Abstract
In percutaneous coronary intervention (PCI) to the culprit lesion of acute myocardial infarction (AMI), unsuccessful guidewire crossing causes immediate poor outcomes. It is important to determine the factors associated with unsuccessful guidewire crossing in AMI lesions. The purpose of this study was to find factors associated with difficulty in crossing the culprit lesion of AMI. We defined the difficult group when the guidewire used to cross the culprit lesion was a polymer jacket type guidewire or a stiff guidewire. We included 937 patients, and divided those into the non-difficult group (n = 876) and the difficult group (n = 61). Proximal reference diameter was significantly smaller in the difficult group than in the non-difficult group (p < 0.001), and degree of calcification was severer in the difficult group than in the non-difficult group (p < 0.001). In the multivariate stepwise logistic regression analysis, proximal reference diameter [odds ratio (OR) 0.313, 95% confidence interval (CI) 0.185–0.529, p < 0.001)], previous PCI (OR 3.065, 95% CI 1.612–5.830, p = 0.001), moderate-severe calcification (OR 4.322, 95% CI 2.354–7.935, p < 0.001), blunt type obstruction (OR 12.646, 95% CI 6.805–23.503, p < 0.001), and the presence of collateral to the culprit lesion (OR 2.110, 95% CI 1.145–3.888, p = 0.017) were significantly associated with difficulty in crossing the culprit lesion. In conclusion, previous PCI, calcification, blunt type obstruction, and the presence of collateral were associated with difficulty in crossing the culprit lesion, whereas proximal reference diameter was inversely associated with difficulty. Our study provides a reference to recognize the difficulty in crossing the culprit lesions of AMI for PCI operators, especially junior operators.
Similar content being viewed by others
Introduction
Percutaneous coronary intervention (PCI) to the culprit lesion of acute myocardial infarction (AMI) accounts for the most significant portion of the contemporary treatment of AMI1,2,3. The mortality and morbidity of AMI have considerably decreased following the development of primary PCI4,5. Among several procedures in PCI, the first step for the successful revascularization is to manipulate the coronary guidewire to cross the culprit lesion of AMI, which is generally not so difficult for non-chronic total occlusion (CTO) lesions6, partly because more than half of the occluded segment of AMI consists of ruptured non-calcified plaque and platelet-mediated thrombus7. In fact, the delay in door-to-balloon time was affected primarily by the time delay from diagnosis in the emergency department to catheterization laboratory transfer rather than a delay in catheterization laboratory arrival to balloon inflation8.
However, even in primary PCI, interventional cardiologists sometimes encounter difficult cases in which the conventional guidewire cannot cross the culprit lesion. If the guidewire cannot cross the culprit lesion of AMI, emergent PCI results in unsuccessful reperfusion, which may lead to serious mechanical complications and subsequent poor clinical outcomes9,10. Several groups reported the determinants of successful or unsuccessful guidewire crossing in the field of PCI to CTO lesions11,12, whereas there has been few literatures regarding the determinants of guidewire crossing in PCI to AMI lesions. Since unsuccessful guidewire crossing would have more serious impact on patient’s immediate outcomes in PCI to AMI lesions than PCI to CTO lesions, it is of utmost importance to determine the factors associated with unsuccessful guidewire crossing in AMI lesions. The purpose of this study was to find factors associated with difficulty in crossing the culprit lesion of AMI.
Methods
Study design
We identified consecutive AMI patients in our institution from January, 2015 to December, 2018. The inclusion criteria were (1) patients with AMI, and (2) patients who underwent PCI to the culprit lesion of AMI. The exclusion criteria were (1) patients who were treated by medical therapy alone, (2) patients who underwent coronary artery bypass graft surgery to the culprit lesion, and (3) patients who underwent PCI to the non-culprit lesion as well as the culprit lesion of AMI simultaneously. The final study population was divided into a difficult group and a non-difficult group according to the guidewire used to cross the culprit lesion. The difficult group was defined as the lesion in which a conventional floppy guidewire failed to cross and a polymer jacket type wire or a stiff guidewire with a tip load of 1.5 g or more was required to cross. The non-difficult group was defined as the lesion in which a conventional floppy guidewire successfully crossed. The primary interest of this study was to find factors associated with the difficult group using multivariate logistic regression analysis. This study was approved by the Institutional Review Board of the Saitama Medical Center, Jichi Medical University (S20-136), and written informed consent was waived by the institutional review board of the Saitama Medical Center, Jichi Medical University, because of the retrospective study design. All methods were performed in accordance with the relevant guidelines and regulations.
