinki) and Good Clinical Practice and approval was given by the local Ethics Committee (Comitato Etico Locale IRCSS Istituto Oncologico “Gabriella Serio”, Bari - Italy). All participants signed a written informed consent to participate after receiving a comprehensive explanation of the study procedures.
Diagnosis of SCZ was made using the Structured Clinical Interview for the DSM IV-TR (SCID)46, which was administered by psychiatrists. Individuals were identified as FEP when they met criteria for DSM-IV-TR affective or non-affective psychotic episode fulfilled within the past 3 months, and when onset of psychosis happened within the past 24 months. FEP were excluded when they underwent AP medication for more than 90 cumulative days.
The ARMS state was defined by: (i) cognitive disturbances (COGDIS), as assessed by the Schizophrenia Proneness Instrument (SPI-A)47, and/or (ii) ultra-high-risk (UHR) criteria for psychosis, according to the Structured Interview for Psychosis-Risk Syndromes criteria48. ARMS were excluded when they had an intake of AP medication for more than 30 cumulative days, and when they had any intake of AP medication within the past 3 months before the study entrance44. In order to allow for inter-individual comparison, doses of AP medication assumed were standardized to olanzapine equivalents according to the methodology indicated in Leucht et al. 49,50.
Clinical symptom severity in ARMS, FEP and SCZ individuals was assessed with the Positive and Negative Syndrome Scale (PANSS)51. Healthy individuals underwent the non-patient version of the SCID52 in order to exclude the presence of any psychiatric disorder.
ARMS, FEP, SCZ and HD individuals underwent Working Memory (WM) behavioral assessment with the N-Back task as described elsewhere53.
All individuals had no history of drug or alcohol abuse within the last 6 months, head trauma with loss of consciousness, or any other clinically significant medical condition.
Human serum collection and preparation
All participants underwent a 10-ml whole blood withdrawal for subsequent serum isolation.
Blood samples, collected in anticoagulant-free tubes, were left at room temperature for about 60 min to allow for coagulation. Samples were then centrifuged at 1900 × g at 4 °C for 10 min. The upper phase containing the serum was transferred to a new tube and centrifuged again to remove any debris. Finally, serum was transferred to a new tube and stored at −80 °C until HPLC analysis.
HPLC analysis of amino acid content
Serum samples (100 µl) were mixed in a 1:10 dilution with HPLC-grade methanol (900 µl) and centrifuged at 13,000 × g for 10 min; supernatants were dried and then suspended in 100 µl of 0.2 M Trichloroacetic acid (TCA). TCA supernatants were then neutralized with 0.2 M NaOH and subjected to precolumn derivatization with o-phthaldialdehyde/N-acetyl-L-cysteine in 50% methanol. AA derivatives were resolved on a UHPLC Nexera X3 system (Shimadzu) by using a Shim-pack GIST C18 3-μm reversed-phase column (Shimadzu, 4.0 × 150 mm) under isocratic conditions (0.1 M sodium acetate buffer, pH 6.2, 1% tetrahydrofuran, and 1 ml/min flow rate). A washing step in 0.1 M sodium acetate buffer, 3% tetrahydrofuran and 47% acetonitrile, was performed after every run. Identification and quantification of AAs were based on retention times and peak areas, compared with those associated with internal standards (Fig. 1). The identity of the D-Asp peak was further evaluated by selective degradation catalyzed by a recombinant human D-aspartate oxidase (hDDO) enzyme54. hDDO enzyme (12.5 μg) was added to the samples, incubated at 30 °C for 3 h, and subsequently derivatized. The detected AA concentrations were expressed as µM, while the ratio between D-AA and total AA (D/D + L) was expressed as a percentage (%).
HPLC chromatogram illustrating the D-aspartate (D-Asp), L-aspartate (L-Asp), L-asparagine (L-Asn), L-glutamate (L-Glu), D-serine (D-Ser), L-serine (L-Ser), L-glutamine (L-Gln) and glycine (Gly) peaks obtained from blood serum samples. The identity of the peaks corresponding to D-Asp and D-Ser was verified by adding internal standards to the serum sample (inset, blue line).
Statistical analysis
Statistical analyses were performed using SPSS software v.27 (SPSS Inc., Chicago, IL, USA) and R Language v.4.3.2 (R Foundation for Statistical Computing, Vienna, Austria). Normality distribution was assessed by q–q plot and Shapiro–Wilk test. Quantitative variables were expressed by median and interquartile range (IQR), while qualitative variables by absolute or relative frequency. Associations between variables were estimated by Fisher’s Exact test. Correlation was evaluated by non-parametric Spearman’s rho. Differences between groups were studied by non-parametric Kruskal–Wallis test followed, if statistically significant, by post-hoc tests performed by Mann–Whitney test with Bonferroni’s correction. The effect of confounders was evaluated by ANCOVA on natural log-transformed variables.
