Abstract
Evidence suggests that tumor cells and tumor-infiltrating lymphocytes (TILs) compete for glucose in the tumor microenvironment and that tumor metabolic parameters correlate with localized immune markers in several solid tumors. We investigated the relationship of the standardized uptake value (SUV) of 18F-fluorodeoxyglucose positron emission tomography computed tomography (18F-FDG-PET-CT) with stromal TIL levels in breast cancer. We included 202 patients who underwent preoperative 18F-FDG-PET-CT and had a tumor measuring ≥ 1 cm. Maximum SUV (SUVmax) was determined using 18F-FDG-PET-CT. Multiple logistic regression was used to identify factors related to high TIL levels (≥ 40%). All tumors were treatment naïve. A significant and weak correlation existed between continuous SUVmax and continuous TIL levels (p = 0.002, R = 0.215). Tumors with high SUVmax (≥ 4) had higher mean TIL levels than those with low SUVmax (< 4). In multivariable analysis, continuous SUVmax was an independent factor associated with high TIL levels; each 1-unit increment in SUVmax corresponded to an odds ratio of 1.14 (95% confidence interval: 1.01–1.29) for high TIL levels. Our study implies that SUV is associated with TILs in breast cancer and provides clinical evidence that elevated glucose uptake by breast tumors can predict the immune system-activated tumor micromilieu.
Similar content being viewed by others
Introduction
The tumor microenvironment (TME) is an ensemble of non-tumor cells including immune cells, fibroblasts, and endothelial cells1 and affects tumor development and progression through dynamic interactions with cancer cells2. Identification of TME interplays depending on the tumor’s metabolic activity has revealed that the TME regulates tumor metabolism3. A previous study has reported that the demand for glucose is increased in tumor cells and tumor-specific immune cells, and this competition for glucose uptake between tumor cells and immune cells can directly influence cancer progression4.
Tumor-infiltrating lymphocytes (TILs) are a cellular component of the immune system in the TME. Several clinical trials have reported the prognostic and predictive importance of TILs in breast cancer. In these trials, TIL levels have been highlighted as a biomarker for predicting treatment response to chemotherapy in patients with breast cancer5,6,7,8. The studies also found that tumors with high TIL levels have shown favorable prognosis among triple negative breast cancer (TNBC) or human epidermal growth factor receptor-2 (HER2)-positive breast cancer7,9,10,11,12. Furthermore, high TIL levels are associated with high-proliferative, high-grade, estrogen receptor (ER)-negative tumors and higher pathologic complete response (pCR) rates8,13,14,15,16,17.
18F-fluorodeoxyglucose-positron emission tomography-computed tomography (18F-FDG-PET-CT) provides important tumor-related qualitative and quantitative information on cancer based on glucose metabolism18. For breast cancer, a high maximum standardized uptake value (SUVmax) is related to tumor aggressiveness, advanced stage, and poor prognosis19,20,21,22,23.
To identify the relationship between tumor metabolic status and tumor immunogenicity, recent studies have reported the correlations between SUVmax and immune markers in gastric cancer, non-small cell lung cancer, and breast cancer24,25,26,27,28,29. In this study, we aimed to explore the correlation between the SUVmax of 18F-FDG-PET-CT and stromal TIL levels in breast cancer.
Results
Baseline characteristics
The characteristics of the 202 patients included in this study are summarized in Table 1. The median patient age was 53.2 years. Most tumors were invasive ductal carcinoma (86.1%) and showed favorable biology such as histological grade I or II (77.2%), nuclear grade 1 or 2 (66.3%), luminal/HER2(−) (71.8%), and low Ki-67 labeling index (L.I.) (55.0%). More than half of the tumors had a small tumor burden; 58.4% tumors had T stage 1 and 73.3% tumors were node-negative. The median SUVmax was 4.68, and the median TIL level was 15%.
Tumor characteristics related to TIL levels
We evaluated the correlation between continuous TIL levels and continuous SUVmax using Pearson’s correlation analysis (Fig. 1). There was a significant and weak correlation between continuous SUVmax and continuous TILs (p = 0.002, Pearson’s r = 0.215).
