Abstract
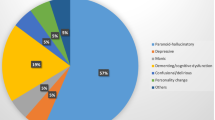
Autoimmune encephalitis (AE) is a treatable neuro-inflammatory disorder that is increasing in incidence. AE can be associated with malignancy (paraneoplastic), but in many patients no tumour is present. The disease presentation of AE can be heterogeneous depending on the type of antibody involved. AE is often caused by neuronal antibodies that bind to extracellular autoantigens (that is, N-methyl-d-aspartate receptor (NMDAR) and LGI1). Binding of these antibodies causes dysfunction of synaptic receptors, which leads to neurological symptoms. In these patients, treatment with immunosuppressive therapies is believed to decrease inflammation and deplete antibodies, and is essential for recovery. AE can also occur in patients with antibodies against intracellular antigens (such as Hu and Ri), often in the setting of malignancy. In these patients, tumour treatment is essential for stabilization or improvement. The most frequent symptoms of AE are cognitive problems, behavioural changes and seizures. Rapid recognition of AE syndromes is essential as earlier treatment of AE leads to better outcomes. For a definite diagnosis, the identification of an autoantibody is essential; however, some patients have seronegative AE. Most patients are severely affected during the acute disease stage, but long-term functional recovery is often good, particularly for patients without cancer. Nevertheless, residual anxiety, fatigue and cognitive problems can considerably affect quality of life. Research focuses on improving the understanding of pathophysiological processes, establishing patient-tailored outcome measures, optimizing treatment prediction models and studying different therapeutic regimens, all aiming to improve treatment and long-term outcomes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Dalmau, J. & Graus, F. Antibody-mediated encephalitis. N. Engl. J. Med. 378, 840–851 (2018).
Leypoldt, F. et al. Herpes simplex virus-1 encephalitis can trigger anti-NMDA receptor encephalitis: case report. Neurology 81, 1637–1639 (2013).
Abboud, H. et al. Autoimmune encephalitis: proposed best practice recommendations for diagnosis and acute management. J. Neurol. Neurosurg. Psychiatry 92, 757–768 (2021).
Dalmau, J. et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 7, 1091–1098 (2008).
Titulaer, M. J. et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 12, 157–165 (2013). This study is the first large cohort description, depicting anti-NMDAR encephalitis, showing the effects of different treatments on long-term outcomes.
Dalmau, J. et al. An update on anti-NMDA receptor encephalitis for neurologists and psychiatrists: mechanisms and models. Lancet Neurol. 18, 1045–1057 (2019).
Bastiaansen, A. E. M. et al. Anti-NMDAR encephalitis in the Netherlands, focusing on late-onset patients and antibody test accuracy. Neurol. Neuroimmunol. Neuroinflamm. 9, e1127 (2022).
van Sonderen, A. et al. The clinical spectrum of Caspr2 antibody-associated disease. Neurology 87, 521–528 (2016).
Irani, S. R. et al. Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann. Neurol. 69, 892–900 (2011). This is the first description of faciobrachial dystonic seizures, the seizure type pathognomonic for anti-LGI1 encephalitis: recognition leads to earlier treatment.
Gaig, C. et al. Clinical manifestations of the anti-IgLON5 disease. Neurology 88, 1736–1743 (2017).
Bastiaansen, A. E. M. et al. Autoimmune encephalitis resembling dementia syndromes. Neurol. Neuroimmunol. Neuroinflamm. https://doi.org/10.1212/NXI.0000000000001039 (2021).
Graus, F. et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 15, 391–404 (2016). This paper is the first international guideline for the diagnosis of autoimmune encephalitis.
van Sonderen, A. et al. Anti-LGI1 encephalitis: clinical syndrome and long-term follow-up. Neurology 87, 1449–1456 (2016).
Thompson, J. et al. The importance of early immunotherapy in patients with faciobrachial dystonic seizures. Brain 141, 348–356 (2018).
Van Steenhoven, R. W. et al. Mimics of autoimmune encephalitis: validation of the 2016 clinical autoimmune encephalitis criteria. Neurol. Neuroimmunol. Neuroinflamm. 10, e200148 (2023). This paper describes the validation of criteria recommended by Graus, and a description of mimics and red flags to identify these mimics.
Graus, F. et al. Updated diagnostic criteria for paraneoplastic neurologic syndromes. Neurol. Neuroimmunol. Neuroinflamm. https://doi.org/10.1212/NXI.0000000000001014 (2021). This paper describes the guideline to diagnose paraneoplastic neurological syndromes with the PNS Care score.
Dubey, D. et al. Randomized placebo-controlled trial of intravenous immunoglobulin in autoimmune LGI1/CASPR2 epilepsy. Ann. Neurol. 87, 313–323 (2020).
Banwell, B. et al. Diagnosis of myelin oligodendrocyte glycoprotein antibody-associated disease: International MOGAD panel proposed criteria. Lancet Neurol. 22, 268–282 (2023).
Wingerchuk, D. M. et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85, 177–189 (2015).
Reindl, M., Jarius, S., Rostasy, K. & Berger, T. Myelin oligodendrocyte glycoprotein antibodies: how clinically useful are they? Curr. Opin. Neurol. 30, 295–301 (2017).
Muniz-Castrillo, S. et al. Novelties in autoimmune and paraneoplastic cerebellar ataxias: twenty years of progresses. Cerebellum 21, 573–591 (2022).
Armangue, T. et al. Frequency, symptoms, risk factors, and outcomes of autoimmune encephalitis after herpes simplex encephalitis: a prospective observational study and retrospective analysis. Lancet Neurol. 17, 760–772 (2018).
Dubey, D. et al. Severe neurological toxicity of immune checkpoint inhibitors: growing spectrum. Ann. Neurol. 87, 659–669 (2020). This paper describes the link between immune checkpoint inhibitor neurotoxicity and autoimmune encephalitis.
