Abstract
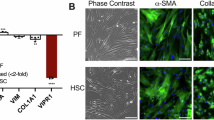
Liver fibrosis is an over-reacted wound healing that becomes lethal in its late stage, when hepatic stellate cells (HSCs) trigger fibrotic response, proliferation of connective tissue and build-up of directional fibrous tissue bands (septa). Current in vitro models of liver fibrosis cannot reproduce liver lobule structure and the dynamic formation of septa at the same time, and the known biochemical cues underlying the progression of liver fibrosis cannot explain directional formation of fibrotic tissue. Here we report a microfabricated in vitro model that reproduces both the hexagonal liver lobule structure and the dynamic directionality of septa formation. By using collagen and primary mouse HSCs or human HSC lines, we found that tension was necessary to coordinate the cell migration that contributes to the band-like cell distribution and that HSCs sensed directional biophysical cues through liquid–liquid phase separation. This system allows the study of the biophysical interaction of HSCs and collagen during the formation of septa structures, and could be used to deepen our understanding of liver fibrosis progression.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
All original data within this paper can be accessed through the corresponding author upon reasonable request. Source data are provided with this paper.
Code availability
The engineering files to prepare the PDMS stamp and the stretching systems, source code for building meshes to simulate collagen distribution after being contracted by cells (Rhino license required, with Grasshopper and Kangaroo Physics plugin), the calculator of collagen preparation formula, and the script to process raw migration data in batches are freely available on GitHub at https://github.com/LUKE-ZZ/nBME2025_Engineering_files (ref. 84) and https://github.com/LUKE-ZZ/nBME2025_Code (ref. 85). The description of these files is summarized in Supplementary Tables 2 and 3.
Material availability
Wild-type or genetically manipulated cell lines and plasmids in this paper can be shared upon reasonable request.
References
Friedman, S. L. Liver fibrosis–from bench to bedside. J. Hepatol. 38, 38–53 (2003).
Devarbhavi, H. et al. Global burden of liver disease: 2023 update. J. Hepatol. 79, 516–537 (2023).
Kisseleva, T. & Brenner, D. Molecular and cellular mechanisms of liver fibrosis and its regression. Nat. Rev. Gastroenterol. Hepatol. 18, 151–166 (2021).
Ortiz, C. et al. Extracellular matrix remodeling in chronic liver disease. Curr. Tissue Microenviron. Rep. 2, 41–52 (2021).
D’Amico, G. et al. Clinical states of cirrhosis and competing risks. J. Hepatol. 68, 563–576 (2018).
Bedossa, P. & Poynard, T. An algorithm for the grading of activity in chronic hepatitis C. Hepatology 24, 289–293 (1996).
Asselah, T. et al. Gene expression and hepatitis C virus infection. Gut 58, 846–858 (2009).
Scheuer, P. J. Classification of chronic viral hepatitis: a need for reassessment. J. Hepatol. 13, 372–374 (1991).
Batts, K. P. & Ludwig, J. Chronic hepatitis: an update on terminology and reporting. Am. J. Surg. Pathol. 19, 1409–1417 (1995).
Ishak, K. Histological grading and staging of chronic hepatitis. J. Hepatol. 22, 696–699 (1995).
Bataller, R. & Brenner, D. A. Liver fibrosis. J. Clin. Invest. 115, 209–218 (2005).
Mederacke, I. et al. Fate tracing reveals hepatic stellate cells as dominant contributors to liver fibrosis independent of its aetiology. Nat. Commun. 4, 2823 (2013).
Geerts, A. History, heterogeneity, developmental biology, and functions of quiescent hepatic stellate cells. Semin. Liver Dis. 21, 311–336 (2001).
Saxena, R. Practical Hepatic Pathology: A Diagnostic Approach E-Book (Elsevier Health Sciences, 2011).
van Grunsven, L. A. 3D in vitro models of liver fibrosis. Adv. Drug Deliv. Rev. 121, 133–146 (2017).