Next, we compared mean TILs according to tumor characteristics (Table 2). Invasive ductal carcinoma (IDC) showed significantly higher mean TIL levels than invasive lobular carcinoma or other histological cancer types. The mean TIL levels were higher in tumors with histological grade (HG) III than in those with HG I or II. Similarly, mean TIL levels were higher in tumors with nuclear grade (NG) 3 than in those with NG 1 or 2. Among the subtypes, luminal/HER2(-) tumors showed the lowest mean TIL levels. When divided by Ki-67 L.I. of 14%, tumors with high Ki-67 L.I. showed higher mean TIL levels than those with low Ki-67 L.I. We also compared mean TIL levels based on the categorized SUVmax with a cutoff value of 420,30. Tumors with a high SUVmax value showed higher mean TIL levels than those with a low SUVmax value (p = 0.028, Mann–Whitney U test).
Predictive factors for tumors with high TIL levels
We identified factors predicting TIL levels ≥ 40% using logistic regression analysis (Table 3). In univariable analysis, the significant variables were age, HG, NG, tumor subtypes, Ki-67 L.I., androgen receptor (AR) percentage, and continuous SUVmax. Because the tumor subtypes were decided based on a combination of estrogen receptor (ER), progesterone receptor (PR), and HER2 status, only tumor subtype was included in the multivariable model to avoid collinearity of variables. In multivariable analysis, tumor subtypes and continuous SUVmax remained an independent variable associated with high TIL levels, and NG was marginally significant (p = 0.050) for predicting high TIL levels. When the SUVmax increased by 1 unit, the probability of high TIL levels increased by 14% (95% confidence interval [CI]: 1.011–1.285, p = 0.032).
Additionally, to evaluate the predictive ability of continuous SUVmax for TIL levels ≥ 40%, we determined the area under the curve (AUC) using receiver operating characteristic (ROC) curves. The ROC curve for SUVmax in relation to TIL levels yielded an AUC of 0.673 (95% CI: 0.582–0.764, p = 0.001; Fig. 2).
Discussion
In this study, we found an association between TIL levels and SUVmax in breast cancer (≥ 1 cm). Tumors with a high SUVmax value showed a higher mean TIL level than those with a low SUVmax value and there was a correlation between continuous SUVmax and TIL level. In multivariable analysis, SUVmax was an independent factor for predicting tumors with high TIL levels.
Correlations between SUVmax and TIL levels have been previously reported in non-small cell lung cancer and gastric cancer. In non-small cell lung cancer, SUVmax was correlated with CD8(+) TILs as well as CD163(+) tumor-associated macrophages, FoxP3(+) Treg cells, and PD-1(+) and PD-L1(+) cells24. In gastric cancer, SUVmax showed a marginal association with CD3(+) lymphocytes and a significant association with FoxP3(+) Treg cells25. In breast cancer, the relationship between SUVmax and TIL levels has been addressed in recent studies. Sasada et al. investigated this relationship using both whole-body positron emission tomography (PET) and dedicated breast PET (DbPET)29. SUVmax correlated with TILs in both whole-body PET and DbPET, and only DbPET was related to TIL levels after propensity score matching analysis. They suggested that DbPET could be more accurate in assessing fluorodeoxyglucose uptake in breast cancer, and their findings are in line with our finding that SUVmax is associated with TIL levels. Collectively, the abovementioned studies support our findings and suggest that SUVmax could have a potential role in assessing the immune system-activated tumor micromilieu.
In addition, these findings indicate that SUVmax can be a potential biomarker associated with immune-targeting therapy. In the study conducted by Hirakata et al.26, there were significant associations between SUVmax and PD-L1(+) TIL levels and between SUVmax and TIL levels. Since PD-L1 expression in immune cells has already been used in clinical practice to determine the use of atezolizumab as an anti-PD-L1-targeting monoclonal antibody in metastatic breast cancer31,32, it is worthwhile to address the predictive function of SUVmax in relation to the response of immune-check point inhibitors (ICIs).
Moreover, our previous genomic study revealed that Transforming growth factor (TGF) pathway genes, which attenuate the response to ICIs33, were significantly downregulated in tumors with a high SUV value34. Further, we found that the SUV signature was significantly associated with ICI responsiveness and improved overall survival in patients with urothelial cancer treated with ICIs. Taken together, our findings provide evidence that SUVmax can be assessed in terms of ICI responsiveness in breast cancer.
