Abstract
An increasing number of centers not necessarily equipped with biplane (BP) angiosuites are performing mechanical thrombectomy (MT) in acute ischemic stroke patients. We assessed whether MT performed on single-plane (SP) is equivalent in terms of safety, effectiveness, radiation and contrast agent exposure. Consecutive patients treated by MT in four high volume centers between January 2014 and May 2017 were included. Demographic and MT characteristics were assessed and compared between SP and BP. Of 906 patients treated by MT, 576 (64%) were handled on a BP system. After multivariate analysis, contrast load and fluoroscopy duration were significantly lower in the BP group [100vs200mL, relative effect 0.85 (CI: 0.79–0.92), p = 0.0002; 22 vs 27 min, relative effect 0.84 (CI: 0.76–0.93), p = 0.0008, respectively]. There was no difference in recanalization (modified Thrombolysis-In-Cerebral-Infarction 2b-3), good clinical outcome (modified Rankin Scale 0–2), complications rates, procedure duration or radiation exposure. A three-vessel diagnostic angiogram performed prior to MT led to a significant increase in procedure duration (15% increase, p = 0.05), radiation exposure (33% increase, p < 0.0001) and contrast load (125% increase, p < 0.0001). Mechanical neuro-thrombectomy seems equally safe and effective on a single or biplane angiography system despite increased contrast load and fluoroscopy duration on the former.
Similar content being viewed by others
Introduction
Multiple randomized controlled trials have demonstrated the benefits of cerebrovascular mechanical thrombectomy (MT) in acute ischemic stroke patients with emergent large vessel occlusion (AIS-ELVO)1,2,3,4,5,6. Two further randomized trials evaluating late-onset strokes with favorable perfusion imaging7,8, have broadened its indications9,10. Adequate training is necessary for these procedures, which are often more complicated than may be anticipated11,12. Most neuro-interventionalists prefer working on biplane (BP) angiosuites since two simultaneous projections of the material and anatomical structures per contrast injection tends to reduce the risk of arterial perforation compared to single plane (SP) procedures12,13. Nonetheless, X-ray and contrast agent exposure remain a major public health concern in terms of carcinogenesis14,15,16,17, risk of renal failure18,19,20 or toxic reactions, respectively21,22.
Since an increasing number of centers are performing MT12 in the context of ELVO without necessarily being equipped with BP angiosuites, there is a need to understand whether MT performed on SP is equivalent in terms of safety, effectiveness, radiation and contrast agent exposure22.
Since evidence regarding safety and effectiveness of MT on SP and BP is contradictory18,23,24,25, we performed a multicentric analysis based on prospectively acquired data from four internationally accredited comprehensive stroke centers to establish which variables are associated with an increased radiation or contrast exposure during MT.
Results
Baseline characteristics
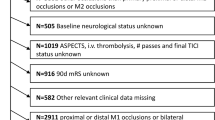
Of the 906 MT included, 330 (36%) and 576 (64%) were performed on SP and BP systems, respectively. Baseline characteristics did not differ significantly (see Table 1 for details) for clinical, imaging and interventional characteristics. For additional details, please check on-line supplemental material. Mean age was 69 ± 15 years (range: 18–100). Median National Institute of Health Stroke Scale (NIHSS) at admission was 17 (Interquartile range or IQR 12–21).
Procedure duration
All procedures were performed within 6 hours of stroke onset according to international recommendations26.
Time from stroke onset to groin puncture as well as procedure time (from initial groin puncture to last image in minutes) are described for all patients and did not differ significantly.
Statistical analysis
After multivariate analyses, there was no significant difference in rates of successful recanalization, periprocedural complication, nor for DAP or air kerma (Tables 1 and 2), whereas contrast load and fluoroscopy duration remained significantly lower on BP compared to SP interventions [100 vs 200 mL (50% decrease, relative effect 0.85,CI: 0.79–0.92, p = 0.0002) and 22 vs 27 min (19% decrease, relative effect 0.84, CI: 0.76–0.93, p = 0.0008), respectively].
There was no significant difference in rates of good clinical outcome (mRS 0–2) between BP and SP (40.1% versus 50%, p = 0.22 after multivariate analyses).
