Abstract
Whether the risks of maternal and paternal suicide attempt during and after pregnancy differ remains unclear. Here, in this nationwide register-based study in Sweden (2,196,276 pregnancies), we defined the year before conception, pregnancy and the year after birth and estimated week-specific incidence rate ratios (IRRs). We identified 7,469 (1.39 per 1,000 person-years) suicide attempts among mothers and 8,338 (1.62 per 1,000 person-years) among fathers. Compared with the corresponding week in the preconception period, mothers had a lower risk of suicide attempt during and after pregnancy (with the lowest IRR of 0.14 (0.11–0.17) at first week postpartum); fathers’ risk of suicide attempt remained largely stable before childbirth, but a lower risk was observed during the first 10 postpartum weeks (IRRs ranging from 0.69 (0.58–0.81) to 0.91 (0.84–0.99)), followed by a higher risk in the later postpartum period (IRRs ranging from 1.10 (1.01–1.21) to 1.72 (1.33–2.24)). Compared with fathers, mothers had a lower risk of suicide attempt during and after pregnancy (for example, IRR of 0.22 (0.18–0.28) at first week postpartum). Compared with the general population, the sex difference of suicide attempt is reversed during and after pregnancy, suggesting pregnancy or childbirth may have a more pronounced association with suicide attempt among mothers than fathers.
Similar content being viewed by others
Main
Suicide is a public health concern that substantially affects families and societies1. Reducing suicide rates has been set out as a target by both the United Nation Sustainable Development Goals and the World Health Organization Global Mental Health Action Plan2. In most parts of the world, completed suicide is more common among men than women3,4, while for suicide attempts, the gender difference is reversed4. A better understanding of the sex/gender differences in suicide attempt, the strongest risk factor of completed suicide, may be informative to tailor gender-based strategies for suicide prevention.
For both women and men, transition into parenthood is a life-changing period that may substantially affect their mental health. Parental suicide attempt during the perinatal period is fortunately rare5,6, but is associated with severe health outcomes for the affected individual and their offspring7,8,9. Compared with fathers, mothers experience more physiological changes during the perinatal period10,11 and are more likely to be affected by perinatal depression12. However, mothers may also gain from the clinical monitoring in maternal care and the activated social support during pregnancy and after childbirth11,13. This may counterbalance vulnerabilities to suicide attempt, and even reverse the female excess in suicide attempt, during this period.
However, the knowledge on sex differences in parental suicide attempt during pregnancy or after childbirth is limited. Several studies have reported that childbirth was associated with a lower risk of suicide attempt and completed suicide among mothers14,15,16,17,18, although this association was not observed among those with severe psychiatric disorders19. Only one study estimated the prevalence of paternal suicide ideation and attempt in the antepartum and postpartum periods6, without comparing with a reference period. To our knowledge, no study has investigated how transition into parenthood may reshape sex differences in suicide attempt. To this end, we described and compared rates of maternal and paternal suicide attempts before, during and after pregnancy and investigated whether mothers and fathers differ in risk of suicide attempt in these time periods. While we recognize the diversity in contemporary families, we focused on heterosexual couples in the present study.
Results
We included 2,196,276 pregnancies from 1,236,816 mothers and 1,175,674 fathers (Supplementary Fig. 1). In the study sample, mothers were younger and had higher educational attainment but lower income than the fathers (P < 0.001; Table 1). In addition, mothers were more likely to have a history of depression and other psychiatric disorders or a history of suicide attempt (P < 0.001). During the follow-up of over 10 million person-years, we identified 7,469 (incidence rate (IR) of 1.39 per 1,000 person-years) suicide attempts among mothers and 8,338 (1.62 per 1,000 person-years) among fathers. Among mothers, IR of suicide attempt was 2.69, 0.74 and 0.85 per 1,000 person-years in the preconception, antepartum and postpartum period, respectively; among fathers, IR of suicide attempt was 1.88, 1.45 and 1.53 per 1,000 person-years in the preconception, antepartum and postpartum periods, respectively (Supplementary Table 1).
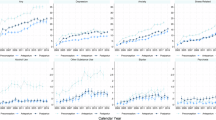
Secular trends in parental suicide attempt
For both mothers and fathers, the annual standardized incidence rate (SIR) of suicide attempts in the preconception and antepartum periods increased from 2001 to 2010 (adjusted P < 0.05), and decreased thereafter in the antepartum and postpartum periods (adjusted P < 0.05; Fig. 1 and Supplementary Table 2).
The incidence rate was standardized by distribution of age group of the accumulated person-years during follow-up. Locally weighted scatterplot smoothing (bandwidth 0.8) was used to estimate the trend (solid line), while the dots indicate the yearly incidence rates. The shaded areas indicate the 95% CI. P values for trend test are two-sided and adjusted for multiple comparison (Supplementary Table 2).
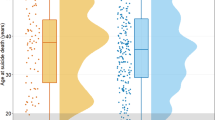
Sex differences in parental suicide attempt
Among mothers, the SIR by week was largely stable in the preconception period, slightly decreased during pregnancy and slightly increased throughout the postpartum period (adjusted P < 0.05; Fig. 2 and Supplementary Table 3). Among fathers, the SIR was largely stable over the three periods (adjusted P < 0.05; Fig. 2 and Supplementary Table 3).
