Abstract
Decompensated cirrhosis describes an advanced clinical stage with clinical complications, such as ascites, variceal bleeding or hepatic encephalopathy, associated with considerable mortality. Portal hypertension is the main risk factor for developing decompensation in patients with compensated cirrhosis, whereas systemic inflammation is the key driving force for organ failure, that is, for acute-on-chronic liver failure in later stages of cirrhosis. As portal hypertension and systemic inflammation coexist in patients with cirrhosis, an improved understanding of their interaction and dynamic role in distinct stages of cirrhosis is an important step forward towards the development of urgently needed therapeutic interventions. Based on emerging evidence from clinical and translational studies, a novel concept of different predominant pathomechanisms of decompensated cirrhosis is presented, which includes portal hypertension-predominant, systemic inflammmation-predominant and mixed portal hypertension–systemic inflammation phenotypes. A comprehensive set of biomarkers and surrogates of portal hypertension and systemic inflammation might assist clinicians in identifying a predominance of one over the other cirrhosis phenotype. As survival rates of patients with decompensated cirrhosis have remained detrimental without liver transplantation over the past decades, future studies should build on this knowledge to develop effective portal hypertension and systemic inflammation-directed therapies for this underserved population.
Key points
-
Cirrhosis decompensation is defined by the development of ascites, variceal bleeding, hepatic encephalopathy, or jaundice and is linked to a considerable increase in the risk for mortality.
-
In compensated cirrhosis, the magnitude of portal hypertension is the key determinant of the risk for developing decompensation.
-
Inflammation, and particularly the severity of systemic inflammation, is particularly pronounced in advanced stages of cirrhosis, that is, in patients with further decompensated cirrhosis or acute-on-chronic liver failure.
-
We propose a concept of ‘pathophysiological’ phenotypes of decompensated cirrhosis by predominance of portal hypertension, systemic inflammation, or even mixed systemic inflammation and portal hypertension.
-
The evidence for the interaction of portal hypertension and systemic inflammation in the key pathomechanism driving cirrhosis decompensation and end-organ dysfunction or failure is presented.
-
A summary of promising therapeutic approaches targeting portal hypertension and systemic inflammation for which translational or clinical studies have been or are being conducted is presented.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
D’Amico, G., Garcia-Tsao, G. & Pagliaro, L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J. Hepatol. 44, 217–231 (2006).
de Franchis, R. et al. Baveno VII — renewing consensus in portal hypertension. J. Hepatol. 76, 959–974 (2022).
Jalan, R. et al. New clinical and pathophysiological perspectives defining the trajectory of cirrhosis. J. Hepatol. 75, S14–S26 (2021).
Trebicka, J. et al. The PREDICT study uncovers three clinical courses of acutely decompensated cirrhosis that have distinct pathophysiology. J. Hepatol. 73, 842–854 (2020).
D’Amico, G., Bernardi, M. & Angeli, P. Towards a new definition of decompensated cirrhosis. J. Hepatol. 76, 202–207 (2022).
Tonon, M. et al. A new clinical and prognostic characterization of the patterns of decompensation of cirrhosis. J. Hepatol. 80, 603–609 (2024).
Ripoll, C. et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology 133, 481–488 (2007).
Paternostro, R. et al. Hepatic venous pressure gradient predicts risk of hepatic decompensation and liver-related mortality in patients with MASLD. J. Hepatol. 81, 827–836 (2024).
Moreau, R. et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 144, 1426–1437 (2013).
Trebicka, J. et al. Addressing profiles of systemic inflammation across the different clinical phenotypes of acutely decompensated cirrhosis. Front. Immunol. 10, 2014 (2019).
Clària, J. et al. Systemic inflammation in decompensated cirrhosis: characterization and role in acute-on-chronic liver failure. Hepatology 64, 1249–1264 (2016).
Gustot, T. et al. Clinical course of acute-on-chronic liver failure syndrome and effects on prognosis. Hepatology 62, 243–252 (2015).
Costa, D. et al. Systemic inflammation increases across distinct stages of advanced chronic liver disease and correlates with decompensation and mortality. J. Hepatol. 74, 819–828 (2021).
Turco, L. et al. Cardiopulmonary hemodynamics and C-reactive protein as prognostic indicators in compensated and decompensated cirrhosis. J. Hepatol. 68, 949–958 (2018).
Colecchia, A. et al. Measurement of spleen stiffness to evaluate portal hypertension and the presence of esophageal varices in patients with HCV-related cirrhosis. Gastroenterology 143, 646–654 (2012).
Ferlitsch, M. et al. Von Willebrand factor as new noninvasive predictor of portal hypertension, decompensation and mortality in patients with liver cirrhosis. Hepatology 56, 1439–1447 (2012).
Simbrunner, B. et al. Non-invasive detection of portal hypertension by enhanced liver fibrosis score in patients with different aetiologies of advanced chronic liver disease. Liver Int. 40, 1713–1724 (2020).
Thorhauge, K. H. et al. Using liver stiffness to predict and monitor the risk of decompensation and mortality in patients with alcohol-related liver disease. J. Hepatol. 81, 876–886 (2024).
Monteiro, S. et al. Differential inflammasome activation predisposes to acute-on-chronic liver failure in human and experimental cirrhosis with and without previous decompensation. Gut 70, 379–387 (2021).
Juanola, A. et al. Novel prognostic biomarkers in decompensated cirrhosis: a systematic review and meta-analysis. Gut 73, 156–165 (2023).
Albillos, A. et al. Cirrhosis-associated immune dysfunction. Nat. Rev. Gastroenterol. Hepatol. 19, 112–134 (2022).
Simbrunner, B. et al. Dysregulated biomarkers of innate and adaptive immunity predict infections and disease progression in cirrhosis. JHEP Rep. 5, 100624 (2023).
Hackstein, C. P. et al. Gut microbial translocation corrupts myeloid cell function to control bacterial infection during liver cirrhosis. Gut 66, 507–518 (2017).
Arvaniti, V. et al. Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis. Gastroenterology 139, 1246–1256 (2010).
Thabut, D. et al. Model for end-stage liver disease score and systemic inflammatory response are major prognostic factors in patients with cirrhosis and acute functional renal failure. Hepatology 46, 1872–1882 (2007).
Fernandez, M. et al. Reversal of portal hypertension and hyperdynamic splanchnic circulation by combined vascular endothelial growth factor and platelet-derived growth factor blockade in rats. Hepatology 46, 1208–1217 (2007).