Hsiao, S. K. et al. An in vitro fibrotic liver lobule model through sequential cell-seeding of HSCs and HepG2 on 3D-printed poly (glycerol sebacate) acrylate scaffolds. J. Mater. Chem. B 10, 9590–9598 (2022).
Maharjan, S. et al. 3D human nonalcoholic hepatic steatosis and fibrosis models. Biodes. Manuf. 4, 157–170 (2021).
Maschmeyer, I. et al. A four-organ-chip for interconnected long-term co-culture of human intestine, liver, skin and kidney equivalents. Lab Chip 15, 2688–2699 (2015).
Leite, S. B. et al. Novel human hepatic organoid model enables testing of drug-induced liver fibrosis in vitro. Biomaterials 78, 1–10 (2016).
Seki, E. et al. TLR4 enhances TGF-β signaling and hepatic fibrosis. Nat. Med. 13, 1324–1332 (2007).
Feaver, R. E. et al. Development of an in vitro human liver system for interrogating nonalcoholic steatohepatitis. JCI Insight 1, e90954 (2016).
Janmey, P. A. & Miller, R. T. Mechanisms of mechanical signaling in development and disease. J. Cell Sci. 124, 9–18 (2011).
Liu, L. et al. Matrix-transmitted paratensile signaling enables myofibroblast–fibroblast cross talk in fibrosis expansion. Proc. Natl Acad. Sci. USA 117, 10832–10838 (2020).
Long, Y., Niu, Y., Liang, K. & Du, Y. Mechanical communication in fibrosis progression. Trends Cell Biol. 32, 70–90 (2022).
El Taghdouini, A., Najimi, M., Sancho-Bru, P., Sokal, E. & van Grunsven, L. A. In vitro reversion of activated primary human hepatic stellate cells. Fibrogenesis Tissue Repair 8, 14 (2015).
Hong, Y., Li, S., Wang, J. & Li, Y. In vitro inhibition of hepatic stellate cell activation by the autophagy-related lipid droplet protein ATG2A. Sci. Rep. 8, 9232 (2018).
Yoneda, A., Sakai-Sawada, K., Niitsu, Y. & Tamura, Y. Vitamin A and insulin are required for the maintenance of hepatic stellate cell quiescence. Exp. Cell Res. 341, 8–17 (2016).
Dewidar, B., Meyer, C., Dooley, S. & Meindl-Beinker, A. N. TGF-β in hepatic stellate cell activation and liver fibrogenesis–updated 2019. Cells 8, 1419 (2019).
Gressner, O. A., Weiskirchen, R. & Gressner, A. M. Evolving concepts of liver fibrogenesis provide new diagnostic and therapeutic options. Comp. Hepatol. 6, 7 (2007).
Baiocchini, A. et al. Extracellular matrix molecular remodeling in human liver fibrosis evolution. PLoS ONE 11, 0151736 (2016).
Gong, J., Tu, W., Liu, J. & Tian, D. Hepatocytes: a key role in liver inflammation. Front. Immunol. 13, 1083780 (2023).
Wang, C. et al. Macrophage polarization and its role in liver disease. Front. Immunol. 12, 803037 (2021).
Wang, Z., Du, K., Jin, N., Tang, B. & Zhang, W. Macrophage in liver fibrosis: identities and mechanisms. Int. Immunopharmacol. 120, 110357 (2023).
Song, L. et al. The differential and dynamic progression of hepatic inflammation and immune responses during liver fibrosis induced by Schistosoma japonicum or carbon tetrachloride in mice. Front. Immunol. 11, 570524 (2020).
Beljaars, L. et al. Hepatic localization of macrophage phenotypes during fibrogenesis and resolution of fibrosis in mice and humans. Front. Immunol. 5, 109533 (2014).
Pakshir, P. et al. Dynamic fibroblast contractions attract remote macrophages in fibrillar collagen matrix. Nat. Commun. 10, 1850 (2019).
