Abstract
The present study examined the safety and efficacy of the ceremonial use of ayahuasca in relation to reports of heightened life event reexperiencing under psychedelics. The study examined (1) the prevalence of specific types of adverse life event reexperiencing, (2) characteristics predictive of reexperiencing, (3) the psychological character of reexperiencing, and (4) the impact of reexperiencing on mental health. Participants were recruited from three ayahuasca healing and spiritual centers in South and Central America (N = 33 military veterans, 306 non-veterans) using self-report data at three timepoints (Pre-retreat, Post-retreat, 3-months post-retreat). Reexperiencing adverse life events under ayahuasca was common, with women showing particularly high probability of reexperiencing sexual assault, veterans reexperiencing combat-related trauma, and individuals with a self-reported lifetime diagnosis of post-traumatic stress disorder exhibiting a substantively higher prevalence of reexperiencing. Reexperiencing was associated with states of cognitive reappraisal, psychological flexibility, and discomfort during ceremonies, and participants who reexperienced adverse life events exhibited greater reductions in trait neuroticism following their ceremonies. Clinical implications of these results for the application of psychedelics to mood and stress disorders are discussed.
Similar content being viewed by others
Introduction
As psychedelic therapies become increasingly accepted as tools for mental health care, many properties of psychedelic experience pertinent to clinical efficacy and safety remain unknown. Paramount among these is the degree to which moderate-to-large doses of psychedelics bring to the surface autobiographical memories of adverse life events and the impact of these memories on long-term mental health outcomes. These properties of psychedelic experience are important to explore as they can inform psychedelic therapy’s suitability for trauma-focused application as well as the need for consent and safeguards surrounding psychedelic-induced trauma re-exposure. Ceremonial ayahuasca and other psychedelic therapies have been proposed by a number of scholars to hold potential for treating post-traumatic stress disorder (PTSD)1,2, with clinical trials examining psilocybin-assisted therapy for PTSD currently underway, and early-stage biotechnology companies joining the exploratory effort. Meanwhile, ayahuasca shamans and ayahuasca healing centers in South America heavily focus on healing trauma, and have become increasingly popular among veterans seeking trauma-focused solutions. However, some clinical scientists have voiced concerns regarding the safety of psychedelic therapies for populations with a trauma history and PTSD, noting the potential for traumatic re-exposure of an uncontrolled and challenging nature3. These concerns are well-considered in view of known reports of unpleasant emotional reactions4 and “bad trips”5; as well as clinical scientists’ point of reference in therapies such as Prolonged Exposure Therapy6, wherein exposure is graduated, controlled, and can be stopped at any time.
Despite these ongoing questions about efficacy and safety, very little empirical data exists to inform them. The purpose of this study is accordingly to investigate the prevalence, proximal etiology (i.e., predictors of recollection), character, and impact of adverse life event reexperiencing during the ceremonial use of ayahuasca and psychedelic experience more broadly. We undertake this investigation in a large sample of adult ayahuasca retreat-goers and a smaller sample of veterans, many of whom have experienced combat-related trauma, served as special operations forces, and possessed a previous diagnosis of PTSD. We believe this empirical study is the first to systematically examine rates of re-exposure to adverse life events under psychedelic drugs, and its consequences for mental health.
Importance of psychedelic therapies in veteran mental health
Exploring these questions in the combat-veteran population is particularly important for two reasons. First, there is concern within the veteran community regarding the adequacy of current psychotherapeutic and pharmacotherapeutic treatments for PTSD. Veterans are increasingly utilizing non-profits such as Heroic Hearts Project, Veterans Exploring Treatment Solutions, and Special Operations Care Fund to pursue treatment alternatives to Veteran Affairs-sponsored mental health services, such as repetitive transcranial magnetic stimulation therapy, hormone replacement, and various psychedelic treatments. Preliminary research on the efficacy of these treatments has been promising7, and MDMA-assisted therapy has demonstrated key strengths relative to gold-standard trauma-focused therapies, chiefly greater tolerance and lower dropout8.
Second, many veterans, particularly those with a special operations forces background, present with a symptom profile that deviates from the traditional Diagnostic and Statistical Manual of Mental Disorders (DSM)9 PTSD category10, raising the possibility that alternative therapies may be better suited. For example, “Operator Syndrome”10 describes a complex array of problems that are thought to stem from operators’ specialized combat training as well as frequent blast-wave exposure. Problems include endocrine dysfunction, sleep disturbance, headaches, memory, concentration, and other cognitive impairments, hypervigilance, interpersonal dysfunction, and challenges in adapting to civilian life. Symptoms of grief, survivor’s guilt, and a sense of foreshortened future are also more common in this population, stemming from their familiarity with mortality and loss, whereas Criteria B and C symptoms involving intrusive thoughts and fear/avoidance are less frequently reported10.
Psychedelic reexperiencing of autobiographical memories
A number of quantitative and qualitative sources link psychedelic compounds, including ayahuasca, to increased autobiographical recollection of previous adverse life events (see Healy11 for review). Direct examinations of the effect of psychedelic compounds on autobiographical recollection however remain limited and mixed. Carhart-Harris et al.12 observed fMRI hyperactivation in visual and sensory brain areas and increased subjective reports of vivid and visual recollection in relation to autobiographical memory cues among healthy participants under psilocybin versus placebo. These findings reflect the possibility of more vivid recollections, but not necessarily more prevalent recollections under psychedelics. Speth et al.13 reported reduced mental time travel to the past under lysergic acid (LSD) in a small sample of healthy volunteers, suggesting a lower prevalence of autobiographical memories.
Examinations of clinical trial and naturalistic survey data have shown preliminary evidence for increased autobiographical reexperiencing under psychedelics as well as its therapeutic value. Three clinical trials examining the efficacy of psilocybin-assisted therapy for anxiety, depression, and cigarette addiction14,15,16 have reported patient reexperiences of childhood sexual assault17,18 and previous physical and emotional abuse in infancy and childhood19,20 during dosing sessions. In addition, five naturalistic studies examining therapeutic mechanisms specific to ayahuasca have similarly shown reports of autobiographical memory reexperiencing2,21,22,23, with some asserting ayahuasca-mediated recollection of suppressed or forgotten memories24. In general, the foregoing reports ascribe therapeutic value to autobiographical reexperiencing, with some patients suggesting that engagement with these memories catalysed healing17, and others attributing the clinical trial’s therapeutic efficacy primarily to productive engagement with previous trauma19. These reports have prompted some scholars and practitioners to point to reexperiencing and associated biological processes as potential mechanisms underlying action on PTSD and other disorders bearing a trauma-related etiology1,25.
Notwithstanding the importance of the foregoing findings, a number of gaps remain. First, these observations were generally obtained from small samples in which adverse life event recollections were not systematically recorded, limiting their ability to yield precise prevalence rates. Second, little is known about how different trauma types (e.g., sexual assault, accident) may be differentially associated with the probability of psychedelic reexperiencing. Furthermore, little is known about whether populations that disproportionately experience certain trauma types (e.g., sexual assault in women26, disaster, harming others, loss in combat-veterans27) are predisposed to a higher probability of reexperiencing such events.
Proposed mechanisms underlying trauma-focused psychedelic therapy
Multiple theories have been put forth accounting for psychedelics’ therapeutic action on PTSD at psychoanalytic, cognitive, and biological levels of analysis. Psychoanalytic theories hold that ayahuasca diminishes defense mechanisms that typically impede the emergence of challenging psychological material21,24. Consistent with emotional processing theory28, psychedelic experience may also assist in activating and modifying trauma memory structures through exposure to avoided stimuli (i.e., memory content) and extinction learning25. Similar to the imaginal exposure component of Prolonged Exposure Therapy, engagement with trauma memories under psychedelics may accompany1 reorganizing the memory, 2 re-examining negative appraisal of conduct during the remembered episode, 3 distinguishing between remembering the trauma and experiencing the trauma, and 4 conveying understanding that the trauma can be remembered without resulting in harm29,30). Wolff et al.25 propose that psychedelics may be particularly effective in revising trauma memory structures through producing sustained, involuntary exposure. Sustained exposure may also be consistent with deficits in cognitive control observed under psychedelics31,32, whereby it is plausible that attentional shifts away from trauma memories are impaired. As a note, exposure-supported extinction learning is the dominant explanation for the action of MDMA-assisted therapy for PTSD33, and may also apply to psychedelic therapies.
