Abstract
Immune checkpoint blockade (ICB) is standard of care in advanced diffuse pleural mesothelioma (DPM), but its role in the perioperative management of DPM is unclear. In tandem, circulating tumor DNA (ctDNA) ultra-sensitive residual disease detection has shown promise in providing a molecular readout of ICB efficacy across resectable cancers. This phase 2 trial investigated neoadjuvant nivolumab and nivolumab/ipilimumab in resectable DPM along with tumor-informed liquid biopsy residual disease assessments. Patients with resectable epithelioid/biphasic DPM enrolled sequentially to nivolumab 240 mg every 2 weeks (q2w) for three cycles (Arm A, n = 16) or nivolumab 3 mg kg−1 q2w for three cycles plus ipilimumab 1 mg kg−1 on cycle 1 (Arm B, n = 14), followed by surgery, optional chemotherapy and/or radiotherapy, and nivolumab 480 mg q4w for 1 year. Co-primary endpoints included safety and feasibility; key exploratory endpoints included progression-free survival (PFS), overall survival (OS) and ctDNA analyses. The trial met its primary endpoints, and, in Arms A and B, 81.3% and 85.7% of patients proceeded to surgery, respectively. Treatment was safe, with a single dose-limiting toxicity in each arm. In Arm A, median PFS and OS were 9.6 months (95% confidence interval (CI): 2.5–27.7) and 19.3 months (95% CI: 14.9–34.7), respectively. In Arm B, median PFS and OS were 19.8 months (7.1–not reached) and 28.6 months (20.4–not reached), respectively. Persistent ctDNA was detected during neoadjuvant therapy in patients who did not undergo complete surgical resection due to disease progression (Fisher’s exact test, P = 0.00013). Patients with detectable ctDNA on cycle 3 and pre-surgery had shorter PFS (log-rank test, P = 0.027 and P = 0.0059, respectively); this association was more pronounced when quantitative ctDNA changes were considered (log-rank test, P = 1.8 × 10−6). Our findings support the feasibility of neoadjuvant ICB and the clinical utility of ctDNA analyses to capture residual disease in resectable DPM. ClinicalTrials.gov identifier: NCT03918252.
Similar content being viewed by others
Main
DPM is a rare malignancy of the pleural lining that is diagnosed in approximately 30,000 individuals worldwide annually, with increased incidence in regions with high asbestos exposure1. DPM is incurable in most cases and for decades encountered little innovation in systemic therapy. However, this changed with the emergence of ICB, and in the phase 3 CheckMate 743 trial, the combination of the anti-PD-1 antibody nivolumab (nivo) plus anti-CTLA-4 antibody ipilimumab (ipi) demonstrated a significant OS benefit over platinum doublet chemotherapy in treatment-naive unresectable DPM2,3. Similarly, the phase 3 IND227 trial showed a significant OS advantage with the combination of the anti-PD-1 agent pembrolizumab and platinum doublet chemotherapy compared to chemotherapy alone in advanced, treatment-naive, unresectable DPM4. Both combinatorial strategies are now approved by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) as frontline therapies for DPM, with pembrolizumab plus chemotherapy approved by the EMA only for non-epithelioid DPM.
The management of potentially resectable DPM is complex and controversial. Several retrospective and small single-arm studies using an aggressive tri-modality approach, including perioperative chemotherapy, surgery and radiotherapy, have shown clinical benefit compared to historical data for systemic therapy alone5,6. However, this efficacy signal has yet to be replicated in prospective randomized trials. The MARS trial, which randomized patients with resectable DPM to systemic therapy plus extrapleural pneumonectomy (EPP) versus systemic therapy alone, was terminated early due to high morbidity associated with EPP7. More recently, the prospective, randomized phase 3 MARS2 trial failed to show an OS benefit with the addition of extended pleurectomy decortication (P/D) to systemic chemotherapy compared to chemotherapy alone for resectable DPM8. That said, these studies completed accrual before the advent of ICB, which has transformed the treatment paradigm of other resectable malignancies, notably non-small cell lung cancer, in which neoadjuvant, perioperative and adjuvant ICB-containing strategies are now standard of care9,10,11,12. Whether perioperative ICB can be safely and feasibly incorporated into the perioperative treatment of resectable DPM remains unknown.
Additional challenges in the management of resectable DPM stem from the inconsistency of conventional imaging-based treatment response assessments. DPM displays a unique pattern of growth around the pleural surface, either as focal pleural thickening or a circumferential sheet around the lung, and often does not produce discrete measurable lesions13. The widely adopted Response Evaluation Criteria in Solid Tumors (RECIST) guidelines14 assume spherical tumor models and are reliant on unidimensional measurements of longest diameter, which can be ill defined in DPM15. Modified RECIST (mRECIST)16,17, which specifically measure tumor thickness perpendicular to the chest wall, were developed to address these challenges and have since become a standard assessment of DPM tumor response17. Nevertheless, accurate and reproducible response identification in DPM remains elusive, necessitating new approaches for reliable and timely disease evaluation during treatment. To this end, liquid biopsies offer a compelling alternative for monitoring treatment response in DPM. Assessment of systemic tumor burden through ctDNA analysis allows for interpretation of therapy efficacy at a molecular level and has been shown to reflect pathological tumor regression and clinical outcomes in several cancer types18,19, including in neoadjuvant immunotherapy settings19,20,21,22,23.
However, ctDNA has yet to be meaningfully studied as a biomarker for mesotheliomas, in large part due to these tumors’ low non-synonymous somatic mutation burden24, which limits the sensitivity of oligo mutation-based ctDNA assays. Recent developments in ctDNA minimal residual disease (MRD) detection assays that are informed by the tumor mutational profile and augmented by interrogation of mutant loci across the genome, coupled with high sequencing depth, have allowed for ultra-sensitive clinically informative ctDNA detection23,25. Although personalized ctDNA detection platforms, where individualized liquid biopsy assays are generated per patient based on the genetic profile of the tumor, may unlock ctDNA as a clinically informative biomarker for resectable cancers, bespoke approaches have limited feasibility due to technical and operational complexities. To this end, approaches that rely on concurrent tumor and cell-free DNA (cfDNA) whole-genome sequencing (WGS), coupled with background noise suppression via machine learning, result in ultra-sensitive ctDNA detection and can alleviate logistical challenges associated with personalized assay development and turnaround time.
In this prospective, multicenter, multiarm phase 2 clinical trial, we investigated neoadjuvant nivo and nivo plus ipi (nivo/ipi) in patients with resectable DPM (NCT03918252) in order to determine the feasibility and safety of this approach as well as to explore the clinical utility of tumor-informed WGS-based cfDNA molecular residual disease assessments.
Results
Study design and endpoints
This multicenter, multiarm, non-comparative phase 2 study enrolled patients with previously untreated DPM adjudicated as resectable by a multidisciplinary team assessment (Fig. 1a and Extended Data Fig. 1). Patients were enrolled sequentially to receive neoadjuvant intravenous nivo 240 mg q2w for three cycles (2 weeks = one cycle in neoadjuvant phase, Arm A) or neoadjuvant intravenous nivo 3 mg kg−1 q2w for three cycles together with ipi 1 mg kg−1 administered on cycle 1 only (Arm B) (Methods). After neoadjuvant therapy, patients in both arms proceeded to planned surgery. After resection, patients could receive up to four cycles of adjuvant platinum/pemetrexed chemotherapy and optional adjuvant radiotherapy. Patients then received adjuvant intravenous nivo 480 mg every 4 weeks for up to 1 year.
a, CONSORT flow diagram depicting patient disposition as follows: 30 patients were screened and sequentially enrolled in the study; 16 patients were enrolled in Arm A and received neoadjuvant nivo; and 14 patients were enrolled in Arm B and received neoadjuvant nivo/ipi ×1 followed by neoadjuvant nivo. Disease progression precluded surgery for three patients in Arm A and two patients in Arm B; of the patients who proceeded to surgery, one patient in each arm was deemed to have unresectable disease intraoperatively. Twelve patients in Arm A and 11 patients in Arm B underwent complete macroscopic resection. In Arm A, nine patients received adjuvant chemotherapy, seven received adjuvant radiotherapy and eight received adjuvant immunotherapy. In Arm B, five patients received adjuvant chemotherapy, five patients received adjuvant radiotherapy and six patients received adjuvant immunotherapy. At the data cutoff date, one patient in Arm A was alive but experienced progression (14 deceased, one lost to follow-up), and eight patients in Arm B were alive, with five determined to be disease free (six deceased). PFS and OS analyses were conducted for all 30 patients in the study cohort. Post-surgery landmark analyses were conducted for 12 patients in Arm A and for 11 patients in Arm B. ORR analyses were conducted for 15 patients in Arm A and for 11 patients in Arm B; RECIST was not performed for one patient in each arm, and two patients in Arm B were not evaluable by RECIST. b, Biospecimen collection schema, depicting the sample collection schedule for the trial. Tumor tissue was collected at pretreatment biopsy and at resection. Serial plasma samples were collected at C1D1 (D–42), C2D1 (D–28), C3D1 (D–14), pre-surgery (D–3), post-surgery before adjuvant therapy initiation and longitudinally during and after adjuvant therapy until the time of recurrence. Created with BioRender.com. Adj., adjuvant; D, day.
The dual co-primary endpoints of the study were feasibility and safety. Feasibility was defined by the proportion of patients who proceeded to surgery without a treatment-related delay exceeding 24 days from the preplanned date, with the hypothesis that 80% or more would proceed to surgery (Methods). Safety was defined by the frequency of dose-limiting toxicities (DLTs) related to nivo or nivo/ipi administered in the neoadjuvant period (Methods). Secondary endpoints included investigator-assessed objective response rate (ORR) after neoadjuvant therapy (pre-surgery), determined using mRECIST version 1.1 (ref. 17) for DPM, and the toxicity profile of adjuvant nivo. Although assessment of pathologic response was an initial secondary objective of the study, due to the complexities of performing and standardizing these assessments for DPM, pathologic response was not evaluated. Clinically relevant exploratory endpoints included PFS, defined as the time from initiation of neoadjuvant therapy to progression precluding surgery, recurrence post-surgery or death, and OS, defined as the time from neoadjuvant therapy initiation to death. Exploratory analyses also included longitudinal assessment of cfDNA tumor fraction (TF) through tumor-informed WGS-based analyses to capture residual disease during the neoadjuvant period and postoperatively (Fig. 1b, Extended Data Fig. 2 and Methods).
Patient characteristics and treatment
Between 29 October 2019 and 22 January 2024, 30 patients were enrolled sequentially to Arms A and B (16: Arm A, 14: Arm B). Eligible patients were 18 years of age or older with epithelioid or biphasic DPM histology and primary tumor amenable to surgical resection, as determined by the multidisciplinary treatment team (Table 1, Fig. 1a and Methods). Other key inclusion criteria included Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 and adequate organ function including glomerular filtration rate ≥45 ml min−1. Key exclusion criteria included patients who were not surgical candidates, had unresectable DPM or had pure sarcomatoid histology (Methods). In Arm A, median age was 63.7 years (range, 33.6–78.0); 81.3% (13/16) of patients were male; and 87.5% (14/16) of patients had epithelioid histology. In Arm B, median age was 67.9 years (range, 57.0–77.6); 57.1% (8/14) of patients were male; and 78.6% (11/14) of patients had epithelioid histology (Table 1).
