Abstract
The pathophysiological mechanisms underlying the development of the athlete’s heart are still poorly understood. To characterize the intracavitary blood flows in the right ventricle (RV) and right-ventricular outflow tract (RVOT) in 2 healthy probands, patients with arrhythmogenic right ventricular cardiomyopathy (ARVC) and 2 endurance athletes, we performed 4D-MRI flow measurements to assess differences in kinetic energy and shear stresses. Time evolution of velocity magnitude, mean kinetic energy (MKE), turbulent kinetic energy (TKE) and viscous shear stress (VSS) were measured both along the whole RV and in the RVOT. RVOT regions had higher kinetic energy values and higher shear stresses levels compared to the global averaging over RV among all subjects. Endurance athletes had relatively lower kinetic energy and shear stresses in the RVOT regions compared to both healthy probands and ARVC patients. The athlete’s heart is characterized by lower kinetic energy and shear stresses in the RVOT, which might be explained by a higher diastolic compliance of the RV.
Similar content being viewed by others
Introduction
Extensive training results in repetitive volume and pressure overloads, which are responsible for cardiac remodeling involving both ventricles. The right ventricle (RV) is particularly susceptible to exercise-related hemodynamic variations, thus leading to a structural, functional and electrical remodeling1,2. The morphologic remodeling in the so-called athlete’s heart and the RV alterations described in arrhythmogenic ventricular cardiomyopathy (ARVC) significantly overlap, although the underlying mechanisms significantly differ3. ARVC is a polygenic disease with different penetrance and degree of gravity involving desmosomal mutations4. There is evidence suggesting that intensive exercise may not only accelerate the development of an adverse RV remodeling in affected patients, but may also induce cardiac fibrosis and a pathologic RV dilation, leading to an increased risk for malignant arrhythmia even in healthy subjects5.
The analysis of fluid dynamics parameters such as mean kinetic energy (MKE), turbulent kinetic energy (TKE) and viscous shear stress (VSS) as measured by MRI have already been tested as hemodynamic indicators of severity in Tetralogy of Fallot, aortic valve stenosis and mitral regurgitation6,7,8.
The aim of this study is to better understand the hemodynamic differences of the blood flow in RV underlying the different RV remodeling pattern in endurance athletes and ARVC patients compared to healthy subjects.
Methods
Study population
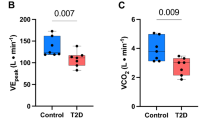
In this observational study, male subjects were categorized into 3 groups as follows: healthy volunteers with mild daily activities (Healthy group, n = 2), athletic male probands with endurance sport activity history (Athlete group, n = 2), and patients with definite ARVC according to the 2010 Task Force Criteria (ARVC group, n = 2)9,10. Athletes underwent MRI examination during their regular training and cardiopulmonary exercise testing showed a VO2peak of 37 ml/min/kg, corresponding to 339 W, 175% of theoretical maximal capacity, and a VO2peak of 43 ml/min/kg, corresponding to 412 W, 197% of theoretical maximal capacity, respectively. ARVC patient #1 was diagnosed during regular health check-up and presented with major imaging criteria and repolarization abnormalities. ARVC patient #2 presented initially with palpitation during sport activity and was diagnosed with major arrhythmia criteria due to the finding of ventricular tachycardia. Both ARVC patients did not perform high-intensity sport neither at the moment of ARVC diagnosis, nor before, but only moderate-intensity leisure activity11. Their functional capacity at exercise testing revealed a good functional capacity of 206 W, corresponding to 99% of the theoretical maximal capacity, and of 239 W, corresponding to 111% of the theoretical maximal capacity, respectively.
All patient groups were screened and recruited for 4D flow MRI scans at the University Hospital of Zurich. Informed consent was obtained for all participants. The study conformed to the principles outlined in the Declaration of Helsinki and was approved by the local Ethical Committee of Canton Zurich (EK-Nr. PB_2016-02109).
In vivo MRI measurements
All subjects were scanned with a 3T Philips Ingenia System (Philips Healthcare, Best, The Netherlands). For 4D Flow imaging, a spoiled gradient echo sequence with multipoint velocity encoding using 10 different velocity encodings (3 per spatial direction plus 1 reference encoding) was applied. The imaging parameters were as follows: spatial resolution 2.5 × 2.5 × 2.5 mm3, field of view 250 × 160 × 50 mm3. The velocity encoding (VENC) values were 40, 100 and 200 cm/s per direction. More technical details can be found in the previous publications of Gülan et al.12,13. The heart rate and cardiac output at the moment of the MRI analysis are reported in Table 2. All the subjects who underwent the investigation were in a clinically euvolemic status, with no signs nor symptoms of a concomitant infection.
