Abstract
Carbohydrate-based therapeutic vaccines are actively pursued as targeted immunotherapy to treat cancer. Aberrant glycosylation is indeed of paramount importance in tumors, leading to the formation of “neo-epitopes”, known as tumor-associated carbohydrate antigens (TACAs), crucial in cancer onset, development and spread. Accordingly, the over-simplified mucin-type O-glycans Tn and STn have been confirmed among the most promising candidates for the development of cancer vaccines. In this work, we first propose genetically manipulated bacteria outer membrane vesicles (OMVs), namely GMMA, as a vaccine formulation platform to display glycan antigens. GMMA were glycosylated with multiple copies of structurally locked Tn mimetic or STn mimetic as cancer vaccine prototypes. These constructs, in non-adjuvanted formulations, showed sounding immunogenic properties in vivo and impressive efficacy in a mouse model of aggressive triple-negative breast cancer. This example of tailor-made therapeutic vaccine might revolutionize the approach to cancer therapy.

Similar content being viewed by others
Introduction
Aberrant glycosylation is of utmost importance in tumors, in that it plays a crucial role in cancer onset, development, and invasion. Several mechanistic pathways can trigger aberrant glycosylation of glycoproteins, glycolipids, or glycosphingolipids, leading to the formation of “neo-epitopes”, known as tumor-associated carbohydrate antigens (TACAs). By interacting with glycan-binding receptors of antigen-presenting cells (APCs, such as MGL, DC-SIGN, or SIGLECs), TACAs are endowed with immunostimulant properties1. For this reason, and thanks to the undoubted success of immunotherapy in oncology, TACA-based strategies to improve antitumor immune responses became a flourishing research field2,3. Nonetheless, the development of therapeutic cancer vaccines based on TACAs remains challenging, mostly because of: (i) the limited number of TACAs identified on cancer cells but absent or poorly expressed on normal cells, (ii) the difficulties in selecting carriers to properly display TACAs to the host’s immune system, and (iii) the paucity of adjuvants which break immune tolerance without inducing hard side effects. In addition, the underestimated patients’ specificity of cancer cell mutations heavily contributed to the failures recorded for vaccines clinically tested4,5.
Among the best-studied TACAs, there are the over-simplified mucin-type O-glycans Tn (Thomsen-neaveau), TF (Thomsen-Friedenreich), and STn (sialyl Tn) (Fig. 1).
Structurally, the Tn antigen is a N-acetylgalactosamine alpha O-linked, through a residue of serine (Ser) or threonine (Thr), to mucins’ (particularly mucin 1 and 4) peptide backbone. Under physiological conditions, the Tn antigen is elongated by specific glycosyl transferases to generate complex oligosaccharides. Conversely, upon malignant transformations, oligosaccharides’ oversimplification takes place along with the abnormal display of the Tn monosaccharide and of the TF and STn disaccharides, as hallmarks of mucins’ tumoral transformations. The high density of Tn found on cancer cells is also significantly associated with tumor progression and patients’ poor prognosis.
It is worthy of noting that the Tn antigen is largely conserved in many adenocarcinomas (90% in breast cancer, 70–90% in colon, lung, ovary, and stomach cancer) and often co-expressed with STn; both Tn and STn are almost absent on normal cells6,7. In 2009 the National Cancer Institute (NCI) prioritized mucin 1 (MUC1) antigens for the development of cancer vaccines8.
In spite of the simple chemical structure, the immunological definition and role in tumor progression of the Tn antigen are utmost complicated and far from fully understood9,10,11. Yet, in the last 15 years, investigations carried out to design antibodies targeting the Tn antigen provided insights useful for the rational design of therapeutic vaccines12,13,14,15. As a matter of fact, it is currently known that multiple copies of the Tn antigen are required to induce an effective anti-Tn immune response16 and that the aminoacidic residue (Ser vs. Thr) bridging the GalNAc moiety to the MUC1 peptide, seems to affect the monosaccharide conformational behavior, modulating the immune properties of the glycotope. Indeed, the GalNAc-Thr less flexible than the GalNAc-Ser, is better recognized by various GalNAc-binding lectins17,18. Alongside, to reduce the intrinsic poor immunogenicity of TACAs and break immune tolerance, Tn has also structurally been modified to obtain non-self analogs or mimetics, more immunogenic and more stable in vivo19,20,21,22.
In the design of cancer vaccines, it is mandatory taking into consideration that carbohydrates are T-independent antigens, therefore, Tn-based vaccines have traditionally been conceived as conjugate to carrier proteins to help foster a cell-mediated response3. As an excellent alternative to protein carriers, outer-membrane vesicles (OMVs) have been the object of fruitful use in antibacterial vaccines23,24. OMVs are nanoscale spherical vesicles, released by Gram-negative bacteria, featuring self-adjuvating properties due to the presence of pathogen-associated molecular patterns (PAMPs). Thanks to the optimal size for immune stimulation and display of multiple copies of the antigen of interest, OMVs are ideal as antigen carriers. Furthermore, PAMPs can elicit potent Th1-skewed immune responses without the need for additional adjuvants25,26. Moreover, since OMVs tend to accumulate in the tumor microenvironment27,28, they may be used for the development of tumor-targeting therapy. Interestingly, genetically modified OMVs displaying distinct peptidic tumor antigens have already been tested in preclinical studies as cancer vaccines to elicit anti-tumor immune responses with positive results29,30.
Some years ago, we developed a mimetic of GalNAcα-O-Thr, namely Tn mimetic (Fig. 1), featuring a tricyclic constrained structure that preserves the native Tn α-O-glycosidic linkage but lacking the NH acetyl residue on the C-2 of the galactopyranose31. The cyclic amide portion of the Tn mimetic mimics the first amino acid of the MUC1 determinant. The Tn mimetic is stable to galactosidases and retains the 4C1 chair conformation of the native antigen which accounts for the binding properties toward galactose-specific lectins32. A multivalent presentation of the Tn mimetic was efficiently obtained by glycosylating a fully synthetic cyclopeptide scaffold33, or the carrier protein CRM19720. CRM197 is one of the most effective carrier proteins34, licensed to treat bacterial infections35. CRM197 glycosylated with four residues of Tn mimetic elicited a robust immune response in triple-negative breast cancer (TNBC) animal model20.
Capitalizing on the promising immunostimulant properties of the Tn mimetic20,36,37,38, and taking into account the expression of Tn and STn antigens in many aggressive adenocarcinomas and mucus carcinomas39,40, a few years ago we reported on the synthesis of a STn mimetic (Fig. 1)41. Tn and STn mimetics are attractive determinants to develop a multi-antigens cancer vaccine, to mimicking the heterogenicity of cancer cells.
In this context, herein we first propose genetically manipulated bacteria OMVs, namely generalized modules for membrane antigens (GMMA)42, glycosylated with multiple copies of Tn mimetic or STn mimetic, as cancer vaccine prototypes.
GMMA are OMVs derived from Gram-negative bacteria engineered to provide an over-vesiculating phenotype. GMMA currently constitutes a straightforward technology based on low-cost production and high purification yields. Recent clinical trials showed good immunogenicity data and confirmed that GMMA is well tolerated43,44. Therefore, GMMA is an ideal platform to display glycan antigens for the design of safe and affordable vaccines42,45. Hence, semi-synthetic constructs were assembled by conjugating Tn derivative 1 or STn derivative 2 (Scheme 1) to GMMA and screened in vivo for their immunogenic properties and efficacy in a mouse model of highly aggressive TNBC.
Results
Synthesis of GMMA glycosylated with derivative 1 (GMMA-Tn) or derivative 2 (GMMA-STn)
Offering the possibility to direct antigens’ conjugation either to the lipopolysaccharides or to the proteins exposed on their surface43, GMMAs are captivating platforms to display glycan antigens. Therefore, taking advantage of the carboxylic group, the Tn and STn mimetics (see Fig. 1) were suitably functionalized to react with the lysine residues exposed on the surface of GMMAs produced from a hyper-vesiculating E. coli strain46. In detail, the carboxylic residue of the triacetyl derivative 320 was reacted with the amino derivative 4 to form, under standard conditions (HOBt, EDAC, NMM in DMF as solvent and at room temperature), the amide 5 in high yield (90%). After the removal of acetyl protecting groups (NH3, 4 M in CH3OH) and reduction of the azido residue (Pd/C, H2, THF/H2O, room temperature) the compound 6 so obtained was reacted with bis-N-hydroxysuccinimide hexanoic acid and NMM in DMF as solvent, affording after purification by chromatography on silica gel, compound 1 (51%) ready to be reacted with GMMA (Scheme 1). Following the same synthetic procedure, derivative 2 was smoothly prepared (see Supplementary for details).
By using reported conditions47, derivatives 1 or 2 were mixed with GMMA in phosphate buffer and at room temperature to afford respectively GMMA-Tn (GMMA displaying multiple copies of Tn mimetic) or GMMA-STn (GMMA displaying multiple copies of STn mimetic) glycoconjugates, respectively (see Supplementary for details).