Primary endpoints: feasibility and safety
All patients received all planned doses of neoadjuvant ICB in both arms (Fig. 1a). In Arm A, 13 of 16 patients proceeded to surgical resection within the protocol-defined feasibility window (three patients had imaging-assessed disease progression precluding surgery), and 12 patients underwent complete macroscopic resection (one patient was deemed unresectable in the operating room). Extended P/D was performed for most patients (83.3%, 10/12), and EPP was performed in 16.7% of patients (2/12). In Arm B, 12 of 14 patients proceeded with surgery within the feasibility window (two patients had imaging-assessed disease progression precluding surgery), and 11 patients underwent complete macroscopic resection (one patient was deemed unresectable intraoperatively). Extended P/D was performed for 81.8% of patients (9/11), and EPP was completed in 18.2% of patients (2/11). In both arms, the feasibility threshold was achieved; the posterior means for feasibility were 78.0% (posterior 90% credible interval (pCI): 60.4–91.5) and 81.0% (90% pCI: 63.7–94.3) for Arms A and B, respectively.
Delivery of neoadjuvant nivo and neoadjuvant nivo/ipi was safe, with an adverse event (AE) profile consistent with the known safety profile of ICB (Fig. 2 and Supplementary Table 2). One DLT related to ICB was observed in each arm (pneumonitis, Arm A; elevated alanine aminotransferase, Arm B), neither of which precluded surgical resection. The DLT rate was 6.3% (95% CI: 0.2–30.2) in Arm A and 7.1% (95% CI: 0.2–33.9) in Arm B. Any-grade AEs related to ICB occurred in 62.5% of patients in Arm A and in 57.1% of patients in Arm B. Grade 3 or higher ICB-related AEs occurred in 18.8% of patients in Arm A and in 7.1% of patients in Arm B (Fig. 2 and Supplementary Table 2). Any-grade treatment-emergent adverse events (TEAEs) occurred in 87.5% and 78.6% of patients in Arms A and B, respectively, among which 37.5% and 28.6% were grade 3 or higher, respectively (Supplementary Table 3).
Any-grade AEs related to nivo or ipi occurring within 100 days of study drug administration or 30 days post-surgery (whichever was longer) were recorded. Any-grade AEs related to ICB occurred in 62.5% of patients in Arm A, of which 18.8% were grade 3 or higher. Grade 3 or higher ICB-related AEs in Arm A included one event each of hypokalemia, pneumonitis and upper respiratory infection. In Arm B, any-grade AEs related to ICB occurred in 57.1% of patients, of which 7.1% were grade 3 or higher. Grade 3 or higher ICB-related AEs in Arm B included one event each of alkaline phosphatase elevation and aspartate aminotransferase elevation. The breakdown of these AEs by arm is shown in light shading (any-grade AEs), whereas grade 3 or higher AEs are shown in dark shading.
Secondary endpoints: radiographic response assessment and safety of adjuvant nivo
In Arm A, 15 patients were evaluable for radiographic response assessment by mRECIST version 1.1 (RECIST assessment not performed in one patient; Fig. 1a). Two patients attained a partial response (ORR: 13.3%; 95% CI: 1.7–40.5), and eight patients (53.3%; 95% CI: 26.6–78.7) had stable disease (Fig. 3a). In Arm B, 11 patients were evaluable (RECIST not performed in one patient and not evaluable in two patients). There were no partial responses (ORR: 0.0%; 95% CI: 0–28.5), and five patients (45.5%; 95% CI: 16.8–76.6) had stable disease (Fig. 3a).
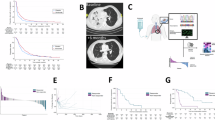
a, Swimmer’s plot of the study cohort stratified by treatment arm. PFS is presented alongside histology, surgery completion status, RECIST response and ctDNA status at C3D1 and pre-surgery for the 30 enrolled patients. Liquid biopsies during neoadjuvant treatment are indicated for relevant timepoints (C1D1 (D−42), C2D1 (D−28), C3D1 (D−14) and pre-surgery (D−3)), as are surgery, progression or recurrence and death. A total of seven patients did not undergo complete surgical resection. Of 28 patients evaluated for RECIST at baseline and pre-surgery, two had non-evaluable disease, 13 had SD, two had PR and 11 experienced PD. Patients in Arm A (n = 16) had a median PFS of 9.6 months (95% CI: 2.5–27.7) (b) and a median OS of 19.3 months (95% CI: 14.9–34.7) (c). Patients in Arm B (n = 14) had a median PFS of 19.8 months (95% CI: 7.1–NR) (d) and a median OS of 28.6 months (95% CI: 20.4–NR) (e). The median follow-up times for Arms A and B were 43.2 months and 24.1 months, respectively. D, day; NR, not reached; PD, progressive disease; PR, partial response; SD, stable disease; UD, undetectable.
Among the 12 patients who underwent surgery in Arm A, nine (75%) received adjuvant chemotherapy, seven (58.3%) received adjuvant radiotherapy and eight (66.7%) received adjuvant nivo (Supplementary Table 1). Of the four patients who did not receive adjuvant nivo, one was lost to follow-up, one died post-surgery, one experienced disease progression and one experienced drug-related pneumonitis with neoadjuvant nivo (precluding additional adjuvant nivo). Among the 11 patients who underwent surgery in Arm B, five (45.5%) received adjuvant chemotherapy, five (45.5%) received adjuvant radiotherapy and six (54.5%) received adjuvant nivo. Of the five patients who did not receive adjuvant nivo in Arm B, two experienced disease progression prior to receipt of nivo, one experienced an extended postoperative recovery precluding additional systemic therapy, one declined nivo after experiencing pain-related complications from radiotherapy and one declined nivo after completing chemotherapy. Adjuvant nivo was safe, with two patients (25%) experiencing an ICB-related AE in Arm A, none of which was high grade. In Arm B, three patients (50%) experienced an ICB-related AE, including one event of grade 3 maculo-papular rash (Supplementary Table 4).
Exploratory endpoints: PFS and OS
At a median follow-up of 43.2 months in the intention-to-treat (ITT) population in Arm A, the median PFS was 9.6 months (95% CI: 2.5–27.7; Fig. 3b), and the median OS was 19.3 months (95% CI: 14.9–34.7; Fig. 3c). At data lock, one patient was alive and none were recurrence free. At a median follow-up of 24.1 months in the ITT population in Arm B, the median PFS was 19.8 months (95% CI: 7.1– not reached; Fig. 3d), and the median OS was 28.6 months (95% CI: 20.4– not reached; Fig. 3e). At data lock, eight of 14 patients were alive, of whom five were recurrence free. In the subset of patients who underwent surgery in Arm A, receipt of adjuvant chemotherapy was associated with a trend in benefit in PFS (log-rank test, P = 0.027; hazard ratio (HR) = 0.14, 95% CI: 0.02–1.04) and OS (log-rank test, P = 0.027; HR = 0.14, 95% CI: 0.02–1.04). Receipt of adjuvant radiotherapy was associated with a PFS trend (log-rank test, P = 0.024; HR = 0.17, 95% CI: 0.03–0.96), although this was not observed for OS (log-rank test, P = 0.071; HR = 0.27, 95% CI: 0.06–1.23). Receipt of adjuvant nivo was also associated with a trend toward longer PFS in Arm A (log-rank test, P = 0.029; HR = 0.20, 95% CI: 0.04–0.99), which was not observed for OS (log-rank test, P = 0.1; HR = 0.31, 95% CI: 0.07–1.39; Extended Data Fig. 3). Among patients who underwent successful resection in Arm B, neither adjuvant chemotherapy nor radiotherapy was associated with a PFS or OS benefit. Adjuvant nivo was associated with a trend toward longer PFS (log-rank test, P = 0.01) and OS (log-rank test, P = 0.01) (Extended Data Fig. 3). HRs were not estimable and, thus, not reported for comparisons by adjuvant immunotherapy status (Methods).
Tumor-informed ctDNA residual disease assessment captures clinical endpoints
As an exploratory objective, we evaluated tumor kinetics and regression during neoadjuvant ICB at a molecular level using an ultra-sensitive tumor-informed WGS-based ctDNA residual disease detection approach (Methods). Serial plasma samples were procured at cycle 1, day 1 (C1D1; n = 28 samples), at cycle 2, day 1 (C2D1) (n = 27 samples), at cycle 3, day 1 (C3D1) (n = 23 samples), preoperatively (n = 27 samples) and postoperatively (n = 18 samples) (Fig. 1b and Extended Data Fig. 1). We performed matched WGS of tumor (n = 30), white blood cell (WBC) DNA (n = 30) and serial cfDNA samples (n = 123) at a target of 80×, 40× and 30× coverage, respectively (Methods and Supplementary Tables 5 and 6). For each case, a high-confidence single-nucleotide variant (SNV) set was generated by intersecting tumor, WBC and cfDNA sequence data and used to determine the presence of cancer in each plasma sample through a random forest machine learning model, followed by comparison to the background signal determined from a reference set of non-cancerous plasma samples (Extended Data Fig. 2). ctDNA status was assessed at C1D1 (n = 26), at C2D1 (n = 25), at C3D1 (n = 21), preoperatively (n = 25) and postoperatively (n = 16). We identified 12 (46%) patients with detectable ctDNA at C1D1, 11 (44%) with detectable ctDNA at C2D1, seven (33%) with detectable ctDNA at C3D1, 13 (52%) with detectable ctDNA preoperatively and two (18%) with detectable ctDNA postoperatively prior to initiation of adjuvant therapy (Fig. 4a and Extended Data Figs. 4 and 5). At C1D1, patients with detectable ctDNA (n = 12) had a median cfDNA TF of 0.11% (interquartile range (IQR), 0.06–0.17; Supplementary Table 6). Between arms, we observed numerically higher ctDNA detection rates across timepoints in Arm A (Extended Data Fig. 5).
a, ctDNA detection at perioperative timepoints, overlaid with PFS outcomes, arm and surgery feasibility/completion status for individual patients. Perioperative ctDNA dynamics for six selected patients are presented alongside treatment arm, histology, surgery completion, mRECIST response label and PFS. b, Sustained cfDNA TF across neoadjuvant timepoints was indicative of surgery-precluding progression for CBUAD_0980, who had a short PFS of 1.58 months. c, Persistent detection of ctDNA postoperatively and after the completion of adjuvant chemotherapy and radiotherapy captured early recurrence for CBUAD_0977; ctDNA status was in line with a short PFS of 8.94 months. d, For CBUAD_1264, a substantial decrease in cfDNA TF from C1D1 to C2D1, followed ultimately by ctDNA clearance at C3D1, was indicative of longer PFS (24.08 months), despite a radiographic assessment of SD. e, For CBUAD_0705, sustained ctDNA clearance from C2D1 onwards accurately captured a longer PFS of 27.73 months, despite a radiographic assessment of SD. f, Detection of ctDNA during postoperative follow-up was indicative of recurrence for CBUAD_0008, who had RECIST-based PR at surgery and, accordingly, had undetectable ctDNA throughout the neoadjuvant period. g, For CBUAD_1045, undetectable ctDNA during neoadjuvant treatment aligned with their longer PFS of 23.26 months; longitudinal monitoring of ctDNA was indicative of recurrence after completion of adjuvant chemotherapy, radiotherapy and nivo. mo, months; on adj nivo, on adjuvant nivolumab; post-adj chemo/RT, post-adjuvant chemotherapy/radiotherapy; post-adj tx, post-adjuvant therapy; PR, partial response; SD, stable disease.