Results
Clinical and demographical characteristics
Group sex and age matching revealed sex was not associated with diagnosis (p = 0.447). ARMS and SCZ groups displayed the lowest and highest age, respectively (Kruskal–Wallis, overall p < 0.001). HD were significantly older than ARMS (Bonferroni’s correction with N = 6, p < 0.01 vs all groups) and younger than patients with SCZ (Bonferroni’s correction with N = 6, p < 0.001). No difference in age was evident between HD and FEP (Table 1). Significant differences in age were also observed between ARMS vs FEP and ARMS vs SCZ groups (Table 1). Finally, FEP and SCZ groups were comparable both for age at onset (p = 0.569) and olanzapine dose equivalents (p = 0.813) (Table 1).
Distribution of amino acid levels
Levels of AAs or their D-to-total ratios are reported in Table 2 and in Figs. 2 and 3. All AAs, except L-Gln (p = 0.263) (Fig. 3A) and L-Asn (p = 0.126) (Fig. 3D), displayed significant differences across groups (Kruskal–Wallis, overall p < 0.001). In particular, L-Ser was higher in patients with SCZ than all other groups (Bonferroni’s correction with N = 6, p-value ranging from 0.017 to <0.001; +23% vs HD, +11% vs ARMS, +25% vs FEP, respectively) (Fig. 2A), while D-Ser showed significantly higher levels among ARMS than in both HD (Bonferroni’s correction with N = 6, p = 0.003; +31%) and SCZ (p < 0.001; +36%) groups (Fig. 2B). The D-Ser/total-Ser ratio (Fig. 2C) paralleled D-Ser levels, but with SCZ displaying significantly lower ratios than all other groups (−24% vs HD, −36% vs ARMS, −30% vs FEP, respectively). The use of ratio increased the statistical significance of the diagnosis effect probably due to the higher L-Ser, hence total Ser, levels among patients with SCZ compared to other groups (Fig. 2A–C).
Distribution of amino acids (L-serine, A; D-serine, B; L-aspartate, D; D-aspartate, E) or their ratio (D-serine/total serine, C; D-aspartate/total aspartate, F) among the groups investigated. Overall and post-hoc comparisons were performed, respectively, by non-parametric Kruskal–Wallis test and Mann–Whitney test with Bonferroni’s correction (N = 6). Only significant p-values are reported. HD Healthy Donors, ARMS At Risk Mental State, FEP First Episode Psychosis, SCZ Schizophrenia.
Distribution of amino acids (L-glutamine, A; L-glutamate, B; L-asparagine, D; Glycine, E) or their ratio (L-glutamine/L-glutamate, C) among the groups investigated. Overall and post-hoc comparisons were performed, respectively, by non-parametric Kruskal–Wallis test and Mann–Whitney test with Bonferroni’s correction (N = 6). Only significant p-values are reported. To improve the visual appearance of Gly, two extreme values (1 for HD and 1 for ARMS, close to 2000 μM) were omitted. HD Healthy Donors, ARMS At Risk Mental State, FEP First Episode Psychosis, SCZ Schizophrenia.
A similar trend was observed for L-Asp, D-Asp and D-Asp/total-Asp ratio (Table 2 and Fig. 2D–F). In particular, similarly to L-Ser, L-Asp was significantly higher in patients with SCZ than all other groups (Bonferroni’s correction with N = 6, p-values ranging from 0.015 to <0.001; +66% vs HD, +108% vs ARMS, +58% vs FEP) (Fig. 2D), while D-Asp was significantly higher among ARMS (+61% vs HD, +45% vs SCZ) and FEP (+83% vs HD, +65% vs SCZ) than HD or SCZ (Fig. 2E). In line with results on single AAs, ARMS and FEP displayed the highest D-Asp/total-Asp ratio (Bonferroni’s correction with N = 6, p < 0.001 vs both HD and SCZ; ARMS, +98% vs HD, +212% vs SCZ, respectively; FEP, +108% vs HD, +228% vs SCZ, respectively) (Fig. 2F). While L-Gln concentrations were not significantly different among groups (Fig. 3A), level of L-Glu was significantly higher in patients with SCZ (Bonferroni’s correction with N = 6, p < 0.001; +213% vs HD, +288% vs ARMS, +189% vs FEP) (Fig. 3B). Thereby, conversely, the L-Gln/L-Glu ratio was significantly lower among SCZ patients than in all other groups (Bonferroni’s correction with N = 6, p < 0.001; −69% vs HD, −73% vs ARMS, −63% vs FEP, respectively) (Fig. 3C).
Similarly, Gly was significantly higher in patients with SCZ (Bonferroni’s correction with N = 6, p-value ranging from <0.001 to 0.006; +28% vs HD, +23% vs ARMS, +32% vs FEP, respectively) (Fig. 3E), while no difference was observed in L-Asn distribution (Fig. 3D). All differences in AA levels (except L-Asn and L-Gln) remained statistically significant after using ANCOVA on natural log-transformed variables to control for the confounding effect of age.