The follow-up during pregnancy was censored at week 40 due to few subsequent cases. Incidence rates were standardized by distribution of age group and calendar period of the accumulated person-days during follow-up. Locally weighted scatterplot smoothing (bandwidth 0.8) was used to estimate the trend (solid line), while the dots indicate the weekly incidence rates. The shaded areas indicate the 95% CI. P values for trend test are two-sided and adjusted for multiple comparison (Supplementary Table 3).
Compared with the preconception period, there was a decreased risk of suicide attempts throughout the antepartum and postpartum periods among the mothers, with the lowest risk observed at first week postpartum, with an incidence rate ratio (IRR) of 0.14 (95% confidence interval (CI) 0.11–0.17) and adjusted P < 0.001 (Fig. 3 and Supplementary Table 4; parameter results are provided in the Supplementary Methods). Compared with corresponding weeks in the preconception period, the risk of paternal suicide attempt was similar during the antepartum period, significantly decreased during the first 10 weeks postpartum and increased in the later postpartum period (Fig. 3; statistics are provided in Supplementary Table 4).
The analyses are based on aggregated data from 2,196,276 pregnancies (1,236,816 mothers and 1,175,674 fathers). The follow-up during pregnancy was censored at week 40 due to few subsequent cases. The dots represent the actual IRRs, and the error bars represent their 95% CI. P values are two-sided and adjusted for multiple comparison (Supplementary Table 4). The dashed lines represent results when using restricted cubic spline with 4 knots, placed at 5th percentile, 35th percentile, 65th percentile and 95th percentile of distribution of weeks on the relevant x axes. The shaded areas indicate 95% CI of the smoothed results. Note that a logarithmic scale was used. The IRRs were adjusted for country of birth, age, calendar year, education level, civil status, category of income, primiparity, history of psychiatric disorders, history of suicide attempt and season, all derived at the start of each period.
Compared with expectant fathers, expectant mothers had a similar risk of suicide attempt throughout the preconception period after adjusting for factors potentially associated with suicide attempt—such as a history of psychiatric disorders and prior suicide attempts—whereas a decreased risk was observed during the antepartum and postpartum periods, with the lowest IRR noted during the first week postpartum (IRR 0.22, 95% CI 0.18–0.28, adjusted P < 0.001) (Fig. 4 and Supplementary Table 5; parameter results are provided in the Supplementary Methods). A similar pattern was seen for IRD; however, the largest IRD was seen at the 16th to 21st week antepartum.
The analyses are based on aggregated data from 2,196,276 pregnancies (1,236,816 mothers and 1,175,674 fathers). The follow-up during pregnancy was censored at week 40 due to few subsequent cases. The dots represent the actual IRRs and IRDs, and the error bars represent their 95% CI. P values are two-sided and adjusted for multiple comparison (Supplementary Table 5). The dashed lines represent results when using restricted cubic spline with 4 knots, placed at 5th percentile, 35th percentile, 65th percentile and 95th percentile of distribution of weeks on the relevant x axes. The shaded areas indicate 95% CI of the smoothed results. The IRRs and IRDs were adjusted for country of birth, age, calendar year, education level, civil status, category of income, primiparity, history of psychiatric disorders, history of suicide attempt and season, all derived at the start of each period.
Secondary analyses
An increasing trend of postpartum suicide attempt was indicated among adolescent fathers (aged 11–19 years) (IRR 1.06 (1.00–1.11), P = 0.037), but the association is no longer significant after adjusting for multiple comparison (adjusted P = 0.096). Meanwhile, IR among adolescent mothers was stable (IRR 1.00 (0.96–1.03), P = 0.891, adjusted P = 0.940) (Supplementary Fig. 2). In addition, we found a decreasing trend of suicide attempts from 2006 onwards among both fathers and mothers with and without depressive disorders (Supplementary Fig. 3 and Supplementary Table 6). However, this decreasing trend was driven mainly by individuals with a history of suicide attempt (Supplementary Fig. 4 and Supplementary Table 7). In addition, the pattern of weekly SIR was similar to main analysis when stratified by depressive disorders (Supplementary Fig. 5 and Supplementary Table 8) and history of suicide attempt (Supplementary Fig. 6 and Supplementary Table 9). The IRRs comparing antepartum and postpartum periods to preconception period were similar regardless of depressive disorders (Supplementary Fig. 7 and Supplementary Table 10) or history of suicide attempt (Supplementary Fig. 8 and Supplementary Table 11).
Overall, we identified 7,178 (45%) cases of suicide attempt by poisoning, 2,239 (14%) by cutting or piercing, and 330 (2%) by falling (Supplementary Table 12). Compared with fathers, the risk of suicide attempt by poisoning, cutting or piercing among mothers was significantly lower in most weeks in the antepartum and postpartum periods; there is a similar pattern in suicide attempt by falling, but only significant during the middle weeks of the antepartum and postpartum periods. Notably, a significantly higher risk of suicide attempt by poisoning was observed among mothers in the preconception period (Supplementary Fig. 9 and Supplementary Table 13). IRR calculated by comparing antepartum and postpartum periods to average IR of preconception period yielded largely similar results on trends, whereas the paternal IRR was no longer statistically significant (Supplementary Fig. 10 and Supplementary Table 14). Furthermore, when excluding week 53 from the analysis, the rise in paternal absolute IR in late postpartum period was less pronounced, yet the CIs overlapped with those from the primary analysis (Supplementary Fig. 11 and Supplementary Table 15) whereas the IRRs changed minimally (Supplementary Figs. 12 and 13 and Supplementary Tables 16 and 17).
