Abstract
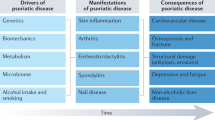
Plaque psoriasis is a chronic, immune-mediated inflammatory skin disease that has considerable effects on patients’ physical, psychological and social well-being. It is strongly influenced by genetic predisposition, with HLA-C*06:02 showing the strongest association, particularly in those with early-onset disease. Additional susceptibility loci, including IL23A, IL12B and IL17RA, are linked to dysregulation of the IL-23–T helper 17 axis, which contributes to chronic inflammation and keratinocyte hyperproliferation. Plaque psoriasis is frequently associated with psoriatic arthritis and other comorbidities, such as cardiovascular disease, metabolic syndrome and psychiatric disorders, all of which contribute to increased morbidity and mortality. Management strategies are tailored to disease severity and the presence of comorbidities. For mild disease, topical therapies remain the first-line treatment, including corticosteroids, vitamin D analogues and topical calcineurin inhibitors. New non-steroidal agents, such as topical PDE4 and aryl hydrocarbon receptor agonists, offer additional options. In moderate-to-severe disease, oral systemic therapies, such as methotrexate, ciclosporin, acitretin, apremilast and deucravacitinib, provide a range of immunomodulatory effects. Biologic therapies targeting TNF, IL-17, IL-23 and IL-12/23 have demonstrated high efficacy in improving both cutaneous and systemic inflammation. Current research on systemic therapies is focused on the development of additional inhibitors of the Tyk2 pathway and inhibitors to IL-23 receptor, IL-17, and TNF. Early screening for psoriatic arthritis, proactive cardiovascular risk reduction and multidisciplinary care are crucial to optimizing long-term outcomes. Ongoing research continues to advance precision medicine approaches, with the goal of enhancing treatment durability and improving quality of life for individuals living with psoriasis.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Armstrong, A. W. & Read, C. Pathophysiology, clinical presentation, and treatment of psoriasis: a review. JAMA 323, 1945–1960 (2020). This comprehensive review details the pathogenesis, clinical presentation and diagnostic approach, comorbidities and risk factors, and treatment approach for psoriasis.
Armstrong, A. W. et al. Patient perspectives on psoriatic disease burden: results from the Global Psoriasis and Beyond Survey. Dermatology 239, 621–634 (2023).
Armstrong, A. W. et al. Psoriasis prevalence in adults in the United States. JAMA Dermatol. 157, 940–946 (2021).
Parisi, R. et al. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ 369, m1590 (2020). This systematic review and meta-analysis applies modelling to generate global, regional and country-specific prevalence estimates for psoriasis.
Pérez-Chada, L. M. et al. Patient-reported outcome measures for health-related quality of life in patients with psoriasis: a systematic review. JAMA Dermatol. 160, 550–563 (2024).
Telfer, N. R. The role of streptococcal infection in the initiation of guttate psoriasis. Arch. Dermatol. 128, 39 (1992).
Mallbris, L. et al. Psoriasis phenotype at disease onset: clinical characterization of 400 adult cases. J. Invest. Dermatol. 124, 499–504 (2005).
Ko, H. C., Jwa, S. W., Song, M., Kim, M. B. & Kwon, K. S. Clinical course of guttate psoriasis: long-term follow-up study. J. Dermatol. 37, 894–899 (2010).
Sbidian, E. et al. Respiratory virus infection triggers acute psoriasis flares across different clinical subtypes and genetic backgrounds. Br. J. Dermatol. 181, 1304–1306 (2019).
Navarini, A. A. et al. European consensus statement on phenotypes of pustular psoriasis. J. Eur. Acad. Dermatol. Venereol. 31, 1792–1799 (2017).
Choon, S. E. et al. International consensus definition and diagnostic criteria for generalized pustular psoriasis from the International Psoriasis Council. JAMA Dermatol. 160, 758–768 (2024).
Boyd, A. S. & Menter, A. Erythrodermic psoriasis. J. Am. Acad. Dermatol. 21, 985–991 (1989).
Gupta, R., Debbaneh, M. G. & Liao, W. Genetic epidemiology of psoriasis. Curr. Dermatol. Rep. 3, 61–78 (2014).
Feng, B. J. et al. Multiple loci within the major histocompatibility complex confer risk of psoriasis. PLoS Genet. 5, e1000606 (2009).
Johnston, A. et al. Susceptibility-associated genetic variation at IL12B enhances Th1 polarization in psoriasis. Hum. Mol. Genet. 22, 1807–1815 (2013).
Gudjonsson, J. E. & Johnston, A. Current understanding of the genetic basis of psoriasis. Expert. Rev. Clin. Immunol. 5, 433–443 (2009).
Dand, N. et al. Psoriasis and genetics. Acta Derm. Venereol. 100, 55–65 (2020).
Dand, N. et al. GWAS meta-analysis of psoriasis identifies new susceptibility alleles impacting disease mechanisms and therapeutic targets. Nat. Commun. 16, 2051 (2025).
Yan, D., Ahn, R., Leslie, S. & Liao, W. Clinical and genetic risk factors associated with psoriatic arthritis among patients with psoriasis. Dermatol. Ther. 8, 593–604 (2018).
Griffiths, C. E. M., Armstrong, A. W., Gudjonsson, J. E. & Barker, J. Psoriasis. Lancet 397, 1301–1315 (2021).
Mrowietz, U., Lauffer, F., Sondermann, W., Gerdes, S. & Sewerin, P. Psoriasis as a systemic disease. Dtsch. Arztebl. Int. 121, 467–472 (2024).
World Health Organization. Global report on psoriasis. WHO www.who.int/publications/i/item/global-report-on-psoriasis (2016).
Mease, P. & Goffe, B. S. Diagnosis and treatment of psoriatic arthritis. J. Am. Acad. Dermatol. 52, 1–19 (2005).
Yeung, H. et al. Psoriasis severity and the prevalence of major medical comorbidity: a population-based study. JAMA Dermatol. 149, 1173–1179 (2013).
Armstrong, A. W., Harskamp, C. T., Ledo, L., Rogers, J. H. & Armstrong, E. J. Coronary artery disease in patients with psoriasis referred for coronary angiography. Am. J. Cardiol. 109, 976–980 (2012).
Armstrong, A. W. et al. Psoriasis and risk of diabetes-associated microvascular and macrovascular complications. J. Am. Acad. Dermatol. 72, 968–977.e2 (2015).
Armstrong, A. W., Harskamp, C. T. & Armstrong, E. J. The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutr. Diabetes 2, e54 (2012).
Armstrong, A. W., Harskamp, C. T. & Armstrong, E. J. Psoriasis and metabolic syndrome: a systematic review and meta-analysis of observational studies. J. Am. Acad. Dermatol. 68, 654–662 (2013).
Gelfand, J. M. et al. Risk of myocardial infarction in patients with psoriasis. JAMA 296, 1735–1741 (2006).
Singh, S., Taylor, C., Kornmehl, H. & Armstrong, A. W. Psoriasis and suicidality: a systematic review and meta-analysis. J. Am. Acad. Dermatol. 77, 425–440.e2 (2017).
Dowlatshahi, E. A., Wakkee, M., Arends, L. R. & Nijsten, T. The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: a systematic review and meta-analysis. J. Invest. Dermatol. 134, 1542–1551 (2014).
Mansouri, B. et al. Comparison of coronary artery calcium scores between patients with psoriasis and type 2 diabetes. JAMA Dermatol. 152, 1244–1253 (2016).
Gelfand, J. M. et al. The risk of stroke in patients with psoriasis. J. Invest. Dermatol. 129, 2411–2418 (2009).
Mehta, N. N. et al. Patients with severe psoriasis are at increased risk of cardiovascular mortality: cohort study using the general practice research database. Eur. Heart J. 31, 1000–1006 (2010).
Armstrong, E. J., Harskamp, C. T. & Armstrong, A. W. Psoriasis and major adverse cardiovascular events: a systematic review and meta-analysis of observational studies. J. Am. Heart Assoc. 2, e000062 (2013).
Li, Q. et al. RNA editing underlies genetic risk of common inflammatory diseases. Nature 608, 569–577 (2022).
Parisi, R., Symmons, D. P., Griffiths, C. E. & Ashcroft, D. M. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J. Invest. Dermatol. 133, 377–385 (2013).
Payne, K. et al. Prevalence of multiple long-term conditions with psoriasis in England: a cohort study using the Clinical Practice Research Datalink. JEADV Clin. Pract. 3, 117–127 (2024).
Springate, D. A. et al. Incidence, prevalence and mortality of patients with psoriasis: a U.K. population-based cohort study. Br. J. Dermatol. 176, 650–658 (2017).
Leder, R. O. & Farber, M. M. The variable incidence of psoriasis in sub-Saharan Africa. Int. J. Dermatol. 36, 911–919 (1997).
Iskandar, I. Y. K. et al. Incidence, prevalence, and mortality of people with psoriasis and psoriatic arthritis in Taiwan: a nationwide cohort study. Acta Derm. Venereol. 102, adv00807 (2022).
Wang, K., Zhao, Y. & Cao, X. Global burden and future trends in psoriasis epidemiology: insights from the Global Burden of Disease Study 2019 and predictions to 2030. Arch. Dermatol. Res. 316, 114 (2024).