Other scientists have observed the role of psychological flexibility in psychedelic-mediated healing34,35,36. Psychological flexibility is defined as the ability to flexibly alternate between and manage challenging thoughts, emotions, or mental sets in the service of carrying out valued actions37. Given that psychological inflexibility has been implicated as a maintaining factor in multiple mental health disorders including PTSD38, it is possible that enhanced flexibility under ayahuasca may accompany therapeutic processes, e.g., cognitive processing of previous trauma and trauma-related beliefs39, fear extinction.
Finally, the entropic brain hypothesis40 and free energy principle41 have also been invoked25 to account for the emergence of trauma memories under psychedelics as well as for their potentially therapeutic action25. Combined in the relaxed beliefs under psychedelics theory (REBUS)42, the theory conceptualizes the brain as an inference-making machine that learns about the world through making predictions, avoiding uncertainty, and updating in response to new (or deviant) external percepts. Through producing entropy (i.e., the degree to which neural activation patterns cannot be predicted by prior states of activation, disorder) in the higher-level (transmodal) control areas of the brain, psychedelics are thought to relax the rigidity of the predictions, which can themselves exert a constraining influence over mental experience. This is theorized to allow an opening of the mind to new sensory (and generally mental) experience, which may revise certain higher-order beliefs about oneself and one’s world. In a therapeutic context, such potential for revising beliefs could conceivably guide reappraisal of rigid maladaptive beliefs underlying mood and stress disorders. For example, a patient with sexual assault history may hold rigid negative beliefs about their blameworthiness and their surroundings’ high risk of harm. Under psychedelics, the weighting of these beliefs may be relaxed, allowing the person to explore alternative perspectives.
Present study
The present study investigated the prevalence, proximal etiology (i.e., predictors of traumatic recollection), character, and impact of adverse life event reexperiencing in relation to the ceremonial use of ayahuasca in a sample of 306 non-veterans and 33 veteran participants. Two aims were primary. First, we aimed to examine the prevalence of adverse life event experience before ayahuasca use and reexperience during use, with focus on multiple types of adverse life events, ranging in severity. Differences between populations (females vs males, veterans vs non-veterans) were examined to identify unique group-level risks and treatment opportunities. Second, we aimed to prospectively examine the therapeutic effect of reexperiencing on mental health, using Five-Factor model (FFM)43 of personality Neuroticism scores. We examined Neuroticism given its versatility as a measure of normal-range negative affectivity and psychopathological-range internalizing44, and its no less dynamic responsiveness to therapy and life experience45,46,47. Notably, Neuroticism bears high overlap with the shared variance of internalizing disorders48, making it ideal as a measure of this principal component of psychopathology.
Secondary aims were to examine predictors of adverse life event reexperiencing to guide enhanced reliability of acute psychedelic effects. We furthermore examined which acute experiences (e.g., mystical-type experience, cognitive reappraisal, discomfort) may covary with reexperiencing, which may be suggestive of either the proximal precursors to reexperiencing or the cognitive states involved in reexperiencing.
Materials and methods
Study procedure, recruitment, and participants
Three-hundred-fifty-one participants were recruited from three ayahuasca retreat centers across South and Central America: Arkana Spiritual Center (Requena, Loreto, Peru), Soltara Healing Center (Gulf of Nicoya, Costa Rica), and La Medicina (Cordilliera Escalera mountain range, Peru) with the assistance of center intake directors and the Heroic Hearts Project, which sponsors alternative mental healthcare options for veterans.
Participants were emailed two weeks before the date of their ayahuasca retreat with an invitation to enroll. In the recruitment consent form, participants were informed that some of the study questionnaires would include questions relating to previous “traumatic experiences” and to “their experiences during the use of ayahuasca in ritual context.” They were informed that some of the questions may be sensitive in nature, and that they had the ability to opt out of answering any questions they did not feel comfortable answering for any reason. Inclusion criteria included being above 18 years of age.
Participants were informed that they would be compensated with entry into a raffle for a week-long retreat (valued at $1580.00). Further monetary incentives of $20.00 and $30.00 were additionally offered with the second and third survey reminders, respectively, to promote compliance and reduce attrition.
On average, study surveys were administered nine days before the retreat start date (baseline), five days after the retreat end date (post), and three months following the retreat end date (~ ± 114 days after retreat end date; follow-up). Data was collected using online surveys supported by the Qualtrics web platform. For full details on study design and procedure, see Weiss and colleagues49.
All participants provided online informed consent in accordance with the Common Rule and the Declaration of Helsinki. All procedures were performed in accordance with the relevant guidelines and regulations of the University of Georgia Institutional Review Board.
Retreat program
The retreat program varied across centers. In general, on the second morning, participants ingested a vomitivo (e.g., Kambo, lemongrass) to induce vomiting. Facilitators subsequently provided an introduction to ayahuasca ceremonial practices and answered questions. Participants typically had occasion to meet individually with shaman ayahuasqueros (in the Shipibo lineage) and facilitators to inform them about their purpose for conducting ceremony and to ask any personal questions. Facilitators requested that participants formulate intentions to bring into ayahuasca ceremony, but these were not formally communicated to ayahuasqueros or facilitators. Ayahuasqueros and facilitators did not engage in any consistent process of guiding participants to remember previous adverse life events, although individual participants may have referenced previous life events in their individual session.
Before ayahuasca ceremonies, participants had flower baths, in which ayahuasqueros poured water with fragrant floral plants over the participants. This ritual is considered to provide protection from certain spirits during ceremonies. During ayahuasca ceremonies, participant group-members drank ayahuasca one by one, contemplating their intentions while drinking. Participants were arranged on individual mats within a spacious maloca while two curanderos typically of mixed gender sang icaro prayers. At some centers, the ayahuasqueros sat in front of participants at opposite sides of the maloca, addressing their songs to one individual at a time before transitioning to the next as they circumambulated the circular perimeter of the maloca. At other centers, the ayahuasqueros sat in one place throughout the ceremony, and participants were brought up to them to receive their icaro. The icaro is a prayer regarded to have originated from previously “dieted” traditional plants/spirits. In the Shipibo ayahuasqueros’ worldview, the icaro opens up “portals” that guide positive spirits (operating as “muses” or “doctors”) to remove “dirty” or “calcified” energy from ceremony participants. In the darkness of the maloca, the ayahuasqueros were typically identified by a faint silhouette and the glowing red embers of their mapacho (tobacco grown in the Peruvian amazon) cigar. In the maloca space, it was typically possible to overhear the utterances of other participants. During ceremony, participants were typically able to request additional portions of ayahuasca from facilitators, as well as to smoke mupacho cigars. On days following ceremony nights, group shares typically took place, in which participants communicated their unique experiences and insights with the larger group.
On average, participants drank ayahuasca in 4.44 (SD = 2.20) ceremonies, over 1.38 (SD = 0.61) weeks, and drank one full glass of ayahuasca per ceremony.
Measures
Adverse life events experience (ALE)
The Life event checklist for DSM-5 (LEC-5)50 is a self-report inventory that measures 17 types of discrete experiences of adversity (e.g., natural disaster, fire or explosion, physical assault, sexual assault). To reduce the burden on participants, the LEC-5 was adapted to contain nine types of adverse life events (ALE) including (1) natural disaster, fire, or explosion, (2) transportation or serious accident at home, work, or during a recreational activity, (3) physical assault, assault with a weapon, (4) sexual assault, (5) Other unwanted or uncomfortable sexual experience, (6) life-threatening illness or injury, (7) sudden death of another, (8) serious injury, harm, or death [one] caused someone else, and (9) any other very stressful event or experience. See Fig. S1 to observe the LEC-5 and adapted study questionnaire. During baseline assessment, participants were asked whether they had experienced each of these events. Following their ceremonies, participants were asked whether they reexperienced any of these events during their ceremonies. Participants who endorsed reexperiencing an ALE were subsequently asked the intensity of their reexperience using a 5-point Likert-scale (1 = Not intense, 5 = Very intense).
Six additional variables were computed from LEC-5 data. First, a binary Any adverse life event variable was computed that indexed whether or not participants endorsed one or more events previously. A reexperiencing-related Any adverse life events variable was additionally computed related to events reexperienced during ceremony. Second, a more severe version of the Any adverse life events variable (Any severe adverse life events) was computed that omitted stressful experiences and sexually uncomfortable experience. A reexperiencing-related Any severe adverse life events variable was computed related to events reexperienced during ceremony. Third, an ALE Index variable was computed that summed the number of discrete events that participants reported. A Reexperiencing Index variable was also computed.