Farina, A. et al. Neurological adverse events of immune checkpoint inhibitors and the development of paraneoplastic neurological syndromes. Lancet Neurol. 23, 81–94 (2024).
de Bruijn, M. et al. Pediatric autoimmune encephalitis: recognition and diagnosis. Neurol. Neuroimmunol. Neuroinflamm. 7, e682 (2020).
Chen, L. W. et al. Antibody investigations in 2,750 children with suspected autoimmune encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 11, e200182 (2024).
Hoftberger, R. et al. Encephalitis and AMPA receptor antibodies: novel findings in a case series of 22 patients. Neurology 84, 2403–2412 (2015).
Kim, T. J. et al. Anti-LGI1 encephalitis is associated with unique HLA subtypes. Ann. Neurol. 81, 183–192 (2017).
van Sonderen, A. et al. Anti-LGI1 encephalitis is strongly associated with HLA-DR7 and HLA-DRB4. Ann. Neurol. 81, 193–198 (2017).
Binks, S. et al. Distinct HLA associations of LGI1 and CASPR2-antibody diseases. Brain 141, 2263–2271 (2018).
Armangue, T. et al. Neurologic complications in herpes simplex encephalitis: clinical, immunological and genetic studies. Brain 146, 4306–4319 (2023). This paper describes the link between HSV1 encephalitis and anti-NMDAR encephalitis.
Mueller, S. H. et al. Genetic predisposition in anti-LGI1 and anti-NMDA receptor encephalitis. Ann. Neurol. 83, 863–869 (2018).
Peris Sempere, V. et al. Human leukocyte antigen association study reveals DRB1*04:02 effects additional to DRB1*07:01 in anti-LGI1 encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 9, e1140 (2022).
Hor, J. Y. & Fujihara, K. Epidemiology of myelin oligodendrocyte glycoprotein antibody-associated disease: a review of prevalence and incidence worldwide. Front. Neurol. 14, 1260358 (2023).
Tietz, A. K. et al. Genome-wide association study identifies 2 new loci associated with anti-NMDAR encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 8, e1085 (2021).
Alsalek, S. et al. Racial and ethnic disparities in the incidence of anti-NMDA receptor encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 11, e200255 (2024).
Jones, H. F. et al. Anti-N-methyl-d-aspartate receptor encephalitis in Maori and Pacific Island children in New Zealand. Dev. Med. Child Neurol. 59, 719–724 (2017).
Gong, X. et al. Efficacy and tolerability of intravenous immunoglobulin versus intravenous methylprednisolone treatment in anti-N-methyl-d-aspartate receptor encephalitis. Eur. J. Neurol. 29, 1117–1127 (2022).
Zhang, H. et al. Long-term prognosis of patients with anti-N-methyl-d-aspartate receptor encephalitis who underwent teratoma removal: an observational study. Front. Neurol. 13, 874867 (2022).
Liu, X. et al. Genome-wide association study identifies IFIH1 and HLA-DQB1*05:02 loci associated with anti-NMDAR encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 11, e200221 (2024).
Kerstens, J. et al. Autoimmune encephalitis and paraneoplastic neurologic syndromes: a nationwide study on epidemiology and antibody testing performance. Neurol. Neuroimmunol. Neuroinflamm. 11, e200318 (2024).
Oyama, M. et al. Association between HLA alleles and autoantibodies in dermatomyositis defined by sarcoplasmic expression of Myxovirus resistance Protein A. J. Rheumatol. 50, 1159–1164 (2023).
Segal, Y. et al. Toward curing neurological autoimmune disorders: biomarkers, immunological mechanisms, and therapeutic targets. Neuron https://doi.org/10.1016/j.neuron.2024.12.006 (2025).
Seute, T., Leffers, P., ten Velde, G. P. & Twijnstra, A. Neurologic disorders in 432 consecutive patients with small cell lung carcinoma. Cancer 100, 801–806 (2004).
Villagran-Garcia, M. et al. Revisiting anti-Hu paraneoplastic autoimmunity: phenotypic characterization and cancer diagnosis. Brain Commun. 5, fcad247 (2023).
Al-Diwani, A. et al. Cervical lymph nodes and ovarian teratomas as germinal centres in NMDA receptor-antibody encephalitis. Brain 145, 2742–2754 (2022).
Yeshokumar, A. K. et al. Neurobehavioral outcomes in autoimmune encephalitis. J. Neuroimmunol. 312, 8–14 (2017).
Chefdeville, A. et al. Immunopathological characterization of ovarian teratomas associated with anti-N-methyl-d-aspartate receptor encephalitis. Acta Neuropathol. Commun. 7, 38 (2019).
de Graaf, M. T. et al. HLA−DQ2+ individuals are susceptible to Hu-Ab associated paraneoplastic neurological syndromes. J. Neuroimmunol. 226, 147–149 (2010).
Camdessanche, J. P. et al. Expression of the onconeural CV2/CRMP5 antigen in thymus and thymoma. J. Neuroimmunol. 174, 168–173 (2006).
Small, M. et al. Genetic alterations and tumor immune attack in Yo paraneoplastic cerebellar degeneration. Acta Neuropathol. 135, 569–579 (2018).
Vialatte de Pemille, C. et al. Transcriptomic immune profiling of ovarian cancers in paraneoplastic cerebellar degeneration associated with anti-Yo antibodies. Br. J. Cancer 119, 105–113 (2018).
Sautes-Fridman, C., Petitprez, F., Calderaro, J. & Fridman, W. H. Tertiary lymphoid structures in the era of cancer immunotherapy. Nat. Rev. Cancer 19, 307–325 (2019).
Mellman, I., Chen, D. S., Powles, T. & Turley, S. J. The cancer-immunity cycle: Indication, genotype, and immunotype. Immunity 56, 2188–2205 (2023).
Cao, L. L. & Kagan, J. C. Targeting innate immune pathways for cancer immunotherapy. Immunity 56, 2206–2217 (2023).