Grjibovski, A. M., Olsen, A. O., Magnus, P. & Harris, J. R. Psoriasis in Norwegian twins: contribution of genetic and environmental effects. J. Eur. Acad. Dermatol. Venereol. 21, 1337–1343 (2007).
Yan, D. et al. New frontiers in psoriatic disease research, part I: genetics, environmental triggers, immunology, pathophysiology, and precision medicine. J. Investig. Dermatol. 141, 2112–2122.e3 (2021).
Jordan, C. T. et al. PSORS2 is due to mutations in CARD14. Am. J. Hum. Genet. 90, 784–795 (2012).
Jordan, C. T. et al. Rare and common variants in CARD14, encoding an epidermal regulator of NF-κB, in psoriasis. Am. J. Hum. Genet. 90, 796–808 (2012).
Rutsch, F. et al. A specific IFIH1 gain-of-function mutation causes Singleton–Merten syndrome. Am. J. Hum. Genet. 96, 275–282 (2015).
Ferreira, C. R. et al. DDX58 and classic Singleton–Merten syndrome. J. Clin. Immunol. 39, 75–80 (2019).
Zou, Y. et al. Prevalence, outcomes and associated factors of SARS-CoV-2 infection in psoriasis patients of Southwest China: a cross-sectional survey. Sci. Rep. 14, 6331 (2024).
Morar, N., Willis-Owen, S. A., Maurer, T. & Bunker, C. B. HIV-associated psoriasis: pathogenesis, clinical features, and management. Lancet Infect. Dis. 10, 470–478 (2010).
Setty, A. R., Curhan, G. & Choi, H. K. Obesity, waist circumference, weight change, and the risk of psoriasis in women: Nurses’ Health Study II. Arch. Intern. Med. 167, 1670–1675 (2007).
Aune, D. et al. Body mass index, abdominal fatness, weight gain and the risk of psoriasis: a systematic review and dose-response meta-analysis of prospective studies. Eur. J. Epidemiol. 33, 1163–1178 (2018).
Carrascosa, J. M. et al. Obesity and psoriasis: inflammatory nature of obesity, relationship between psoriasis and obesity, and therapeutic implications. Actas Dermosifiliogr. 105, 31–44 (2014).
Guzik, T. J., Mangalat, D. & Korbut, R. Adipocytokines – novel link between inflammation and vascular function? J. Physiol. Pharmacol. 57, 505–528 (2006).
Davidovici, B. B. et al. Psoriasis and systemic inflammatory diseases: potential mechanistic links between skin disease and co-morbid conditions. J. Invest. Dermatol. 130, 1785–1796 (2010).
Maglio, C., Peltonen, M., Rudin, A. & Carlsson, L. M. S. Bariatric surgery and the incidence of psoriasis and psoriatic arthritis in the Swedish Obese Subjects study. Obesity 25, 2068–2073 (2017).
Egeberg, A., Sørensen, J. A., Gislason, G. H., Knop, F. K. & Skov, L. Incidence and prognosis of psoriasis and psoriatic arthritis in patients undergoing bariatric surgery. JAMA Surg. 152, 344–349 (2017).
Phan, K., Lee, G. & Fischer, G. Pediatric psoriasis and association with cardiovascular and metabolic comorbidities: systematic review and meta-analysis. Pediatr. Dermatol. 37, 661–669 (2020).
Armstrong, A. W., Harskamp, C. T., Dhillon, J. S. & Armstrong, E. J. Psoriasis and smoking: a systematic review and meta-analysis. Br. J. Dermatol. 170, 304–314 (2014).
Fortes, C. et al. Relationship between smoking and the clinical severity of psoriasis. Arch. Dermatol. 141, 1580–1584 (2005).
Brenaut, E. et al. Alcohol consumption and psoriasis: a systematic literature review. J. Eur. Acad. Dermatol. Venereol. 27, 30–35 (2013).
Choi, J. et al. Dose-response analysis between alcohol consumption and psoriasis: a systematic review and meta-analysis. J. Dtsch. Dermatol. Ges. 22, 641–652 (2024).
Hall, J. M. et al. Psychological stress and the cutaneous immune response: roles of the HPA axis and the sympathetic nervous system in atopic dermatitis and psoriasis. Dermatol. Res. Pract. 2012, 403908 (2012).
Mrowietz, U. et al. ActiPso: definition of activity types for psoriatic disease: a novel marker for an advanced disease classification. J. Eur. Acad. Dermatol. Venereol. 35, 2027–2033 (2021).
Kowalewska, B., Krajewska-Kulak, E. & Sobolewski, M. The impact of stress-coping strategies and the severity of psoriasis on self-esteem, illness acceptance and life satisfaction. Dermatol. Ther. 12, 529–543 (2022).
Li, Y. et al. Assessing causal relationships between gut microbiota and psoriasis: evidence from two sample Mendelian randomization analysis. Sci. Rep. 14, 8831 (2024).
Chen, L. et al. Skin and gut microbiome in psoriasis: gaining insight into the pathophysiology of it and finding novel therapeutic strategies. Front. Microbiol. 11, 589726 (2020).
Wu, R. et al. Psoriasis and gut microbiota: a Mendelian randomization study. J. Cell Mol. Med. 28, e18023 (2024).
Danlos, F. X. et al. Safety and efficacy of anti-programmed death 1 antibodies in patients with cancer and pre-existing autoimmune or inflammatory disease. Eur. J. Cancer 91, 21–29 (2018).
Ritchlin, C. T., Colbert, R. A. & Gladman, D. D. Psoriatic arthritis. N. Engl. J. Med. 376, 957–970 (2017).
Mody, E., Husni, M. E., Schur, P. & Qureshi, A. A. Multidisciplinary evaluation of patients with psoriasis presenting with musculoskeletal pain: a dermatology: rheumatology clinic experience. Br. J. Dermatol. 157, 1050–1051 (2007).
Dowlatshahi, E. A. et al. Psoriasis is not associated with atherosclerosis and incident cardiovascular events: the Rotterdam study. J. Invest. Dermatol. 133, 2347–2354 (2013).
Gao, N. et al. The association between psoriasis and risk of cardiovascular disease: a Mendelian randomization analysis. Front. Immunol. 13, 918224 (2022).
Patrick, M. T. et al. Shared genetic risk factors and causal association between psoriasis and coronary artery disease. Nat. Commun. 13, 6565 (2022).
Gelfand, J. M. et al. The risk of mortality in patients with psoriasis: results from a population-based study. Arch. Dermatol. 143, 1493–1499 (2007).
Samarasekera, E. J., Neilson, J. M., Warren, R. B., Parnham, J. & Smith, C. H. Incidence of cardiovascular disease in individuals with psoriasis: a systematic review and meta-analysis. J. Invest. Dermatol. 133, 2340–2346 (2013).
Ma, C., Schupp, C. W., Armstrong, E. J. & Armstrong, A. W. Psoriasis and dyslipidemia: a population-based study analyzing the National Health and Nutrition Examination Survey (NHANES). J. Eur. Acad. Dermatol. Venereol. 28, 1109–1112 (2014).
Ruan, Z. et al. Association between psoriasis and nonalcoholic fatty liver disease among outpatient US adults. JAMA Dermatol. 158, 745–753 (2022).
Belinchon-Romero, I. et al. Non-alcoholic fatty liver disease is associated with bacterial translocation and a higher inflammation response in psoriatic patients. Sci. Rep. 11, 8593 (2021).
Rinella, M. E. et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 79, 1542–1556 (2023).
Wu, K. K. & Armstrong, A. W. Suicidality among psoriasis patients: a critical evidence synthesis. G. Ital. Dermatol. Venereol. 154, 56–63 (2019).
Mrowietz, U., Sumbul, M. & Gerdes, S. Depression, a major comorbidity of psoriatic disease, is caused by metabolic inflammation. J. Eur. Acad. Dermatol. Venereol. 37, 1731–1738 (2023).
Korman, A. M., Dane, H., Ali, A. & Feldman, S. R. Impact and management of depression in psoriasis patients. Expert. Opin. Pharmacother. 17, 147–152 (2016).
Wan, J. et al. Risk of moderate to advanced kidney disease in patients with psoriasis: population based cohort study. BMJ 347, f5961 (2013).
Chi, C. C. et al. Risk of incident chronic kidney disease and end-stage renal disease in patients with psoriasis: a nationwide population-based cohort study. J. Dermatol. Sci. 78, 232–238 (2015).
Fu, Y., Lee, C. H. & Chi, C. C. Association of psoriasis with inflammatory bowel disease: a systematic review and meta-analysis. JAMA Dermatol. 154, 1417–1423 (2018).
Fitch, E., Harper, E., Skorcheva, I., Kurtz, S. E. & Blauvelt, A. Pathophysiology of psoriasis: recent advances on IL-23 and Th17 cytokines. Curr. Rheumatol. Rep. 9, 461–467 (2007).
Di Cesare, A., Di Meglio, P. & Nestle, F. O. The IL-23/Th17 axis in the immunopathogenesis of psoriasis. J. Investig. Dermatol. 129, 1339–1350 (2009). This is the key review describing the importance of the IL-23–TH17 pathway in psoraisis pathogenesis.