Our study has several limitations. First, this was a retrospective study conducted in a single institution, and there was a difference between patient characteristics, especially tumor subtypes. Because we excluded patients who received neoadjuvant chemotherapy, there were a small number of cases with more aggressive tumor types (HER2(+) or TNBC) and advanced disease. To overcome this, multivariable analysis was performed to demonstrate the independent capability of SUVmax in predicting high TIL levels. Second, although we used previously reported cutoff values for TIL levels and SUVmax, there are no standard cutoff values. Third, more specific immune biomarkers such as PD-L1 or the subpopulations of TILs were not assessed. A more detailed analysis is needed to comprehensively understand the mechanism underlying the relationship between TIL levels and SUVmax. Lastly, survival analysis was not performed due to the short follow-up period. Assessment of clinical outcomes could be helpful in identifying the prognostic capability of this relationship. Despite these shortcomings, our study has the advantage of enrolling the largest number of patients thus far.
In conclusion, we found associations between the SUVmax of 18F-FDG-PET-CT and stromal TIL levels in breast cancer. These results suggest that elevated glucose uptake in breast tumors can be used to predict the activation of the immune system in the TME. Further studies are warranted to comprehensively understand the interactions between the immune and metabolic systems in the TME and identify the clinical role of SUVmax of 18F-FDG-PET-CT in predicting TIL levels.
Methods
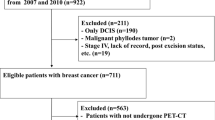
Patients
Between August 2016 and December 2017, we enrolled 202 patients with stage I-III breast cancer who underwent preoperative 18F-FDG-PET-CT followed by primary surgery at Gangnam Severance Hospital, Yonsei College of Medicine, South Korea. In these patients, we successfully evaluated the SUVmax values and stromal TIL levels. To circumvent the effect of chemotherapy on SUVmax values and TIL levels, patients who underwent preoperative chemotherapy were excluded. To address more clear relationship between SUVmax and stromal TIL levels by reducing the partial-volume effect of PET35, we included only patients with tumors measuring ≥ 1 cm.
Clinical data on age at the time of surgery, HG, NG, tumor size, ER status, PR status, HER2 status, AR percentage, and Ki-67 L.I. were collected from the medical database. Tumors were classified according to the tumor–node–metastasis staging of the American Joint Committee on Cancer, 7th edition, and tumor grade was determined using the modified Scarf-Bloomer-Richardson grading system36. The study was approved by the Institutional Review Board (IRB) of Gangnam Severance Hospital (Local IRB number: 2020-0950-001), which waived the requirement of informed consent due to the retrospective study design. The study was performed in accordance with good clinical practice guidelines and the Declaration of Helsinki.
Assessment of TIL levels
TIL levels were measured as described in previous studies37,38. A pathologist (Y.J.C.) performed hematoxylin and eosin staining to review the histological features of treatment-naïve surgical specimens. Stromal TIL levels were evaluated according to the standardized methodology proposed by the international TIL Working Group11. The tumor area, defined by the presence of invasive tumor cells, was identified. All mononuclear cells including lymphocytes and plasma cells, but not polymorphonuclear leukocytes, were counted. The areas outside the tumor border, around the intraductal component, and around the normal lobules were excluded. Within the tumor border, areas showing crush artifacts and necrosis were also excluded. For each case, the average TIL level was measured using a representative section of the whole tumor, and the average level was reported as a percentage.
In this study, the cutoff value of high TIL level was set as 40%, which was used to analyze associations between TIL levels and pathological CR (pCR) or event-free survival in the NeoALTTO study39.
18F-FDG-PET-CT estimation
The procedure for 18F-FDG-PET-CT was the same as that previously reported20. After at least 8 h of fasting, patients received an intravenous injection of 18F-FDG (0.14 MBq) in the arm contralateral to the primary tumor. Sixty minutes after injection of 18F-FDG, whole-body positron emission tomography scans were obtained using a Philips Allegro PET camera (Philips Medical Systems, Cleveland, OH, USA). During the scans, patients were placed in the supine position with their arms raised. The SUV was calculated by measuring the 18F-FDG uptake by the primary tumor in the region of interest using the following formula: SUV = (maximal radioactivity concentration in the region of interest)/(injected dose/patient’s weight (kg)). The SUV cutoff value of 4 was determined according to previous studies20,30,34.