HPLC-SEC analysis of each conjugate revealed the absence of free mimetic after purification by ultrafiltration and revealed its presence in the permeate collected during the purification step (Fig. 2A). The increased absorbance at 214 nm of the two conjugates compared to starting GMMA, when analyzed at same total protein concentration, suggested the occurred conjugation of mimetics on GMMA surface (Fig. 2A). SDS–PAGE analysis confirmed conjugates formation by showing a different protein profile with respect to GMMA alone (Fig. 2B). Analysis by DLS indicated that the integrity of GMMA was maintained (Fig. 2C). Since the complex heterogenicity of GMMA outer membrane prevented MALDI analysis, TNBS (trinitrobenzene sulfonate) assay was performed to estimate the percentage of lysine residues involved in the conjugation: the amount of linked 1 or 2 corresponded to 38% and 26%, respectively, with the consequently mimetic/protein w/w ratios of 0.33 and 0.34.
Synthesis of CRM197 glycosylated with 16 residues of TnThr mimetic (CRM-Tn)
Thanks to the promising results previously obtained in vivo with CRM197 conjugated with multiple copies of Tn mimetic20, herein, we used glycosylated CRM197 as a positive control. The carrier protein featuring multiple (39 + 1) lysine residues, was thus reacted with an excess of derivative 1, characterized by a terminal carboxylic acid activated as succinimide (see Scheme 1). The conjugation was performed with N-methyl morpholine (NMM) as a base, in DMF as a solvent, overnight at room temperature. According to previous data20, CRM197 decorated with an average of 16 residues of Tn mimetic, namely CRM-Tn, (loading 40%, mimetic/protein w/w = 0.17) was successfully obtained (see Supplementary).
GMMA-Tn and GMMA-STn formulations elicited antigen-specific antibodies in outbred mice
Outbred CD1 mice were immunized with GMMA-Tn, GMMA-STn, and the physical combination of GMMA with Tn mimetic (GMMA+Tn) or STn mimetic (GMMA+STn) (see Fig. 1) (7 μg of Tn mimetic or STn mimetic antigen/dose, two doses given at day 0 and 28, see Supplementary for immunization details). CRM-Tn was also tested as a benchmark control and administered with the same schedule. Immunoglobulin (Ig) production in response to treatments was evaluated at day 27 (post 1, T27) and 42 from baseline (post 2, T42, 14 days after the second dose) by multiplex enzyme-linked assay (ELISA). The total serum concentration of IgGs and IgM present in all groups was not significantly altered during immunization (data not shown). The specific IgG response versus Tn and STn mimetics was then assessed by testing serial dilutions of pooled sera (from 1:100 to 1:24.300) from each experimental group on an ELISA plate coated with Tn mimetic or STn mimetic antigens (by treatment with glycosylated bovine serum albumin (BSA), see Supplementary). As shown in Table 1 specific antibodies were detected against both antigens, in high titers. Notably, at day 27 (post 1), specific antibodies against the two antigens were detected in high titers, especially in groups treated with GMMA-Tn and CRM-Tn. On day 42, after the second immunization (post 2), the groups treated with CRM-Tn, GMMA-Tn, and GMMA-STn contained higher levels of IgG against both antigens. The physical mixtures, GMMA+Tn and GMMA+STn, were globally less effective than the corresponding glycosylated GMMA since they required two immunizations to achieve a comparable level of antibodies. Pre-immune sera, which were also analyzed to evaluate the level of non-specific reactivity, were negative in this assay (data not shown) confirming the absence of any non-specific response.
To assess the homogeneity of serum IgG titers within each experimental group, and better compare the difference between the two carriers, (i.e., GMMA vs. CRM), sera from every single animal immunized with GMMA-Tn and CRM-Tn were screened by ELISA, increasing the number of dilution points (from 1:900 to 1:1.96 × 106) (Fig. 3). As clearly shown, antigen-specific IgG responses elicited by GMMA-Tn were significantly higher than those elicited by CRM-Tn, both after first (post 1) and second injection (post 2). It is worth noting that sera raised by GMMA-Tn also efficiently recognized STn mimetic, though with a more scattered profile (Fig. 3, right panel).
IgGs specific for Tn mimetic (left panel) and STn mimetic (right panel) were measured by ELISA in sera after the first immunization (post 1) and after the second immunization (post 2). BSA conjugated with derivative 16 (see Supplementary) or 2 (see Scheme 1) was used for ELISA plate coating. Data represent geometrical mean titers (GMT) of IgG titer of individual mouse sera ± SD of 3 replicates. Statistical significance was calculated by using the two-way ANOVA Tukey’s multiple comparison test; *P-value < 0.05; ****P-value < 0.0001.
We also investigated the ability of Tn mimetic to produce IgGs able to recognize Tn antigen by ELISA (BSA glycosylated with natural Tn as coating, see Fig. 1 and Supplementary). Of note, IgGs induced by GMMA-Tn showed a higher reactivity for native Tn antigen than those elicited by CRM-Tn (used as positive control) thus confirming the cross-reactivity of sera raised by GMMA-Tn and the potential of GMMA as carrier (Fig. 4).
Individual sera of each immunization group were tested by ELISA plate coated with multiple copies of native Tn antigen conjugated to BSA (see Supplementary). Data are represented as a mean of 3 replicates. Statistical significance was calculated by using the two-way ANOVA Tukey’s multiple comparison test; *P-value < 0.05; ***P-value < 0.001.
Tn- or STn-specific antibodies elicited by glycosylated GMMA bind cancer cells
We then analyzed sera by flow cytometry to assess their ability to bind T47D and MCF7 breast cancer cell lines endogenously expressing Tn and/or STn antigens (dilution 1:100). A first analysis was performed by using pools of sera obtained upon immunization with CRM-Tn (control), GMMA-Tn or GMMA-STn and with the physical mixtures GMMA+Tn and GMMA+STn. Data showed that sera pools from all groups bound to the surface of both cell lines, with a higher efficiency for the Tn-containing formulations (Fig. 5A), highlighting that the immunization induces antibodies that can specifically recognize native Tn or STn on the surface of human tumor cells. The flow cytometry analysis was then repeated by assessing the binding homogeneity of individual sera of CRM-Tn or GMMA-Tn groups to T47D and MCF7 cell lines. Sera elicited by GMMA-Tn immunization did bind specifically to the surface of T47D and MCF7 cells reaching higher median fluorescence values (MFI) than the CRM-Tn group, confirming the contribution of GMMA to the immunogenicity of Tn antigen (Fig. 5B).
A and B T47D and MCF7 cell lines were grown to subconfluence, collected, and stained using pools of sera of each mice group (pool of n = 8 mice per experimental group) collected at T42 (A) or of individual sera (B) (1:100 serum dilution). Detection was done using an Alexa Fluor-647-conjugated anti-mouse IgG secondary antibody. Controls (dashed lines) included sera from mice immunized with raw GMMA carrier and Mouse IgG Isotype Control-APC. The results were expressed as the median fluorescence intensity (MFI) values ± standard error (SE). C Flow cytometry analysis of T47D cells using pooled sera from GMMA-Tn immunization depleted or not of GMMA antisera (1:100 dilution). Each experimental group consists of a pool of n = 8 mice. Data are represented as MFI values of sera from immunized mice subtracted by MFI value of pre-immune pooled sera value ± standard error (SE). D Flow cytometry analysis of T47D cells using pooled sera from GMMA-Tn immunization depleted or not of GMMA antisera and pre-incubated with 20 μg/ml of Tn mimetic or native Tn (pool of n = 8 mice per experimental group). The graph reports the fold change of MFI values normalized on sera without competition with Tn ± standard error (SE). Statistical significance was calculated by using the Mann–Whitney test and two-way ANOVA; *P-value < 0.05; ***P-value < 0.001. All experiments were conducted in triplicate.
Since good binding was also seen for pool sera from GMMA mixed to Tn or STn, we used a pool of sera against GMMA carrier alone to set the positivity threshold and to single out the specific contribution of anti-Tn antibodies to cancer cells’ binding. Most anti-GMMA-Tn sera showed higher MFI values than anti-GMMA sera on cells expressing Tn and/or STn antigen, with frequencies of 7/8 (87.5%) and 6/8 (75%) on T47D and MCF7, respectively (Fig. 5B). To further demonstrate that the observed binding was ascribed to specific recognition of the Tn antigen present on the surface of T47D tumor cells, the pool of sera of the GMMA-Tn group was first depleted of antibodies against the GMMA carrier (by absorption on GMMA-coated plates) and then used in competitive flow cytometry assay with synthetic Tn mimetic or native Tn. As expected, removal of anti-GMMA antibodies reduced the cell binding (by about 40%) (Fig. 5C), but competition with Tn mimetic or native Tn further reduced the cell binding (Fig. 5D). These results clearly indicate that: (a) antibodies elicited against Tn mimetic can recognize Tn and STn displayed on the surface of cancer cells, (b) after depletion of anti-GMMA response, Tn-specific antibodies are clearly detectable in GMMA-Tn immunization sera, and (c) the competition with native Tn or Tn mimetic reduced the binding of CRM-Tn and GMMA-Tn serum groups (Fig. 5D), confirming that both CRM-Tn and GMMA-Tn formulations elicit Tn-specific antibodies.
