Abstract
Acute kidney injury (AKI) increases the risk of morbidity, mortality, and progression to chronic kidney disease (CKD). There are few data on the risk of CKD following community-acquired AKI (CA-AKI) and its predictors from developing countries. We evaluated the association of a panel of serum and urine biomarkers at the time of hospital discharge with 4-month renal outcome in CA-AKI. Patients of either sex, aged between 18 and 70 years, with no underlying CKD, and with CA-AKI were recruited at the time of discharge from hospital in this prospective observational study. Levels of serum and urine biomarkers were analyzed and association between these markers and development of CKD, defined as eGFR < 60 ml/min/1.73 m2 or dialysis dependence at 4 month after discharge, were analyzed using multivariate logistic regression analysis and penalized least absolute shrinkage and selection operator logistic regression. Out of a total 126 patients followed up for 4 months, 25 developed CKD. Those who developed CKD were older (p = 0.008), had higher serum creatinine (p < 0.001) and lower serum albumin (p = 0.001) at discharge. Adjusted logistic regression showed that each 10% increase in standardized serum myo-inositol oxygenase (MIOX) level increased the odds of progression to CKD by 13.5%. With 10% increase in standardized urine Neutrophil gelatinase-associated lipocalin (NGAL), serum creatinine and urine protein creatinine ratio (uPCR), increase in the odds of progression to CKD was 10.5%, 9.6% and 8%, respectively. Multivariable logistic model including serum MIOX, discharge serum creatinine and discharge uPCR, was able to predict the progression of CKD [AUC ROC 0.88; (95% CI 0.81, 0.95)]. High level serum MIOX levels at the time of discharge from hospital are associated with progression to CKD in patients with CA-AKI.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a rising global health concern. In developing countries, especially in the in rural areas, AKI frequently develops in community settings in association with infections, envenomation, diarrhea, and is generally more common in the otherwise healthy population1.
Existing literature suggests the role of AKI in increasing the risk of morbidity, mortality, and progression to chronic kidney disease (CKD)2,3. Patients with AKI who had incomplete or non-recovery, had an increased risk of mortality and adverse renal outcomes when compared with fully recovered patients4. The ability to forecast renal recovery in an individual patient will help in clinical decision-making and facilitate clinical research in this field. If the patients who survive AKI and are at an increased risk for progression to CKD can be identified, they can be subjected to better follow-up and their natural history might be impacted favorably5. Improved understanding of pathophysiological mechanism of the worsening of AKI could help in developing novel medications that can hamper the progression of AKI and thus improve the long-term outcome of AKI.
Serum creatinine, the currently used marker for AKI, lacks sensitivity and is affected by a number of factors including muscle mass, fluid balance during ICU stay, and decreased production during critical illness6,7. Robust research is ongoing to identify biomarkers for risk assessment, early detection of AKI, prognostication, and prediction of the chance of progression to CKD. The 23rd Acute Disease Quality Initiative Consensus Conference recommends that the biomarkers predictive of CKD progression should be incorporated into a comprehensive post-AKI/acute kidney disease (AKD) care bundle (Grade C recommendation)8. They also suggest that a combination of damage and functional biomarkers, along with clinical information be used to improve patient care and outcomes (Grade C recommendation)8. The FROG-ICU study in 1207 intensive care unit (ICU) patients showed that abnormal values of plasma and urine neutrophil gelatinase-associated lipocalin (NGAL), plasma proenkephalin A and plasma cystatin C at hospital discharge were predictive of higher mortality at 1-year9. Neutrophil gelatinase-associated lipocalin (NGAL), Kidney injury molecule (KIM-1), Liver-type fatty acid-binding protein(L-FABP), Myoinositol oxygenase (MIOX) and Yes-associated protein (YAP) are emerging as important biomarkers for early detection of AKI in various settings and would be logical choices to evaluate for prediction of recovery from AKI10,11,12,13,14,15. New interest has been seen in the field of Nicotinamide adenine dinucleotide (NAD+) biosynthesis. Urinary quinolinate /tryptophan ratio(uQ/T), indicative of reduced quinolinate phosphoribosyltransferase (QPRT), an enzyme involved in NAD+ biosynthesis, was found to predict AKI and other adverse outcomes in animal studies and in critically ill patients16.