Hawkes, J. E., Yan, B. Y., Chan, T. C. & Krueger, J. G. Discovery of the IL-23/IL-17 signaling pathway and the treatment of psoriasis. J. Immunol. 201, 1605–1613 (2018).
Arakawa, A. et al. Melanocyte antigen triggers autoimmunity in human psoriasis. J. Exp. Med. 212, 2203–2212 (2015).
Girolomoni, G. et al. The role of IL-23 and the IL-23/TH17 immune axis in the pathogenesis and treatment of psoriasis. J. Eur. Acad. Dermatol. Venereol. 31, 1616–1626 (2017).
Fries, A. et al. Differentiation of IL-26+ TH17 intermediates into IL-17A producers via epithelial crosstalk in psoriasis. Nat. Commun. 14, 3878 (2023).
Ma, F. et al. Single cell and spatial sequencing define processes by which keratinocytes and fibroblasts amplify inflammatory responses in psoriasis. Nat. Commun. 14, 3455 (2023).
Francis, L. et al. Single-cell analysis of psoriasis resolution demonstrates an inflammatory fibroblast state targeted by IL-23 blockade. Nat. Commun. 15, 913 (2024).
Wu, D. et al. A single-cell atlas of IL-23 inhibition in cutaneous psoriasis distinguishes clinical response. Sci. Immunol. 9, eadi2848 (2024).
Van Der Fits, L., Van Der Wel, L. I., Laman, J. D., Prens, E. P. & Verschuren, M. C. M. In psoriasis lesional skin the type I interferon signaling pathway is activated, whereas interferon-α sensitivity is unaltered. J. Investig. Dermatol. 122, 51–60 (2004).
Shallev, L. et al. Decreased A-to-I RNA editing as a source of keratinocytes’ dsRNA in psoriasis. RNA 24, 828–840 (2018).
Funk, J., Langeland, T., Schrumpf, E. & Hanssen, L. E. Psoriasis induced by interferon-α. Br. J. Dermatol. 125, 463–465 (1991).
Patel, U., Mark, N. M., Machler, B. C. & Levine, V. J. Imiquimod 5% cream induced psoriasis: a case report, summary of the literature and mechanism: Correspondence. Br. J. Dermatol. 164, 670–672 (2011).
Ragimbeau, J. et al. The tyrosine kinase Tyk2 controls IFNAR1 cell surface expression. EMBO J. 22, 537–547 (2003).
Strober, B. et al. Deucravacitinib versus placebo and apremilast in moderate to severe plaque psoriasis: efficacy and safety results from the 52-week, randomized, double-blinded, phase 3 Program fOr evaluation of TYK2 inhibitor psoriasis second trial. J. Am. Acad. Dermatol. 88, 40–51 (2023).
Hollox, E. J. et al. Psoriasis is associated with increased β-defensin genomic copy number. Nat. Genet. 40, 23–25 (2008).
Lande, R. et al. Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature 449, 564–569 (2007).
Lande, R. et al. The antimicrobial peptide LL37 is a T-cell autoantigen in psoriasis. Nat. Commun. 5, 5621 (2014).
Zaba, L. C., Krueger, J. G. & Lowes, M. A. Resident and “inflammatory” dendritic cells in human skin. J. Investig. Dermatol. 129, 302–308 (2009).
Hänsel, A. et al. Human slan (6-sulfo LacNAc) dendritic cells are inflammatory dermal dendritic cells in psoriasis and drive strong TH17/TH1 T-cell responses. J. Allergy Clin. Immunol. 127, 787–794.e9 (2011).
Mehta, H. et al. Differential changes in inflammatory mononuclear phagocyte and T-cell profiles within psoriatic skin during treatment with guselkumab vs. secukinumab. J. Investig. Dermatol. 141, 1707–1718.e9 (2021).
Blauvelt, A. & Chiricozzi, A. The immunologic role of IL-17 in psoriasis and psoriatic arthritis pathogenesis. Clin. Rev. Allergy Immunol. 55, 379–390 (2018).
Cheuk, S. et al. Epidermal Th22 and Tc17 cells form a localized disease memory in clinically healed psoriasis. J. Immunol. 192, 3111–3120 (2014).
Blauvelt, A. Resident memory T cells in psoriasis: key to a cure? J. Psoriasis Psoriatic Arthritis 7, 157–159 (2022).
Whitley, S. K. et al. Local IL-23 is required for proliferation and retention of skin-resident memory TH17 cells. Sci. Immunol. 7, eabq3254 (2022).
Lin, A. M. et al. Mast cells and neutrophils release IL-17 through extracellular trap formation in psoriasis. J. Immunol. 187, 490–500 (2011).
Zenobia, C. & Hajishengallis, G. Basic biology and role of interleukin‐17 in immunity and inflammation. Periodontol. 2000 69, 142–159 (2015).
Chiricozzi, A. et al. Integrative responses to IL-17 and TNF-α in human keratinocytes account for key inflammatory pathogenic circuits in psoriasis. J. Investig. Dermatol. 131, 677–687 (2011).
Harper, E. G. et al. Th17 cytokines stimulate CCL20 expression in keratinocytes in vitro and in vivo: implications for psoriasis pathogenesis. J. Investig. Dermatol. 129, 2175–2183 (2009).
Miossec, P. & Kolls, J. K. Targeting IL-17 and TH17 cells in chronic inflammation. Nat. Rev. Drug. Dis. 11, 763–776 (2012).
Zhang, P. et al. Analysis of Th1/Th2 response pattern for erythrodermic psoriasis. J. Huazhong Univ. Sci. Technol. Med. Sci. 34, 596–601 (2014).
Xing, X. et al. IL-17 responses are the dominant inflammatory signal linking inverse, erythrodermic, and chronic plaque psoriasis. J. Invest. Dermatol. 136, 2498–2501 (2016).
Tauber, M. et al. IL36RN mutations affect protein expression and function: a basis for genotype-phenotype correlation in pustular diseases. J. Invest. Dermatol. 136, 1811–1819 (2016).
Zhu, T., Jin, H., Shu, D., Li, F. & Wu, C. Association of IL36RN mutations with clinical features, therapeutic response to acitretin, and frequency of recurrence in patients with generalized pustular psoriasis. Eur. J. Dermatol. 28, 217–224 (2018).
Johnston, A. et al. IL-1 and IL-36 are dominant cytokines in generalized pustular psoriasis. J. Allergy Clin. Immunol. 140, 109–120 (2017).
Wang, T. S. et al. Correlation of IL36RN mutation with different clinical features of pustular psoriasis in Chinese patients. Arch. Dermatol. Res. 308, 55–63 (2016).
Takahashi, T., Fujimoto, N., Kabuto, M., Nakanishi, T. & Tanaka, T. Mutation analysis of IL36RN gene in Japanese patients with palmoplantar pustulosis. J. Dermatol. 44, 80–83 (2017).
Misiak-Galazka, M., Zozula, J. & Rudnicka, L. Palmoplantar pustulosis: recent advances in etiopathogenesis and emerging treatments. Am. J. Clin. Dermatol. 21, 355–370 (2020).
Bachelez, H. et al. Trial of spesolimab for generalized pustular psoriasis. N. Engl. J. Med. 385, 2431–2440 (2021).
Burden, A. D. et al. Spesolimab efficacy and safety in patients with moderate-to-severe palmoplantar pustulosis: a multicentre, double-blind, randomised, placebo-controlled, phase IIb, dose-finding study. Dermatol. Ther. 13, 2279–2297 (2023).
Mrowietz, U. et al. Spesolimab, an anti-interleukin-36 receptor antibody, in patients with palmoplantar pustulosis: results of a phase IIa, multicenter, double-blind, randomized, placebo-controlled pilot study. Dermatol. Ther. 11, 571–585 (2021).
Gkini, M. A. et al. Psoriasis in people with skin of color: an evidence-based update. Int. J. Dermatol. 64, 667–677 (2025).
Hong, J. J. et al. Genital and inverse/intertriginous psoriasis: an updated review of therapies and recommendations for practical management. Dermatol. Ther. 11, 833–844 (2021).
Jiaravuthisan, M. M., Sasseville, D., Vender, R. B., Murphy, F. & Muhn, C. Y. Psoriasis of the nail: anatomy, pathology, clinical presentation, and a review of the literature on therapy. J. Am. Acad. Dermatol. 57, 1–27 (2007).
Farley, E., Masrour, S., McKey, J. & Menter, A. Palmoplantar psoriasis: a phenotypical and clinical review with introduction of a new quality-of-life assessment tool. J. Am. Acad. Dermatol. 60, 1024–1031 (2009).
Piaserico, S. et al. Comparative effectiveness of biologics for patients with moderate-to-severe psoriasis and special area involvement: week 12 results from the observational Psoriasis Study of Health Outcomes (PSoHO). Front. Med. 10, 1185523 (2023).
Huang, I. H., Wu, P. C., Chiu, H. Y. & Huang, Y. H. Small-molecule inhibitors and biologics for palmoplantar psoriasis and palmoplantar pustulosis: a systematic review and network meta-analysis. Am. J. Clin. Dermatol. 25, 347–358 (2024).