PCI to the culprit of AMI
PCI procedures were performed on a biplane fluoroscopy system. The choice of PCI devices such as guidewire, balloon, thrombectomy device, rotational atherectomy device, and stent was left at the discretion of interventional cardiologists at our cardiology center. First, we selected a conventional floppy wire to cross the culprit lesion of AMI. Our catheter laboratory had the following conventional floppy wire during the study period: Sion blue (Asahi Intecc, Aichi, Japan), Sion (Asahi Intecc, Aichi, Japan), Runthrough NS Floppy (Terumo, Tokyo, Japan), and ETNA (FMD, Tokyo, Japan). If the floppy wire could not cross the culprit lesion, we used a microcatheter to enhance backup or used a polymer jacket type guidewire. During the study period, the following polymer jacket type guidewires were used for this purpose: Sion black (Asahi Intecc, Aichi, Japan) and XT-R (Asahi Intecc, Aichi, Japan). Although microcatheters were used in most cases of lesions required polymer jacket guidewires, Sion black was sometimes used without microcatheter. If the polymer jacket type guidewire could not cross the lesion, we used a stiff guidewire with a tip load of 1.5 g or more. When we used a stiff guidewire, microcatheters were always used. During the study period, the following stiff guidewires were used for this purpose: Gaia First (Asahi Intecc, Aichi, Japan), Gaia Next 1 (Asahi Intecc, Aichi, Japan), ULTIMATE Bros 3 (Asahi Intecc, Aichi, Japan), and Conquest Pro 12 (Asahi Intecc, Japan). Our university hospital had many operators including junior operators. However, each PCI was strictly supervised by staff operators even in mid-night or holidays. Staff operators did not hesitate to take over procedures, when junior operators felt any difficulties in procedures such as the guidewire crossing the culprit lesion, the delivering device to the culprit lesion, etc. The decision to use a polymer jacket guidewire or a stiff guidewire was not made by junior operators, but by staff operators. Successful PCI was defined as angiographical residual diameter stenosis < 50% with decrease in minimum stenosis with TIMI flow grade ≥ 213.
Definition
Acute myocardial infarction (AMI) was defined based on universal definition of myocardial infarction14,15. Hypertension was defined as medical treatment for hypertension and/or a history of hypertension before admission16. Dyslipidemia was defined as a total cholesterol level ≥ 220 mg/dL or low-density lipoprotein cholesterol level ≥ 140 mg/dL or medical treatment for dyslipidemia or a history of dyslipidemia16,17. Diabetes mellitus was defined as a hemoglobin A1c level ≥ 6.5% (as NGSP value) or medical treatment for diabetes mellitus or a history of diabetes mellitus16,17. We calculated the estimated glomerular filtration rate (eGFR) from the serum creatinine level, age, weight, and gender using the following formula: eGFR = 194 × Cr-1.094 × age-0.287 (male), eGFR = 194 × Cr-1.094 × age-0.287 × 0.739 (female)18.
Angiographical analysis
Quantitative coronary angiography (QCA) parameters were measured using a cardiovascular angiography analysis system (QAngio XA 7.3, MEDIS Imaging Systems, Leiden, Netherlands). QCA parameters such as lesion length and reference diameter were measured after the acquisition of reperfusion (after ballooning or thrombectomy) if the lesion was occluded. However, these QCA parameters might not be accurate especially in the measurement of distal reference diameter. We separately measured proximal reference diameter in all cases using the published method19. We did not use reference diameter or lesion lengths in the multivariate analysis, but used proximal reference diameter in the multivariate logistic regression analysis. The definition of lesion characteristics including lesion length, eccentricity, tortuosity, lesion angle, ostial lesion, bifurcation lesion has been previously described20. As known, bifurcation lesion is defined as the side branch requiring wire protection from the culprit lesion20. In an original ACC/AHA definition, tortuosity was defined as follows: stenoses distal to two bends were defined as moderately tortuous, and those distal to three or more bends were defined as excessive tortuosity20. However, since the above definition of tortuosity has poor objectivity, we additionally defined tortuosity as follows: “ ≤ 1” moderate to excessive bend (< 120°) was defined as mild tortuosity, “2” moderate to excessive bend (< 120°) was defined as moderate tortuosity, and “ ≥ 3” moderate to excessive bend (< 120°) was defined as excessive tortuosity21. Calcification was identified as readily apparent radiopacities within the vascular wall at the site of the stenosis, and was classified as none/mild, moderate (radiopacities noted only during the cardiac cycle before contrast injection), and severe (radiopacities noted without cardiac motion before contrast injection generally compromising both sides of the arterial lumen)22. The lesion morphology was classified into either blunt type or tapered type based on the definition of the J-CTO score11. The degree of collateral artery was classified as grade 0–3 based on the Rentrop classification, and the presence of collateral was defined as Rentrop grade ≥ 123. Thrombus was classified based on the TIMI thrombus grade24.