Discussion
In this nationwide cohort including 2,196,276 pregnancies from 1,236,816 mothers and 1,175,674 fathers in Sweden, we found a lower IR of suicide attempt among mothers compared to fathers during and after pregnancy, which is opposite to the sex differences in the general population. Compared with the year before pregnancy, mothers had a decreased risk of suicide attempt throughout pregnancy and one year postpartum. However, fathers had a decreased risk after childbirth, and a higher risk of suicide attempt in the later postpartum period only when compared with corresponding weeks in preconception year.
Secular trends of suicide attempt
Three studies, all from the USA, reported on the secular trend of perinatal suicide attempt among mothers20,21,22. Two studies reported an increasing rate of perinatal suicide attempt from 2006 to 201820,21, whereas one reported a stable trend between 2006 and 201222. We did not identify any studies that reported on the secular trend of paternal suicide attempts. In our study, in some periods, SIR of perinatal suicide attempt increased from 2001 to 2010 but decreased afterwards among both mothers and fathers. In 2010, Sweden launched a national programme for maternal postpartum depression screening23. Such screening may reasonably result in early detection of depression and prevention of suicide attempts among postpartum mothers. However, we did not find a drop in SIR specific to the postpartum period among mothers, indicating that other factors are at play. Sweden has also implemented a national programme for suicide prevention since 2008, including distributing knowledge on suicide-reducing strategies24. This may contribute to the recent decline in the risk of suicide attempt in the general population in Sweden25, as well as in parents in the perinatal period. In addition, childbirth rate in Sweden has declined since 201026, possibly due to financial uncertainty and labour market insecurity27. We hypothesize that individuals who were healthier and economically more advantaged may have been more likely to choose to engage in pregnancy during this period than those less advantaged.
Teenage pregnancy has been linked to several adverse health outcomes among adolescent mothers28,29. Studies have reported a decreasing number of children born to teenage mothers30, but a stable or slight increase in teenage pregnancy rates in Sweden31,32. Our results indicated an increasing rate of postpartum suicide attempt over calendar time among adolescent fathers, although the association is no longer significant after adjusting for multiple comparison. No increasing trend was indicated for adolescent mothers. Further research is needed to focus on adolescent fathers and to explore sex differences in postpartum mental health among teenage parents.
Sex difference in preconceptional suicide attempt
Preconception is considered as a relative healthy period when expectant mothers plan for pregnancy33, and possibly for fathers as well. Our study observed a largely stable SIR of suicide attempt over the weeks in preconception period. This suggests such ‘health bias’ may not notably affect the weekly trend of suicide attempts before pregnancy. In addition, we found a similar risk of suicide attempt among mothers and fathers over weeks throughout the preconception period. The trend of weekly SIRs in preconception period among fathers somewhat echoed the trend among mothers. This is consistent with previous literature reporting a positive link on suicide risk between spouses, possibly due to stress brought by suicide of a partner, or shared environmental factors between the cohabitating partners or selective mating34,35.
Sex differences in antepartum suicide attempt
Few studies reported a decreased rate of suicide attempt, or completed suicide, among women during pregnancy compared with the general female population14,15. However, preexisting risk factors of suicide can also affect the chance of entering into motherhood36. Such confounders were not addressed sufficiently in earlier studies. Similarly to a study in Canada16, our study found a decreased risk of maternal suicide attempt during pregnancy, when comparing the risk of suicide attempt during pregnancy with the period before pregnancy, which serves as a more valid comparison group in terms of controlling for confounding. In addition, our results also indicated a similar risk of paternal suicide attempt during antepartum period when compared with corresponding weeks in the preconception period. Our results suggest that, compared with corresponding weeks in the preconception period, the risk of suicide attempt decreased during pregnancy among mothers36, but not among fathers. Despite this, maternal perinatal suicide may involve more violent suicide methods, as it may represent a more severe psychopathology37,38, and parental suicide attempts are associated with mental health problems in their offsprings7. Therefore, close surveillance on suicidality among expectant parents remains critical.
Notably, the reduction in risk of suicide attempt during the antepartum period was observed only among mothers. It is plausible that mothers have a better support network than fathers during pregnancy39. For example, mothers usually gain support from female relatives, whereas fathers often turn to colleagues at work40. Alternatively, mothers have more contacts with health professionals than fathers during pregnancy. Maternal psychiatric symptoms may be detected earlier, demonstrating the potential benefit of maternity care41. In addition, progesterone has anxiolytic effects, and studies on suicidality across menstrual cycles have shown that women tend to commit suicide at premenstrual and menstrual phases, when the progesterone level is low42,43. It is plausible that the increased level of progesterone during pregnancy protects mothers against suicide. Although more research is needed to understand the male excess in suicide attempt during pregnancy, clinicians should recognize that female excess in suicide attempt in the general population is reversed to male excess during pregnancy.