Duffin, K. C., Hwang, S. T. & Krueger, J. G. Advances and controversies in our understanding of guttate and plaque psoriasis. J. Rheumatol. 50, 4–7 (2023).
Munera-Campos, M., Ballesca, F. & Carrascosa, J. M. Paradoxical reactions to biologic therapy in psoriasis: a review of the literature. Actas Dermosifiliogr. 109, 791–800 (2018).
Bhutani, T. & Farberg, A. S. Clinical and disease burden of patients with generalized pustular psoriasis: a review of real-world evidence. Dermatol. Ther. 14, 341–360 (2024).
Li, L. et al. Variants of CARD14 are predisposing factors for generalized pustular psoriasis (GPP) with psoriasis vulgaris but not for GPP alone in a Chinese population. Br. J. Dermatol. 180, 425–426 (2019).
Mossner, R. et al. The genetic basis for most patients with pustular skin disease remains elusive. Br. J. Dermatol. 178, 740–748 (2018).
Brunasso, A. M. et al. Clinical and epidemiological comparison of patients affected by palmoplantar plaque psoriasis and palmoplantar pustulosis: a case series study. Br. J. Dermatol. 168, 1243–1251 (2013).
Smith, M. P. et al. Acrodermatitis continua of Hallopeau: clinical perspectives. Psoriasis 9, 65–72 (2019).
Singh, R. K. et al. Erythrodermic psoriasis: pathophysiology and current treatment perspectives. Psoriasis 6, 93–104 (2016).
Jackson, J. M., Alexis, A., Zirwas, M. & Taylor, S. Unmet needs for patients with seborrheic dermatitis. J. Am. Acad. Dermatol. 90, 597–604 (2024).
Joshi, T. P. & Duvic, M. Pityriasis rubra pilaris: an updated review of clinical presentation, etiopathogenesis, and treatment options. Am. J. Clin. Dermatol. 25, 243–259 (2024).
Craiglow, B. G. et al. CARD14-associated papulosquamous eruption: a spectrum including features of psoriasis and pityriasis rubra pilaris. J. Am. Acad. Dermatol. 79, 487–494 (2018).
Kimmel, G. W. & Lebwohl, M. in Evidence-Based Psoriasis: Diagnosis and Treatment (eds T. Bhutani, T., Liao, W. & M. Nakamura, M.) 1–16 (Springer, 2018).
Choon, S. E., Navarini, A. A. & Pinter, A. Clinical course and characteristics of generalized pustular psoriasis. Am. J. Clin. Dermatol. 23, 21–29 (2022).
Menter, A. et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J. Am. Acad. Dermatol. 80, 1029–1072 (2019).
Murphy, M., Kerr, P. & Grant-Kels, J. M. The histopathologic spectrum of psoriasis. Clin. Dermatol. 25, 524–528 (2007).
Golinska, J., Sar-Pomian, M. & Rudnicka, L. Dermoscopic features of psoriasis of the skin, scalp and nails – a systematic review. J. Eur. Acad. Dermatol. Venereol. 33, 648–660 (2019).
Robinson, A., Kardos, M. & Kimball, A. B. Physician Global Assessment (PGA) and Psoriasis Area and Severity Index (PASI): why do both? A systematic analysis of randomized controlled trials of biologic agents for moderate to severe plaque psoriasis. J. Am. Acad. Dermatol. 66, 369–375 (2012).
Langley, R. G., Feldman, S. R., Nyirady, J., van de Kerkhof, P. & Papavassilis, C. The 5-point investigator’s global assessment (IGA) scale: a modified tool for evaluating plaque psoriasis severity in clinical trials. J. Dermatol. Treat. 26, 23–31 (2015).
Cappelleri, J. C. & Bushmakin, A. G. Interpretation of patient-reported outcomes. Stat. Methods Med. Res. 23, 460–483 (2014).
Strober, B. et al. Recategorization of psoriasis severity: Delphi consensus from the International Psoriasis Council. J. Am. Acad. Dermatol. 82, 117–122 (2020). This consensus statement from the International Psoriasis Council proposes categorization of psoriasis disease severity based on body surface area, special areas affected and topical treatment response or failure following a modified Delphi approach to develop consensus.
Dauden, E. et al. Position statement for the management of comorbidities in psoriasis. J. Eur. Acad. Dermatol. Venereol. 32, 2058–2073 (2018).
Elmets, C. A. et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J. Am. Acad. Dermatol. 80, 1073–1113 (2019). These comprehensive guidelines from the American Academy of Dermatologists and the National Psoriasis Foundation provide guidance on the management of extracutaneous manifestations of psoriasis and other psoriasis-associated medical comorbidities.
Khraishi, M. et al. High prevalence of psoriatic arthritis in a cohort of patients with psoriasis seen in a dermatology practice. J. Cutan. Med. Surg. 16, 122–127 (2012).
Ibrahim, G., Waxman, R. & Helliwell, P. S. The prevalence of psoriatic arthritis in people with psoriasis. Arthritis Care Res. 61, 1373–1378 (2009).
Helliwell, P. S. Psoriasis Epidemiology Screening Tool (PEST): a report from the GRAPPA 2009 annual meeting. J. Rheumatol. 38, 551–552 (2011).
Husni, M. E., Meyer, K. H., Cohen, D. S., Mody, E. & Qureshi, A. A. The PASE questionnaire: pilot-testing a Psoriatic Arthritis Screening and Evaluation tool. J. Am. Acad. Dermatol. 57, 581–587 (2007).
Gladman, D. D. et al. Development and initial validation of a screening questionnaire for psoriatic arthritis: the Toronto Psoriatic Arthritis Screen (ToPAS). Ann. Rheum. Dis. 68, 497–501 (2009).
Khraishi, M., Landells, I. & Mugford, G. The self-administered Psoriasis and Arthritis Screening Questionnaire (PASQ): a sensitive and specific tool for the diagnosis of early and established psoriatic arthritis. Psoriasis Forum 16a, 9–16 (2010).
Tinazzi, I. et al. The early psoriatic arthritis screening questionnaire: a simple and fast method for the identification of arthritis in patients with psoriasis. Rheumatology 51, 2058–2063 (2012).
Salaffi, F. et al. A validation study of the Simple Psoriatic Arthritis Screening (SiPAS) questionnaire to screen psoriasis patients for psoriatic arthritis. Clin. Exp. Rheumatol. 36, 127–135 (2018).
Audureau, E. et al. Psoriatic arthritis screening by the dermatologist: development and first validation of the ‘PURE-4 scale’. J. Eur. Acad. Dermatol. Venereol. 32, 1950–1953 (2018).
Belinchón, I. et al. Dermatologists’ role in the early diagnosis of psoriatic arthritis: expert recommendations. Actas Dermosifiliogr. 111, 835–846 (2020).
Haroon, M., Gallagher, P. & FitzGerald, O. Diagnostic delay of more than 6 months contributes to poor radiographic and functional outcome in psoriatic arthritis. Ann. Rheum. Dis. 74, 1045–1050 (2015).
Taylor, W. et al. Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheumatism 54, 2665–2673 (2006).
Mrowietz, U. et al. Definition of treatment goals for moderate to severe psoriasis: a European consensus. Arch. Dermatol. Res. 303, 1–10 (2011).
Nast, A. et al. EuroGuiDerm guideline on the systemic treatment of psoriasis vulgaris – part 1: treatment and monitoring recommendations. J. Eur. Acad. Dermatol. Venereol. 34, 2461–2498 (2020).
Nast, A. et al. EuroGuiDerm guideline on the systemic treatment of psoriasis vulgaris – part 2: specific clinical and comorbid situations. J. Eur. Acad. Dermatol. Venereol. 35, 281–317 (2021). These EuroGuiDerm guidelines on approaching systemic treatment of psoriasis in the setting of special clinical scenarios include guidance on when to upgrade psoriasis severity classification from mild to moderate-to-severe.
Garshick, M. S., Ward, N. L., Krueger, J. G. & Berger, J. S. Cardiovascular risk in patients with psoriasis: JACC review topic of the week. J. Am. Coll. Cardiol. 77, 1670–1680 (2021).
Song, W. B., Soffer, D. E. & Gelfand, J. M. Using guidelines of care to lower cardiovascular risk in patients with psoriasis. Dermatol. Clin. 42, 417–428 (2024).
Berna-Rico, E. et al. Cardiovascular screening practices and statin prescription habits in patients with psoriasis among dermatologists, rheumatologists and primary care physicians. Acta Derm. Venereol. 103, adv5087 (2023).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med. Care 41, 1284–1292 (2003).
Kromer, C. et al. Screening for depression in psoriasis patients during a dermatological consultation: a first step towards treatment. J. Dtsch. Dermatol. Ges. 19, 1451–1461 (2021).
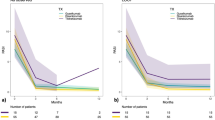
Schakel, K. et al. Early disease intervention with guselkumab in psoriasis leads to a higher rate of stable complete skin clearance (‘clinical super response’): week 28 results from the ongoing phase IIIb randomized, double-blind, parallel-group, GUIDE study. J. Eur. Acad. Dermatol. Venereol. 37, 2016–2027 (2023).