Meffre, E. & O’Connor, K. C. Impaired B-cell tolerance checkpoints promote the development of autoimmune diseases and pathogenic autoantibodies. Immunol. Rev. 292, 90–101 (2019).
Sun, B. et al. Permissive central tolerance plus defective peripheral checkpoints license pathogenic memory B cells in CASPR2-antibody encephalitis. Sci. Adv. 11, eadr9986 (2025).
Damato, V. et al. Rituximab abrogates aquaporin-4-specific germinal center activity in patients with neuromyelitis optica spectrum disorders. Proc. Natl Acad. Sci. USA 119, e2121804119 (2022).
Esser, D. et al. Activated alphabeta T- and reduced mucosa-associated invariant T cells in LGI1- and CASPR2-encephalitis. Brain https://doi.org/10.1093/brain/awaf096 (2025).
Kornau, H. C. et al. Human cerebrospinal fluid monoclonal LGI1 autoantibodies increase neuronal excitability. Ann. Neurol. 87, 405–418 (2020).
Theorell, J. et al. Ultrahigh frequencies of peripherally matured LGI1- and CASPR2-reactive B cells characterize the cerebrospinal fluid in autoimmune encephalitis. Proc. Natl Acad. Sci. USA 121, e2311049121 (2024).
Malviya, M. et al. NMDAR encephalitis: passive transfer from man to mouse by a recombinant antibody. Ann. Clin. Transl. Neurol. 4, 768–783 (2017).
Dalmau, J., Geis, C. & Graus, F. Autoantibodies to synaptic receptors and neuronal cell surface proteins in autoimmune diseases of the central nervous system. Physiol. Rev. 97, 839–887 (2017).
Patterson, K. R., Dalmau, J. & Lancaster, E. Mechanisms of Caspr2 antibodies in autoimmune encephalitis and neuromyotonia. Ann. Neurol. 83, 40–51 (2018).
Zrzavy, T. et al. Neuropathological variability within a spectrum of NMDAR-encephalitis. Ann. Neurol. 90, 725–737 (2021).
Hara, A. et al. Circulating plasmablasts and follicular helper T-cell subsets are associated with antibody-positive autoimmune epilepsy. Front. Immunol. 13, 1048428 (2022).
Martinez-Hernandez, E. et al. Analysis of complement and plasma cells in the brain of patients with anti-NMDAR encephalitis. Neurology 77, 589–593 (2011).
Leypoldt, F. et al. Investigations on CXCL13 in anti-N-methyl-d-aspartate receptor encephalitis: a potential biomarker of treatment response. JAMA Neurol. 72, 180–186 (2015).
Magliozzi, R. et al. Meningeal B-cell follicles in secondary progressive multiple sclerosis associate with early onset of disease and severe cortical pathology. Brain 130, 1089–1104 (2007).
Wang, Y. et al. Early developing B cells undergo negative selection by central nervous system-specific antigens in the meninges. Immunity 54, 2784–2794.e2786 (2021).
Roberts, W. K. et al. Patients with lung cancer and paraneoplastic Hu syndrome harbor HuD-specific type 2 CD8+ T cells. J. Clin. Invest. 119, 2042–2051 (2009).
Voltz, R., Dalmau, J., Posner, J. B. & Rosenfeld, M. R. T-cell receptor analysis in anti-Hu associated paraneoplastic encephalomyelitis. Neurology 51, 1146–1150 (1998).
Bernal, F. et al. Immunohistochemical analysis of anti-Hu-associated paraneoplastic encephalomyelitis. Acta Neuropathol. 103, 509–515 (2002).
Vega, F. et al. Intrathecal synthesis of the anti-Hu antibody in patients with paraneoplastic encephalomyelitis or sensory neuronopathy: clinical−immunologic correlation. Neurology 44, 2145–2147 (1994).
Tanaka, K., Ding, X. & Tanaka, M. Effects of antineuronal antibodies from patients with paraneoplastic neurological syndrome on primary-cultured neurons. J. Neurol. Sci. 217, 25–30 (2004).
Sillevis Smitt, P. A., Manley, G. T. & Posner, J. B. Immunization with the paraneoplastic encephalomyelitis antigen HuD does not cause neurologic disease in mice. Neurology 45, 1873–1878 (1995).
Thaler, F. S. et al. Rituximab treatment and long-term outcome of patients with autoimmune encephalitis: real-world evidence from the GENERATE registry. Neurol. Neuroimmunol. Neuroinflamm. 8, e1088 (2021).
Planaguma, J. et al. Human N-methyl D-aspartate receptor antibodies alter memory and behaviour in mice. Brain 138, 94–109 (2015). This study provides the first description of passive transfer of human NMDAR autoantibodies into mice.
Lai, M. et al. Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. Lancet Neurol. 9, 776–785 (2010).
Lancaster, E. et al. Investigations of caspr2, an autoantigen of encephalitis and neuromyotonia. Ann. Neurol. 69, 303–311 (2011).
Irani, S. R. et al. Antibodies to Kv1 potassium channel-complex proteins leucine-rich, glioma inactivated 1 protein and contactin-associated protein-2 in limbic encephalitis, Morvan’s syndrome and acquired neuromyotonia. Brain 133, 2734–2748 (2010).
Sabater, L. et al. A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. Lancet Neurol. 13, 575–586 (2014).
Koneczny, I. et al. Common denominators in the immunobiology of IgG4 autoimmune diseases: what do glomerulonephritis, pemphigus vulgaris, myasthenia gravis, thrombotic thrombocytopenic purpura and autoimmune encephalitis have in common? Front. Immunol. 11, 605214 (2020).
van der Neut Kolfschoten, M. et al. Anti-inflammatory activity of human IgG4 antibodies by dynamic Fab arm exchange. Science 317, 1554–1557 (2007).
Huijbers, M. G. et al. MuSK myasthenia gravis monoclonal antibodies: valency dictates pathogenicity. Neurol. Neuroimmunol. Neuroinflamm. 6, e547 (2019).