We then performed a comparison analysis of AA levels between male and female individuals within each clinical group. In HD patients, we found significantly higher L-Gln (p < 0.001) and L-Glu levels (p < 0.001), and a lower L-Gln/L-Glu ratio (p < 0.001) in males, compared to females (Table 3A). In ARMS individuals, L-Glu was significantly higher in males than in females (p = 0.029) (Table 3B). No sex-dependent AA level alterations were found in FEP patients (Table 3C). Finally, in patients with SCZ, L-Ser and Gly levels were significantly higher in females compared with males (borderline p = 0.051 and p = 0.014, respectively) (Table 3D).
After, we analyzed the correlation between AA levels and age. In HD individuals, AA levels were not associated with age (Table 3A).
Within the ARMS group, age was positively correlated with L-Glu (rho=0.284, p = 0.053) and negatively correlated with D-Ser (rho = −0.429, p = 0.003), L-Gln/L-Glu ratio (rho = −0.290, p = 0.048) and Gly (rho = −0.307, p = 0.036) (Table 3B).
Among FEP subjects, age was positively correlated with levels of D-Asp (rho = 0.582, p = 0.002) and L-Glu (rho = 0.634, p = 0.001) (Table 3C). Furthermore, similarly to ARMS group, a negative correlation between age and L-Gln/L-Glu ratio (rho = −0.631, p = 0.001) was observed in the FEP group (Table 3C).
Similarly to what observed in the ARMS and FEP groups, in patients with SCZ, age was positively correlated with both D-Asp (rho = 0.256, p = 0.020) and L-Glu (rho = 0.255, p = 0.021) serum levels (Table 3D). Additionally, among patients with SCZ, age positively correlated with D-Ser (rho = 0.223, p = 0.044) (Table 3D).
Finally, in both FEP and SCZ patients, no association was detected between AA levels and olanzapine equivalents (Table 3C and D).
Association between serum amino acid levels, clinical severity and working memory performance
In ARMS and SCZ patients, correlation analyzes revealed that AA levels were not correlated with PANSS scores (Table S1). However, in the FEP group, a moderate positive correlation between PANSS Positive subscale scores and D-Asp levels (rho = 0.677, p = 0.004) was observed (Table S1).
Among HD, serum levels of L-Gln were positively correlated with accuracy as the correct response percentage at the 1-Back task (rho = 0.223, p = 0.026) and negatively correlated with reaction time at the 2-Back task (rho = −0.214, p = 0.033). Among ARMS, levels of D-Ser/total Ser ratio were negatively correlated with the 1-Back reaction time (rho = −0.383, p = 0.019), while levels of L-Glu positively correlated with 1-Back accuracy (rho = −0.334, p = 0.044). Among FEP, no association was found between AA levels and the N-Back scores (Table S2).
Among patients with SCZ, none of the AA levels correlated with the N-Back scores (Table S2).
Discussion
Different lines of research indicate that the modulation of NMDAR is implicated in the early stages of psychosis and chronic SCZ4 and that various neuroactive AAs modulating this class of ionotropic receptors, including Glu, Gly, D-Asp and D-Ser, play a role in psychosis evolution. Here, we explored the hypothesis that distinct changes in the circulating levels of NMDAR-regulating AAs track psychosis phases and impact related symptoms and cognitive deficits.
To test this hypothesis, we compared serum levels of different D- and L-AAs, as well as D-Ser/total Ser and D-Asp/total Asp ratios, among four groups of individuals diagnosed with ARMS, FEP, SCZ and HD. Moreover, we performed an exploratory analysis to investigate the relationship between AA serum profile, psychotic symptom severity and WM performance, assessed with the PANSS and the N-Back task, respectively.
Remarkably, our HPLC results highlight a significant increase in serum D-Asp and D-Ser levels in ARMS compared to HD individuals, indicating an abnormal upregulation of these atypical AAs in the pre-morbid stage of psychosis, and a specific D-Asp increase in FEP compared to both HD and SCZ subjects. Importantly, we found that both D-Ser/total Ser and D-Asp/total Asp ratios significantly increased in ARMS and FEP compared to SCZ and HD individuals, suggesting that such upregulation may be due to higher D-Ser and D-Asp blood levels in these early psychosis stages.
Our data also indicate that the blood levels of L-Ser were prominently upregulated in SCZ compared to HD, ARMS and FEP individuals, suggesting that D-Ser/total Ser ratio reduction was due to an altered Ser enantiomers conversion in SCZ patients. The present finding on L-Ser serum accumulation nicely aligns with previous studies performed on smaller-size samples of patients with SCZ12.
Given the critical importance of SR, DAO, its activator DAOA/G72, and DDO in regulating Ser and Asp L-to-D-enantiomer balance, our findings most likely involve changes in the expression or activity of these enzymes across the progression of psychosis. In line with this assumption, SR has been identified in GWAS as a risk gene for SCZ30 and the SCZ-associated allelic variant has been shown to reduce SR expression55. Accordingly, a previous study has posited the involvement of an SR activity reduction in serum L-to-D-Ser imbalance in patients with SCZ compared to healthy individuals12. Hence, the D-Ser/total Ser ratio decrease observed in SCZ may reflect a reduction of SR-mediated L-to-D-Ser conversion.