Flow field analysis
The anatomical segmentation was performed using an in-house algorithm in MATLAB. Four different hemodynamics parameters, namely velocity, mean kinetic energy (MKE), turbulent kinetic energy (TKE) and viscous shear stress (VSS) were utilized as an indicator of the hemodynamics performance in the circulatory system. The voxelwise total kinetic energy can be decomposed into mean kinetic energy (MKE) and turbulent kinetic energy (TKE). The mean kinetic energy (MKE) is calculated for each voxel for different phases of the cardiac cycle12,13 as half of the blood density times the square of the phase averaged velocity:
where ρ is the blood viscosity, \(\overline{{U }_{i}}\) is the three dimensional phase averaged velocity, and I is the velocity component. Similarly, TKE can be calculated for each voxel for different phases of the cardiac cycle as the sum over the three spatial axis of the product of half the blood density and the square of the fluctuating velocity:
where \({{u}_{i}}^{^{\prime}}\) is the three dimensional fluctuating velocity and i is the velocity component.
Finally, viscous shear stresses (VSS) are calculated as the gradient of the mean velocity profile:
where μ is the dynamic viscosity of the fluid, as previously described13.
Echocardiographic measurements
RV and LV end-diastolic diameters indexed for body surface area were measured in parasternal long axis according to current guidelines14.
Results
The baseline characteristics of the male subjects are summarized in Table 1. Intracavitary blood flow parameters obtained via 4D-MRI in vivo for all patient are summarized in Table 2.
Velocity analysis
Temporal evolution of velocity magnitude spatially averaged over RV is shown in Fig. 1a. The temporal trends of blood velocity in healthy probands, athletes and patients with ARVC are similar, i.e. an increase in systole due to high velocity regions in the vicinity of RVOT where RV forward the ventricular blood volume into pulmonary artery7 and a second peak in diastole due to the high velocity regions in the vicinity of the tricuspid region where the atrial blood flow fills the RV. Figure 1b depicts the velocity magnitude averaged over RVOT. The temporal trends is different from the ones averaged over the entire RV (Fig. 1a). During the ventricular contraction, i.e. systolic phase, higher velocities develop in the RVOT region. The ARVC patients show higher velocity regions during this phase of the cycle. In the diastolic phase, the magnitude of the velocity becomes smaller as compared to the systolic velocities.
Kinetic energy analysis
Temporal evolution of MKE averaged over the entire RV is shown in Fig. 2a. The athletes show lower MKE during the systolic phase whereas the patients with ARVC develop higher MKE during the ventricular contraction phase. To have a better understanding on the spatial distribution of MKE, temporal evolution of MKE averaged over RVOT was depicted in Fig. 2b. As see, athletes show considerably lower MKE levels in the systolic phase compared to the patients with ARVC and healthy probands.
Similar to the MKE analysis, temporal evolution of TKE averaged over the entire RV was presented in Fig. 3a. The temporal trends of TKE for all population vary during the heart cycle. The athletes show relatively lower TKE levels in late systole compared to the health probands and patients with ARVC. The TKE intensity variation during a heart cycle for all population is shown in Fig. 3b. Athletes show lower TKE values during the entire heart cycle. The healthy probands and patients with ARVC develop higher TKE regions compared to the athletes.
Shear stress analysis
Finally, the temporal trend of viscous shear stress is investigated. As shown in Fig. 4a, athletes show lower shear stresses in the systolic phase, yet higher stresses in the diastolic phase. Similar to Fig. 4a, temporal evolution of VSS averaged over the RVOT is depicted in Fig. 4b. Compared to the RV averaged stresses, RVOT averaged stresses show lower values for the athletes.
Discussion
This study demonstrates time dependent, 3D blood flow patterns in the RV and RVOT as extracted using 4D-MRI flow measurements. To the best of our knowledge, this is the first study assessing the kinetic energy and shear stresses in the RV, and more specifically in the RVOT, by 4D-MRI in healthy probands, endurance athletes and ARVC patients.
In this study, we compared fluid dynamics of both RV and RVOT in healthy probands, endurance athletes and ARVC patients. RV and RVOT flow patterns have already been investigated in a previous study both in vivo and in vitro, showing that healthy probands and ARVC patients are subjected to higher MKE and WSS levels in the RVOT regions as compared to the rest of the RV13. The present data show that these findings apply to endurance athletes, as well: RVOT has higher kinetic energies and shear stresses compared to the global averaging over RV in all population analyzed. This finding might explain the high incidence of idiopathic tachycardias originating from the RVOT even in absence of structural heart disease15,16.