There is little research, however in the utility of these biomarkers in community-acquired AKI (CA-AKI) in developing countries. In this study, we evaluated the association of a panel of serum and urine biomarkers (MIOX, YAP, NGAL, KIM-1, LFABP1 and urinary quinolinate/tryptophan ratio) at the time of hospital discharge with the renal outcomes at 4 months in CA-AKI.
Results
A total of 1,453 patients with a diagnosis of AKI were screened between February 2017 and January 2020. After excluding 1203 patients, 250 patients were enrolled. A total of 124 patients died or were lost to follow-up, leaving 126 patients for the final analysis (Fig. 1). The mean age of study participants was 37.23 ± 15.20 years and 43.7% were females. 93.7% of patients were in stage 3 of AKI. The main cause of CA-AKI was infection (47%) followed by obstetric (16%), envenomation (14%), over the counter or indigenous drug related (7%), and other causes (16%). Infections included acute gastroenteritis (37%), undifferentiated acute febrile illness (27%), urinary tract infection (10%), scrub typhus (9%), leptospirosis (5%), malaria (5%) and others (7%). Out of 126 patients, progression to CKD at 4 months was observed in 19.84% (n = 25).
The patient characteristics including laboratory investigations are shown in Tables 1 and 2. Patients who progressed to CKD were older (44.40 ± 15.32 vs 35.46 ± 14.72 years, p = 0.008), had longer duration of hospitalization (16.40 ± 9.02 vs 12.29 ± 9.45 days, p = 0.052), and had higher serum creatinine (p < 0.001), and lower serum albumin at discharge (p = 0.001). Further, uPCR at the time of hospital discharge was higher in these patients as compared to recovered patients [896 (317, 2128) vs 232 (131, 588) mg/gm, p < 0.001].
Biomarkers and recovery from CA-AKI
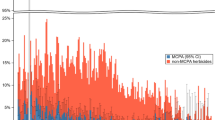
The serum and urine biomarkers at the time of hospital discharge have been tabulated in Table 2 and Fig. 2. Urine biomarker values were normalized using spot urine creatinine concentration. Serum MIOX was higher in patient who progressed to CKD [4995 (3280, 6107) vs 3005 (2221, 3807) pg/ml, p < 0.001]. High level of urine NGAL/creatinine [159.75 (51.26, 357.69) vs 44.93 (15.32, 116.14) ng/g, p < 0.001] and uPCR [896 (317, 2128) vs 232 (131, 588) mg/g, p < 0.001] whereas low urine LFABP/creatinine [10.98 (5.24, 287.11) vs 274.79 (7.50, 911.97) ng/g, p = 0.035] was also noted in these subjects as compared to patient who recovered from AKI. There was no statistically significant difference between groups with regards to urinary MIOX level, serum and urinary YAP levels, urine KIM-1 and quinolinate to tryptophan ratio (uQ/T) (Table 2).
Box and whisker plot showing the levels of serum and urine biomarkers in recovered patients and those who progressed to CKD from CA-AKI. sMIOX serum myo-inositol oxygenase, uMIOX urine myo-inositol oxygenase, sYAP serum Yes-associated protein, uYAP urine Yes-associated protein, uKIM-1 urine kidney injury molecule-1, uNGAL urine neutrophil gelatinase-associated lipocalin, uL-FABP urine liver-type fatty acid binding protein, uPCR urine protein creatinine ratio, sCr serum creatinine, Cr; creatinine.
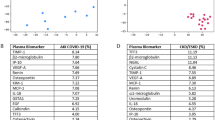
Unadjusted logistic regression analysis showed that a 10% increase in standardized serum MIOX level increased the odds of progression to CKD by 12.8% [OR 3.58, 95% CI (1.84, 6.96), p < 0.001]. With every 10% increase in standardized urine NGAL [OR 2.69, 95% CI (1.56, 4.63), p < 0.001], and standardized serum creatinine [OR 2.69 95% CI (1.54, 4.69), p < 0.001], the odds of progression to CKD increased by 9.8%. For 10% increase in standardized uPCR [OR 2.61 95% CI (1.61, 4.23), p < 0.001] level, odds of progression to CKD rose by 9.5%. (Table 3).