DeLeve, L. D., Wang, X. & Guo, Y. Sinusoidal endothelial cells prevent rat stellate cell activation and promote reversion to quiescence. Hepatology 48, 920–930 (2008).
Xie, G. et al. Role of differentiation of liver sinusoidal endothelial cells in progression and regression of hepatic fibrosis in rats. Gastroenterology 142, 918–927.e6 (2012).
Xie, G. et al. Hedgehog signalling regulates liver sinusoidal endothelial cell capillarisation. Gut 62, 299–309 (2013).
Copple, B. L., Bai, S., Burgoon, L. D. & Moon, J.-O. Hypoxia-inducible factor-1α regulates the expression of genes in hypoxic hepatic stellate cells important for collagen deposition and angiogenesis. Liver Int. 31, 230–244 (2011).
Gracia-Sancho, J. et al. Endothelial expression of transcription factor Kruppel-like factor 2 and its vasoprotective target genes in the normal and cirrhotic rat liver. Gut 60, 517–524 (2011).
Shah, V. et al. Impaired endothelial nitric oxide synthase activity associated with enhanced caveolin binding in experimental cirrhosis in the rat. Hepatology 46, 537–547 (2007).
Gracia-Sancho, J. et al. Increased oxidative stress in cirrhotic rat livers: a potential mechanism contributing to reduced nitric oxide bioavailability. Hepatology 47, 1248–1256 (2008).
Rockey, D. C. & Weisiger, R. A. Endothelin induced contractility of stellate cells from normal and cirrhotic rat liver: implications for regulation of portal pressure and resistance. Hepatology 23, 1193–1201 (1996).
Gracia-Sancho, J. et al. Enhanced vasoconstrictor prostanoid production by sinusoidal endothelial cells increases portal perfusion pressure in cirrhotic rat livers. J. Hepatol. 47, 220–227 (2007).
Zhou, Q. et al. Intrahepatic upregulation of RhoA and Rho-kinase signalling contributes to increased hepatic vascular resistance in rats with secondary biliary cirrhosis. Gut 55, 1296–1305 (2006).
Julien, B. et al. Antifibrogenic role of the cannabinoid receptor CB2 in the liver. Gastroenterology 128, 742–755 (2005).
Abraldes, J. G. et al. Mild increases in portal pressure upregulate vascular endothelial growth factor and endothelial nitric oxide synthase in the intestinal microcirculatory bed, leading to a hyperdynamic state. Am. J. Physiol. Gastrointest. Liver Physiol. 290, G980–G987 (2006).
Goh, B. J. Nitric oxide synthase and heme oxygenase expressions in human liver cirrhosis. World J. Gastroenterol. 12, 588–593 (2006).
Ros, J. et al. Endogenous cannabinoids: a new system involved in the homeostasis of arterial pressure in experimental cirrhosis in the rat. Gastroenterology 122, 85–93 (2002).
Erario, M. et al. Role of heme oxygenase/carbon monoxide pathway on the vascular response to noradrenaline in portal hypertensive rats. Clin. Exp. Pharmacol. Physiol. 32, 196–201 (2005).
Thabut, D. et al. Cirrhotic patients with portal hypertension-related bleeding and an indication for early-TIPS: a large multicentre audit with real-life results. J. Hepatol. 68, 73–81 (2018).
Liu, B. et al. Innovative angiography: a new approach to discover more hepatic vein collaterals in patients with cirrhotic portal hypertension. BMC Gastroenterol. 23, 144 (2023).
Colle, I. O. et al. Vascular hyporesponsiveness in the mesenteric artery of anaesthetized rats with cirrhosis and portal hypertension: an in-vivo study. Eur. J. Gastroenterol. Hepatol. 16, 139–145 (2004).
Klein, S. et al. Janus-kinase-2 relates directly to portal hypertension and to complications in rodent and human cirrhosis. Gut 66, 145–155 (2015).
Casey, S. et al. Activation of the alternate renin-angiotensin system correlates with the clinical status in human cirrhosis and corrects post liver transplantation. J. Clin. Med. 8, 517 (2019).
Grace, J. A. et al. Activation of the MAS receptor by angiotensin-(1-7) in the renin-angiotensin system mediates mesenteric vasodilatation in cirrhosis. Gastroenterology 145, 874–884 (2013).
Salerno, F. et al. Vasopressin release and water metabolism in patients with cirrhosis. J. Hepatol. 21, 822–830 (1994).
Kumar, A. et al. Hemodynamic studies in acute-on-chronic liver failure. Dig. Dis. Sci. 54, 869–878 (2009).
Sánchez-Aldehuelo, R. et al. Progressive systemic inflammation precedes decompensation in compensated cirrhosis. JHEP Rep. 7, 101231 (2025).
Albillos, A. et al. Increased lipopolysaccharide binding protein in cirrhotic patients with marked immune and hemodynamic derangement. Hepatology 37, 208–217 (2003).
Weiss, E. et al. Characterization of blood immune cells in patients with decompensated cirrhosis including ACLF. Front. Immunol. 11, 619039 (2021).
Clària, J., Arroyo, V. & Moreau, R. Roles of systemic inflammatory and metabolic responses in the pathophysiology of acute-on-chronic liver failure. JHEP Rep. 5, 100807 (2023).
Fernández, J., Piano, S., Bartoletti, M. & Wey, E. Q. Management of bacterial and fungal infections in cirrhosis: the MDRO challenge. J. Hepatol. 75, S101–S117 (2021).
Moreau, R., Périanin, A. & Arroyo, V. Review of defective NADPH oxidase activity and myeloperoxidase release in neutrophils from patients with cirrhosis. Front. Immunol. 10, 1044 (2019).
Bernsmeier, C. et al. Patients with acute-on-chronic liver failure have increased numbers of regulatory immune cells expressing the receptor tyrosine kinase MERTK. Gastroenterology 148, 603–615.e14 (2015).
Bernsmeier, C. et al. CD14+ CD15+ HLA-DR− myeloid-derived suppressor cells impair antimicrobial responses in patients with acute-on-chronic liver failure. Gut 67, 1155–1167 (2018).
Geng, A. et al. Circulating monocytes upregulate CD52 and sustain innate immune function in cirrhosis unless acute decompensation emerges. J. Hepatol. 83, 146–160 (2025).