Spatola, M. et al. Humoral signatures of MOG-antibody-associated disease track with age and disease activity. Cell Rep. Med. 4, 100913 (2023).
Jamet, Z. et al. NMDA receptor autoantibodies primarily impair the extrasynaptic compartment. Brain 147, 2745–2760 (2024).
Maudes, E., Jamet, Z., Marmolejo, L., Dalmau, J. O. & Groc, L. Positive allosteric modulation of NMDARs prevents the altered surface dynamics caused by patients’ antibodies. Neurol. Neuroimmunol. Neuroinflamm. 11, e200261 (2024).
Planaguma, J. et al. Ephrin-B2 prevents N-methyl-d-aspartate receptor antibody effects on memory and neuroplasticity. Ann. Neurol. 80, 388–400 (2016).
Carceles-Cordon, M. et al. NMDAR antibodies alter dopamine receptors and cause psychotic behavior in mice. Ann. Neurol. 88, 603–613 (2020).
Ramberger, M. et al. Distinctive binding properties of human monoclonal LGI1 autoantibodies determine pathogenic mechanisms. Brain 143, 1731–1745 (2020).
Michalski, K. et al. Structural and functional mechanisms of anti-NMDAR autoimmune encephalitis. Nat. Struct. Mol. Biol. 31, 1975–1986 (2024).
Maudes, E. et al. Neuro-immunobiology and treatment assessment in a mouse model of anti-NMDAR encephalitis. Brain https://doi.org/10.1093/brain/awae410 (2024).
Petit-Pedrol, M. et al. LGI1 antibodies alter Kv1.1 and AMPA receptors changing synaptic excitability, plasticity and memory. Brain 141, 3144–3159 (2018).
Abboud, H. et al. The clinical trial landscape in autoimmune encephalitis: challenges and opportunities. Neurology 104, e213487 (2025).
Ceanga, M. et al. Human NMDAR autoantibodies disrupt excitatory-inhibitory balance, leading to hippocampal network hypersynchrony. Cell Rep. 42, 113166 (2023).
Benoit, J. et al. Early-stage contactin-associated protein-like 2 limbic encephalitis: clues for diagnosis. Neurol. Neuroimmunol. Neuroinflamm. 10, e200041 (2023).
Day, G. S. Rapidly progressive dementia. Continuum 28, 901–936 (2022).
Flanagan, E. P. et al. Autoimmune encephalitis misdiagnosis in adults. JAMA Neurol. 80, 30–39 (2023).
Dalmau, J. & Graus, F. Diagnostic criteria for autoimmune encephalitis: utility and pitfalls for antibody-negative disease. Lancet Neurol. 22, 529–540 (2023).
van Steenhoven, R. W. et al. Clinical impact and safety of brain biopsy in unexplained central nervous system disorders: a real-world cohort study. Ann. Clin. Transl. Neurol. https://doi.org/10.1002/acn3.70000 (2025).
Lee, W. J. et al. Seronegative autoimmune encephalitis: clinical characteristics and factors associated with outcomes. Brain 145, 3509–3521 (2022).
Hartung, T. J. et al. MRI findings in autoimmune encephalitis. Rev. Neurol. 180, 895–907 (2024).
Spatola, M. et al. Investigations in GABA(A) receptor antibody-associated encephalitis. Neurology 88, 1012–1020 (2017).
Kelly, M. J. et al. Magnetic resonance imaging characteristics of LGI1-antibody and CASPR2-antibody encephalitis. JAMA Neurol. 81, 525–533 (2024).
Lee, W. J., Lee, S. T., Kim, D. Y., Kim, S. & Chu, K. Disease progression and brain atrophy in NMDAR encephalitis: associated factor and clinical implication. Ann. Clin. Transl. Neurol. 9, 912–924 (2022).
Gadoth, A. et al. Elevated LGI1-IgG CSF index predicts worse neurological outcome. Ann. Clin. Transl. Neurol. 5, 646–650 (2018).
Schmitt, S. E. et al. Extreme delta brush: a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology 79, 1094–1100 (2012).
Sonderen, A. V. et al. Predictive value of electroencephalography in anti-NMDA receptor encephalitis. J. Neurol. Neurosurg. Psychiatry 89, 1101–1106 (2018).
Leypoldt, F. et al. Fluorodeoxyglucose positron emission tomography in anti-N-methyl-d-aspartate receptor encephalitis: distinct pattern of disease. J. Neurol. Neurosurg. Psychiatry 83, 681–686 (2012).
Probasco, J. C. et al. Decreased occipital lobe metabolism by FDG-PET/CT: an anti-NMDA receptor encephalitis biomarker. Neurol. Neuroimmunol. Neuroinflamm. 5, e413 (2018).
Dechelotte, B. et al. Diagnostic yield of commercial immunodots to diagnose paraneoplastic neurologic syndromes. Neurol. Neuroimmunol. Neuroinflamm. 7, e701 (2020).
Gresa-Arribas, N. et al. Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol. 13, 167–177 (2014).
Guasp, M., Modena, Y., Armangue, T., Dalmau, J. & Graus, F. Clinical features of seronegative, but CSF antibody-positive, anti-NMDA receptor encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 7, e659 (2020).
Flanagan, E. P. et al. Glial fibrillary acidic protein immunoglobulin G as biomarker of autoimmune astrocytopathy: analysis of 102 patients. Ann. Neurol. 81, 298–309 (2017).
McCracken, L. et al. Improving the antibody-based evaluation of autoimmune encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 4, e404 (2017).
Ruiz-Garcia, R., Martinez-Hernandez, E., Saiz, A., Dalmau, J. & Graus, F. The diagnostic value of onconeural antibodies depends on how they are tested. Front. Immunol. 11, 1482 (2020).
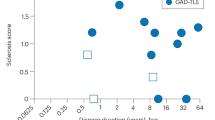
Munoz-Lopetegi, A. et al. Neurologic syndromes related to anti-GAD65: clinical and serologic response to treatment. Neurol. Neuroimmunol. Neuroinflamm. 7, e696 (2020).
