Abstract
Diagnosis of pulmonary lymphoma using small tissue samples is difficult and often requires surgical procedures; thus, a less invasive sampling method is desirable. We previously showed that pulmonary mucosa-associated lymphoid tissue (MALT) lymphoma can be diagnosed by detecting MALT lymphoma translocation gene 1 (MALT1) translocations in bronchoalveolar lavage fluid (BALF) cells. Analysis of B-cell clonality based on immunoglobulin heavy chain (IGH) gene rearrangements was also reportedly useful for diagnosing pulmonary lymphoma. The aim of this prospective multicenter study was to evaluate the yet unknown diagnostic potential of combined detection of MALT1 translocations and clonality using BALF. We analyzed B- and T-cell clonality based on IGH and T-cell receptor (TCR) rearrangements together with MALT1 translocations using BALF of patients with clinically suspected pulmonary lymphomas. In total, 39 patients were evaluated and categorized into three groups: B-cell lymphoma, lymphoproliferative disorders, and other diseases. IGH rearrangement detection for B-cell lymphoma diagnosis exhibited sensitivity and specificity of 88.9% and 90.0%, respectively. TCR rearrangements were not observed in patients with B-cell lymphomas. The presence of IGH rearrangements together with the absence of TCR rearrangements indicated 96.0% specificity for the diagnosis of B-cell lymphoma. The sensitivity and specificity of MALT1 translocations for diagnosing MALT lymphoma were 28.6% and 100%, respectively. The combined detection of lymphocyte clonality and MALT1 translocations using BALF is suitable for screening and diagnosis of B-cell lymphomas. Analysis of specific genes such as MALT1 should improve the precision of B-cell lymphoma diagnosis.
Similar content being viewed by others
Introduction
Pulmonary lymphomas account for 0.5–1% of all pulmonary malignancies1,2,3. Among 1500 patients with lung cancer, 1.7% were diagnosed with primary pulmonary lymphoma and 2.7%—with secondary involvement of the lung by lymphoma4. Mucosa-associated lymphoid tissue (MALT) lymphoma is a low-grade B-cell malignancy representing the most frequently diagnosed type of pulmonary lymphomas3,5; other types include diffuse large B-cell lymphomas and T-cell lymphomas. Owing to their relative rarity and the difficulty associated with diagnosing this cancer, pulmonary lymphomas are challenging to manage, and their diagnostic strategy is not well established.
Minimally invasive techniques, such as bronchoscopy and computed tomography (CT)-guided lung biopsy, are often employed for diagnosing lung lesions to avoid more invasive surgical interventions3. However, tissue samples obtained via transbronchial lung biopsy (TBLB) or CT-guided lung biopsy are small and contain a mixture of infiltrates, including neoplastic lymphoid cells and other inflammatory cells3. These problems complicate the diagnosis of pulmonary lymphomas, necessitating diagnostic surgical interventions1,3,4,6,7,8 in 55.7–100% of patients1,6,8,9,10. Therefore, a less invasive diagnostic procedure is desirable.
Lymphocytic alveolitis is indicative of pulmonary lymphoma and can be detected by analyzing bronchoalveolar lavage fluid (BALF)3,11. In most lymphoproliferative disorders, T- and B-lymphocytes constitute > 90% and < 10% of the total BALF lymphocytes, respectively. In pulmonary B-cell lymphomas, bronchoalveolar B-lymphocyte levels increase to more than 10%3,12,13,14, and the clonality of B-lymphocytes, along with rearrangements of the immunoglobulin heavy chain-encoding IGH gene, may contribute to the diagnosis. Rearrangements of the T-cell receptor-encoding TCR gene have been reported to indicate T-cell lymphomas15,16,17,18,19; however, the diagnostic utility of analyzing this biomarker in BALF remains unclear. Rearrangements in the MALT1 gene located on chromosome 18q21 and encoding MALT lymphoma translocation protein 1 are specific for MALT lymphomas; they include IGH/MALT1 translocation and API2/MALT1 fusion between the API2 (apoptosis inhibitor 2) and MALT1 genes20,21. We have previously shown that the detection of MALT1 translocations in BALF cells by fluorescence in situ hybridization (FISH) is specific for pulmonary MALT lymphoma and could be used for diagnostic purposes22.