Statistical analysis
Data are shown as the mean ± SD or percentage. Categorical variables are presented as numbers (percentage), and were compared using the Pearson’s chi-square test. Continuous variables were compared between the groups using the unpaired Student’s test. Univariate and multivariate logistic regression analyses were performed to find the association between clinical variables and difficulty in crossing the culprit lesion of AMI. In this model, the difficult group was used as the dependent variable. In the multivariate stepwise logistic regression model, the selection of independent variables was derived from the results of univariate logistic regression analysis (p < 0.05 in univariate analysis). However, variables with missing values were not included in the model. Furthermore, when there are ≥ 2 similar variables, only one variable was entered into the multivariable model to avoid multi-collinearity. The multivariate logistic regression analysis with likelihood ratio statistical criteria using backward elimination method was performed. The odds ratio (OR) and the 95% confidence interval (CI) were also calculated. A P value < 0.05 was considered statistically significant. We analyzed all data by IBM SPSS statistics version 24 (Chicago, Illinois, USA).
Results
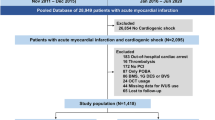
During the study period, we had 1089 AMI patients in our medical center. We excluded 152 patients according to the exclusion criteria. Our final study population was 937 patients, and was divided into the difficult group (n = 61) and the conventional group (n = 876). The study flowchart is shown in Fig. 1. The used guidewire in the difficult group were Sion black (n = 36), XT-R (n = 16), Gaia First (n = 3), Gaia Next 1 (n = 2), Ultimate Bros 3 (n = 3), and Conquest Pro 12 (n = 1), whereas the used guidewire in the non-difficult group were Sion blue (n = 664), Sion (n = 210), Runthrough NS floppy (n = 1), and ETNA (n = 1). There were no unsuccessful PCI cases in the final study population. There were 46 patients who changed their approach site from radial arteries to femoral arteries. Of 46 patients, 18 patients were due to radial artery spasm or narrowing, 17 patients were due to severe meandering of peripheral arteries such as brachiocephalic artery, and 11 patients were due to insufficient back-up support.
The comparison of clinical, lesion and procedural characteristics is shown in Table 1. Proximal reference diameter was significantly smaller in the difficult group than in the non-difficult group (2.43 ± 0.65 mm vs. 2.79 ± 0.65 mm, p < 0.001). Degree of calcification was severer in the difficult group than in the non-difficult group (p < 0.001). In the lesion morphology, the prevalence of blunt type was greater in the difficult group than in the non-difficult group (p < 0.001). Collateral to the culprit lesion was more common in the difficult group than in the non-difficult group (p = 0.001). There were no patients who required bi-directional approach (i.e. antegrade approach and retrograde approach) to complete PCI to the culprit lesion of AMI, but there were 5 patients who required contralateral injection to identify collateral arteries.
The univariate logistic regression model to find the factors associated with the difficulty in crossing the culprit lesion is shown in Table 2. Complex lesion characteristics such as small proximal reference diameter, calcification, blunt type obstruction, and the presence of collateral were associated with difficulty in crossing the culprit lesion. Furthermore, some procedural characteristics such as size of guiding catheter, number of guidewires, and use of microcatheter were also associated with the difficulty in crossing the culprit lesion.