Sex difference in postpartum suicide attempt
Throughout the postpartum period, we found a slightly increasing SIR of suicide attempts among mothers. Adjusting to demands of early parenting creates stress for new parents44, whereas current postpartum care does not seem to provide enough information on early parenthood45. However, more research is needed to further understand the rebound of suicide attempt postpartum.
Compared with the preconception period, mothers still had a decreased risk of suicide attempt throughout the postpartum period, whereas fathers had a decreased risk only in the first 10 weeks postpartum. These differences may be related to the fact that mothers are usually the primary caregivers during the first months and may therefore develop closer emotional bonds with their children than fathers, which in turn may buffer against poor mental health in mothers36. In addition, in some qualitative studies, fathers claimed that difficulties in balancing needs of family and work were important sources of stress in the year after birth46. In addition, fathers may experience hormonal and neurofunctional alterations after childbirth47, but more research is needed to understand whether these biological changes are associated with paternal suicide attempt postpartum. As mental health screening is not in place for fathers yet, health providers may stay alert of paternal risk during the postpartum period.
Strengths and limitations
Our study is a nationwide population-based cohort study, with relatively precise definition of the exposure periods based on delivery date and gestational age. The large sample size provided the possibility to study the temporal pattern of suicide attempt among fathers and mothers in a weekly manner, and the comparison with the preconception period allowed us to minimize confounding by parenthood. However, our study has several limitations. First, as the Medical Birth Register (MBR) records only live births and stillbirths that reach 22 weeks of gestation, we cannot assess suicide attempts in pregnancies terminated before 22 weeks of gestation. Second, we may have included some cases of non-suicidal self-harm. However, such events are often milder compared with suicide attempts and are less likely to be recorded in registers. Third, we may have included some cases of fatal suicide if the suicide attempt led to death several days later. In addition, as we can only identify fathers who were alive at least at conception and mothers who were alive by childbirth, we were unable to study completed suicide in the preconception period for both parents or in antepartum period among mothers. Fourth, we had preconception year as the reference period, which may be a mentally and physically healthier period compared with other periods in life33. We would thus expect stronger associations for childbirth with suicide attempts if compared with the general population. Sixth, due to data availability, we were unable to identify individuals whose gender does not align with sex assigned at birth. Although our results may not be generalizable to these groups, further research is needed. Seventh, as Sweden is a high-income country with family-friendly policies (for example, free prenatal care, paid parental leave for both parents and other generous welfare benefits during and after pregnancy), our results may generalize only to countries with similar healthcare systems and social welfare.
In conclusion, our results illustrate a lower risk of suicide attempt among both mothers and fathers after childbirth, supporting that childbirth may be a protective factor against suicidality among mothers. Our study also illustrates that the well-established female excess in suicide attempt in the general population is reversed during and after pregnancy. Although perinatal suicidal events are relatively rare, clinical action is needed due to the costly consequence in contrast to the preventable nature. Clinicians may take opportunities of the current scheme of maternal and child health services to identify high-risk individuals, implement suicide risk assessment and enhance suicide prevention strategies for both mothers and fathers.
Methods
Study population and design
We conducted a prospective population-based cohort study based on Swedish registers. The Swedish MBR was established in 1973 and includes antenatal and obstetric records for 98% of all births in Sweden48. The data from the MBR included year and month, but not date, at delivery due to the data holder’s policy. Due to the need of precise timeline for our statistical analyses, we imputed the date at delivery using a validated algorithm based on admission and discharge dates to delivery wards together with parity and mode of delivery (Supplementary Methods). Gestational length was estimated primarily on the basis of the ultrasound assessment performed around the 18th week of gestation48. We used delivery date and length of gestation to estimate the start of pregnancy and to define three time windows: 1 year before pregnancy (preconception period), during pregnancy (antepartum period) and 1 year after delivery (postpartum period). This study is approved by the Swedish Ethical Review Authority (2018/1515-31 and 2021-02775). Informed consent is waived for register-based studies in Sweden.
In Sweden, sex is assigned at birth, although a small number of individuals medically and legally changed their gender later in life49. Based on the MBR, we first identified 1,258,824 women and their 2,263,596 pregnancies during 2001–2021 in Sweden. After excluding women who had an invalid personal identification number, missing information on length of gestation, conflicting information (for example, died before start of pregnancy or delivery date) and erroneous records, 1,236,816 women and 2,196,276 pregnancies remained in the analysis (Supplementary Fig. 1). The Multi-Generation Register (MGR) provides information on familial linkages for individuals born since 1932 in Sweden50 and was used to identify fathers who share biological children with these women. Because fathers were not reported for 2% of children in the MGR, we complemented the identification of fathers as partners of women who reported as cohabitating with ‘the-father-to-be’ at their first antenatal visit, based on the MBR. Among the 1,213,034 fathers identified, we excluded those who had invalid personal identification numbers or conflicting information, leaving 1,175,674 fathers in the analysis (Supplementary Fig. 1).
Participants were followed from 1 year before pregnancy, moving to Sweden, or 1 January 2001, whichever came later, until 1 year after delivery, death, moving out of Sweden, or 31 December 2021, whichever came earlier.