In this study, we analyzed the feasibility of using BALF for combined detection of lymphocyte clonality based on IGH and TCR rearrangements as well as MALT1 translocations to diagnose pulmonary lymphomas.
Methods
Study design
This prospective multicenter cohort study was conducted in the University of Occupational and Environmental Health, Japan, Wakamatsu Hospital of University of Occupational and Environmental Health, Japan and five related hospitals (Nagasaki University Hospital, Fukuoka University Hospital, Kokura Kinen Hospital, Oita University Hospital, and University of Miyazaki Hospital). The study was performed according to the Declaration of Helsinki and approved by the Ethics Committee of Medical Research, University of Occupational and Environmental Health, Japan (Approval number: H25-109 and H27-094) and by each institutional review board (the Institutional Review Board at Nagasaki University Hospital, the Fukuoka University Hospital Institutional Review Board, the Ethics Committee of Kokura Memorial Hospital, the Ethics Committee of Oita University, and the Ethics Committees of Faculty of Medicine, University of Miyazaki). All adult participants provided written informed consent to participate in this study.
Patients’ clinical and laboratory characteristics
Patients suspected of having pulmonary lymphoma by attending physicians based on their clinical history, laboratory data, and chest high-resolution CT (HRCT) results and admitted to our hospitals between October 2013 to March 2018 were enrolled. For all patients, the data regarding sex, age, smoking history, levels of serum lactate dehydrogenase (LDH) and soluble interleukin 2 receptor (sIL-2R), chest HRCT results, pathological findings, and final diagnosis were collected and analyzed. According to a previous report on the pattern-based classification of pulmonary lesions involved in MALT lymphoma6, lung lesion identified via chest HRCT were categorized into following types: (1) single nodule or solitary ground glass opacity, (2) multiple nodules or multiple and/or diffuse ground glass opacity, (3) single mass or single areas of airspace consolidation, (4) multiple mass or multiple areas of airspace consolidation. Lymphomas were diagnosed and classified according to the 2016 revision of the World Health Organization classification of lymphoid neoplasms23. Each patient’s final diagnosis was based on clinical, laboratory, and pathological evaluations, the opinions of pulmonologists, hematologists, radiologists, and pathologists, and the clinical course.
BALF collection
BALF was obtained using flexible bronchofiberscopy for evaluation and diagnosis before treatment. After adequate local anesthesia with lidocaine, three 50 mL fractions of sterile saline were injected into the most extensively involved pulmonary segment determined by chest HRCT, gently retrieved using a suction syringe, and placed into sterile containers for microbiological and cytological examinations. BALF samples (30 mL) were stored at 4 °C until analysis of IGH and TCR rearrangements (15 mL) and MALT1 translocations (15 mL). Patients from whom sufficient BALF volumes could not be recovered were excluded from the study.
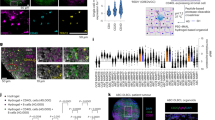
Detection of IGH and TCR rearrangements and MALT1 translocations
IGH and TCR rearrangements in BALF lymphocytes were examined using IdentiClone® IGH and TCRB Gene Clonality Assays (Invivoscribe Technologies, Inc., San Diego, CA, USA)24,25, which detect VH(FR1)/JH, VH(FR2)/JH, VH(FR3)/JH, DH1-6/JH, and DH7/JH regions in IGH and Vβ/Jβ1, Vβ/Jβ2, and Dβ/Jβ regions in TCRB by polymerase chain reaction (PCR) and capillary electrophoresis. When the electrophoresis pattern showed one distinct peak on a low background, which was higher than the peak of positive control (monoclonal pattern), the sample was considered positive, whereas samples with peaks lower than that of positive control or those with several higher peaks without individualization of one peak (oligoclonal pattern) were considered negative13 (Fig. 1). When the monoclonal pattern was observed in at least one of IGH or TCR regions, the gene was considered to have undergone rearrangement.