Five factor model personality domains
A 120-item set of the International Personality Item Pool (IPIP-NEO-120)51 was used to index self-reported personality traits. The IPIP-NEO-120 consists of five 24-item FFM domain subscales (Neuroticism, Extraversion, Openness, Agreeableness, Conscientiousness). Items used a 5-point Likert-type scale (1 = Strongly disagree, 5 = Strongly agree). The IPIP-NEO-120 has demonstrated good reliability and construct validity when compared to the Revised NEO Personality Inventory43,51. FFM domains have shown adequate test–retest reliability across an average interval of four weeks (rs > 0.77)52. Longitudinal measurement invariance has also been supported at the metric and scalar level in large samples53,54. Neuroticism was used as an index of mental health at baseline, post, and 3-month follow-up, whereas the other traits were used as predictors of reexperiencing. Internal consistency for Neuroticism ranged from 0.92 (3-month follow-up) to 0.93 (baseline); and for the other domains ranged from 0.79 (Agreeableness) to 0.92 (Extraversion).
Measures of acute experience
Mystical experience
The Mystical Experience Questionnaire (MEQ-30)55 is a 30-item scale used to assess mystical aspects of participants’ experiences during their ayahuasca ceremonies. For the purpose of this study, the Mystical subscale (15-item; e.g. “Experience of the fusion of your self into a larger whole”) was used. Items used a 6-point Likert-type scale (1 = None, 6 = Extreme (more than any other time in my life and stronger than 5)) and asked participants to consider the degree to which they had experienced mystical phenomena at any time during the ceremonies. One of the items from the Mystical subscale (item 30) was excluded due to administrator error, but internal consistency remained strong (α = 0.95).
Ayahuasca experience
The Ayahuasca Experience Inventory56 was developed to measure thoughts, feelings, behaviours, and attitudes that arise within ayahuasca ceremonies. The AEI consists of three factors: Clarity (32 items; α = 0.97) captures clarity, peace, self-connection, and self-esteem; Reappraisal (30 items; α = 0.96) captures cognitive reappraisal of negative beliefs about self/others as well as the meaning of challenging life experiences; and Discomfort (15 items; α = 0.94) captures unpleasant feelings of torment, discomfort, and isolation that seemed unending. Items asked participants to consider the degree to which they had experienced phenomena at any time during the ceremony. Items were measured using a 6-point Likert scale (1 = None, 6 = Extreme (more than any other time in my life and stronger than 4)). The AEI Reappraisal scale is a novel measure that was piloted in the primary study49. As the scale is not yet published, more explanation of its psychometric properties is provided in Supplementary Materials II).
Lifetime diagnosis of post-traumatic stress disorder
During baseline assessment, participants were asked to share, with open-ended responses, any mental health diagnoses they had previously received. These responses were then coded and a categorical, binary variable was computed indexing the presence or absence of participants’ previous diagnosis of PTSD.
Qualitative intention variables
At post-retreat assessment, participants were asked to describe their pre-ceremony intentions open-endedly (“What intentions did you bring into your ceremonies?”). Responses were then coded for whether they contained intentions related to either resolving stress surrounding previous ALEs (Trauma Healing Intention) or more general mental health-related healing (Healing Intention). The first and second authors both performed this coding, and deliberated in cases of disagreement to reach consensus. The Trauma Healing Intention and Healing Intention variables were categorical and binary, with each participant scoring either 0 (absent) or 1 (present).
Validity criteria
Two 8-item validity scales from the Elemental Psychopathy Assessment57 were used to detect invalid responding on measures of personality. These scales were the Infrequency scale and the Unlikely Virtue scale. In line with guidelines57, participants who endorsed more than three Infrequency scale items and more than two Unlikely Virtue scale items were eliminated.
Ceremony characteristics
Participants were asked about characteristics of their retreat experience including the number of ceremonies in which they consumed ayahuasca, retreat length, average dosage of ayahuasca, and experiences with other plant medicines (e.g., huachuma, sapo). Dosage was computed as the approximate ayahuasca quantity consumed across ceremonies in terms of glasses (e.g., one and one-half glasses). Of note, glass size was not standardized and varied within and across retreat centers. Complete data for dosage and frequency of ceremonies were available for 276 participants.
Analytic plan
Five primary sets of analyses were planned. The statistical significance threshold was set at p < 0.05, and the Benjamini and Hochberg58 False Discovery Rate (FDR) adjustment was applied to correct for multiple comparisons, using the Sgof R package59. All data met assumptions of normality according to guidelines indicated by60,61.
The first set of analyses counted the number of veterans and non-veterans who reported previous adverse life events and reexperiences of previous adverse life events during ceremony. The second set of analyses tested differences in the prevalence of ALEs and reexperiencing between subsamples (veterans vs non-veterans; PTSD diagnosis vs no PTSD diagnosis) and sexes. The third set of analyses calculated correlations between acute factors and reexperiencing.
In the fourth set of analyses, linear mixed effects (LME) models were conducted using the ‘lme4’62 package in R software to examine the moderation-based effect of previous ALE experience and ALE reexperiencing on change in Neuroticism. Neuroticism scores were regressed onto the interaction between Timepoint (a categorical variable with levels baseline, post, and follow-up) and each moderator, separately, with a random effect of intercept specified. As such, these models were used to test whether ALE experience or reexperience scores significantly moderated estimated changes in Neuroticism, i.e., the effect of Timepoint on Neuroticism. Because all timepoints were included in the model, results were indicative of the degree of moderation of change between baseline and post, and between baseline and follow-up. Given a positive moderation-based effect of age on change in Neuroticism, Age was included as a covariate. Accordingly, the mathematical model and R code are presented below:where Yij = level of Neuroticism for person j at timepoint (categorical variable with levels of baseline, post, follow-up). For these analyses, we generated unstandardized (B) coefficients for the interaction term, representing the effect of a one-unit increase in the moderator on the magnitude of the relationship between Timepoint and Neuroticism (i.e., difference between two timepoints in Neuroticism scores).
Mathematical model | Level 1: Yij = β0j + β1j(Timepoint)j + β2j(Age) + rij |
Level 2: β0j = γ00 + γ01(Moderator)j + u0j (random intercept) | |
Level 2: β1j = γ10 + γ11(Moderator)j | |
R formula | lmer(Y ~ Timepoint*Moderator + Age (1 | participant) , data = data frame) |
Five supplementary sets of analysis were also undertaken. No adjustment for multiple comparisons was used for these analyses, attending inflated Type I error. The first set of analyses examined whether change in Neuroticism was significantly greater in the veteran versus non-veteran sample (Supplementary Materials III). The first set of analyses calculated correlations between baseline characteristics (demographic characteristics, baseline traits, pre-ceremony intentions) and reexperiencing ALEs (Supplementary Materials IV). The third set of analyses identified open-ended responses in which participants reflected on how their ceremony experiences modified their relationship to previous ALEs (Supplementary Materials V).
Ethical approval
This research was approved by the University of Georgia Institutional Review Board.
Results
Participant sample
Of 351 participants who were recruited, 2% (N = 6) did not meet the validity criteria (see Measures), and 2% (N = 6) did not report on previous adverse life events, leaving a final sample of 339 validly responding participants with adverse life event information. Three-hundred-thirteen participants of these responded at baseline and at least one subsequent time point (i.e., post, 3-months post-experience), and were thus eligible for prospective analyses. Sample size was originally determined on the basis of obtaining statistical power to detect a change in trait neuroticism of at least 0.20 standard deviations49.
Non-veteran sample
The final non-veteran sample consisted of 306 participants. Two-hundred-eighty-one participants of these responded at baseline and at least one subsequent time point, and were thus eligible for prospective analyses (mean age = 34.97 ± 10.03; ethnicity: 91% non-Hispanic White, 2% Black, 6% Asian American/Native Hawaiian or Other Pacific Islander, 7% Latinx, and 3% Indian). Because a larger number of participants reported on two timepoints versus all three, datasets were used to examine the change between baseline and post (Nfull = 273; Nadverse life events endorsing = 229), and baseline and 3-month follow-up (Nfull = 249; Nadverse life events endorsing = 207). The sample consisted of 183 participants who self-identified as males (Nadverse life events endorsing = 153) and 121 who self-identified as females (Nadverse life events endorsing = 106).
Approximately 19% of participants reported an annual income of less than $30,000, 29% reported annual income greater than $30,000 but less than $60,000, 15% reported greater than $60,000 but less than $90,000, and 31% greater than $90,000. Approximately 28% of participants reported completing some high school, 38% reported graduating high school, 16% reported completing some college, and 17% reported obtaining at least a bachelor’s degree. Approximately 11% of participants had self-reported diagnoses of major depression, 4% with PTSD, and 5% with anxiety disorder.
