Abstract
Over the last decade, attribution science has shown that climate change is responsible for substantial death, disability and illness. However, health impact attribution studies have focused disproportionately on populations in high-income countries, and have mostly quantified the health outcomes of heat and extreme weather. A clearer picture of the global burden of climate change could encourage policymakers to treat the climate crisis like a public health emergency.
Similar content being viewed by others
Main
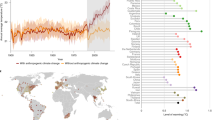
Scientists agree that recent climate change is outside the realm of normal natural variability, that natural factors in the earth system cannot explain the observed changes and that anthropogenic influences are responsible for, at the time of writing1, roughly +1.3 °C of global warming from preindustrial levels. They have developed this consensus through a set of quantitative methods that are grouped under the joint umbrella of climate change detection (showing that the climate has changed) and attribution (distinguishing the relative contributions of both anthropogenic and natural influences on the global climate system). In the past decade, researchers have also started using the same methods to isolate the effects of anthropogenic forcings on the social and ecological consequences of climate change. These end-to-end impact attribution studies2 account for a small fraction of total research on climate change impacts, but represent some of the strongest evidence in terms of both methodological rigour and ability to articulate clear, quantitative estimates of historical and present-day impacts.
Human health—especially loss of life, but also illness, disability and poor well-being—is one of the most visible categories of climate change impacts. However, most work on the health impacts of climate change has stopped a step short of end-to-end attribution, focusing on long-term trends in health outcomes and their relationship with temperature and precipitation, or on the health outcomes of specific extreme weather events3,4,5. The first end-to-end health impact attribution study, which estimated the contribution of human-caused climate change to heat-related mortality during the 2003 European heat wave, was conducted in 20166. Over the past decade, at least 20 studies have estimated the present-day health impacts of human-caused climate change (Fig. 1; see the Methods for search criteria).
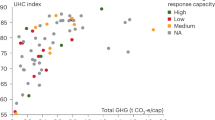
a, The distribution of research effort by health impact and geography of the affected population. The map is divided by World Health Organization global regions. Circle size is proportional to the number of applicable studies focused on each region, ranging from 7 in the Americas to 14 in Europe. b–e, The distribution of studies across years (b) and study focus (c–e). Some studies are in multiple categories.
With a single exception7, every health impact attribution study so far has reported a substantial negative health impact of climate change—most often, loss of life due to rising temperatures or extreme weather. Estimates of community-level mortality have ranged from 10 deaths (on a single day of the 2006 heat wave in London8) to 1,683 deaths (associated with heat in Zurich between 1969 and 20189); at the national level and above, mortality estimates have ranged from 370 deaths (associated with the summer 2022 heat wave in Switzerland10) to 271,656 deaths (associated with heat across 43 countries between 1991 and 201811) (Extended Data Table 1). So far, research effort has been heavily biased towards temperature-related risks (n = 17 of 20), mortality (n = 11 of 20) and extreme weather events in Europe (n = 4 of 6). However, these studies have diversified over time, with recent research addressing the growing burden of mosquito-borne viral diseases12,13, mortality due to air pollution from wildfires14, population displacement by floods15 and several unique health risks experienced by children16, including neonatal deaths17,18, preterm births (and life-long associations with asthma, type 1 and 2 diabetes and cognitive disabilities)18, low birth weight19 and childhood malaria20.
