Abstract
In endoscopic biliary drainage (EBD) for various benign and malignant biliary disorders, the appropriate timing to replace or change a plastic stent (PS) with a self-expandable metallic stent (SEMS) remains unclear. This study aimed to define the best period to replace or change a PS with a SEMS. Between January 1, 2012, and December 31, 2018, 1,887 consecutive EBD procedures, including 170 SEMS placements, were retrospectively identified. The period to recurrent biliary obstruction (PRBO) was estimated and compared between the malignant and benign groups and according to each disease using time to event analysis and competing risk analysis. Compared with the benign group, the malignant group had significantly shorter median PRBO with interquartile range (IQR) after PS placement [108 (39 – 270) vs. 613 (191 – 1,329) days, P < 0.001], even on multivariate analysis, with a subdistribution hazard ratio (SHR) of 3.58 (P < 0.001). The shortest PRBO distribution from the first quartile of the non-RBO period was seen in Mirizzi syndrome cases (25 days, P = 0.030, SHR = 3.32) in the benign group and in cases of pancreatic cancer (32 days, P = 0.041, SHR = 2.06); perihilar bile duct cancer (27 days, P = 0.006, SHR = 2.69); and ampullary cancer (22 days, P = 0.001, SHR = 3.78) in the malignant group. Our study supports that stent replacement for the benign group is feasible after 6 months, and the best period to replace or change a PS with a SEMS should be decided on the basis of the underlying disease to prevent RBO.
Similar content being viewed by others
Introduction
Endoscopic biliary drainage (EBD) procedures are indispensable options in patients with acute cholangitis or an obstructive jaundice in both benign and malignant diseases1,2,3,4. In benign biliary disorders, temporary placement of a plastic stent (PS) has been useful for bile duct stones5,6, postoperative biliary leaks5,7, and benign biliary strictures with multiple PS placement1,8. In malignant biliary disorders, particularly in extrahepatic biliary strictures and inoperable perihilar strictures, self-expandable metallic stent (SEMS) has the advantage of a longer patency period, compared with PS9,10,11,12,13. However, PS is usually used in many cases because of the usability from the cost effectiveness or technical aspect1,3,14,15,16,17,18,19. Conversely, the development of recurrent biliary obstruction (RBO) after PS placement for malignant diseases could prevent chemotherapy or surgical therapy or worsen the patients’ quality of life or induce life-threatening complications associated with acute cholangitis1,14,20,21,22.
Up to the present time, the recommended period for PS replacement in malignant cases has been 3−6 months, based on studies that evaluated and compared the period to RBO (PRBO) between PS and SEMS13,16. Despite this recommendation, the actual period to recurrent biliary obstruction (PRBO) frequently seemed to be shorter in daily medical practice23. Likewise, the appropriate interval for PS replacement in benign diseases had been unclear. Because few studies on PS have reported details on the suitable interval or timing of replacement or change to SEMS according to the risk factors for RBO in each biliary disorder, the actual PRBO is not known in the field1,9. Therefore, the primary aim of this study was to define the best period to replace or change a PS with a SEMS in each disease, after resolving the risk factors for RBO.
Materials and methods
Study design
The present retrospective cohort study investigated PRBO after PS and SEMS placement. This study complied with “the TOKYO criteria 2014” for a time to event analysis with “the International consensus statements for endoscopic management of distal biliary stricture” and with the other guidelines on survival analyses1,22,24,25.
Patients
Consecutive patients with suspected hepatobiliary–pancreatic disorders who underwent EBD attempts between January 1, 2012 and December 31, 2018 were retrospectively included in this study.
Regarding eligibility, the population of stent placement included consecutive patients after PS placement. In preoperative stent placement, patients who received neoadjuvant chemotherapy were excluded from the accountment of the time to surgery. We excluded the cases of failure of endoscopic biliary stenting, endoscopic nasobiliary drainage, and indetermination of diagnosis (Fig. 1). The cases of duodenal stricture were also all excluded.