Patients for whom surgery was not feasible or aborted intraoperatively showed persistent ctDNA levels throughout neoadjuvant ICB (Fig. 4a). As a representative example, patient CBUAD_0980 experienced a steady increase in ctDNA levels across all timepoints during neoadjuvant ICB, which was consistent with disease progression precluding surgery and reflected in a short PFS of 1.58 months (Fig. 4b). Longitudinal ctDNA assessment provided additional insights into predicting recurrence for patients who underwent surgery. Patient CBUAD_0977 had persistent detectable ctDNA during neoadjuvant ICB and postoperatively, which accurately captured early disease progression and a PFS of 8.94 months (Fig. 4c). By contrast, patients who showed early ctDNA clearance attained long PFS in both Arm A and Arm B. As examples, patients CBUAD_1264 (Fig. 4d) and CBUAD_0705 (Fig. 4e) showed ctDNA clearance during neoadjuvant ICB at C3D1 and C2D1, respectively, which was consistent with successful completion of surgery and long PFS of 24.08 months and 27.73 months. Interestingly, all four patients described above had stable disease by mRECIST, highlighting the inherent challenges with radiographic response assessment in DPM. In longitudinal monitoring of ctDNA levels from neoadjuvant ICB through the postoperative period, we noted that ctDNA MRD detection was informative with regard to disease recurrence. Patients CBUAD_0008 (Fig. 4f) and CBUAD_1045 (Fig. 4g) had undetectable ctDNA levels during neoadjuvant ICB, but both had postoperative ctDNA detected before imaging-assessed recurrence. Taken together, assessment of ctDNA status per timepoint and ctDNA kinetics across timepoints can capture residual disease and clinical outcomes.
Aligning with the trial’s primary feasibility endpoint, we next evaluated the association between ctDNA detection by timepoint and completion of surgery. Compared to patients who did not complete surgery (n = 7), patients who successfully underwent complete macroscopic resection (n = 23) had lower ctDNA detection rates at C1D1 (32% versus 86%, Fisher’s exact test, P = 0.026), at C2D1 (32% versus 83%, Fisher’s exact test, P = 0.056), at C3D1 (7% versus 100%, Fisher’s exact test, P = 0.00013) and pre-surgery (37% versus 100%, Fisher’s exact test, P = 0.015) (Fig. 5a–e). Similarly, compared to patients for whom resection was not feasible (n = 5), patients who proceeded to surgical resection within the protocol-defined feasibility window (n = 25) had lower ctDNA detection rates at C1D1 (33% versus 100%, Fisher’s exact test, P = 0.012), at C2D1 (33% versus 100%, Fisher’s exact test, P = 0.026) and at C3D1 (12% versus 100%, Fisher’s exact test, P = 0.001), with a similar trend at the pre-surgery timepoint (43% versus 100%, Fisher’s exact test, P = 0.096) (Extended Data Fig. 6). In quantitative assessment of cfDNA TF across timepoints by surgery completion, we found consistently higher TFs at C1D1, C2D1, C3D1 and pre-surgery for patients who did not complete surgery (Mann–Whitney test, P = 0.011, P = 0.036, P = 0.0002 and P = 0.003, respectively). These findings suggest that ctDNA residual disease tracking can identify early disease progression during the neoadjuvant period, including in patients who were radiographically and clinically eligible for definitive surgery but ultimately experienced disease progression intraoperatively.
a, ctDNA status per timepoint is indicated by circles colored according to ctDNA detection (yellow for detectable ctDNA, blue for undetectable ctDNA) and connected by a line ending at surgical resection. The line color represents the degree of ctDNA reduction: blue depicts ≥95% cfDNA TF reduction at pre-surgery or undetectable ctDNA across the neoadjuvant window; orange indicates <95% reduction; and gray denotes unevaluable timepoints. b, Patients who did not complete surgery (n = 7) had a significantly higher ctDNA detectable rate at C1D1 compared to patients who completed surgery (n = 19; 86% versus 32%, respectively; Fisher’s exact test, P = 0.026). c, Similarly, patients who did not complete surgery (n = 6) had a numerically higher ctDNA detectable rate at C2D1 compared to patients who completed surgery (n = 19) (83% versus 32%, respectively; Fisher’s exact test, P = 0.056). d, At C3D1, patients who did not complete surgery (n = 6) had a significantly higher ctDNA detectable rate compared to patients who underwent surgery (n = 15) (100% versus 7%, respectively; Fisher’s exact test, P = 0.00013). e, At the pre-surgery timepoint, patients who did not complete surgery (n = 6) had a significantly higher ctDNA detectable rate compared to patients who completed surgery (n = 19) (100% versus 37%, respectively; Fisher’s exact test, P = 0.015). f, Patients with undetectable ctDNA at C3D1 (n = 14) had longer PFS compared to patients with detectable ctDNA at C3D1 (n = 7) (median PFS 19.84 months versus 1.41 months, respectively; log-rank test, P = 0.027; HR = 0.32 (95% CI: 0.11–0.92)). g, Patients with undetectable ctDNA pre-surgery (n = 12) had longer PFS compared to patients with detectable ctDNA pre-surgery (n = 13) (median PFS 23.26 months versus 2.46 months, respectively; log-rank test, P = 0.0059; HR = 0.29 (95% CI: 0.12–0.73)). h, In addition to the above single-timepoint analyses, we assessed ctDNA dynamics by considering patients who experienced ≥95% reduction in cfDNA TF at the C3D1 and pre-surgery timepoints relative to C1D1 (n = 3), along with patients who had sustained undetectable ctDNA throughout the neoadjuvant interval (n = 9). These 12 patients had longer PFS compared to patients who had <95% reduction in cfDNA TF at C3D1 (n = 6) (median PFS 23.26 months versus 1.4 months, respectively; log-rank test, P = 1.8 × 10−6). i, Patients who had ≥95% reduction in cfDNA TF pre-surgery relative to C1D1 or had undetectable ctDNA throughout (n = 12) had longer PFS compared to patients who had <95% reduction in cfDNA TF (n = 11) (median PFS 23.26 months versus 1.68 months, respectively; log-rank test, P = 5.9 × 10−5; HR = 0.13 (95% CI: 0.04–0.4)). Reported P values are two-sided. UD, undetectable.
We then assessed whether ctDNA levels during neoadjuvant ICB were associated with PFS and OS. We hypothesized that undetectable ctDNA in a single-timepoint assessment would identify patients with longer survival independent of radiographic response. Consistent with our hypothesis, we found that patients with undetectable ctDNA at C3D1 had longer PFS (median PFS 19.84 months versus 1.41 months for ctDNA undetectable and ctDNA detectable, respectively) (log-rank test, P = 0.027; HR = 0.32, 95% CI: 0.11–0.92; Fig. 5f and Supplementary Table 7). Similarly, patients with undetectable ctDNA at the pre-surgery timepoint attained longer PFS (median PFS 23.26 months versus 2.46 months for ctDNA undetectable and ctDNA detectable, respectively) (log-rank test, P = 0.0059; HR = 0.29, 95% CI: 0.12–0.73; Fig. 5g). We observed numerically longer OS for patients with undetectable ctDNA at the pre-surgery timepoint (median OS 27.73 months versus 15 months; log-rank test, P = 0.16; HR = 0.5, 95% CI: 0.18–1.36), which was more pronounced for patients in Arm A (median OS 27.3 months versus 15 months; log-rank test, P = 0.065; HR = 0.33, 95% CI: 0.1–1.13; Extended Data Fig. 7). ctDNA status or TF at C1D1 was not associated with PFS or OS (Extended Data Fig. 7). In evaluating the association between ctDNA status and PFS by study arm, we noted longer PFS for patients with undetectable ctDNA in Arm A as early as the C2D1 timepoint (median PFS 22.49 months versus 2.07 months for ctDNA undetectable and ctDNA detectable, respectively; log-rank test, P = 0.00065) and extending to the C3D1 (median PFS 15.66 months versus 1.58 months, for ctDNA undetectable and ctDNA detectable, respectively; log-rank test, P = 0.0018) and pre-surgery timepoints (median PFS 22.49 months versus 2.07 months for ctDNA undetectable and ctDNA detectable, respectively; log-rank test, P = 0.00029); these trends were less obvious in Arm B (Extended Data Fig. 8). These findings suggest that molecular readout of residual disease at the C3D1 and pre-surgery timepoints may more optimally classify patients by risk of recurrence compared to earlier ctDNA assessments, where the therapeutic benefit has yet to be achieved.
The divergence between mRECIST assessments and ctDNA residual disease in relation to clinical outcomes led us to further evaluate the concordance between ctDNA kinetics and radiographic responses (Extended Data Fig. 9). We observed considerable heterogeneity in ctDNA kinetics for patients with radiographically stable or progressive disease, whereas two patients with mRECIST partial response had sustained undetectable ctDNA. Furthermore, we found that ctDNA dynamics and changes in the sum of longest diameters (SLD) were discordant with regard to the direction of the actual tumor burden kinetics (Extended Data Fig. 9). These findings highlight the challenges with radiographic assessment of treatment efficacy in resectable DPM that could be overcome using ultra-sensitive liquid biopsies.
We next expanded the single-timepoint analyses and evaluated dynamic changes in ctDNA levels between baseline (C1D1) and on-treatment timepoints (Supplementary Table 7). Patients who had either ≥95% cfDNA TF reduction from C1D1 to C3D1 or undetectable ctDNA throughout neoadjuvant ICB had longer PFS (median PFS 23.26 months versus 1.4 months; log-rank test, P = 1.8 × 10−6; Fig. 5h). Similarly, patients who had ≥95% cfDNA TF reduction from C1D1 to pre-surgery or undetectable ctDNA throughout neoadjuvant ICB had a trend toward longer PFS (median PFS 23.26 months versus 1.68 months; log-rank test, P = 5.9 × 10−5; HR = 0.13, 95% CI: 0.04–0.4; Fig. 5i) and numerically longer OS (median OS 27.73 months versus 15.47 months; log-rank test, P = 0.065; HR = 0.39, 95% CI: 0.14–1.1; Extended Data Fig. 10). Among those who underwent surgical resection, patients with either a ≥95% cfDNA TF reduction pre-surgery or undetectable ctDNA throughout the neoadjuvant interval had longer PFS (median PFS 23.26 months versus 7.26 months; log-rank test, P = 0.0063; HR = 0.2, 95% CI: 0.05–0.71) and OS (median OS 27.73 months versus 14.95 months; log-rank test, P = 0.031; HR = 0.22, 95% CI: 0.05–0.99; Extended Data Fig. 10). Collectively, these findings suggest that ultra-sensitive tumor-informed WGS-based liquid biopsies can quantify DPM-derived ctDNA during neoadjuvant ICB and consistently identify individuals at risk for disease recurrence, supporting the clinical utility of ctDNA residual disease analyses in this setting.
Discussion
In this prospective, multicenter, multiarm phase 2 clinical trial, we demonstrated that incorporating either perioperative nivo or neoadjuvant nivo/ipi plus adjuvant nivo was feasible and safe, without delaying planned surgery. Furthermore, neoadjuvant nivo/ipi followed by adjuvant nivo showed a promising clinical efficacy signal compared to historical data with systemic therapy alone. This trial demonstrates the feasibility of perioperative nivo monotherapy and combination nivo/ipi in resectable DPM, along with an ultra-sensitive molecular readout of neoadjuvant ICB using liquid biopsies.
Our results demonstrating the feasibility of ICB prior to resection in DPM align with previous studies of neoadjuvant ICB-containing regimens in resectable thoracic malignancies. In our study, over 80% of patients in both arms (Arm A: 81.3%, Arm B: 85.7%) proceeded to planned surgical resection within 24 days from the preplanned surgery date, meeting the protocol-defined feasibility threshold. This closely mirrors the resection rates seen in several large phase 3 clinical trials of both neoadjuvant and perioperative chemo-immunotherapy in resectable non-small cell lung cancer, in which in-trial resection rates ranged from 77% to 83%10,11,12. In DPM, our data align closely with a previously presented single-arm clinical study of neoadjuvant nivo plus platinum/pemetrexed chemotherapy in resectable DPM (NCT04162015)26, which used a feasibility cutpoint of 30 days from the preplanned surgery date and found that 95% of patients proceeded to attempted resection. The rates of attrition precluding surgery in our study align closely with larger prospective studies of neoadjuvant systemic therapy in resectable DPM. In the phase 3 MARS2 study8, although the trial was overall negative for survival, surgical resection was technically feasible, as only approximately 7% of patients randomized to chemotherapy plus surgery did not undergo resection after the planned two doses of chemotherapy. This suggests that, although resection using modern surgical techniques is feasible in DPM, more effective systemic treatment strategies are necessary to improve the chances of lasting clinical benefit after resection.