Veteran sample
The final veteran sample consisted of 33 participants. Thirty-two participants of these responded at baseline and at least one subsequent time point, and were thus eligible for prospective analyses (N = 30 at baseline and post, N = 30 at baseline and 3-month follow-up; mean age = 34.97, SD ± 10.03; ethnicity: 97% non-Hispanic White, 15% Latinx, and 6% Indian). The sample consisted of 30 participants who self-identified as males and three as self-identified females.
In total, 16 Army veterans (including two Green Berets, seven Rangers, one Special Air Serviceman, one Mortarman), 10 Marine veterans (including one Scout Sniper), three Navy veterans (including two SEALs), two Air Force veterans (including two Pararescuers), one Canadian Army special forces veteran, and one British Army Special Air Service veteran participated in retreats. Fifty-two-percent of the sample had a special operations forces background, 85% of veterans reported combat exposure, and 67% of veterans disclosed a lifetime PTSD diagnosis. Diagnosis was not directly assessed by study personnel.
Approximately 15% of participants reported an annual income of less than $30,000, 30% reported annual income greater than $30,000 but less than $60,000, 15% reported greater than $60,000 but less than $90,000, and 39% greater than $90,000. Approximately 33% of participants reported completing some high school, 36% reported graduating high school, 15% reported completing some college, and 15% reported obtaining at least a bachelor’s degree. Approximately 24% of participants had self-reported diagnoses of major depression, 67% post-traumatic stress disorder, and 12% anxiety disorder.
Examining the prevalence of adverse life events and reexperiencing
Non-veteran sample
Of the 306 non-veteran participants, the majority (85%) reported previous experiences of ALEs, and 53% reported previous experiences of severe ALEs. The most prevalent ALE was stressful experience, reported by 54% of participants, whereas the most prevalent severe ALE was loss of a significant other, reported by 35% of participants. The most commonly reported ALEs ranged from 5% (perpetration) to 54% (stressful experience).
Of the 85% of non-veteran participants who endorsed a previous ALE, 42% reported reexperiencing a previous ALE during their ceremony experiences while under the acute effects of ayahuasca (mean intensity 3.94 ± 0.94). Of the 53% of participants who endorsed previous experiences of severe ALEs, 27% reported reexperiencing a severe ALE during ceremony (mean intensity 3.92 ± 1.07). The proportion of ALE-endorsing participants who reported reexperiencing at least one ALE ranged from 2% (disaster) to 39% (stressful experience). The proportion of severe ALE-endorsing participants who reported reexperiencing at least one severe ALE ranged from 2% (disaster) to 33% (sexual assault).
Notably, among severe ALE types, sexual assault carried the highest reexperiencing rate, such that among the 17% of participants endorsing previous sexual assault, 33% reported reexperiencing during ayahuasca ceremony (mean intensity = 3.86 ± 0.95). Sexually uncomfortable experiences were endorsed by 32% of participants, with 24% reexperiencing (mean intensity 3.38 ± 1.28).
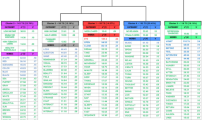
Figure 1 and Table 1 illustrate the percentage of experiencing and reexperiencing associated with each ALE type and the mean intensity of participants’ recollections.
Percentage prevalence of ALE experiencing and ALE reexperiencing in military veterans (n = 33) and non-veterans (n = 306). Plot (A) shows differences between subgroups in the prevalence of ALE experience. Plot (B) shows differences in prevalence of ALE re-experience. Asterisks indicate statistically significant differences: *p < 0.05, **p < 0.01, ***p < 0.005.
Veteran sample
Of the 33 veteran participants, all reported experiencing severe ALEs prior to their participation in the study. The most commonly reported ALEs ranged from 15% (sexual assault) to 88% (stressful experience). Six of the nine ALE types were endorsed by more than 50% of veterans, including disaster, accident, physical assault, loss, perpetration, and stressful experience.
Fifty-nine percent of veterans reported reexperiencing an ALE during ceremonies (mean intensity 3.79 ± 1.18), and 47% reported reexperiencing a severe ALE (mean intensity 3.95 ± 1.33). The proportion of ALE-endorsing participants who reported reexperiencing at least one ALE ranged from 0% (sexual assault) to 54% (loss). Veterans reported reexperiencing illness/injury, loss, and perpetration at a proportion above 50%.
Figure 1 and Table 1 provide detailed results.
Comparing the prevalence of adverse life events and reexperiencing between veterans and non-veterans
Veterans reported previous severe ALEs at significantly higher rates than non-veterans. Higher prevalence was observed for ALEs including disaster, accident, physical assault, illness/injury, loss, perpetration, and stressful experience (p < 0.005).
Veterans also exhibited a higher rate of reexperiencing severe ALEs (X2 = 12.09, p = 0.004), disaster (X2 = 37.34, p < 0.001), accident (X2 = 18.80, p < 0.001), physical assault (X2 = 13.73, p = 0.001), illness/injury (X2 = 20.32, p < 0.001), loss (X2 = 24.25, p < 0.001), and perpetration (X2 = 36.23, p < 0.001).
Figure 1, Table 1, and Table S2 present these results.
Comparing the prevalence of adverse life events and reexperiencing between males and females
Male and female non-veteran participants were relatively similar in their reporting of previous ALE history. Of the 121 female participants, 88% endorsed at least one ALE, and 57% of women reported reexperiencing at least one severe ALE. Of the 183 male participants, 84% endorsed at least one ALE, and 52% endorsed at least one severe ALE. However, female participants exhibited a higher prevalence of previous ALEs involving sexual assault (32% vs 7% for males; X2 = 30.69, p < 0.001), and sexually uncomfortable experience (52% vs 20% for males; X2 = 33.35, p < 0.001).
Females generally reexperienced ALEs (57% females vs 32% males; X2 = 9.99, p = 0.008) at significantly higher rates than males. Contributing to this pattern, female participants reexperienced sexual assault at a significantly higher rate (41% females vs 10% males; X2 = 14.73, p = 0.001).
The veteran sample only included three individuals who identified as female; therefore, comparisons could not be validly undertaken. All three female participants reported previous sexual assault and sexually uncomfortable experience. However, reexperiencing rates could not be validly estimated as only one woman (33%) reported re-experiencing sexually uncomfortable behaviour, whereas two out of three did not volunteer a response.
Figure 2, Table 2, and Tables S1 and S2 present these results.
Percentage prevalence of ALE and ALE reexperiencing in non-veteran male (n = 183) and female (n = 121) participants. Plot (A ) shows differences between subgroups in the prevalence of ALE experience. Plot (B) shows differences in prevalence of ALE re-experience. Asterisks indicate statistically significant differences: *p < 0.05, **p < 0.01, ***p < 0.005.
Comparing the prevalence of adverse life events and reexperiencing between participants with versus without a self-reported lifetime diagnosis of PTSD
Participants with a lifetime PTSD diagnosis reported all ALEs with the exception of sexual assault and sexually uncomfortable experiences at significantly higher rates than participants without a PTSD diagnosis.
Participants with a PTSD diagnosis also exhibited a higher rate of reexperiencing ALEs (X2 = 6.83, p = 0.024), severe ALEs (X2 = 14.60, p < 0.001), disaster (X2 = 15.44, p < 0.001), accident (X2 = 8.80, p < 0.011), physical assault (X2 = 10.47, p = 0.004), illness/injury (X2 = 5.48, p = 0.045), loss (X2 = 8.33, p = 0.014), and perpetration (X2 = 13.35, p < 0.001).
Figure 3, Table 3, and Table S2 present these results.
Percentage prevalence of ALE and ALE reexperiencing in participants with a lifetime PTSD diagnosis (n = 32) and without a lifetime PTSD diagnosis (n = 128). Plot (A) shows differences between subgroups in the prevalence of ALE experience. Plot (B ) shows differences in prevalence of ALE re-experience. Asterisks indicate statistically significant differences: *p < 0.05, **p < 0.01, ***p < 0.005.
Examining the association between acute factors and ALE reexperiencing
In the non-veteran sample, reexperiencing at least one ALE was significantly associated with MEQ Mystical (r = 0.18, p = 0.022), AEI Reappraisal (r = 0.24, p = 0.004), and AEI Discomfort (r = 0.33, p < 0.001), constructs reflecting mystical-type experience, introspective reappraising of difficult life experiences, and arduous acute experience, respectively. The number of distinct ALE types non-veterans reexperienced during ceremonies (Reexperiencing Index) was additionally associated with AEI Reappraisal (r = 0.18, p = 0.045) and AEI Discomfort (r = 0.25, p = 0.004).