Furthermore, a very recent investigation by Camporesi and colleagues confirmed that patients with SCZ, classified as clinically limited-responders and resistant to treatments, exhibit reduced serum levels of SR, while showing a disrupted relationship between D-Ser serum levels and cognitive performance, compared to healthy individuals56. However, since SR activity is counteracted by that of DAO, we cannot rule out that increased DAO-mediated D-Ser degradation may contribute to serum L-Ser accumulation, ultimately resulting in a lower D-Ser/total Ser ratio in SCZ57.
Consistent with our biochemical observations, genetic investigation by Mossner and coll58. reported a DAOA/G72 haplotype associated with susceptibility for progression from prodromal syndromes to First Episode Psychosis. Moreover, Addington and coll59. found that polymorphisms in the 13q33.2 region of G72/G30 genes were associated with childhood-onset SCZ.
Noteworthy, we should consider that luminal-membrane transporters and DAO activity in the intestine and kidney also regulate plasma Ser enantiomer homeostasis60,61, suggesting that these physiological processes may contribute to present observations.
In line with reports implicating NMDAR-mediated glutamatergic alteration in transition from early to full-blown psychosis62,63, and considering the ability of D-Ser and D-Asp to efficiently cross the blood-brain barrier64,65 one possible explanation for our observations is that changes in peripheral metabolism of NMDAR‐related AAs reflect, to some extent, a compensatory response of the organism to an incipient glutamatergic signaling impairment in early stage of disease.
Previous publications suggest that exposure to NMDAR antagonists triggers neuroinflammation responses, resulting in psychosis-related brain structural changes66. Accordingly, increased plasma concentrations of the inflammatory mediator interleukin 6 have been reported in ARMS and AP naïve FEP individuals67, while a potential anti-inflammatory action of NMDAR-stimulating AAs was described68,69,70. This evidence suggests that the increased serum D-Ser and D-Asp levels we observed in ARMS and FEP individuals may be a biological correlate of psychosis onset via modulation of the pro-vs-anti-inflammatory balance. Consistent with our hypothesis, preclinical studies also showed that NMDAR co-agonists D-Ser- and Gly-transport inhibitors can reverse brain changes typically associated with the onset of psychosis71.
Besides D-AAs, our results also confirmed previous findings indicating SCZ-related variation of excitatory L-AA homeostasis13,14,15,17,18,19,21,27, as we found increased serum levels of L-Glu and L-Asp in full-blown SCZ patients who were undergoing treatment, compared to individuals with ARMS, FEP patients and HD individuals. As a result of increased L-Glu levels, we found a reduced L-Gln-to-L-Glu ratio in patients with full-blown SCZ, compared with both HD and ARMS/FEP individuals. In addition, our data aligns with a previous study that showed a decreased Gln/Glu ratio in patients with SCZ compared to healthy subjects43.
Given the relevance of these excitatory AAs in regulating neurotransmission at central glutamatergic synapse, future research is essential to determine whether the reported peripheral changes in the L-Gln/L-Glu ratio also reflect variations in SCZ brains, as previously observed in patients with autism and healthy volunteers72,73.
Here, we also highlighted greater serum levels of the NMDAR co-agonist Gly in patients with SCZ, compared to HD, ARMS and FEP individuals. Even though modifications in brain Gly-mediated NMDAR signaling can occur early in the psychosis spectrum39,74,75, our results indicate that Gly dysmetabolism may become peripherally relevant only after SCZ clinical full onset.
Despite the exploratory nature of our clinical investigation, we discovered that D- and L-AA serum levels were quite weakly correlated with psychosis symptom severity and WM performance.
In particular, limited to FEP individuals, serum levels of D-Asp showed a relatively moderate correlation with the PANSS Positive subscale scores. Conversely, no significant association was observed between serum neuroactive AA levels and WM measures in the same group of individuals. In the ARMS subsample, D-Ser/total Ser ratio was inversely correlated with reaction time on the 1-Back task while L-Glu levels positively correlated with this clinical parameter. Finally, in HD individuals, serum levels of L-Gln were positively correlated with accuracy on the 1-Back task and negatively correlated with reaction time on the 2-Back task.
Overall, our HPLC results revealed distinct variations in circulating AAs acting on NMDAR signaling in specific phases of psychosis that do not fully reflect more distal clinical and behavioral phenotypes, possibly due to a non-linear relationship between metabolic changes involving the body periphery and brain molecular events that eventually lead to psychosis onset. In this perspective, the positive correlation between D-Asp serum levels and PANSS Positive subscale scores in FEP but not ARMS individuals may suggest that D-Asp serum increase, while already detectable in psychosis at-risk-mental-states, becomes clinically relevant only after psychosis clinical onset.