Data on endoscopic retrograde cholangiopancreatography (ERCP) procedures were retrieved from the Jikei University ERCP database, which was updated immediately after each procedure and contained data on > 6 months of follow up. All patients provided written informed consent to undergo EBD; they were aware of the opportunity to opt out of study participation (opt-out method of informed consent) because this study was an observational research. This study was approved by the Human Subjects Committee of Jikei University School of Medicine [ID no. 31-099 (9598)] and was subsequently registered with the University Hospital Medical Information Network Clinical Trials Registry (identification no. UMIN000037640). This study was conducted in accordance with the ethical principles of the Declaration of Helsinki (Fortaleza revision).
Stent placement
PS used was of the 7-, 8.5-, or 10-Fr straight tube type (Flexima/Advanix J; Boston Scientific, USA and Japan or Quick Place V; Olympus Medical Systems, Tokyo, Japan). The length (5–15 cm) was chosen by the stricture location from the papilla. In some cases, a 7-Fr (5–12 cm) inside stent (CATHEX; Gadelius Medical, Tokyo, Japan or Advanix J; Boston Scientific) was needed.
In bile duct stone cases, PS without stone extraction was usually installed at first ERCP session in this study because patients with bile duct stone usually had on going acute cholangitis and/or obstructive jaundice. After the cholangitis or jaundice was cured, stent removal and stone extraction were performed at second ERCP session, which was considered right censoring22. Preoperative placement of PS was also included, and after surgeries, such as cholecystectomy, stent removal and stone extraction were performed at second ERCP session. The other cases included patients with severe complications who had difficulty undergoing cholecystectomy and stone extraction using EST and/or EPBD. In such situations, plastic stents were installed alone, and when RBO occurred, we exchanged the plastic stents.
If a spontaneous passage of bile duct stones was identified during ERCP, the patients with cholelithiasis underwent biliary stent placement to prevent the possible recurrence of choledocholithiasis owing to the gallstone passing through the common bile duct before cholecystectomy. As for reason, some patients with cholelithiasis underwent biliary stent placement.
When endoscopic drainage was required in Bismuth types II–IV strictures, the drainage of ≥ 50% of the liver volume was attempted5. If the bilateral drainage was difficult, unilateral drainage was attempted, prioritizing the bigger portion of liver volume.
ERCP procedures
ERCP was performed under fluoroscopic view by experts who have performed > 200 ERCPs per year or by trainees with experts’ interference, depending on the situation. All patients who underwent ERCP were conscious but sedated with intravenous midazolam and pethidine administration during the ERCP procedure.
In almost all cases of stone extraction, endoscopic sphincterotomy (EST) with medium incision was performed. After stent placement in patients with bile duct stone, we did not prescribe ursodeoxycholic acid. In all cases of multiple PS placement, EST with small incision was performed. When medium incision of EST could not be performed owing to periampullary diverticulum or intradiverticular papilla, small incision of EST and balloon sphincteroplasty were performed. All procedures of stone extraction were conducted by the stone lithotripsy method. In cases of bile duct strictures, brush cytology and/or intraductal biopsies, in some cases using a spyglass, were performed during ERCP to exclude malignancy.
Definitions of follow up and RBO factors
Based on “the TOKYO criteria 2014”, the recurrent biliary obstruction (RBO) was defined as a composite endpoint of either symptomatic occlusion or symptomatic migration, and the PRBO was defined as the time from SEMS/PS placement to the RBO22. The consecutive patients were followed up until June 30, 2019 by right censoring25. Patients were censored if they were lost to follow up without RBO, had asymptomatic migration on the day of routine replacement (i.e., non-cholangitis and/or non-jaundice), or when the stent was extracted during operation22. In this study, the independent variables of RBO risk factors were defined as age, sex, body mass index, antithrombotic agents, serum total bilirubin, grade of acute cholangitis, periampullary diverticulum, intradiverticular papilla, SEMS, the diameter and type of PS, total number of stentings, location and length of the biliary stricture, types of major papilla, altered gastrointestinal anatomy, and malignant and benign group. Time to surgery was defined as the duration from the initial day of ERCP to the day of the surgery. The diagnostic criteria and severity grading of acute cholangitis were based on the TOKYO Guidelines 201820. The other definitions for PRBO, functional success, and severity grading of adverse events were based on the TOKYO criteria 2014 and International consensus statements for endoscopic management of distal biliary stricture1,22. Mirizzi syndrome was diagnosed by surgery, or when surgical resection was not indicated, ERCP and magnetic resonance cholangiopancreatography (MRCP) were used26. Bile duct stone clearance was verified by MRCP and blood test with no symptoms after stone extraction.