In some cases, the estimated economic impact or value of these losses has been substantial. For example, one study estimated that medical costs related to heat wave-related preterm births in China could exceed US$300 million per year, and the loss of lifetime earnings associated with cognitive disabilities could exceed US$1 billion per year18. Another study estimated that life-years lost due to Hurricane Harvey could be worth roughly US$17 billion21, while a global study of 185 extreme weather events estimated an average attributable loss of life valued at US$22.7 billion per year22. Here, we apply standard estimates of the value of statistical life (VSL)23 to compute monetized losses due to other attributable health impacts. Using both the US Environmental Protection Agency (EPA) VSL and an adjusted version of this figure that accounts for the finding that willingness to pay for reductions in mortality risk varies systematically across countries23,24, we estimate that annual losses are also on the order of at least US$10 billion (Methods). For example, we estimate attributable annual adjusted losses equivalent to US$29.5 billion (unadjusted, using the US EPA VSL: US$106.0 billion) due to temperature-related neonatal deaths in 29 low- and middle-income countries17; US$31.0 billion (unadjusted: US$111.6 billion) due to heat-related deaths across 43 countries11; and US$40.2 billion (unadjusted: US$144.5 billion) due to global fine particulate matter (PM2.5) air pollution from wildfires14. In some cases, directly quantified losses could be approaching the trillions (Table 1): for example, Vicedo-Cabrera et al.’s estimate of 271,656 climate change-attributable heat-related deaths across 43 countries between 1991 and 2018 would be equivalent to a loss of US$869.3 billion (unadjusted: US$3.1 trillion)11. These kinds of estimates are likely to be increasingly important as countries seek financing for loss and damage resulting from climate change25, particularly given that human health impacts dominate estimates of aggregate economic damages from future climate change26.
Another important frontier for health impact attribution is source attribution, a set of methods that quantify the contributions of specific major greenhouse gas emitters to extreme events, long-term warming trends and, in some cases, downstream impacts. For example, a recent preprint9 estimated that dozens of heat-related deaths in Switzerland between 1969 and 2018 could be attributed to specific fossil fuel companies, led by Chevron (59 deaths), ExxonMobil (54 deaths) and Saudi Aramco (53 deaths). Using the same VSL approach as above, these estimates would be equivalent to losses of US$188.8 million (unadjusted: US$678.5 million), US$172.8 million (unadjusted: US$621.0 million) and US$169.6 million (unadjusted: US$609.5 million) attributable to each emitter, respectively. Source attribution studies are likely to have a unique relevance to legal actions against emitters and governments, which can be supported by evidence linking anthropogenic greenhouse gas emissions—and, potentially, the specific emissions of the defendant company—to the claimants’ losses27,28 (Supplementary Text 1).
Increasingly, these studies represent the strongest available line of evidence regarding the present-day health impacts of climate change. In many cases, they are already substantially more up to date than modelling-based estimates: the only comprehensive estimate of present-day (circa 2000) global mortality and morbidity due to climate change was published 20 years ago29,30; in 2014, these estimates were extended from 2030 through 205031. For some health impacts, such as heat- and extreme weather-related mortality, attribution studies have been broadly concordant with these projections (Table 1). In other cases, the divergence has been notable: for example, climate change-attributable mortality related to dengue fever has been an order of magnitude greater than expected, while malaria mortality is estimated to be an order of magnitude lower (Methods). Some major expected sources of mortality have still not been reassessed. For example, one attribution study estimated that every 1 °C of anthropogenic warming has resulted in a 1–2% increase in food insecurity32, but no estimate exists of attributable mortality from malnutrition. Similarly, there have been no impact attribution studies focused on diarrhoeal diseases, despite several closely related observational studies33,34.
New health impact attribution research continues to be published. As the field of health impact attribution continues to grow, these studies can provide a more comprehensive view of the impacts of climate change on mortality, morbidity, life expectancy and well-being. In particular, future studies could assess the impact of climate change on dozens of infectious diseases; non-communicable diseases, including asthma, cancer, diabetes, heart disease and kidney disease35; health impacts of food insecurity, including malnutrition, stunting and direct mortality32; and mental health, including anxiety, depression and suicides36. Future studies should also explore the uneven impacts of climate change within populations. These analyses are currently rare in the attribution literature, although one study found that women and the elderly accounted for 60% and 90% of attributable heat-related deaths, respectively, with older women experiencing mortality at 1.8 times the rate of the general population10.