Elmets, C. A. et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with topical therapy and alternative medicine modalities for psoriasis severity measures. J. Am. Acad. Dermatol. 84, 432–470 (2021).
Lé, A. M. & Torres, T. New topical therapies for psoriasis. Am. J. Clin. Dermatol. 23, 13–24 (2022).
Guenther, L., Lynde, C. & Poulin, Y. Off-label use of topical calcineurin inhibitors in dermatologic disorders. J. Cutan. Med. Surg. 23, 27S–34S (2019).
Lebwohl, M. G. et al. Phase 3 trials of tapinarof cream for plaque psoriasis. N. Engl. J. Med. 385, 2219–2229 (2021).
Yelamos, O. et al. Non-invasive clinical and microscopic evaluation of the response to treatment with clobetasol cream vs. calcipotriol/betamethasone dipropionate foam in mild to moderate plaque psoriasis: an investigator-initiated, phase IV, unicentric, open, randomized clinical trial. J. Eur. Acad. Dermatol. Venereol. 35, 143–149 (2021).
Patel, N. U., Felix, K., Reimer, D. & Feldman, S. R. Calcipotriene/betamethasone dipropionate for the treatment of psoriasis vulgaris: an evidence-based review. Clin. Cosmet. Investig. Dermatol. 10, 385–391 (2017).
Pinter, A. et al. Randomized phase 3 trial demonstrating high efficacy, favourable safety and convenience of a novel calcipotriol and betamethasone dipropionate cream for the treatment of psoriasis. J. Eur. Acad. Dermatol. Venereol. 37, 2327–2335 (2023).
Nogueira, M., Puig, L. & Torres, T. JAK inhibitors for treatment of psoriasis: focus on selective TYK2 inhibitors. Drugs 80, 341–352 (2020).
Catlett, I. M. et al. Molecular and clinical effects of selective tyrosine kinase 2 inhibition with deucravacitinib in psoriasis. J. Allergy Clin. Immunol. 149, 2010–2020.e8 (2022).
Schafer, P. Apremilast mechanism of action and application to psoriasis and psoriatic arthritis. Biochem. Pharmacol. 83, 1583–1590 (2012).
Papp, K. et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J. Am. Acad. Dermatol. 73, 37–49 (2015).
Terui, T. et al. Efficacy and safety of apremilast for the treatment of Japanese patients with palmoplantar pustulosis: results from a phase 2, randomized, placebo-controlled study. Am. J. Clin. Dermatol. 24, 837–847 (2023).
Paul, C. et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br. J. Dermatol. 173, 1387–1399 (2015).
Rich, P. et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in patients with difficult-to-treat nail and scalp psoriasis: results of 2 phase III randomized, controlled trials (ESTEEM 1 and ESTEEM 2). J. Am. Acad. Dermatol. 74, 134–142 (2016).
Amor, K. T., Ryan, C. & Menter, A. The use of cyclosporine in dermatology: part I. J. Am. Acad. Dermatol. 63, 925–946 (2010).
Maza, A. et al. Oral cyclosporin in psoriasis: a systematic review on treatment modalities, risk of kidney toxicity and evidence for use in non‐plaque psoriasis. J. Eur. Acad. Dermatol. Venereol. 25, 19–27 (2011).
Menter, A. et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J. Am. Acad. Dermatol. 82, 1445–1486 (2020).
Chen, L. et al. Circulating microRNA profile unveils mechanisms of action of acitretin for psoriasis vulgaris. Bioengineered 12, 1838–1850 (2021).
Lebwohl, M. et al. Consensus conference: acitretin in combination with UVB or PUVA in the treatment of psoriasis. J. Am. Acad. Dermatol. 45, 544–553 (2001).
van de Kerkhof, P. C. & de Rooij, M. J. Multiple squamous cell carcinomas in a psoriatic patient following high-dose photochemotherapy and cyclosporin treatment: response to long-term acitretin maintenance. Br. J. Dermatol. 136, 275–278 (1997).
Yan, K. et al. Methotrexate restores the function of peripheral blood regulatory T cells in psoriasis vulgaris via the CD73/AMPK/mTOR pathway. Br. J. Dermatol. 179, 896–905 (2018).
Thomas, S. et al. Methotrexate is a JAK/STAT pathway inhibitor. PLoS ONE 10, e0130078 (2015).
West, J., Ogston, S. & Foerster, J. Safety and efficacy of methotrexate in psoriasis: a meta-analysis of published trials. PLoS ONE 11, e0153740 (2016).
Dos Santos Pereira, M. et al. Evaluation of liver fibrosis by transient elastography in Brazilian patients with psoriasis using methotrexate. J. Eur. Acad. Dermatol. Venereol. https://doi.org/10.1111/jdv.20654 (2025).
van Huizen, A. M., Sikkel, R., Caron, A. G. M., Menting, S. P. & Spuls, P. I. Methotrexate dosing regimen for plaque-type psoriasis: an update of a systematic review. J. Dermatol. Treat. 33, 3104–3118 (2022).
Ghoreschi, K. et al. Fumarates improve psoriasis and multiple sclerosis by inducing type II dendritic cells. J. Exp. Med. 208, 2291–2303 (2011).
Atwan, A. et al. Oral fumaric acid esters for psoriasis. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD010497.pub2 (2015).
Bolognia, J. L., Jorizzo, J. L. & Schaffer, J. V. Dermatology 3rd edn (Elsevier, 2012).
Tran, B. N. et al. Higher order structures of adalimumab, infliximab and their complexes with TNFα revealed by electron microscopy. Protein Sci. 26, 2392–2398 (2017).
Cessak, G. et al. TNF inhibitors – mechanisms of action, approved and off-label indications. Pharmacol. Rep. 66, 836–844 (2014).
Jadon, D. R. et al. Management of concomitant inflammatory bowel disease or uveitis in patients with psoriatic arthritis: an updated review informing the 2021 GRAPPA treatment recommendations. J. Rheumatol. 50, 438–450 (2023).
Gelfand, J. M. & Garshick, M. TNF inhibitors and cardiovascular risk: friend or foe? J. Eur. Acad. Dermatol. Venereol. 38, 995–996 (2024).
Gonzalez-Cantero, A. et al. Impact of biological agents on imaging and biomarkers of cardiovascular disease in patients with psoriasis: a systematic review and meta-analysis of randomized placebo-controlled trials. J. Invest. Dermatol. 141, 2402–2411 (2021).
Mantravadi, S., Ogdie, A. & Kraft, W. K. Tumor necrosis factor inhibitors in psoriatic arthritis. Expert. Rev. Clin. Pharmacol. 10, 899–910 (2017).
Gisondi, P., Bellinato, F., Targher, G., Idolazzi, L. & Girolomoni, G. Biological disease-modifying antirheumatic drugs may mitigate the risk of psoriatic arthritis in patients with chronic plaque psoriasis. Ann. Rheum. Dis. 81, 68–73 (2022).
Acosta Felquer, M. L. et al. Treating the skin with biologics in patients with psoriasis decreases the incidence of psoriatic arthritis. Ann. Rheum. Dis. 81, 74–79 (2022).
Rosenthal, Y. S., Schwartz, N., Sagy, I. & Pavlovsky, L. Incidence of psoriatic arthritis among patients receiving biologic treatments for psoriasis: a nested case-control study. Arthritis Rheumatol. 74, 237–243 (2022).
Semble, A. L., Davis, S. A. & Feldman, S. R. Safety and tolerability of tumor necrosis factor-α inhibitors in psoriasis: a narrative review. Am. J. Clin. Dermatol. 15, 37–43 (2014).
Davila-Seijo, P. et al. Infections in moderate to severe psoriasis patients treated with biological drugs compared to classic systemic drugs: findings from the BIOBADADERM registry. J. Invest. Dermatol. 137, 313–321 (2017).
Fouache, D. et al. Paradoxical adverse events of anti-tumour necrosis factor therapy for spondyloarthropathies: a retrospective study. Rheumatology 48, 761–764 (2009).
Ko, J. M., Gottlieb, A. B. & Kerbleski, J. F. Induction and exacerbation of psoriasis with TNF-blockade therapy: a review and analysis of 127 cases. J. Dermatol. Treat. 20, 100–108 (2009).
Adams, R. et al. Bimekizumab, a novel humanized IgG1 antibody that neutralizes both IL-17A and IL-17F. Front. Immunol. 11, 1894 (2020).
Langley, R. G. et al. Secukinumab in plaque psoriasis – results of two phase 3 trials. N. Engl. J. Med. 371, 326–338 (2014).
Gordon, K. B. et al. Phase 3 trials of ixekizumab in moderate-to-severe plaque psoriasis. N. Engl. J. Med. 375, 345–356 (2016).
Targan, S. R. et al. A randomized, double-blind, placebo-controlled phase 2 study of brodalumab in patients with moderate-to-severe Crohn’s disease. Am. J. Gastroenterol. 111, 1599–1607 (2016).
Elewski, B. E. et al. Psoriasis patients with Psoriasis Area and Severity Index (PASI) 90 response achieve greater health-related quality-of-life improvements than those with PASI 75-89 response: results from two phase 3 studies of secukinumab. J. Dermatol. Treat. 28, 492–499 (2017).