Ban, E. et al. Strong triaxial coupling and anomalous Poisson effect in collagen networks. Proc. Natl Acad. Sci. USA 116, 6790–6799 (2019).
Fan, Q. et al. Dynamically re-organized collagen fiber bundles transmit mechanical signals and induce strongly correlated cell migration and self-organization. Angew. Chem. Int. Ed. 60, 11858–11867 (2021).
Dıaz, F., Kaufmann, G. & Galizzi, G. Determination of residual stresses using hole drilling and digital speckle pattern interferometry with automated data analysis. Optics Lasers Eng. 33, 39–48 (2000).
Shi, Q. et al. Rapid disorganization of mechanically interacting systems of mammary acini. Proc. Natl Acad. Sci. USA 111, 658–663 (2014).
Kilarski, W. W., Samolov, B., Petersson, L., Kvanta, A. & Gerwins, P. Biomechanical regulation of blood vessel growth during tissue vascularization. Nat. Med. 15, 657–664 (2009).
May, J. et al. GPIIb-IIIa antagonists cause rapid disaggregation of platelets pre-treated with cytochalasin D. Evidence that the stability of platelet aggregates depends on normal cytoskeletal assembly. Platelets 9, 227–232 (1998).
Das, R. K., Gocheva, V., Hammink, R., Zouani, O. F. & Rowan, A. E. Stress-stiffening-mediated stem-cell commitment switch in soft responsive hydrogels. Nat. Mater. 15, 318–325 (2016).
Han, Y. L. et al. Cell contraction induces long-ranged stress stiffening in the extracellular matrix. Proc. Natl Acad. Sci. USA 115, 4075–4080 (2018).
Roeder, B. A., Kokini, K., Sturgis, J. E., Robinson, J. P. & Voytik-Harbin, S. L. Tensile mechanical properties of three-dimensional type I collagen extracellular matrices with varied microstructure. J. Biomech. Eng. 124, 214–222 (2002).
Vader, D., Kabla, A., Weitz, D. & Mahadevan, L. Strain-induced alignment in collagen gels. PLoS ONE 4, 5902 (2009).
Bangasser, B. L. et al. Shifting the optimal stiffness for cell migration. Nat. Commun. 8, 15313 (2017).
Wang, W. Y., Davidson, C. D., Lin, D. & Baker, B. M. Actomyosin contractility-dependent matrix stretch and recoil induces rapid cell migration. Nat.Commun. 10, 1186 (2019).
Baker, B. M. et al. Cell-mediated fibre recruitment drives extracellular matrix mechanosensing in engineered fibrillar microenvironments. Nat. Mater. 14, 1262–1268 (2015).
Schiller, H. B., Friedel, C. C., Boulegue, C. & Fässler, R. Quantitative proteomics of the integrin adhesome show a myosin II-dependent recruitment of LIM domain proteins. EMBO Rep. 12, 259–266 (2011).
James, V. et al. LIM-domain proteins, LIMD1, Ajuba, and WTIP are required for microRNA-mediated gene silencing. Proc. Natl Acad. Sci. USA 107, 12499–12504 (2010).
Ibar, C. et al. Tension-dependent regulation of mammalian Hippo signaling through LIMD1. J. Cell Sci. 131, 214700 (2018).
Hyman, A. A., Weber, C. A. & Jülicher, F. Liquid–liquid phase separation in biology. Annu. Rev. Cell Dev. Biol. 30, 39–58 (2014).
Wang, Y. et al. LIMD1 phase separation contributes to cellular mechanics and durotaxis by regulating focal adhesion dynamics in response to force. Dev. Cell 56, 1313–1325 (2021).
Hinman, S. S., Wang, Y., Kim, R. & Allbritton, N. L. In vitro generation of self-renewing human intestinal epithelia over planar and shaped collagen hydrogels. Nat. Protoc. 16, 352–382 (2021).