Measures
Ascertainment of suicide attempt
We identified diagnoses of suicide attempt from the National Patient Register (NPR), both inpatient and outpatient register, using the International Classification of Diseases (ICD) codes. Consistent with previous studies51,52, we included both definite (ICD8/9: E950-E959; ICD10: X60-X84) and indeterminate (ICD8/9: E980-E989; ICD10: Y10-Y34) suicide attempts (Supplementary Table 18). The first suicide attempt during each period was considered as the outcome. Any suicide attempt before the start of each period was used as a covariate. The positive predictive value for injuries in the NPR is 95% (ref. 53), but no validation study has been specifically conducted for suicide attempt in Swedish registers.
Ascertainment of covariates
Covariates were derived for mothers and fathers respectively, at the start of each period. Demographic factors, including birth year and country of birth, were collected from the Total Population Register (TPR). Proxies of socioeconomic status, including education level and income, were obtained from the Longitudinal Integration Database for Health Insurance and Labor Market Studies (LISA). Income was further classified into five quantiles, with quantile 1 representing the lowest, that is the 0–20th percentile of the income distribution. Information on civil status was collected from the MBR and the TPR. From MBR, for mothers we collected data on parity, and for fathers we collected data on parity of the woman they shared a biological child with. The national guideline in Sweden recommends that (semi-)structured diagnostic interviews be carried out when diagnosing psychiatric disorders54. We identified history of any psychiatric disorder using ICD-8/9/10 codes from NPR; to supplement with psychiatric diagnoses made in primary care by general practitioners, we also retrieved information on filled psychotropic prescriptions using Anatomical Therapeutic Chemical codes based on the Prescribed Drug Register (Supplementary Table 18). Previous studies suggest that the validity of the diagnoses of psychiatric disorders in NPR and primary care is good55,56,57,58,59. As Sweden launched in 2010 a national screening programme for maternal perinatal depression, which may influence sex differences in suicide attempt among individuals with depressive disorders, we also categorized psychiatric disorders into depressive disorders and other psychiatric disorders.
Statistical analyses
Basic characteristics between mothers and fathers were compared using the χ2 test. In the analysis of the secular trend in risk of suicide attempt, we first calculated annual sex-specific IRs of suicide attempt during preconception, antepartum and postpartum periods, as the number of first suicide attempt divided by accumulated person-years. Then, we calculated SIRs through direct standardization, using the distribution of age group of the accumulated person-years during follow-up between 2001 and 2021 as the standard. The 95% CI for SIR was calculated on the basis of the standard error60 and two-sided Z value (SIR ± 1.96 × standard error). Locally weighted scatterplot smoothing, with 0.8 as the bandwidth, was used to smooth the SIR and its 95% CIs61. As Sweden launched a national screening programme for maternal depression in 2010, for each period and sex, we examined the association between calendar year and IR of suicide attempt before/at and after 2010 separately and adjusted for groups of age. As a total of 12 comparisons were performed, we adjusted P values using the Benjamini–Hochberg method, to account for multiple testing62.
As pregnancy length is measured by week in clinical practice, in the analysis of sex differences in suicide attempt, we first calculated sex-specific IRs of suicide attempt by week in the preconception, antepartum and postpartum year. We then estimated SIR through direct standardization, using the distribution of age group and calendar period of the accumulated person-days during follow-up between 2001 and 2021 as the standard. The 95% CI for SIR was calculated on the basis of the standard error60 and two-sided Z value (SIR ± 1.96 × standard error). Locally weighted scatterplot smoothing, with 0.8 as the bandwidth, was used to smooth the SIR and its 95% CI. In addition, for each period and sex, we performed Poisson regression to examine the association between week and IR of suicide attempts, when adjusting for group of age and calendar year. We applied the Benjamini–Hochberg method to adjust P values over six comparisons.
To compare the week-specific IRs of suicide attempt in the antepartum and postpartum periods with corresponding weeks in the preconception period, we used multivariable Poisson regression to estimate the IRR and 95% CI of maternal and paternal suicide attempt. Comparing weekly rates allows us to control for season, which is a potential confounder to the studied association63. IRRs were adjusted for country of birth, age, calendar year, education level, civil status, category of income, primiparity, history of psychiatric disorders, history of suicide attempt and season, all derived at the start of each period. To investigate a potential nonlinear relationship between IRRs and week, we applied restricted cubic spline on week, and placed 4 knots at the 5th percentile, 35th percentile, 65th percentile and 95th percentile of distribution of weeks on the relevant x axes64, to visualize weekly IRRs. The parameterization can be found in the Supplementary Methods. The 95% CI was calculated on the basis of the standard error estimated from the delta method and z critical value. Due to small number of events beyond week 40 in the antepartum period, we did not test IRRs over week 40 in the antepartum period; therefore, the Benjamini–Hochberg method was applied to adjust for multiple comparisons over a total of 186 tests (40 in the antepartum period, and 53 in the postpartum period for each sex).