Endpoints
The primary endpoint of the present study was PRBO in each disease. The secondary endpoints were (1) comparison of the RBO factors between the benign and malignant groups; (2) resolution of the risk factors for RBO in the benign and malignant groups; and (3) evaluation of the risk factors in each disease.
Statistical analysis
PRBO was estimated using the Kaplan–Meier analysis and compared between the benign and malignant groups using the log-rank test. The event of patient death was treated as a censor. In the multivariate analysis, to avoid imbalances when there were seven or fewer events (= RBOs) per confounder, the number of dependent variables was adopted within the number of dependent variables / 7 items27. In the analysis, Fine and Gray model, which is based on a subdistribution hazard model (SHR)28, was used for competing risk regression analysis. To include death in the informative censoring for potential RBO in this model, death without RBO was treated as a competing risk. In this situation, Gray test was used for comparison of PRBO between the benign and malignant groups or within a group. After the initial multivariate analysis, the significant variables were adopted into the next multivariate analyses in each disease.
When appropriate, data were presented as mean (standard deviation: SD) or frequencies. The benign and malignant groups were compared using the Chi-square test or Fisher’s exact test for the proportions of categorical variables (e.g., technical success rates) and the Mann–Whitney U-test for the mean values of the continuous variables (e.g., time to 50% decrease or normalization of the bilirubin level). Missing values were excluded for complete case analysis. Two-sided P < 0.05 was considered significant. All analyses were performed using Stata version 15 (StataCorp LP; College Station, TX, USA).
Results
Patients
In the setting of a retrospective continuous series, 1,887 eligible patients who underwent EBD procedures using PSs or SEMSs were enrolled in the present study (Fig. 1 and Table 1). No significant differences in age and sex were noted between the benign and malignant groups. However, the proportion of cases with acute cholangitis at the initial EBD was significantly higher in the malignant group than in the benign group (54.7% vs. 48.8%, P = 0.04). In the malignant group, the mean time to surgery was 29.0 days (Table 1). PS placement after balloon sphincteroplasty only, large incision of EST, and multiple placement of PS without EST (small incision) were unintentionally not included in this series.