Lario, M. et al. Defective thymopoiesis and poor peripheral homeostatic replenishment of T-helper cells cause T-cell lymphopenia in cirrhosis. J. Hepatol. 59, 723–730 (2013).
Kwok, A. J. et al. Neutrophils and emergency granulopoiesis drive immune suppression and an extreme response endotype during sepsis. Nat. Immunol. 24, 767–779 (2023).
Medzhitov, R. Origin and physiological roles of inflammation. Nature 454, 428–435 (2008).
Bajaj, J. S., Kamath, P. S. & Reddy, K. R. The evolving challenge of infections in cirrhosis. N. Engl. J. Med. 384, 2317–2330 (2021).
Alvarez-Silva, C. et al. Compartmentalization of immune response and microbial translocation in decompensated cirrhosis. Front. Immunol. 10, 69 (2019).
Crispe, I. N. Immune tolerance in liver disease. Hepatology 60, 2109–2117 (2014).
Soffientini, U. et al. The lipopolysaccharide-sensing caspase(s)-4/11 are activated in cirrhosis and are causally associated with progression to multi-organ injury. Front. Cell Dev. Biol. 9, 668459 (2021).
Trawalé, J.-M. et al. The spectrum of renal lesions in patients with cirrhosis: a clinicopathological study. Liver Int. 30, 725–732 (2010).
Ventura-Cots, M. et al. Clinical, histological and molecular profiling of different stages of alcohol-related liver disease. Gut 71, 1856–1866 (2022).
Kondo, T. et al. The role of RIPK1 mediated cell death in acute on chronic liver failure. Cell Death Dis. 13, 5 (2022).
Macdonald, S. et al. Cell death markers in patients with cirrhosis and acute decompensation. Hepatology 67, 989–1002 (2018).
Moreau, R. et al. Blood metabolomics uncovers inflammation-associated mitochondrial dysfunction as a potential mechanism underlying ACLF. J. Hepatol. 72, 688–701 (2020).
Ganeshan, K. et al. Energetic trade-offs and hypometabolic states promote disease tolerance. Cell 177, 399–413.e12 (2019).
Bernardi, M. & Caraceni, P. Novel perspectives in the management of decompensated cirrhosis. Nat. Rev. Gastroenterol. Hepatol. 15, 753–764 (2018).
Gracia-Sancho, J. Sinusoidal Cells in Liver Diseases: Role in Their Pathophysiology, Diagnosis, and Treatment (Academic Press, 2024).
Albillos, A., de Gottardi, A. & Rescigno, M. The gut–liver axis in liver disease: pathophysiological basis for therapy. J. Hepatol. 72, 558–577 (2020).
Trebicka, J. et al. Expression of vasoactive proteins in gastric antral mucosa reflects vascular dysfunction in patients with cirrhosis and portal hypertension. Liver Int. 35, 1393–1402 (2015).
Hennenberg, M., Trebicka, J., Sauerbruch, T. & Heller, J. Mechanisms of extrahepatic vasodilation in portal hypertension. Gut 57, 1300–1314 (2008).
Schierwagen, R. et al. Circulating microbiome in blood of different circulatory compartments. Gut 68, 578–580 (2019).
Queck, A. et al. Role of portal venous platelet activation in patients with decompensated cirrhosis and TIPS. Gut 69, 1535–1536 (2020).
Boyer, T. The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension: update 2009. Hepatology 51, 808–815 (2010).
Simbrunner, B. et al. Bacterial translocation occurs early in cirrhosis and triggers a selective inflammatory response. Hepatol. Int. 17, 1045–1056 (2023).
Moreau, R., Gao, B., Papp, M., Bañares, R. & Kamath, P. S. Acute-on-chronic liver failure: a distinct clinical syndrome. J. Hepatol. 75, S27–S35 (2021).
Simonetto, D. A. et al. Chronic passive venous congestion drives hepatic fibrogenesis via sinusoidal thrombosis and mechanical forces. Hepatology 61, 648–659 (2015).
McDonald, B. et al. Intravascular danger signals guide neutrophils to sites of sterile inflammation. Science 330, 362–366 (2010).
Wree, A. et al. NLRP3 inflammasome activation results in hepatocyte pyroptosis, liver inflammation, and fibrosis in mice. Hepatology 59, 898–910 (2014).
Taru, V., Szabo, G., Mehal, W. & Reiberger, T. Inflammasomes in chronic liver disease: hepatic injury, fibrosis progression and systemic inflammation. J. Hepatol. 81, 895–910 (2024).
Jansen, C. et al. Increase in liver stiffness after transjugular intrahepatic portosystemic shunt is associated with inflammation and predicts mortality. Hepatology 67, 1472–1484 (2018).
Königshofer, P. et al. Distinct structural and dynamic components of portal hypertension in different animal models and human liver disease etiologies. Hepatology 75, 610–622 (2022).
Gracia-Sancho, J., Marrone, G. & Fernández-Iglesias, A. Hepatic microcirculation and mechanisms of portal hypertension. Nat. Rev. Gastroenterol. Hepatol. 16, 221–234 (2019).
Sandahl, T. D. et al. The macrophage activation marker sCD163 combined with markers of the enhanced liver fibrosis (ELF) score predicts clinically significant portal hypertension in patients with cirrhosis. Aliment. Pharmacol. Ther. 43, 1222–1231 (2016).
Bai, L. et al. M2-like macrophages exert hepatoprotection in acute-on-chronic liver failure through inhibiting necroptosis-S100A9-necroinflammation axis. Cell Death Dis. 12, 93 (2021).
Tritto, G. et al. Evidence of neutrophil functional defect despite inflammation in stable cirrhosis. J. Hepatol. 55, 574–581 (2011).
Trebicka, J., Macnaughtan, J., Schnabl, B., Shawcross, D. L. & Bajaj, J. S. The microbiota in cirrhosis and its role in hepatic decompensation. J. Hepatol. 75, S67–S81 (2021).
Lisman, T. et al. Elevated levels of von Willebrand factor in cirrhosis support platelet adhesion despite reduced functional capacity. Hepatology 44, 53–61 (2006).
Zenlander, R. et al. Neutrophil extracellular traps in patients with liver cirrhosis and hepatocellular carcinoma. Sci. Rep. 11, 18025 (2021).