Griffiths, C. E. M. et al. Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trials. Lancet 386, 541–551 (2015).
Gordon, K. B. et al. Bimekizumab efficacy and safety in moderate to severe plaque psoriasis (BE READY): a multicentre, double-blind, placebo-controlled, randomised withdrawal phase 3 trial. Lancet 397, 475–486 (2021).
Merola, J. F. et al. AB1089 Bimekizumab efficacy in high-impact areas for patients with moderate to severe plaque psoriasis: pooled results through two years from the Be Sure and Be Radiant phase 3 trials [abstract]. Ann. Rheum. Dis. 82, 1766–1767 (2023).
McInnes, I. B. et al. Secukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 386, 1137–1146 (2015).
Mease, P. J. et al. Ixekizumab, an interleukin-17A specific monoclonal antibody, for the treatment of biologic-naive patients with active psoriatic arthritis: results from the 24-week randomised, double-blind, placebo-controlled and active (adalimumab)-controlled period of the phase III trial SPIRIT-P1. Ann. Rheum. Dis. 76, 79–87 (2017).
Baraliakos, X. et al. Secukinumab in patients with psoriatic arthritis and axial manifestations: results from the double-blind, randomised, phase 3 MAXIMISE trial. Ann. Rheum. Dis. 80, 582–590 (2021).
Langley, R. G. et al. Long‐term efficacy and safety of ustekinumab, with and without dosing adjustment, in patients with moderate‐to‐severe psoriasis: results from the PHOENIX 2 study through 5 years of follow‐up. Br. J. Dermatol. 172, 1371–1383 (2015).
Papp, K. A. et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2). Lancet 371, 1675–1684 (2008).
Poizeau, F. et al. Association between early severe cardiovascular events and the initiation of treatment with the anti-interleukin 12/23p40 antibody ustekinumab. JAMA Dermatol. 156, 1208–1215 (2020).
Blauvelt, A. et al. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the continuous treatment of patients with moderate to severe psoriasis: results from the phase III, double-blinded, placebo- and active comparator-controlled VOYAGE 1 trial. J. Am. Acad. Dermatol. 76, 405–417 (2017).
Gordon, K. B. et al. Efficacy of guselkumab in subpopulations of patients with moderate-to-severe plaque psoriasis: a pooled analysis of the phase III VOYAGE 1 and VOYAGE 2 studies. Br. J. Dermatol. 178, 132–139 (2018).
Reich, K. et al. Maintenance of clinical response and consistent safety profile with up to 3 years of continuous treatment with guselkumab: Results from the VOYAGE 1 and VOYAGE 2 trials. J. Am. Acad. Dermatol. 82, 936–945 (2020).
Reich, K. et al. Guselkumab versus secukinumab for the treatment of moderate-to-severe psoriasis (ECLIPSE): results from a phase 3, randomised controlled trial. Lancet 394, 831–839 (2019).
Gordon, K. B. et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet 392, 650–661 (2018).
Strober, B. et al. Efficacy of long-term risankizumab treatment for moderate-to-severe plaque psoriasis: subgroup analyses by baseline characteristics and psoriatic disease manifestations through 256 weeks (LIMMitless trial). J. Eur. Acad. Dermatol. Venereol. 38, 864–872 (2024).
Reich, K. et al. Tildrakizumab versus placebo or etanercept for chronic plaque psoriasis (reSURFACE 1 and reSURFACE 2): results from two randomised controlled, phase 3 trials. Lancet 390, 276–288 (2017).
Cameron, H. et al. A randomized, observer‐blinded trial of twice vs. three times weekly narrowband ultraviolet B phototherapy for chronic plaque psoriasis. Br. J. Dermatol. 147, 973–978 (2002).
Tartar, D., Bhutani, T., Huynh, M., Berger, T. & Koo, J. Update on the immunological mechanism of action behind phototherapy. J. Drugs Dermatol. 13, 564–568 (2014).
Ye, J. et al. NB-UVB irradiation attenuates inflammatory response in psoriasis. Dermatol. Ther. 33, e13626 (2020).
Wan, J. et al. Dermatologist preferences for first-line therapy of moderate to severe psoriasis in healthy adult patients. J. Am. Acad. Dermatol. 66, 376–386 (2012).
Koo, J. & Lebwohl, M. Duration of remission of psoriasis therapies. J. Am. Acad. Dermatol. 41, 51–59 (1999).
McCoy, T. et al. Systematic review and estimated cost-efficacy of biologics compared with narrowband ultraviolet B light for the treatment of moderate to severe psoriasis and atopic dermatitis. Int. J. Dermatol. 62, 986–999 (2023).
Almutawa, F. et al. Efficacy of localized phototherapy and photodynamic therapy for psoriasis: a systematic review and meta-analysis. Photodermatol. Photoimmunol. Photomed. 31, 5–14 (2015).
Mehta, N. N. et al. Effect of 2 psoriasis treatments on vascular inflammation and novel inflammatory cardiovascular biomarkers: a randomized placebo-controlled trial. Circ. Cardiovasc. Imaging 11, e007394 (2018).
Lim, J. L. & Stern, R. S. High levels of ultraviolet B exposure increase the risk of non-melanoma skin cancer in psoralen and ultraviolet A-treated patients. J. Investig. Dermatol. 124, 505–513 (2005).
Elmets, C. A. et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis with phototherapy. J. Am. Acad. Dermatol. 81, 775–804 (2019). These guidelines from the American Academy of Dermatologists and the National Psoriasis Foundation provide comprehensive guidance on the management of psoriasis with phototherapy.
Thatiparthi, A., Martin, A., Liu, J. & Wu, J. J. Risk of skin cancer with phototherapy in moderate-to-severe psoriasis: an updated systematic review. J. Clin. Aesthet. Dermatol. 15, 68–75 (2022).
Maruani, A. et al. Non-antistreptococcal interventions for acute guttate psoriasis or an acute guttate flare of chronic psoriasis. Cochrane Database Syst. Rev. 4, CD011541 (2019).
Fernandez-Guarino, M. et al. Phototherapy with narrow-band UVB in adult guttate psoriasis: results and patient assessment. Dermatology 232, 626–632 (2016).
Puig, L. et al. Generalized pustular psoriasis: a global Delphi consensus on clinical course, diagnosis, treatment goals and disease management. J. Eur. Acad. Dermatol. Venereol. 37, 737–752 (2023).
Rosenbach, M. et al. Treatment of erythrodermic psoriasis: from the medical board of the National Psoriasis Foundation. J. Am. Acad. Dermatol. 62, 655–662 (2010).
Carrasquillo, O. Y. et al. Treatment of erythrodermic psoriasis with biologics: a systematic review. J. Am. Acad. Dermatol. 83, 151–158 (2020).
Grimsrud, K. N. et al. Special population considerations and regulatory affairs for clinical research. Clin. Res. Regulatory Aff. 32, 45–54 (2015).
Murase, J. E., Chan, K. K., Garite, T. J., Cooper, D. M. & Weinstein, G. D. Hormonal effect on psoriasis in pregnancy and post partum. Arch. Dermatol. 141, 601–606 (2005).
Bobotsis, R., Gulliver, W. P., Monaghan, K., Lynde, C. & Fleming, P. Psoriasis and adverse pregnancy outcomes: a systematic review of observational studies. Br. J. Dermatol. 175, 464–472 (2016).
Smith, C. H. et al. British Association of Dermatologists guidelines for biologic therapy for psoriasis 2020: a rapid update. Br. J. Dermatol. 183, 628–637 (2020).
Murase, J. E., Heller, M. M. & Butler, D. C. Safety of dermatologic medications in pregnancy and lactation. J. Am. Acad. Dermatol. 70, 401.e1–401.e14 (2014).
Shavit, E. & Shear, N. H. An update on the safety of apremilast for the treatment of plaque psoriasis. Expert. Opin. Drug. Saf. 19, 403–408 (2020).
Grunnet, E., Nyfors, A. & Hansen, B. Studies on human semen in topical corticosteroid-treated and in methotrexate-treated psoriatics. Dermatology 154, 78–84 (1977).
Weber-Schoendorfer, C., Hoeltzenbein, M., Wacker, E., Meister, R. & Schaefer, C. No evidence for an increased risk of adverse pregnancy outcome after paternal low-dose methotrexate: an observational cohort study. Rheumatology 53, 757–763 (2014).
Brown, S. M., Aljefri, K., Waas, R. & Hampton, P. Systemic medications used in treatment of common dermatological conditions: safety profile with respect to pregnancy, breast feeding and content in seminal fluid. J. Dermatol. Treat. 30, 2–18 (2019).
Esteve-Solé, A. et al. Immunological changes in blood of newborns exposed to anti-TNF-α during pregnancy. Front. Immunol. 8, 1123 (2017).
European Medicines Agency. Summary of product characteristics: Cimzia (certolizumab pegol), solution for injection. EMA www.ema.europa.eu/en/documents/product-information/cimzia-epar-product-information_en.pdf (2014).
Food and Drug Administration. Highlights of prescribing information: Cimzia (certolizumab pegol), solution for subcutaneous injection. FDA www.accessdata.fda.gov/drugsatfda_docs/label/2008/125160s000lbl.pdf (2008).