Comparison of the outcomes between the benign and malignant groups
The malignant group had significantly lower median PRBO with 95% CI [108 (79–138) days vs. 613 (367–not applicable) days, P < 0.001; Fig. 2A and Table 2]; significantly lower technical success rate of stent insertion (91.7% vs. 96.2%, P < 0.001; Table 2); and significantly lower functional success rate of PS insertion (80.2% vs. 94.5%, P < 0.001; Table 2) the benign group, even in cases of altered gastrointestinal anatomy (61.4% vs. 80.0%, P < 0.001; Table 2). The time to 50% decrease or normalization of the bilirubin level with PS placement was significantly longer in the malignant group than in the benign group [4.4 (3.4) days vs. 3.3 (2.2) days, P = 0.001; Table 2]. The malignant group had lower nonobstruction rates than the benign group after PS placement at 3 months (65.8% vs. 88.7%, P = 0.008); 6 months (44.5% vs. 79.1%, P = 0.005); and 12 months (25.7% vs. 63.0%, P < 0.001) (Table 2). With regard to the adverse events after PS placement, compared with the benign group, the malignant group had higher rates for early (< 30 days) causes of RBO (12.4% vs. 3.9%, P < 0.001); late (≥ 31 days) causes of RBO (18.1% vs. 7.6%, P < 0.001); sludge formation (17.8% vs. 7.9%, P < 0.001); proximal symptomatic migration (0.6% vs. 0%, P = 0.017); and hemobilia (1.7% vs. 0.1%, P < 0.001) (Table 2). In addition, some cases in the benign group that underwent PS placement showed luminal obstruction by sludge without acute cholangitis (Supplementary Fig. S1 online). In contrast, the rate of distal symptomatic migration was higher in the benign group than in the malignant group (3.4% vs. 1.7%, P = 0.02) (Table 2). In the benign group, distal symptomatic migration was significantly higher in 7-Fr PS than in 8.5-Fr and 10-Fr PS (P = 0.001; Supplementary Table S1 online), and there was no significant change in distal symptomatic migration in the malignant group (P = 0.110; Supplementary Table S1 online). No statistically significant differences were noted between the benign and malignant groups with respect to adverse events, other than RBO, and there were no cases of nonobstructive cholangitis and bleeding after stent insertion (Table 2).
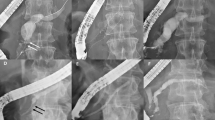
Comparison of the benign and malignant groups in terms of nonobstruction and recurrent biliary obstruction (RBO) rates using Univariate Kaplan–Meier analysis (A) and Multivariate Competing-risks model (B). (A) In the Kaplan–Meier analysis for nonobstruction rates, patients who died were censored, and those in whom self-expandable metallic stents (SEMS) were placed were excluded. (B) In the competing risk model for RBO rates, mortality was assigned as the competing risk, and the other independent factors (Table 3) were assigned as covariates. Cases in which SEMSs were placed were included.
Risk factors for RBO using multivariate competing risk regression analysis
In the multivariate competing risk regression analysis, a significantly longer PRBO was observed with SEMS placement [SHR = 0.37, P = 0.001]; use of 8.5-Fr PS (SHR = 0.58, P = 0.030); and Billroth II anatomy (SHR = 0.56 × 10−5, P < 0.001). In contrast, a significantly shorter PRBO was observed in the malignant group (SHR = 3.58, P < 0.001; Table 3 and Fig. 2B).
Risk factors for RBO and the best period to replace a PS in benign diseases
In the benign group, a long PRBO was observed with the use of 8.5-Fr PS (SHR = 0.58, P = 0.006; Table 4). Compared with the results shown in Table 3, Billroth II anatomy did not affect PRBO. Among the benign diseases, a significantly long PRBO was seen in IgG4-related sclerosing cholangitis (SHR = 0.07 × 10−8, P < 0.001; Table 4 and Fig. 3A), whereas a short PRBO was seen in Mirizzi syndrome (SHR = 3.32, P = 0.030; Table 4 and Fig. 3A). The longest PRBO after the first quartile of a non-RBO period was 1,329 days in chronic pancreatitis with biliary stricture (Table 4). In cases with bile duct stone, the median PRBO was 613 days (Table 4). Mirizzi syndrome cases had the shortest PRBO of 25 days after the first quartile of a non-RBO period, with a median PRBO of 63 days (Table 4). Overall, in the benign group, the first quartile and median period of a non-RBO period were 191 and 613 days, respectively (Table 4).
Competing risk model for recurrent biliary obstruction rates for each patient with (A) benign and (B) malignant diseases were compared. Mortality was assigned as the competing risk, and the other benign and malignant diseases (Tables 4 and 5) were assigned as covariates. Cases in which self-expandable metallic stents were placed were excluded.