Interestingly, such an increase is no longer observable in full-blown SCZ, where D-Asp levels return to be unrelated to PANSS scores.
Concerning the relationship between AA serum levels and WM performance, our observation of a coherent correlation between L-Gln levels and performance in both 1- and 2-Back tasks in the HD group confirms previous reports about the physiological role of Gln homeostasis in cognition76.
Nonetheless, we found that correlations between AA serum levels and N-Back task performance in pre-morbid and clinical subsamples were relatively limited or completely absent, possibly indicating that peripheral AA modifications may only moderately reflect behavioral alterations.
We are aware that a confounding factor limiting the interpretation of our results is that AA variations are most likely affected by nutrition and biochemical processes involving peripheral organ metabolism, while psychosis itself is a complex brain-routed phenomenon. However, from a system-biology perspective, considering the emerging role of continuous brain-body-microbiota crosstalk77, it is plausible that the neuroactive AA serum changes identified are related to CNS-body-periphery molecular interaction supporting the pathophysiology of psychosis. Within this perspective, future research should take into account system-level variables potentially impacting peripheral neuroactive AA metabolism, including kidney and liver function, gut microbiota composition and dietary factors. In this regard, the timing of the last meal before blood sampling on blood AA levels should be considered of critical relevance78,79,80,81.
A major strength point of our study is that we ran an inclusive HPLC analysis on main NMDAR-modulating D- and L-AAs and their precursors in over 250 individuals, therefore presenting the first large-scale serum AA profiling in psychosis staging. From this perspective, our findings offer an important contribution to the future identification of biomarkers for the early detection and staging of psychosis.
Data availability
Experimental and/or clinical data analyzed in this study is available from the corresponding author upon reasonable request.
References
James, S. L. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1789–1858 (2018).
McCutcheon, R. A., Keefe, R. S. E. & McGuire, P. K. Cognitive impairment in schizophrenia: aetiology, pathophysiology, and treatment. Mol. Psychiatry 28, 1902–1918 (2023).
Bertolino, A. et al. Functional variants of the dopamine receptor D2 gene modulate prefronto-striatal phenotypes in schizophrenia. Brain 132, 417–425 (2009).
Coyle, J. T., Ruzicka, W. B. & Balu, D. T. Fifty years of research on schizophrenia: the ascendance of the glutamatergic synapse. Am. J. Psychiatry 177, 1119–1128 (2020).
Pergola, G. et al. DRD2 co-expression network and a related polygenic index predict imaging, behavioral and clinical phenotypes linked to schizophrenia. Transl. Psychiatry 7, e1006–e1006 (2017).
Rampino, A. et al. Association of functional genetic variation in PP2A with prefrontal working memory processing. Behav. Brain Res. 316, 125–130 (2017).
Trubetskoy, V. et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature 604, 502–508 (2022).
Souza, I. N. D. O., Roychaudhuri, R., De Belleroche, J. & Mothet, J.-P. d-Amino acids: new clinical pathways for brain diseases. Trends Mol. Med. 29, 1014–1028 (2023).
Coyle, J. T., Balu, D. & Wolosker, H. d-Serine, the shape-shifting NMDA receptor co-agonist. Neurochem. Res. 45, 1344–1353 (2020).
Errico, F., Cuomo, M., Canu, N., Caputo, V. & Usiello, A. New insights on the influence of free d-aspartate metabolism in the mammalian brain during prenatal and postnatal life. Biochim. Biophys. Acta BBA - Proteins Proteom. 1868, 140471 (2020).
Molinaro, G. et al. d-Aspartate activates mGlu receptors coupled to polyphosphoinositide hydrolysis in neonate rat brain slices. Neurosci. Lett. 478, 128–130 (2010).
Hashimoto, K. et al. Decreased serum levels of D-serine in patients with schizophrenia: evidence in support of the N -Methyl- D -aspartate receptor hypofunction hypothesis of schizophrenia. Arch. Gen. Psychiatry 60, 572 (2003).
Hashimoto, K. et al. Reduced d-serine to total serine ratio in the cerebrospinal fluid of drug naive schizophrenic patients. Prog. Neuropsychopharmacol. Biol. Psychiatry 29, 767–769 (2005).
Cho, S.-E., Na, K.-S., Cho, S.-J. & Kang, S. G. Low d-serine levels in schizophrenia: a systematic review and meta-analysis. Neurosci. Lett. 634, 42–51 (2016).
Hons, J. et al. Impairment of executive functions associated with lower D-serine serum levels in patients with schizophrenia. Front. Psychiatry 12, 514579 (2021).
Yamada, K. et al. Identification of multiple serine racemase (SRR) mRNA isoforms and genetic analyses of SRR and DAO in schizophrenia and D-serine levels. Biol. Psychiatry 57, 1493–1503 (2005).