Factors associated with increased dose or contrast
Three variables were independently associated with an increased DAP, kerma and contrast load, namely cervical dissection as ELVO etiology (207 Gy.cm² vs 148 for other stroke etiology p < 0.0001), tandem occlusion (239 Gy.cm² vs 148 for other occlusion types p < 0.0001) or the need for stenting and/or angioplasty (271 Gy.cm² vs 137 without angioplasty or stenting, p < 0.0001). Use of a stent-retriever and general anesthesia were associated with increased radiation dose in univariate but not in multivariate analyses.
After adjustment for potential confounders, a three or four vessel diagnostic cerebral angiogram before MT significantly increased radiation dose: DAP 161 Gy.cm² vs 122 without diagnostic angiograms (33% increase, p < 0.0001). The same effect was observed for contrast load and procedure duration: 180 vs 80 mL (125% increase, p < 0.0001) and 46 vs 40 minutes (15% increase, p = 0.05), respectively, without affecting the rates of successful recanalization, periprocedural complication or good clinical outcome.
Discussion
According to our multicentric data, MT performed on BP does not improve efficacy or safety compared to SP interventions, despite the added subjective sense of comfort acknowledged by the majority of operators (which was not specifically measured).
Overall, biplane use significantly reduced contrast load (50% decrease, p < 0.0001) and fluoroscopy duration (19% decrease, p = 0.0056). DAP and kerma, however, were not affected after adjusting for potential confounders, contrary to the effect of radiation reduction dose-systems as showed in the literature27.
Likewise, rates of successful recanalization, periprocedural complications, good functional outcome and total procedure duration did not differ between BP and SP interventions. As expected, more complex and time-consuming interventions, such as those associated with cervical dissection, tandem occlusions28, stenting and/or angioplasty were associated with increased contrast load and radiation doses. Use of stent-retriever, contact aspiration29, general anesthesia or conscious sedation30 were associated with similar rates of safety and effectiveness. Despite increased radiation exposure with stent-retrievers use or general anesthesia in univariate analyses, this was no longer significant after multivariate analysis.
Our results contradict a recent literature review suggesting reduced radiation, contrast load, risk of complications and procedure duration with biplane angiosuites13. As recognized by the authors of the latter, however, the level of evidence was low. Moreover, MT was not the sole intervention studied, as opposed to the data present. It is noteworthy that neurointerventional procedures31, when compared to coronary angioplasty18 and angiography32, may be associated with a lower DAP on BP systems.
Based on the higher acquisition and maintenance costs of BP systems and the absence of an obvious clinical benefit for MT13, there is currently no evidence to recommend performing such procedures exclusively on BP or to withhold MT from SP systems. One could even argue that the latter appears to be more cost-effective and that the number of treatment sites capable of offering MT could be expanded if BP is not mandatory. One should emphasize, however, that our data was acquired only in high-volume academic centers with expertly trained operators, meaning our results do not necessarily apply to other clinical settings33.
Although some physicians believe that a three or four vessel diagnostic cerebral angiogram, including both internal carotid arteries and at least the dominant vertebral artery, is essential before performing MT, mainly to assess all collateral flow routes34, our results indicate that this may be more harmful by increasing contrast load, procedure duration and radiation exposure unnecessarily. Although the additional diagnostic runs do not negatively influence clinical outcome, collateral flow is nowadays sufficiently well assessed on admission computed-tomography or magnetic-resonance-imaging, especially when advanced imaging such as multiphase computed-tomography angiogram or perfusion studies are performed35. Moreover, additional diagnostic runs are unlikely to modify the therapeutic approach in the vast majority of situations, since thrombectomy will be attempted as long as an ELVO is still present. Lastly, the cumulative radiation dose from DSA, computed-tomography, computed-tomography perfusion and angiography prior to MT should be minimized as much as possible.
Our study is the first to compare SP and BP with such a high number of patients, international centers and focusing on a large variety of both technical and clinical outcomes. Our approach let us describe a game-changing result in the assessment of collateral flow, showing that invasive assessment of a four vessel diagnostic cerebral angiogram before a MT procedure could be more harmful for patients than useful.
We do believe the SP versus BP comparison is a major issue when more and more centers tend to treat patients for MT. Whether facilities without biplane systems are able to perform MT whether the installation of a biplane system is required are major organizational issues.
Lastly, on the contrary to a recent similar analysis36, our results emphasized the importance of both AP and lateral views in interventional neuroradiology, showing a complete different technical approach than Friedrich&al. Their results showed a similar contrast load with twice the radiation dose for biplane angiosuites, implying they performed the same number of runs on SP and BP: the second view was not useful for them. In these circumstances, rates of complication and successful recanalisations they describe may be difficult to grasp and interpret knowing the low level of evidence of a study with less than 200 patients.