Prophylactic vaccination with GMMA-Tn or GMMA-STn inhibits tumor growth in a murine orthotopic breast cancer model
Based on the evidence that treatments with Tn or STn mimetics conjugated to GMMA as carrierinduced high antigen-specific IgGs in the outbred CD1 mouse strain, we planned to evaluate the protective activity of this response to prevent tumor onset in a murine syngeneic orthotopic tumor model of TNBC, using BALB/c mice. Briefly, 56 five-week-old female BALB/c mice were divided into 6 groups (8 mice/group) and initially treated with two doses (at T0 and T28, 7 μg/dose of antigen/s) of: GMMA carrier (group 1), GMMA+Tn mimetic (group 2), GMMA-Tn (group 3), GMMA+STn mimetic (group 4), GMMA-STn (group 5) and CRM-Tn (group 6) respectively. The immunization schedule was the same as used in CD1 mice (see Supplementary).
We first assessed IgG response versus Tn mimetic and STn mimetic in BALB/c mice. Pools of sera collected at T27 (post 1) and T35 (post 2) from each experimental group were screened by ELISA (serum dilution from 1:100 to 1:24000) to measure the specific IgG1, IgG2a, and IgG2b response against Tn mimetic (Table S1). At post 1, specific antibodies against Tn mimetic were detected in high titers particularly in mice immunized with GMMA-Tn and GMMA-STn for all the three IgG subtypes analyzed. In general, at post 2, Ig titers remained sustained or further increased. Concerning the CRM-Tn formulation, at post 1 it preferentially elicited a specific IgG1 response, while IgG2a and IgG2b titers were induced by the second immunization, though reaching lower titers than the other groups (Table S1).
We then investigated the protective immunity of prophylactic vaccination with GMMA-Tn or GMMA-STn in a Tn-expressing mouse TNBC model. To this aim, groups 1, 3, and 5 received additional 4 doses of, respectively, GMMA, GMMA-Tn, or GMMA-STn, administered weekly, corresponding to a total of six immunizations before tumor engraftment (Fig. 6A). No adverse effects48 occurred throughout the experimental session (e.g. local inflammation, systemic reactions, weight loss or death of treated mice), indicating good tolerability of the GMMA-based formulations (data not shown).
A Schematic representation of the immunization schedule used to test efficacy in BALB/c mice. Mice received six repeated immunizations with raw GMMA or GMMA-Tn or GMMA-STn formulation, as indicated. Blood samples were collected at baseline (pre-immune) and at the indicated timepoints for serological analysis. B Antibody titers elicited in BALB/c mice sera after 6 immunizations with GMMA-Tn and GMMA-STn (post 6), as assessed by measuring Tn-specific IgG1, IgG2a, IgG2b subclasses. Data are represented as mean ± SD of 3 replicates. C Flow cytometry analysis of 4T1-Luc cells stained with pooled sera from GMMA, GMMA-Tn, or GMMA-STn immunization. The cells were stained with 1:100 dilution of sera, followed by an Alexa Fluor-647-conjugated anti-mouse IgG secondary antibody. Data are represented as fold change versus pre-immune pooled serum value and were expressed as the mean ± standard error (SE). D Concentration of the indicated cytokines in post 6 serum samples (four pools of two sera each per group) treated with GMMA-Tn or GMMA-STn. Panel A was created with BioRender®.
Mice of the selected groups (groups 1, 3, and 5) were then inoculated with murine 4T1-Luc2 mammary carcinoma tumor cells into the mammary fat pad of the third pair of mammary glands. The efficacy of immunotherapy was evaluated weekly (W) by assessing tumor growth over a period of 28 days (4 W). In the first 21 days (W1, W2, W3), tumor growth was monitored by using bioluminescence imaging (BLI), while at day 28 (W4) tumor volumes were measured manually by caliper, to avoid possible BLI artefactual measurements caused by tissue necrosis in such a prolonged observation time. One week after the last immunization (post 6, T70, Fig. 6B) and at the endpoint (post 6 + 5 W, Table S2), serum samples were collected to evaluate the specific IgG subclass response anti-Tn mimetic by ELISA.
In general, Tn-specific IgG1/IgG2a/IgG2b titers at post 6 were sustained or further boosted by the repeated immunizations, maintaining the same relative profile observed at post 2 (Fig. 6B and Table S1). Notably, IgGs were still well detectable at post 6 + 5 W, with IgG1 titers having the highest persistence (Table S2). Individual sera at post 6 were also successfully tested for their ability to bind to Tn or STn antigens on the surface of 4T1-Luc2 cell lines by flow cytometry (Fig. 6C).
In addition, to assess the elicitation of a cellular immune response, in post-6 serum samples, we also measured a panel of Th1/Th2 cytokines and soluble receptors. Compared to the GMMA group, mice immunized with GMMA-Tn showed a specific activation/effector profile, based on a higher production of GM-CSF, IL-2, IFNγ, IFNβ, Granzyme B, IL-6, with moderate increase of IFNα, IL-1β, and TNFα. The higher concentration of these mediators in the GMMA-Tn was also paralleled by a higher level of the immune checkpoint PD-L1. Mice immunized with GMMA-STn mirrored a similar activation profile, though at a lower level than the GMMA-Tn group (Fig. 6D).
The ability of the elicited immune responses to inhibit tumor growth was repeatedly assessed weekly for three weeks after tumor cell implantation (by estimating tumor size with BLI). The inhibition of tumor growth was measured relative to the GMMA group (Figs. 7A and S4). Results showed that in all mice immunized with GMMA-Tn (group 3) and GMMA-STn (group 5) tumor growth was significantly impaired compared to mice immunized with raw GMMA (group 1) (Fig. 7B, left panel). A moderate capability of raw GMMA to control tumor growth was observed as previously described30. By day 21, animals treated with GMMA-Tn and GMMA-STn showed a significant reduction (p < 0.05) of the bioluminescence signal of 4T1Luc2 cells, as compared to control mice treated with raw GMMA, retaining only 10% residual bioluminescence (Fig. 7B, right panel). The significant tumor growth inhibition was maintained at day 28, as assessed by tumor volume manual measurement (Fig. 7C). The immune cells (both lymphoid and myeloid cell populations) infiltrating 4T1-Luc2 mammary tumor sections from mice treated for 4 weeks (28-day post-implantation, Fig. 6A) with raw GMMA or GMMA-Tn or GMMA-STn formulations, were investigated by immunofluorescence analyses, by using antibodies directed against CD3 (T lymphocytes), CD11c (myeloid cells, highly expressed in dendritic cells), F4-80 (macrophages), and CD19 (B lymphocytes) (Fig. 7D). These markers allowed to investigate the role of GMMA-Tn or GMMA-STn triggering antigen-specific immune cells that infiltrate the tumor lesions.
Two weeks after the last immunization mice were engrafted with 4T-1-Luc2 cells and tumor growth was monitored weekly using bioluminescence imaging (BLI) over a period of 21 days (W1, W2, W3) and using caliper at day 28 (W4). Analysis of bioluminescence intensity (A, B). A Representative images of bioluminescence intensity related to the mammary carcinoma tumor mass in mice immunized with raw GMMA or GMMA-Tn or GMMA-STn, at 3 weeks after inoculation with 4T1-Luc2 cells. Tumor growth monitoring (B and C). B Tumor growth monitoring by BLI analysis was collected weekly for 3 weeks after implantation of 4T1-Luc2 cells in individual mice immunized with the indicated formulations. Decrease in BLI intensity of photons over time demonstrated tumor growth inhibition. Left panel: BLI analysis of total photons flux of individual mice. Right panel: reduction of BLI signal in mice immunized with GMMA-Tn or GMMA-STn relative to the GMMA control. C Tumor growth measurement at W4 after tumor implantation by calliper measurement. The tumor volumes were determined by two-dimensional measurement with a manual caliper at day 28 post-tumor inoculation. Tumor volumes were calculated according to the formula: Tumor volume=(l × w²)×0.5 where l = largest diameter and w = width (perpendicular diameter) of the tumor (in mm). D Immunofluorescence (IF) staining of formalin-fixed, paraffin-embedded (FFPE) tumor tissue sections from transplanted mice immunized for 4 weeks with raw GMMA or GMMA-Tn or GMMA-STn. Images show a selected field of view at ×20 magnification. The specific primary antibodies used to visualize the different populations of the tumor infiltrate are: anti-CD3 for T lymphocytes, anti-CD11c for dendritic cells, anti-F4-80 for macrophages, and anti-CD19 for B lymphocytes. Alexa Fluor 647-labeled anti-rabbit secondary antibody was used to detect all primary antibodies (red). DAPI was used for the visualization of cell nuclei locations (blue). Scale bar = 100 μm. The graph shows the percentage of positive cells counted in the fluorescence staining using ImageJ software. The percentages were calculated from the count of positive cells for a specific marker related to the total nuclei for each section. E and F Pearson correlation correlogram of efficacy and immunological parameters in BALB/c mice immunized with GMMA-Tn and GMMA-STn. The correlogram shows the correlation among tumor inhibition values based on BLI data at W3, titers of immunoglobulin subsets, and selected serum cytokines elicited at post 6 by vaccination with GMMA-Tn (E), and GMMA-STn (F). The strength of the correlation between two variables is represented by the color of the square at the intersection of those variables; color range from bright blue (strong positive correlation, i.e. r2 = 1.0) to bright red (strong negative correlation, i.e. r2 = −1.0).