Similarly, to illustrate sex differences in the risk of suicide attempts during each period, we used multivariable Poisson regression to estimate the IRR of suicide attempts, comparing mothers with fathers on a weekly basis from preconception through the postpartum period. To shed light on absolute sex differences, we further used Poisson regression to estimate the weekly incidence rate difference (IRD)65. To visualize IRRs and IRDs, we also applied restricted cubic spline on week, and placed 4 knots at the 5th percentile, 35th percentile, 65th percentile and 95th percentile of distribution of weeks on the relevant x axes. The parameterization can be found in the Supplementary Methods. The 95% CI was calculated on the basis of the standard error estimated from the delta method and z value. The models were adjusted for country of birth, age, calendar year, education level, civil status, category of income, parity, history of psychiatric disorders, history of suicide attempt and season, all derived at the start of each period. For both IRR and IRD, the Benjamini–Hochberg method was applied to adjust for multiple comparisons over a total of 146 tests (53 weeks in the preconception and postpartum periods, respectively, and 40 weeks in the antepartum period).
Secondary analyses
We estimated the trend in parental suicide attempt by age group. We also performed Poisson regression to test the secular trend. In addition, to illustrate potential risk modification by depressive disorders and history of suicide attempt, we stratified analyses on time-dependent depressive disorders as well as history of suicide attempt. Furthermore, to shed light on potential prevention strategies, we also identified common methods for suicide attempts and calculated method-specific IRRs comparing mothers with fathers by the three most common suicide methods. In addition, because the SIR in the preconception period fluctuated over weeks, we also estimated IRR comparing the antepartum and the postpartum to the preconception period, using the average IR in the preconception year as the reference. Finally, due to the small number of person-years, we excluded week 53 from the analyses, calculated the SIR by week, and estimated IRRs comparing antepartum and postpartum periods with preconception, as well as comparing mothers with fathers during preconception and postpartum. In all secondary analyses, we applied the Benjamini–Hochberg method to adjust for multiple comparisons.
Data were cleaned using SAS, version 9.4 (SAS Institute) and analysed using Stata 18.0 (STATA). To account for the false discovery rate, we applied the Benjamini–Hochberg method to adjust P values. A two-sided adjusted P < 0.05 was considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The Public Access to Information and Secrecy Act in Sweden prohibits individual-level data being publicly available. Researchers who are interested in replicating this study can apply for individual-level data from TPR, MGR and LISA Sweden (https://www.scb.se/en/services/ordering-data-and-statistics/ordering-microdata/). Data on patient health from the Swedish MBR, NPR and Prescribed Drug Register can be requested through Socialstyrelsen (https://www.socialstyrelsen.se/en/statistics-and-data/registers/).
Code availability
Analysis coding is available via GitHub at https://github.com/yihuiyang2/ParentalSuicide.
References
Turecki, G. et al. Suicide and suicide risk. Nat. Rev. Dis. Prim. 5, 1–22 (2019).
WHO launches new resources on prevention and decriminalization of suicide. WHO https://www.who.int/news/item/12-09-2023-who-launches-new-resources-on-prevention-and-decriminalization-of-suicide (2023).
Schmidtke, A. et al. Attempted suicide in Europe: rates, trends and sociodemographic characteristics of suicide attempters during the period 1989–1992. Results of the WHO/EURO Multicentre Study on Parasuicide. Acta Psychiatr. Scand. 93, 327–338 (1996).
Miranda-Mendizabal, A. et al. Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Int J. Public Health 64, 265–283 (2019).
Rao, W. W. et al. Worldwide prevalence of suicide attempt in pregnant and postpartum women: a meta-analysis of observational studies. Soc. Psychiatry Psychiatr. Epidemiol. 56, 711–720 (2021).
Quevedo, L. et al. Risk of suicide and mixed episode in men in the postpartum period. J. Affect. Disord. 132, 243–246 (2011).
Ortin-Peralta, A. et al. Parental suicide attempts and offspring mental health problems in childhood and adolescence. J. Child Psychol. Psychiatry 64, 886–894 (2023).
Gandhi, S. G. et al. Maternal and neonatal outcomes after attempted suicide. Obstet. Gynecol. 107, 984–990 (2006).
Flint, C., Larsen, H., Nielsen, G. L., Olsen, J. & Sørensen, H. T. Pregnancy outcome after suicide attempt by drug use: a Danish population-based study. Acta Obstet. Gynecol. Scand. 81, 516–522 (2002).
Munk-Olsen, T., Laursen, T. M., Pedersen, C. B., Mors, O. & Mortensen, P. B. New parents and mental disorders: a population-based register study. JAMA 296, 2582–2589 (2006).
Sundström Poromaa, I., Comasco, E., Georgakis, M. K. & Skalkidou, A. Sex differences in depression during pregnancy and the postpartum period. J. Neurosci. Res. 95, 719–730 (2017).
Cameron, E. E., Sedov, I. D. & Tomfohr-Madsen, L. M. Prevalence of paternal depression in pregnancy and the postpartum: an updated meta-analysis. J. Affect. Disord. 206, 189–203 (2016).
Metzger, S. & Gracia, P. Gender differences in mental health following the transition into parenthood: longitudinal evidence from the UK. Adv. Life Course Res. 56, 100550 (2023).
Weiss, H. B. Pregnancy-associated injury hospitalizations in Pennsylvania, 1995. Ann. Emerg. Med. 34, 626–636 (1999).