The intersection between neoadjuvant immunotherapy and definitive intent surgery has shown substantial efficacy across solid tumors27,28,29. Although the present study was not powered for an assessment of clinical efficacy, a potential signal of durable benefit was observed in patients treated with neoadjuvant nivo/ipi despite this arm encompassing less overall therapy (lower rates of adjuvant chemotherapy and/or radiation) than patients enrolled to the nivo monotherapy arm. Although the median PFS of 19.8 months and OS of 28.6 months are consistent with prior retrospective and single-arm studies evaluating a tri-modality approach of chemotherapy, radiotherapy and surgery, the potential of durable clinical benefit with dual ICB is notable, as eight of 14 patients in the combination ICB arm in our study were alive at the data cut date, of whom five were recurrence free on clinical and radiographic assessment. In addition, these data compare favorably to historical data for systemic therapy alone; in the phase 3 CheckMate 743 study, the median OS observed with combination nivo/ipi was 18.1 months, and the magnitude of benefit was most pronounced in patients with non-epithelioid DPM3. In our trial, enrollment was limited to patients with epithelioid and biphasic histology DPM. Patients with sarcomatoid histology were excluded, as standard practice for patients with sarcomatoid histology did not include surgery during the enrollment phase of this study, and enrollment was ongoing when results of the CheckMate 743 study were published, indicating robust clinical benefit of dual ICB in non-epithelioid DPM. Unfortunately, the limited number of patients with biphasic histology enrolled to the present study (five total: Arm A, 2; Arm B, 3) precludes an efficacy analysis of this subset. An ongoing prospective non-randomized phase 2 trial, A082101, is exploring neoadjuvant nivo/ipi in resectable sarcomatoid DPM (NCT05647265)30. The clinical efficacy for perioperative nivo in resectable DPM in our study was more modest, and, given the trend toward improved PFS/OS for patients who received perioperative nivo and chemotherapy in Arm A, our data highlight the potential importance of chemotherapy when a dual checkpoint blockade regimen is not used. Nevertheless, these data must be interpreted with caution given small numbers and confounding variables in those who proceeded to adjuvant chemotherapy.
In parallel, ctDNA ultra-sensitive residual disease detection approaches have been shown to be increasingly important in providing a molecular readout of ICB efficacy in resectable cancers. The potential of ctDNA approaches in refining response assessments has been increasingly recognized, including by the RECIST Working Group31. Such emerging technologies are needed for optimization of management of patients with resectable DPM, especially given the challenges with radiographic response in capturing tumor burden and therapy response23,32. Although tracking of molecular residual disease by tumor-naive liquid biopsy approaches is being incorporated into clinical trials in the metastatic setting18, the clinical utility of ctDNA residual disease is being actively investigated for resectable cancers, including in the neoadjuvant ICB setting11,20,23,33,34. Resectable DPM presents unique challenges in implementing liquid biopsies in clinical management, due to the low tumor mutation burden of mesotheliomas that limits the number of mutant loci detectable by conventional liquid biopsies relying on detecting coding non-synonymous mutations. Additionally, the low circulating tumor burden in patients with DPM necessitates ultra-sensitive methods with limit of detection (LOD) several orders of magnitude lower than those of tumor-naive approaches. Despite the promise of bespoke tumor-informed liquid biopsies in capturing MRD, these methods, including tracking chromosomal junctions35 and point mutations36 in patients with pleural and peritoneal mesothelioma, are limited by feasibility and operational and technical complexities. To this end, we employed a tumor-informed WGS-based ctDNA residual disease detection method that capitalizes on concurrent sequencing of matched tumor-normal DNA and cfDNA, followed by machine-learning-informed detection of high-confidence tumor-specific SNVs and calibration to a non-cancerous cfDNA reference to eliminate background noise. The novelty and clinical feasibility of this approach relies on the intersection of tumor and cfDNA WGS data to derive a credible set of SNVs, augmented by machine-learning-driven elimination of sequencing artifacts. Concurrent WGS analyses of tumor and cfDNA resulting in ultra-sensitive TF detection can alleviate challenges with personalized assay development as well as processing times. From a technical standpoint, we attained a 93.3% success rate in informative assays across the study cohort, and, notably, single and serial assessment of ctDNA levels during neoadjuvant ICB and immediately prior to surgery clearly captured disease progression during the neoadjuvant period as well as recurrence after definitive surgery. This molecular readout of neoadjuvant therapy is particularly important for patients with DPM, where both radiographic and pathologic response assessments are difficult to assess and do not capture the timing and magnitude of therapy response. Certainly, larger studies are required to solidify the timing, definition and clinical sensitivity of ctDNA residual disease in the context of neoadjuvant therapy for patients with DPM. Future studies will clarify the value of ctDNA status as an early endpoint in clinical trials to expedite efficacy analyses or as a tool for stratifying patient populations during treatment.
Our study has several notable limitations. From a clinical perspective, although the study was powered to evaluate the safety and feasibility of perioperative ICB in potentially resectable DPM, it was not sufficiently powered to evaluate efficacy. Therefore, key efficacy measures, such as PFS and OS, were exploratory in nature. In addition, the design of the study, with sequential enrollment to study arms, may have introduced potential confounding factors impacting the clinical outcomes. As an example, a greater proportion of patients enrolled in Arm A were male (81% versus 57% in Arm B), which itself is a negative prognostic factor in DPM and other tumor types37. As such, our findings should be interpreted with caution, and additional studies are warranted to prospectively evaluate the clinical efficacy of perioperative immunotherapy-containing regimens in resectable DPM. Furthermore, it is important to note that this study was conducted at centers with expertise in the perioperative management and surgical techniques required for potentially resectable DPM. The applicability of our findings may, therefore, have a more limited generalizability to centers that lack such a level of experience.
From a liquid biopsy methodology standpoint, the yield of our ultra-sensitive tumor-informed WGS ctDNA residual disease assay depends on the number of informative SNVs derived from tumor-normal WGS, which imposes a challenge with ctDNA detection in tumors with low tumor mutation burden, such as mesotheliomas. These challenges have previously precluded meaningful ctDNA analyses in patients with mesothelioma, especially in the early-stage setting where ctDNA levels are very low. In tandem, the mode of spreading of pleural mesothelioma in a locally invasive rather than vascular dissemination pattern imposes further challenges to ctDNA detection in peripheral blood. Despite these challenges, in recovering a median of 861 informative SNVs (IQR, 720–1,120) across the study cohort, we detected a sizable fraction of cases at baseline and during the neoadjuvant interval (12/46 (46%) and 43/97 (44.3%) plasma samples, respectively). By contrast, previous studies employing tumor-informed droplet digital polymerase chain reaction (ddPCR)-based methods showed a detection rate of 30–36% in resectable mesotheliomas36,38, which further highlights the benefit of employing tumor-informed genome-wide liquid biopsy approaches compared to single-mutation tracking.
Taken together, our findings support the feasibility and safety of neoadjuvant ICB for patients with resectable DPM and highlight the potential of ctDNA analyses to detect residual disease and further optimize precision therapeutic interventions.
Methods
Study design, eligibility criteria and participants
This was a prospective, multicenter, multiarm phase 2 clinical trial enrolling patients at the Johns Hopkins Sidney Kimmel Comprehensive Cancer Center (JHSKCCC) (Baltimore, Maryland), The University of Texas MD Anderson Cancer Center (MDACC) (Houston, Texas) and the University of Maryland Greenebaum Comprehensive Cancer Center (UMGCCC) (Baltimore, Maryland) (ClinicalTrials.gov identifier: NCT03918252, study preregistration date: 15 April 2019). The study protocol and all amendments were approved by the institutional review board (IRB) of Johns Hopkins University (Johns Hopkins Medicine IRB 6) as well as the individual IRBs of all participating institutions. A detailed summary of all protocol amendments can be found in Supplementary Table 8. The study was conducted in accordance with the Declaration of Helsinki and the international standards of Good Clinical Practice. Written informed consent was obtained from all study participants; participants were not compensated monetarily for participation in this trial. The first patient was enrolled onto the trial on 29 October 2019, and the last patient was enrolled on 22 January 2024. The database lock date for this analysis was 4 January 2025. Patients aged 18 years of age or older with epithelioid or biphasic DPM histology and primary tumor amenable to surgical resection as determined by the multidisciplinary treatment team were eligible to enroll in the trial. All patients had to have ECOG performance status of 0 or 1 as determined by the treating investigator as well as adequate organ function and cardiovascular fitness for surgery (full inclusion criteria are listed below). Sex was self-reported. Both females and males were eligible for enrollment, and sex was not a stratification criterion. Patients were excluded from the study if they were poor surgical candidates, had unresectable DPM or had pure sarcomatoid histology. Patients were also excluded if they had active autoimmune disease, had a clinically significant active concurrent malignancy or had received prior treatment with an anti-PD-(L)1 or anti-CTLA-4 agent (full exclusion criteria are listed below).
Inclusion criteria
-
Men and women ≥18 years of age
-
Primary tumor amenable to safe research biopsy. A tumor biopsy is required for study entry.
-
Histology-proven epithelial or biphasic DPM:
-
Diagnostic core biopsy specimens must be reviewed by a faculty pathologist at JHSKCCC, MDACC or UMGCCC.
-
Either a formalin-fixed paraffin block that has been confirmed by a pathologist to contain tumor or a minimum of 20 5-µm tissue sections (slides) of tumor biopsy sample must be available for biomarker evaluation (study pathologist must review for adequacy of sampling). This can be obtained from archival tissue (if adequate) or from a new biopsy if needed.
-
-
Resectable DPM (stage I–III) deemed to be potentially surgically resectable as assessed by faculty surgeons at JHSKCCC, MDACC or UMGCCC
-
ECOG performance status 0 or 1
-
Adequate organ function as follows:
-
Leukocytes ≥2,000 per mm3
-
Absolute neutrophil count ≥1,000 per mm3
-
Platelet count ≥100,000 per mm3
-
Hemoglobin ≥9 g dl−1
-
Creatinine ≤1.5× upper limit of normal (ULN) or creatinine clearance ≥40 ml min−1 (if using the Cockcroft–Gault formula)
-
Total bilirubin ≤1.5× institutional ULN (except patients with Gilbert syndrome who can have total bilirubin <3.0 mg dl−1)
-
Aspartate aminotransferase (serum glutamic-oxaloacetic transaminase), alanine transaminase (serum glutamic-pyruvic transaminase) and alkaline phosphatase ≤3 times the institutional ULN
-
Adequate lung function to permit surgical resection determined by pre-enrollment pulmonary function tests, to include diffusing capacity of the lungs for carbon monoxide
-
-
Women of childbearing potential (WOCBP) and men must agree to use adequate contraception prior to study entry and for the duration of study participation up to and including 23 weeks after the last dose of nivo. Should a woman become pregnant or suspect she is pregnant while she or her partner is participating in this study, she should inform her treating physician immediately. Sexually active fertile men must use effective barrier birth control if their partners are WOCBP for up to 31 weeks after the last dose of nivo. WOCBP must have a negative serum or urine pregnancy test within 2 weeks of registration. Women must not be breastfeeding.
Patient understands the study regimen and its requirements, risks and discomforts and is able and willing to sign the informed consent form. Voluntary signed and dated IRB/independent ethics committee (IEC)-approved written informed consent form in accordance with regulatory and institutional guidelines must be obtained before the performance of any protocol-related procedure.