After adjusting with age, sex, hypertension, diabetes, requirement of kidney replacement therapy (KRT), quick sequential organ failure assessment (qSOFA) score, and duration of hospitalization; serum MIOX, urinary NGAL, serum creatinine and uPCR were independently associated with progression to CKD (Table 4). 10% increase in standardized serum MIOX level increased the odds of progression to CKD by 13.5% [OR 3.81, 95% CI (1.66, 8.73)]. With 10% increase in standardized urine NGAL level [OR 2.88, 95% CI (1.39, 5.99)], and standardized serum creatinine level [OR 2.63, 95% CI (1.30, 5.31)], increase in the odds of progression to CKD was 10.5% and 9.6%, respectively. For standardized uPCR [OR 2.27, 95% CI (1.29, 3.98)], 10% increase in its level would rise odds of progression to CKD by 8%.
Penalized LASSO logistic regression with AKI to CKD progression as the outcome and all serum and urine biomarkers plus other parameters including age, sex, diabetes, hypertension, qSOFA score, requirement of KRT, and hospital duration as potential predictors resulted in a final model containing age, sex, hypertension, hospital duration, serum MIOX, discharge uPCR, and discharge serum creatinine. Linear predictor values for all study subjects were calculated using the intercept and coefficients from the multivariable model (shown in Supplementary Table 1). Finally, the logistic regression model was fit for only the select variables obtained from penalized LASSO regression to assess the association with progression to CKD. The ROC-AUC of the multivariable logistic model with selected parameters was 0.88; (95% CI 0.81, 0.95) and was significantly greater than those of any of the 3 variables analysed individually; serum MIOX (AUC 0.85; 95% CI 0.78, 0.93), discharge serum creatinine (AUC = 0.85; 95% CI = 0.87, 0.92) and discharge uPCR (AUC 0.83; 95% CI 0.74, 0.91) (Fig. 3).
Discussion
In this first of its kind prospective cohort study of patients with CA-AKI from a developing country, we show that serum MIOX, urine NGAL, serum creatinine and uPCR at the time of discharge were independently associated with progression to CKD from CA-AKI after adjusting for gender, age, hypertension, diabetes, requirement of renal replacement therapy and duration of hospitalization. Further, in multivariable model using penalized LASSO regression with selected variables, serum MIOX, serum creatinine and uPCR remained independent predictors of CKD progression from CA-AKI and multivariable model including these three markers performed better as compared to individual markers in LASSO regression analysis.
In the panel of analyzed biomarkers, serum MIOX was the only one that remained independent predictor of CKD progression from CA-AKI along after multivariable regression analysis as well as in the multivariable predictive model. MIOX is a monomeric renal-specific proximal tubule protein that oxidizes myo-inositol to glucuronic acid17,18. High levels of serum MIOX has been associated with AKI, and levels of serum MIOX increased even before the rise in serum creatinine suggestive of markers for detection of AKI11,12. A recent study investigated the effectiveness of MIOX in the early diagnosis in ischemia–reperfusion mice models and found increased serum MIOX levels in the early stages of AKI19. In another study, overexpression of MIOX led to worsening of AKI in cisplatin-induced injury, and disruption in MIOX gene seemed to be protective against cisplatin-induced AKI20, Further, in type 2 diabetic nephropathy (T2DN), expression of MIOX correlates with tubulointerstitial damage21 A few studies have explored pathways that might explain the mechanism of the role of MIOX in AKI-CKD progression. In vitro overexpression of MIOX triggers production of inflammatory cytokines and generation of reactive oxygen species21. Tominaga et al.22 showed that MIOX-induced oxidative stress linked to tunicamycin-induced endoplasmic reticulum stress may step-up the tubulointerstitial injury. Sharma et al.23 showed that gentamycin induced cellular injury in the AKI is further exacerbated by the overexpression of MIOX. Further, MIOX-mediated redox injury and necroptosis are involved in the pathogenesis of cadmium-induced renal injury24. Another study showed that ferroptosis is modulated by MIOX overexpression in cisplatin-induced AKI25. There are no data, however, on the predictive ability of MIOX for progression to acute kidney disease (AKD) or CKD. In the current study, serum MIOX showed an AUC of 0.85, which suggest that serum MIOX levels can be used to identify patients for whom a closer follow-up after discharge will be needed, as AUC above 0.80 is strongly considered clinically useful26.