Greenblatt, J. F., Dannenberg, A. L. & Johnson, C. J. Incidence of hospitalized injuries among pregnant women in Maryland, 1979–1990. Am. J. Prev. Med. 13, 374–379 (1997).
Mota, N. P. et al. Mental disorders and suicide attempts in the pregnancy and postpartum periods compared with non-pregnancy: a population-based study. Can. J. Psychiatry 64, 482–491 (2019).
Lysell, H. et al. Maternal suicide—Register based study of all suicides occurring after delivery in Sweden 1974–2009. PLoS ONE 13, e0190133 (2018).
Appleby, L. Suicide during pregnancy and in the first postnatal year. Br. Med. J. 302, 137–140 (1991).
Appleby, L., Mortensen, P. B. & Faragher, E. B. Suicide and other causes of mortality after post-partum psychiatric admission. Br. J. Psychiatry 173, 209–211 (1998).
Admon, L. K. et al. Trends in suicidality 1 year before and after birth among commercially insured childbearing individuals in the United States, 2006–2017. JAMA Psychiatry 78, 171–176 (2021).
Schiff, M. A. & Grossman, D. C. Adverse perinatal outcomes and risk for postpartum suicide attempt in Washington State, 1987–2001. Pediatrics 118, e669–e675 (2006).
Zhong, Q. Y. et al. Suicidal behavior-related hospitalizations among pregnant women in the United States, 2006–2012. Arch. Women’s Ment. Health 19, 463–472 (2016).
Bränn, E. et al. Who do we miss when screening for postpartum depression? A population-based study in a Swedish region. J. Affect. Disord. 287, 165–173 (2021).
Brochure for the national action programme for suicide prevention. Public Health Agency of Sweden (Folkhälsomyndigheten) https://www.regionkronoberg.se/contentassets/d58d0c91a5c24ff4abcdbe566c6da697/nationellt_handlingsprogram_suicidprevention_16001_webb.pdf (2016).
Suicide attempts in Sweden. National Centre for Suicide Research and Prevention https://ki.se/en/nasp/suicide-attempts-in-sweden (2025).
Childbirth continues downwards—lowest in 20 years. Statistikmyndigheten SCB https://www.scb.se/pressmeddelande/barnafodandet-fortsatter-nedat--lagsta-pa-20-ar/ (2023).
Comolli, C. L. et al. Beyond the economic gaze: childbearing during and after recessions in the Nordic countries. Eur. J. Popul. 37, 473–520 (2021).
Scholl, T. O. et al. Young maternal age and parity. Influences on pregnancy outcome. Ann. Epidemiol. 2, 565–575 (1992).
Rah, J. H. et al. Pregnancy and lactation hinder growth and nutritional status of adolescent girls in rural Bangladesh. J. Nutr. 138, 1505–1511 (2008).
Age of parents in Sweden. Statistikmyndigheten SCB https://www.scb.se/hitta-statistik/sverige-i-siffror/manniskorna-i-sverige/foraldrars-alder-i-sverige/ (2025).
McKay, A. & Barrett, M. Trends in teen pregnancy rates from 1996–2006: a comparison of Canada, Sweden, U.S.A., and England/Wales. Can. J. Hum. Sex. 19, 43–52 (2010).
Sedgh, G., Finer, L. B., Bankole, A., Eilers, M. A. & Singh, S. Adolescent pregnancy, birth, and abortion rates across countries: levels and recent trends. J. Adolesc. Health 56, 223–230 (2015).
Khan, N. N., Boyle, J. A., Lang, A. Y. & Harrison, C. L. Preconception health attitudes and behaviours of women: a qualitative investigation. Nutrients 11, 1490 (2019).
Agerbo, E. Risk of suicide and spouse’s psychiatric illness or suicide: nested case–control study. Br. Med. J. 327, 1025–1026 (2003).
Jang, J. et al. Risks of suicide among family members of suicide victims: a nationwide sample of South Korea. Front. Psychiatry 13, 995834 (2022).
Dehara, M. et al. Parenthood is associated with lower suicide risk: a register‐based cohort study of 1.5 million Swedes. Acta Psychiatr. Scand. 143, 206–215 (2021).
Esscher, A. et al. Suicides during pregnancy and 1 year postpartum in Sweden, 1980–2007. Br. J. Psychiatry 208, 462–469 (2016).
Khalifeh, H., Hunt, I. M., Appleby, L. & Howard, L. M. Suicide in perinatal and non-perinatal women in contact with psychiatric services: 15 year findings from a UK national inquiry. Lancet Psychiatry 3, 233–242 (2016).
Jungmarker, E. B., Lindgren, H. & Hildingsson, I. Playing second fiddle is okay—Swedish fathers’ experiences of prenatal care. J. Midwifery Women’s Health 55, 421–429 (2010).
Deave, T., Johnson, D. & Ingram, J. Transition to parenthood: the needs of parents in pregnancy and early parenthood. BMC Pregnancy Childbirth 8, 30 (2008).
Carcel, C. et al. A life-course approach to tackling noncommunicable diseases in women. Nat. Med. 30, 51–60 (2024).