Examples of case analysis. (A,B) Positive results for the rearrangement of the VH(FR3)/JH region in the IGH gene of BALF lymphocytes. A peak higher than that of the positive control is detected on a low background (monoclonal pattern; A) or several distinct peaks are seen on a polyclonal background (oligoclonal pattern; B). (C) A peak for the positive control. (D,E) Results of MALT1 translocation analysis by FISH. In case of MALT1 translocations, the orange and green signals are separated (D), whereas in a normal cell they are fused (E).
MALT1 translocations were detected using FISH with the MALT1 probe (Vysis MALT1 Break Apart FISH Probe Kit, Abbott Japan, Tokyo, Japan) consisting of a 460-kb 5′-end fragment labeled with SpectrumOrange and a 660-kb 3′-end fragment labeled with SpectrumGreen, as previously described22,26,27,28. Cells with MALT1 translocations would exhibit split orange and green signals (Fig. 1D), whereas normal cells would exhibit fused orange-green signals (Fig. 1E). Hybridized signals for each probe were evaluated in the interphase nuclei of 1,000 cells and positive cut-off values were set at 1.2% based on the analysis of blood samples from 30 healthy subjects performed by LSI Medience Corporation (Tokyo, Japan).
Statistical analyses
The data are presented as the median (range) or the number of patients (%). All calculations were performed using the StatFlex software version 6 (Artech, Osaka, Japan). Continuous variables were compared by the Mann–Whitney U-test with Kruskal–Wallis test, and categorical variables—by chi-square or Fisher's exact tests as appropriate. P < 0.05 was considered to indicate statistical significance.
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki and was approved by the Human and Animal Ethics Review Committee, of the University of Occupational and Environmental Health, Japan (Approval numbers: H25-109 and H27-094) and by each institutional review board. All adult participants provided written informed consent to participate in this study.
Results
Patients’ characteristics
In total, 46 patients were enrolled in the study; however, 5 patients with unconfirmed final diagnoses and 2 with BALF samples inadequate for molecular examination were excluded (Fig. 2). The 39 patients included for further analysis were divided into the B-cell lymphoma group (9 patients: 7 with MALT, 1 with lymphoplasmacytic, and 1 with follicular lymphomas), the lymphoproliferative disorder (LPD) group (12 patients: 5 with interstitial lung diseases due to Sjögren's syndrome, 4 with methotrexate (MTX)-related lymphoproliferative disorders, 2 with sarcoidosis, and 1 with multicentric Castleman’s disease), and the “Others” group (18 patients: 6 with infectious diseases, 5 with interstitial lung diseases, 3 with lung cancer, 1 with vasculitis, 1 with lung involvement in multiple myeloma, 1 with relapsing polychondritis, and 1 with granulomatous lung disease). None of the patients had T-cell lymphomas. The demographic and baseline characteristics of patients in each group are shown in Table 1. There were no significant differences among the groups in age, sex, smoking status, and serum levels of LDH and sIL-2R; median serum sIL-2R levels were higher than normal in all groups. There was no significant difference in chest HRCT findings among the groups in the ratio of hilar and/or mediastinal lymphadenopathy; however, the values of lung nodule and/or ground glass opacity were significantly lower, and the lung mass and/or airspace consolidation were significantly higher in the B-cell lymphoma group than in the LPD group. The median percentage of lymphocytes among BALF cells was increased (more than 10%) in all groups. TBLB was performed in 100%, 91.7%, and 83.3%, and surgical lung biopsy (SLB)—in 33.1%, 16.7%, and 5.5% of patients in the B-cell lymphoma, LPD, and other groups, respectively.
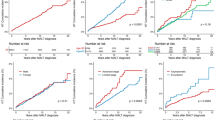
IGH and TCR rearrangements
The total rate of IGH rearrangement was significantly higher in the B-cell lymphoma group (88.9%) than in the LPD group (16.7%, p < 0.01) and the other group (5.5%, p < 0.01) (Fig. 3A). Rearrangements in specific IGH regions (VH(FR1)/JH, VH(FR2)/JH, VH(FR3)/JH, DH1-6/JH, and DH7/JH) are shown in Supplementary Figure S1 and Table S1. The sensitivity, specificity, and positive and negative predictive values of the total IGH rearrangement rate for the diagnosis of B-cell lymphoma were 88.9% 90.0%, 72.7%, and 96.4%, respectively.