Stevens, K. R. et al. In situ expansion of engineered human liver tissue in a mouse model of chronic liver disease. Sci. Transl. Med. 9, 5505 (2017).
Xie, G. et al. Role of differentiation of liver sinusoidal endothelial cells in progression and regression of hepatic fibrosis in rats. Gastroenterology 142, 918–927 (2012).
Zbodakova, O., Chalupsky, K., Tureckova, J. & Sedlacek, R. Metalloproteinases in liver fibrosis: current insights. Metalloproteinases Med. 2017, 25–35 (2017).
Yang, F. et al. Crosstalk between hepatic stellate cells and surrounding cells in hepatic fibrosis. Int. Immunopharmacol. 99, 108051 (2021).
Ollier, R. C., Xiang, Y., Yacovelli, A. M. & Webber, M. J. Biomimetic strain-stiffening in fully synthetic dynamic-covalent hydrogel networks. Chem. Sci. 14, 4796–4805 (2023).
Nguyen, H., Dayan, P. & Goodhill, G. J. How receptor diffusion influences gradient sensing. J. R. Soc. Interface 12, 20141097 (2015).
Winer, J. P., Oake, S. & Janmey, P. A. Non-linear elasticity of extracellular matrices enables contractile cells to communicate local position and orientation. PLoS ONE 4, 6382 (2009).
Barriga, E. H., Franze, K., Charras, G. & Mayor, R. Tissue stiffening coordinates morphogenesis by triggering collective cell migration in vivo. Nature 554, 523–527 (2018).
Harris, A. K., Stopak, D. & Wild, P. Fibroblast traction as a mechanism for collagen morphogenesis. Nature 290, 249–251 (1981).
Doyle, A. D. & Yamada, K. M. Mechanosensing via cell-matrix adhesions in 3D microenvironments. Exp. Cell Res. 343, 60–66 (2016).
Campbell, S., Zitnay, R., Mendoza, M. & Bidone, T. C. Computational model of 3D cell migration based on the molecular clutch mechanism. Preprint at bioRxiv https://doi.org/10.1101/2021.09.29.462287 (2021).
You, Z., Zhou, L., Li, W., Huang, C. & Du, Y. Mechanical microenvironment as a key cellular regulator in the liver. Acta Mech. Sin. 35, 289–298 (2019).
Weiskirchen, R. et al. Genetic characteristics of the human hepatic stellate cell line LX–2. PLoS ONE 8, e75692 (2013).
Uphoff, C. C. & Drexler, H. G. in Cancer Cell Culture. Methods in Molecular Biology Vol 731 (ed. Cree, I.) 93–103 (Humana Press, 2011).
Mederacke, I., Dapito, D. H., Affò, S., Uchinami, H. & Schwabe, R. F. High-yield and high-purity isolation of hepatic stellate cells from normal and fibrotic mouse livers. Nat. Protoc. 10, 305–315 (2015).
Yamamuro, C. et al. Loss of function of a rice brassinosteroid insensitive1 homolog prevents internode elongation and bending of the lamina joint. Plant Cell 12, 1591–1605 (2000).
Geraldo, S., Simon, A. & Vignjevic, D. M. Revealing the cytoskeletal organization of invasive cancer cells in 3D. J. Vis. Exp. 80, e50763 (2013).
Pande, M., Kumari, N. P., Dubey, V. K., Tripathi, P. & Jagannadham, M. Stability and unfolding studies on alkaline denatured state (Ip) of pepsin. Process Biochem. 44, 906–911 (2009).
Zhang, Q. et al. Collagen gel contraction assays: from modelling wound healing to quantifying cellular interactions with three-dimensional extracellular matrices. Eur. J. Cell Biol. 101, 151253 (2022).
Grinnell, F., Ho, C.-H., Lin, Y.-C. & Skuta, G. Differences in the regulation of fibroblast contraction of floating versus stressed collagen matrices. J. Biol. Chem. 274, 918–923 (1999).