Ross, J. M. et al. Predicting acute changes in suicidal ideation and planning: a longitudinal study of symptom mediators and the role of the menstrual cycle in female psychiatric outpatients with suicidality. Am. J. Psychiatry 181, 57–67 (2024).
Baca-Garcia, E. et al. Suicide attempts among women during low estradiol/low progesterone states. J. Psychiatr. Res. 44, 209–214 (2010).
Gay, C. L., Lee, K. A. & Lee, S. Y. Sleep patterns and fatigue in new mothers and fathers. Biol. Res Nurs. 5, 311–318 (2004).
Ellberg, L., Högberg, U. & Lindh, V. We feel like one, they see us as two’: new parents’ discontent with postnatal care. Midwifery 26, 463–468 (2010).
Johansson, M., Benderix, Y. & Svensson, I. Mothers’ and fathers’ lived experiences of postpartum depression and parental stress after childbirth: a qualitative study. Int J. Qual. Stud. Health Well-being. 15, 1722564 (2020).
Sobral, M. et al. Neurobiological correlates of fatherhood during the postpartum period: a scoping review. Front. Psychol. 13, 745767 (2022).
Cnattingius, S. et al. The Swedish Medical Birth Register during five decades: documentation of the content and quality of the register. Eur. J. Epidemiol. 38, 109–120 (2023).
Determination of sex. Socialstyrelsen https://www.socialstyrelsen.se/om-socialstyrelsen/organisation/rad-och-namnder/rattsliga-radet/konstillhorighet/ (2019).
Ekbom, A. The Swedish Multi-Generation Register. Methods Mol. Biol. 675, 215–220 (2011).
Tidemalm, D., Långström, N., Lichtenstein, P. & Runeson, B. Risk of suicide after suicide attempt according to coexisting psychiatric disorder: Swedish cohort study with long term follow-up. Br. Med. J. 337, a2205 (2008).
Yu, H. et al. Perinatal depression and risk of suicidal behavior. JAMA Netw. Open. 7, e2350897 (2024).
Bergström, M. F., Byberg, L., Melhus, H., Michaelsson, K. & Gedeborg, R. Extent and consequences of misclassified injury diagnoses in a national hospital discharge registry. Inj. Prev. 17, 108–113 (2011).
National guidelines for care for depression and anxiety disorders. Socialstyrelsen https://www.socialstyrelsen.se/contentassets/5e4ef79d53d34793b4119029c1253bff/2021-4-7339.pdf (2021).
Fazel, S. et al. Depression and violence: a Swedish population study. Lancet Psychiatry 2, 224–232 (2015).
Meier, S. M. et al. Secondary depression in severe anxiety disorders: a population-based cohort study in Denmark. Lancet Psychiatry 2, 515–523 (2015).
Kendler, K. S., Maes, H. H., Sundquist, K., Ohlsson, H. & Sundquist, J. Genetic and family and community environmental effects on drug abuse in adolescence: a Swedish national twin and sibling study. Am. J. Psychiatry 171, 209–217 (2014).
Hollander, A. C. et al. Validation study of randomly selected cases of PTSD diagnoses identified in a Swedish regional database compared with medical records: is the validity sufficient for epidemiological research? BMJ Open 9, e031964 (2019).
Sundquist, J., Ohlsson, H., Sundquist, K. & Kendler, K. S. Common adult psychiatric disorders in Swedish primary care where most mental health patients are treated. BMC Psychiatry 17, 235 (2017).
Cochran WG. Sampling Techniques 3rd edn (Wiley, 1977).
Jacoby, W. G. Loess:: a nonparametric, graphical tool for depicting relationships between variables. Elect. Stud. 19, 577–613 (2000).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Series B 57, 289–300 (1995).
To, S., Messias, E., Burch, L. & Chibnall, J. Seasonal variation in suicide: age group and summer effects in the United States (2015–2020). BMC Psychiatry 24, 856 (2024).
Harrell, F. E. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis (Springer, 2001).
Falcaro, M., Newson, R. B. & Sasieni, P. Stata tip 146: using margins after a Poisson regression model to estimate the number of events prevented by an intervention. Stata J. https://doi.org/10.1177/1536867X221106437 (2022).
Acknowledgements
This work is supported by the scholarship from the China Scholarship Council (no. 202106100010 to Y.Y.), grant 2020-01003 from the Swedish Research Council (Vetenskapsrådet) (to D.L.), grants 2020-00971 and 2023-00399 from the Swedish Research Council for Health, Working Life, and Welfare (FORTE) (to D.L.) and a grant from Karolinska Institutet Strategic Research Area in Epidemiology and Biostatistics (to D.L.). The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Funding
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
Y.Y. and D.L. conceived of the study and analysed the data. Y.Y. drafted the paper. All authors interpreted the results, reviewed the paper and approved the decision to submit the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks Luciana Á. de Ávila Quevedo, Luule Sakkeus and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Methods and Figs. 1–13.
Supplementary Tables
Supplementary Tables 1–18.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, Y., Bränn, E., Fransson, E. et al. Sex difference in parental risk of suicide attempt during and after pregnancy in Sweden. Nat Hum Behav (2025). https://doi.org/10.1038/s41562-025-02311-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41562-025-02311-5