The data obtained showed increased levels of both T cells and dendritic cells in GMMA-Tn or GMMA-STn-treated mice compared with carrier alone, with greater evidence in GMMA-STn-treated mice. This suggests that the vaccines are able to modulate the recruitment of both antigen-presenting cells and T cells in the tumor microenvironment of the treated mice. Interestingly, macrophage infiltration increased in treated mice compared with the carrier-only control, but with a larger component in GMMA-Tn-treated mice. Interestingly, in sections from mice treated with GMMA-Tn or GMMA-STn, the data show a significant increase in B lymphocytes, which are completely absent in controls (Fig. 7D).
Overall, immunofluorescence staining indicates that GMMA-Tn and GMMA-STn vaccines have different capabilities in modulating the recruitment of T lymphocytes, dendritic cells, and tumor-associated macrophages into the tumor microenvironment.
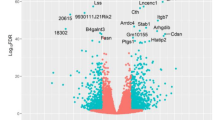
Finally, a correlogram analysis was used to display the correlation among multiple parameters (tumor growth inhibition vs. raw GMMA by BLI analysis at W3, serum cytokines/receptors, and Tn- or STn-specific IgG1, IgG2a and IgG2b at post 6) in the GMMA-Tn and GMMA-STn groups.
Collectively, several positive correlations, particularly evident in the GMMA-Tn, group were observed among efficacy and effector immune response parameters (Fig. 7E, F), strengthening the evidence that GMMA-glycan formulations are able to activate both the cellular and humoral arms of the immune system resulting in a prophylactic anti-tumor efficacy.
Discussion
Therapeutic cancer vaccines and active immunotherapy, exploit patients’ immune systems as a weapon to fight cancer and are considered one of the most deserving “personalized” cancer therapy3. Although at present more than 40 clinical trials are ongoing, the development of clinically validated therapeutic vaccines still is a challenging target.
In the design of successful therapeutic vaccines, one main issue is the selection of the antigen(s) which should be highly tumor-selective and suitably displayed to properly mimic the native antigens’ presentation on tumor cells. In this frame, “tailor-made” synthetic immunogens offer several advantages over native-based constructs, including increased safety, stability, and reliability.
Unprecedently, in this study GMMA vesicles have been selected as a platform for the multivalent presentation of MUC1 Tn and STn antigen mimetics (see Fig. 1), to develop affordable semi-synthetic vaccine prototypes. Tn-mimetic derivative 1 and STn-mimetic derivative 2 have indeed been synthesized (see Scheme 1) and reacted with lysine residues of GMMA to smoothly afford glycosyl vesicles named GMMA-Tn (GMMA glycosylated with multiple copies of Tn mimetic) and GMMA-STn (GMMA glycosylated with multiple copies of STn mimetic). These two different types of glycosylated GMMA, endowed with similar size distribution (see Fig. 2C) and comparable amounts of linked mimetics, were used to immunize CD1 and BALB/c mice. No additional adjuvant was used in the formulations tested as GMMA provides self-adjuvanticity. A relevant humoral immune response against GMMA-Tn or GMMA-STn has been observed in both CD1 and BALB/c mice. In agreement with data reported for bacteria vaccines49,50,51, GMMA used as a carrier and herein glycosylated with Tn mimetic (GMMA-Tn) showed higher immunogenicity compared to conventional carrier protein CRM197 glycosylated with the same mimetic (CRM-Tn) (see Table S1 and S2). The IgG antibody response appeared persistent in mice and the high IgG titers suggested a robust T-cell-dependent immune response that was elicited by our glycosylated GMMA vaccine formulations.
Noteworthy, flow cytometry analysis revealed that elicited antibodies specifically recognize human Tn-positive cancer cells, indicating that they could exert a long-lasting targeting activity involving different mechanisms of action. Indeed, we also showed that antigen-specific IgG1, IgG2a, and IgG2b subtypes arose in mice treated with GMMA-based formulations, indicating a Th1/Th2 immune response. Conversely to “more traditional” carrier-adjuvants (like CRM197), GMMA promoted a shift towards a Th1 response, engaging both Th2 and Th1 immunity.
Different IgG isotypes, with their Fc tail, bind to different Fc receptors (FcRs) on immune cells and can thus induce diverse immune responses. Mouse IgG2a offers superior Fc-dependent activity to mouse IgG1, due to its high affinity for activating FcRs and low affinity for the inhibitory one. Consequently, in mouse cancer models, the tumor-targeting mouse IgG2a is mainly responsible for tumor control by Fc-dependent effector functions, while mouse IgG1 may prevalently act by blocking signaling downstream effects on cancer cells. The situation is reversed for human IgG1, which has a higher affinity for activating FcRs than human IgG2a. Our observation that Tn- and STn mimetic antigens formulated with GMMA elicited different IgG subtypes suggests that the humoral response is potentially multifunctional against cancer cells. Moreover, antibodies can engage the complement system as well as different effector cells such as natural killer (NK) cells and macrophages, thus triggering antibody-dependent cell-mediated cytotoxicity (ADCC), antibody-dependent cell-mediated phagocytosis, and complement-dependent cytotoxicity (CDC) against tumor cells52,53.
The antigen-specific immune response was also paralleled by the elicitation of a higher level of different circulating activation/effector cytokines and soluble immune mediators induced by GMMA-Tn and GMMA-STn, as compared to raw GMMA immunization. Indeed, our efficacy study in a TNBC mouse model showed that prophylactic vaccination with GMMA-Tn or GMMA-STn significantly inhibits tumor growth in treated mice. Furthermore, such tumor inhibition event was associated with the production of antigen-specific antibodies and several cell-mediated immune response parameters elicited by vaccination, suggesting that the antigens mimetics induced a global immune response targeting breast cancer 4T1 cells, efficiently inhibiting tumor establishment and growth.
Finally, our study provides a preliminary indication that the synthetic vaccine formulated with GMMA is well tolerated, provides a consistent immune response, and breaks self-tolerance, a key problem in cancer immunotherapy. In particular, we observed for GMMA-Tn an excellent functionality and ability to induce specific antibodies cross-reactive on Tn as well as STn native antigens. These thrilling properties represent an added value because, in the development of a vaccine, they may be translated into a single component (rather than mixtures) with no need for additional adjuvants. These features represent a significant advantage for manufacturing and regulatory approval processes.
In our study, we used a repeated immunization regimen to provide the proof-of-concept that GMMA-Tn/STn induces an efficacious immune response in a prophylactic breast cancer model. Further research is needed to optimize the vaccination regimen and reduce the number of doses needed to inhibit cancer growth in the perspective of future clinical studies, to confirm the prophylactic efficacy of the GMMA-Tn or GMMA-STn formulations in different cancer preclinical models, and to thoroughly investigate the immunological mechanism(s) underlining the observed tumor-inhibition effect. Yet, the clear reduction of tumoral growth recorded in the prophylactic trial lets us postulate the potential use of the GMMA-Tn and/or GMMA-STn as cutting-edge therapeutic vaccines.
Methods
Production, purification, and characterization of E. coli GMMA
GMMA was produced from a ΔtolR E. coli BL21(DE3) mutant strain, mutated in order to increase the rate of vesicle release through the deletion of tolR gene. Briefly, an overnight Luria-Bertani broth preinoculum was diluted 1:50 in HTMC medium to grow bacteria at 30 °C under shaking (180 rpm). After 8 h, bacteria were pelleted with a 45’ centrifugation to collect the supernatant containing GMMA vesicles. GMMA were then purified through tangential flow filtration (100 kDa Hydrosart membrane, Sartorius), followed by an ultracentrifugation step (50,000 rpm, 1 h, 4 °C), resuspending GMMA pellet in PBS. Purity and integrity of GMMA were verified by HPLC-SEC analysis using TSKgel 6000PW + G4000PW columns in series and by DLS, respectively54.