Muñoz, L. et al. Intestinal immune dysregulation driven by dysbiosis promotes barrier disruption and bacterial translocation in rats with cirrhosis. Hepatology 70, 925–938 (2019).
du Plessis, J. & van der Merwe, S. W. Reply to: Uncovering the molecular events associated with increased intestinal permeability in liver cirrhosis: the pivotal role of enterocyte tight junctions and future perspectives. J. Hepatol. 59, 1146–1147 (2013).
du Plessis, J. et al. Activated intestinal macrophages in patients with cirrhosis release NO and IL-6 that may disrupt intestinal barrier function. J. Hepatol. 58, 1125–1132 (2013).
Trebicka, J. et al. Soluble TNF-α-receptors I are prognostic markers in TIPS-treated patients with cirrhosis and portal hypertension. PLoS One 8, e83341 (2013).
Bellot, P. et al. Bacterial DNA translocation is associated with systemic circulatory abnormalities and intrahepatic endothelial dysfunction in patients with cirrhosis. Hepatology 52, 2044–2052 (2010).
Garcia-Tsao, G., Albillos, A., Barden, G. E. & West, B. A. Bacterial translocation in acute and chronic portal hypertension. Hepatology 17, 1081–1085 (1993).
Verbeke, L., Nevens, F. & Laleman, W. Bench-to-beside review: acute-on-chronic liver failure — linking the gut, liver and systemic circulation. Crit. Care 15, 233 (2011).
Simbrunner, B. et al. FXR-FGF19 signaling in the gut–liver axis is dysregulated in patients with cirrhosis and correlates with impaired intestinal defence. Hepatol. Int. 18, 929–942 (2024).
Engelmann, C., Clària, J., Szabo, G., Bosch, J. & Bernardi, M. Pathophysiology of decompensated cirrhosis: portal hypertension, circulatory dysfunction, inflammation, metabolism and mitochondrial dysfunction. J. Hepatol. 75, S49–S66 (2021).
Trebicka, J. et al. Endotoxin and tumor necrosis factor-receptor levels in portal and hepatic vein of patients with alcoholic liver cirrhosis receiving elective transjugular intrahepatic portosystemic shunt. Eur. J. Gastroenterol. Hepatol. 23, 1218–1225 (2011).
Kajita, M. et al. iNOS expression in vascular resident macrophages contributes to circulatory dysfunction of splanchnic vascular smooth muscle contractions in portal hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 300, H1021–H1031 (2011).
Zapater, P. et al. Norfloxacin modulates the inflammatory response and directly affects neutrophils in patients with decompensated cirrhosis. Gastroenterology 137, 1669–1679.e1 (2009).
Liu, Y. et al. Associations between changes in the gut microbiota and liver cirrhosis: a systematic review and meta-analysis. BMC Gastroenterol. 25, 16 (2025).
Iwakiri, Y. & Trebicka, J. Portal hypertension in cirrhosis: pathophysiological mechanisms and therapy. JHEP Rep. 3, 100316 (2021).
Verbeke, L. et al. FXR agonist obeticholic acid reduces hepatic inflammation and fibrosis in a rat model of toxic cirrhosis. Sci. Rep. 6, 33453 (2016).
Lorenzo-Zúñiga, V. et al. Oral bile acids reduce bacterial overgrowth, bacterial translocation, and endotoxemia in cirrhotic rats. Hepatology 37, 551–557 (2003).
Pérez-Paramo, M. et al. Effect of propranolol on the factors promoting bacterial translocation in cirrhotic rats with ascites. Hepatology 31, 43–48 (2000).
Reiberger, T. et al. Non-selective betablocker therapy decreases intestinal permeability and serum levels of LBP and IL-6 in patients with cirrhosis. J. Hepatol. 58, 911–921 (2013).
Mookerjee, R. P. et al. Treatment with non-selective beta blockers is associated with reduced severity of systemic inflammation and improved survival of patients with acute-on-chronic liver failure. J. Hepatol. 64, 574–582 (2016).
Berres, M. L. et al. CXCL9 is a prognostic marker in patients with liver cirrhosis receiving transjugular intrahepatic portosystemic shunt. J. Hepatol. 62, 332–339 (2015).
Lehmann, J. M. et al. Circulating CXCL10 in cirrhotic portal hypertension might reflect systemic inflammation and predict ACLF and mortality. Liver Int. 38, 875–884 (2018).
Mehta, G., Mookerjee, R. P., Sharma, V. & Jalan, R. Systemic inflammation is associated with increased intrahepatic resistance and mortality in alcohol-related acute-on-chronic liver failure. Liver Int. 35, 724–734 (2015).
Trebicka, J. et al. Rebleeding and mortality risk are increased by ACLF but reduced by pre-emptive TIPS. J. Hepatol. 73, 1082–1091 (2020).
Piano, S. et al. Association between grade of acute on chronic liver failure and response to terlipressin and albumin in patients with hepatorenal syndrome. Clin. Gastroenterol. Hepatol. 16, 1792–1800.e3 (2018).
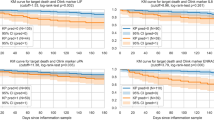
Semmler, G. et al. Non-invasive tests for clinically significant portal hypertension after HCV cure. J. Hepatol. 77, 1573–1585 (2022).
Shah, N. et al. Increased renal expression and urinary excretion of TLR4 in acute kidney injury associated with cirrhosis. Liver Int. 33, 398–409 (2013).
Nadim, M. K. et al. Acute kidney injury in patients with cirrhosis: Acute Disease Quality Initiative (ADQI) and International Club of Ascites (ICA) joint multidisciplinary consensus meeting. J. Hepatol. 81, 163–183 (2024).
Danielsen, K. V. et al. Cardiovascular mapping in cirrhosis from the compensated stage to hepatorenal syndrome: a magnetic resonance study. Am. J. Gastroenterol. 117, 1269–1278 (2022).
Izzy, M. et al. Redefining cirrhotic cardiomyopathy for the modern era. Hepatology 71, 334–345 (2020).
Liu, H., Nguyen, H. H., Yoon, K. T. & Lee, S. S. Pathogenic mechanisms underlying cirrhotic cardiomyopathy. Front. Netw. Physiol. 2, 849253 (2022).
Gaskari, S. A., Liu, H., D’mello, C., Kunos, G. & Lee, S. S. Blunted cardiac response to hemorrhage in cirrhotic rats is mediated by local macrophage-released endocannabinoids. J. Hepatol. 62, 1272–1277 (2015).