Calcia, M. A. et al. Plasma levels of D-serine in Brazilian individuals with schizophrenia. Schizophr. Res. 142, 83–87 (2012).
Yamamori, H. et al. Changes in plasma d-serine, l-serine, and glycine levels in treatment-resistant schizophrenia before and after clozapine treatment. Neurosci. Lett. 582, 93–98 (2014).
Bendikov, I. et al. A CSF and postmortem brain study of d-serine metabolic parameters in schizophrenia. Schizophr. Res. 90, 41–51 (2007).
Fuchs, S. A. et al. Cerebrospinal fluid d-serine and glycine concentrations are unaltered and unaffected by olanzapine therapy in male schizophrenic patients. Eur. Neuropsychopharmacol. 18, 333–338 (2008).
Fukushima, T. et al. Quantitative analyses of schizophrenia-associated metabolites in serum: serum D-lactate levels are negatively correlated with gamma-glutamylcysteine in medicated schizophrenia patients. PLoS ONE 9, e101652 (2014).
Liu, R. et al. Correlation of functional GRIN2A gene promoter polymorphisms with schizophrenia and serum d-serine levels. Gene 568, 25–30 (2015).
Hashimoto, A. et al. The presence of free D‐serine in rat brain. FEBS Lett. 296, 33–36 (1992).
Errico, F. et al. Decreased levels of d-aspartate and NMDA in the prefrontal cortex and striatum of patients with schizophrenia. J. Psychiatr. Res. 47, 1432–1437 (2013).
Nuzzo, T. et al. Decreased free d-aspartate levels are linked to enhanced d-aspartate oxidase activity in the dorsolateral prefrontal cortex of schizophrenia patients. Npj Schizophr. 3, 16 (2017).
De Rosa, A. et al. Machine learning algorithm unveils glutamatergic alterations in the post-mortem schizophrenia brain. Schizophrenia 8, 8 (2022).
Garofalo, M. et al. Decreased free D-aspartate levels in the blood serum of patients with schizophrenia. Front. Psychiatry 15, 1408175 (2024).
Schumacher, J. et al. Examination of G72 and D-amino-acid oxidase as genetic risk factors for schizophrenia and bipolar affective disorder. Mol. Psychiatry 9, 203–207 (2004).
Chumakov, I. et al. Genetic and physiological data implicating the new human gene G72 and the gene for d -amino acid oxidase in schizophrenia. Proc. Natl. Acad. Sci. 99, 13675–13680 (2002).
Schizophrenia Working Group of the Psychiatric Genomics Consortium. Biological insights from 108 schizophrenia-associated genetic loci. Nature 511, 421–427 (2014).
Hashimoto, K., Malchow, B., Falkai, P. & Schmitt, A. Glutamate modulators as potential therapeutic drugs in schizophrenia and affective disorders. Eur. Arch. Psychiatry Clin. Neurosci. 263, 367–377 (2013).
Durrant, A. R. & Heresco-Levy, U. D-serine in neuropsychiatric disorders: new advances. Adv. Psychiatry 2014, 1–16 (2014).
Sehatpour, P. et al. Dose-dependent augmentation of neuroplasticity-based auditory learning in schizophrenia: a double-blind, placebo-controlled, randomized, target engagement clinical trial of the NMDA glutamate receptor agonist d-serine. Biol. Psychiatry 94, 164–173 (2023).
Goff, D. The Therapeutic role of d-cycloserine in schizophrenia. Adv. Pharmacol. 76, 39–66 (2016).
Van Berckel, B. D-cycloserine increases positive symptoms in chronic schizophrenic patients when administered in addition to antipsychotics a double-blind, parallel, placebo-controlled study. Neuropsychopharmacology 21, 203–210 (1999).
Lane, H.-Y. et al. Add-on treatment of benzoate for schizophrenia: a randomized, double-blind, placebo-controlled trial of d -Amino acid oxidase inhibitor. JAMA Psychiatry 70, 1267 (2013).
Lin, C.-H. & Lane, H.-Y. Sodium benzoate: a novel multi-target pharmaceutical approach to rescue clozapine-resistant schizophrenia. Schizophr. Res. S0920996423001718 https://doi.org/10.1016/j.schres.2023.05.001 (2023).
Kim, S.-Y. et al. In vivo brain glycine and glutamate concentrations in patients with first-episode psychosis measured by echo time–averaged proton magnetic resonance spectroscopy at 4T. Biol. Psychiatry 83, 484–491 (2018).
Waziri, R., Baruah, S. & Sherman, A. D. Abnormal serine-glycine metabolism in the brains of schizophrenics. Schizophr. Res. 8, 233–243 (1993).
Tsai, G. & Lin, P.-Y. Strategies to enhance N-Methyl-D-Aspartate receptor-mediated neurotransmission in schizophrenia, a critical review and meta-analysis. Curr. Pharm. Des. 16, 522–537 (2010).
Garip, B. & Kayir, H. Alteration in NMDAR‐related amino acids in first episode psychosis. Synapse 73, e22127 (2019).