Varley, J. A. et al. Absence of neuronal autoantibodies in neuropsychiatric systemic lupus erythematosus. Ann. Neurol. 88, 1244–1250 (2020).
Titulaer, M. J. et al. Overlapping demyelinating syndromes and anti-N-methyl-d-aspartate receptor encephalitis. Ann. Neurol. 75, 411–428 (2014).
Lee, W. J. et al. MOG antibody-associated encephalitis in adult: clinical phenotypes and outcomes. J. Neurol. Neurosurg. Psychiatry 94, 102–112 (2023).
Gravier-Dumonceau, A. et al. Glial fibrillary acidic protein autoimmunity: a French cohort study. Neurology 98, e653–e668 (2022).
Muniz-Castrillo, S. et al. Anti-CASPR2 clinical phenotypes correlate with HLA and immunological features. J. Neurol. Neurosurg. Psychiatry 91, 1076–1084 (2020).
Yogeshwar, S. M. et al. HLA-DQB1*05 subtypes and not DRB1*10:01 mediates risk in anti-IgLON5 disease. Brain 147, 2579–2592 (2024).
Dubey, D. et al. Expanded clinical phenotype, oncological associations, and immunopathologic insights of paraneoplastic Kelch-like Protein-11 encephalitis. JAMA Neurol. 77, 1420–1429 (2020).
Titulaer, M. J. et al. Screening for tumours in paraneoplastic syndromes: report of an EFNS task force. Eur. J. Neurol. 18, 19–e13 (2011).
Lee, W. J. et al. Teratoma removal, steroid, IVIG, rituximab and tocilizumab (T-SIRT) in anti-NMDAR encephalitis. Neurotherapeutics 18, 474–487 (2021).
Villagran-Garcia, M. et al. Paraneoplastic neurological syndromes associated with renal or bladder cancer: case series and PRISMA-IPD systematic review. J. Neurol. 270, 283–299 (2023).
Abbatemarco, J. R. et al. Autoimmune neurology: the need for comprehensive care. Neurol. Neuroimmunol. Neuroinflamm. 8, e1033 (2021).
Abboud, H. et al. Autoimmune encephalitis: proposed recommendations for symptomatic and long-term management. J. Neurol. Neurosurg. Psychiatry 92, 897–907 (2021).
de Montmollin, E. et al. Anti-N-methyl-d-aspartate receptor encephalitis in adult patients requiring intensive care. Am. J. Respir. Crit. Care Med. 195, 491–499 (2017).
Nosadini, M. et al. Use and safety of immunotherapeutic management of N-methyl-d-aspartate receptor antibody encephalitis: a meta-analysis. JAMA Neurol. 78, 1333–1344 (2021).
Greenlee, J. E. et al. Paraneoplastic and other autoimmune encephalitides: antineuronal antibodies, T lymphocytes, and questions of pathogenesis. Front. Neurol. 12, 744653 (2021).
de Bruijn, M. et al. Evaluation of seizure treatment in anti-LGI1, anti-NMDAR, and anti-GABA(B)R encephalitis. Neurology 92, e2185–e2196 (2019).
Witt, K. A. & Sandoval, K. E. Steroids and the blood–brain barrier: therapeutic implications. Adv. Pharmacol. 71, 361–390 (2014).
Zanatta, E., Cozzi, M., Marson, P. & Cozzi, F. The role of plasma exchange in the management of autoimmune disorders. Br. J. Haematol. 186, 207–219 (2019).
Klemencic Kozul, T., Yudina, A., Donovan, C., Pinto, A. & Osman, C. Cost-minimisation analysis of plasma exchange versus IVIg in the treatment of autoimmune neurological conditions. BMC Health Serv. Res. 22, 904 (2022).
Chaigne, B. & Mouthon, L. Mechanisms of action of intravenous immunoglobulin. Transfus. Apher. Sci. 56, 45–49 (2017).
Forsthuber, T. G., Cimbora, D. M., Ratchford, J. N., Katz, E. & Stuve, O. B cell-based therapies in CNS autoimmunity: differentiating CD19 and CD20 as therapeutic targets. Ther. Adv. Neurol. Disord. 11, 1756286418761697 (2018).
Makuch, M. et al. N-Methyl-d-aspartate receptor antibody production from germinal center reactions: therapeutic implications. Ann. Neurol. 83, 553–561 (2018).
Bar-Or, A., O’Brien, S. M., Sweeney, M. L., Fox, E. J. & Cohen, J. A. Clinical perspectives on the molecular and pharmacological attributes of anti-CD20 therapies for multiple sclerosis. CNS Drugs 35, 985–997 (2021).
Damato, V., Evoli, A. & Iorio, R. Efficacy and safety of rituximab therapy in neuromyelitis optica spectrum disorders: a systematic review and meta-analysis. JAMA Neurol. 73, 1342–1348 (2016).
Kosmidis, M. L. & Dalakas, M. C. Practical considerations on the use of rituximab in autoimmune neurological disorders. Ther. Adv. Neurol. Disord. 3, 93–105 (2010).
Dale, R. C. et al. Utility and safety of rituximab in pediatric autoimmune and inflammatory CNS disease. Neurology 83, 142–150 (2014).
Nepal, G. et al. Efficacy and safety of rituximab in autoimmune encephalitis: a meta-analysis. Acta Neurol. Scand. 142, 449–459 (2020).
van Swieten, J. C., Koudstaal, P. J., Visser, M. C., Schouten, H. J. & van Gijn, J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19, 604–607 (1988).
Cree, B. A. C. et al. Inebilizumab for the treatment of neuromyelitis optica spectrum disorder (N-MOmentum): a double-blind, randomised placebo-controlled phase 2/3 trial. Lancet 394, 1352–1363 (2019).
Wong, K. H. et al. A phase-2B double-blind randomized international prospective trial of inebilizumab in NMDAR encephalitis: the ExTINGUISH trial. Neurol. Open. Access. 1, e000007 (2025).