Gregolin, C. S. et al. Myocardial dysfunction in cirrhotic cardiomyopathy is associated with alterations of phospholamban phosphorylation and IL-6 levels. Arch. Med. Res. 52, 284–293 (2021).
Kao, Y. H. et al. Tumor necrosis factor-α decreases sarcoplasmic reticulum Ca2+-ATPase expressions via the promoter methylation in cardiomyocytes. Crit. Care Med. 38, 217–222 (2010).
Bortoluzzi, A. et al. Positive cardiac inotropic effect of albumin infusion in rodents with cirrhosis and ascites: molecular mechanisms. Hepatology 57, 266–276 (2013).
Praktiknjo, M. et al. Cardiodynamic state is associated with systemic inflammation and fatal acute-on-chronic liver failure. Liver Int. 40, 1457–1466 (2020).
Jansen, C. et al. Significant reduction in heart rate variability is a feature of acute decompensation of cirrhosis and predicts 90-day mortality. Aliment. Pharmacol. Ther. 50, 568–579 (2019).
Rose, C. F. et al. Hepatic encephalopathy: novel insights into classification, pathophysiology and therapy. J. Hepatol. 73, 1526–1547 (2020).
Córdoba, J. et al. Characteristics, risk factors and mortality of cirrhotic patients hospitalized for hepatic encephalopathy with and without acute-on-chronic liver failure. J. Hepatol. 73, 1256–1266 (2020).
Greinert, R. et al. Covert hepatic encephalopathy and spontaneous portosystemic shunts increase the risk of developing overt hepatic encephalopathy. Liver Int. 40, 3093–3102 (2020).
Ripoll, C. et al. Influence of NOD2 risk variants on hepatic encephalopathy and association with inflammation, bacterial translocation and immune activation. Liver Int. 43, 1793–1802 (2023).
Görg, B., Bidmon, H.-J. & Häussinger, D. Gene expression profiling in the cerebral cortex of patients with cirrhosis with and without hepatic encephalopathy. Hepatology 57, 2436–2447 (2013).
Wright, G. et al. Endotoxemia produces coma and brain swelling in bile duct ligated rats. Hepatology 45, 1517–1526 (2007).
Macías-Rodríguez, R. U. et al. Cerebral haemodynamics in cirrhotic patients with hepatic encephalopathy. Liver Int. 35, 344–352 (2015).
Jalan, R. & Rose, C. F. Heretical thoughts into hepatic encephalopathy. J. Hepatol. 77, 539–548 (2022).
Córdoba, J. et al. The development of low-grade cerebral edema in cirrhosis is supported by the evolution of 1H-magnetic resonance abnormalities after liver transplantation. J. Hepatol. 47, 219–227 (2007).
Weissenborn, K. et al. Liver transplantation improves hepatic myelopathy: evidence by three cases. Gastroenterology 124, 346–351 (2003).
Rose, C. & Jalan, R. Is minimal hepatic encephalopathy completely reversible following liver transplantation? Liver Transpl. 10, 84–87 (2004).
Rodríguez-Roisin, R. & Krowka, M. J. Hepatopulmonary syndrome — a liver-induced lung vascular disorder. N. Engl. J. Med. 358, 2378–2387 (2008).
Schenk, P. et al. Prognostic significance of the hepatopulmonary syndrome in patients with cirrhosis. Gastroenterology 125, 1042–1052 (2003).
Luo, B. et al. ET-1 and TNF-α in HPS: analysis in prehepatic portal hypertension and biliary and nonbiliary cirrhosis in rats. Am. J. Physiol. Gastrointest. Liver Physiol. 285, G131–G138 (2003).
Fallon, M. B. et al. The role of endothelial nitric oxide synthase in the pathogenesis of a rat model of hepatopulmonary syndrome. Gastroenterology 113, 606–612 (1997).
Zhang, J. et al. Pulmonary angiogenesis in a rat model of hepatopulmonary syndrome. Gastroenterology 136, 1070–1080 (2009).
Benz, F., Mohr, R., Tacke, F. & Roderburg, C. Pulmonary complications in patients with liver cirrhosis. J. Transl. Intern. Med. 8, 150–158 (2020).
Krowka, M. J. & Edwards, W. D. A spectrum of pulmonary vascular pathology in portopulmonary hypertension. Liver Transpl. 6, 373–382 (2000).
Nunes, H. et al. Role of nitric oxide in hepatopulmonary syndrome in cirrhotic rats. Am. J. Respir. Crit. Care Med. 164, 879–885 (2001).
Talwalkar, J. A., Swanson, K. L., Krowka, M. J., Andrews, J. C. & Kamath, P. S. Prevalence of spontaneous portosystemic shunts in patients with portopulmonary hypertension and effect on treatment. Gastroenterology 141, 1673–1679 (2011).
Groszmann, R. J. et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N. Engl. J. Med. 353, 2254–2261 (2005).
Villanueva, C. et al. Bacterial infections adversely influence the risk of decompensation and survival in compensated cirrhosis. J. Hepatol. 75, 589–599 (2021).
D’Amico, G. et al. Competing risks and prognostic stages of cirrhosis: a 25-year inception cohort study of 494 patients. Aliment. Pharmacol. Ther. 39, 1180–1193 (2014).
Bruno, S. et al. Mortality risk according to different clinical characteristics of first episode of liver decompensation in cirrhotic patients: a nationwide, prospective, 3-year follow-up study in Italy. Am. J. Gastroenterol. 108, 1112–1122 (2013).
Remmler, J. et al. Increased level of interleukin 6 associates with increased 90-day and 1-year mortality in patients with end-stage liver disease. Clin. Gastroenterol. Hepatol. 16, 730–737 (2018).
Cervoni, J. P. et al. Prognostic value of C-reactive protein in cirrhosis: external validation from the CANONIC cohort. Eur. J. Gastroenterol. Hepatol. 28, 1028–1034 (2016).
Huang, C. H. et al. Hepatic encephalopathy and spontaneous bacterial peritonitis improve cirrhosis outcome prediction: a modified seven-stage model as a clinical alternative to MELD. J. Pers. Med. 10, 1 (2020).
Fernández, J. et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology 157, 149–162 (2019).
Trebicka, J. et al. PREDICT identifies precipitating events associated with the clinical course of acutely decompensated cirrhosis. J. Hepatol. 74, 1097–1108 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT03056612 (2019).