The multivariate stepwise logistic regression analysis to find the factors associated with difficulty in crossing the culprit lesion is shown in Table 3. The initial stepwise model included the following variables: age, proximal reference diameter, previous PCI, triple vessels disease (vs. ≤ 2 vessel diseases), initial TIMI flow grade 3 of culprit (vs. grade 0–2), moderate-severe calcification (vs. none-mild), blunt type obstruction (vs. tapered type), collateral to the culprit lesion, in-stent lesion, and TIMI thrombus grade 4–5 (vs. grade 0–3). In the final model, proximal reference diameter (OR 0.313, 95% CI 0.185–0.529, p < 0.001), history of previous PCI (OR 3.065, 95% CI 1.612–5.830, p = 0.001), moderate-severe calcification (vs. none-mild: OR 4.322, 95% CI 2.354–7.935, p < 0.001), blunt type obstruction (OR 12.646, 95% CI 6.805–23.503, p < 0.001), and the presence of collateral to the culprit lesion (OR 2.110, 95% CI 1.145–3.888, p = 0.017) were significantly associated with difficulty in crossing the culprit lesion.
Discussion
We included 937 patients who underwent PCI to the culprit lesion of AMI, and divided those into the conventional group (n = 876) and the difficult group (n = 61) according to the difficulty in crossing the culprit lesion of AMI. In other words, approximately 7% of AMI lesions required a polymer jacket type guidewire or a stiff guidewire to cross the culprit lesion. In the multivariate stepwise logistic regression analysis, history of previous PCI, moderate-severe calcification, blunt type obstruction, and the presence of collateral to the culprit lesion were significantly associated with difficulty in crossing the culprit lesion, whereas proximal reference diameter was inversely associated with difficulty in crossing the culprit lesion.
In the present study, proximal reference diameter was inversely associated with difficulty in crossing the culprit lesion. Thus, the small vessel diameter was a factor associated with difficulty in crossing the lesion. In the pathology of AMI, there are 3 major underlying diseases: plaque rupture, plaque erosion, and calcified nodule7,25. Of these 3 underlying diseases, plaque rupture is closely associated with positive remodeling, whereas other 2 underlying diseases are not26. Therefore, the small vessel diameter may indicate that the underlying disease of the difficult cases were not plaque rupture, but plaque erosion or calcified nodule27. Although there were no studies to directly compare the difficulty in crossing lesions among 3 underlying diseases, most interventional cardiologists might be more familiar with crossing the lesion associated with plaque rupture rather than plaque erosion or calcified nodule.
We should discuss why history of previous PCI was associated with difficulty in crossing the lesion. History of previous PCI means that AMI occurred even after the patient had some secondary prevention drugs such as statin or aspirin28. Chronic statin treatment might reduce soft plaque components such as necrotic core29, which might affect the difficulty in crossing the lesion. Furthermore, most patients with history of previous PCI had coronary stents before AMI onset. Therefore, the type of occlusion in patients with history of previous PCI might be different from that in patients without history of previous PCI. For example, in-stent failure (restenosis or thrombosis) should be only observed in patients with history of previous PCI. However, it is still unknown why AMI lesions in patients with history of previous PCI was difficult to cross.
We should also discuss why moderate-severe calcification was associated with the difficulty in crossing the culprit lesion. Although there were few reports showing that calcification was the factor of difficulty in crossing the culprit lesion of AMI, it is widely known that calcification is associated with the difficulty of PCI21. Severe calcification causes unsuccessful device delivery, stent under-expansion, and long-term stent failure30,31. Moreover, moderate-severe calcification suggests that the underlying disease of AMI was calcified nodule rather than plaque rupture. When the underlying disease of AMI was calcified nodule, it might be difficult to cross the lesions by using conventional guidewires32, and might require polymer jacket type guidewires.
Blunt type obstruction was significantly associated with the difficulty in crossing the culprit lesion in the present study. In PCI to CTO lesions, it is widely known that it is more difficult to cross the lesion in blunt type obstructions than in tapered type obstructions33. Our results confirmed that blunt type obstruction can be a maker of the difficulty in crossing the lesion even in PCI to AMI lesions. The presence of collateral to the culprit lesion was also associated with the difficulty in crossing the lesion. Developed collateral arteries imply that there had been a severe stenosis before the complete obstruction occurred at the onset of AMI34, which suggests that the plaque components were not occupied by fresh thrombus, but by organized thrombus35.
In this study, the prevalence of admission within 24 h from onset was significantly less in the difficult group than in the non-difficult group. In general, thrombotic lesions are expected to become organized over time36, which made wire crossing difficult. Although we did not include admission within 24 h from onset in the multivariate logistic regression analysis because of missing value, lapsed time from the onset might be an important factor that determined the difficulty in crossing the culprit lesion of AMI.