Risk factors for RBO and the best period to replace a PS in malignant diseases
In the malignant group, a long PRBO was observed in cases that received chemotherapy after stent placement (SHR = 0.69, P = 0.016; Table 5). Conversely, unlike the results shown in Tables 3 and 4, the use of 8.5-Fr PS did not affect PRBO (Table 5). In addition, cancer stage was not associated with PRBO (Table 5). Among the malignant diseases, a significantly short PRBO was seen in cases of pancreatic cancer (SHR = 2.06, P = 0.041); perihilar bile duct cancer (SHR = 2.69, P = 0.006); and ampullary cancer (SHR = 3.78, P = 0.001) (Table 5 and Fig. 3B). The longest PRBO after the first quartile of a non-RBO was 73 days in gallbladder cancer (Table 5). In cases with colon cancer, the median PRBO was 420 days (Table 5). Cases of ampullary cancer had the shortest PRBO of 22 days after the first quartile of a non-RBO, with a median PRBO of 40 days (Table 5). Overall, in the malignant group, the first quartile and median period of a non-RBO were 39 and 108 days, respectively (Table 5).
Discussion
In the present study, we evaluated PRBO after PS or SEMS placement and evaluated the various factors related to RBO, according to each disease. Malignant diseases significantly differed from benign diseases, particularly with respect to PRBO, nonobstruction rate, cause of RBO, and technical and functional success rates. The multivariate competing risk analysis revealed that the use of SEMS, 8.5-Fr PS, and Billroth II anatomy was the factor that significantly prolonged PRBO. In contrast, the factor that significantly shortened PRBO was the malignant disease. Among the benign diseases, the factor that significantly prolonged PRBO was IgG4-related sclerosing cholangitis and 8.5-Fr PS, not Billroth II anatomy. In contrast, Mirizzi syndrome was the only significant factor that shortened PRBO. Among the malignant diseases, the factors that significantly shortened PRBO were pancreatic cancer, perihilar bile duct cancer, and ampullary cancer, not the use of 8.5-Fr PS and Billroth II anatomy. Chemotherapy after PS insertion was the only factor that prolonged PRBO.
Although SEMS has shown the advantage of a longer patency than PS5,9,13,17, its use upon initial insertion had been hesitated for the following cases: (1) placement of an uncovered SEMS before pathologic diagnosis mentioned differentiation between benign and malignant conditions5,18, (2) perihilar bile duct cancer before a decision to choose between surgery or nonsurgery, based on the clinical stage5,16, (3) operable malignant perihilar stricture in specific situations, such as acute cholangitis, ≤ 30% predicted volume of liver remnant following surgery5, (4) intake of anticoagulant agents and placement of fully covered SEMS without EST5,15,29,30, (5) more cost-effective use of PS in patients with short life expectancy1,16,17, (6) dilemma between unilateral and bilateral drainage for palliative EBD in perihilar bile duct cancer, such as Bismuth II–IV type5, and (7) benign diseases1,5,16.
In the present study, benign diseases without Mirizzi syndrome showed a long PRBO, suggesting that the interval to replace a PS may be feasible at 191 days after the first quartile, with a median of 613 days (Table 4), for patients with special circumstances, such as those with severe complications and who could not undergo EST and clearance of bile duct stone or cholecystectomy and those with benign biliary stricture from IgG4-related or chronic pancreatitis. The reason for a longer PRBO in benign nonbiliary stricture from bile duct stone or other benign biliary strictures than in malignant diseases might be the tighter stricture in malignant cases; even in benign diseases that develop luminal obstruction with sludge, the bile flow along with PS may prevent RBO (Supplementary Fig. S1 online). In fact, our results showed that the number of cases with sludge as the cause of RBO was significantly fewer in benign than in malignant diseases (Table 1). Moreover, we believed that prolonged factor for PRBO was not only the presence or absence of the biliary stricture but also the presence of strong stricture such as malignant disease (Supplementary Fig. S1 online) because our multivariate competing risk analysis (Table 4 and Fig. 3A) revealed that “IgG4-related sclerosing cholangitis” coupled with biliary stricture showed significantly prolonged PRBO compared with other benign diseases, including “bile duct stone” coupled with non-stricture. In addition, the multivariate competing risk analysis revealed that the use of 8.5-Fr PS was the factor that significantly prolonged PRBO in the benign group. This result may indicate that 8.5-Fr PS is the best thickness for longer intervals in benign disease because 10-Fr PS may be too thick for the bile flow, along with PS against benign stricture, and 7-Fr PS may involve a risk of distal symptomatic migration (Table 2, Supplementary Table S1 online). Thus, contrary to the published standards within 3–6 months intervals5,31, our results indicate that longer intervals for routine exchange of 8.5-Fr PS may be acceptable32.