Owczarek, W. et al. The use of biological drugs in psoriasis patients prior to pregnancy, during pregnancy and lactation: a review of current clinical guidelines. Adv. Dermatol. Allergol. 37, 821–830 (2020).
McMullan, P. et al. Safety of dermatologic medications in pregnancy and lactation: an update – part I: pregnancy. J. Am. Acad. Dermatol. 91, 619–648 (2024).
Mahé, E. Childhood psoriasis. Eur. J. Dermatol. 26, 537–548 (2016).
Cordoro, K. M. et al. Skin-infiltrating, interleukin-22-producing T cells differentiate pediatric psoriasis from adult psoriasis. J. Am. Acad. Dermatol. 77, 417–424 (2017).
Kim, J., Kim, S., Soh, B. & Lee, E. Comparison of cytokine expression in paediatric and adult psoriatic skin. Acta Derm. Venereol. 100, adv00058 (2020).
Bronckers, I. et al. Safety of systemic agents for the treatment of pediatric psoriasis. JAMA Dermatol. 153, 1147–1157 (2017).
Menter, A. et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis in pediatric patients. J. Am. Acad. Dermatol. 82, 161–201 (2020). These guidelines from the American Academy of Dermatologists and the National Psoriasis Foundation provide comprehensive guidance on the management of psoriasis specifically in paediatric patients.
Ergun, T. et al. Efficacy, safety and drug survival of conventional agents in pediatric psoriasis: a multicenter, cohort study. J. Dermatol. 44, 630–634 (2017).
Hebert, A. A. et al. Managing pediatric psoriasis: update on treatments and challenges – a review. J. Dermatol. Treat. 33, 2433–2442 (2022).
Popadic, S. & Nikolic, M. Pustular psoriasis in childhood and adolescence: a 20-year single-center experience. Pediatr. Dermatol. 31, 575–579 (2014).
Halverstam, C. P., Zeichner, J. & Lebwohl, M. Lack of significant skeletal changes after long-term, low-dose retinoid therapy: case report and review of the literature. J. Cutan. Med. Surg. 10, 291–299 (2006).
Caruso, C. et al. Mechanisms of immunosenescence. Immun. Ageing 6, 10 (2009).
Myers, B. et al. Biologic treatment of 4 HIV-positive patients: a case series and literature review. J. Psoriasis Psoriatic Arthritis 6, 19–26 (2021).
Montes-Torres, A. et al. Safety and effectiveness of conventional systemic therapy and biological drugs in patients with moderate to severe psoriasis and HIV infection: a retrospective multicenter study. J. Dermatol. Treat. 30, 461–465 (2019).
Lambert, J. L. W. et al. Practical recommendations for systemic treatment in psoriasis in case of coexisting inflammatory, neurologic, infectious or malignant disorders (BETA‐PSO: Belgian evidence‐based treatment advice in psoriasis; part 2). J. Eur. Acad. Dermatol. Venereol. 34, 1914–1923 (2020).
Papp, K. A. et al. Use of systemic therapies for treatment of psoriasis in patients with a history of treated solid tumours: inference-based guidance from a multidisciplinary expert panel. Dermatol. Ther. 13, 867–889 (2023).
Waldman, A. & Schmults, C. Cutaneous squamous cell carcinoma. Hematol. Oncol. Clin. North. Am. 33, 1–12 (2019).
Rapp, S. R., Feldman, S. R., Exum, M. L., Fleischer, A. B. Jr. & Reboussin, D. M. Psoriasis causes as much disability as other major medical diseases. J. Am. Acad. Dermatol. 41, 401–407 (1999).
Gelfand, J. M. et al. Determinants of quality of life in patients with psoriasis: a study from the US population. J. Am. Acad. Dermatol. 51, 704–708 (2004).
Maul, J. T. et al. Correlation between Dermatology Life Quality Index and Psoriasis Area and Severity Index in patients with psoriasis: a cross-sectional global healthcare study on psoriasis. Acta Derm. Venereol. 104, adv20329 (2024).
Bewley, A., Burrage, D. M., Ersser, S. J., Hansen, M. & Ward, C. Identifying individual psychosocial and adherence support needs in patients with psoriasis: a multinational two-stage qualitative and quantitative study. J. Eur. Acad. Dermatol. Venereol. 28, 763–770 (2014).
Fried, R. G. et al. Trivial or terrible? The psychosocial impact of psoriasis. Int. J. Dermatol. 34, 101–105 (1995).
Fortune, D. G., Richards, H. L. & Griffiths, C. E. Psychologic factors in psoriasis: consequences, mechanisms, and interventions. Dermatol. Clin. 23, 681–694 (2005).
Devrimci-Ozguven, H., Kundakci, T. N., Kumbasar, H. & Boyvat, A. The depression, anxiety, life satisfaction and affective expression levels in psoriasis patients. J. Eur. Acad. Dermatol. Venereol. 14, 267–271 (2000).
Krueger, G. et al. The impact of psoriasis on quality of life: results of a 1998 National Psoriasis Foundation patient-membership survey. Arch. Dermatol. 137, 280–284 (2001).
Choi, J. & Koo, J. Y. Quality of life issues in psoriasis. J. Am. Acad. Dermatol. 49, S57–S61 (2003).
Luck-Sikorski, C. et al. Assessment of stigma related to visible skin diseases: a systematic review and evaluation of patient-reported outcome measures. J. Eur. Acad. Dermatol. Venereol. 36, 499–525 (2022).
Halioua, B. et al. Extent of misconceptions, negative prejudices and discriminatory behaviour to psoriasis patients in France. J. Eur. Acad. Dermatol. Venereol. 30, 650–654 (2016).
Pearce, D. J. et al. The negative impact of psoriasis on the workplace. J. Dermatol. Treat. 17, 24–28 (2006).
Finlay, A. Y. & Coles, E. C. The effect of severe psoriasis on the quality of life of 369 patients. Br. J. Dermatol. 132, 236–244 (1995).
Feldman, S. R. et al. The economic impact of psoriasis increases with psoriasis severity. J. Am. Acad. Dermatol. 37, 564–569 (1997).
Vanderpuye-Orgle, J. et al. Evaluating the economic burden of psoriasis in the United States. J. Am. Acad. Dermatol. 72, 961–967.e5 (2015).
Warren, R. B., Kleyn, C. E. & Gulliver, W. P. Cumulative life course impairment in psoriasis: patient perception of disease-related impairment throughout the life course. Br. J. Dermatol. 164, 1–14 (2011).
Ros, S., Puig, L. & Carrascosa, J. M. Cumulative life course impairment: the imprint of psoriasis on the patient’s life. Actas Dermosifiliogr. 105, 128–134 (2014).
Armstrong, A. W. et al. Comparison of biologics and oral treatments for plaque psoriasis: a meta-analysis. JAMA Dermatol. 156, 258–269 (2020).
Schmitt, J. et al. Efficacy and safety of systemic treatments for moderate-to-severe psoriasis: meta-analysis of randomized controlled trials. Br. J. Dermatol. 170, 274–303 (2014).
de Ruiter, C. C. & Rustemeyer, T. Biologics can significantly improve dermatology life quality index (DLQI) in psoriatic patients: a systematic review. Psoriasis 12, 99–112 (2022).
Puig, L., Thom, H., Mollon, P., Tian, H. & Ramakrishna, G. S. Clear or almost clear skin improves the quality of life in patients with moderate-to-severe psoriasis: a systematic review and meta-analysis. J. Eur. Acad. Dermatol. Venereol. 31, 213–220 (2017).
Revicki, D. A. et al. Relationship between clinical response to therapy and health-related quality of life outcomes in patients with moderate to severe plaque psoriasis. Dermatology 216, 260–270 (2008).
Ghoreschi, K., Balato, A., Enerback, C. & Sabat, R. Therapeutics targeting the IL-23 and IL-17 pathway in psoriasis. Lancet 397, 754–766 (2021).
Gisondi, P. et al. Risk of developing psoriatic arthritis in patients with psoriasis initiating treatment with different classes of biologics. Ann. Rheum. Dis. 84, 435–441 (2025).
Dand, N. et al. HLA-C*06:02 genotype is a predictive biomarker of biologic treatment response in psoriasis. J. Allergy Clin. Immunol. 143, 2120–2130 (2019).
Batalla, A. et al. IL17RA gene variants and anti-TNF response among psoriasis patients. Pharmacogenomics J. 18, 76–80 (2018).
Coto-Segura, P. et al. Common and rare CARD14 gene variants affect the antitumour necrosis factor response among patients with psoriasis. Br. J. Dermatol. 175, 134–141 (2016).
Menter, A. et al. Adalimumab therapy for moderate to severe psoriasis: a randomized, controlled phase III trial. J. Am. Acad. Dermatol. 58, 106–115 (2008).
Leonardi, C. L. et al. Etanercept as monotherapy in patients with psoriasis. N. Engl. J. Med. 349, 2014–2022 (2003).
Gottlieb, A. B. et al. Certolizumab pegol for the treatment of chronic plaque psoriasis: results through 48 weeks from 2 phase 3, multicenter, randomized, double-blinded, placebo-controlled studies (CIMPASI-1 and CIMPASI-2). J. Am. Acad. Dermatol. 79, 302–314.e6 (2018).