TCR rearrangements in BALF cells were evaluated in 6 of 8, 9 of 12, and 15 of 18 patients with B-cell lymphoma, LPD, and other diseases, respectively, and the total rearrangement rates were calculated as 0.0%, 33.3% and 13.3%, respectively (Fig. 3B, Supplementary Figure S2 and Table S2). Although the differences between the groups were not statistically significant, the results indicated that all patients with B-cell lymphoma were negative for TCR rearrangements in BALF cells. The sensitivity, specificity, and positive and negative predictive values of the combination of IGH rearrangement-positive and TCR rearrangement-negative results for the diagnosis of B-cell lymphoma were 100%, 96.0%, 85.7%, and 100%, respectively.
MALT1 translocations
Analysis of MALT1 translocation frequencies in each group indicated that 28.6% (2/7) patients with MALT lymphoma were positive, whereas all other patients, including those with non-MALT B-cell lymphoma, were negative for MALT1 translocation (Fig. 4A). The sensitivity and specificity of MALT1 translocation detection for MALT lymphoma diagnosis were 28.6% and 100%, respectively. The rate of MALT1 translocations among patients with MALT lymphoma was significantly higher than that in the other group (p < 0.05). The proportions of MALT1 translocation-positive lymphocytes in BALF were 30.5% and 10.0% in the 2 positive patients (Fig. 4B) who also had IGH rearrangements (Table 2). These 2 patients, as well as 6 of 9 patients with B-cell lymphomas (66.7%), could be diagnosed without SLB.
Discussion
This is the first study to analyze the diagnostic utility of IGH and TCR rearrangements in clonality analyses in addition to MALT1 translocation in BALF of patients with clinically suspected pulmonary lymphoma. In our study, the sensitivity and specificity of IGH rearrangement results for B-cell lymphoma diagnosis were 88.9% and 90.0%, respectively. All patients with B-cell lymphoma were negative for TCR rearrangements, and the specificity of combined IGH rearrangement-positive and TCR rearrangement-negative results for the B-cell lymphomas diagnosis was 96.0%. The sensitivity and specificity of MALT1 translocation testing for MALT lymphoma diagnosis were 28.6% and 100%, respectively. These findings suggest that the combined detection of IGH and TCR rearrangements in BALF cells is useful for the screening and diagnosis of B-cell lymphomas and that analysis of specific genes such as MALT1 can improve diagnostic accuracy.
It is difficult to detect pulmonary lymphomas using small tissue samples obtained by TBLB or CT-guided lung biopsy, and 55.7–100% of patients need surgical interventions for definitive diagnosis1,6,8,9,10. In a retrospective review of 24 patients with pulmonary lymphomas, only 3 of 13 patients with pulmonary MALT lesions underwent complete surgical resection, whereas the others received chemotherapy9. In another retrospective study of 61 patients with pulmonary MALT lymphomas, no differences were observed in the time to progression between patients who underwent invasive surgical resection and those who received chemotherapy8. Thus, the development of molecular methods that enable diagnosis using small tissue samples is essential to help avoid invasive procedures. In the present study, 66.7% of patients with B-cell lymphomas were diagnosed without SLB, including 2 patients positive for both IGH rearrangements and MALT1 translocations, indicating that the combined detection of these genetic aberrations can provide a more accurate diagnosis through a less invasive procedure.