Competing risk analysis showed a shorter PRBO after PS placement for malignant diseases than for benign diseases. For pancreatic cancer, routine PS replacement within 32 days after the first quartile or early change to SEMS may be needed to keep up with the scheduled surgery or chemotherapy. For perihilar bile duct cancer and ampullary cancer, the required interval for PS replacement or changing to SEMS would be within 27 days and 22 days, respectively, after the first quartile.
More recently, SEMS has been recommended to patients who have > 3 months of life expectancy, from the point of view of cost effectiveness and PRBO1,13,16,19. However, our study indicated that even patients with pancreatic cancer, perihilar bile duct cancer, and ampullary cancer who have more than 1 month of life expectancy may be recommended to receive SEMS placement. PS had been used during the initial EBD for suspected inoperable malignant biliary strictures in our hospital, because a pathologic diagnosis would be required before chemotherapy, including neoadjuvant chemotherapy33, and to repeat ERCP, in case the biopsy material was inadequate for pathologic diagnosis. Initial placement of a PS may be useful in such situations, because initial placement of an uncovered SEMS would render repeated ERCP for pathologic diagnosis difficult5. In contrast, it is also easy to replace a fully covered SEMS and PS; however, a fully covered SEMS is more expensive than a PS34.
Nowadays, preoperative EBD in distal malignant stricture has not been recommended due to the risk for postoperative pancreatic fistula, except for ongoing cholangitis or severe obstructive jaundice (serum bilirubin ≥ 300 μmol/L)1,5,10,16,35,36,37. However, many institutions in Japan tend to perform preoperative EBD owing to the long wait to surgery (range, 28.0–33.5 days), which, in itself, is a high risk factor for preoperative cholangitis arising out of non-symptomatic obstructive jaundice because preoperative cholangitis is related to postoperative pancreatic fistula36,37,38,39. A previous randomized controlled trial showed that the mean waiting time to surgery was only 8.4 days or 1.2 weeks35. The reason for this prolonged waiting time to surgery in Japan may be the detailed preoperative examinations, including examination of the whole body for complication and the decision on clinical stage and preoperative pathology38,39. The present study showed that the frequency of acute cholangitis at initial EBD for malignant disease was 54.7%, with a waiting time to surgery of 29 days. Taking together these results, preoperative EBD using a PS may be proposed and recommended for cases without pancreatic cancer and ampullary cancer, considering the cost effectiveness, because earlier routine replacement of a PS might be recommended for these two diseases1,13. In summary, only patients with ongoing cholangitis or severe obstructive jaundice may be required to undergo preoperative EBD with rapid triage to surgery within 22 days for ampullary cancer, including 32 days of pancreatic cancer, after PS placement or may require a fully covered SEMS1,10.
Our study had several limitations. First limitation was the retrospective and single-center design of the study. Second, several selection biases may have been included; for example, the choice of the diameter and type of PS were not fixed under a given condition and were left to the preference of the endoscopist. Thus, further prospective study is needed for prolonged PRBO of 8.5-Fr PS in the benign group. Finally, this study contained many confounding background factors that differed among the diseases.
In conclusion, our study supports that stent replacement for the benign group is feasible after 6 months, and the best period to replace or change a PS with a SEMS should be decided on the basis of underlying disease to prevent RBO.