In the veteran sample, reexperiencing at least one ALE was significantly associated with AEI Clarity (r = 0.52, p = 0.021) and AEI Reappraisal (r = 0.72, p < 0.001). Reexperiencing at least one severe ALE was significantly associated with AEI Reappraisal (r = 0.50, p = 0.028) AEI Discomfort (r = 0.55, p = 0.014). The number of distinct ALE types veterans reexperienced during ceremonies was associated with AEI Reappraisal (r = 0.57, p = 0.011) and AEI Discomfort (r = 0.58, p = 0.011).
In the non-veteran female sample, reexperiencing at least one ALE was significantly associated with MEQ Mystical (r = 0.29, p = 0.022), AEI Clarity (r = 0.30, p = 0.024), AEI Reappraisal (r = 0.36, p = 0.004), and AEI Discomfort (r = 0.30, p = 0.024). The number of distinct ALE types reexperienced during ceremonies was associated with AEI Discomfort (r = 0.27, p = 0.044).
In the non-veteran male sample, reexperiencing at least one ALE was significantly associated with only AEI Discomfort (r = 0.30, p = 0.004).
In the PTSD sample, reexperiencing at least one ALE (r = 0.44, p = 0.040), reexperiencing at least one severe ALE (r = 0.51, p = 0.019), and the number of distinct ALE types (r = 0.50, p = 0.017) were significantly associated with AEI Discomfort.
In the non-PTSD sample, reexperiencing at least one ALE was associated with AEI Reappraisal (r = 0.32, p = 0.008) and AEI Discomfort (r = 0.36, p < 0.001). Similarly, the number of distinct ALE types was associated with AEI Reappraisal (r = 0.28, p = 0.021) and AEI Discomfort (r = 0.28, p = 0.022).
Table 4 presents these results. Table S3 provides item-level correlations between AEI Reappraisal and Discomfort items and reexperiencing in the full sample.
Examining whether change in Neuroticism is moderated by previous ALEs or ALE reexperiencing
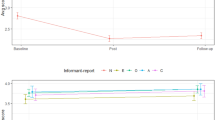
Consistent with previous analyses49, the combined sample exhibited a significant reduction in Neuroticism. Participants showed a decline of 0.53 units (on 5-point Likert-scale) in Neuroticism between baseline and post, and a decline of 0.47 units between baseline and follow-up.
Eleven models were subsequently conducted testing the moderating influence of ALE experience and reexperience variables on estimated changes in Neuroticism between baseline and subsequent timepoints. Results from these models can be found in Table 5 and detailed results can be found in Table S4.
As presented in Table 5 Section A, none of the three tested ALE experience variables did not significantly moderate change between baseline and subsequent timepoints.
As presented in Table 5 Section B, using data from the full sample (i.e., not only participants who endorsed previous ALEs), reexperiencing one or more ALEs showed evidence of potentiating reductions in Neuroticism, such that reexperiencing was associated with an incremental 0.21 and 0.19 unit decrease in Neuroticism between baseline and post (p = 0.003), and baseline and follow-up (p = 0.009), respectively. Reexperiencing one or more severe ALEs similarly showed evidence of potentiating reductions in Neuroticism between baseline and post (B = 0.012, p = 0.031). Lastly, reexperiencing an additional ALE event type (represented by the Reexperiencing Index moderator) was associated with an incremental 0.06 unit decrease in Neuroticism between baseline and post (p = 0.004), and 0.05 between baseline and follow-up (p = 0.022).
As a caveat, participants were included in this set of analyses who did not endorse previous ALEs, but nevertheless reported reexperiencing previous ALEs. These individuals were believed to have either temporarily forgotten their previous ALE history at baseline (or neglected to report them), experienced false memories during ceremony, or reexperienced repressed memories during ceremony.
As presented in Table 5 Section C, analyses were also conducted using data from only participants who previously endorsed ALEs. Here, the combined sample was examined along with female and male subsamples. Results reflected a similar pattern to the above.
Figure 4 illustrates the pattern of moderation of change in Neuroticism by reexperiencing in the full sample; other instances of significant moderation noted above reflected the same pattern.
False discovery rate results
The False Discovery Rate adjustment was applied to one-hundred-sixty p-values (corresponding to main analyses). A false discovery rate of 1.78% was observed, and adjusted p-values reflected an estimated 71 rejections of the null hypothesis at p < 0.05. Results within the main text reflect these adjusted p-values.
Discussion
Using a large sample of ayahuasca retreat-goers, the present study set out to investigate whether ceremonial ayahuasca promotes autobiographical reexperiencing of adverse life events, how well reexperiencing can be predicted from individual characteristics, and the impact of reexperiencing on mental health. Understanding psychedelic-induced autobiographical reexperiencing holds substantial clinical relevance as recollections of adverse or traumatic events could pose psychological harm under unsupportive conditions, and/or may hold therapeutic value within the context of trauma-focused psychedelic treatment.
Does psychedelic experience in the ceremonial ayahuasca context amplify autobiographical reexperiencing of adverse life events?
Our principle finding was that reexperiencing adverse life events was common among all participants, with four in ten non-veteran participants reporting reexperiencing of adverse life events, and over a quarter reporting reexperiencing of more severe adverse life events, i.e., excluding stressful experiences and sexually uncomfortable experiences. These observations are consistent with observations from clinical trials17,18,20 and naturalistic studies21,22 of autobiographical reexperiencing under psilocybin and ayahuasca. Participants notably rated their reexperiences at a relatively high intensity (i.e., average rating of 3.94 out of 5 for adverse life events), which is consistent with Carhart-Harris and colleagues’12 observations of functional hyperactivation of visual and sensory brain areas and vivid subjective recollections under LSD when cued to recollect autobiographical memories.
Our observations are the first to show the relative prevalence of different types of adverse life event reexperiencing. Approximately a quarter or more of non-veteran participants reexperienced sexual assault, sexually uncomfortable events, loss of significant others, and general stressful experiences.
The contents of participants’ reexperiences was not precisely examined in our study, but participants who reported reexperiencing were more likely to report experiences of discomfort, as well as constructive engagement with challenging emotional material during ceremony (i.e., reappraisal, psychological flexibility), including discovering positive meaning in past trauma and feeling gratitude for previous life challenges. Although these associations could be suggestive that psychedelic reexperiencing is generally characterized by qualities of reappraisal and discomfort, it could also be the case that psychedelic experiences of reappraisal and discomfort prime the emergence of adverse life event recollections. The latter possibility is supported by evidence that negative mood states promote mood-congruent (i.e., negative) memories (63,64;c.f. 65), and the fact that acute experiences of reappraisal and discomfort were measured globally (i.e., degree of acute experience), whereas reexperiencing was measured discretely (i.e., presence or absence of discrete episodes).
Given that reexperiencing has been associated in the literature with multiple substances that share serotonergic 2A agonism as a cellular mechanism of action, we believe the present findings respecting ayahuasca are likely to generalize to other classic psychedelic substances. Nevertheless, other factors associated with the use of ayahuasca may influence the emergence of autobiographical memories, including ceremonial elements, group context, molecules unique to ayahuasca (e.g., harmine), and/or spiritual forces (recognized within Shipibo metaphysics).
Do certain populations reexperience at a higher probability?
Our results pointed to two major observations regarding which populations may possess a higher probability of reexperiencing. First, women exhibited a greater likelihood of reexperiencing adverse life events than men, despite an equal rate of overall previous adverse life events between groups. This result was substantively driven by differences between females and males in reexperiencing sexual assault, with four in ten women with previous history of sexual assault recollecting their assault experiences compared to just one in ten men doing so. It is not clear what factors account for an overall higher reexperiencing rate among women, but our analyses indicated that reexperiencing women tended to report more mystical-type experience and cognitive reappraisal during ceremony than non-reexperiencing women with a similar adverse life event history, whereas men did not exhibit this pattern. These observations are the first to show differential risk of reexperiencing among women versus men, and should inform future protocols for psychedelic therapy, as will be explored below.