Exclusion criteria
-
Stage I–III DPM deemed to be unresectable, a poor surgical candidate or unfit for study therapy as assessed by study investigators
-
Pure sarcomatoid histology
-
Active, known or suspected autoimmune disease
-
Patients are permitted to enroll if they have vitiligo, type 1 diabetes mellitus, residual hypothyroidism due to an autoimmune condition requiring only hormone replacement, psoriasis not requiring systemic treatment or conditions not expected to recur in the absence of an external trigger.
-
-
Patient with a condition requiring systemic treatment with either corticosteroids (>10-mg daily prednisone equivalents) or other immunosuppressive medications within 14 days of study drug administration. Inhaled or topical steroids and adrenal replacement doses >10-mg daily prednisone equivalents are permitted in the absence of active autoimmune disease. As there is potential for hepatic toxicity with nivo or nivo/ipi combinations, drugs with a predisposition to hepatotoxicity should be used with caution in patients treated with a nivo-containing regimen.
-
Administration of chemotherapy or any other cancer therapy in the preoperative period
-
Patients with active concurrent malignancies are excluded—that is, cancers other than DPM (except non‐melanoma skin cancers, cervical dysplasia and in situ cancers of bladder, stomach, breast, colon and cervix).
-
Patients with a history of symptomatic interstitial lung disease
-
Active systemic infection requiring therapy as well as presence of acute or chronic hepatitis B or active hepatitis C or HIV infection. Patients with resolved hepatitis B virus infection (defined as the presence of hepatitis B core antibody (HBcAb) and absence of hepatitis B surface antigen (HBsAg)) are eligible provided the hepatitis virus DNA test is negative. Patients positive for hepatitis C antibody are eligible only if PCR is negative for hepatitis C virus RNA. Testing for HIV is required only if clinically indicated and is not mandated for this study.
-
Known positive history or positive test for HIV or AIDS
-
History of allergy to study drug components
-
Women who are pregnant or nursing
-
Men with female partners (WOCBP) who are unwilling to use contraception.
-
Prior therapy with an anti-PD-1, anti-PD-L1, anti-PD-L2 or anti-CTLA-4 antibody (or any other antibody targeting T cell co-regulatory pathways)
-
History of any other condition that may require the initiation of anti-TNF therapies or other immunosuppressant medications during the study
-
Underlying medical conditions that, in the investigator’s opinion, will make the administration of study drug hazardous or obscure the interpretation of toxicity or AEs
-
Prisoners or individuals who are involuntarily incarcerated or compulsorily detained for treatment of either a psychiatric or physical (for example, infectious disease) illness
Treatment and protocol amendments
Patients were enrolled in two treatment cohorts consecutively. The decision to pursue sequential enrollment to each study arm rather than randomization was based on the primary endpoints of safety and feasibility, coupled with the historically increased incidence of immunotherapy-related toxicity with combination anti-PD-1/anti-CTLA-4 immunotherapy compared to anti-PD-1 monotherapy. The goal was to determine these primary endpoints with neoadjuvant nivo monotherapy (and ensure that the protocol-defined safety and feasibility stopping rules were not met) before proceeding to evaluate combination nivo/ipi. The original intent was to enroll 15 patients sequentially in each treatment arm. In addition, the protocol specified that patients who did not undergo surgical resection would be replaced and not count toward the overall accrual goal. However, this was not executed for the study duration, which overlapped with the emergence of the COVID-19 pandemic, resulting in a discrepancy in accrual, with 16 patients enrolled to Arm A and 14 patients enrolled to Arm B. In Arm A, patients received intravenous nivo 240 mg q2w for three doses. In Arm B, patients received intravenous nivo 3 mg kg−1 q2w for three doses together with intravenous ipi 1 mg kg−1 administered on day 1 only. In both cohorts, after neoadjuvant therapy, patients proceeded to surgical resection using the surgical technique (EPP or P/D) deemed most appropriate by the treating surgeon. After surgery, patients received four cycles of adjuvant platinum/pemetrexed combination chemotherapy (cisplatin preferred if clinically appropriate) according to accepted standard dosing and schedules. After chemotherapy, postoperative radiotherapy was administered for all patients who underwent EPP and was offered to patients undergoing P/D at the discretion of the treatment team. After this, patients received intravenous nivo 480 mg q4w for a planned 1-year duration of therapy or until unacceptable toxicity/clinical progression, whichever came first. A list of all protocol amendments is included in Supplementary Table 8.
Assessments and endpoints
The co-primary endpoints were feasibility and safety. We hypothesized that the administration of neoadjuvant nivo and nivo/ipi, respectively, would be feasible without an extended treatment-related delay in resection, defined as a delay of more than 24 days from the preplanned initial surgery date. We anticipated a high feasibility rate, with 80% or more of patients proceeding to surgery within this window. Feasibility was monitored using a Bayesian framework with a Beta(8,2) prior distribution. Using this framework, a treatment approach would be considered feasible if the 90% pCI included the 80% threshold. A stopping rule was implemented such that enrollment would be paused if the posterior probability that fewer than 80% of patients would proceed to surgery without delay exceeded 90%. Safety was assessed per Common Terminology Criteria for Adverse Events version 5.0, with DLTs monitored through 100 days after the last neoadjuvant dose or 30 days after surgery (whichever was longer). A safety stopping rule was implemented using a Beta prior distribution with parameters 1 and 3, such that if the posterior probability of risk of grade 3–4 treatment-related toxicities exceeding 25% is 70% or higher, based on Bayes’ rule and the assumption implied by the prior, the study will stop.
Secondary endpoints included ORR, safety profile of adjuvant nivo and pathologic response assessment. Radiographic response was determined using mRECIST for malignant pleural mesothelioma (version 1.1) on computed tomography scans before and after neoadjuvant therapy. Positron emission tomography/computed tomography and chest computed tomography with intravenous contrast were performed during screening (up to 28 days prior to the first dose of neoadjuvant therapy) and within 72 hours prior to planned surgical resection. After surgery, chest computed tomography with intravenous contrast was performed after four cycles of adjuvant chemotherapy, prior to radiation therapy (if needed for radiation planning) and every 3 months during adjuvant nivo. The toxicity profile of adjuvant nivo was assessed by determining the frequency of grade 3–4 AEs related to nivo in both study arms occurring within 100 days of last study drug administration. Pathologic response assessment to neoadjuvant immunotherapy, although listed as a planned secondary objective, was not assessed due to the complexities of performing and standardizing pathologic response for DPM.
Key exploratory objectives included PFS and OS. PFS was defined as the time from initiation of neoadjuvant therapy to progression precluding surgery, recurrence post-surgery or death. OS was defined as the time from neoadjuvant therapy initiation to death. Patients who did not experience an event of interest at the data cut date (4 January 2025) were censored at the date they were last known to be alive and recurrence free (for PFS) or alive (for OS). Follow-up for PFS and OS occurred every 3–6 months for 2 years and then every 6–12 months for 5 years.
Longitudinal ctDNA assessment was a key exploratory objective, described in detail below. Additional protocol-defined exploratory objectives under active investigation that are not reported in this paper include the following: (1) to determine the changes in the genomic landscape, global expression and expression of select immune markers compared to baseline in blood, primary tumor tissue and tumor-draining lymph nodes as well as to evaluate the changes in tumor-infiltrating lymphocytes and to compare findings in tumor/draining lymph nodes to those of a parallel stage-matched cohort of untreated patients; (2) to evaluate the potential effects of neoadjuvant therapy on normal pleural tissues; (3) to explore the association between ICB exposure and select pharmaco-dynamic biomarkers, such as PD-1 receptor occupancy; (4) to evaluate baseline and serial markers of immunogenicity among ICB-treated patients and with patients who did not receive ICB prior to surgery on a parallel tissue collection protocol; and (5) to explore biologic features of the gut microbiome and correlate with clinical response.
WGS cfDNA MRD analyses
WGS was performed on matched tumor (n = 30 samples), WBC (n = 30 samples) and serial plasma (n = 123 samples) for all 30 enrolled patients. Primary tumor material was collected from pretreatment biopsies and from surgical resections and then formalin fixed and paraffin embedded (FFPE). Serial blood samples were collected before therapy initiation, on day 1 of cycles 2 and 3, immediately before surgical resection and at several postoperative follow-ups. Postoperative timepoints were collected with the intent to both capture MRD after curative intent surgery and to continue assessment of systemic tumor burden during the adjuvant window. Tumor DNA was macrodissected from FFPE tumor tissue using a QIAamp DNA FFPE Tissue Kit and briefly sheared using Covaris Focused-ultrasonicators (Covaris). Germline DNA was isolated from WBCs using a QIAamp DNA Blood Mini Kit (Qiagen), and cfDNA was isolated using a QIAamp Circulating Nucleic Acid Kit (Qiagen).
Labcorp Plasma Detect, a Clinical Laboratory Improvement Amendments (CLIA)-certified and College of American Pathologists (CAP)-accredited tumor-informed WGS ctDNA assay, was used to perform MRD analyses39,40. WGS was performed on tumor tissue, WBCs and plasma-derived DNA using up to 200 ng, 50 ng and 10 ng of input material, respectively, with the Illumina NovaSeq 6000 platform at targets of 80×, 40× and 30× coverage depth, respectively (Supplementary Tables 5 and 6). Tumor-specific SNVs were identified from tumor and germline datasets, from which a candidate variant set was used to determine the presence of ctDNA within plasma DNA through a random forest machine learning model. Specifically, candidate tumor-specific SNVs identified in the test sample were scored (ranging from 0 to 1) using a random forest machine learning algorithm trained using the ‘caret’ package (version 6.0.90) within the R statistical computing environment (version 4.1.1). Model training occurred independently of the clinical trial cohort, using a combination of contrived reference cell line and non-cancerous donor specimens, ultimately leveraging 500 trees, approximately 7–8 levels and approximately 150,000 leaves. To avoid overfitting, model training used five-fold cross-validation and limited the number of selected variables per split procedure (hyperparameter ‘mtry’) to the square root of the total number of input features. Finally, variants present in properly paired mapped fragments with a random forest score greater than 0.25 were further assessed, requiring an alternate read mapping quality of ≥30 and a read-based mutation rate of ≤5. ctDNA status was determined based on the aggregate level of signal observed across all candidate variants compared to a commercially procured reference population of non-cancerous donor plasma samples (n = 80, obtained under IRB approval from Discovery Life Sciences), and a cutoff of 1 s.d. above the maximum observed value was required to report a plasma sample as ctDNA positive. An estimated TF was then calculated for each ctDNA-positive sample based on the aggregate variant allele observations observed as a proportion of the total unique coverage of all individual tumor-specific variants assessed. The paired tumor-normal WGS analyses of two patients were uninformative due to low numbers of received SNVs, precluding robust ctDNA-level assessments in 10 plasma samples. The median number of SNVs comprising the 28 informative patient-specific mutation signatures was 861 (IQR, 720–1,120; Supplementary Table 5).
The LOD of the Labcorp Plasma Detect assay was previously reported at a level of 0.005% tumor content for LOD95% and 0.001% tumor content for LOD50%40. The assay has an analytical specificity of 99.6%, determined through analyses of non-cancerous donor plasma specimens and evaluated against reference whole-genome somatic mutation datasets. The reproducibility of the assay was tested in contrived reference control samples of known tumor content, with a coefficient of variation of 7.2%, indicating robust reproducibility across sequencing runs39,40.