Finally, future studies should aim to provide a more geographically representative view of the health impacts of climate change. For example, almost all studies at the subnational level have so far focused on communities in high-income countries (n = 6 of 7). These biases represent the research community behind these efforts, which are almost entirely led out of global north institutions—even when focused on health impacts in the global south (Extended Data Fig. 1). The authorship dynamics in this subfield are not atypical in global health, which suffers from a deeply inequitable and colonial system for exchanging data, knowledge, scientific credit and international aid37. Some researchers have suggested that surfacing more open-access health datasets from governments in the global south will help close this gap5, but this is at best a partial solution and at worst will reinforce existing dynamics by making it easier for global north researchers to bypass collaboration altogether. The best way to increase knowledge about the health impacts of climate change is to increase investment in research led by climate scientists and public health researchers living at the frontlines of climate injustice: as one expert recently observed, “knowledge from the global South is in the global South”38.
Methods
Search strategy
In this study, we focus on studies that conduct end-to-end health impact attribution, which we define as a statistical analysis that quantifies present-day or historical health impacts or risks resulting from anthropogenic (human-caused) forcings on the climate through the comparison of factual and counterfactual scenarios (where the counterfactual scenario usually excludes all anthropogenic forcings). These studies constitute some of the strongest evidence for the health impacts of climate change. However, this is a narrow definition: for example, most health outcomes that are attributable to climate change, based on the broader definition used by the Intergovernmental Panel on Climate Change39, have not been identified through the use of an end-to-end impact attribution study.
We used the following keyword set to search for relevant literature on the detection and attribution of human health outcomes to human-caused climate change: (‘climate chang*’ OR ‘climatic change’ OR ‘changing climate’ OR ‘global warming’ OR ‘drought’ OR ‘flood*’ OR ‘storm*’ OR ‘cyclone’ OR ‘extreme weather’ OR ‘monsoon’ OR ‘sea level rise’ OR ‘sea-level rise’ OR ‘heat stress’ OR ‘global heating’) AND (health OR mortality OR morbidity OR ‘infectious disease’ OR ‘non-communicable disease’ OR suicide OR stunting OR miscarriage OR diarrhea OR diarrhoea OR injuries OR cancer OR diabetes OR cardiovascular disease OR stroke OR malnutrition OR malnourish OR anxiety OR depression) AND (attribut* OR counterfactual OR ‘excess mortality’ OR ‘excess cases’ OR DAMIP).
We screened PubMed for studies containing these keywords anywhere in the title, abstract or full text (search conducted 21 July 2023) and, to ensure completeness, ran a second search of Web of Science for additional studies containing these keywords in the title or abstract (search conducted 11 September 2023). In total, we screened 3,677 study abstracts for broad relevance to the health impacts of climate change and evaluated the full text of the 552 studies that passed the first round of screening. This led to the identification of only five eligible studies (Extended Data Fig. 2). However, given the lack of standardized language across studies, which we found limited the completeness of the systematic search, we also searched Google Scholar using ad hoc combinations of keywords related to climate change, health and attribution. We also searched five preprint servers (arXiv, medRxiv, bioRxiv, ResearchSquare and SSRN) using the same ad hoc approach. In total, this approach led to the identification of 13 eligible studies in our original systematic search5, including one that was originally excluded in a prior version of the search15, based on a narrower definition of health impacts.
Since the conclusion of our original systematic literature search, we have continued to monitor Google Scholar and preprint servers for newly published or preprinted studies and have periodically added new studies to an open-access database of health impact attribution literature called the Health Attribution Library (http://healthattribution.org/). Here, we include all seven additional publications and preprints that were posted by 31 December 2024. For completeness, we also note that after this study was concluded, an additional relevant publication from 2024 was identified40 that had been overlooked, due to similarities to a preprint already included in the sample41.