Gong, X. & Mills, K. L. Large-scale patterning of single cells and cell clusters in hydrogels. Sci. Rep. 8, 3849 (2018).
Doyle, A. D., Sykora, D. J., Pacheco, G. G., Kutys, M. L. & Yamada, K. M. 3D mesenchymal cell migration is driven by anterior cellular contraction that generates an extracellular matrix prestrain. Dev. Cell 56, 826–841 (2021).
Sandker, G., Slooff, M. & Groothuis, G. Drug transport, viability and morphology of isolated rat hepatocytes preserved for 24 hours in University of Wisconsin solution. Biochem. Pharmacol. 43, 1479–1485 (1992).
Taylor, S. E., Cao, T., Talauliker, P. M. & Lifshitz, J. Objective morphological quantification of microscopic images using a fast Fourier transform (FFT) analysis. Curr. Protoc. Essent. Lab. Tech. 7, 9.5.1–9.5.12 (2013).
Harris, G. M., Raitman, I. & Schwarzbauer, J. E. Cell-derived decellularized extracellular matrices. Methods Cell Biol. 143, 97–114 (2018).
Pena, E., Calvo, B., Martinez, M., Palanca, D. & Doblaré, M. Finite element analysis of the effect of meniscal tears and meniscectomies on human knee biomechanics. Clin. Biomech. 20, 498–507 (2005).
Krishnan, L., Weiss, J. A., Wessman, M. D. & Hoying, J. B. Design and application of a test system for viscoelastic characterization of collagen gels. Tissue Eng. 10, 241–252 (2004).
Hughes, A. J. et al. Engineered tissue folding by mechanical compaction of the mesenchyme. Dev. Cell 44, 165–178 (2018).
Zhou, L. et al. nBME2025 Engineering files. GitHub https://github.com/LUKE-ZZ/nBME2025_Engineering_files (2025).
Zhou, L. et al. nBME2025 Code. GitHub https://github.com/LUKE-ZZ/nBME2025_Code (2025).
Acknowledgements
We thank the Animal Core Facility and State Key Laboratory of Membrane Biology Imaging Branch at Tsinghua University for technical assistance; Tsinghua University Branch of China National Center for Protein Sciences (Beijing) and Tsinghua University Technology Center for Protein Research and Cell Function Analyzing Facility; Z. Cui for assisting in preparing the PDMS stamp; R. Lu and P. Zhao for helping during cell culture; and Z. Zeng from Fudan University for providing LX-2s. This work was financially supported by the National Natural Science Foundation of China (82125018, 32430058 and 82061148010 to Y.D.).
Author information
Authors and Affiliations
Contributions
L.Z., Z.Y. and Y.D. conceived and designed the project. Y.D. is the principal investigator. L.Z., Z.S. and Z.Y. contributed to design and preparation of the PDMS stamp. L.Z. developed the method to prepare PDMS pillar array with laser engraving. Z.S. optimized the method to prepare the cover with lithography. Z.Y. designed the strategy to combine the pillar array and the cover to prepare the PDMS stamp. L.Z. prepared the in vitro models of liver fibrosis using LX-2s and primary mouse HSCs. L.Z. tested the effect of collagen of higher concentration on the in vitro model. L.Z. isolated primary mouse HSCs, characterized the activation on TCP and optimized the PDMS stamp for primary cells. L.Z. tested the longevity of the in vitro models constructed using LX-2s and primary mouse HSCs. L.Z. induced THP-1s to macrophages and co-cultured them with the in vitro model. L.Z. prepared pepsin-digested collagen and tested its effect in the in vitro model. L.Z. and X.Y. performed loss-of-function assays with laser cutting and molecular treatment. X.Y. established the method to estimate cell surface stress on the basis of FEA. L.Z., H.Y., Z.Z. and Z.S. established the method to prepare the stretching systems. L.Z. improved the stretching systems on the basis of H.Y.’s prototype. Z.Z. fine tuned the PMMA components. Z.Z. and Z.S. assisted in preparing the silicone chambers. Z.S. made the diagrams and videos to explain the assembly process of stretching systems. J.Z. and X.Y. processed