The diagnosis of ARVC is often challenging particularly at the early stages of disease, as it mostly involves young subjects. Furthermore, ARVC patients involved in both amateur and professional endurance sport activities are more likely to present with more severe clinical manifestations of ARVC. A better understanding of RV and RVOT fluid dynamics might help comprehend why genetically predisposed ARVC patients performing endurance activity develop a more severe phenotype and why otherwise healthy endurance athletes develop an ARVC-like phenotype even in absence of its corresponding genotype5,17.
Contrary to healthy probands and athletes, we found that ARVC patients experience in particular a second peak in flow velocity even during the diastole in the subtricuspid region, which is one of the first regions presenting with structural anomalies during the early stages of the disease.
Despite high RV and RVOT flow velocities, athletes had lower MKE values both along the whole RV and more specifically in the RVOT regions during both systole and diastole compared to ARVC patients. This finding likely reflects the differences in RV compliance, which is higher in athletes, whereas ARVC patients can develop RV diastolic dysfunction, which imply a negative prognosis18.
The analysis of blood stream turbulence was performed by assessing TKE, which has already been associated with adverse RV remodeling in patients with tetralogy of Fallot and relevant pulmonary valve regurgitation8. We found that athletes constantly showed lower TKE levels both along the whole RV and more specifically in the RVOT regions during all heart cycle phases compared to healthy probands and ARVC patients. This finding was confirmed also when shear stress originating from viscous fluid was analyzed. Our group previously demonstrated that there are higher shear stresses in the RVOT regions in a similar fashion in both healthy probands and ARVC patients13.
Interestingly we found that endurance athletes had both global RV and locally in the RVOT area lower shear stress values not only compared to ARVC patients, but also to healthy probands. The athlete’s heart is defined as a set of structural, electrical and functional remodeling as response to repetitive intense or extensive exercise. Endurance athletes present with four-chamber enlargement and higher biventricular mass in response to repetitive volume challenges19,20,21. Despite a resting biventricular systolic ejection fraction on the lower normal range, early diastolic function is usually normal to enhanced22,23. The current findings about lower RV shear stress in athletes might be related to a higher adaptation capability of the athlete’s heart to dynamic intracavitary stress related to blood flow, leading to an increased ventricular diastolic compliance.
Limitations
The three groups investigated (healthy probands, athletes and ARVC patients) are represented only by two subjects each. Thus, interindividual variability could not be taken into account and formal statistical analyses were not possible. The proposed study reflects the observation of different physiological and pathological flow mechanics in these 3 groups and did not aim to provide definite answers, also because statistical analyses were not possible due to the low numbers. Our study can rather be regarded as hypothesis generating.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to technical reasons but are available from the corresponding author on reasonable request.
References
Pelliccia, A., Maron, B. J., Spataro, A., Proschan, M. A. & Spirito, P. The upper limit of physiologic cardiac hypertrophy in highly trained elite athletes. N. Engl. J. Med. 324(5), 295–301 (1991).
Papadakis, M. et al. The prevalence, distribution, and clinical outcomes of electrocardiographic repolarization patterns in male athletes of African/Afro-Caribbean origin. Eur. Heart J. 32(18), 2304–2313 (2011).
Bauce, B. et al. Differences and similarities between arrhythmogenic right ventricular cardiomyopathy and athlete’s heart adaptations. Br. J. Sports Med. 44(2), 148–154 (2010).
Saguner, A. M., Duru, F. & Brunckhorst, C. B. Arrhythmogenic right ventricular cardiomyopathy: A challenging disease of the intercalated disc. Circulation 128(12), 1381–1386 (2013).
Venlet, J. et al. Isolated subepicardial right ventricular outflow tract scar in athletes with ventricular tachycardia. J. Am. Coll. Cardiol. 69(5), 497–507 (2017).
Binter, C. et al. Turbulent kinetic energy assessed by multipoint 4-dimensional flow magnetic resonance imaging provides additional information relative to echocardiography for the determination of aortic stenosis severity. Circ. Cardiovasc. Imaging 10(6), 5486 (2017).
Dyverfeldt, P. et al. Hemodynamic aspects of mitral regurgitation assessed by generalized phase-contrast MRI. J. Magn. Reson. Imaging 33(3), 582–588 (2011).