Inclusion criteria
We identified a total of 20 peer-reviewed publications and preprints that have conducted end-to-end attribution of human health outcomes to human-caused climate change. These studies all include (1) a statistical model that relates health outcomes to climate variables and (2) an estimate of the health impact of human-caused climate change, isolated through the use of a counterfactual scenario that captures natural climate variability without anthropogenic forcings. We excluded studies that quantified health effects of observed climate change by comparing health outcomes at different points in time (for example, refs. 42,43), rather than comparing present-day impacts with a present-day counterfactual that omitted anthropogenic influence on the climate. However, we included one study that compared present-day temperature anomalies, baselined on 1880–1910, with a ‘preindustrial’ climate defined as an anomaly of +0 °C (ref. 41). We also excluded a small number of studies that used present-day counterfactual climate scenarios that did not sufficiently distinguish natural and anthropogenic sources of variability44,45. Finally, we excluded studies that included a health-related analysis alongside a climate change attribution component, but stopped short of end-to-end attribution of health impacts46.
VSL analyses
Following Newman and Noy22, we conducted a secondary analysis of economic losses based on the studies in Extended Data Table 1. Like Newman and Noy, we use the VSL to assess the economic value of deaths attributable to human-caused climate change. Such an approach monetizes lives lost by leveraging estimates of how individuals make their own trade-offs between income and mortality risk. These estimates are recovered using diverse methods, ranging from empirical assessments of how people trade off wages versus mortality risk in the labour market47 to stated preference surveys24. Resulting calculations reflect the willingness of individuals to pay to avoid the elevated risk of death and are widely used for policy evaluation48. However, such a valuation approach does not account for any broader societal economic losses, such as costs to a public healthcare system induced by elevated morbidity or mortality.
To implement this, we follow Newman and Noy in using the US EPA’s value for the VSL, and we treat VSL as equivalent across countries on equity-related grounds. However, we adjust the EPA figure for inflation (US$7.4 million in 2006 = US$11.5 million in 2024 US dollars). We also present two options for how to adjust VSL estimates derived by the EPA for the US population to global populations. This adjustment is motivated by the consistent finding that VSL estimates vary systematically with income, due to lower-income populations having a higher marginal benefit from income (for example, ref. 23). In option 1, we adjust for the difference between US and global purchasing power parity-adjusted gross domestic product (GDP) per capita (using World Bank estimates of 2023 GDP adjusted for inflation to 2024 US dollars using the Federal Reserve Economic Data (FRED) GDP deflator49 gives a US GDP per capita of US$84,211 versus global average GDP per capita of US$23,403) using an income elasticity of the VSL of 1, reflecting recent economic consensus48. This approach reduces our global average VSL estimate to US$3.2 million. In option 2 (which we present in parentheticals throughout), we use the full USA-based value of US$11.5 million everywhere, as Newman and Noy did.
Estimating climate change-attributable mortality from vector-borne diseases
To supplement the three studies that generated global, cause-specific estimates of climate change-attributable mortality11,22, we also extrapolated mortality resulting from two vector-borne diseases, based on preliminary results from two preprints12,20. For dengue fever, we used Childs et al.’s estimate that 18% (95% confidence interval (CI) 11% to 27%) of present-day (1995–2014) cases are due to climate change. We multiplied this proportion by an estimated 21,803 (95% CI 17,408 to 26,030) deaths per year due to dengue fever over the same time frame, derived from the Global Burden of Disease study database50. For malaria, we used Carlson et al.’s estimate that climate change was responsible for 0.09 (95% CI −0.30 to 0.51) percentage points of the prevalence of malaria in children (ages 2–10) in sub-Saharan Africa between 2010 and 2014, compared with an estimated continent-wide prevalence of 24% in 201551. In the absence of an epidemiological model relating changes in childhood malaria prevalence to age-structured incidence dynamics (and, ideally, accounting for interventions52), we assumed that changes in prevalence reflect proportional changes in mortality and used an estimate of 631,000 total deaths (95% CI 394,000 to 914,000) across ages and across the continent in 201553.