Pittock, S. J. Association of B cell subsets and aquaporin-4 antibody titers with disease activity in participants in the N-MOmentum trial receiving inebilizumab treatment Neurology https://doi.org/10.1212/WNL.0000000000202362 (2023).
Karlowicz, J. R. et al. Predictors of hospitalization due to infection in rituximab-treated MS patients. Mult. Scler. Relat. Disord. 71, 104556 (2023).
Faissner, S. et al. Successful use of anti-CD19 CAR T cells in severe treatment-refractory stiff-person syndrome. Proc. Natl Acad. Sci. USA 121, e2403227121 (2024).
Qin, C. et al. Anti-BCMA CAR T-cell therapy CT103A in relapsed or refractory AQP4-IgG seropositive neuromyelitis optica spectrum disorders: phase 1 trial interim results. Signal Transduct. Target. Ther. 8, 5 (2023).
Muller, F. et al. CD19 CAR T-cell therapy in autoimmune disease — a case series with follow-up. N. Engl. J. Med. 390, 687–700 (2024).
Makhani, N. et al. Cyclophosphamide therapy in pediatric multiple sclerosis. Neurology 72, 2076–2082 (2009).
Le Guenno, G. et al. Incidence and predictors of urotoxic adverse events in cyclophosphamide-treated patients with systemic necrotizing vasculitides. Arthritis Rheum. 63, 1435–1445 (2011).
Liu, M. et al. Mycophenolate mofetil reduces the risk of relapse in anti-leucine-rich glioma-inactivated protein 1 encephalitis: a prospective observational cohort study. Neurol. Sci. https://doi.org/10.1007/s10072-023-06968-6 (2023).
Azodi, S. & Jacobson, S. Cytokine therapies in neurological disease. Neurotherapeutics 13, 555–561 (2016).
Khan, A. W., Farooq, M., Hwang, M. J., Haseeb, M. & Choi, S. Autoimmune neuroinflammatory diseases: role of interleukins. Int. J. Mol. Sci. 24, 7960 (2023).
Erta, M., Quintana, A. & Hidalgo, J. Interleukin-6, a major cytokine in the central nervous system. Int. J. Biol. Sci. 8, 1254–1266 (2012).
Kleiter, I. et al. Long-term efficacy of satralizumab in AQP4-IgG-seropositive neuromyelitis optica spectrum disorder from SAkuraSky and SAkuraStar. Neurol. Neuroimmunol. Neuroinflamm. 10, e200071 (2023).
Yamamura, T. et al. Trial of satralizumab in neuromyelitis optica spectrum disorder. N. Engl. J. Med. 381, 2114–2124 (2019).
Lee, S. T. et al. Innovation and optimization in autoimmune encephalitis trials: the design and rationale for the phase 3, randomized study of satralizumab in patients with NMDAR-IgG-antibody-positive or LGI1-IgG-antibody-positive autoimmune encephalitis (CIELO). Front. Neurol. 15, 1437913 (2024).
Pyzik, M., Kozicky, L. K., Gandhi, A. K. & Blumberg, R. S. The therapeutic age of the neonatal Fc receptor. Nat. Rev. Immunol. 23, 415–432 (2023).
Newland, A. C. et al. Phase 2 study of efgartigimod, a novel FcRn antagonist, in adult patients with primary immune thrombocytopenia. Am. J. Hematol. 95, 178–187 (2020).
Bril, V. et al. Efficacy and safety of rozanolixizumab in moderate to severe generalized myasthenia gravis: a phase 2 randomized control trial. Neurology 96, e853–e865 (2021).
Karunaratne, K. et al. Bortezomib for anti-NMDAR encephalitis following daclizumab treatment in a patient with multiple sclerosis. BMJ Neurol. Open 3, e000096 (2021).
Scheibe, F. et al. Bortezomib for treatment of therapy-refractory anti-NMDA receptor encephalitis. Neurology 88, 366–370 (2017).
Turnbull, M. T. et al. Early bortezomib therapy for refractory anti-NMDA receptor encephalitis. Front. Neurol. 11, 188 (2020).
Simmons, M. L. & Perez, K. A. Bortezomib for treatment of anti-NMDA receptor encephalitis in a pediatric patient refractory to conventional therapy. Am. J. Health Syst. Pharm. 78, 395–400 (2021).
Wickel, J. et al. Generate-Boost: study protocol for a prospective, multicenter, randomized controlled, double-blinded phase II trial to evaluate efficacy and safety of bortezomib in patients with severe autoimmune encephalitis. Trials 21, 625 (2020).
Huehnchen, P. et al. Bortezomib at therapeutic doses poorly passes the blood-brain barrier and does not impair cognition. Brain Commun. 2, fcaa021 (2020).
Mittal, M. K. et al. Autoimmune encephalitis in the ICU: analysis of phenotypes, serologic findings, and outcomes. Neurocrit. Care 24, 240–250 (2016).
Schubert, J. et al. Management and prognostic markers in patients with autoimmune encephalitis requiring ICU treatment. Neurol. Neuroimmunol. Neuroinflamm. 6, e514 (2019).
Dalmau, J. et al. Clinical analysis of anti-Ma2-associated encephalitis. Brain 127, 1831–1844 (2004).
Banks, J. L. & Marotta, C. A. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke 38, 1091–1096 (2007).
Morgan, A. et al. Longitudinal disability, cognitive impairment, and mood symptoms in patients with anti-NMDA receptor encephalitis. Neurology 102, e208019 (2024).
Munoz-Lopetegi, A., Graus, F., Dalmau, J. & Santamaria, J. Sleep disorders in autoimmune encephalitis. Lancet Neurol. 19, 1010–1022 (2020).
Diaz-Arias, L. A. et al. Fatigue in survivors of autoimmune encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 8, e1064 (2021).