Limitations
There were several limitations due to the retrospective nature of our study. Exposure related to flat panel computed tomography following MT completion (mainly to evaluate vessel perforation in selected cases) may have unduly increased the mean DAP. Given the low total number of complications, however, this appears to be insignificant. Secondly, the cumulative dose of patients screened with CT at admission was not incorporated in our analyses, although the proportion screened with this modality in the BP and SP population were similar. Thirdly, while individual skills, experience, speed and radioprotection knowledge may differ from one center to the next or within a given institution and influence the results, it is unlikely to have played a significant role considering the similar experience, fellow involvement and interventional protocols in the four participating comprehensive stroke centers. Fourthly, estimation of reperfusion success, self-assessed by non-core-lab adjudicated mTICI evaluations, may have incorporated suboptimal single-plane evaluations with possible missing antero-posterior or lateral views before and after recanalization. Fifthly, the SP and BP arms were unbalanced and not primarily randomized to study their performance for MT, our results may then be limited, randomized trials would be necessary to assess this matter. A relatively high number of patients between 2015 and 2017 were treated on upgraded angiosuites equipped with dose reduction technologies, they were not included in the present study to avoid bias in radiation doses analyses, the impact of dose reduction technology was not evaluated. The scale to report the amount of contrast agent administered was not specifically described for each center however, inclusion of centers in the multivariate analysis may have limited bias. Lastly, number of attempts and number of devices used for MT were not reported in our study.
Conclusion
Mechanical neuro-thrombectomy seems equally safe and effective on a single or biplane angiography system, despite increased contrast load and fluoroscopy duration on the former, especially if a three or four vessel pre-interventional diagnostic angiogram is performed.
Materials and Methods
The study protocol was approved by the institutional review board of each of the four certified comprehensive stroke centers in France, Switzerland and the United States of America (See Supplemental material). Patient informed consent was waived for this retrospective analysis of pooled anonymized prospectively acquired data. Adherence to the STROBE criteria37 and compliance with the Health Insurance Portability and Accountability Act were enforced.
Population
All consecutive patients who underwent MT for AIS-ELVO confirmed by magnetic-resonance-imaging or computed-tomography38,39 between January 2014 and May 2017 on a biplane (BP) or single-plane (SP) angiosuite were included.
Functional outcome using the modified Rankin Scale (mRS)40 was assessed at 90 days by a certified stroke neurologist.
Over the 3-year study period, fellow involvement ranged from assistance to supervised or fully independent MT but was not recorded.
Dose metrics
Variables assessed were Kerma (Gy), dose-area product (DAP) (Gy.cm²) and total fluoroscopy time (minutes).
Imaging system parameters
The technical parameters of each angiosuite (see Supplement Tables 1 and 2) were reported and verified by two radio-physicists (F.C. and S.M.). A 27 or 32 cm field-of-view was used for the vast majority of treatments. DAP, kerma and fluoroscopy duration were extracted from the dose reports of the picture archiving systems by one of the local interventional neuro-radiologist or medical physicist. Angiosuites were regularly calibrated and controlled according to national and international standards.
Statistics/data analysis
The primary outcome was the rate of good functional outcome at 90 days (defined as a mRS of 0 to 2) dichotomized into SP and BP interventions.
Secondary outcome measures were rates of successful recanalization (defined as modified Thrombolysis In Cerebral Infarction score [mTICI] 2b or 3), complications (periprocedural perforation, hemorrhage, and iatrogenic thromboembolic events), procedure and fluoroscopy time (from initial groin puncture to last image), total radiation dose (air kerma and DAP) and contrast agent volume injected in SP versus BP then depending on the angiosuite brand. Furthermore, we assessed which variables were associated with an increased radiation or contrast load during MT.
Since MT focuses on the head and neck region, we assumed there was no need to correct for automated weight-adapted variation of radiation dose, as occasionally described41,42,43. Nonetheless, the absence of interaction with all variables was statistically tested.