Statistical analysis
Pearson’s correlation coefficient was calculated to measure the correlation between continuous TIL levels and SUV. According to tumor characteristics, mean TILs levels were compared using the Mann–Whitney U test or Kruskal–Wallis test. The Kolmogorov–Smirnov test was used to test the normal distribution of TIL data. The distributions of nonparametric variables were compared using the Mann–Whitney U test or Kruskal–Wallis test. The clinicopathological factors associated with high TIL levels (≥ 40%) were analyzed using logistic regression analysis. Variables that showed a significant difference (p < 0.10) in univariate analysis were entered in multivariable analysis. To evaluate the ability of continuous SUVmax to predict TIL levels ≥ 40%, we determined the AUC using ROC curves. All statistical tests were two tailed, and p < 0.05 was considered statistical significant. All statistical analyses were performed using SPSS, version 26.0 (SPSS, Chicago, IL, USA).
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Gupta, S., Roy, A. & Dwarakanath, B. S. Metabolic cooperation and competition in the tumor microenvironment: implications for therapy. Front. Oncol. 7, 68. https://doi.org/10.3389/fonc.2017.00068 (2017).
Lu, P., Weaver, V. M. & Werb, Z. The extracellular matrix: a dynamic niche in cancer progression. J. Cell Biol. 196, 395–406. https://doi.org/10.1083/jcb.201102147 (2012).
Reina-Campos, M., Moscat, J. & Diaz-Meco, M. Metabolism shapes the tumor microenvironment. Curr. Opin. Cell Biol. 48, 47–53. https://doi.org/10.1016/j.ceb.2017.05.006 (2017).
Chang, C. H. et al. Metabolic competition in the tumor microenvironment is a driver of cancer progression. Cell 162, 1229–1241. https://doi.org/10.1016/j.cell.2015.08.016 (2015).
Denkert, C. et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 19, 40–50. https://doi.org/10.1016/s1470-2045(17)30904-x (2018).
De Angelis, C. et al. Evaluation of the predictive role of tumor immune infiltrate in patients with HER2-positive breast cancer treated with neoadjuvant anti-HER2 therapy without chemotherapy. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 26, 738–745. https://doi.org/10.1158/1078-0432.Ccr-19-1402 (2020).
Gao, G., Wang, Z., Qu, X. & Zhang, Z. Prognostic value of tumor-infiltrating lymphocytes in patients with triple-negative breast cancer: a systematic review and meta-analysis. BMC Cancer 20, 179. https://doi.org/10.1186/s12885-020-6668-z (2020).
Denkert, C. et al. Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J. Clin. Oncol. 28, 105–113. https://doi.org/10.1200/jco.2009.23.7370 (2010).
Dieci, M. V. et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in two phase III randomized adjuvant breast cancer trials. Ann. Oncol. 26, 1698–1704. https://doi.org/10.1093/annonc/mdv239 (2015).
Mao, Y. et al. The prognostic value of tumor-infiltrating lymphocytes in breast cancer: a systematic review and meta-analysis. PLoS ONE 11, e0152500. https://doi.org/10.1371/journal.pone.0152500 (2016).
Salgado, R. et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann. Oncol. 26, 259–271. https://doi.org/10.1093/annonc/mdu450 (2015).
West, N. R. et al. Tumour-infiltrating FOXP3(+) lymphocytes are associated with cytotoxic immune responses and good clinical outcome in oestrogen receptor-negative breast cancer. Br. J. Cancer 108, 155–162. https://doi.org/10.1038/bjc.2012.524 (2013).
Loi, S. et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02–98. J. Clin. Oncol. 31, 860–867. https://doi.org/10.1200/jco.2011.41.0902 (2013).
Loi, S. et al. Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann. Oncol. 25, 1544–1550. https://doi.org/10.1093/annonc/mdu112 (2014).