In the past, levels of urine and or serum NGAL, KIM and LFABP1 have been explored as a early predictive biomarkers for renal recovery from AKI. Out of these, NGAL has been recognized as a potential candidate biomarker for outcome of AKI in recent reports27,28,29,30 and has received the most attention. In our study high urinary NGAL was independently associated with progression to CKD from CA-AKI in univariate and multivariable logistic regression analysis. These results are similar to the data reported by Srisawat et al., in 181 patients with community acquired pneumonia and AKI. High plasma NGAL level at first day of diagnosis by Risk, Injury, Failure, Loss, and End-stage kidney disease (RIFLE-F) classification, predicted failure to recovery of renal function. Recovery of renal function was defined as being alive at discharge and KRT independence during hospitalization and no persistent RIFLE-F at hospital discharge (AUC 0.71)29. In another study on 76 critically ill AKI patient requiring KRT, the decrease of urinary NGAL from day 1 to day 14 predicted renal recovery (AUC 0.70) defined as being alive and without requirement for dialysis by day 6028. In the study by Moon et in 66 AKI patients, low urinary NGAL at day 0 was able to predict renal recovery (AUC 0.78) (50% or more decrease in plasma creatinine from the maximum level)27. Another study on 145 hospital acquired AKI, elevated levels of urinary NGAL at the time of AKI diagnosis predicted poor long term (6 months) outcome (new onset of end stage kidney disease or all-cause mortality)31.
The timing of biomarker analysis is an important consideration while looking at the value of biomarkers as a predictive tool in AKI survivors. Currently, there is no standardized or appropriate timepoint to measure the biomarkers for prediction of recovery form AKI. The timing of biomarker analysis for prediction of recovery depends on the context of AKI. Levels of biomarkers may be affected by the stages or severity of AKI and may not be accurate in predicting the long-term renal outcome. We investigated the predictive ability of biomarkers at the time of discharge from hospital, as risk stratification is of greatest value when performed at the time of discharge to develop plans for follow up and monitoring32. This allows efficient utilization of resources and reduces waste. Also, we used penalized LASSO logistic regression model to assess the predicting ability of the biomarkers for progression to CKD. As compared to traditional methods, penalised regression methods are preferred when there are far more variables than observations which in turn could raise the issue of multicollinearity and overfitting. This results in shrinking the coefficients of the less contributive variables toward zero and thus removing them from final multivariable model. Another strength of this study is that it is a unique cohort of CA-AKI patients selected with stringent inclusion and exclusion criteria with a complete 4 month follow up.
A few limitations of our study need to be acknowledged, however. They include its single-center observational nature, small sample size; relatively short follow up, and the possibility of an effect of kidney function on the biomarker levels. Most of the patients with AKI were in advanced stage of AKI. Further, this analysis has not been validated in an external cohort.
In conclusion, serum level of MIOX at the hospital discharge could be used as predictive biomarker for renal recovery from community acquired AKI either alone or in multivariable model including serum creatinine and uPCR. The results of this study need validation in larger population of AKI with longer follow up to establish this association and utility of this model in clinical decision making for further stratification of patients at the risk of developing CKD.
Materials and methods
Study setting
This study was a prospective, observational cohort study in patients with CA-AKI conducted in a tertiary care hospital Postgraduate Institute of Medical Education & Research (PGIMER), Chandigarh, India.
Study population
The study was conducted between February 2017 and January 2020. All subjects between the ages of 18 and 70 years admitted at PGIMER and diagnosed to have AKI at any time during hospital stay and discharged from hospital were eligible for screening. CA-AKI was defined as established AKI at the time of admission or AKI developed withing 48 h of initial contact with health care services. Patients with pre-existing CKD, and a diagnosis of glomerulonephritis, obstructive uropathy, malignancies, decompensated chronic liver disease, heart failure, or who had received solid-organ or bone marrow transplants were excluded. Lastly, patients who had a high likelihood of re-hospitalization or death in the following 4 months were also excluded. The study was approved by Institute Ethics Committee of PGIMER, Chandigarh, India, and informed consent was obtained from each patient before enrolment in this study. All experiments were performed in accordance with relevant guidelines and regulations.