the data of PIV tracking. Z.Z. and J.Z. processed the FFT data. X.Y. and L.Z. developed the methods for cutting live sections of fibrotic mouse livers and inducing incisions using trimmed razor blades. L.Z. and Z.L. performed experiments on optical tweezers for collagen stiffening in the stretching system. L.Z. performed experiments of optical tweezers of collagen stiffening in the in vitro models of LX-2s and primary HSCs and processed the data. L.Z. characterized cell migration of LX-2s and primary HSCs on strained collagen and Y.N. developed the MATLAB file to analyse the migration trends in batches. L.Z. recorded the time-lapse video of trapped quiescent primary HSCs. L.Z., Yuying Zhang, L.D., X.Y., J.Z. and J.H. constructed the overexpression plasmid of LIMD1-turboGFP. Y.W. and C.W. provided the plasmids to generate the functional knockout line of LIMD1. L.Z. performed the FRAP assay and analysed the data. Y.L. assisted in lentivirus packaging and cell labelling. Z.W. assisted in data processing. L.Z., Yan Zhang and C.L. optimized the methods of isolation of primary mouse HSCs. L.Z., Z.S. and Y.D. drafted and revised the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Biomedical Engineering thanks Geoffrey Gurtner and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 2 The methods to prepare the PDMS stamp for the in vitro liver fibrosis model with the hexagonal liver lobule structure.
Key results are included in Fig. 2m. a, The blueprint of the PMMA (polymethyl methacrylate) mould with thin holes (A1). b, Preparation of the solid portal pillar (A2) by casting A1 with PDMS. c, The blueprint of the PMMA mould with thick holes (A3). d, Preparation of the hollow portal pillar (A4) by aligning A2 with A3, and casting with PDMS. e, The photomask (B1). f, Preparation of the photoresist pillar (B2) by lithography on glass substrate. g, Preparation of the PDMS pit (B3) by casting B2 with PDMS. h, Preparation of the PDMS pillar (B4) by casting B3 with PDMS. i, Preparation of the PDMS cover with through holes (B5) by smearing PDMS onto portal pillar tip of B4, crosslinking with PDMS substrate, and casting with PDMS. j, Preparation of the PDMS stamp (C) by aligning A4 with B5, and casting with PDMS. ‘P’ and ‘C’ represent the micro-structure corresponding to portal and central area in the in vitro model of liver fibrosis. j is partially created with BioRender.com. Engineering files of a, c and e can be accessed with the link in Supplementary Table 2.
Extended Data Fig. 3 Long-term culture of the in vitro micro-tissue model of liver fibrosis constructed with LX-2s.
a, After 6-day culture. Scale bar, 500 μm. Total, the whole in vitro model of liver fibrosis. Local, one liver lobule. The experiment in a was repeated 3 times independently with similar results.
Extended Data Fig. 4 Long-term culture of the in vitro micro-tissue model of liver fibrosis constructed with primary mouse hepatic stellate cells.
a, After 12-day culture. Scale bar, 500 μm. Total, the whole in vitro model of liver fibrosis. Local, one liver lobule. The experiment was repeated 3 times independently with similar results.
Extended Data Fig. 5 Laser cut the in vitro model constructed with LX-2s vertically to the ‘portal to portal’ direction.
a, The shape change of the incision after cutting. Scale bar, 100 μm. b, The stacked incision borders. c, The aspect ratio of the incision. d, The diagram to explain why the dilation indicates tension in the ‘portal to portal’ direction. The video is Supplementary Video 6. Data in c (n= 5 biological replicates) are mean ± s.d. Statistical analysis in (c) was performed with the matched nonparametric Friedman test because the aspect ratio data were measured as a matched series from each individual sample. Exact P values are labeled.