Galvez, M. et al. Clinicopathological predictors of long-term benefit in breast cancer treated with neoadjuvant chemotherapy. World J. Clin. Oncol. 9, 33–41. https://doi.org/10.5306/wjco.v9.i2.33 (2018).
Krishnamurti, U., Wetherilt, C. S., Yang, J., Peng, L. & Li, X. Tumor-infiltrating lymphocytes are significantly associated with better overall survival and disease-free survival in triple-negative but not estrogen receptor-positive breast cancers. Hum. Pathol. 64, 7–12. https://doi.org/10.1016/j.humpath.2017.01.004 (2017).
Luen, S. J. et al. Tumour-infiltrating lymphocytes in advanced HER2-positive breast cancer treated with pertuzumab or placebo in addition to trastuzumab and docetaxel: a retrospective analysis of the CLEOPATRA study. Lancet Oncol. 18, 52–62. https://doi.org/10.1016/s1470-2045(16)30631-3 (2017).
Palsson-McDermott, E. M. & O’Neill, L. A. The Warburg effect then and now: from cancer to inflammatory diseases. BioEssays 35, 965–973. https://doi.org/10.1002/bies.201300084 (2013).
Kim, Y. H. et al. The clinical significance of standardized uptake value in breast cancer measured using 18F-fluorodeoxyglucose positron emission tomography/computed tomography. Nucl. Med. Commun. 36, 790–794. https://doi.org/10.1097/mnm.0000000000000330 (2015).
Ahn, S. G. et al. Standardized uptake value of 18F-fluorodeoxyglucose positron emission tomography for prediction of tumor recurrence in breast cancer beyond tumor burden. Breast Cancer Res. 16, 502. https://doi.org/10.1186/s13058-014-0502-y (2014).
Diao, W., Tian, F. & Jia, Z. The prognostic value of SUV(max) measuring on primary lesion and ALN by (18)F-FDG PET or PET/CT in patients with breast cancer. Eur. J. Radiol. 105, 1–7. https://doi.org/10.1016/j.ejrad.2018.05.014 (2018).
Shimoda, W., Hayashi, M., Murakami, K., Oyama, T. & Sunagawa, M. The relationship between FDG uptake in PET scans and biological behavior in breast cancer. Breast Cancer 14, 260–268. https://doi.org/10.2325/jbcs.14.260 (2007).
Mavi, A. et al. The effects of estrogen, progesterone, and C-erbB-2 receptor states on 18F-FDG uptake of primary breast cancer lesions. J. Nucl. Med. 48, 1266–1272. https://doi.org/10.2967/jnumed.106.037440 (2007).
Wang, Y. et al. New insight on the correlation of metabolic status on (18)F-FDG PET/CT with immune marker expression in patients with non-small cell lung cancer. Eur. J. Nucl. Med. Mol. Imag. 47, 1127–1136. https://doi.org/10.1007/s00259-019-04500-7 (2020).
Lee, S., Choi, S., Kim, S. Y., Yun, M. J. & Kim, H. I. Potential utility of FDG PET-CT as a non-invasive tool for monitoring local immune responses. J. Gastric. Cancer 17, 384–393. https://doi.org/10.5230/jgc.2017.17.e43 (2017).
Hirakata, T. et al. FDG uptake reflects breast cancer immunological features: the PD-L1 expression and degree of TILs in primary breast cancer. Breast Cancer Res. Treat. 181, 331–338. https://doi.org/10.1007/s10549-020-05619-0 (2020).
Kajáry, K. et al. Dynamic FDG-PET/CT in the initial staging of primary breast cancer: clinicopathological correlations. Pathol. Oncol. Res. 26, 997–1006. https://doi.org/10.1007/s12253-019-00641-0 (2020).
Murakami, W. et al. Correlation between (18)F-FDG uptake on PET/MRI and the level of tumor-infiltrating lymphocytes (TILs) in triple-negative and HER2-positive breast cancer. Eur. J. Radiol. 123, 108773. https://doi.org/10.1016/j.ejrad.2019.108773 (2020).