Fredriksson, A. et al. Turbulent kinetic energy in the right ventricle: Potential MR marker for risk stratification of adults with repaired Tetralogy of Fallot. J. Magn. Reson. Imaging 47(4), 1043–1053 (2018).
Corrado, D. et al. Arrhythmogenic right ventricular cardiomyopathy: Evaluation of the current diagnostic criteria and differential diagnosis. Eur. Heart J. 41(14), 1414–1429 (2020).
Marcus, F. I. et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: Proposed modification of the Task Force Criteria. Eur. Heart J. 31(7), 806–814 (2010).
Costa, S. et al. Changes in exercise capacity and ventricular function in arrhythmogenic right ventricular cardiomyopathy: The impact of sports restriction during follow-up. J. Clin. Med. 11, 5 (2022).
Gulan, U., Binter, C., Kozerke, S. & Holzner, M. Shear-scaling-based approach for irreversible energy loss estimation in stenotic aortic flow—An in vitro study. J. Biomech. 56, 89–96 (2017).
Gulan, U. et al. Hemodynamic changes in the right ventricle induced by variations of cardiac output: A possible mechanism for arrhythmia occurrence in the outflow tract. Sci. Rep. 9(1), 100 (2019).
Rudski, L. G. et al. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 23(7), 685–713 (2010).
Fuenmayor, A. J. Treatment or cure of right ventricular outflow tract tachycardia. J. Atr. Fibrillat. 7(1), 1038 (2014).
Lerman, B. B., Stein, K. M. & Markowitz, S. M. Idiopathic right ventricular outflow tract tachycardia: A clinical approach. Pacing Clin. Electrophysiol. 19(12 Pt 1), 2120–2137 (1996).
Oezcan, S. et al. Pectus excavatum: Echocardiography and cardiac MRI reveal frequent pericardial effusion and right-sided heart anomalies. Eur. Heart J. Cardiovasc. Imaging 13(8), 673–679 (2012).
Sadeghpour, A. et al. Presence and prognostic value of ventricular diastolic function in arrhythmogenic right ventricular cardiomyopathy. Echocardiography 37(11), 1766–1773 (2020).
Bohm, P. et al. Right and left ventricular function and mass in male elite master athletes: A controlled contrast-enhanced cardiovascular magnetic resonance study. Circulation 133(20), 1927–1935 (2016).
Scharhag, J. et al. Athlete’s heart: Right and left ventricular mass and function in male endurance athletes and untrained individuals determined by magnetic resonance imaging. J. Am. Coll. Cardiol. 40(10), 1856–1863 (2002).
Petersen, S. E. et al. Sex-specific characteristics of cardiac function, geometry, and mass in young adult elite athletes. J. Magn. Reson. Imaging 24(2), 297–303 (2006).
Galderisi, M. et al. The multi-modality cardiac imaging approach to the athlete’s heart: An expert consensus of the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 16(4), 353 (2015).
Fagard, R., Van den Broeke, C. & Amery, A. Left ventricular dynamics during exercise in elite marathon runners. J. Am. Coll. Cardiol. 14(1), 112–118 (1989).
Acknowledgements
The Zurich ARVC Program is supported by research grants from the Georg und Bertha Schwyzer-Winiker Foundation, Baugarten Foundation, University Hospital Zurich Foundation (Dr. Wild Grant), the Swiss Heart Foundation and the Swiss National Science Foundation (SNF).
Author information
Authors and Affiliations
Contributions
U.G. and V.A.R. wrote the manuscript; A.G., R.M. and U.G. performed the data acquisition; D.N., U.G. and A.G. designed the work. All authors critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
AMS received educational grants through his institution from Abbott, Bayer Healthcare, Biosense Webster, Biotronik, Boston Scientific, BMS/Pfizer, and Medtronic; and speaker/advisory board/consulting fees from Abbott, Bayer Healthcare, Daiichi-Sankyo, Medtronic, Novartis and Pfizer. UG is a shareholder at Hi-D Imaging. DN received speaker/advisory board/consulting fees from Abbott, Amgen, Astra Zeneca, Bayer Healthcare, Boeringer Ingelheim, Daiichi-Sankyo, Novartis, and Pfizer. Other authors do not have any competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gülan, U., Rossi, V.A., Gotschy, A. et al. A comparative study on the analysis of hemodynamics in the athlete’s heart. Sci Rep 12, 16666 (2022). https://doi.org/10.1038/s41598-022-20839-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-20839-8