Synthesis of compound 5
To a solution of compound 3 (252 mg, 0.55 mmol) in DMF (5 mL), HOBt (335 mg, 2.2 mmol), EDAC (420 mg, 2.2 mmol), and NMM (600 µL, 3.3 mmol) were added. The suspension was stirred at rt for 10 min and then linker 3 (260 mg, 0.66 mmol) was added. The mixture was stirred at rt for 2 h until TLC (CH2Cl2:CH3OH = 9:1) showed the disappearance of the starting material. The suspension was diluted with EtOAc (50 mL), washed with citric acid 10% (w/w) (3 × 30 mL), then with NaHCO3 s.s. (1 × 30 mL) and eventually brine (1 × 30 mL). The organic layers were dried over Na2SO4 and concentrated under vacuum to obtain a crude product (426 mg) that was purified by flash column chromatography on silica gel (CH2Cl2:CH3OH = 95:5) to give compound 5 (317 mg, 0.48 mmol, 90% yield) as a white foam. For characterization data see Supplementary.
Synthesis of compound 7
Compound 5 (360 mg, 0.61 mmol) was dissolved in NH3 in CH3OH 4 M (5.5 mL). After stirring for 3 h, the reaction mixture was concentrated under vacuum to give derivative 7 (288 mg, >95% yield) as a light-yellow foam, which was used in the next step without any further purification. For characterization data see Supplementary.
Synthesis of compound 6
To a solution of compound 7 (166 mg, 0.36 mmol) in CH3OH (5 mL) and 5 drops of H2O, Pd/C (80 mg, 0.18 mmol) was added under the N2 atmosphere. The mixture was stirred at rt under H2 atmosphere for 18 h until TLC control (CH2Cl2:CH3OH = 8:2) showed no presence of the starting material. The mixture was filtered through a pad of Celite® and the solvent was evaporated under a vacuum to obtain pure compound 6 (140 mg, >95% yield) as a white foam. For characterization data see Supplementary.
Synthesis of compound 1
To a solution of crude compound 6 (105 mg, 0.24 mmol) and NMM (110 µL, 0.97 mmol) in dry DMF (2 mL), bis-succinimide adipate 8 (330 mg, 0.97 mmol) was added. After stirring the mixture for 16 h at rt the precipitate was discarded, and the solvent was evaporated under vacuum. The residue was suspended in EtOAc and the precipitate was purified by flash chromatography on silica gel (CH2Cl2:CH3OH = 85:15 to 70:30) to give pure compound 1 (55 mg, 40% over 3 steps). For characterization data see Supplementary.
Synthesis of compound 9
To a suspension of 7 (140 mg, 0.3 mmol) in acetone (3 mL), DMP (2 mL, 15 mmol) and pTsOH (until pH 3) were added and the solution was stirred at room temperature for 15 h. After complete conversion, the mixture was quenched with Et3N (pH 8), diluted with CH2Cl2 (50 mL), and washed with HCl 1 M (2 × 25 mL) and water (2 × 25 mL). The organic layer was dried over Na2SO4 and concentrated under a vacuum. The crude was purified by flash chromatography on silica gel (EtOAc:CH3OH = 95:5 to 90:10) to afford compound 9 as a white solid (115 mg, 65% yield). For characterization data see Supplementary.
Synthesis of compound 11
To a suspension compound 9 (454 mg, 0.91 mmol) and 10 (1.92 g, 2.9 mmol) in a mixture of dry CH3CN:CH2Cl2 = 10:1 (v/v, 11 mL) cooled to –40 °C, NIS (1.0 g, 4.55 mmol) and TfOH (140 μL, 2.3 mmol) were added and the solution was stirred at –40 °C under N2 atmosphere. After 2 h, the reaction was quenched with Et3N until pH 8 and the mixture was diluted with CH2Cl2 (100 mL) and washed with Na2S2O3 1 M (4 × 50 mL). The organic layer was dried over Na2SO4 and concentrated under a vacuum to give the crude product. This latter was solubilized in AcOH 80% in H2O (v/v, 10 mL) and the reaction mixture was stirred overnight at 40 °C. The solvent was removed under vacuum and the product was purified by flash chromatography on silica gel (CH2Cl2:CH3OH = 96:4 to 90:10) to give 11 (541 mg, 65% yield calculated over 2 steps). For characterization data see Supplementary.
Synthesis of compound 12
To a solution of compound 11 (345 mg, 0.34 mmol) in EtOH (20 mL) Pd/C (200 mg, 1.0 mmol) was added under the N2 atmosphere. The mixture was stirred at rt under H2 atmosphere for 3 days then the mixture was filtered through a pad of Celite® and the solvent was evaporated under vacuum to obtain crude as a light-brown foam. The crude was dissolved in NH3 4 M in CH3OH (4 mL) and the reaction mixture was stirred at room temperature. After 2 days, the solvent was removed under vacuum and the product was purified by washing several times with Et2O to give pure 12 (170 mg, 70% yield over two steps) as light-brown foam. For characterization data see Supplementary.
Synthesis of compound 2
To a solution of compound 12 (40 mg, 0.06 mmol) in dry DMF (2 mL) and NMM (50 µL, 0.25 mmol), bis-succinimide adipate 8 (75 mg, 0.22 mmol) was added. After stirring the mixture for 16 h at rt the precipitate was filtered off, and the solvent was evaporated in vacuo. The residue was suspended in EtOAc and the precipitate was washed several times with EtOAc to give activated compound 2 (25 mg, 50% yield) as a light-brown foam which was used immediately. For characterization data see Supplementary.
Synthesis of compound 14
To a solution of compound 3 (253 mg, 0.46 mmol) in DMF (8 mL), HOBt (250 mg, 1.84 mmol), EDAC (350 mg, 1.84 mmol), and NMM (300 µL, 2.76 mmol) were added. The suspension was stirred at rt for 10 min and then 13 (228 mg, 0.69 mmol) was added. The mixture was stirred at rt for 1.5 h until TLC (CH2Cl2:CH3OH = 9:1) showed the disappearance of the starting material. The suspension was diluted with EtOAc (100 mL), and washed with H2O (6 × 70 mL). The organic layers were dried over Na2SO4 and concentrated under vacuum to afford pure compound 14 (247 mg, 92% yield) as a light-yellow foam. For characterization data see Supplementary.
Synthesis of compound 15
To a solution of compound 14 (211 mg, 0.36 mmol) in a mixture of THF:H2O = 4:1 (v/v, 10 mL) LiOH.H2O was added (75 mg, 1.8 mmol). The mixture was stirred at rt for 19 h until TLC (CH2Cl2:CH3OH = 8:2) showed the disappearance of the starting material. The mixture was evaporated under reduced pressure to give crude compound 15 (260 mg, >95% yield) as a white foam which was used without any further purification. For characterization data see Supplementary.
Synthesis of compound 16
To a dispersion of compound 15 (73 mg, 0.17 mmol) in dry DMF (5 mL), HBTU (120 mg, 0.32 mmol), and DIPEA (80 µL, 0.45 mmol) were added. The mixture was stirred at rt until dissolution and then NHS (33 mg, 0.29 mmol) was added. The mixture was stirred at rt and monitored via TLC (CH2Cl2:CH3OH = 8:2) for 16 h until the disappearance of the starting material. The dispersion was evaporated under reduced pressure to give crude (270 mg) which was dispersed in acetone. The precipitate was filtered and washed with acetone (3 × 2 mL) to give activated compound 16 (57 mg, 62%) as a light-brown cerous solid which was stored under an N2 atmosphere at −10 °C. For characterization data see Supplementary.
Synthesis of Tn_mime[28]BSA
BSA (19.8 mg, 0.3 µmol) was dissolved in NAPi Phosphonate Buffer (2 mL, 150 mM, pH 7.4) and slowly treated with a solution of 16 (57 mg, 46 µmol) dissolved in dry DMF (150 µL). The mixture was stirred at 4 °C for 24 h, the success of the reaction was proved by an SDS–PAGE, and then the conjugate was centrifuged to remove the brown solid precipitate. The water layer was purified by HPLC-SEC and concentrated to 100 µM. using a 35 kDa MWCO membrane centrifugal device (Millipore). The number of functionalized lysine was confirmed by MALDI/TOF-TOF UltraFlex III analysis: about 28 glycans were linked to BSA (Tn_mime[28]BSA) (see Fig. S1).
Synthesis of STn_mime[8]BSA
BSA (10 mg, 0.15 µmol) was dissolved in NAPi Phosphonate Buffer (2 mL, 150 mM, pH 7.4) and slowly treated with a solution of 2 (25 mg, 26 µmol) dissolved in dry DMF (150 µL). The mixture was stirred at 4 °C for 24 h, the success of the reaction was proved by an SDS-PAGE, then the conjugate was centrifuged to remove the brown solid precipitate. The water layer was purified by HPLC-SEC and concentrated to 100 µM. using a 35 kDa MWCO membrane centrifugal device (Millipore). The number of functionalized lysine was confirmed by MALDI/TOF-TOF UltraFlex III analysis: 8 glycans were linked to BSA (STn_mime[8]BSA) (see Fig. S2).
Synthesis of derivative 18
To a solution of compound 173 (126 mg, 0.27 mmol) in dry DMF (7.5 mL) and NMM (50 µL, 0.25 mmol), bis-succinimide adipate 8 (342 mg, 1.0 mmol) was added. After stirring the mixture for 18 h at rt the precipitate was filtered off, and the solvent was evaporated in vacuo. The residue was suspended in EtOAc and the precipitate was washed several times with EtOAc to give activated compound 18 (93 mg, 50% yield) as a yellowish foam which was used immediately. For characterization data see Supplementary.