Hashimoto, K. et al. Elevated glutamine/glutamate ratio in cerebrospinal fluid of first episode and drug naive schizophrenic patients. BMC Psychiatry 5, 6 (2005).
Madeira, C. et al. Blood levels of glutamate and glutamine in recent onset and chronic schizophrenia. Front. Psychiatry 9, 713 (2018).
Antonucci, L. A. et al. Machine learning-based ability to classify psychosis and early stages of disease through parenting and attachment-related variables is associated with social cognition. BMC Psychol. 9, 47 (2021).
Gold, J. M. et al. Working memory impairment across psychotic disorders. Schizophr. Bull. 45, 804–812 (2019).
First, M. B. et al. Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders-research Version. (Biometrics Research, New York, 1996).
Schultze-Lutter, F. et al. Development and evaluation of the schizophrenia proneness instrument, adult version (SPI-A). Schizophr. Res. 86, 4–44 (2006).
Miller, T. J. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr. Bull. 29, 703–715 (2003).
Leucht, S. et al. Dose equivalents for second-generation antipsychotic drugs: the classical mean dose method. Schizophr. Bull. 41, 1397–1402 (2015).
Leucht, S., Samara, M., Heres, S. & Davis, J. M. Dose equivalents for antipsychotic drugs: the DDD method: table 1. Schizophr. Bull. 42, S90–S94 (2016).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
First, M. B. et al. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP) (Biometrics Research, New York, 2002).
Raio, A. et al. Similarities and differences between multivariate patterns of cognitive and socio-cognitive deficits in schizophrenia, bipolar disorder and related risk. Schizophrenia 9, 11 (2023).
Katane, M. et al. Rat d -aspartate oxidase is more similar to the human enzyme than the mouse enzyme. Biochim. Biophys. Acta BBA - Proteins Proteom. 1866, 806–812 (2018).
Birnbaum, R. et al. Serine racemase (SRR) and schizophrenia risk: functional genomic characterization of SCZ GWAS risk SNP rs4523957 by RNA sequencing. American College of Neuropsychopharmacology 2014 (Abstracts).
Camporesi, S. et al. Neurocognition and NMDAR co-agonists pathways in individuals with treatment resistant first-episode psychosis: a 3-year follow-up longitudinal study. Mol. Psychiatry https://doi.org/10.1038/s41380-024-02631-4 (2024).
Kuo, C.-Y., Lin, C.-H. & Lane, H.-Y. Targeting d-Amino Acid Oxidase (DAAO) for the treatment of schizophrenia: rationale and current status of research. CNS Drugs 36, 1143–1153 (2022).
Mössner, R. et al. DAOA/G72 predicts the progression of prodromal syndromes to first episode psychosis. Eur. Arch. Psychiatry Clin. Neurosci. 260, 209–215 (2010).
Addington, A. M. et al. Polymorphisms in the 13q33.2 gene G72/G30 are associated with childhood-onset schizophrenia and psychosis not otherwise specified. Biol. Psychiatry 55, 976–980 (2004).
Taniguchi, K. et al. D-amino acids as a biomarker in schizophrenia. Diseases 10, 9 (2022).
Sasabe, J. et al. Ischemic acute kidney injury perturbs homeostasis of serine enantiomers in the body fluid in mice: early detection of renal dysfunction using the ratio of serine enantiomers. PLoS ONE 9, e86504 (2014).
Schobel, S. A. et al. Differential targeting of the CA1 subfield of the hippocampal formation by schizophrenia and related psychotic disorders. Arch. Gen. Psychiatry 66, 938 (2009).
Schobel, S. A. et al. Imaging patients with psychosis and a mouse model establishes a spreading pattern of hippocampal dysfunction and implicates glutamate as a driver. Neuron 78, 81–93 (2013).
Pernot, P. et al. d-Serine diffusion through the blood–brain barrier: effect on d-serine compartmentalization and storage. Neurochem. Int. 60, 837–845 (2012).
Usiello, A. et al. New evidence on the role of D-aspartate metabolism in regulating brain and endocrine system physiology: from preclinical observations to clinical applications. Int. J. Mol. Sci. 21, 8718 (2020).
Behrens, M. M. & Sejnowski, T. J. Does schizophrenia arise from oxidative dysregulation of parvalbumin-interneurons in the developing cortex? Neuropharmacology 57, 193–200 (2009).
Upthegrove, R., Manzanares-Teson, N. & Barnes, N. M. Cytokine function in medication-naive first episode psychosis: a systematic review and meta-analysis. Schizophr. Res. 155, 101–108 (2014).
Aguayo-Cerón, K. A. et al. Glycine: the smallest anti-inflammatory micronutrient. Int. J. Mol. Sci. 24, 11236 (2023).
Ling, Z.-N. et al. Amino acid metabolism in health and disease. Signal Transduct. Target. Ther. 8, 345 (2023).