Data availability
All data are publicly available via GitHub at https://github.com/carlsonlab/AttributableLosses and via Zenodo at https://doi.org/10.5281/zenodo.15685967 (ref. 54).
Code availability
All code is publicly available via GitHub at https://github.com/carlsonlab/AttributableLosses and via Zenodo at https://doi.org/10.5281/zenodo.15685967 (ref. 54).
References
Forster, P. M. et al. Indicators of Global Climate Change 2023: annual update of key indicators of the state of the climate system and human influence. Earth Syst. Sci. Data 16, 2625–2658 (2024).
Carlson, C. J. et al. Designing and describing climate change impact attribution studies: a guide to common approaches. earthRxiv https://doi.org/10.31223/X5CD7M (2024).
Ebi, K. L., Ogden, N. H., Semenza, J. C. & Woodward, A. Detecting and attributing health burdens to climate change. Environ. Health Perspect. 125, 085004 (2017).
Ebi, K. L. et al. Using detection and attribution to quantify how climate change is affecting health. Health Aff. 39, 2168–2174 (2020).
Carlson, C. J. et al. Detection and attribution of climate change impacts on human health: a data science framework. Wellcome Open Res. 9, 245 (2024).
Mitchell, D. et al. Attributing human mortality during extreme heat waves to anthropogenic climate change. Environ. Res. Lett. 11, 074006 (2016).
Hajat, S., Gampe, D. & Petrou, G. Contribution of cold versus climate change to mortality in London, UK, 1976–2019. Am. J. Public Health 114, 398–402 (2024).
Perkins-Kirkpatrick, S. E. et al. On the attribution of the impacts of extreme weather events to anthropogenic climate change. Environ. Res. Lett. 17, 024009 (2022).
Stuart-Smith, R. et al. Quantifying heat-related mortality attributable to human-induced climate change. Research Square https://doi.org/10.21203/rs.3.rs-2702337/v2 (2023).
Vicedo-Cabrera, A. M. et al. The footprint of human-induced climate change on heat-related deaths in the summer of 2022 in Switzerland. Environ. Res. Lett. 18, 074037 (2023).
Vicedo-Cabrera, A. M. et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat. Clim. Chang. 11, 492–500 (2021).
Childs, M. L., Lyberger, K., Harris, M., Burke, M. & Mordecai, E. A. Climate warming is expanding dengue burden in the Americas and Asia. Preprint at medRxiv https://doi.org/10.1101/2024.01.08.24301015 (2024).
Erazo, D. et al. Contribution of climate change to the spatial expansion of West Nile virus in Europe. Nat. Commun. 15, 1196 (2024).
Park, C. Y. et al. Attributing human mortality from fire PM2.5 to climate change. Nat. Clim. Chang. 14, 1193–1200 (2024).
Mester, B. et al. Human displacements from Tropical Cyclone Idai attributable to climate change. Nat. Hazards Earth Syst. Sci. 23, 3467–3485 (2023).
Chapman, S. et al. Past and projected climate change impacts on heat-related child mortality in Africa. Environ. Res. Lett. 17, 074028 (2022).
Dimitrova, A. et al. Temperature-related neonatal deaths attributable to climate change in 29 low- and middle-income countries. Nat. Commun. 15, 5504 (2024).
Zhang, Y. et al. The burden of heatwave-related preterm births and associated human capital losses in China. Nat. Commun. 13, 7565 (2022).
Zhu, Z. et al. Estimating the burden of temperature-related low birthweight attributable to anthropogenic climate change in low-income and middle-income countries: a retrospective, multicentre, epidemiological study. Lancet Planet. Health 8, e997–e1009 (2024).
Carlson, C. J., Carleton, T. A., Odoulami, R. C. & Trisos, C. H. The historical fingerprint and future impact of climate change on childhood malaria in Africa. Preprint at bioRxiv https://doi.org/10.1101/2023.07.16.23292713 (2023).