Statistical analyses
For the clinical trial endpoints, analyses were descriptive. PFS and OS were summarized using the Kaplan–Meier method, with median estimates and associated 95% CIs. No formal hypothesis testing or between-arm comparisons were conducted. Exploratory analyses of ctDNA were conducted to investigate associations with clinical outcomes. Comparisons of survival between ctDNA-defined subgroups were performed using the log-rank test. A univariate Cox proportional hazards model was used to determine the HRs and the corresponding 95% CIs for individual explanatory variables. When the HR was undefined because the event times in one group entirely preceded those in the other, log-rank P values were provided as a descriptive comparison. Associations between categorical variables were assessed using Fisher’s exact test due to small sample sizes, and non-parametric comparisons of continuous variables were evaluated using the Mann–Whitney U-test to relax the assumption of normality. Summary statistics were calculated using all available observations for a given parameter. Given the variability in the number of patients evaluable at specific timepoints for ctDNA analyses, the number of available observations is listed alongside summary statistics where applicable. Missing data for ctDNA analyses are explicitly described in Supplementary Table 7. To evaluate deep cfDNA TF reduction between baseline and an on-therapy timepoint, we limited the analysis to patients with available baseline and timepoint of interest cfDNA WGS data. Patients were categorized into two groups: (1) patients with ≥95% reduction of cfDNA TF between baseline and the timepoint of interest or those with undetectable ctDNA across all neoadjuvant timepoints who had cfDNA WGS data available for baseline and timepoint of interest; and (2) patients with <95% reduction of cfDNA TF between baseline and the timepoint of interest. Patients who did not have either baseline or timepoint cfDNA WGS data were excluded from the analysis as TF reduction could not be quantified. Similarly, patients with undetectable ctDNA at both baseline and timepoint of interest who had detectable ctDNA in at least one other neoadjuvant timepoint were excluded from analysis. No imputation was performed, as the pattern of missingness could not be reliably assessed to support unbiased inference. Two-sided nominal P values less than 0.05 were considered statistically significant for exploratory analyses. No correction for multiple testing was applied, consistent with the prespecified statistical analysis plan and the exploratory nature of the liquid biopsy analyses. All analyses were conducted using R software version 4.4.3.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
WGS data from tumor and normal DNA alongside serial plasma cfDNA are deposited and can be retrieved from the European Genome-phenome Archive (EGA study accession EGAS50000001195, EGA dataset EGAD50000001701). The following Data Use Ontologies (DUO) are linked with this EGA dataset, related to privacy restrictions included in the informed consent. (1) Not-for-profit, non-commercial use only; this data use modifier indicates that use of the data is limited to not-for-profit organizations and not-for-profit use, non-commercial use. (2) Ethics approval required; this data use modifier indicates that the requestor must provide documentation of local IRB/ERB approval. (3) User-specific restriction; this data use modifier indicates that use is limited to use by approved users. (4) Project-specific restriction; this data use modifier indicates that use is limited to use within an approved project. To retrieve the dataset, access can be requested from the Data Access Committee (EGA accession EGAC50000000706) through the EGA portal. After the request for access, the requester will receive a data access agreement that must be completed with a description of the research in which the dataset will be used. Commercial/for-profit use of the dataset is not allowed per regulatory mandates, and the requester must provide documentation of local IRB approval. After review and sign-off by the requester and the requester’s institution’s regulatory official, the data access agreement will be reviewed by the Office of Research Administration at Johns Hopkins University. Upon finalization of the data access agreement, the dataset will be released to the requester through the EGA. The timeline for the above process depends on the speed of regulatory review required. Source data for all figures are provided in the Supplementary Tables.
References
Huang, J. et al. Global incidence, risk factors, and temporal trends of mesothelioma: a population-based study. J. Thorac. Oncol. 18, 792–802 (2023).
Baas, P. et al. First-line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): a multicentre, randomised, open-label, phase 3 trial. Lancet 397, 375–386 (2021).
Peters, S. et al. First-line nivolumab plus ipilimumab versus chemotherapy in patients with unresectable malignant pleural mesothelioma: 3-year outcomes from CheckMate 743. Ann. Oncol. 33, 488–499 (2022).
Chu, Q. et al. Pembrolizumab plus chemotherapy versus chemotherapy in untreated advanced pleural mesothelioma in Canada, Italy, and France: a phase 3, open-label, randomised controlled trial. Lancet 402, 2295–2306 (2023).
de Perrot, M. et al. Trimodality therapy with induction chemotherapy followed by extrapleural pneumonectomy and adjuvant high-dose hemithoracic radiation for malignant pleural mesothelioma. J. Clin. Oncol. 27, 1413–1418 (2009).
Krug, L. M. et al. Multicenter phase II trial of neoadjuvant pemetrexed plus cisplatin followed by extrapleural pneumonectomy and radiation for malignant pleural mesothelioma. J. Clin. Oncol. 27, 3007–3013 (2009).
Treasure, T. et al. Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol. 12, 763–772 (2011).
Lim, E. et al. Extended pleurectomy decortication and chemotherapy versus chemotherapy alone for pleural mesothelioma (MARS 2): a phase 3 randomised controlled trial. Lancet Respir. Med. 12, 457–466 (2024).
Cascone, T. et al. Perioperative nivolumab in resectable lung cancer. N. Engl. J. Med. 390, 1756–1769 (2024).
Wakelee, H. et al. Perioperative pembrolizumab for early-stage non-small-cell lung cancer. N. Engl. J. Med. 389, 491–503 (2023).
Forde, P. M. et al. Neoadjuvant nivolumab plus chemotherapy in resectable lung cancer. N. Engl. J. Med. 386, 1973–1985 (2022).
Heymach, J. V. et al. Perioperative durvalumab for resectable non-small-cell lung cancer. N. Engl. J. Med. 389, 1672–1684 (2023).
Van Schil, P. Malignant pleural mesothelioma: staging systems. Lung Cancer 49, S45–S48 (2005).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
Oxnard, G. R., Armato, S. G. III & Kindler, H. L. Modeling of mesothelioma growth demonstrates weaknesses of current response criteria. Lung Cancer 52, 141–148 (2006).
Byrne, M. J. & Nowak, A. K. Modified RECIST criteria for assessment of response in malignant pleural mesothelioma. Ann. Oncol. 15, 257–260 (2004).
Armato, S. G. III & Nowak, A. K. Revised Modified Response Evaluation Criteria in Solid Tumors for assessment of response in malignant pleural mesothelioma (version 1.1). J. Thorac. Oncol. 13, 1012–1021 (2018).
Anagnostou, V. et al. ctDNA response after pembrolizumab in non-small cell lung cancer: phase 2 adaptive trial results. Nat. Med. 29, 2559–2569 (2023).
Anagnostou, V. et al. Dynamics of tumor and immune responses during immune checkpoint blockade in non-small cell lung cancer. Cancer Res. 79, 1214–1225 (2019).
Kelly, R. J. et al. Neoadjuvant nivolumab or nivolumab plus LAG-3 inhibitor relatlimab in resectable esophageal/gastroesophageal junction cancer: a phase Ib trial and ctDNA analyses. Nat. Med. 30, 1023–1034 (2024).
Cascone, T. et al. Neoadjuvant durvalumab alone or combined with novel immuno-oncology agents in resectable lung cancer: the phase II NeoCOAST platform trial. Cancer Discov. 13, 2394–2411 (2023).
Anagnostou, V. & Velculescu, V. E. Pushing the boundaries of liquid biopsies for early precision intervention. Cancer Discov. 14, 615–619 (2024).
Aredo, J. V. et al. Liquid biopsy approaches for cancer characterization, residual disease detection, and therapy monitoring. Am. Soc. Clin. Oncol. Educ. Book 45, e481114 (2025).
Bueno, R. et al. Comprehensive genomic analysis of malignant pleural mesothelioma identifies recurrent mutations, gene fusions and splicing alterations. Nat. Genet. 48, 407–416 (2016).
Frydendahl, A. et al. Whole-genome sequencing of cell-free DNA reveals DNA of tumor origin in plasma from patients with colorectal adenomas. Mol. Oncol. 19, 984–993 (2025).
Offin, M. et al. Feasibility and safety of neoadjuvant nivolumab and chemotherapy for resectable diffuse pleural mesotheliomas: results of a prospective pilot study. J. Clin. Oncol. 42, 8003–8003 (2024).
Blank, C. U. et al. Neoadjuvant nivolumab and ipilimumab in resectable stage III melanoma. N. Engl. J. Med. 391, 1696–1708 (2024).
Forde, P. M. et al. Overall survival with neoadjuvant nivolumab plus chemotherapy in lung cancer. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2502931 (2025).
Janjigian, Y. Y. et al. Perioperative durvalumab in gastric and gastroesophageal junction cancer. N. Engl. J. Med. 393, 217–230 (2025).
Mansfield, A. S. et al. Neoadjuvant immunotherapy in sarcomatoid mesothelioma (Alliance A082101). J. Clin. Oncol. 41, TPS8602 (2023).
Wyatt, A. W. et al. Plasma ctDNA as a treatment response biomarker in metastatic cancers: evaluation by the RECIST Working Group. Clin. Cancer Res. 30, 5034–5041 (2024).
Kindler, H. L. et al. Treatment of pleural mesothelioma: ASCO guideline update. J. Clin. Oncol. 43, 1006–1038 (2025).
Reck, M. et al. LBA59 Associations of ctDNA clearance and pathological response with neoadjuvant treatment in patients with resectable NSCLC from the phase III AEGEAN trial. Ann. Oncol. 34, S1300 (2023).
Black, J. R. M. et al. Ultrasensitive ctDNA detection for preoperative disease stratification in early-stage lung adenocarcinoma. Nat. Med. 31, 70–76 (2025).
Parikh, K. et al. Individualized cell-free DNA monitoring with chromosomal junctions for mesothelioma. JTO Clin. Res. Rep. 5, 100692 (2024).
Hylebos, M. et al. Tumor-specific genetic variants can be detected in circulating cell-free DNA of malignant pleural mesothelioma patients. Lung Cancer 124, 19–22 (2018).
Alpert, N., van Gerwen, M., Flores, R. & Taioli, E. Gender differences in outcomes of patients with mesothelioma. Am. J. Clin. Oncol. 43, 792–797 (2020).
Zhang, M. et al. Clonal architecture in mesothelioma is prognostic and shapes the tumour microenvironment. Nat. Commun. 12, 1751 (2021).
Alarcon, C. et al. Abstract 6559: Clinical validity of post-surgery circulating tumor DNA testing in stage III colon cancer patients treated with adjuvant chemotherapy: the PROVENC3 study. Cancer Res. 84, 6559 (2024).
Georgiadis, A. et al. Abstract ST135: Detecting molecular residual disease through integrated tumor tissue, germline, and plasma whole genome sequencing analyses. Association for Molecular Pathology 2023 Annual Meeting Abstracts. J. Mol. Diagn. https://doi.org/10.1016/S1525-1578(23)00249-0 (2023).
Acknowledgements
This trial was an investigator-initiated study supported by a research grant from Bristol Myers Squibb. We would like to thank the clinical research team at the Johns Hopkins Upper Aerodigestive Malignancies Program for their contributions to patient enrollment and clinical trial operations and N. Rao and K. Velliangiri for sample processing. This work was supported, in part, by Department of Defense Congressionally Directed Medical Research Programs grant CA190755 (V.A. and P.M.F.), the Johns Hopkins Sidney Kimmel Comprehensive Cancer Center core grant (National Cancer Institute CCSG P30 CA006973 (V.A.)), FDA grant U01FD005942-FDA (V.A.), National Institutes of Health grant CA121113 (V.A.), the Bloomberg–Kimmel Institute for Cancer Immunotherapy (V.A., J.R.B., P.M.F., J.T., K.N.S. and D.M.P.), ECOG-ACRIN Thoracic Malignancies Integrated Translational Science Center grant UG1CA233259 (V.A.), the Robyn Adler Fellowship Award (E.O.), the Commonwealth Foundation (V.A.), the Mark Foundation for Cancer Research (J.T., K.N.S. and D.M.P.), the Mesothelioma Applied Research Foundation (J.E.R.) and the Florence Lomax Eley Fund (V.A. and J.R.B.).