A descriptive analysis was first performed. Categorical variables were summarized using frequency, individual and cumulative percentages. Continuous variables were expressed by mean, standard deviation, quartiles and interquartile range. Shapiro-Wilk tests served to test the normality of the continuous variables. The eight variables of interest (mTICI, mRS at 3 months, periprocedural complication rate, scopy duration, procedure duration, DAP, kerma and contrast load) were compared and dichotomized according to angiosuite type (SP or BP) using the Mann-Whitney or Fisher test for continuous or categorical variables, respectively. Then, to eliminate the effect of potential confounders, eight different models were tested. For continuous variables, a linear regression with logarithmically transformed variables was finally used after having checked that residual plots did not deviate from normality. For binary variables, we used a logistic regression. Potential confounders were determined based on a previous literature review. To retain only the most significant, a univariate analysis with the Mann-Whitney tests for quantitative variables and a Fisher exact test for qualitative variables was performed. Only variables showing a statistically significant difference were finally selected as potential confounders in the multivariate models. Multiple regression was used to adjust for age, number of pre-interventional angiograms, anesthesia type (conscious sedation or general anesthesia), MT technique (stent-retriever, contact aspiration, combination thereof), center, etiology and date of the intervention. Bonferroni correction was used to minimize inflation of type I error for the eight independent models used. We used the R Statistical Software (version 3.4.2, Foundation for Statistical Computing, Vienna, Austria) for all statistical analyses.
Statistical analysis
Kevin ZUBER (MSc) conducted all the statistical analyses.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Berkhemer, O. A. et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N. Engl. J. Med. 372, 11–20, https://doi.org/10.1056/NEJMoa1411587 (2015).
Campbell, B. C. et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N. Engl. J. Med. 372, 1009–1018, https://doi.org/10.1056/NEJMoa1414792 (2015).
Jovin, T. G. et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N. Engl. J. Med. 372, 2296–2306, https://doi.org/10.1056/NEJMoa1503780 (2015).
Saver, J. L. et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N. Engl. J. Med. 372, 2285–2295, https://doi.org/10.1056/NEJMoa1415061 (2015).
Bracard, S. et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet. Neurol. 15, 1138–1147, https://doi.org/10.1016/S1474-4422(16)30177-6 (2016).
Goyal, M. et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387, 1723–1731, https://doi.org/10.1016/S0140-6736(16)00163-X (2016).
Albers, G. W. et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N. Engl. J. Med. 378, 708–718, https://doi.org/10.1056/NEJMoa1713973 (2018).
Nogueira, R. G. et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N. Engl. J. Med. 378, 11–21, https://doi.org/10.1056/NEJMoa1706442 (2018).
Hopkins, L. N. & Holmes, D. R. Jr. Public Health Urgency Created by the Success of Mechanical Thrombectomy Studies in Stroke. Circulation 135, 1188–1190, https://doi.org/10.1161/CIRCULATIONAHA.116.025652 (2017).
Society of NeuroInterventional, S., American Association of Neurological, S., Congress of Neurological, S., Society of, V. & Interventional, N. Letter by the Society of NeuroInterventional Surgery, the Cerebrovascular Section of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons, and the Society of Vascular and Interventional Neurology Regarding Article, “Public Health Urgency Created by the Success of Mechanical Thrombectomy Studies in Stroke”. Circulation 136, 779–780, https://doi.org/10.1161/CIRCULATIONAHA.117.028820 (2017).
Lavine, S. D. et al. Training Guidelines for Endovascular Ischemic Stroke Intervention: An International Multi-Society Consensus Document. AJNR Am. J. Neuroradiol. 37, E31–34, https://doi.org/10.3174/ajnr.A4766 (2016).
Hornung, M. et al. TCT-211 Technical Success of Acute Stroke Interventions Performed by Cardiologists – Single Center Experience. J. Am. Coll. Cardiology 72, B89, https://doi.org/10.1016/j.jacc.2018.08.1332 (2018).
Bellemare, C. A. & Poder, T. G. Effectiveness of biplane angiography compared to monoplane angiography for vascular neuro-interventions: a systematic review of the literature. Clin. radiology 72, 612.e611–612.e615, https://doi.org/10.1016/j.crad.2017.02.020 (2017).
Brenner, D. J. & Hall, E. J. Computed tomography–an increasing source of radiation exposure. N. Engl. J. Med. 357, 2277–2284, https://doi.org/10.1056/NEJMra072149 (2007).
The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann. ICRP 37, 1–332, https://doi.org/10.1016/j.icrp.2007.10.003 (2007).