Study procedure and follow-up
Baseline characteristics including demographic details, comorbidities, markers of severity of AKI including dialysis details, and laboratory data were collected. Blood and urine samples were collected at the time of discharge from hospital and stored at − 80 °C for analysis of serum and urine biomarkers MIOX and YAP, urine NGAL, KIM1, L-FABP, urine quinolinate and tryptophan levels and spot urine protein creatinine ratio (uPCR). The patients were followed up at 4 months after hospital discharge for assessment of renal outcome.
Measurement of biomarkers
Levels of MIOX and YAP in serum were measured using ELISA kits by USCN Life Science Inc., Wuhan, Hubei, China, and MyBioSource Inc., San Diego, CA, USA, respectively. MIOX and YAP concentrations in urine samples were measured using ELISA kits by Bioassay Technology Laboratory, Yangpu, Shanghai, China. Urinary NGAL and KIM-1 were measured by Quantikine® ELISA kits (R&D Systems, Inc., Minneapolis, MN, USA). Urinary L-FABP, was measured using ELISA kit by Elabscience, Houston, TX, USA.
Measurement of quinolinate and tryptophan in spot urine samples was done by high-performance liquid chromatography (HPLC) method using UltiMate 3000 UHPLC (Thermo Fisher Scientific Inc., Waltham, MA USA). Samples were thawed and 300 μL sample was taken in a 1.8 mL tube. Samples were then vortexed strongly for 1 min. 300 μL of 100% ethanol was then added to the sample followed by strong vortex for 30 s. The samples were then incubated at − 20 °C for 20 min followed by centrifugation at 12,000×g for 20 min at 4 °C. Finally, 100 μL of supernatant was taken carefully and transferred to new vials and 20 μL of volume was injected for HPLC analysis under the following conditions: flow rate: 1 mL/min; injection volume: 20 μL; UV HPLC range: 210 nm; running time: 10 min; machine temperature: 30 °C. Standards for tryptophan and quinolinate were also run along with the samples and were used for analyse the levels of tryptophan and quinolinate in urine samples.
Study outcome
Study outcome was progression to CKD from CA-AKI at 4 months after hospital discharge. Renal recovery was defined as eGFR (CKD EPI-2009) > 60 ml/min/1.73 m2 and spot urine protein to creatinine ratio (uPCR) < 500 mg/g. Patients who had eGFR < 60 ml/min/1.73 m2 or were dialysis dependent at 4 month after discharge were defined as having progressed to CKD.
Statistical considerations
Descriptive statistics was used to describe the baseline demographic and clinical characteristics of study subjects. Continuous data were presented as mean ± standard deviation (SD) or median (25th, 75th percentile), and categorical data were presented as frequency (percentage). To compare continuous data, student t-test or Mann–Whitney U test was performed. Categorical data was compared using the chi-square or Fisher exact test. Association between CKD progression and each biomarker was assessed separately using logistic regression. Adjusted logistic regression was used to study whether biomarker is independently associated with progression to CKD, after adjusting for other clinical parameters and demographic variables. Penalized least absolute shrinkage and selection operator (LASSO) logistic regression model was performed on all serum and urine biomarkers to do variable selection. Finally, multivariable logistic regression was fit for only select variables obtained from penalized LASSO model to assess their association with progression to CKD. Receiver operating characteristic (ROC) curves were plotted for multivariable model including multiple biomarkers in addition to ROC curves for the individual biomarkers. The area under the curve (AUC) values at 95% CI were reported for the multivariable logistic regression model and individual biomarkers. Non-normally distributed continuous variables namely, serum MIOX (pg/ml), serum YAP (pg/ml), urine MIOX/creatinine (pg/g), urine YAP/creatinine (ng/g), urine KIM-1/creatinine (pg/g), urine NGAL/creatinine (ng/g), urine l-FABP/creatinine (ng/g), urine quinolinate/tryptophan (Q/T), uPCR (mg/m), discharge creatinine was standardized log transformed for logistic regression analysis. All P values were two-tailed and considered significant when < 0.05. All analyses were performed using STATA version 22 (IBM Corp., Armonk, NY, USA).