Author information
Authors and Affiliations
Contributions
P.M.F., J.E.R. and V.A. conceived the study and contributed to the study design, data analyses and manuscript writing. R.J.M., R.J.B., R.K.H., J.F., B.S., J.S.D., T.C., J.T., P.B.I., K.N.S., D.M.P., A.S.T. and J.R.B. contributed to study investigation and manuscript writing. C.H., M.Z. and S.K. contributed to statistical analyses, manuscript writing and data visualization. P.K.L. and Q.M. performed experiments. P.K.L., A.J., M.N., N.N., J.W. and E.O. contributed to data curation, analysis and visualization. G.P. and S.H.N. contributed to biospecimen curation and project administration. M.S. contributed to data interpretation and manuscript writing. All authors edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
J.E.R. receives research funding to his institution from Genentech/Roche, Verastem, Nuvalent, Arcus, Revolution Medicines, Regeneron, Amgen, DualityBio and AstraZeneca and serves in a consultant/advisory role for AstraZeneca, Bristol Myers Squibb, Daiichi Sankyo, Seagen, Gilead, Janssen, Novocure, Regeneron, Summit Therapeutics, Pfizer, Eli Lilly, Natera, Merck, EMD Serono, Roche Diagnostics and OncoHost. C.H. serves in a consultant/advisory role for Belay Diagnostics and Johnson & Johnson. N.N. is an inventor on patent application 17/598,690 submitted by Johns Hopkins University related to genomic features of response to immunotherapy. M.S. is employed by and owns stock in Labcorp. J.S.D. receives research funding to the institution from Bristol Myers Squibb and is a consultant for NextPoint Therapeutics. J.T. has participated on advisory boards for AstraZeneca, Bristol Myers Squibb, Merck, Regeneron, Elephas, Lunaphore, Roche and Moderna and has received research grants from Bristol Myers Squibb and Akoya Biosciences. T.R.C. reports research funding received by the institution from Janssen; receiving honoraria from AstraZeneca, the Society for Immunotherapy of Cancer and TotalCME; and being named on a patent for a machine learning algorithm for immune-related pathologic response criteria. P.B.I. reports consulting/advisory board membership for AstraZeneca, Bristol Myers Squibb, Roche, Sanofi, AbbVie, Merus and Agilent. K.N.S. has received honoraria from Adaptive Biotechnologies and Illumina; has received research support from AbbVie, Bristol Myers Squibb and AstraZeneca; holds several patents related to the MANAFEST technology and TCR discovery; and is a scientific founder of Clasp Therapeutics. D.M.P. holds equity in Aduro Biotech, DNAtrix, Ervaxx, Five Prime Therapeutics, Immunomic, Potenza and Trieza Therapeutics. D.M.P. is a member of scientific advisory boards for Bristol Myers Squibb, Camden Nexus II, Five Prime Therapeutics and WindMIL. D.M.P. is a member of the board of directors for Dracen Pharmaceuticals. A.S.T. receives research funding to the institution from Ariad, Bristol Myers Squibb, Eli Lilly, Genentech, Millennium, Polaris, AstraZeneca, Boehringer Ingelheim, Epizyme, Merck, Novartis and Seattle Genetics and receives consulting fees from Ariad, Bristol Myers Squibb, Eli Lilly, Genentech, Merck, Pfizer, Seattle Genetics, AstraZeneca, Boehringer Ingelheim, EMD Serono, GlaxoSmithKline, Novartis and Roche. J.R.B. receives research funding to Johns Hopkins University from AstraZeneca and Bristol Myers Squibb; serves in a consultant/advisory role for AstraZeneca, RAPT Therapeutics, Mestag, GlaxoSmithKline, Amgen, Sanofi Aventis, Summit Therapeutics, Genentech and Bayer; and is on the Data Safety and Monitoring Board (DSMB) for Genmab. P.M.F. has received research funding (directly to the institution) from AstraZeneca, Bristol Myers Squibb, Novartis, Regeneron, Kyowa and BioNTech; has served in a consultant/advisory role for AstraZeneca, AbbVie, Amgen, Ascendis, BioNTech, Bristol Myers Squibb, ChromaCode, Daiichi Sankyo, F-Star, Genelux, Gilead, iTeos, Novartis, Novocure, Regeneron, Tavotek, Teva, Genentech, Sanofi, Surface, Janssen, G1 and Merck; and has served on DSMBs for Polaris and Flame. V.A. receives research funding to Johns Hopkins University from AstraZeneca and Personal Genome Diagnostics; has received research funding to Johns Hopkins University from Bristol Myers Squibb and Delfi Diagnostics in the past 5 years; is an advisory board member for AstraZeneca and NeoGenomics (compensated); and receives honoraria from Foundation Medicine, Guardant Health, Roche and Personal Genome Diagnostics. These arrangements have been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies. V.A. is an inventor on patent applications (63/276,525, 17/779,936, 16/312,152, 16/341,862, 17/047,006 and 17/598,690) submitted by Johns Hopkins University related to cancer genomic analyses, ctDNA therapeutic response monitoring and immunogenomic features of response to immunotherapy that have been licensed to one or more entities. Under the terms of these license agreements, the university and inventors are entitled to fees and royalty distributions. The other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Melina Marmarelis, Ana Vivancos and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Saheli Sadanand, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Clinical trial schema and sample disposition for the trial participants.
(a) Patients with surgically resectable epithelioid and biphasic DPM were consecutively enrolled in the following two treatment cohorts: Nivolumab 240 mg IV on D-42, D-28 and D-14 (Arm A) or nivolumab 3 mg/kg + ipilimumab 1 mg/kg IV on D-42, followed by nivolumab 3 mg/kg IV on D-28 and D-14 (Arm B), followed by surgical resection (D0). Adjuvant chemotherapy and adjuvant radiation were not mandatory but were offered to patients after surgery. Adjuvant nivolumab was administered after any adjuvant chemotherapy and/or radiation for 1 year. The dual primary endpoints of the trial were safety and feasibility, and exploratory endpoints included PFS, OS, and longitudinal assessment of tumor-informed plasma cfDNA WGS to capture ctDNA residual disease. (b) This diagram illustrates the biospecimens procured for tumor-informed liquid biopsy analyses collected from the 30 patients enrolled in the clinical trial NCT03918252. A tumor-informed WGS-based approach allowed for ultra-sensitive detection of ctDNA across 123 serial plasma samples. WGS of paired tumor and WBC DNA samples generated 28 informative patient-specific SNV sets to be tracked longitudinally in matched serial plasma cfDNA; tumor-WBC DNA pairs from 2 patients were uninformative due to a low number of SNVs detected in the tumor samples, precluding analysis of 10 plasma samples (from the two corresponding patients). Of the 113 evaluable plasma samples, 26 were collected at C1D1, 25 were collected at C2D1, 21 were collected at C3D1, 25 were collected pre-surgery, and 16 were collected post-surgery; 11 of the 16 post-operative samples were collected prior to any adjuvant treatment, while the remaining 5 were collected during or after adjuvant treatment. For two-timepoint ctDNA analyses, 21 patients had paired C1D1 and C3D1 samples and 23 patients had paired C1D1 and pre-surgery plasma samples. Created in BioRender. Jamali, A. (2025) https://BioRender.com/9s9ahv3. Abbreviations: ECOG, Eastern Cooperative Oncology Group; DPM, diffuse pleural mesothelioma; PFS, progression-free survival; OS, overall survival; WGS, whole-genome sequencing; cfDNA, cell-free DNA; ctDNA, circulating tumor DNA; WBC, white blood cell; SNV, single nucleotide variant; C1D1, cycle 1 day 1; C2D1, cycle 2 day 1; C3D1, cycle 3 day 1.
Extended Data Fig. 2 Schematic of the tumor-informed whole-genome sequencing molecular residual disease liquid biopsy approach.
WGS was performed on matched tumor- and WBC-derived DNA and plasma cfDNA at targets of 80x, 40x, and 30x total depth, respectively. A candidate set of somatic tumor-specific SNVs was generated from the intersection of tumor and WBC DNA WGS data and evaluated in plasma cfDNA WGS data. A random forest machine learning model was utilized to generate variant quality scores for candidate mutations found in cfDNA; ctDNA status was determined based on the aggregate level of signal across all detected candidate variants compared to a reference population of noncancerous donor plasma samples (n = 80). For samples with detectable ctDNA, tumor fraction was calculated based on aggregated variant allele frequencies. Created in BioRender. Lee, P. (2025) https://BioRender.com/hz2nk4g. Abbreviations: cfDNA, cell-free DNA; FFPE, formalin-fixed paraffin-embedded; WBC, white blood cell; WGS, whole-genome sequencing; SNV, single nucleotide variant; ctDNA, circulating tumor DNA.
Extended Data Fig. 3 Progression-free and overall survival estimates stratified by adjuvant immunotherapy.
(a) Patients who received adjuvant immunotherapy in Arm A (n = 8) had a trend toward longer PFS compared to patients who did not (n = 4), with a median PFS of 15.92 versus 5.92 months, respectively (log-rank test, p = 0.029; HR = 0.20, 95% CI: 0.038–0.99). (b) Patients who received adjuvant immunotherapy in Arm B (n = 6) had a trend toward longer PFS when compared to patients who did not (n = 5), with a median PFS of 21.88 versus 17.68 months, respectively (log-rank test, p = 0.01; HR not estimable). (c) Patients who received adjuvant immunotherapy in Arm A (n = 8) had no clear difference in OS compared to patients who did not (n = 4), with a median OS of 21.60 versus 12.85 months, respectively (log-rank test, p = 0.1; HR = 0.31, 95% CI: 0.067 – 1.39). (d) Patients who received adjuvant immunotherapy in Arm B (n = 6) had a trend toward longer OS when compared to patients who did not (n = 5), with a median OS of 28.85 versus 18.79 months, respectively (log-rank test, p = 0.01; HR not estimable). Survival intervals for these analyses were computed with surgery date as the landmark time. For the survival analyses where hazards ratios were not estimable, this was driven by the fact that all PFS and OS events occurred first in the subset of patients who did not receive adjuvant immunotherapy before any events occurred in those who received adjuvant immunotherapy. Abbreviations: PFS, progression-free survival; OS, overall survival; HR, hazard ratio.
Extended Data Fig. 4 ctDNA detection and kinetics by treatment arm.
ctDNA status and cfDNA TF were determined at C1D1, C2D1, C3D1, pre-surgery, and post-surgery timepoints. Samples with aggregate candidate variant scores exceeding a threshold of one standard deviation above the maximum variant score determined across 80 noncancerous reference samples were deemed to have detectable ctDNA; estimated cfDNA TFs were subsequently calculated for samples with detectable ctDNA. Reference variant scores are displayed for each patient (circles). ctDNA status (purple squares indicate detectable ctDNA and open squares denote undetectable ctDNA) and cfDNA TF values are shown across timepoints for 22 out of 28 evaluable patients (the 6 remainder evaluable patients are shown in Fig. 4). Patients who did not undergo surgery (n = 4) or had surgery aborted intraoperatively (n = 2) are shown in the top row (one additional patient is shown in Fig. 4 and is omitted from this figure to avoid duplication of visualizations); ctDNA kinetics for patients in Arm A are shown on the left, while ctDNA kinetics for patients in Arm B are shown on the right. Notably, ctDNA was consistently detectable in patients who either did not proceed to surgery or for whom surgery was aborted intraoperatively due to progression. Pre-surgery timepoint refers to the blood collection time three days before surgery (D-3) and post-surgery timepoint refers to the blood collection time prior to any adjuvant treatment. Abbreviations: cfDNA, cell-free DNA; ctDNA, circulating tumor DNA; TF, tumor fraction; C1D1, cycle 1 day 1; C2D1, cycle 2 day 1; C3D1, cycle 3 day 1.
Extended Data Fig. 5 Summary of ctDNA detection across all patients per timepoint and by treatment arm.