Pompili, E. et al. Predictors of clinical trajectories of patients with acutely decompensated cirrhosis. An external validation of the PREDICT study. Liver Int. 44, 72–82 (2024).
Gu, W. et al. Trends and the course of liver cirrhosis and its complications in Germany: nationwide population-based study (2005 to 2018). Liver Int. 44, 1515–1526 (2024).
Tonon, M. et al. Outcomes and mortality of grade 1 ascites and recurrent ascites in patients with cirrhosis. Clin. Gastroenterol. Hepatol. 19, 358–366.e8 (2021).
Patidar, K. R. & Bajaj, J. S. Covert and overt hepatic encephalopathy: diagnosis and management. Clin. Gastroenterol. Hepatol. 13, 2048–2061 (2015).
Arroyo, V. et al. The systemic inflammation hypothesis: towards a new paradigm of acute decompensation and multiorgan failure in cirrhosis. J. Hepatol. 74, 670–685 (2021).
Verma, N. et al. Clinical and pathophysiological characteristics of non-acute decompensation of cirrhosis. J. Hepatol. 82, 1234–1244 (2025).
Bahceci, M. et al. The correlation between adiposity and adiponectin, tumor necrosis factor alpha, interleukin-6 and high sensitivity C-reactive protein levels. Is adipocyte size associated with inflammation in adults? J. Endocrinol. Invest. 30, 210–214 (2007).
Emerging Risk Factors Collaboration et al. C-reactive protein, fibrinogen, and cardiovascular disease prediction. N. Engl. J. Med. 367, 1310–1320 (2012).
Bertoni, A. G. et al. Inflammation and the incidence of type 2 diabetes: the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 33, 804–810 (2010).
Spranger, J. et al. Inflammatory cytokines and the risk to develop type 2 diabetes: results of the prospective population-based European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Diabetes 52, 812–817 (2003).
Wang, Q. et al. Validation of Baveno VII criteria for recompensation in entecavir-treated patients with hepatitis B-related decompensated cirrhosis. J. Hepatol. 77, 1564–1572 (2022).
Hui, V. W. K. et al. Baveno VII criteria for recompensation predict transplant-free survival in patients with hepatitis B-related decompensated cirrhosis. JHEP Rep. 5, 100–110 (2023).
Sánchez-Torrijos, Y. et al. Recompensation of decompensated cirrhosis in hepatitis C patients after SVR: prognostic implications. J. Hepatol. 82, 1250–1259 (2025).
Mandorfer, M. et al. Sustained virologic response to interferon-free therapies ameliorates HCV-induced portal hypertension. J. Hepatol. 65, 692–699 (2016).
Pose, E. et al. A notable proportion of liver transplant candidates with alcohol-related cirrhosis can be delisted because of clinical improvement. J. Hepatol. 75, 275–283 (2021).
Aravinthan, A. D. et al. Characteristics of liver transplant candidates delisted following recompensation and predictors of such delisting in alcohol-related liver disease: a case–control study. Transpl. Int. 30, 1140–1149 (2017).
Hofer, B. S. et al. Hepatic recompensation according to Baveno VII criteria is linked to a significant survival benefit in decompensated alcohol-related cirrhosis. Liver Int. 43, 2220–2231 (2023).
Fernandez, M. Molecular pathophysiology of portal hypertension. Hepatology 61, 1406–1415 (2015).
Villanueva, C. et al. Carvedilol reduces the risk of decompensation and mortality in patients with compensated cirrhosis in a competing-risk meta-analysis. J. Hepatol. 77, 1014–1025 (2022).
Abraldes, J. G. et al. Simvastatin lowers portal pressure in patients with cirrhosis and portal hypertension: a randomized controlled trial. Gastroenterology 136, 1651–1658 (2009).
Tandon, P., Abraldes, J. G., Berzigotti, A., Garcia-Pagan, J. C. & Bosch, J. Renin-angiotensin-aldosterone inhibitors in the reduction of portal pressure: a systematic review and meta-analysis. J. Hepatol. 53, 273–282 (2010).
Simon, T. G., Patorno, E. & Schneeweiss, S. Glucagon-like peptide-1 receptor agonists and hepatic decompensation events in patients with cirrhosis and diabetes. Clin. Gastroenterol. Hepatol. 20, 1382–1393.e19 (2022).
Kuchay, M. S. et al. Effect of empagliflozin on liver fat in patients with type 2 diabetes and nonalcoholic fatty liver disease: a randomized controlled trial (E-LIFT Trial). Diabetes Care 41, 1801–1808 (2018).
Harrison, S. A. et al. Design of the phase 3 MAESTRO clinical program to evaluate resmetirom for the treatment of nonalcoholic steatohepatitis. Aliment. Pharmacol. Ther. 59, 51–63 (2024).
Zipprich, A., Gittinger, F., Winkler, M., Dollinger, M. M. & Ripoll, C. Effect of ET-A blockade on portal pressure and hepatic arterial perfusion in patients with cirrhosis: a proof of concept study. Liver Int. 41, 554–561 (2021).
Lawitz, E. J. et al. Safety and pharmacokinetics of BI 685509, a soluble guanylyl cyclase activator, in patients with cirrhosis: a randomized phase Ib study. Hepatol. Commun. 7, e0276 (2023).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT03842761 (2021).
Villa, E. et al. Enoxaparin prevents portal vein thrombosis and liver decompensation in patients with advanced cirrhosis. Gastroenterology 143, 1253–1260 (2012).
Jachs, M. et al. Amelioration of systemic inflammation in advanced chronic liver disease upon beta-blocker therapy translates into improved clinical outcomes. Gut 70, 1758–1767 (2021).
Tergast, T. L. et al. Systemic arterial blood pressure determines the therapeutic window of non-selective beta blockers in decompensated cirrhosis. Aliment. Pharmacol. Ther. 50, 696–706 (2019).
Pose, E. et al. Simvastatin and rifaximin in decompensated cirrhosis: a randomized clinical trial. JAMA 333, 864–874 (2025).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT03780673 (2023).
Larrue, H. et al. TIPS prevents further decompensation and improves survival in patients with cirrhosis and portal hypertension in an individual patient data meta-analysis. J. Hepatol. 79, 692–703 (2023).
Stockhoff, L. et al. TIPS Insertion Leads to Partial Reversal of Systemic Inflammation in Patients with Decompensated Liver Cirrhosis https://www.postersessiononline.eu/173580348_eu/congresos/ILC2022/aula/-FRI_485_ILC2022.pdf (2022).