Synthesis of native Tn[22]BSA
BSA (20.0 mg, 0.3 µmol) was dissolved in NAPi Phosphonate Buffer (2 mL, 150 mM, pH 7.4) and slowly treated with a solution of derivative 18 (31 mg, 45 µmol) dissolved in dry DMF (150 µL). The mixture was stirred at 4 °C for 24 h, the success of the reaction was proved by an SDS-PAGE, then the conjugate was centrifuged to remove the dark yellow solid precipitate. The water layer was purified by HPLC-SEC and concentrated to 100 µM. using a 35 kDa MWCO membrane centrifugal device (Millipore). The number of functionalized lysine was confirmed by MALDI/TOF-TOF UltraFlex III analysis: about 22 glycans were linked to BSA (Native Tn[22]BSA) (see Fig. S3).
Synthesis and characterization of GMMA conjugates
After concentration of GMMA at ~10 mg/mL in 50 mM phosphate buffer pH 7.2, conjugation of each functionalized mimetic was performed with a GMMA/mimetic w/w ratio of 1:1, keeping reaction mixtures under agitation with a rotating wheel at room temperature overnight. Conjugates were purified through centrifugal ultrafiltration using Amicon Ultra device with a membrane cut-off of 100 kDa (Merck, Darmstadt, Germany), and removal of unconjugated mimetic was verified by HPLC-SEC following absorbance at 214 nm. The purified conjugates were analyzed by SDS–PAGE analysis to verify conjugate formation, as previously described (Vaccines. Vaccines 2020, 8, 540). Total protein recovery was quantified by Micro BCA, and the amount of conjugated mimetic was indirectly estimated by quantifying the remaining free amino groups on GMMA with 2,4,6-trinitrobenzenesulfonic acid (TNBS) assay55. Conjugates’ size distribution was determined by DLS.
Animals
Five-week-old female CD1 and BALB/c mice were purchased from Charles River (Italy). Animals were housed 4 per cage under a light-dark (12 h/12 h) cycle with ad libitum access to water and food. Experimental manipulations were performed under inhalation anesthesia induced by 4% and maintained by a 2.3% mixture of isofluorane in oxygen administered through facial masks. At the end of the study, all animals were anasthetized with gas anesthesia (2.5% isofluorane), to perform final blood collection and then sacrificed by cervical dislocation. Experiments were carried out in compliance with the bioethical principles adopted by Directive 2010/63/EU on the protection of animals used for scientific purposes and Italian Legislative Decree 4 March 2014, no. 26. Implementation of Directive 2010/63/EU on the protection of animals used for scientific purposes. The experimental protocol was approved by the Local Ethical Committee (Toscana Life Sciences Foundation’s Animal Welfare Body) and authorized by the Italian Ministry of Health (authorization nos. 924/2020-PR and 924/2020-PR).
Mice immunizations
For immunogenicity studies, 5-week-old female CD1 (8 mice/group) were subcutaneously immunized with two doses of different antigen formulations, given at 4 weeks intervals (day 0, T0; day 28, T28): (Group 1) GMMA-Tn (7 µg antigen/dose, conjugated to 21.4 µg of GMMA), (Group 2) a combination of GMMA and unconjugated Tn mimetic (21.4 µg GMMA + 7 µg Tn mimetic), (Group 3) GMMA-STn (7 µg antigen/dose conjugated to 20.5 µg GMMA), (Group 4) a combination of GMMA and unconjugated STn mimetic (20.5 µg GMMA + 7 µg STn mimetic), and (Group 5) CRM-Tn (7 µg antigen/dose conjugated to 41.7 µg CRM) used as benchmark control to compare the antibody responses. Sera were collected for immunogenicity analysis at day 27 (T27, post 1) and 42 from baseline (T42, 14 days after the second dose, post 2).
For efficacy studies, 5-week-old female BALB/c mice (8 mice/group) before tumor cells implantation were subcutaneously immunized with 6 doses, with the first and the second given at 4-week-interval (day 0, T0; day 28, T28) and the remaining 4 doses given at 1-week interval (day 36, T36; day 42, T42; day 56, T56; day 63, T63). Mice received the same antigenic formulations used for CD1 immunization; one additional mice group was included and treated with raw GMMA as negative control, in detail: (Group 1) raw GMMA (21.4 µg), (Group 2) a combination of GMMA and unconjugated Tn mimetic, (Group 3) GMMA-Tn, (Group 4) a combination of GMMA and unconjugated STn mimetic, (Group 5) GMMA-STn and (Group 6) CRM-Tn. Sera were collected for immunogenicity analysis before the first immunization (pre-immune), at day 27 (T27, 7 days after the first immunization, post 1) at day 35 (T35, 7 days after the second immunization, post 2), and at day 70 (T70, 7 days after the last immunization, post 6).
Cell lines
Murine 4T1-Luc2, T47D, and MCF7 were purchased from ATTC. Cells were cultured and passaged as recommended by the manufacturers. 4T1-Luc2 is a luciferase-expressing cell line derived from parental line CRL-2539 by transduction with a lentiviral vector encoding firefly luciferase gene (luc2) under the control of EF-1 alpha promoter.
Analysis of antigen-specific antibodies response by ELISA
The antibody response induced by immunizations against the Tn- and STn-mimetics or native Tn antigen, was measured by multiplex Enzyme-Linked Assay (ELISA). 384-well Maxisorp plates (Nunc, Thermo Fisher Scientific) were coated with: Tn mimetic or STn mimetic or native Tn, by adding 10 mL/well of a 5 mg/mL antigen-BSA conjugates’ solution in PBS buffer, followed by incubation overnight at 4 °C. After three washings with PBS buffer containing 0.05% Tween 20 (Sigma) (TPBS), a blocking step was performed by adding 35 mL of BSA solution at 5% in TPBS and incubating the plates for 1 h at 37 °C. After washing as above, up to eight two-fold serial dilutions of pre-immune, in TPBs were then performed along each column, plates were incubated for 1 h at 37 °C and washed 3×. Twenty mL/well of secondary antibody coupled to HRP, appropriately diluted in TPBS (goat anti-mouse IgG, Invitrogen) were added and the plates were incubated for 1 h at 37 °C. After four more washes, 20 mL/well of 3,3´,5,5´-tetramethylbenzidine (TMB) solution was added. After 10 min of incubation at room temperature, plates were read at 450 nm.
Flow cytometry analysis
For binding assays, T47D and 4T1 cells were grown to sub-confluency, harvested using enzyme-free cell dissociation buffer (Gibco), and centrifuged, counted, and resuspended in MACS buffer (Miltenyi Biotec) at a concentration of 105 cells/ml. Sera from different groups of mice (final dilution 1:100) were added to 50 μL of cells and incubated for 30 min at 4 °C. After two washes with MACS buffer, the cells were incubated with APC conjugated donkey anti-mouse IgG (Thermo Fisher Scientific) as a secondary antibody at a 1:500 dilution for 30 min at room temperature and in the dark to detect the bound antibody. Cells were washed and then stained with Live/Dead® Fixable Aqua Dead Cell Stain (Thermo Fisher Scientific) in order to eliminate dead cells contaminating the data. Cells were washed again before data acquisition on a BD FACSAria II Flow Cytometer (BD Biosciences) equipped with FACS DiVa software and quantified by FLOWJO software version 10 (LLC). Cells stained with sera from mice immunized with GMMA were designated as threshold.
To evaluate the effect of the presence of anti-GMMA antibodies on the specific binding of anti-Tn antibodies on the surface of T-47D cells, sera were depleted of anti-GMMA antibodies. Briefly, mouse sera were diluted 1:10 in 100 μL (two wells for each serum sample) of MACS buffer and incubated for one hour at 37 °C with GMMA precoated 96-well plates (Nunc MaxiSorp® flat-bottom). Sera incubated in the absence of GMMA antigen were used as a control. After incubation, the remaining depleted samples were collected and tested by flow cytometry analysis following the protocol described previously. To evaluate the content of specific anti-Tn antibodies in mouse sera, 10 μl of Tn mimetic or Tn native at 20 μg/ml in MACS buffer were mixed with 10 μl of sera for 1 h at 37 °C. After incubation 50 × 103 T47D cells were suspended in 80 μl of MACS buffer and added for 30 min at 4 °C. After two washes with MACS buffer, the cells were incubated with a secondary antibody following the protocol described previously.
Cytokines quantification
A ProcartaPlexTM Mouse and Rat Mix & Match Panels (Invitrogen, Cat. Number PPX-15-MXNKUN7) were used to measure a panel of cytokines and receptors. Mouse serum was diluted 1:10 for cytokines analysis. Sample preparation, together with kit standards, detection antibody, and streptavidin-PE, was performed according to the manufacturer’s magnetic immunoassay protocol. Standards and samples were run in duplicate. Cytokine fluorescence intensity was detected using the BioPlex 200 System machine with Multiplex Bio-Assay Analyzer. The standard data points (concentration vs. measurement) were plotted on semi-log axes and a five-parameter logistic (5PL) was made through the points. The concentrations of the samples were determined from the fit with specified dilution factors applied with BioPlex ManagerTM software version 5.0.