Frame, D. J., Wehner, M. F., Noy, I. & Rosier, S. M. The economic costs of Hurricane Harvey attributable to climate change. Clim. Change 160, 271–281 (2020).
Newman, R. & Noy, I. The global costs of extreme weather that are attributable to climate change. Nat. Commun. 14, 6103 (2023).
Kniesner, T. J. & Viscusi, W. K. The value of a statistical life. Oxford Res. Encycl. Econ. Finance https://doi.org/10.1093/acrefore/9780190625979.013.138 (2019).
Lindhjem, H., Navrud, S., Braathen, N. A. & Biausque, V. Valuing mortality risk reductions from environmental, transport, and health policies: a global meta-analysis of stated preference studies. Risk Anal. 31, 1381–1407 (2011).
Noy, I. et al. Event attribution is ready to inform loss and damage negotiations. Nat. Clim. Chang. 13, 1279–1281 (2023).
Report on the Social Cost of Greenhouse Gases: Estimates Incorporating Recent Scientific Advances (US Environmental Protection Agency, 2022); https://www.epa.gov/system/files/documents/2023-12/epa_scghg_2023_report_final.pdf
Stuart-Smith, R. F. et al. Filling the evidentiary gap in climate litigation. Nat. Clim. Chang. 11, 651–655 (2021).
Burger, M., Wentz, J. & Horton, R. The law and science of climate change attribution. Colum. J. Envtl. L. 45, 57 (2020).
McMichael, A. J. et al. in Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors (eds Ezzati, M., Lopez, A. D., Rodgers, A. A. & Murray, C. J.) Ch. 20 (World Health Organization, 2004).
Carlson, C. J. After millions of preventable deaths, climate change must be treated like a health emergency. Nat. Med. 30, 622 (2024).
Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s (World Health Organization, 2014).
Dasgupta, S. & Robinson, E. J. Z. Attributing changes in food insecurity to a changing climate. Sci. Rep. 12, 4709 (2022).
Wang, P., Asare, E., Pitzer, V. E., Dubrow, R. & Chen, K. Associations between long-term drought and diarrhea among children under five in low- and middle-income countries. Nat. Commun. 13, 3661 (2022).
Wang, P., Asare, E. O., Pitzer, V. E., Dubrow, R. & Chen, K. Floods and diarrhea risk in young children in low- and middle-income countries. JAMA Pediatr. 177, 1206–1214 (2023).
Rother, H.-A. Controlling and preventing climate-sensitive noncommunicable diseases in urban sub-Saharan Africa. Sci. Total Environ. 722, 137772 (2020).
Carleton, T. A. Crop-damaging temperatures increase suicide rates in India. Proc. Natl Acad. Sci. USA 114, 8746–8751 (2017).
Abimbola, S. The foreign gaze: authorship in academic global health. BMJ Glob. Health 4, e002068 (2019).
Abimbola, S. Knowledge from the global South is in the global South. J. Med. Ethics 49, 337–338 (2023).
Hegerl, G.C. et al. Good Practice Guidance Paper on Detection and Attribution Related to Anthropogenic Climate Change. In Meeting Report of the Intergovernmental Panel on Climate Change Expert Meeting on Detection and Attribution of Anthropogenic Climate Change (eds Stocker, T. F. et al.) pp. 1–8 (IPCC Working Group I Technical Support Unit, Univ. Bern, 2010).
Beck, T. M. et al. Mortality burden attributed to anthropogenic warming during Europe’s 2022 record-breaking summer. NPJ Clim. Atmos. Sci. 7, 245 (2024).
Beck, T. et al. Increasing likelihood of heat-related mortality events with global warming: a continental epidemiological extreme event attribution study. Research Square https://doi.org/10.21203/rs.3.rs-5549732/v1 (2024).
Oudin Åström, D., Forsberg, B., Ebi, K. L. & Rocklöv, J. Attributing mortality from extreme temperatures to climate change in Stockholm, Sweden. Nat. Clim. Chang. 3, 1050–1054 (2013).