Ethics approval and consent to participate
Study was approved from the Institute Ethics Committee and patients were enrolled in this study after getting the written prior to study procedures.
Consent for publication
Consent form available on request.
Data availability
The data which are presented in this study are available with the corresponding author.
References
Cerda, J., Bagga, A., Kher, V. & Chakravarthi, R. M. The contrasting characteristics of acute kidney injury in developed and developing countries. Nat. Clin. Pract. Nephrol. 4, 138–153. https://doi.org/10.1038/ncpneph0722 (2008).
Chawla, L. S., Amdur, R. L., Amodeo, S., Kimmel, P. L. & Palant, C. E. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int. 79, 1361–1369 (2011).
Ronco, C., Bellomo, R. & Kellum, J. A. Acute kidney injury. Lancet 394, 1949–1964 (2019).
Pannu, N., James, M., Hemmelgarn, B., Klarenbach, S. & Network, A. K. D. Association between AKI, recovery of renal function, and long-term outcomes after hospital discharge. Clin. J. Am. Soc. Nephrol. 8, 194–202 (2013).
Chawla, L. S. & Kimmel, P. L. Acute kidney injury and chronic kidney disease: an integrated clinical syndrome. Kidney Int. 82, 516–524 (2012).
Doi, K. et al. Reduced production of creatinine limits its use as marker of kidney injury in sepsis. J. Am. Soc. Nephrol. 20, 1217–1221 (2009).
Kashani, K. B. et al. Evaluating muscle mass by using markers of kidney function: development of the sarcopenia index. Crit. Care Med. 45, e23–e29 (2017).
Ostermann, M. et al. Recommendations on acute kidney injury biomarkers from the acute disease quality initiative consensus conference: a consensus statement. JAMA Netw. Open 3, e2019209–e2019209 (2020).
Legrand, M. et al. One-year prognosis of kidney injury at discharge from the ICU: A multicenter observational study. Crit. Care Med. 47, e953–e961 (2019).
Chen, J. et al. EGF receptor–dependent YAP activation is important for renal recovery from AKI. J. Am. Soc. Nephrol. 29, 2372–2385 (2018).
Gaut, J. P. et al. Development of an immunoassay for the kidney-specific protein myo-inositol oxygenase, a potential biomarker of acute kidney injury. Clin. Chem. 60, 747–757 (2014).
Mertoglu, C., Gunay, M., Gurel, A. & Gungor, M. Myo–inositol Oxygenase as a novel marker in the diagnosis of acute kidney injury. J. Med. Biochem. 37, 1 (2018).
Kamijo-Ikemori, A. et al. Urinary L-type fatty acid binding protein (L-FABP) as a new urinary biomarker promulgated by the Ministry of Health, Labour and Welfare in Japan. Rinsho byori. Jpn. J. Clin. Pathol. 61, 635–640 (2013).
Shao, X. et al. Diagnostic value of urinary kidney injury molecule 1 for acute kidney injury: a meta-analysis. PLoS ONE 9, e84131 (2014).
Haase, M. et al. Accuracy of neutrophil gelatinase-associated lipocalin (NGAL) in diagnosis and prognosis in acute kidney injury: A systematic review and meta-analysis. Am. J. Kidney Dis. 54, 1012–1024 (2009).
Poyan Mehr, A. et al. De novo NAD+ biosynthetic impairment in acute kidney injury in humans. Nat. Med. 24, 1351–1359 (2018).
Hankes, L., Politzer, W., Touster, O. & Anderson, L. Myo-inositol catabolism in human pentosurics: the predominant role of the glucuronate-xylulose-pentose phosphate pathway. Ann. N. Y. Acad. Sci. 165, 564–576 (1970).
Charalampous, F. C. Biochemical studies on inositol: V. purification and properties of the enzyme that cleaves inositol to d-glucuronic acid. J. Biol. Chem. 234, 220–227 (1959).
Mertoglu, C. et al. Effectiveness of myo-inositol oxygenase in the early diagnosis of experimental acute kidney injury. Bratisl. Lek. Listy 121, 565–570 (2020).