Sasada, S. et al. The relationship between ring-type dedicated breast PET and immune microenvironment in early breast cancer. Breast Cancer Res. Treat. 177, 651–657. https://doi.org/10.1007/s10549-019-05339-0 (2019).
Ahn, S. G. et al. [18F]-fluorodeoxyglucose positron emission tomography can contribute to discriminate patients with poor prognosis in hormone receptor-positive breast cancer. PLoS ONE 9, e105905. https://doi.org/10.1371/journal.pone.0105905 (2014).
Schmid, P. et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N. Engl. J. Med. 379, 2108–2121. https://doi.org/10.1056/NEJMoa1809615 (2018).
Schmid, P. et al. Atezolizumab plus nab-paclitaxel as first-line treatment for unresectable, locally advanced or metastatic triple-negative breast cancer (IMpassion130): updated efficacy results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 21, 44–59. https://doi.org/10.1016/s1470-2045(19)30689-8 (2020).
Mariathasan, S. et al. TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 554, 544–548. https://doi.org/10.1038/nature25501 (2018).
Kim, S. K. et al. Genomic signature of the standardized uptake value in (18)F-fluorodeoxyglucose positron emission tomography in breast cancer. Cancers (Basel) https://doi.org/10.3390/cancers12020497 (2020).
Soret, M., Bacharach, S. L. & Buvat, I. Partial-volume effect in PET tumor imaging. J. Nucl. Med. 48, 932–945. https://doi.org/10.2967/jnumed.106.035774 (2007).
Elston, C. W. & Ellis, I. O. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19, 403–410. https://doi.org/10.1111/j.1365-2559.1991.tb00229.x (1991).
Ahn, S. G. et al. Comparisons of tumor-infiltrating lymphocyte levels and the 21-gene recurrence score in ER-positive/HER2-negative breast cancer. BMC Cancer 18, 320. https://doi.org/10.1186/s12885-018-4228-6 (2018).
Cha, Y. J. et al. Comparison of tumor-infiltrating lymphocytes of breast cancer in core needle biopsies and resected specimens: a retrospective analysis. Breast Cancer Res. Treat. 171, 295–302. https://doi.org/10.1007/s10549-018-4842-7 (2018).
Salgado, R. et al. Tumor-infiltrating lymphocytes and associations with pathological complete response and event-free survival in HER2-positive early-stage breast cancer treated with lapatinib and trastuzumab: a secondary analysis of the NeoALTTO trial. JAMA Oncol. 1, 448–454. https://doi.org/10.1001/jamaoncol.2015.0830 (2015).
Funding
This work was supported by funds from the Basic Science Research Program through the NRF (NRF-2019R1C1C1002830), Republic of Korea.
Author information
Authors and Affiliations
Contributions
S.P., C.C., S.J.B., D.K., J.L., J.J., and S.G.A. conceived and designed the study. Y.J.C. was responsible for reviewing the pathology of the surgical specimen. E.M. collected the data. S.P. analyzed the data. S.P., E.M., and S.G.A. interpreted the data. S.P. wrote the manuscript. S.G.A. revised the drafts and the final version of the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, S., Min, Ek., Bae, S.J. et al. Relationship of the standard uptake value of 18F-FDG-PET-CT with tumor-infiltrating lymphocytes in breast tumors measuring ≥ 1 cm. Sci Rep 11, 12046 (2021). https://doi.org/10.1038/s41598-021-91404-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-021-91404-y
This article is cited by
-
Assessment of tertiary lymphoid structures via 18F-FDG PET/CT scan in patients with pancreatic adenocarcinoma
Cancer Immunology, Immunotherapy (2025)
-
Are [18F]FDG PET/CT imaging and cell blood count-derived biomarkers robust non-invasive surrogates for tumor-infiltrating lymphocytes in early-stage breast cancer?
Annals of Nuclear Medicine (2025)
-
Method for co-registration of high-resolution specimen PET-CT with histopathology to improve insight into radiotracer distributions
EJNMMI Physics (2024)
-
Tumor infiltrating lymphocytes and radiological picture of the tumor
Medical Oncology (2023)
-
Radionuclide imaging and therapy directed towards the tumor microenvironment: a multi-cancer approach for personalized medicine
European Journal of Nuclear Medicine and Molecular Imaging (2022)