Second, veterans exhibited a greater likelihood of reexperiencing certain adverse life events than non-veterans. These events included memories of disasters, loss of significant others, and episodes of harming others. Veterans with special operations forces and combat experiences possess a trauma profile involving loss of significant others, personal injuries, as well as episodes of inflicting harm on others in addition to being harmed themselves10,27. Our data were suggestive that these types of life events were substantially more likely to emerge during ceremony, with more than 50% of veterans with a trauma history recollecting episodes of adverse life events in general, and illness or injury, loss, and harming others, specifically. This pattern is suggestive both of risks presented by psychedelic treatments to the veteran community (and perhaps especially those with a history of combat-exposure and special operations service), as well as opportunities for constructive emotional processing under appropriate therapeutic conditions. Relevant to risk, in the present sample, reexperiencing veterans were more likely than reexperiencing non-veterans to experience discomfort within their ceremonies. Relevant to treatment, reexperiencing veterans were more likely to engage in cognitive reappraisal and psychological flexibility. Finally, our supplementary analyses were suggestive that for veterans, being higher in neuroticism was associated with a greater probability of reexperiencing. Clinicians may view this as a risk-factor or a promotive-factor depending on treatment focus.
Third, participants with a self-reported lifetime diagnosis of PTSD exhibited a greater likelihood of reexperiencing most adverse life events than participants without a lifetime diagnosis. These events included memories of disasters, accidents, physical assaults, illnesses or injuries, loss of significant others, and episodes of harming others. Our data were suggestive that these types of life events were substantially more likely to emerge during ceremony, with more than 60% of participants with a lifetime diagnosis recollecting episodes of adverse life events in general. These results are perhaps not surprising given that a diagnosis of PTSD involves persisting attention to previous trauma, impacts on self-, other-, and world-beliefs, and sensitivity to trauma-related cues.
Does reexperiencing confer therapeutic benefit?
A substantive body of qualitative research presents accounts by psychedelic users showing that psychedelic reexperiencing of past trauma may be promotive of healing, and our qualitative findings were consistent with this. Individuals who recollected adverse life events during ceremony were more likely to report decreased neuroticism both immediately following ceremonies as well as three months later.
Conservatively, we conclude that psychedelic-induced change in neuroticism was invariant to reexperiencing adverse life events, with one possible implication being that psychedelic reexperiencing of traumatic events does not appear to interfere with the therapeutic effect of ayahuasca. Previous history of adverse life events was similarly not related to outcome, suggesting that the therapeutic effect of ayahuasca ceremony and psychedelics more broadly is not augmented or reduced by an individual’s previous trauma history.
A more liberal interpretation would be that our data is the first to systematically demonstrate the association between psychedelic reexperiencing and positive mental health outcomes. It is conceivable that the cognitive mechanisms underlying these changes involve ways of relating to trauma and adverse life events under ayahuasca that are distinctly therapeutic. For example, our results demonstrated that our reappraisal factor was generally associated with reexperiencing, raising the possibility that reappraisal represents one such mechanism. Item level analyses foregrounded the following items (in order of correlational magnitude, Table S3) as showing moderate associations with reexperiencing:
-
1.
I was able to see new positive meaning in a past trauma (r = 0.39)
-
2.
I felt that I was forced to confront negative perceptions I've had of myself (r = 0.37)
-
3.
I wrestled with my inner conflicts (r = 0.34)
-
4.
I identified aspects of myself that cause me pain (r = 0.30)
-
5.
I faced my fears (r = 0.29)
-
6.
I considered that I am too hard on myself (r = 0.26)
-
7.
Laughter or humor helped me overcome conflicts, fears, or difficult past experiences (r = 0.26)
Some of these elements are common to trauma-focused therapies recommended by the American Psychological Association, such as Cognitive-Processing Therapy39 and Prolonged Exposure Therapy, in which patients work toward displacing self-blame (e.g., addressing assimilation), and contemplating aversive memories and self-schemas without a sympathetic stress response. The first and last item, however, may provide a glimpse into what may be unique to psychedelic reexperiencing (though more research is needed, and meaning-making can emerge within the context of conventional trauma-focused therapies). These items along with item 6 are indicative of holding different perspectives on previous traumas such that the original negative meaning is not quite as resonant.
It is worth considering the cognitive states that would support this way of relating to previous hardship. Two possibilities include psychedelic-induced1 disposition toward connectedness versus separateness and 2 enhanced metacognition. Connectedness describes states of consciousness including connection to self, others, and world66, unitive consciousness involving merging with a larger whole67, alterations to attachment68, nature-relatedness69, and absorption in external phenomena70. Although connectedness is generally discussed in terms of these discrete phenomena, it is conceivable that these represent states of consciousness afforded by an underlying cognitive substrate involving a heightened capacity to recognize the meaningfulness of (or ascribe meaning to) inner and external phenomena. It is accordingly plausible that within psychedelic reexperiencing, adverse life events are themselves connected to in a new way, for example, in the form of viewing positive meaning in them and in oneself.
Metacognition describes the capacity of individuals to process and attend to their own mental states, including patterns of thoughts, emotions, as well as mental states underlying behavior71,72. Researchers have found evidence that ayahuasca and other psychedelics promote decentering73,74,75, involving the ability to observe thoughts and feelings as mental events (rather than representations of reality), and disidentify from internal experience, affording non-reactivity. Decentering in the context of reexperiencing may enable individuals to invalidate incorrect or unhelpful schemas about self, others, and world, and to hold new perspectives. For example, an individual reflecting on an episode of sexual assault may grapple with the adequacy of long-held beliefs about their blameworthiness for placing themselves in the situation, or may question the reasonableness of their generalized perception of threat in the external environment. It is likely that metacognitive processes of decentering support psychological flexibility, which has shown evidence of psychedelic-induced enhancement, both acutely34 and post-acutely35,36,76. Psychological flexibility in the context of reexperiencing may enable individuals to flexibly consider challenging beliefs about self and world in the service of reaching more adaptive perspectives, e.g., containing self-forgiveness and -compassion, resolving anger/fear, and honoring the formidable challenges they have faced.
An additional consideration pertinent to the therapeutic value of reexperiencing is whether the processes underlying the emergence of vivid psychedelic reexperiencing of genuine past events also underlie mistaken recollections of events that never took place but nevertheless emerge vividly in consciousness. As other scholars have suggested77, this latter category of reexperiencing warrants sensitive treatment from therapists, as dismissing possibly false memories that pose psychological challenge could provoke emotionally destabilizing consequences. Although our data cannot speak directly to the emergence of false or repressed memories, it bears noting that approximately 3% of participants in our sample claimed to reexperience adverse life event types that they did not report having experienced prior to their ceremonies (see Table S5).
Implications for therapeutic practice
The present results hold implications for the preparation, administration, and integration phases of psychedelic therapy. In the preparation phase, we believe it will be important for researchers and clinicians to prepare subjects/patients for the possibility of reexperiencing adverse life events in the course of informed consent. Numerous scholars have advocated for a comprehensive and supportive consent process including detailed psychoeducation regarding the range of experiences that can result from psychedelic compounds78,79,80,81. The present results support Smith and Appelbaum’s3 call for explicit reference to the potential for re-exposure to trauma within the informed consent process. Furthermore, given that women, veterans, and individuals with a lifetime PTSD diagnosis were disproportionately more likely to encounter certain adverse life events, it may be important to share the heightened risk of re-exposure with these populations, particularly. From a research perspective, it may also be conditionally prudent to screen out certain participants with particular types of trauma history from participation (e.g., sexual assault trauma).
In the administration and integration phases, we believe there is value in researchers and clinicians being prepared with trauma-focused therapeutic skills regardless of the psychiatric condition under examination. These skills may enable clinicians to productively engage with subjects/patients’ trauma memory structures and stuckpoints. Indeed, although episodes of psychedelic reexperiencing show increasing evidence of being therapeutically constructive, more distressed accounts of reexperiencing have also been reported77, raising the potential value of applying trauma-focused skills. In addition, skills in trauma-focused modalities such as Prolonged Exposure Therapy and Cognitive Processing Therapy could be additionally specialized to the population being seen, as our observations point to a higher probability of reexperiencing sexual assault among women, and of reexperiencing disaster, accident, loss, physical assault, illness/injury, and episodes of harming others among combat-veterans.
Limitations
A number of limitations should be noted. First, any claims regarding increased reexperiencing under ayahuasca should be qualified by the lack of a control condition, without which it cannot be known the rate of reexperiencing over the course of many hours of contemplative time. Mitigating this validity threat were participants’ high intensity ratings, which we regard as being suggestive of a pharmacological origin. Second, it should be stated that trauma, i.e., related to death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence by DSM-5, was not formally assessed in this study, and our results, related more broadly to adverse life events, are not expected to generalize perfectly to populations with formal trauma history. Third, the validity of the present findings rest on the absence of memory biases related to psychedelic cognitive states. Future research on the reliability of reporting on acute phenomena is encouraged. However, evidence of post-acute memory deficits have not been shown, and high average intensity ratings of reexperiences may at least be suggestive of vividness and reliability. Fourth, one caution regarding the observed sex difference in reexperiencing is that men presented with lower rates of sexual assault history relative to women (N = 10 vs N = 32), making the reexperiencing estimate for men less reliable, and the significant sex difference itself deserving of replication.