The usefulness of detecting IGH rearrangements in BALF cells has already been assessed in several studies. Thus, it was shown that PCR analysis of IGH rearrangements in patients with B-cell pulmonary lymphomas was sensitive (6 of 7 patients) and specific (0 of 9 control individuals)12. Positive results were also obtained in 83% and 82% of patients with B-cell and MALT lymphomas at 90% and 97% specificity, respectively13,14. In the present study, we observed a similar sensitivity (88.9%) and specificity (90.0%) of IGH rearrangement detection for B-cell lymphoma diagnosis. We also analyzed TCR rearrangements using the TCRB clonal assay, which is considered a standard lymphoma diagnostic tool in Europe, detecting clonal TCRB rearrangements in 39.3–91.0% of T-cell lymphomas and in 3.8–16.0% of B-cell lymphomas16,17,18,19. In the present study, TCR rearrangements were absent in BALF cells of patients with B-cell lymphomas but present in 33.3% and 13.3% of patients with LPD and other diseases, respectively. Unfortunately, we did not analyze patients with T-cell pulmonary lymphoma because of its rarity. Our results revealed that the presence of IGH rearrangements combined with the absence of TCR rearrangements had 96% specificity for the diagnosis of B-cell lymphoma. Multiple analysis methods are employed in the diagnosis of lymphomas, such as clonality analyses, pathological findings, genetic profiles, and other clinical and laboratory findings. However, these tests are insufficient to confirm lymphoma and identify its subtype. Detection of IGH and TCR rearrangements may be a valuable diagnostic avenue for detection of pulmonary lymphoma. Unexpectedly, 75% of patients with MTX-related LPD exhibited clonal patterns (Supplementary Table S2), suggesting that TCR rearrangements may also be useful for diagnosing MTX-related LPD. Further studies are needed to evaluate the utility of TCR rearrangement testing in BALF cells for pulmonary T-cell lymphoma diagnosis.
Chromosomal translocations associated with MALT lymphoma include API2/MALT1, IGH/MALT1, BCL10/IGH, and trisomy 3 and 1814,23,27. The API2/MALT1 translocation was detected in 30–70% of MALT lymphoma lung tissues obtained by SLB20,21,27,28,29, whereas the IGH/MALT1 translocation was observed in 6–10% of patients with MALT lymphoma27,28. The probe for MALT1 translocation used in the present study detected both API2/MALT1 and IGH/MALT1 translocations, and the MALT1 translocation rate in patients with pulmonary MALT lymphomas observed here (28.6%) was consistent with previous reports20,21,27,28,29. Owing to its 100% specificity, the FISH-based detection of MALT1 rearrangements in BALF cells would significantly improve the diagnostic accuracy for MALT lymphomas. Furthermore, the increased detection of genetic aberrations frequently observed in B-cell lymphomas, including BCL2, BCL6, IGH, and MALT1 translocations, should promote the development of lymphoma gene panels for BALF in the era of next-generation sequencing.
Besides clonality and gene translocation testing, phenotyping using various markers such as cluster of differentiation (CD) can be employed to diagnose lymphomas30. In Europe, the detection of rearrangements in heavy and light immunoglobulin chain genes (IGH, IGK, and IGL) and TCR genes (TCRB, TCRD, and TCRG) by PCR is a standard approach used to diagnose B- and T-cell lymphomas16,17,19,31; however, the combination of these gene rearrangements in BALF cells has not been analyzed. The detection of both IGH rearrangements and CD expression in BALF cells has been shown to aid in diagnosing pulmonary B-cell lymphoma: it revealed B-cell clonality as well as an increase in B-cell (CD19- or CD20-positive) lymphocytes to over 10% of total BALF lymphocytes3,12,13,14. Collectively, these data suggest that the combined analysis of disease markers such as clonality, gene translocations, and CD expression in BALF should aid in diagnosing pulmonary lymphomas through a less invasive method.
Conclusions
In conclusion, we evaluated the utility of the combined detection of clonality and MALT1 translocations in BALF for the diagnosis of pulmonary lymphomas. Our results suggest that this combinatorial approach should help in identifying B-cell lymphomas through a less invasive method. Detection of additional genetic aberrations such as MALT1 translocations in BALF cells can further specify the type of pulmonary lymphoma. Future studies should explore other combinatorial tools such as phenotyping along with IGH/TCR rearrangements to screen for pulmonary lymphomas.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- API2:
-
Apoptosis inhibitor 2
- BALF:
-
Bronchoalveolar lavage fluid
- CD:
-
Cluster of differentiation
- CT:
-
Computed tomography
- FISH:
-
Fluorescence in situ hybridization
- HRCT:
-
High-resolution CT
- IGH:
-
Immunoglobulin heavy chain
- LDH:
-
Lactate dehydrogenase
- LN:
-
Lymph node
- LPD:
-
Lymphoproliferative disorder
- MALT:
-
Mucosa-associated lymphoid tissue
- MALT1 :
-
Mucosa-associated lymphoid tissue lymphoma translocation gene 1
- MTX:
-
Methotrexate
- sIL-2R:
-
Soluble interleukin-2 receptor
- SLB:
-
Surgical lung biopsy
- TBLB:
-
Transbronchial lung biopsy
- TCR:
-
T-cell receptor
- TCRB :
-
TCR-beta gene
References
Ferraro, P. et al. Primary non-Hodgkin’s lymphoma of the lung. Ann. Thorac. Surg. 69, 993–997 (2000).