Binks, S. N. M. et al. Residual fatigue and cognitive deficits in patients after leucine-rich glioma-inactivated 1 antibody encephalitis. JAMA Neurol. 78, 617–619 (2021).
Cai, M. T. et al. Validation of the clinical assessment scale for autoimmune encephalitis: a multicenter study. Neurol. Ther. 10, 985–1000 (2021).
Aboseif, A. et al. Clinical determinants of longitudinal disability in LGI-1-IgG autoimmune encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 11, e200178 (2024).
Galioto, R., Aboseif, A., Krishnan, K., Lace, J. & Kunchok, A. Cognitive outcomes in anti-LGI-1 encephalitis. J. Int. Neuropsychol. Soc. 29, 541–550 (2023).
Finke, C. et al. Cognitive deficits following anti-NMDA receptor encephalitis. J. Neurol. Neurosurg. Psychiatry 83, 195–198 (2012).
de Bruijn, M. et al. Long-term neuropsychological outcome following pediatric anti-NMDAR encephalitis. Neurology 90, e1997–e2005 (2018).
Heine, J. et al. Long-term cognitive outcome in anti-N-Methyl-D-aspartate receptor encephalitis. Ann. Neurol. 90, 949–961 (2021). This paper describes the long term neurocognitive outcomes in anti-NMDAR encephalitis.
Guasp, M. et al. Clinical characterisation of patients in the post-acute stage of anti-NMDA receptor encephalitis: a prospective cohort study and comparison with patients with schizophrenia spectrum disorders. Lancet Neurol. 21, 899–910 (2022).
Tellez-Martinez, A. et al. Suicidal thoughts and behaviors in anti-NMDA receptor encephalitis: psychopathological features and clinical outcomes. J. Neuropsychiatry Clin. Neurosci. https://doi.org/10.1176/appi.neuropsych.20220200 (2023).
Dalmau, J. et al. Paraneoplastic anti-N-methyl-d-aspartate receptor encephalitis associated with ovarian teratoma. Ann. Neurol. 61, 25–36 (2007). This study first described anti-NMDAR encephalitis, opening the field of autoimmune encephalitis, and (in)directly leading to the discovery of many new diseases in the years following.
Munoz-Lopetegi, A. et al. Neurological, psychiatric, and sleep investigations after treatment of anti-leucine-rich glioma-inactivated protein 1 (LGI1) encephalitis in Spain: a prospective cohort study. Lancet Neurol. 23, 256–266 (2024).
Geis, C., Planaguma, J., Carreno, M., Graus, F. & Dalmau, J. Autoimmune seizures and epilepsy. J. Clin. Invest. 129, 926–940 (2019).
Rada, A. et al. Seizures associated with antibodies against cell surface antigens are acute symptomatic and not indicative of epilepsy: insights from long-term data. J. Neurol. 268, 1059–1069 (2021).
Smith, K. M. et al. Seizure characteristics and outcomes in patients with neurological conditions related to high-risk paraneoplastic antibodies. Epilepsia 64, 2385–2398 (2023).
Shen, C. H. et al. Seizures and risk of epilepsy in anti-NMDAR, anti-LGI1, and anti-GABA(B) R encephalitis. Ann. Clin. Transl. Neurol. 7, 1392–1399 (2020).
Smith, K. M., Dubey, D., Liebo, G. B., Flanagan, E. P. & Britton, J. W. Clinical course and features of seizures associated with LGI1-antibody encephalitis. Neurology 97, e1141–e1149 (2021).
Baumgartner, T. et al. Seizure underreporting in LGI1 and CASPR2 antibody encephalitis. Epilepsia 63, e100–e105 (2022).
Feyissa, A. M., Chiriboga, A. S. L. & Britton, J. W. Antiepileptic drug therapy in patients with autoimmune epilepsy. Neurol. Neuroimmunol. Neuroinflamm. 4, e353 (2017).
Heine, J. et al. Patient-reported outcome measures in NMDA receptor encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 12, e200343 (2025).
Brenner, J. et al. Long-term cognitive, functional, and patient-reported outcomes in patients with anti-NMDAR encephalitis. Neurology 103, e210109 (2024).
Kelly, M. J. et al. Capturing what matters: patient-reported LGI1-ANTibody encephalitis outcome RatiNg scale (LANTERN). Ann. Clin. Transl. Neurol. 12, 821–831 (2025).
Brenner, J. et al. PROSE: a newly developed patient-reported outcome scale for encephalitis. Neurology 103, S117–S117 (2024).
Dubey, D., Pittock, S. J. & McKeon, A. Antibody prevalence in epilepsy and encephalopathy score: increased specificity and applicability. Epilepsia 60, 367–369 (2019).
de Bruijn, M. et al. Antibodies contributing to focal epilepsy signs and symptoms score. Ann. Neurol. 89, 698–710 (2021).
Guasp, M. et al. Neurofilament light chain levels in anti-NMDAR encephalitis and primary psychiatric psychosis. Neurology 98, e1489–e1498 (2022).
Dubey, D. et al. Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Ann. Neurol. 83, 166–177 (2018).
Zuliani, L. et al. Epidemiology of neuronal surface antibody-mediated autoimmune encephalitis and antibody-based diagnostics. J. Neuroimmunol. 357, 577598 (2021).
Granerod, J. et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect. Dis. 10, 835–844 (2010).
Hebert, J. et al. Epidemiology of paraneoplastic neurologic syndromes and autoimmune encephalitides in France. Neurol. Neuroimmunol. Neuroinflamm. 7, e883 (2020).
Nissen, M. S. et al. NMDA-receptor encephalitis in Denmark from 2009 to 2019: a national cohort study. J. Neurol. 269, 1618–1630 (2022).
Wong, C. K. et al. High incidence of NMDAR encephalitis among Austronesians: a population-based study in Sabah, Malaysia. J. Neuroimmunol. 356, 577584 (2021).