Chaudhari, U. et al. Efficacy and safety of infliximab monotherapy for plaque-type psoriasis: a randomised trial. Lancet 357, 1842–1847 (2001).
Gottlieb, A. B. et al. Infliximab induction therapy for patients with severe plaque-type psoriasis: a randomized, double-blind, placebo-controlled trial. J. Am. Acad. Dermatol. 51, 534–542 (2004).
McInnes, I. B. et al. Efficacy and safety of ustekinumab in patients with active psoriatic arthritis: 1 year results of the phase 3, multicentre, double-blind, placebo-controlled PSUMMIT 1 trial. Lancet 382, 780–789 (2013).
Fernandez, A. P. et al. Tildrakizumab efficacy and safety in patients with psoriasis and concomitant metabolic syndrome: post hoc analysis of 5-year data from reSURFACE 1 and reSURFACE 2. J. Eur. Acad. Dermatol. Venereol. 36, 1774–1783 (2022).
Fiorillo, L. et al. Efficacy and safety of apremilast in pediatric patients with moderate-to-severe plaque psoriasis: 16-week results from SPROUT, a randomized controlled trial. J. Am. Acad. Dermatol. 90, 1232–1239 (2024).
Wren, A. A. et al. Multidisciplinary pain management for pediatric patients with acute and chronic pain: a foundational treatment approach when prescribing opioids. Children 6, 33 (2019).
Paller, A. S. et al. Etanercept treatment for children and adolescents with plaque psoriasis. N. Engl. J. Med. 358, 241–251 (2008).
Paller, A. S. et al. Long-term safety and efficacy of etanercept in children and adolescents with plaque psoriasis. J. Am. Acad. Dermatol. 74, 280–287.e3 (2016).
Landells, I. et al. Ustekinumab in adolescent patients age 12 to 17 years with moderate-to-severe plaque psoriasis: results of the randomized phase 3 CADMUS study. J. Am. Acad. Dermatol. 73, 594–603 (2015).
Philipp, S. et al. Ustekinumab for the treatment of moderate-to-severe plaque psoriasis in paediatric patients (≥6 to <12 years of age): efficacy, safety, pharmacokinetic and biomarker results from the open-label CADMUS Jr study. Br. J. Dermatol. 183, 664–672 (2020).
Bodemer, C. et al. Secukinumab demonstrates high efficacy and a favourable safety profile in paediatric patients with severe chronic plaque psoriasis: 52-week results from a phase 3 double-blind randomized, controlled trial. J. Eur. Acad. Dermatol. Venereol. 35, 938–947 (2021).
Paller, A. S. et al. Efficacy and safety of ixekizumab in a phase III, randomized, double-blind, placebo-controlled study in paediatric patients with moderate-to-severe plaque psoriasis (IXORA-PEDS). Br. J. Dermatol. 183, 231–241 (2020).
Strober, B. E. et al. Clinical goals and barriers to effective psoriasis care. Dermatol. Ther. 9, 5–18 (2019).
Kromer, C., Celis, D., Sonntag, D. & Peitsch, W. K. Biologicals and small molecules in psoriasis: a systematic review of economic evaluations. PLoS ONE 13, e0189765 (2018).
Villanueva, G. et al. Access to methotrexate monitoring in Latin America: a multicountry survey of supportive care capacity. Pediatr. Hematol. Oncol. 41, 135–149 (2024).
Torres, A. E., Lyons, A. B., Hamzavi, I. H. & Lim, H. W. Role of phototherapy in the era of biologics. J. Am. Acad. Dermatol. 84, 479–485 (2021).
Contento, M., Cline, A. & Russo, M. Steroid phobia: a review of prevalence, risk factors, and interventions. Am. J. Clin. Dermatol. 22, 837–851 (2021).
Abo-Tabik, M. et al. Development and evaluation of an online training tool to aid in the diagnosis of chronic plaque psoriasis. JEADV Clin. Pract. 4, 174–180 (2025).
Author information
Authors and Affiliations
Contributions
Introduction (A.W.A.); Epidemiology (A.W.A.); Mechanisms/pathophysiology (A.B.); Diagnosis, screening and prevention (Y.-H.H); Management (A.W.A., K.C.D., L.J.S. and J.F.M.); Quality of life (L.G.); Outlook (A.W.A. and A.B.); overview of the Primer (A.W.A. and L.G.).
Corresponding author
Ethics declarations
Competing interests
A.W.A. has served as a research investigator, scientific adviser or speaker for AbbVie, Amgen, Almirall, Arcutis, ASLAN, Beiersdorf, BI, BMS, EPI, Incyte, Leo, UCB, Janssen, Lilly, Mindera, Nimbus, Novartis, Ortho, Sun, Dermavant, Dermira, Sanofi, Takeda, Organon, Regeneron, Pfizer and Ventyx. A.B. has served as a speaker (received honoraria) for Eli Lilly and Company and UCB; has served as a scientific adviser (received honoraria) for AbbVie, Almirall, Alumis, Amgen, Anaptysbio, Apogee, Arcutis, Boehringer Ingelheim, Bristol Myers Squibb, Celltrion, Corvus, Dermavant, Eli Lilly and Company, Galderma, GlaxoSmithKline, Immunovant, Incyte, IQVIA, Janssen, Leo, Lipidio, Merck, Novartis, Oruka, Paragon, Pfizer, Regeneron, Sanofi, Spherix Global Insights, Sun Pharma, Syncona, Takeda, UCB and Union; has acted as a clinical study investigator (institution has received clinical study funds) for AbbVie, Acelyrin, Almirall, Alumis, Amgen, Arcutis, Boehringer Ingelheim, Bristol Myers Squibb, Dermavant, Eli Lilly and Company, Galderma, Incyte, Janssen, Leo, Merck, Novartis, Pfizer, Regeneron, Sanofi, Sun Pharma, Takeda and UCB; owns stock in Lipidio and Oruka; and has acted as Member and Owner of Blauvelt Consulting, LLC. In this capacity, A.B. has provided scientific consulting services (for example, protocol development, data analysis) to the following companies: AbbVie, Almirall, Alumis, Amgen, Anaptysbio, Apogee, Arcutis, Astria, Boehringer Ingelheim, Bristol Myers Squibb, Celltrion, Corvus, Dermavant, Eli Lilly and Company, Galderma, GlaxoSmithKline, Immunovant, Incyte, IQVIA, Janssen, Leo, Lipidio, Merck, Novartis, Oruka, Paragon, Pfizer, Regeneron, Sanofi, Spherix Global Insights, Sun Pharma, Syncona, Takeda, UCB, Union and Zai Lab. K.C.D. has served as a consultant (received honoraria) for AbbVie, Amgen/Celgene, Boehringer Ingelheim, Bristol Myers Squibb, Lilly, FIDE (which is sponsored by multiple pharmaceutical companies), CorEvitas, Janssen, Leo, Novartis, Pfizer, Stiefel and CorEvitas; and as an investigator for AbbVie, Amgen/Celgene, Boehringer Ingelheim, Bristol Myers Squibb, CorEvitas, Lilly, Janssen, Novartis, Pfizer, Regeneron, Stiefel and UCB. Y.-H.H. has conducted clinical trials or received honoraria as a consultant for Abbvie, Bristol Myers Squibb, Celgene, Janssen-Cilag Pharmaceuticals, Novartis and Pfizer Pharmaceuticals. L.J.S. has provided education or served on the advisory boards for AbbVie, Almirall, Amgen, Aspire Pharma, Biogen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Celltrion, Fresenius Kabi, Galderma, Janssen, Leo, Lilly, Medac, Moonlake, Novartis, Pfizer, Sanofi, Takeda and UCB; and has received research funding from Janssen, Novartis and Pfizer. J.F.M. is a consultant and/or investigator for Amgen, Astra-Zeneca, Boehringer Ingelheim, Bristol Myers Squibb, Abbvie, Dermavant, Eli Lilly, Moonlake, Novartis, Janssen, UCB, Sanofi, Regeneron, Sun Pharma, Biogen and Pfizer. L.G. declares no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks V. Chandran, G. Girolomoni, Y. Tada and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Armstrong, A.W., Blauvelt, A., Callis Duffin, K. et al. Psoriasis. Nat Rev Dis Primers 11, 45 (2025). https://doi.org/10.1038/s41572-025-00630-5
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41572-025-00630-5
This article is cited by
-
Nanozymes for ATP/cAMP balance restoration and ROS scavenging in inflammatory dermatosis treatment and recurrence prevention
Journal of Nanobiotechnology (2026)
-
Renal biopsy findings in psoriasis patients with renal involvement: a descriptive clinicopathologic study
BMC Nephrology (2026)
-
A bilayered microneedle patch loaded with methotrexate and dexamethasone for transdermal treatment of psoriasis
Scientific Reports (2026)
-
Environmental toxicant ochratoxin A induces psoriasis based on network toxicology machine learning and molecular docking analyses
Scientific Reports (2026)
-
CYLD Limits Neutrophil-Driven Psoriatic Inflammation
Inflammation (2026)