Implantation of 4T1-Luc2 TNBC cells in Syngeneic Mice and Tumor growth analysis
One week after the last immunization only mice groups 1, 3, and 5 were orthotopically implanted with a suspension of 8 × 104 4T1-Luc2 in 50 μl of PBS into the fat pad of the third pair of mammary glands using insulin syringes with 32 G needles. Tumor growth was assessed by bioluminescence imaging (BLI) (Ivis Lumina X-5; Perkin Elmer) at days 7 (W1), 14 (W2), and 21 (W3). At day 28 (W4) tumor volume was manually measured with a caliper. For BLI measurement, BALB/c mice bearing 4T1-LUC syngenic orthotopic tumors were injected intraperitoneally with 150 mg/kg of d-Luciferin (Caliper Life Sciences). Ten minutes post-injection, mice were anesthetized with 2% isoflurane and placed in a supine position with their abdomen facing the camera. Images were acquired for 10 seconds using the IVIS Lumina X5 Imaging System (PerkinElmer) following the manufacturer’s recommendations. Regions of interest (ROIs) were drawn around the tumor, and the total radiant efficiency (in photons/s/cm2/Sr) of the tumor was measured using Living Image 2.5 software.
Tumor volumes were calculated according to the formula: Tumor volume = (l × w²)× 0.5, where l = largest diameter and w = width (perpendicular diameter) of the tumor (in mm). Tumor growth was monitored based on the current applicable Directive 2010/63/EU and national law and mice were sacrificed if the tumor size reached 1000 mm3.
Immunofluorescence staining
Primary tumors were fixed in 4% paraformaldehyde (PFA) and embedded in paraffin. Tissue sections (7 μm-thick) on slides were heated overnight at 70° and were deparaffinized in Xylene Substitute (A5597; Sigma) for 30 min at RT and rehydrated in sequential incubation over ethanol scale (100%–90%–70%–50% and 30%) than washed with deionized water and phosphate-buffered saline PBS 1X. For antigen retrieval, slides were placed in preheated Tris–EDTA-based pH 9 buffer, enriched with NP40 0.5% and Tween 20 0.5% and incubated at 90 °C for 30 min, then let cool down at room temperature for 30 min in the same buffer, prior to immunofluorescence staining procedure. As to decrease the non-specific background fluorescence, tissue sections were washed with PBS 1X and then blocked with a blocking solution containing 5% normal goat serum blocking solution (S-1000-20; Vector Laboratories) in PBS for 1 h at room temperature. Primary antibodies staining was performed overnight at 4 °C: anti-rabbit CD3 (78588; Cell Signaling, 1:300), CD11c (97585; Cell Signaling, 1:300), F4-80 (70076; Cell Signaling, 1:300), CD19 (90176; Cell Signaling, 1:300). Tissue sections were washed in PBS 1X and were incubated with secondary antibody, anti-rabbit Alexa Fluor 647 (A-21245; Thermo Fisher, 1:500). Nuclei were stained with DAPI (62248; Thermo Fisher, 1:1000), washed with PBS 1X and mounted using Prolong Diamond mounting reagent (P36970; Thermo Fisher). Images were acquired using spinning disk confocal microscopy on a Nikon instrument (Ti; Nikon Europe) equipped with X-Light-V2 + VCS spinning disk head (CrestOptics) and EM-CCD Camera (iXon DU888; ANdor Technologies) with laser excitation (LDI Ltd), employing ×5, ×10, and ×20 objectives (Nikon Europe).
Ultrasound analyses of tumor growth in animal control group (saline)
A control mouse group treated with saline solution was included in the trial. However, in this group, we observed a very rapid outgrowth of orthotopic tumors compared to the groups treated with GMMA formulations, which did not allow a fair quantitative comparison by bioluminescence imaging analysis. Ultrasound tridimensional imaging was thus used. In Table S3 data are reported.
Animals and tumor model
Immunocompetent female BALB/c mice aged 6–8 weeks were used. The orthotopic breast tumor was generated by injecting 4T1-Luc mammary tumor cells into the fourth mammary gland. The cells were suspended in PBS and inoculated in a volume of 50 µL. Animals were monitored for tumor growth and overall well-being. All animal experiments were conducted in accordance with institutional guidelines and approved by the animal experimentation ethics committee.
Ultrasound system
Ultrasound analyses were performed using a high-frequency ultrasound system (Vevo 2100, VisualSonics) with a 40 MHz probe for high-resolution tumor imaging.
Animal preparation for ultrasound
Mice were anesthetized with isoflurane (2–3% oxygen) and positioned on a heated platform to maintain body temperature. Hair in the mammary region was removed using depilatory cream to improve image quality. Ultrasound gel was applied to prevent air bubbles between the probe and the skin.
Image acquisition
Ultrasound images were acquired in B-mode for tumor morphology assessment. The tumor area was measured using an integrated function for the quantification of ultrasound images in the Vevo 2100 software
Statistical analyses
Statistical analyses of serological data, flow cytometry, and bioluminescence were performed using GraphPad Prism (version 9.4.1). Statistical significance between groups was determined using the Mann–Whitney test to compare ranks or using two-way ANOVA Tukey’s multiple comparison test. P-values < 0.05 were considered significant. The correlation matrix was represented as a correlogram between tumor inhibition values, titers of immunoglobulin subsets, and serum cytokine levels and was performed using the Pearson correlation coefficient.
Data availability
All data generated or analyzed during this study are included in this published article or in its supplementary information file. All the datasets and raw data, necessary to interpret, replicate and build upon the methods or findings reported in the article, are properly recorded in internal Laboratory Notebooks and are accessible for further evaluation following formal written request.
References
Berois, N., Pittini, A. & Osinaga, E. Targeting tumor glycans for cancer therapy: successes. Cancers (Basel) 14, 645 (2022).
Johannssen, T. & Lepenies, B. Glycan-based cell targeting to modulate immune responses. Trends Biotechnol. 35, 334–346 (2017).
Barchi, J. J. Glycoconjugate nanoparticle-based systems in cancer immunotherapy: novel designs and recent updates. Front. Immunol. 13, 1–22 (2022).
Caproni, E. et al. Anti-tumor efficacy of in situ vaccination using bacterial outer membrane vesicles. Cancers (Basel) 15, 3328 (2023).
Turley, J. L. & Lavelle, E. C. Resolving adjuvant mode of action to enhance vaccine efficacy. Curr. Opin. Immunol. 77, 102229 (2022).
Mazal, D. et al. Monoclonal antibodies toward different Tn-amino acid backbones display distinct recognition patterns on human cancer cells. Implications for effective immuno-targeting of cancer. Cancer Immunol. Immunother. 62, 1107–1122 (2013).
Springer, G. F. Immunoreactive T and Tn epitopes in cancer diagnosis, prognosis, and immunotherapy. J. Mol. Med. 75, 594–602 (1997).
Cheever, M. A. et al. The prioritization of cancer antigens: a National Cancer Institute pilot project for the acceleration of translational research. Clin. Cancer Res. 15, 5323–5337 (2009).
Gill, D. J. et al. Initiation of GalNAc-type O-glycosylation in the endoplasmic reticulum promotes cancer cell invasiveness. Proc. Natl Acad. Sci. USA 110, E3152-61 (2013).
Terasawa, K. et al. T. Expression of Tn and sialyl-Tn antigens in the neoplastic transformation of uterine cervical epithelial cells. Cancer Res. 56, 2229–2232 (1996).
Pinto, D. & Parameswaran, R. Role of truncated O-GalNAc glycans in cancer progression and metastasis in endocrine cancers. Cancers (Basel) 15, 1–14 (2023).
Venturi, F. et al. A new scaffold for the stereoselective synthesis of alpha-O-linked glycopeptide mimetics. J. Org. Chem. 69, 6153–6155 (2004).
Slovin, S. F. et al. Fully synthetic carbohydrate-based vaccines in biochemically relapsed prostate cancer: clinical trial results with α-N-acetylgalactosamine-O-serine/threonine conjugate vaccine. J. Clin. Oncol. 21, 4292–4298 (2003).
Rosenbaum, P. et al. The fully synthetic glycopeptide MAG-Tn3 therapeutic vaccine induces tumor-specific cytotoxic antibodies in breast cancer patients. Cancer Immunol. Immunother. 69, 703–716 (2020).
Scheid, E. et al. Tn-MUC1 DC vaccination of rhesus macaques and a Phase I/II trial in patients with nonmetastatic castrate-resistant prostate cancer. Cancer Immunol. Res. 4, 881–892 (2016).
Ganneau, C. et al. Large-scale synthesis and structural analysis of a synthetic glycopeptide dendrimer as an anti-cancer vaccine candidate. Org. Biomol. Chem. 15, 114–123 (2017).