Cardenas-Garcia, J., Talwar, A., Shah, R. & Fein, A. Update in primary pulmonary lymphomas. Curr. Opin. Pulm. Med. 21, 333–337 (2015).
Borie, R. et al. Pulmonary mucosa-associated lymphoid tissue lymphoma revisited. Eur. Resp. J. 47, 1244–1260 (2016).
William, J., Variakojis, D., Yeldandi, A. & Raparia, K. Lymphoproliferative neoplasms of the lung: A review. Arch. Patho Lab. Med. 137, 382–391 (2013).
Fiche, M. et al. Primary pulmonary non-Hodgkin’s lymphomas. Histopathology 26, 529–537 (1995).
Ahmed, S. et al. Bronchial-associated lymphoid tissue lymphoma: A clinical study of a rare disease. Eur. J. Cancer 40, 1320–1326 (2004).
Bae, Y. A. et al. Marginal zone B-cell lymphoma of bronchus-associated lymphoid tissue: Imaging findings in 21 patients. Chest 133, 433–440 (2008).
Oh, S. Y. et al. Pulmonary marginal zone B-cell lymphoma of MALT type–what is a prognostic factor and which is the optimal treatment, operation, or chemotherapy? Consortium for improving survival of lymphoma (CISL) study. Ann. Hematol. 89, 563–568 (2010).
Kim, J. H. et al. Primary pulmonary non-Hodgkin’s lymphoma. Jpn. J. Clin. Oncol. 34, 510–514 (2004).
Graham, B. B., Mathisen, D. J., Mark, E. J. & Takvorian, R. W. Primary pulmonary lymphoma. Ann. Thorac. Surg. 80, 1248–1253 (2005).
Drent, M. et al. Bronchoalveolar lavage fluid profiles in sarcoidosis, tuberculosis, and non-Hodgkin’s and Hodgkin’s disease. An evaluation of differences. Chest 105, 514–519 (1994).
Philippe, B. et al. B-cell pulmonary lymphoma: gene rearrangement analysis of bronchoalveolar lymphocytes by polymerase chain reaction. Chest 115, 1242–1247 (1999).
Zompi, S. et al. Clonality analysis of alveolar B lymphocytes contributes to the diagnostic strategy in clinical suspicion of pulmonary lymphoma. Blood 103, 3208–3215 (2004).
Borie, R. et al. Clonality and phenotyping analysis of alveolar lymphocytes is suggestive of pulmonary MALT lymphoma. Respir. Med. 105, 1231–1237 (2011).
Hodges, E., Krishna, M. T., Pickard, C. & Smith, J. L. Diagnostic role of tests for T cell receptor (TCR) genes. J. Clin. Pathol. 56, 1–11 (2003).
van Krieken, J. H. et al. Improved reliability of lymphoma diagnostics via PCR-based clonality testing: report of the BIOMED-2 concerted action BHM4-CT98-3936. Leukemia 21, 201–206 (2007).
Evans, P. A. et al. Significantly improved PCR-based clonality testing in B-cell malignancies by use of multiple immunoglobulin gene targets. Report of the BIOMED-2 concerted action BHM4-CT98–3936. Leukemia 21, 207–214 (2007).
Chen, Y. L. et al. BIOMED-2 protocols to detect clonal immunoglobulin and T-cell receptor gene rearrangements in B- and T-cell lymphomas in southern Taiwan. Leuk Lymphoma 51, 650–655 (2010).
Kim, Y., Choi, Y. D., Choi, C. & Nam, J. H. Diagnostic utility of a clonality test for lymphoproliferative diseases in Koreans using the BIOMED-2 PCR assay. Korean J Pathol. 47, 458–465 (2013).