Fetterly, K. et al. Head and Neck Radiation Dose and Radiation Safety for Interventional Physicians. JACC Cardiovasc. Interv. 10, 520–528, https://doi.org/10.1016/j.jcin.2016.11.026 (2017).
Salaun, E. et al. High Radiation Exposure of the Imaging Specialist During Structural Heart Interventions With Echocardiographic Guidance. JACC Cardiovasc. Interv. 10, 626–627, https://doi.org/10.1016/j.jcin.2017.01.016 (2017).
Sadick, V. et al. Impact of biplane versus single-plane imaging on radiation dose, contrast load and procedural time in coronary angioplasty. Br. J. Radiol. 83, 379–394, https://doi.org/10.1259/bjr/21696839 (2010).
Freeman, R. V. et al. Nephropathy requiring dialysis after percutaneous coronary intervention and the critical role of an adjusted contrast dose. Am. J. cardiology 90, 1068–1073 (2002).
Kane, G. C. et al. Ultra-low contrast volumes reduce rates of contrast-induced nephropathy in patients with chronic kidney disease undergoing coronary angiography. J. Am. Coll. Cardiology 51, 89–90, https://doi.org/10.1016/j.jacc.2007.09.019 (2008).
Marycz, D. & Ziada, K. M. Nonrenal Complications of Contrast Media. Interv. Cardiol. Clin. 3, 341–348, https://doi.org/10.1016/j.iccl.2014.03.004 (2014).
Weisbord, S. D. et al. Outcomes after Angiography with Sodium Bicarbonate and Acetylcysteine. The New England journal of medicine, https://doi.org/10.1056/NEJMoa1710933 (2017).
Bashore, T. M. et al. American College of Cardiology/Society for Cardiac Angiography and Interventions Clinical Expert Consensus Document on cardiac catheterization laboratory standards. A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J. Am. Coll. Cardiology 37, 2170–2214 (2001).
Pantos, I., Patatoukas, G., Katritsis, D. & Efstathopoulos, E. Patient Radiation Doses in Interventional Cardiology Procedures. Curr. Cardiology Rev. 5, 1–11, https://doi.org/10.2174/157340309787048059 (2009).
Friedrich, B. et al. Endovascular Stroke Treatment on Single-Plane vs. Bi-Plane Angiography Suites: Technical Considerations and Evaluation of Treatment Success. Clin. Neuroradiol, https://doi.org/10.1007/s00062-017-0655-z (2018).
Powers, W. J. et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, https://doi.org/10.1161/STR.0000000000000158 (2018).
Guenego, A. et al. Proposed achievable levels of dose and impact of dose-reduction systems for thrombectomy in acute ischemic stroke: an international, multicentric, retrospective study in 1096 patients. Eur. Radiol, https://doi.org/10.1007/s00330-019-06062-6 (2019).
Papanagiotou, P. et al. Carotid Stenting With Antithrombotic Agents and Intracranial Thrombectomy Leads to the Highest Recanalization Rate in Patients With Acute Stroke With Tandem Lesions. JACC Cardiovasc. Interv. 11, 1290–1299, https://doi.org/10.1016/j.jcin.2018.05.036 (2018).
Lapergue, B. et al. Effect of Endovascular Contact Aspiration vs Stent Retriever on Revascularization in Patients With Acute Ischemic Stroke and Large Vessel Occlusion: The ASTER Randomized Clinical Trial. JAMA 318, 443–452, https://doi.org/10.1001/jama.2017.9644 (2017).
Schonenberger, S. et al. Effect of Conscious Sedation vs General Anesthesia on Early Neurological Improvement Among Patients With Ischemic Stroke Undergoing Endovascular Thrombectomy: A Randomized Clinical Trial. JAMA 316, 1986–1996, https://doi.org/10.1001/jama.2016.16623 (2016).
Johnson, C. S. J., Kyrion, J. & Taylor, W. J. Comparing the performance of mono- and biplane fluoroscopy systems in diagnostic and interventional neuroangiography using the dose-area product. Neuroradiology 43, 728–734 (2001).
Lin, A. et al. Optimisation of coronary angiography exposures requires a multifactorial approach and careful procedural definition. Br. J. Radiol. 86, 20120028, https://doi.org/10.1259/bjr.20120028 (2013).
Saber, H. et al. Real-World Treatment Trends in Endovascular Stroke Therapy. Stroke 50, 683–689, https://doi.org/10.1161/STROKEAHA.118.023967 (2019).