Clinical implications of the present study should be noted. Unlike PCI to CTO lesions, junior PCI operators sometimes perform PCI to the culprit lesion of AMI without senior operator’s backup37, partly because AMI occurs anytime irrespective of on-hours or off-hours. Although most PCI to AMI lesions may be successfully managed by junior PCI operators, some AMI lesions require polymer jacket type guidewires or stiff guidewires which junior PCI operators are unfamiliar with. Our results would help junior PCI operators to consult with senior operators about backup support. If the culprit lesion morphology is blunt type obstruction with severe calcification, it may be better for junior PCI operators to ask senior operator’s support before trying polymer jacket type guidewires or stiff guidewires. Once the pseudo-lumen was enlarged by immature manipulation, it is very difficult even for senior operators to select the compressed true-lumen.
Study limitations
First, because this study was a single-center retrospective observational study, there is a risk of patient selection bias. Second, we defined the difficult group as the lesion in which a conventional floppy guidewire failed to cross and a polymer jacket wire or a stiff guidewire with a tip load of 1.5 g or more was required to cross, which may lack objectivity. Although it would be better to define the unsuccessful guidewire crossing as the difficult case, there were no unsuccessful cases during the study period, probably because all AMI cases were supported by staff operators in our catheter laboratory. Since there were no cases when operators used polymer jacket type guidewires or stiff guidewires before trying conventional guidewires and the decision to use those specific guidewires was made by experienced staff operators, it may be acceptable to mention that our difficult cases were not technically easy. Furthermore, since most of our PCI cases were completed by the combination of junior operators and staff operators, it was difficult to adjust operator’s experience as one of confounding factors in multivariate analysis. Third, although we comprehensively judged the culprit lesion of AMI by reviewing angiogram, electrocardiogram, and echocardiogram, there is a possibility that we might misunderstand the culprit lesion in multivessel disease. We might perform PCI to CTO lesions as the culprit of AMI in multivessel disease, because we could not compare emergent angiogram with previous angiogram in most cases.
Conclusions
In PCI to the culprit lesion of AMI, history of previous PCI, moderate-severe calcification, blunt type obstruction, and the presence of collateral to the culprit lesion were significantly associated with difficulty in crossing the culprit lesion, whereas proximal reference diameter was inversely associated with difficulty in crossing the culprit lesion. Our study provides a reference to identify difficulty in crossing the culprit lesions of AMI for PCI operators, especially junior operators.
Data availability
All data are available from the corresponding author on reasonable request.
References
F Ragmin and Fast Revascularisation during InStability in Coronary artery disease (FRISC II) investigators. Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. FRagmin and Fast Revascularisation during InStability in Coronary artery disease Investigators. Lancet. 354, 708–715 (1999).
Keeley, E. C. & Hillis, L. D. Primary PCI for myocardial infarction with ST-segment elevation. N. Engl. J. Med. 356, 47–54. https://doi.org/10.1056/NEJMct063503 (2007).
Roffi, M. et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European society of cardiology (ESC). Eur. Heart J. 37, 267–315. https://doi.org/10.1093/eurheartj/ehv320 (2016).
Yamamoto, T., Yoshida, N. & Takayama, M. Temporal trends in acute myocardial infarction incidence and mortality between 2006 and 2016 in Tokyo: Report from the Tokyo CCU network. Circ. J. 83, 1405–1409. https://doi.org/10.1253/circj.CJ-19-0187 (2019).
Plakht, Y., Gilutz, H. & Shiyovich, A. Temporal trends in acute myocardial infarction: What about survival of hospital survivors? Disparities between STEMI & NSTEMI remain. Soroka acute myocardial infarction II (SAMI-II) project. Int. J. Cardiol. 203, 1073–1081. https://doi.org/10.1016/j.ijcard.2015.11.072 (2016).
Galassi, A. R. et al. Retrograde recanalization of chronic total occlusions in Europe: Procedural, in-hospital, and long-term outcomes from the multicenter ERCTO registry. J. Am. Coll. Cardiol. 65, 2388–2400. https://doi.org/10.1016/j.jacc.2015.03.566 (2015).
Virmani, R., Kolodgie, F. D., Burke, A. P., Farb, A. & Schwartz, S. M. Lessons from sudden coronary death: A comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler. Thromb. Vasc. Biol. 20, 1262–1275. https://doi.org/10.1161/01.atv.20.5.1262 (2000).