Dutta, R. K. et al. Beneficial effects of myo-inositol oxygenase deficiency in cisplatin-induced AKI. J. Am. Soc. Nephrol. 28, 1421–1436 (2017).
Sharma, I., Deng, F., Liao, Y. & Kanwar, Y. S. Myo-inositol oxygenase (MIOX) overexpression drives the progression of renal tubulointerstitial injury in diabetes. Diabetes 69, 1248–1263 (2020).
Tominaga, T. et al. Myo-inositol oxygenase accentuates renal tubular injury initiated by endoplasmic reticulum stress. Am. J. Physiol. Renal Physiol. 316, F301–F315. https://doi.org/10.1152/ajprenal.00534.2018 (2019).
Sharma, I., Liao, Y., Zheng, X. & Kanwar, Y. S. Modulation of gentamicin-induced acute kidney injury by myo-inositol oxygenase via the ROS/ALOX-12/12-HETE/GPR31 signaling pathway. JCI Insight https://doi.org/10.1172/jci.insight.155487 (2022).
Zheng, X., Deng, F., Sharma, I. & Kanwar, Y. S. Myo-inositol oxygenase overexpression exacerbates cadmium-induced kidney injury via oxidant stress and necroptosis. Am. J. Physiol. Renal Physiol. 322, F344–F359. https://doi.org/10.1152/ajprenal.00460.2021 (2022).
Deng, F., Sharma, I., Dai, Y., Yang, M. & Kanwar, Y. S. Myo-inositol oxygenase expression profile modulates pathogenic ferroptosis in the renal proximal tubule. J. Clin. Invest. 129, 5033–5049. https://doi.org/10.1172/JCI129903 (2019).
Hosmer, D. W. Assessing the fit of the model. Appl. Log. Regress. 1, 143–202 (2000).
Moon, S. J., Park, H. B., Yoon, S. Y. & Lee, S. C. Urinary biomarkers for early detection of recovery in patients with acute kidney injury. J. Korean Med. Sci. 28, 1181–1186 (2013).
Srisawat, N. et al. Urinary biomarkers and renal recovery in critically ill patients with renal support. Clin. J. Am. Soc. Nephrol. 6, 1815–1823 (2011).
Srisawat, N. et al. Plasma neutrophil gelatinase-associated lipocalin predicts recovery from acute kidney injury following community-acquired pneumonia. Kidney Int. 80, 545–552 (2011).
Srisawat, N. et al. Neutrophil gelatinase associated lipocalin (NGAL) in leptospirosis acute kidney injury: a multicenter study in Thailand. PLoS ONE 10, e0143367 (2015).
Singer, E. et al. Urinary NGAL-positive acute kidney injury and poor long-term outcomes in hospitalized patients. Kidney Int. Rep. 1, 114–124 (2016).
Silver, S. A. & Sawhney, S. Biomarkers to predict CKD after acute kidney injury: News or noise?. Am. J. Kidney Dis. 79, 620–622 (2022).
Funding
This study was partially supported by the grant from Department of Biotechnology/Wellcome Trust India Alliance (Grant No. IA/CPHI/19/1/504609).
Author information
Authors and Affiliations
Contributions
A.K.Y. and V.K.; conceptualized the study, T.J.K., V.N., J.S.; subjects’ enrolment, J.K., K.K. and P.K.; laboratory experiments, H.S.K., K.L.G., V.K., J.S.; follow up and clinical outcome evaluation, M.K., A.G., A.K.Y.; statistical analysis, T.M., J.K.; manuscript writing, V.K., A.K.Y. and V.J.; supervised the study, reviewed, and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
VJ has received grant funding from GSK, Baxter Healthcare, and Biocon and honoraria from Bayer, AstraZeneca, Boeringer Ingelheim, NephroPlus and Zydus Cadilla, under the policy of all honoraria being paid to the organization. All other authors reported no conflict.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kakkanattu, T.J., Kaur, J., Nagesh, V. et al. Serum myo-inositol oxygenase levels at hospital discharge predict progression to chronic kidney disease in community-acquired acute kidney injury. Sci Rep 12, 13225 (2022). https://doi.org/10.1038/s41598-022-17599-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-17599-w