Goudarzvand, M. et al. Hydroxycitric acid ameliorates inflammation and oxidative stress in mouse models of multiple sclerosis. Neural Regen. Res. 11, 1610 (2016).
Gozzi, A. et al. Pharmacological stimulation of NMDA receptors via co-agonist site suppresses fMRI response to phencyclidine in the rat. Psychopharmacology 201, 273–284 (2008).
Alfredsson, G., Wiesel, F.-A. & Tylec, A. Relationships between glutamate and monoamine metabolites in cerebrospinal fluid and serum in healthy volunteers. Biol. Psychiatry 23, 689–697 (1988).
Hassan, T. H. et al. Blood and brain glutamate levels in children with autistic disorder. Res. Autism Spectr. Disord. 7, 541–548 (2013).
Woods, S. W. et al. Glycine treatment of the risk syndrome for psychosis: Report of two pilot studies. Eur. Neuropsychopharmacol. 23, 931–940 (2013).
Javitt, D. C. Glycine transport inhibitors in the treatment of schizophrenia. In Novel Antischizophrenia Treatments, vol. 213 (eds. Geyer, M. A. & Gross, G.) 367–399 (Springer Berlin Heidelberg, Berlin, Heidelberg, 2012).
Baek, J. H. et al. The role of glutamine homeostasis in emotional and cognitive functions. Int. J. Mol. Sci. 25, 1302 (2024).
Li, J., Xiang, H. & Xiong, J. Editorial: current trends in the crosstalk between nervous systems and other body systems. Front. Mol. Neurosci. 16, 1157672 (2023).
Sjøberg, K., Schmoll, D., Piper, M., Kiens, B. & Rose, A. Effects of short-term dietary protein restriction on blood amino acid levels in young men. Nutrients 12, 2195 (2020).
Schmidt, J. A. et al. Plasma concentrations and intakes of amino acids in male meat-eaters, fish-eaters, vegetarians and vegans: a cross-sectional analysis in the EPIC-oxford cohort. Eur. J. Clin. Nutr. 70, 306–312 (2016).
Holeček, M. Side effects of amino acid supplements. Physiol. Res. 29–45 https://doi.org/10.33549/physiolres.934790 (2022).
Genchi, G. An overview on d-amino acids. Amino Acids 49, 1521–1533 (2017).
Acknowledgements
We are grateful to Prof Hiroshi Homma and Prof Masumi Katane for the generous gift of an aliquot of the DDO recombinant enzyme and thank Prof Uriel Heresco Levy for the valuable discussion. We would also like to thank Rosa Barca, Riccarda Lomuscio, and Milena Tartarelli (Department of Translational Biomedicine and Neuroscience, UNIBA) for their administrative support. A.B. was in part funded by The Apulian regional government for the project: “Early Identification of Psychosis Risk”. M.F. and S.S. were funded by the Italian Ministry of Economic Development (MISE) for the project #F/200044/01-03/X45-CUP: B98I20000100005. A.B., A.U., and F.E. have been past recipients of grants from the Brain and Behavior Research Foundation (2013 NARSAD Independent Investigator Grant, no. 20353 to A.B. and A.U., and 2015 NARSAD Young Investigator Grant, no. 23968 to F.E.). A.U. and T.N. were supported by #NEXTGENERATIONEU (NGEU) funded by the Ministry of University and Research (MUR), National Recovery and Resilience Plan (NRRP), project MNESYS (PE0000006) – A Multiscale integrated approach to the study of the nervous system in health and disease (DN. 1553 11.10.2022). AU and FE were supported by the Italian Ministry of Universities and Research (Ministero dell’Università e della Ricerca, MUR) through PRIN 2017 - Project nr 2017M42834 and PRIN PNRR 2022, financed by the European Union – Next Generation EU - Project nr P2022ZEMZF.
Author information
Authors and Affiliations
Contributions
A.R. and A.U. contributed to the design of the study. A.R., M.G., A.B., M.F., S.S., R.M., M.G.A., and T.C.P. contributed to the acquisition of the data. A.R., A.U., M.V., D.B., D.A., F.E., and T.N. provided the analysis and interpretation of the data for the work. A.R. did the primary drafting of the manuscript. A.U. did interpretation of the study and revised the work critically for important intellectual content. All authors approved the final version to be published and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
A.R. received travel fees by Lundbeck. AB received consulting fees by Biogen and lecture fees by Otsuka, Janssen, Lundbeck. All other authors have no biomedical financial interests and no potential conflicts of interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rampino, A., Garofalo, M., Nuzzo, T. et al. Variations of blood D-serine and D-aspartate homeostasis track psychosis stages. Schizophr 10, 115 (2024). https://doi.org/10.1038/s41537-024-00537-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-024-00537-2
This article is cited by
-
Aspartate in the Brain: A Review
Neurochemical Research (2025)
-
Multi-omics Analysis of Energy Metabolism Pathways Across Major Psychiatric Disorders
Molecular Neurobiology (2025)