Higashida, R. T. et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 34, e109–137, https://doi.org/10.1161/01.STR.0000082721.62796.09 (2003).
Guenego, A. et al. Hypoperfusion ratio predicts infarct growth during transfer for thrombectomy. Ann. Neurol. 84, 616–620, https://doi.org/10.1002/ana.25320 (2018).
Friedrich, B. et al. Endovascular Stroke Treatment on Single-Plane vs. Bi-Plane Angiography Suites: Technical Considerations and Evaluation of Treatment Success. Clin. Neuroradiol. 29, 303–309, https://doi.org/10.1007/s00062-017-0655-z (2019).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370, 1453–1457, https://doi.org/10.1016/S0140-6736(07)61602-X (2007).
Powers, W. J. et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment. Stroke 46, 3020–3035, https://doi.org/10.1161/STR.0000000000000074 (2015).
Fiehler, J. et al. European Recommendations on Organisation of Interventional Care in Acute Stroke (EROICAS). Int. J. Stroke 11, 701–716, https://doi.org/10.1177/1747493016647735 (2016).
van Swieten, J. C., Koudstaal, P. J., Visser, M. C., Schouten, H. J. & van Gijn, J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19, 604–607 (1988).
Chapple, C. L., Broadhead, D. A. & Faulkner, K. A phantom based method for deriving typical patient doses from measurements of dose-area product on populations of patients. Br. J. Radiol. 68, 1083–1086, https://doi.org/10.1259/0007-1285-68-814-1083 (1995).
Miller, D. L. et al. Radiation doses in interventional radiology procedures: the RAD-IR study: part I: overall measures of dose. J. Vasc. Interv. Radiol. 14, 711–727 (2003).
Miyake, H. et al. Medical electrical equipment - part 2-43: particular requirements for the basic safety and essential performance of X-ray equipment for interventional procedures. Nihon Hoshasen Gijutsu Gakkai Zasshi 67, 298–301 (2011).
Acknowledgements
I, A.G., certify that: (1) persons who have made substantial contributions to the research and/or manuscript, but who do not fulfill authorship criteria, are named with their specific contributions, (2) all persons named in the Acknowledgments section have provided the corresponding author with permission to be named in the manuscript. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. There are no relationships with industry.
Author information
Authors and Affiliations
Author notes
A comprehensive list of consortium members appears at the end of the paper.
Consortia
Contributions
A.G., P.J.M., M.W., J.J.H., K.Z., T.D., J.A.L., P.N., D.G.M., J.M.O., N.G.N., R.B., V.M.P., J.G., J.K., R.F., M.P., C.C. as well as RADON investigators (E.P., P.M., F.Z., C.D., F.B., J.D., I.V., A.C.J., S.M., C.M., P.T., M.M., J.P.D., G.C., S.S., H.R., B.M., B.W.M., E.G., F.C.) made substantial contributions to the conception or design of the work, approved the submitted version and agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. A.G., P.J.M., made substantial contributions to the conception and design of the work; and the acquisition, analysis, and interpretation of data; and drafted the work and substantively revised it. M.W., J.J.H., K.Z., T.D., J.A.L., P.N., D.G.M., J.M.O., N.G.N., R.B., V.M.P., J.G., J.K., R.F., M.P., C.C., RADON investigators (E.P., P.M., F.Z., C.D., F.B., J.D., I.V., A.C.J., S.M., C.M., P.T., M.M., J.P.D., G.C., S.S., H.R., B.M., B.W.M., E.G., F.C.) made substantial contributions to the acquisition of data; and drafted the work and substantively revised it.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guenego, A., Mosimann, P.J., Wintermark, M. et al. Safety and Effectiveness of Neuro-thrombectomy on Single compared to Biplane Angiography Systems. Sci Rep 10, 4470 (2020). https://doi.org/10.1038/s41598-020-60851-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-020-60851-4
This article is cited by
-
Mechanical Thrombectomy for Middle Cerebral Artery Medium Vessel Occlusions Using Single Plane Angiography
Clinical Neuroradiology (2025)
-
Occlusion Type, Number of Recanalization Passages and Dose Program Determine Radiation Dose in Endovascular Stroke Thrombectomy
Clinical Neuroradiology (2022)
-
Radiation exposure in endovascular stroke treatment of acute basilar artery occlusions—a matched-pair analysis
Neuroradiology (2020)