Data availability
Data has been made available at https://osf.io/uxqcv/.
References
Labate, B. C. & Cavnar, C. The Therapeutic Use of Ayahuasca (Springer, 2014).
Perkins, D. & Sarris J. Ayahuasca and childhood trauma: Potential therapeutic applications. In Ayahuasca healing & science (eds Labate, B. C. & Cavnar, C.) 99–115 (Springer, Berlin, 2021).
Smith, W. R. & Appelbaum, P. S. Novel ethical and policy issues in psychiatric uses of psychedelic substances. Neuropharmacology 216, 109165 (2022).
Wolff, T. J., Ruffell, S., Netzband, N. & Passie, T. A phenomenology of subjectively relevant experiences induced by ayahuasca in Upper Amazon vegetalismo tourism. J. Psychedelic Stud. 3(3), 295–307 (2019).
Ona, G. Inside bad trips: Exploring extra-pharmacological factors. J. Psychedelic Stud. 2(1), 53–60 (2018).
Foa, E., Hembree, E. & Rothbaum, B. O. Prolonged exposuretherapy for PTSD. (Oxford University Press, New York, NY, 2007).
Davis, A. K., Averill, L. A., Sepeda, N. D., Barsuglia, J. P. & Amoroso, T. Psychedelic treatment for trauma-related psychological and cognitive impairment among US special operations forces veterans. Chronic Stress 4, 2470547020939564 (2020).
Jerome, L. et al. Long-term follow-up outcomes of MDMA-assisted psychotherapy for treatment of PTSD: A longitudinal pooled analysis of six phase 2 trials. Psychopharmacology 237(8), 2485–2497 (2020).
Association, A. P. American Psychiatric Association, D., and American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5 5th edn, Vol. 5 (American psychiatric association, Washington, DC, 2013).
Frueh, B. C. et al. “Operator syndrome”: A unique constellation of medical and behavioral health-care needs of military special operation forces. Int. J. Psychiatry Med. 55(4), 281–295 (2020).
Healy, C. The acute effects of classic psychedelics on memory in humans. Psychopharmacology 238(3), 639–653 (2021).
Carhart-Harris, R. L. et al. Implications for psychedelic-assisted psychotherapy: Functional magnetic resonance imaging study with psilocybin. Br. J. Psychiatry 200(3), 238–244 (2012).
Speth, J. et al. Decreased mental time travel to the past correlates with default-mode network disintegration under lysergic acid diethylamide. J. Psychopharmacol. 30(4), 344–353 (2016).
Carhart-Harris, R. L. et al. Psilocybin with psychological support for treatment-resistant depression: An open-label feasibility study. Lancet Psychiatry 3(7), 619–627 (2016).
Ross, S. et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: A randomized controlled trial. J. Psychopharmacol. 30(12), 1165–1180 (2016).
Johnson, M. W., Garcia-Romeu, A., Cosimano, M. P. & Griffiths, R. R. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. J. Psychopharmacol. 28(11), 983–992 (2014).
Malone, T. C. et al. Individual experiences in four cancer patients following psilocybin-assisted psychotherapy. Front. Pharmacol. 9, 256 (2018).
Swift, T. C. et al. Cancer at the dinner table: Experiences of psilocybin-assisted psychotherapy for the treatment of cancer-related distress. J. Humanist. Psychol. 57(5), 488–519 (2017).
Noorani, T., Garcia-Romeu, A., Swift, T. C., Griffiths, R. R. & Johnson, M. W. Psychedelic therapy for smoking cessation: Qualitative analysis of participant accounts. J. Psychopharmacol. 32(7), 756–769 (2018).
Watts, R., Day, C., Krzanowski, J., Nutt, D. & Carhart-Harris, R. Patients’ accounts of increased “connectedness” and “acceptance” after psilocybin for treatment-resistant depression. J. Humanist. Psychol. 57(5), 520–564 (2017).
Kjellgren, A., Eriksson, A. & Norlander, T. Experiences of encounters with ayahuasca—“The vine of the soul”. J. Psychoact. Drugs 41(4), 309–315 (2009).
González, D., Carvalho, M., Cantillo, J., Aixalá, M. & Farré, M. Potential use of ayahuasca in grief therapy. OMEGA-J. Death Dying 79(3), 260–285 (2019).
Renelli, M. et al. An exploratory study of experiences with conventional eating disorder treatment and ceremonial ayahuasca for the healing of eating disorders. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 25(2), 437–444 (2020).
Horák, M., Hasíková, L. & Verter, N. Therapeutic potential ascribed to ayahuasca by users in the Czech republic. J. Psychoact. Drugs 50(5), 430–436 (2018).
Wolff, M. et al. Learning to let go: A cognitive-behavioral model of how psychedelic therapy promotes acceptance. Front. Psych. 11, 5 (2020).
Tolin, D. F. & Foa, E. B. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research (2008).
Nacasch, N. et al. Prolonged exposure therapy for combat-and terror-related posttraumatic stress disorder: A randomized control comparison with treatment as usual. J. Clin. Psychiatry 71(9), 15752 (2010).
Foa, E. B. & Kozak, M. J. Emotional processing of fear: exposure to corrective information. Psychol. Bull. 99(1), 20 (1986).
Foa, E. B. Prolonged exposure therapy: Past, present, and future. Depress. Anxiety. https://doi.org/10.1002/da.20907 (2011).
Powers, M. B., Halpern, J. M., Ferenschak, M. P., Gillihan, S. J. & Foa, E. B. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clin. Psychol. Rev. 30(6), 635–641 (2010).
Doss, M. K. et al. Models of psychedelic drug action: Modulation of cortical-subcortical circuits. Brain 145(2), 441–456 (2022).
Pokorny, T., Duerler, P., Seifritz, E., Vollenweider, F. X. & Preller, K. H. LSD acutely impairs working memory, executive functions, and cognitive flexibility, but not risk-based decision-making. Psychol. Med. 50(13), 2255–2264 (2020).
Mithoefer, M. C., Wagner, M. T., Mithoefer, A. T., Jerome, L. & Doblin, R. The safety and efficacy of ± 3, 4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: The first randomized controlled pilot study. J. Psychopharmacol. 25(4), 439–452 (2011).
Agin-Liebes, G. et al. Prospective examination of the therapeutic role of psychological flexibility and cognitive reappraisal in the ceremonial use of ayahuasca. J. Psychopharmacol. 36(3), 295–308 (2022).
Close, J. B., Hajien, E. C., Watts, R., Roseman, L. & Carhart-Harris, R. L. Psychedelics and psychological flexibility–Results of a prospective web-survey using the Acceptance and Action Questionnaire II. J. Context. Behav. Sci. https://doi.org/10.1016/j.jcbs.2020.01.005 (2020).
Zeifman, R. J. et al. Post-psychedelic reductions in experiential avoidance are associated with decreases in depression severity and suicidal ideation. Front. Psychiatry https://doi.org/10.3389/fpsyt.2020.00782 (2020).
Hayes, S. C., Strosahl, K. D. & Wilson, K. G. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change (Guilford Press, 2011).
Cheng, Z. H. et al. Investigating the role of psychological inflexibility, mindfulness, and self-compassion in PTSD. J. Context. Behav. Sci. 22, 102–107 (2021).
Resick, P. A., Monson, C. M. & Chard, K. M. Cognitive Processing Therapy for PTSD: A Comprehensive Manual (Guilford Publications, 2016).
Carhart-Harris, R. L. The entropic brain-revisited. Neuropharmacology 142, 167–178 (2018).
Friston, K. The free-energy principle: A unified brain theory?. Nat. Rev. Neurosci. 11(2), 127–138 (2010).
Carhart-Harris, R. L. & Friston, K. REBUS and the anarchic brain: Toward a unified model of the brain action of psychedelics. Pharmacol. Rev. 71(3), 316–344 (2019).
Costa, P. T. Jr. & McCrae, R. R. The Revised Neo Personality Inventory (neo-pi-r) (Sage Publications Inc, 2008).
Watson, D. et al. The development of preliminary HiTOP internalizing spectrum scales. Assessment 29(1), 17–33 (2022).
Hopwood, C. J., Wright, A. G. & Bleidorn, W. Person–environment transactions differentiate personality and psychopathology. Nat. Rev. Psychol. 1(1), 55–63 (2022).