Magid, D. J. et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA 294, 803–812. https://doi.org/10.1001/jama.294.7.803 (2005).
Shiomi, H. et al. Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ 344, e3257. https://doi.org/10.1136/bmj.e3257 (2012).
Gramegna, M. et al. Impella RP support in refractory right ventricular failure complicating acute myocardial infarction with unsuccessful right coronary artery revascularization. Int. J. Cardiol. 302, 135–137. https://doi.org/10.1016/j.ijcard.2019.12.024 (2020).
Morino, Y. et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: The J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc. Interv. 4, 213–221. https://doi.org/10.1016/j.jcin.2010.09.024 (2011).
Opolski, M. P. et al. Coronary computed tomographic prediction rule for time-efficient guidewire crossing through chronic total occlusion: insights from the CT-RECTOR multicenter registry (Computed Tomography Registry of Chronic Total Occlusion Revascularization). JACC Cardiovasc. Interv. 8, 257–267. https://doi.org/10.1016/j.jcin.2014.07.031 (2015).
Mizuno, Y. et al. Comparison of the incidence of periprocedural myocardial infarction between percutaneous coronary intervention with versus without rotational atherectomy using propensity score-matching. Sci. Rep. 11, 11140. https://doi.org/10.1038/s41598-021-90042-8 (2021).
Thygesen, K. et al. Fourth universal definition of myocardial infarction (2018). J. Am. Coll. Cardiol. 72, 2231–2264. https://doi.org/10.1016/j.jacc.2018.08.1038 (2018).
Sawano, M. et al. Contemporary use and trends in percutaneous coronary intervention in Japan: An outline of the J-PCI registry. Cardiovasc. Interv. Ther. 35, 218–226. https://doi.org/10.1007/s12928-020-00669-z (2020).
Noguchi, M. et al. The comparison of clinical outcomes between inferior ST-elevation myocardial infarction with right ventricular infarction versus without right ventricular infarction. Int. Heart J. 60, 560–568. https://doi.org/10.1536/ihj.18-515 (2019).
Kubota, M. et al. Mid-term clinical outcomes of immediate protamine use following elective percutaneous coronary interventions. Int. Heart J. 61, 865–871. https://doi.org/10.1536/ihj.20-126 (2020).
Matsuo, S. et al. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 53, 982–992. https://doi.org/10.1053/j.ajkd.2008.12.034 (2009).
Suzuki, N. et al. Clinical expert consensus document on quantitative coronary angiography from the Japanese Association of Cardiovascular Intervention and Therapeutics. Cardiovasc. Interv. Ther. 35, 105–116. https://doi.org/10.1007/s12928-020-00653-7 (2020).
Ellis, S. G. et al. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group. Circulation 82, 1193–1202. https://doi.org/10.1161/01.cir.82.4.1193 (1990).
Asada, S. et al. Association of the long fluoroscopy time with factors in contemporary primary percutaneous coronary interventions. PLoS ONE 15, e0237362. https://doi.org/10.1371/journal.pone.0237362 (2020).
Mintz, G. S. et al. Patterns of calcification in coronary artery disease. A statistical analysis of intravascular ultrasound and coronary angiography in 1155 lesions. Circulation 91, 1959–1965. https://doi.org/10.1161/01.cir.91.7.1959 (1995).
Allahwala, U. K., Weaver, J. C. & Bhindi, R. Spontaneous coronary collateral recruitment in patients with recurrent ST elevation myocardial infarction (STEMI). Heart Vessels 35, 291–296. https://doi.org/10.1007/s00380-019-01493-z (2020).
Tanboga, I. H. et al. Determinants of angiographic thrombus burden in patients with ST-segment elevation myocardial infarction. Clin. Appl. Thromb. Hemost. 20, 716–722. https://doi.org/10.1177/1076029613483169 (2014).
Little, W. C. et al. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease?. Circulation 78, 1157–1166. https://doi.org/10.1161/01.cir.78.5.1157 (1988).
Moreno, P. R. et al. Plaque neovascularization is increased in ruptured atherosclerotic lesions of human aorta: Implications for plaque vulnerability. Circulation 110, 2032–2038. https://doi.org/10.1161/01.Cir.0000143233.87854.23 (2004).
van der Wal, A. C., Becker, A. E., van der Loos, C. M. & Das, P. K. Site of intimal rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation 89, 36–44. https://doi.org/10.1161/01.cir.89.1.36 (1994).