References
Nakai, Y. et al. International consensus statements for endoscopic management of distal biliary stricture (J. Gastroenterol, Hepatol, 2019).
Mukai, S. et al. Indications and techniques of biliary drainage for acute cholangitis in updated Tokyo Guidelines 2018. J. Hepatobiliary. Pancreat. Sci. 24, 537–549 (2017).
Lai, E. C. et al. Endoscopic biliary drainage for severe acute cholangitis. N. Engl. J. Med. 326, 1582–1586 (1992).
Speer, A. G. et al. Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet 2, 57–62 (1987).
Dumonceau, J. M. et al. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy 50, 910–930 (2018).
Chopra, K. B. et al. Randomised study of endoscopic biliary endoprosthesis versus duct clearance for bileduct stones in high-risk patients. Lancet 348, 791–793 (1996).
Adler, D. G. et al. Clinical outcomes in patients with bile leaks treated via ERCP with regard to the timing of ERCP: a large multicenter study. Gastrointest. Endosc. 85, 766–772 (2017).
Haapamaki, C. et al. Randomized multicenter study of multiple plastic stents vs. covered self-expandable metallic stent in the treatment of biliary stricture in chronic pancreatitis. Endoscopy 47, 605–610 (2015).
Almadi, M. A., Barkun, A. & Martel, M. Plastic vs. Self-Expandable Metal Stents for Palliation in Malignant Biliary Obstruction: A Series of Meta-Analyses. Am. J. Gastroenterol. 112, 260–273 (2017).
Tol, J. A. et al. Metal or plastic stents for preoperative biliary drainage in resectable pancreatic cancer. Gut 65, 1981–1987 (2016).
Sangchan, A., Kongkasame, W., Pugkhem, A., Jenwitheesuk, K. & Mairiang, P. Efficacy of metal and plastic stents in unresectable complex hilar cholangiocarcinoma: a randomized controlled trial. Gastrointest. Endosc. 76, 93–99 (2012).
Soderlund, C. & Linder, S. Covered metal versus plastic stents for malignant common bile duct stenosis: a prospective, randomized, controlled trial. Gastrointest. Endosc. 63, 986–995 (2006).
Davids, P. H., Groen, A. K., Rauws, E. A., Tytgat, G. N. & Huibregtse, K. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet 340, 1488–1492 (1992).
Almadi, M. A., Barkun, J. S. & Barkun, A. N. Stenting in Malignant Biliary Obstruction. Gastrointest. Endosc. Clin. N. Am. 25, 691–711 (2015).
Martins, F. P., Kahaleh, M. & Ferrari, A. P. Management of liver transplantation biliary stricture: Results from a tertiary hospital. World J. Gastrointest. Endosc. 7, 747–757 (2015).
ASGE Technology Assessment Committee et al. Pancreatic and biliary stents. Gastrointest. Endosc. 77, 319–327 (2013).
Mukai, T. et al. Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J. Hepatobiliary. Pancreat. Sci. 20, 214–222 (2013).
Siriwardana, H. P. & Siriwardena, A. K. Systematic appraisal of the role of metallic endobiliary stents in the treatment of benign bile duct stricture. Ann. Surg. 242, 10–19 (2005).
Prat, F. et al. A randomized trial of endoscopic drainage methods for inoperable malignant strictures of the common bile duct. Gastrointest. Endosc. 47, 1–7 (1998).
Kiriyama, S. et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J. Hepatobiliary. Pancreat. Sci. 25, 17–30 (2018).
Kiriyama, S. et al. Clinical application and verification of the TG13 diagnostic and severity grading criteria for acute cholangitis: an international multicenter observational study. J. Hepatobiliary. Pancreat. Sci. 24, 329–337 (2017).
Isayama, H. et al. TOKYO criteria 2014 for transpapillary biliary stenting. Dig. Endosc. 27, 259–264 (2015).
Ge, P. S. et al. Plastic biliary stent patency in patients with locally advanced pancreatic adenocarcinoma receiving downstaging chemotherapy. Gastrointest. Endosc. 81, 360–366 (2015).