Boesen, M. S., Born, A. P., Lydolph, M. C., Blaabjerg, M. & Borresen, M. L. Pediatric autoimmune encephalitis in Denmark during 2011–17: a nationwide multicenter population-based cohort study. Eur. J. Paediatr. Neurol. 23, 639–652 (2019).
Wright, S. et al. N-Methyl-d-aspartate receptor antibody-mediated neurological disease: results of a UK-based surveillance study in children. Arch. Dis. Child. 100, 521–526 (2015).
Ho, A. C. et al. Anti-N-methyl-d-aspartate receptor encephalitis in children: incidence and experience in Hong Kong. Brain Dev. 40, 473–479 (2018).
Liem, B. et al. Encephalitis in adults in the Auckland and Northland regions of New Zealand, 2009 to 2018. J. Clin. Neurosci. 107, 172–177 (2023).
Vogrig, A. et al. Epidemiology of paraneoplastic neurological syndromes: a population-based study. J. Neurol. 267, 26–35 (2020).
Shah, S. et al. Population-based epidemiology study of paraneoplastic neurologic syndromes. Neurol. Neuroimmunol. Neuroinflamm. 9, e1124 (2022).
Author information
Authors and Affiliations
Contributions
Introduction (M.J.T. and M.A.A.M.d.B.); Epidemiology (M.J.T., M.A.A.M.d.B., F.L. and J.D.); Mechanisms/pathophysiology (M.J.T., M.A.A.M.d.B., F.L. and J.D.); Diagnosis, screening and prevention (M.J.T., M.A.A.M.d.B., S.-T.L. and J.H.); Management (M.J.T., M.A.A.M.d.B., S.L.C. and S.R.I.); Quality of life (M.J.T., M.A.A.M.d.B., A.E. and A.K.); Outlook (M.J.T. and M.A.A.M.d.B.); overview of the Primer (M.J.T. and M.A.A.M.d.B.).
Corresponding author
Ethics declarations
Competing interests
F.L. is supported by E-Rare Joint Transnational research support (ERA-Net, LE3064/2-1), European Joint Program for Neurodegenerative Diseases (EJPRD) IGNITEMIND (01ED2506B), ERA-Net MICE-AE (01EW2507B), Stiftung Pathobiochemie of the German Society for Laboratory Medicine and HORIZON MSCA 2022 Doctoral Network 101119457 — IgG4-TREAT and discloses speaker honoraria from Grifols, Teva, Biogen, Bayer, Roche, Novartis, Fresenius, travel funding from Merck, Grifols and Bayer and serving on advisory boards for Roche, Biogen and Alexion. J.D. declares research funding to the institution from Instituto de Salud Carlos III, La Caixa Foundation, Edmond J. Safra Foundation, Department of Health, Generalitat de Catalunya; a research contract from Sage Therapeutics; unrestricted research support from Euroimmun, Inc; and royalties paid to the author from Euroimmun, Inc. for the use of NMDAR, GABAa, GABAb, DPPX and IgLOn5 as antibody tests. S.-T.L. is a steering committee member of the CIELO trial (Roche/Genentech) and has served on advisory boards for Argenx, Arialys Therapeutics, Advanced Neural Technologies and Piehealthcare. He is a named inventor of the CASE score. S.L.C. is a principal investigator of the ExTINGUISH Trial for NMDAR Encephalitis, supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under award number U01NS120901. Additional support was provided by Amgen for this investigator-initiated trial. This report does not represent the official view of the National Institute of Neurological Disorders and Stroke (NINDS), the National Institutes of Health (NIH) or any part of the US Federal Government. No support or endorsement of this article by the NINDS or NIH is intended or should be inferred. S.L.C. is editorial board member for Neurology: Neuroimmunology & Neuroinflammation. S.R.I. has performed this research funded in whole or in part by a senior clinical fellowship from the Medical Research Council (MR/V007173/1) and Wellcome Trust Fellowship (104079/Z/14/Z), the Kogod Centre on Aging and by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC). For the purpose of Open Access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript (AAM) version arising from this submission. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. S.R.I. has received honoraria/research support from Amgen, Argenx, UCB, Roche, Janssen, IQVIA, Clarivate, Slingshot Insights, Cerebral therapeutics, BioHaven therapeutics, CSL Behring and ONO Pharma. S.R.I. receives licensed royalties on patent application WO/2010/046716 entitled ‘Neurological Autoimmune Disorders’, and has filed two other patents entitled ‘Diagnostic method and therapy’ (WO2019211633 and US app 17/051,930; PCT application WO202189788A1) and ‘Biomarkers’ (WO202189788A1, US App 18/279,624; PCT/GB2022/050614). M.J.T. has received research funds for serving on a scientific advisory board of AmGen, UCB, Arialys and ArgenX; received funds from Dioraphte (2001 0403); filed a patent for methods for typing neurologic disorders and cancer, and devices for use therein; obtained a copyright (on behalf of Erasmus MC) for the PROSE, an AE-specific patient-reported outcome measure; received research funds for consultation at Guidepoint Global LLC, an unrestricted research grant from CSL Behring (Interlaken Leadership Award) and an unrestricted research grant from Euroimmun. He was supported by an E-RARE3 grant (UltraAIE, ZonMW), ACT-MD (ZonMW), PARADE-VIMP (ZonMW) and ItsME. M.J.T. has received publishing royalties from UpToDate Inc. M.J.T. served as an associate editor for the Dutch Journal of Neurology and Neurosurgery (Tijdschrift voor Neurologie en Neurochirurgie, TNN) and as editorial board member for Neurology: Neuroimmunology & Neuroinflammation. M.J.T. is a scientific advisory board member for Encephalitis International, Autoimmune Encephalitis Alliance and ItsME (patient advocacy foundations). The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks H. Wiendl, C. Finke and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Bruijn, M.A.A.M., Leypoldt, F., Dalmau, J. et al. Autoimmune encephalitis. Nat Rev Dis Primers 11, 65 (2025). https://doi.org/10.1038/s41572-025-00650-1
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41572-025-00650-1