Extended Data Fig. 6 Alive liver sections of mouse indicate tension in the center of ‘portal to portal’ direction.
a, The method to cut alive liver sections of a mouse and induce incisions. b, The shape change after loading an incision in the alive liver section. Scale bar, 200 μm. c, The stacked incision borders. d, The ratio of the width to the height of the incision. The experiment in b was repeated 3 times independently with similar results. Data in d (n= 3 biological replicates) are mean ± s.d. Statistical analysis in (d) was performed with the matched nonparametric Friedman test because the aspect ratio data were measured as a matched series from each individual sample. Exact P values are labeled. The video is Supplementary Video 5. a was created with BioRender.com.
Extended Data Fig. 7 The sections of the time-lapse video indicate that quiescent primary HSCs could be trapped around activated primary HSC clusters.
Red line, the migration track. Arrow, the trapped quiescent primary HSC. Scale bar, 100 μm. The video is Supplementary Video 7.
Extended Data Fig. 8 The potential mechanism of the cell migration speed trends on collagen of gradient strain48.
a, The four steps in the classic ‘motor-clutch’ model of cell migration. We focus on the release stage to explain the cell migration trends. b, The potential mechanism to explain why quiescent HSCs have the ‘increase and decrease’ trend of migration speed on collagen of gradient strain. c, The potential mechanism to explain why the migration speed of activated HSCs don’t change evidently on collagen of gradient strain.
Extended Data Fig. 9 The in vitro model of liver fibrosis constructed using activated LX-2s (LIMD1 KO) and quiescent WT LX-2s.
a, After 1-day culture. b, After 4-day culture. Total, the whole in vitro model of liver fibrosis. Local, one liver lobule. Scale bar, 1 mm. The experiments in a-b were repeated 3 times independently with similar results.
Extended Data Fig. 10 Migration tracks of quiescent and activated HSCs on collagen loaded with different strain.
a, Migration tracks of quiescent HSCs. b, Migration tracks of activated HSCs. θ, the average migration angel. The average migration angel of a cell that migrates randomly is close to 45∘, whereas the average migration angel of a cell that migrates ideally along the strain direction is 90∘. How migration speed and average migration angel are calculated from time-lapse videos is explained in Supplementary Fig. 12.
Supplementary information
Supplementary Information
Supplementary Notes 1–8, Figs. 1–20 and Tables 1–9.
Supplementary Video 1
The stretching system compatible with optical tweezers (Fig. 5a) can sustain up to ~60% strain. The video was synthesized from single pictures at different strain which was loaded manually.
Supplementary Video 2
The miniaturized stretching system (Fig. 5j) compatible with live-cell workstation can sustain up to ~50% strain. The video was synthesized from single pictures at different strain which was loaded manually.
Supplementary Video 5
Time-lapse video of the shape change of the incision after cutting the live section of a fibrotic mouse liver. Video snapshots and the quantified analysis are in Extended Data Fig. 6. Playing speed, 10×. Scale bar, 200 μm.
Supplementary Video 6
Time-lapse video of the incision in the in vitro model of liver fibrosis after laser cutting. Video snapshots and the quantified analysis are in Extended Data Fig. 5. Playing speed, 3×. Scale bar, 200 μm.
Supplementary Video 7
Time-lapse video of the quiescent primary HSC trapped around activated primary HSC clusters. Video sections are in Extended Data Fig. 7. Orange, activated primary HSC cluster. Cyan, quiescent primary HSC. Red, migration track. Playing speed, 6,000×. Scale bar, 100 μm.
Source data
Source Data Figures and Extended Data Figures
Statistical source data Figs. 2, 4, 5 and 6, and Extended Data Figs. 5, 6 and 10.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, L., Shi, Z., Yang, X. et al. Tension-induced directional migration of hepatic stellate cells potentially coordinates liver fibrosis progression. Nat. Biomed. Eng 9, 1453–1470 (2025). https://doi.org/10.1038/s41551-025-01381-0
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41551-025-01381-0