Hayden, J. A., van der Windt, D. A., Cartwright, J. L., Cote, P. & Bombardier, C. Assessing bias in studies of prognostic factors. Ann. Intern. Med. 158, 280–286 (2013).
Abraira, V. et al. Reporting quality of survival analyses in medical journals still needs improvement. A minimal requirements proposal. J. Clin. Epidemiol. 66, 1340–6.e5 (2013).
Chen, H., Siwo, E. A., Khu, M. & Tian, Y. Current trends in the management of Mirizzi Syndrome: A review of literature. Medicine (Baltimore) 97, e9691 (2018).
Cepeda, M. S., Boston, R., Farrar, J. T. & Strom, B. L. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am. J. Epidemiol. 158, 280–287 (2003).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94, 496–509 (1999).
ASGE Standards of Practice Committee et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest. Endosc. 83, 3–16 (2016).
Veitch, A. M. et al. Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Gut 65, 374–389 (2016).
Di Giorgio, P. et al. Endoscopic plastic stenting for bile duct stones: stent changing on demand or every 3 months. A prospective comparison study. Endoscopy 45, 1014–1017 (2013).
Slattery, E., Kale, V., Anwar, W., Courtney, G. & Aftab, A. R. Role of long-term biliary stenting in choledocholithiasis. Dig. Endosc. 25, 440–443 (2013).
Tempero, M. A. et al. Pancreatic Adenocarcinoma, Version 1.2019. J. Natl. Compr. Canc Netw. 17, 202–210 (2019).
Gardner, T. B. et al. Cost-effectiveness and clinical efficacy of biliary stents in patients undergoing neoadjuvant therapy for pancreatic adenocarcinoma in a randomized controlled trial. Gastrointest. Endosc. 84, 460–466 (2016).
van der Gaag, N. A. et al. Preoperative biliary drainage for cancer of the head of the pancreas. N. Engl. J. Med. 362, 129–137 (2010).
Sauvanet, A. et al. Severe jaundice increases early severe morbidity and decreases long-term survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. J. Am. Coll. Surg. 221, 380–389 (2015).
Ohgi, K. et al. Bacterobilia may trigger the development and severity of pancreatic fistula after pancreatoduodenectomy. Surgery 160, 725–730 (2016).
Kaneko, T. et al. Influence of cholangitis after preoperative endoscopic biliary drainage on postoperative pancreatic fistula in patients with middle and lower malignant biliary strictures. Dig. Endosc. 30, 90–97 (2018).
Kitahata, Y. et al. Preoperative cholangitis during biliary drainage increases the incidence of postoperative severe complications after pancreaticoduodenectomy. Am. J. Surg. 208, 1–10 (2014).
Acknowledgements
The authors thank the Department of Surgery, and Division of Gastroenterology and Hepatology for patient recruitment. The authors also thank Enago for the English language editing of this paper.
Author information
Authors and Affiliations
Contributions
Conception and design: M.C., M.K. Performing endoscopic examinations: M.C., M.K., Y.K., N.S., Y.T., T.A., Y.K., S.K., K.K., S.T., Y.T., H.T., K.I.. Acquisition of data: M.C., M.K., Y.K., N.S., Y.T., T.A. Statistical analysis: M.C., M.K.. Analysis and interpretation of the data: M.C., M.K., Y.K., N.S., Y.T., T.A., Y.K., S.K., K.K., K.T., S.T., M.N., Y.T., H.A. Statistical analysis: M.C., M.K.. Writing of the original paper: M.C., M.K., K.S. Revision of the paper: M.C., M.K.. Approval of the final draft submitted: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chiba, M., Kato, M., Kinoshita, Y. et al. Best period to replace or change plastic stents with self-expandable metallic stents using multivariate competing risk regression analysis. Sci Rep 10, 13080 (2020). https://doi.org/10.1038/s41598-020-70081-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-020-70081-3