Number (a) and fraction (b) of patients with detectable ctDNA across all sampled timepoints in all patients and by treatment arm. Plasma samples were analyzed in 28 out of 30 patients; one patient from each treatment arm was excluded due to uninformative tumor-normal WGS analysis. At C1D1, 12 patients had detectable ctDNA (n = 8 out of 13 for Arm A; n = 4 out of 13 for Arm B), while 11 patients (n = 8 out of 14 for Arm A; n = 3 out of 11 for Arm B) had detectable ctDNA at C2D1, 7 patients (n = 3 out of 9 for Arm A; n = 4 out of 12 for Arm B) had detectable ctDNA at C3D1, 13 patients (n = 8 out of 14 for Arm A; n = 5 out of 11 for Arm B) had detectable ctDNA pre-surgery, and 2 patients (n = 1 out of 6 for Arm A; n = 1 out of 5 for Arm B) had detectable ctDNA post-surgery, prior to any adjuvant treatment. The fraction of patients with detectable ctDNA was numerically higher in Arm A compared to Arm B at C1D1 (61.54% versus 30.77%), at C2D1 (57.14% versus 27.27%), and at the pre-surgery (52.00% versus 45.45%) timepoints. The fraction of patients with detectable ctDNA were similar between arms at C3D1 (33.33%) and numerically lower in Arm A at the post-surgery timepoint (16.67% versus 20.00%). Abbreviations: ctDNA, circulating tumor DNA; C1D1, cycle 1 day 1; C2D1, cycle 2 day 1; C3D1, cycle 3 day 1; WGS, whole-genome sequencing.
Extended Data Fig. 6 Correlation between ctDNA status at serial timepoints during neoadjuvant ICB and feasibility of surgery.
(a) A significantly higher fraction of patients for whom surgery was not feasible (n = 5) had detectable ctDNA at C1D1 compared to patients who underwent surgery as planned (n = 21) (100% versus 33%, respectively; Fisher’s exact test, p = 0.012). (b) Patients for whom surgery was not feasible (n = 4) had significantly higher ctDNA detectable rates at C2D1 compared to patients who underwent surgery (n = 21; 100% versus 33%, respectively; Fisher’s exact test, p = 0.026). (c) Patients for whom surgery was not feasible (n = 5) had significantly higher ctDNA detectable rates at C3D1 compared to patients who underwent surgery (n = 16; 100% versus 12%, respectively; Fisher’s exact test, p = 0.001). (d) A similar trend based on ctDNA detection was noted at the pre-surgery timepoint amongst patients for whom surgery was not feasible (n = 4) compared to the patients who underwent surgery as planned (n = 21; 100% versus 43% ctDNA detectable respectively, Fisher’s exact test, p = 0.096). All p values were two-sided. Abbreviations: ctDNA, circulating tumor DNA; ICB, immune checkpoint blockade; C1D1, cycle 1 day 1; C2D1, cycle 2 day 1; C3D1, cycle 3 day 1.
Extended Data Fig. 7 Progression-free and overall survival analyses by ctDNA status at serial timepoints.
(a) There were no differences in PFS between patients with undetectable ctDNA at C1D1 (n = 14) compared to patients with detectable ctDNA (n = 12; median PFS of 17.25 versus 2.07 months; log-rank test, p = 0.36; HR = 0.65, 95% CI: 0.26 − 1.65). (b) Similarly, there were no differences in PFS between patients with undetectable ctDNA at C2D1 (n = 14) compared to patients with detectable ctDNA (n = 11; median PFS of 19.84 versus 2.46 months; log-rank test, p = 0.22; HR = 0.56, 95% CI: 0.22 − 1.42). (c) We noted numerically longer OS for patients with undetectable ctDNA at the pre-surgery timepoint (n = 12) compared to patients with detectable ctDNA, though these findings were not statistically significant (n = 13; median OS of 27.73 versus 15.47 months; log-rank test, p = 0.16; HR = 0.5, 95% CI: 0.18 − 1.36). (d) Longer OS was noted for patients in Arm A with undetectable ctDNA at the pre-surgery timepoint (n = 6) compared to patients in Arm A with detectable ctDNA (n = 8), though findings did not reach statistical significance (median OS of 27.30 versus 15.21 months; log-rank test, p = 0.065; HR = 0.33, 95% CI: 0.1 − 1.13). Abbreviations: ctDNA, circulating tumor DNA; TF, tumor fraction; PFS, progression-free survival; OS, overall survival; HR, hazard ratio.
Extended Data Fig. 8 ctDNA status and association with progression-free survival by timepoint and study arm.
(a) At C1D1, patients in Arm A with undetectable ctDNA (n = 5) had numerically longer PFS compared to patients with detectable ctDNA (n = 8), with a median PFS of 14.06 versus 2.07 months (log-rank test, p = 0.11; HR = 0.37, 95% CI: 0.1−1.32). (b) Patients in Arm B with undetectable ctDNA (n = 9) did not have significantly longer PFS compared to patients with detectable ctDNA at C1D1 (n = 4; log-rank test, p = 0.6; HR = 1.57, 95% CI: 0.29−8.55). (c) At C2D1, patients in Arm A with undetectable ctDNA (n = 6) had longer PFS compared to patients with detectable ctDNA (n = 8), with a median PFS of 22.49 versus 2.07 months (log-rank test, p = 0.00065; HR not estimable). (d) Patients in Arm B with undetectable ctDNA (n = 8) did not have longer PFS compared to patients with detectable ctDNA at C2D1 (n = 3; log-rank test, p = 0.22; HR = 3.66, 95% CI: 0.4 − 33.24). (e) At C3D1, patients in Arm A with undetectable ctDNA (n = 6) had longer PFS compared to patients with detectable ctDNA (n = 3), with a median PFS of 15.66 versus 2 months; log-rank test, p = 0.0018, HR not estimable. (f) Patients in Arm B with undetectable ctDNA (n = 8) did not have significantly longer PFS compared to patients with detectable ctDNA at C3D1 (n = 4; log-rank test, p = 0.3; HR = 0.46, 95% CI: 0.11 − 2.02). (g) At the pre-surgery timepoint, patients in Arm A with undetectable ctDNA (n = 6) had significantly longer PFS compared to patients with detectable ctDNA (n = 8), with a median PFS of 22.49 versus 2 months; log-rank test, p = 0.00029; HR not estimable. (h) Patients in Arm B with undetectable ctDNA (n = 6) did not have significantly longer PFS compared to patients with detectable ctDNA at the pre-surgery timepoint (n = 5; log-rank test, p = 0.32; HR = 0.47, 95% CI: 0.1 − 2.14). Abbreviations: ctDNA, circulating tumor DNA; PFS, progression-free survival; HR, hazard ratio; CI: confidence interval, C1D1, cycle 1 day 1; C2D1, cycle 2 day 1; C3D1, cycle 3 day 1.
Extended Data Fig. 9 Comparison of ctDNA status with mRECIST response.
(a) Per patient differential ctDNA detectable status (yellow circles indicate detectable ctDNA, blue circles denote undetectable ctDNA) and kinetics (blue connecting lines indicate ≥95% cfDNA TF reduction at pre-surgery or undetectable ctDNA across neoadjuvant timepoints, orange connecting lines indicate <95% cfDNA TF reduction pre-surgery, while gray denotes unevaluable cases. Patients are grouped based on radiographic imaging response by mRECIST. Patients with a radiographic partial response by mRECIST (n = 2) had undetectable ctDNA throughout their neoadjuvant treatment, while significant heterogeneity with respect to ctDNA status and kinetics was noted for patients with mRECIST stable disease (n = 11) or progressive disease (n = 11). (b) Waterfall plot showing quantitative comparison between mRECIST kinetics (estimated by the change in sum of longest diameters [SLD] from baseline to three days before surgery [D-3]) and ctDNA dynamics (as percentage cfDNA TF change from C1D1 to pre-surgery). Patients in Arm A are ordered on the left and patients in Arm B are ordered on the right. Changes in cfDNA TF did not mirror changes in mRECIST SLD. Abbreviations: PR, partial response; SD, stable disease; PD, progressive disease; RECIST, Response Evaluation Criteria in Solid Tumors; mRECIST, modified Response Evaluation Criteria in Solid Tumors; cfDNA, cell-free DNA; ctDNA, circulating tumor DNA; TF, tumor fraction; UD, undetectable; C1D1, cycle 1 day 1; C2D1, cycle 2 day 1; C3D1, cycle 3 day 1; SLD, sum of longest diameters.
Extended Data Fig. 10 Pre-surgery ctDNA dynamics and association with progression-free and overall survival.
(a) At the pre-surgery timepoint, patients who had ≥95% reduction in cfDNA TF or undetectable ctDNA throughout neoadjuvant treatment (n = 12) had numerically longer -though not statistically significant- OS compared to patients who had <95% reduction in cfDNA TF (n = 11), with a median OS of 27.73 versus 15.47 months (log-rank test, p = 0.065; HR = 0.39, 95% CI: 0.14−1.1). (b) Amongst the subset of patients who completed surgery, those who had ≥95% reduction in cfDNA TF or undetectable ctDNA throughout neoadjuvant treatment (n = 12) had significantly longer PFS compared to patients with <95% reduction in cfDNA TF (n = 5), with a median PFS of 23.26 versus 7.26 months (log-rank test, p = 0.0063; HR = 0.2, 95% CI: 0.05 − 0.71). (c) At the pre-surgery timepoint, patients in Arm A who underwent surgery and had ≥95% reduction in cfDNA TF or undetectable ctDNA throughout neoadjuvant treatment (n = 5) had significantly longer PFS compared to patients who had <95% reduction in cfDNA TF (n = 3), with a median PFS of 17.25 versus 7.26 months (log-rank test, p = 0.0042; HR not estimable). (d) At the pre-surgery timepoint, patients who underwent surgery and had ≥95% reduction in cfDNA TF or undetectable ctDNA throughout neoadjuvant treatment (n = 12) had significantly longer OS compared to patients who had <95% reduction in cfDNA TF (n = 5), with a median OS of 27.73 versus 14.95 months (log-rank test, p = 0.031; HR = 0.22, 95% CI: 0.05 − 0.99). (e) At the pre-surgery timepoint, patients in Arm A who underwent surgery and had ≥95% reduction in cfDNA TF or undetectable ctDNA throughout neoadjuvant treatment (n = 5) had numerically longer -though not statistically significant- OS compared to patients who had <95% reduction in cfDNA TF (n = 3), with a median OS of 26.87 versus 14.95 months (log-rank test, p = 0.12; HR = 0.26, 95% CI: 0.04 − 1.61). Abbreviations: pre-surg, pre-surgery; ctDNA, circulating tumor DNA; cfDNA, cell-free DNA; TF, tumor fraction; UD, undetectable; OS, overall survival; PFS, progression-free survival; HR, hazard ratio; CI, confidence interval.
Supplementary information
Supplementary Tables
Supplementary Table 1. Patient-level characteristics. Supplementary Table 2. Acute AEs* attributed to study drug. Supplementary Table 3. Acute AEs* regardless of attribution. Supplementary Table 4. AEs attributed to adjuvant nivo. Supplementary Table 5. Tumor-normal DNA WGS characteristics. Supplementary Table 6. cfDNA WGS characteristics. Supplementary Table 7. Patient-level ctDNA status per timepoint and longitudinal dynamics. Supplementary Table 8. Summary of protocol amendments.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Reuss, J.E., Lee, P.K., Mehran, R.J. et al. Perioperative nivolumab or nivolumab plus ipilimumab in resectable diffuse pleural mesothelioma: a phase 2 trial and ctDNA analyses. Nat Med 31, 4097–4108 (2025). https://doi.org/10.1038/s41591-025-03958-3
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41591-025-03958-3
This article is cited by
-
Liquid biopsies across the cancer care continuum
Nature Medicine (2025)