Taguchi, I. et al. High-dose versus low-dose pitavastatin in Japanese patients with stable coronary artery disease (REAL-CAD): A randomized superiority trial. Circulation 137, 1997–2009. https://doi.org/10.1161/circulationaha.117.032615 (2018).
Jinnouchi, H. et al. Effect of chronic statin treatment on vascular remodeling determined by intravascular ultrasound in patients with acute myocardial infarction. Am. J. Cardiol. 113, 924–929. https://doi.org/10.1016/j.amjcard.2013.11.054 (2014).
Tripolino, C., Tassone, E. J., Morabito, G., Grillo, P. & Missiroli, B. ST-elevation myocardial infarction due to stent underexpansion managed with coronary lithoplasty. Rev. Recent Clin. Trials 14, 292–295. https://doi.org/10.2174/1574887114666190927164253 (2019).
de Waha, S. et al. Rotational atherectomy before paclitaxel-eluting stent implantation in complex calcified coronary lesions: Two-year clinical outcome of the randomized ROTAXUS trial. Catheter. Cardiovasc. Interv. 87, 691–700. https://doi.org/10.1002/ccd.26290 (2016).
Kassimis, G. et al. How should we treat heavily calcified coronary artery disease in contemporary practice? From atherectomy to intravascular lithotripsy. Cardiovasc. Revasc. Med. 20, 1172–1183. https://doi.org/10.1016/j.carrev.2019.01.010 (2019).
Christopoulos, G. et al. Application and outcomes of a hybrid approach to chronic total occlusion percutaneous coronary intervention in a contemporary multicenter US registry. Int. J. Cardiol. 198, 222–228. https://doi.org/10.1016/j.ijcard.2015.06.093 (2015).
Meier, P. et al. The impact of the coronary collateral circulation on outcomes in patients with acute coronary syndromes: Results from the ACUITY trial. Heart 100, 647–651. https://doi.org/10.1136/heartjnl-2013-304435 (2014).
Sakakura, K. et al. Comparison of pathology of chronic total occlusion with and without coronary artery bypass graft. Eur. Heart J. 35, 1683–1693. https://doi.org/10.1093/eurheartj/eht422 (2014).
LATE Study Group. Late Assessment of Thrombolytic Efficacy (LATE) study with alteplase 6–24 hours after onset of acute myocardial infarction. Lancet. 342, 759–766 (1993).
Chen, M. et al. Improvement of clinical outcome in patients with ST-elevation myocardial infarction between 1999 and 2016 in China: The prospective, multicentre registry MOODY study. Eur. J. Clin. Invest. 50, e13197. https://doi.org/10.1111/eci.13197 (2020).
Acknowledgements
The authors acknowledge all staff in the catheter laboratory, ICU/CCU, and cardiology ward in Saitama Medical Center, Jichi Medical University, for their technical support in this study.
Author information
Authors and Affiliations
Contributions
S.I. and K.S. conceived the idea of the study. S.I., K.S., S.A., Y.T., H.J., T.T., K.Y., M.S., and H.W. collected the data. S.I. performed statistical analysis, and drafted a manuscript. K.S. revised the manuscript. K.S. and H.F. interpreted the data. All authors commented on the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
Dr. Sakakura has received speaking honoraria from Abbott Vascular, Asahi Intecc, Boston Scientific, Kaneka, Medtronic Cardiovascular, Terumo, OrbusNeich, Japan Lifeline, and NIPRO. He has served as a proctor for Rotablator for Boston Scientific and has served as a consultant for Abbott Vascular and Boston Scientific. Dr. Jinnouchi has received speaking honoraria from Abbott Vascular. Prof. Fujita served as a consultant for Mehergen Group Holdings, Inc.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ishibashi, S., Sakakura, K., Asada, S. et al. Factors associated with difficulty in crossing the culprit lesion of acute myocardial infarction. Sci Rep 11, 21403 (2021). https://doi.org/10.1038/s41598-021-00832-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-021-00832-3
This article is cited by
-
Association between the long-term dialysis due to diabetic nephropathy and clinical outcomes in patients with coronary artery disease and chronic renal failure
Cardiovascular Intervention and Therapeutics (2025)
-
Factors associated with intensive care unit delirium in patients with acute myocardial infarction
Heart and Vessels (2023)