Motegi, M. et al. API2-MALT1 chimeric transcripts involved in mucosa-associated lymphoid tissue type lymphoma predict heterogeneous products. Am. J. Pathol. 156, 807–812 (2000).
Okabe, M. et al. API2-MALT1 fusion defines a distinctive clinicopathologic subtype in pulmonary extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. Am. J. Pathol. 162, 1113–1122 (2003).
Kido, T. et al. Detection of MALT1 gene rearrangements in BAL fluid cells for the diagnosis of pulmonary mucosa-associated lymphoid tissue lymphoma. Chest 141, 176–182 (2012).
Swerdlow, S. H. et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 127, 2375–2390 (2016).
van Dongen, J. J. et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: Report of the BIOMED-2 concerted action BMH4-CT98-3936. Leukemia 17, 2257–2317 (2003).
Sandberg, Y. et al. BIOMED-2 multiplex immunoglobulin/T-cell receptor polymerase chain reaction protocols can reliably replace Southern blot analysis in routine clonality diagnostics. J. Mol. Diagn. 7, 495–503 (2005).
Akagi, T. et al. A novel gene, MALT1 at 18q21, is involved in t(11;18) (q21;q21) found in low-grade B-cell lymphoma of mucosa-associated lymphoid tissue. Oncogene 18, 5785–5794 (1999).
Streubel, B. et al. Variable frequencies of MALT lymphoma-associated genetic aberrations in MALT lymphomas of different sites. Leukemia 18, 1722–1726 (2004).
Remstein, E. D. et al. The incidence and anatomic site specificity of chromosomal translocations in primary extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) in North America. Am. J. Surg. Pathol. 30, 1546–1553 (2006).
Yonezumi, M. et al. Detection of AP12-MALT1 chimaeric gene in extranodal and nodal marginal zone B-cell lymphoma by reverse transcription polymerase chain reaction (PCR) and genomic long and accurate PCR analyses. Br. J. Haematol. 115, 588–594 (2001).
Harris, N. L. et al. New approaches to lymphoma diagnosis. Hematol. Am. Soc. Hematol. Educ. Program 1, 194–220 (2001).
Droese, J. et al. Validation of BIOMED-2 multiplex PCR tubes for detection of TCRB gene rearrangements in T-cell malignancies. Leukemia 18, 1531–1538 (2004).
Acknowledgements
We thank LSI Medience Corporation for outsourcing the contract for the detection of IGH and TCR rearrangement and MALT1 translocation, and Mr. Osamu Takeyama and Ryouta Kukimoto (LSI Medience Corporation) for contributing to the outsourcing contract agreement. We would also like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported by JSPS KAKENHI (Grant number 15K09201) and The Japanese Foundation for Research and Promotion of Endoscopy grant. It was also partially supported by the Practical Research Project for Rare Intractable Diseases, the Japan Agency for Medical Research and Development (AMED), and a grant from the Ministry of Health, Labour and Welfare of Japan awarded to the study group working on diffuse pulmonary disorders and scientific research on intractable diseases.
Author information
Authors and Affiliations
Contributions
T. Kido, H.M., and K.Y. were involved in the conceptualization process, and T. Kido was responsible for data curation and formal analysis. Investigations were performed by T. Kido, H. Ishimoto, H. Ishii, K.H., H.K., M.O., T. Kawanami., Y.S., H.Y., A.H., N.S., N.M., C.Y., J.F., M.F., M.N., J.K., and K.Y. The methodology to be used was decided by T. Kido and K.Y. T. Kido, H.M., and K.Y. were responsible for project administration. T. Kido, N.S., and K.Y. wrote the original of the manuscript. T. Kido, H. Ishimoto, H. Ishii, K.H., H.K., M.O.,T. Kawanami, Y.S., H.Y., A.H., N.S., N.M., C.Y., J.F., M.F., M.N., J.K., and K.Y. reviewed and edited the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kido, T., Ishimoto, H., Ishii, H. et al. Combined detection of lymphocyte clonality and MALT1 translocations in bronchoalveolar lavage fluid for diagnosing pulmonary lymphomas. Sci Rep 11, 23430 (2021). https://doi.org/10.1038/s41598-021-02861-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-021-02861-4