Van der Merwe, S., Chokshi, S., Bernsmeier, C. & Albillos, A. The multifactorial mechanisms of bacterial infection in decompensated cirrhosis. J. Hepatol. 75, S82–S100 (2021).
Zeng, X. et al. Low-dose rifaximin prevents complications and improves survival in patients with decompensated liver cirrhosis. Hepatol. Int. 15, 155–165 (2021).
Moreau, R. et al. Effects of long-term norfloxacin therapy in patients with advanced cirrhosis. Gastroenterology 155, 1816–1827.e9 (2018).
Macnaughtan, J. et al. A double blind, randomised, placebo-controlled study to assess safety and tolerability of oral enterosorbent Carbalive (Yaq-001) in cirrhotic patients. Gut 70, A5–A6 (2021).
Bajaj, J. S. et al. Fecal microbiota transplant from a rational stool donor improves hepatic encephalopathy: a randomized clinical trial. Hepatology 66, 1727–1738 (2017).
Bajaj, J. S. et al. Microbiota transplant for hepatic encephalopathy in cirrhosis: the THEMATIC trial. J. Hepatol. 83, 81–91 (2025).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT03796598 (2025).
Saeidinejad, M. M. et al. Novel therapeutic approaches in treatment of acute-on-chronic liver failure. Semin. Liver Dis. 43, 429–445 (2023).
Hu, J. J. et al. FDA-approved disulfiram inhibits pyroptosis by blocking gasdermin D pore formation. Nat. Immunol. 21, 736–745 (2020).
Engelmann, C. et al. Toll-like receptor 4 is a therapeutic target for prevention and treatment of liver failure. J. Hepatol. 73, 102–112 (2020).
Engelmann, C. et al. Combination of G-CSF and a TLR4 inhibitor reduce inflammation and promote regeneration in a mouse model of ACLF. J. Hepatol. 77, 1325–1338 (2022).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT04620148 (2021).
Trebicka, J. & Garcia-Tsao, G. Controversies regarding albumin therapy in cirrhosis. Hepatology 81, 288–303 (2025).
Bernardi, M. et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut 69, 1127–1138 (2020).
Caraceni, P. et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial. Lancet 391, 2417–2429 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT01288794 (2017).
Solà, E. et al. Midodrine and albumin for prevention of complications in patients with cirrhosis awaiting liver transplantation: a randomized placebo-controlled trial. J. Hepatol. 69, 1250–1259 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT00839358 (2016).
China, L. et al. A randomized trial of albumin infusions in hospitalized patients with cirrhosis. N. Engl. J. Med. 384, 808–817 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT03451292 (2025).
O’Leary, J. G. et al. Efficacy and safety of long-term human albumin therapy in cirrhotic patients with acute decompensation and ascites: topline results of the PRECIOSA trial. J. Hepatol. 82, S10 (2025).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03702920 (2019).
Torp, N. et al. Personalised human albumin in patients with cirrhosis and ascites: design and rationale for the ALB-TRIAL – a randomised clinical biomarker validation trial. BMJ Open 14, e079309 (2024).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT05056220 (2025).
Agarwal, B. et al. Randomized, controlled clinical trial of the DIALIVE liver dialysis device versus standard of care in patients with acute-on-chronic liver failure. J. Hepatol. 79, 79–92 (2023).
Bañares, R. et al. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: the RELIEF trial. Hepatology 57, 1153–1162 (2013).
Rifai, K. et al. Prometheus® — a new extracorporeal system for the treatment of liver failure. J. Hepatol. 39, 984–990 (2003).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT03065699 (2021).
Ballester, M. P. et al. Development and validation of the AMMON-OHE model to predict risk of overt hepatic encephalopathy occurrence in outpatients with cirrhosis. J. Hepatol. 79, 967–976 (2023).
Rahimi, R. S. et al. Efficacy and safety of ornithine phenylacetate for treating overt hepatic encephalopathy in a randomized trial. Clin. Gastroenterol. Hepatol. 19, 2626–2635.e7 (2021).
European Clinical Trials Register https://www.clinicaltrialsregister.eu/ctr-search/trial/2021-002617-33/DE (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT05900050 (2025).
D’Amico, G. et al. Further decompensation in cirrhosis: results of a large multicenter cohort study supporting Baveno VII statements. Hepatology 79, 869–881 (2024).
Hartl, L. et al. The systemic and hepatic alternative renin–angiotensin system is activated in liver cirrhosis, linked to endothelial dysfunction and inflammation. Sci. Rep. 13, 953 (2023).
Turco, L., Reiberger, T., Vitale, G. & La Mura, V. Carvedilol as the new non-selective beta-blocker of choice in patients with cirrhosis and portal hypertension. Liver Int. 43, 1183–1194 (2023).
Weiss, E. et al. Sympathetic nervous activation, mitochondrial dysfunction and outcome in acutely decompensated cirrhosis: the metabolomic prognostic models (CLIF-C MET). Gut 72, 1581–1591 (2023).
Mandorfer, M. et al. Von Willebrand factor indicates bacterial translocation, inflammation, and procoagulant imbalance and predicts complications independently of portal hypertension severity. Aliment. Pharmacol. Ther. 47, 980–988 (2018).
Lluch, P. et al. Plasma concentrations of nitric oxide and asymmetric dimethylarginine in human alcoholic cirrhosis. J. Hepatol. 41, 55–59 (2004).
Zhang, I. W. et al. Mitochondrial dysfunction governs immunometabolism in leukocytes of patients with acute-on-chronic liver failure. J. Hepatol. 76, 93–106 (2022).
Tazi, K. A. et al. In vivo altered unfolded protein response and apoptosis in livers from lipopolysaccharide-challenged cirrhotic rats. J. Hepatol. 46, 1075–1088 (2007).
Robic, M. A. et al. Liver stiffness accurately predicts portal hypertension related complications in patients with chronic liver disease: a prospective study. J. Hepatol. 55, 1017–1024 (2011).
Colecchia, A. et al. Spleen stiffness measurement can predict clinical complications in compensated HCV-related cirrhosis: a prospective study. J. Hepatol. 60, 1158–1164 (2014).
Jachs, M. et al. Decreasing von Willebrand factor levels upon nonselective beta blocker therapy indicate a decreased risk of further decompensation, acute-on-chronic liver failure, and death. Clin. Gastroenterol. Hepatol. 20, 1362–1373.e6 (2022).