Roberts, B. W. et al. A systematic review of personality trait change through intervention. Psychol. Bull. 143(2), 117 (2017).
Bleidorn, W., Hopwood, C. J. & Lucas, R. E. Life events and personality trait change. J. Pers. 86(1), 83–96 (2018).
Griffith, J. W. et al. Neuroticism as a common dimension in the internalizing disorders. Psychol. Med. 40(7), 1125–1136 (2010).
Weiss, B., Miller, J., Carter, N. & Campbell, W. Examining changes in personality following shamanic ceremonial use of ayahuasca. Sci. Rep. 11(1), 1–15 (2021).
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P. & Schnurr, P. P. The ptsd checklist for dsm-5 (pcl-5) (2013).
Maples, J. L., Guan, L., Carter, N. T. & Miller, J. D. A test of the international personality item pool representation of the revised NEO personality inventory and development of a 120-item IPIP-based measure of the five-factor model. Psychol. Assess. 26(4), 1070 (2014).
Gnambs, T. A meta-analysis of dependability coefficients (test–retest reliabilities) for measures of the Big Five. J. Res. Pers. 52, 20–28 (2014).
Lucas, R. E. & Donnellan, M. B. Personality development across the life span: Longitudinal analyses with a national sample from Germany. J. Pers. Soc. Psychol. 101(4), 847 (2011).
Wortman, J., Lucas, R. E. & Donnellan, M. B. Stability and change in the big five personality domains: Evidence from a longitudinal study of Australians. Psychol. Aging 27(4), 867 (2012).
Barrett, F. S., Johnson, M. W. & Griffiths, R. R. Validation of the revised mystical experience questionnaire in experimental sessions with psilocybin. J. Psychopharmacol. 29(11), 1182–1190 (2015).
Weiss, B., Miller, J., Carter, N. & Campbell, W. Development of the Ayahuasca Experience Inventory (AEI). Open Science Foundation (OSF) (2021).
Lynam, D. R. et al. Assessing the basic traits associated with psychopathy: Development and validation of the elemental psychopathy assessment. Psychol. Assess. 23(1), 108 (2011).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B (Methodol.) 57(1), 289–300 (1995).
Castro-Conde, I. & de Uña-Álvarez, J. sgof: An R package for multiple testing problems. R J. 6(2), 96 (2014).
Hair, J. F., Black, W. C., Babin, B. J. & Anderson, R. E. Multivariate Data Analysis (8. Baskı) 8th edn. (Cengage: Learning EMEA, 2019).
Byrne, B. M. Structural Equation Modeling with Mplus: Basic Concepts, Applications, and Programming (Routledge, 2013).
Bates, D., Mächler, M., Bolker, B. & Walker S. Fitting linear mixed-effects models using lme4. arXiv preprint arXiv:1406.5823 (2014).
Bower, G. H. Mood and memory. Am. Psychol. 36(2), 129 (1981).
Matt, G. E., Vázquez, C. & Campbell, W. K. Mood-congruent recall of affectively toned stimuli: A meta-analytic review. Clin. Psychol. Rev. 12(2), 227–255 (1992).
Parrott, W. G. & Sabini, J. Mood and memory under natural conditions: Evidence for mood incongruent recall. J. Pers. Soc. Psychol. 59(2), 321 (1990).
Watts, R. et al. The Watts Connectedness Scale: A new scale for measuring a sense of connectedness to self, others, and world. Psychopharmacology 239(11), 3461–3483 (2022).
MacLean, K. A., Leoutsakos, J. M. S., Johnson, M. W. & Griffiths, R. R. Factor analysis of the mystical experience questionnaire: A study of experiences occasioned by the hallucinogen psilocybin. J. Sci. Study Relig. 51(4), 721–737 (2012).
Stauffer, C. S., Anderson, B. T., Ortigo, K. M. & Woolley, J. Psilocybin-assisted group therapy and attachment: Observed reduction in attachment anxiety and influences of attachment insecurity on the psilocybin experience. ACS Pharmacol. Transl. Sci. 4(2), 526–532 (2020).
Kettner, H., Gandy, S., Haijen, E. C. & Carhart-Harris, R. L. From egoism to ecoism: Psychedelics increase nature relatedness in a state-mediated and context-dependent manner. Int. J. Environ. Res. Public Health 16(24), 5147 (2019).
Gandy, S. Predictors and potentiators of psychedelic-occasioned mystical experiences. J. Psychedelic Stud. 6(1), 31–47 (2022).
Pedone, R. et al. Development of a self-report measure of metacognition: The Metacognition Self-Assessment Scale (MSAS). Instrument description and factor structure. Clin. Neuropsychiatry 14(3), 185–194 (2017).
Bernstein, A. et al. Decentering and related constructs: A critical review and metacognitive processes model. Perspect. Psychol. Sci. 10(5), 599–617 (2015).
Franquesa, A. et al. Psychological variables implied in the therapeutic effect of ayahuasca: A contextual approach. Psychiatry Res. 264, 334–339 (2018).
Murphy-Beiner, A. & Soar, K. Ayahuasca’s ‘afterglow’: Improved mindfulness and cognitive flexibility in ayahuasca drinkers. Psychopharmacology 237(4), 1161–1169 (2020).
Soler, J. et al. Four weekly ayahuasca sessions lead to increases in “acceptance” capacities: A comparison study with a standard 8-week mindfulness training program. Front. Pharmacol. 9, 224 (2018).
Davis, A. K., Barrett, F. S. & Griffiths, R. R. Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. J. Context. Behav. Sci. 15, 39–45 (2020).
Timmermann, C., Rosalind, W. & David, D. Towards psychedelic apprenticeship: Developing a gentle touch for the mediation and validation of psychedelic-induced insights and revelations. Transcultural Psychiatry 59(5), 691–704 (2022).
Johnson, M. W., Richards, W. A. & Griffiths, R. R. Human hallucinogen research: Guidelines for safety. J. Psychopharmacol. 22(6), 603–620 (2008).
Bradberry, M. M., Gukasyan, N. & Raison, C. L. Toward risk-benefit assessments in psychedelic-and MDMA-assisted therapies. JAMA Psychiat. https://doi.org/10.1001/jamapsychiatry.2022.0665 (2022).
Barnett, B. S. & Greer, G. R. Psychedelic psychiatry and the consult-liaison psychiatrist: A primer. J. Acad. Consult. Liaison Psychiatry 62(4), 460–471 (2021).
Holoyda, B. Psychedelic psychiatry: Preparing for novel treatments involving altered states of consciousness. Psychiatr. Serv. 71(12), 1297–1299 (2020).
Acknowledgements
The authors thank all participants (target and informant) who contributed their valuable time to this study. This work could not have been possible without the support of the Heroic Hearts Project, RLB, Soltara Healing Center, La Medicina, and Arkana Spiritual Center. All opinions, conclusions, and recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the Source Research Foundation, Soltara Healing Center, La Medicina, Arkana Spiritual Center, or Heroic Hearts Project.
Author information
Authors and Affiliations
Contributions
Conceptualization: B.W., W.K.C., and DE; Methodology: B.W. and W.K.C.; Formal Analysis: B.W. and A.W.; Investigation: B.W. and W.K.C.; Writing—Original Draft Preparation: B.W. and A.W.; Writing—Review & Editing: B.W., W.K.C., and D.E.
Corresponding author
Ethics declarations
Competing interests
DE reports receiving consulting fees from Field Trip and Mydecine. AW reports employment at Clerkenwell Health. The other authors declare no competing interests with respect to the authorship or the publication of this article. This work was supported by an award from the Source Research Foundation.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weiss, B., Wingert, A., Erritzoe, D. et al. Prevalence and therapeutic impact of adverse life event reexperiencing under ceremonial ayahuasca. Sci Rep 13, 9438 (2023). https://doi.org/10.1038/s41598-023-36184-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-023-36184-3
This article is cited by
-
Recalled childhood trauma and post-psychedelic trajectories of change in a mixed-methods study
Scientific Reports (2025)
-
Decreased CO2 saturation during circular breathwork supports emergence of altered states of consciousness
Communications Psychology (2025)
-
Psychedelics and autobiographical memory – six open questions
Psychopharmacology (2025)
-
A prospective ecological momentary assessment study of an ayahuasca retreat: exploring the salutary impact of acute psychedelic experiences on subacute affect and mindfulness skills in daily life
Psychopharmacology (2025)
-
Cognitive functioning associated with acute and subacute effects of classic psychedelics and MDMA - a systematic review and meta-analysis
Scientific Reports (2024)