Sanz-Martinez, I. et al. Molecular recognition of GalNAc in Mucin-type O-glycosylation. Acc. Chem. Res. 56, 548–560 (2023).
Nativi, C. et al. Tn antigen analogues: the synthetic way to ‘upgrade’ an attracting tumour associated carbohydrate antigen (TACA). Chem. Commun. 55, 7729–7736 (2019).
Kurfiřt, M. et al. Development of α-selective glycosylation for the synthesis of deoxyfluorinated TNAntigen analogues. J. Org. Chem. 86, 5073–5090 (2021).
Amedei, A. et al. A structurally simple vaccine candidate reduces progression and dissemination of triple-negative breast cancer. iScience 23, 101250 (2020).
Gabba, A. et al. MUC1 glycopeptide vaccine modified with a GalNAc glycocluster targets the macrophage galactose C-type lectin on dendritic cells to elicit an improved humoral response. J. Am. Chem. Soc. 145, 13027–13037 (2023).
Guillen-Poza, P. A. et al. Amplified detection of breast cancer autoantibodies using MUC1-based Tn antigen mimics. J. Med. Chem. 63, 8524–8533 (2020).
Van Der Put, R. M. F. et al. Validation of an FFF-MALS method to characterize the production and functionalization of outer-membrane vesicles for conjugate vaccines. Anal. Chem. 94, 12033–12041 (2022).
Huang, Y. et al. Outer membrane vesicles (OMVs) enabled bio-applications: a critical review. Biotechnol. Bioeng. 119, 34–47 (2022).
Liu, Q. et al. Recombinant outer membrane vesicles delivering eukaryotic expression plasmid of cytokines act as enhanced adjuvants against Helicobacter pylori infection in mice. Infect. Immun. 91, 1–19 (2023).
Kim, O. Y. et al. Bacterial outer membrane vesicles suppress tumor by interferon-γ-mediated antitumor response. Nat. Commun. 8, 626 (2017).
Kim, J.-B. et al. Non-Invasive detection of a small number of bioluminescent cancer cells in vivo. PLoS ONE 5, e9364 (2010).
Kuerban, K. et al. Doxorubicin-loaded bacterial outer-membrane vesicles exert enhanced anti-tumor efficacy in non-small-cell lung cancer. Acta Pharm. Sin. B 10, 1534–1548 (2020).
Wang, S. et al. Bacterial outer membrane vesicles as a candidate tumor vaccine platform. Front. Immunol. 13, 1–15 (2022).
Grandi, A. et al. Vaccination with a FAT1-derived B cell epitope combined with tumor-specific B and T cell epitopes elicits additive protection in cancer mouse models. Front. Oncol. 8, 1–14 (2018).
Jiménez-Barbero, J. et al. α-O-Linked glycopeptide mimetics: synthesis, conformation analysis, and interactions with viscumin, a galactoside-binding model lectin. Chemistry-Eur. J. 15, 10423–10431 (2009).
Ardá, A. et al. Structural insights into the binding of sugar receptors (lectins) to a synthetic tricyclic Tn mimetic and its glycopeptide version. Eur. J. Org. Chem. 2015, 6823–6831 (2015).
Richichi, B. et al. A cancer therapeutic vaccine based on clustered Tn-antigen mimetics induces strong antibody-mediated protective immunity. Angew. Chem. Int. Ed. 53, 11917–11920 (2014).
Malito, E. et al. Structural basis for lack of toxicity of the diphtheria toxin mutant CRM197. Proc. Natl Acad. Sci. USA 109, 5229–5234 (2012).
Pecetta, S. et al. Carrier priming effect of CRM197 is related to an enhanced B and T cell activation in meningococcal serogroup A conjugate vaccination. Immunological comparison between CRM197 and diphtheria toxoid. Vaccine 34, 2334–2341 (2016).
Manuelli, M. et al. Iron oxide superparamagnetic nanoparticles conjugated with a conformationally blocked α-Tn antigen mimetic for macrophage activation. Nanoscale 6, 7643–7655 (2014).
Gracia, R. et al. Biocompatible single-chain polymer nanoparticles loaded with an antigen mimetic as potential anticancer vaccine. ACS Macro Lett. 7, 196–200 (2018).
Corzana, F. et al. Detection of tumor‐associated autoantibodies in the sera of pancreatic cancer patients using engineered MUC1 glycopeptide nanoparticle probes. Angew. Chem. Int. Ed. 2200, e202407131 (2024).
Tozawa, E. et al. Mucin expression, p53 overexpression, and peritumoral lymphocytic infiltration of advanced colorectal carcinoma with mucus component: Is mucinous carcinoma a distinct histological entity? Pathol. Res. Pract. 203, 567–574 (2007).
Chang, T. C. et al. Precise immunological evaluation rationalizes the design of a self-adjuvanting vaccine composed of glycan antigen, TLR1/2 ligand, and T-helper cell epitope. RSC Adv. 12, 18985–18993 (2022).
Papi, F., Pâris, A., Lafite, P., Daniellou, R. & Nativi, C. Synthesis of an STnThr analogue, structurally based on a TnThr antigen mimetic. Org. Biomol. Chem. 18, 7366–7372 (2020).
Mancini, F. et al. GMMA-based vaccines: the known and the unknown. Front. Immunol. 12, 1–7 (2021).
Micoli, F. et al. Outer membrane vesicle vaccine platforms. BioDrugs 38, 47–59 (2024).
Leroux-Roels, I. et al. Safety and immunogenicity of a 4-component generalized modules for membrane antigens shigella vaccine in healthy European adults: randomized, phase 1/2 study. J. Infect. Dis. 230, 971–984 (2024).
Piccioli, D., Bartolini, E. & Micoli, F. GMMA as a ‘plug and play’ technology to tackle infectious disease to improve global health: context and perspectives for the future. Expert Rev. Vaccines 21, 163–172 (2022).
Roier, S. et al. A novel mechanism for the biogenesis of outer membrane vesicles in Gram-negative bacteria. Nat. Commun. 7, 1–13 (2016).
Micoli, F. et al. Generalized modules for membrane antigens as carrier for polysaccharides: impact of sugar length, density, and attachment site on the immune response elicited in animal models. Front. Immunol. 12, 1–12 (2021).
Hau, J., Schapiro, S. J. & Hau, J. Handbook of Laboratory Animal Science Essential Principles and Practices Vol. I. Handbook of Laboratory Animal Science (CRC Press, 2002).
Palmieri, E. et al. GMMA as an alternative carrier for a glycoconjugate vaccine against Group A Streptococcus. Vaccines 10, 1034 (2022).
Micoli, F. et al. GMMA is a versatile platform to design effective multivalent combination vaccines. Vaccines 8, 1–16 (2020).
Micoli, F. et al. Comparative immunogenicity and efficacy of equivalent outer membrane vesicle and glycoconjugate vaccines against nontyphoidal Salmonella. Proc. Natl Acad. Sci. USA 115, 10428–10433 (2018).
Chenoweth et al. Harnessing the immune system via FcγR function in immune therapy: a pathway to next-gen mAbs. Immunol. Cell Biol. 98, 287–304 (2020).
Bordron, A. et al. Hyposialylation must be considered to develop future therapies in autoimmune diseases. Int. J. Mol. Sci. 22, 3402 (2021).
Micoli, F. et al. Methods for assessment of OMV/GMMA quality and stability. Methods Mol. Biol. 2414, 227–279 (2022).
Satake, K. et al. The spectrophotometric determination of amine, amino acid and peptide with 2,4,6- trinitrobenzene 1-sulfonic acid. J. Biochem. 47, 654–660 (1960).
Acknowledgements
Authors thank Dr. Piero Pileri (Fondazione Toscana Life Sciences, Siena, Italy) for fruitful discussions. This work has been supported by the Italian “Progetto Dipartimenti di Eccellenza 2023–2027” (DICUS, University of Firenze and Department of Clinical Sciences and Community Health, University of Milano). We acknowledge Fondazione AIRC under IG 2021-ID 25762 project—P.I. Cristina Nativi, for financial support.
Author information
Authors and Affiliations
Contributions
C.N., R.G., and F.M. conceived the project; M.F., F.B., E.P., S.V., and C.T. discussed the data, C.N., R.G., and F.M. wrote the paper; E.P., A.S., E.P., F.P., C.C., S.V., M.R., and A.D.R. performed the experiments and prepared the Supplementary Information.
Corresponding authors
Ethics declarations
Competing interests
E.P., F.B., F.M., and F.P. are employees of the GSK group of companies. GSK Vaccines Institute for Global Health s.r.l. is an affiliate of GlaxoSmithKline Biologicals SA; R.G. is an employee of Checkmab s.r.l. All the other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pesce, E., Sodini, A., Palmieri, E. et al. GMMA decorated with mucin 1 Tn/STn mimetics elicit specific antibodies response and inhibit tumor growth. npj Vaccines 10, 71 (2025). https://doi.org/10.1038/s41541-025-01127-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41541-025-01127-8