Solé, C. et al. Characterization of inflammatory response in acute-on-chronic liver failure and relationship with prognosis. Sci. Rep. 6, 32341 (2016).
Paternostro, R. et al. Plasma renin concentration represents an independent risk factor for mortality and is associated with liver dysfunction in patients with cirrhosis. J. Gastroenterol. Hepatol. 32, 184–190 (2017).
Hartl, L. et al. The differential activation of cardiovascular hormones across distinct stages of portal hypertension predicts clinical outcomes. Hepatol. Int. 15, 1160–1173 (2021).
Kerbert, A. J. C. et al. Copeptin in acute decompensation of liver cirrhosis: relationship with acute-on-chronic liver failure and short-term survival. Crit. Care 21, 321 (2017).
Lisotti, A. et al. Indocyanine green retention test as a noninvasive marker of portal hypertension and esophageal varices in compensated liver cirrhosis. Hepatology 59, 643–650 (2014).
Tranah, T. H. et al. Plasma ammonia levels predict hospitalisation with liver-related complications and mortality in clinically stable outpatients with cirrhosis. J. Hepatol. 77, 1554–1563 (2022).
Shawcross, D. L. et al. Ammonia impairs neutrophil phagocytic function in liver disease. Hepatology 48, 1202–1212 (2008).
Faisal Sheikh, M., Mookerjee, R. P., Agarwal, B., Kumar Acharya, S. & Jalan, R. Prognostic role of ammonia in patients with cirrhosis. Hepatology 70, 982–994 (2019).
Jalan, R. et al. Ammonia produces pathological changes in human hepatic stellate cells and is a target for therapy of portal hypertension. J. Hepatol. 64, 823–833 (2016).
Jalan, R. et al. Alterations in the functional capacity of albumin in patients with decompensated cirrhosis is associated with increased mortality. Hepatology 50, 555–564 (2009).
Jalan, R. & Bernardi, M. Effective albumin concentration and cirrhosis mortality: from concept to reality. J. Hepatol. 59, 918–920 (2013).
Buck, M. et al. Novel inflammatory biomarkers of portal pressure in compensated cirrhosis patients. Hepatology 59, 1052–1059 (2014).
Navasa, M. et al. Tumor necrosis factor and interleukin-6 in spontaneous bacterial peritonitis in cirrhosis: relationship with the development of renal impairment and mortality. Hepatology 27, 1227–1232 (1998).
Cao, Z. et al. Blood markers for type-1,-2, and -3 inflammation are associated with severity of acutely decompensated cirrhosis. J. Hepatol. 82, 836–850 (2025).
Rainer, F. et al. Soluble CD163 and soluble mannose receptor predict survival and decompensation in patients with liver cirrhosis, and correlate with gut permeability and bacterial translocation. Aliment. Pharmacol. Ther. 47, 657–664 (2018).
Ariza, X. et al. Neutrophil gelatinase-associated lipocalin is a biomarker of acute-on-chronic liver failure and prognosis in cirrhosis. J. Hepatol. 65, 57–65 (2016).
Gambino, C. et al. Diagnostic and prognostic performance of urinary neutrophil gelatinase-associated lipocalin in patients with cirrhosis and acute kidney injury. Hepatology 77, 1630–1638 (2023).
Woolbright, B. L. et al. Cell death and prognosis of mortality in alcoholic hepatitis patients using plasma keratin-18. Gene Expr. 17, 301–312 (2017).
Acknowledgements
The authors acknowledge Lidia Garcia-Campmany for her valuable contribution in designing Fig. 3 of the manuscript.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
J.T. has received speaking and/or consulting fees from Versantis, Gore, Boehringer-Ingelheim, Falk, Grifols, Genfit and CSL Behring. C.R. has received speaker fees from GORE, Falk Foundation and Bristol-Myers Squibb, and has acted as a consultant for Boerhinger-Ingelheim. C.R. receives funding from the DFG (Deutsche Forschung Gemeinschaft) project number 431667134 and the European Union Horizon 2020 research and innovation programme under grant agreement 101136299 ARTEMIS. R.J. is the founder of Yaqrit Discovery Limited, which owns Amalive Limited and Enterosorb Limited; is a co-founder of Cyberliver Limited and Hepyx Limited; has received payment for sponsored talks and grant reviews from Grifols; and has received consulting fees from Boehringer Ingelheim. T.R. has received grant support from Abbvie, Boehringer Ingelheim, Gilead, Intercept/Advanz Pharma, MSD, Myr Pharmaceuticals, Philips Healthcare, Pliant, Siemens and W. L. Gore & Associates; speaking/writing honoraria from Abbvie, Echosens, Gilead, GSK, Intercept/Advanz Pharma, Pfizer, Roche, MSD, Siemens and W. L. Gore & Associates; consulting/advisory board fees from Abbvie, Astra Zeneca, Bayer, Boehringer Ingelheim, Gilead, Intercept/Advanz Pharma, MSD, Resolution Therapeutics and Siemens; and travel support from Abbvie, Boehringer Ingelheim, Dr. Falk Pharma, Gilead and Roche. D.C. and R.M. declare no competing interests.
Peer review
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks Chien-Hao Huang and the other, anonymous, reviewers for their contribution to the peer review of this work.
Additional information
We dedicate this article, which provides an integrated view on the pathogenesis of cirrhosis complications, to the memory of Professor Jaume Bosch — a great teacher, mentor, colleague and dear friend to all of us, whose pioneering efforts in developing new concepts and therapies in the field of portal hypertension are immeasurable. Jaume was more than a brilliant clinician–scientist; he was a source of inspiration, wisdom, generosity and warmth for everyone privileged to work with him. His passion for advancing knowledge in the field of cirrhosis was matched only by his zest for life and love for his friends and family. Many of us owe our careers — and our love for hepatology — to his guidance and example. This article stands as a small tribute to a remarkable man whose legacy will continue to shape and inspire us.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
CANONIC: https://efclif.com/projects/canonic-chronic-liver-failure-acute-on-chronic-liver-failure/
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Costa, D., Trebicka, J., Ripoll, C. et al. Interaction of inflammation and portal hypertension in cirrhosis progression. Nat Rev Gastroenterol Hepatol (2025). https://doi.org/10.1038/s41575-025-01107-2
Accepted:
Published:
DOI: https://doi.org/10.1038/s41575-025-01107-2