Silva, R. A. et al. Global premature mortality due to anthropogenic outdoor air pollution and the contribution of past climate change. Environ. Res. Lett. 8, 034005 (2013).
Alonso, D., Bouma, M. J. & Pascual, M. Epidemic malaria and warmer temperatures in recent decades in an East African highland. Proc. Biol. Sci. 278, 1661–1669 (2011).
Head, J. R. et al. Effects of precipitation, heat, and drought on incidence and expansion of coccidioidomycosis in western USA: a longitudinal surveillance study. Lancet Planet. Health 6, e793–e803 (2022).
Harris, M. J. et al. Extreme precipitation, exacerbated by anthropogenic climate change, drove Peru’s record-breaking 2023 dengue outbreak. Preprint at medRxiv https://doi.org/10.1101/2024.10.23.24309838 (2024).
Kniesner, T. J., Viscusi, W. K., Woock, C. & Ziliak, J. P. The value of a statistical life: evidence from panel data. Rev. Econ. Stat. 94, 74–87 (2012).
Viscusi, W. K. The role of publication selection bias in estimates of the value of a statistical life. Am. J. Health Econ. 1, 27–52 (2015).
International Monetary Fund. Gross domestic product deflator for United States [NGDPDIXUSA]. Federal Reserve Bank of St. Louis https://fred.stlouisfed.org/series/NGDPDIXUSA (2025).
GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2100–2132 (2024).
Snow, R. W. et al. The prevalence of Plasmodium falciparum in sub-Saharan Africa since 1900. Nature 550, 515–518 (2017).
Bhatt, S. et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature 526, 207–211 (2015).
Gething, P. W. et al. Mapping Plasmodium falciparum mortality in Africa between 1990 and 2015. N. Engl. J. Med. 375, 2435–2445 (2016).
Carlson, C. J. & Carleton, T. carlsonlab/AttributableLosses: Publication plus corrected README (v2.1.1). Zenodo https://doi.org/10.5281/zenodo.15685967 (2025).
Haddaway, N. R., Page, M. J., Pritchard, C. C. & McGuinness, L. A. PRISMA2020: an R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 18, e1230 (2022).
Acknowledgements
We thank F. J. Colon-Gonzalez and C. Callahan for thoughtful conversations about health impact attribution. This project was supported by funding from the Wellcome Trust to C.J.C. and C.H.T.
Author information
Authors and Affiliations
Contributions
C.J.C. and D.M. designed the study. C.J.C., R.G., T.E.L., C.A.L., M.L.-S., M.A.N., S.J.R. and D.S.S. generated data. C.J.C., R.G. and T.C. contributed to data analysis and data visualization. C.J.C., D.M., R.G., R.F.S.-S., T.C., T.E.L., C.A.L., M.L.-S., M.A.N., S.J.R., D.S.S., M.C., M.N. and C.H.T. contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Climate Change thanks Ilan Noy and the other, anonymous, reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Geography of study scope and author affiliations.
Gray values indicate no studies were applicable. (Middle and bottom panel legends indicate the number of studies with at least one author, or lead author, with an affiliation listed in that country).
Extended Data Fig. 2 Results of the systematic literature review.
The PRISMA template was generated by the PRISMA2020 R Shiny app [ref. 55].
Supplementary information
Supplementary Information
Supplementary Text 1. Health impact attribution and litigation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Carlson, C.J., Mitchell, D., Gibb, R. et al. Health losses attributed to anthropogenic climate change. Nat. Clim. Chang. 15, 1052–1055 (2025). https://doi.org/10.1038/s41558-025-02399-7
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41558-025-02399-7
This article is cited by
-
Enduring impacts of El Niño on life expectancy in past and future climates
Nature Climate Change (2026)
-
Health risks of oil and gas development
Nature Reviews Nephrology (2026)