Abstract
Postoperative delirium (POD) is one of the most common complications of surgery. This study aimed to identify the risk factors for POD in patients undergoing cholecystectomy for acute cholecystitis. This retrospective study included 77 patients who underwent cholecystectomy for acute cholecystitis between January 2015, and December 2020. Multiple logistic regression analysis was used to identify the factors associated with the development of delirium as the primary endpoint. Patients were divided into POD (n = 18) and non-POD (n = 59) groups and their demographic features and clinical results were compared. A significant model associated with delirium onset was predicted (Nagelkerke’s R2 = 0.382), and the significantly correlated factors were C-reactive protein/albumin ratio (CAR), Subjective Global Assessment (SGA) score, and history of psychiatric disease. The predictive value of CAR for POD was evaluated using ROC analysis; the area under the curve of CAR was 0.731, with a cutoff value of 3.69. CAR, SGA score, and a history of psychiatric disease were identified as factors associated with the development of POD in patients with acute cholecystitis. In particular, the new preoperative evaluation of CAR may be beneficial as an assessment measure of the risk factor for the development of POD.
Similar content being viewed by others
Introduction
Delirium is a common postoperative complication. postoperative delirium (POD) is transient and reversible in most cases but is associated with worse functional outcomes, increased complications, prolonged hospital stay, and mortality1–3. Numerous studies have demonstrated the detrimental effect of higher POD severity on short- and long-term outcomes4. Therefore, identifying patients at high risk for delirium and providing more attentive care to prevent POD are essential for improving postoperative clinical outcomes in the postoperative period. Multiple risk factors for POD have been identified, and Pisani et al. published an evidence-based consensus statement on the preoperative, intraoperative, and postoperative risk factors for POD5. Preoperative factors included advanced age, comorbidities, preoperative fasting and dehydration, hyponatremia or hypernatremia, and use of anticholinergic medications. Intraoperatively, the surgical site (abdomen or chest) and intraoperative bleeding were significant factors for POD. Pain was identified as a postoperative risk factor. However, there are a variety of risk factors for POD, depending on the disease and surgical technique used.
Acute cholecystitis can lead to serious complications and even death, if left untreated. For acute cholecystitis, the Tokyo Guidelines recommend cholecystectomy as soon as possible within 72 h to 1 week of onset6. However, the Tokyo Guidelines do not mention POD and the risk factors are not clear. Low BMI, a history of neuropsychiatric disease, hypo or hyperkalaemia, and prolonged operative time have been reported as significant risk factors for delirium after chronic and acute cholecystitis7. Despite the widespread use of cholecystectomy for acute cholecystitis, predictors of POD after cholecystectomy remain unclear. Therefore, this study aimed to evaluate the association between the increased incidence of POD after acute cholecystitis and the pre- and intraoperative predictors.
Materials and methods
Study design and patients
Patients who underwent cholecystectomy under general anesthesia between January 2015 and December 2020 at Kansai Medical University Medical Center were included. Patients with a pathological diagnosis of acute cholecystitis were included, and those with a diagnosis of cholelithiasis, chronic cholecystitis, and gallbladder polyps were excluded. Finally, the patients with a pathological diagnosis of acute cholecystitis were divided into POD and non-POD groups to compare their demographic characteristics and clinical outcomes.
Data collection
Patient demographics and perioperative variables were obtained from the medical records at our institution. Demographic variables included age, sex, pathology, acute cholecystitis severity6, Data on Charlson comorbidity index (CCI)8, body mass index (BMI), Subjective Global Assessment (SGA)9, Prognostic Nutritional Index (PNI = (10 × albumin (g/dL) + (0.005 × TLC: total lymphocyte count (mm3))10, American Society of Anesthesiologists (ASA) classification, number of hospital days, smoking, alcohol consumption, medical history (mental illness, diabetes mellitus (DM), hypertension (HTN), cardiovascular disease (CVD), cerebrovascular disease (CVA), pulmonary disease, renal disease), and perioperative benzodiazepine (BZD) medication use were included. Preoperative laboratory values included measures for white blood cells (WBC), C-reactive protein (CRP), aspartate transaminase (AST), alanine transaminase (ALT), gamma-GTP, serum albumin (ALB), and CRP/ALB ratio (CAR). Surgical variables included additional epidural anesthesia, time from diagnosis to surgery, surgery within 72 h of onset, operative time, blood loss, technique (open, laparoscopic, or laparotomy transition), drain use, and need for blood transfusion. Outcome measures included postoperative complications (except delirium), mortality, and length of hospital stay. POD data (calculated from the date of surgery to the date of discharge) were collected from medical and nursing records. POD was diagnosed by an experienced psychiatrist, T. F., in accordance with the delirium section of the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5).
Statistical analysis
Results are expressed as mean ± standard deviation (SD), median (interquartile range), or number (percentage), as appropriate. Chi-squared or Fisher’s exact tests were used to compare categorical data. Variables with p < 0.05 in univariate analysis were included in the multivariate analysis by backward elimination. Multiple logistic regression analysis was used to identify risk factors for POD. Receiver Operating Characteristic (ROC) curve analysis was used to determine the cutoff value of CAR for POD. p < 0.05 was considered statistically significant. All data were obtained using SPSS Statistics (version 27.0; IBM Corp., Armonk, NY, USA).
Results
Basic characteristics and intraoperative parameters
We studied 531 patients; 77 with a pathological diagnosis of acute cholecystitis were included (Fig. 1). The patients were divided into POD (n = 18) and non-POD (n = 59) groups. The demographic data and perioperative variables of the study population are presented in Table 1. The total incidence of POD was 23.3% (18/77). The mean age of the patients was 75.6 ± 11.772 (range: 44–93) years for the POD group and 69.2 ± 13.292 (range: 27–93) years for the non-POD group. In the POD group, 18 patients (100%) had a history of alcohol consumption, whereas 45 patients (76.3) had a history of alcohol consumption in the non-POD group, a significant difference between the two groups (P = 0.022). For SGA, the measures were 2.56 ± 0.86 in the POD group and 1.86 ± 0.8 in the non-POD group, a significant difference between the two groups (P = 0.002). The POD group was discharged 16.56 ± 16.41 days postoperatively and the non-POD group was discharged after 13.88 ± 11.43 days, with no significant difference (p = 0.438).
Laboratory measurements
The preoperative CRP and ALB levels and CAR for patients in the POD group were 23.36 ± 10.76 mg/L, 2.72 ± 0.61 g/L, and 8.97 ± 5.82, respectively, while those in the non-POD group had CRP of 14.37 ± 10.82 mg/L, ALB of 3.38 ± 0.76 g/L, and CAR of 4.71 ± 3.88. There were statistically significant differences in CRP and ALB levels and CAR between the two groups (all p < 0.001) (Table 2).
Risk factors for POD
Variables with p < 0.05 in univariate analysis (alcohol consumption, history of psychiatric disease, SGA score, and CAR) were included in the multivariate analysis by backward elimination. Finally, eight factors (age, sex, alcohol consumption, CCI, history of psychiatric disease, SGA score, CAR, and operative time) were included in the multivariate logistic regression model (forward selection (likelihood ratio), p < 0.001, Nagelkerke’s R2 = 0.382). Results showed that CAR (β = 0.15; odds ratio = 1.161; 95% confidence interval (CI), 1.006–1.341; P = 0.041), SGA score (β = 0.953; odds ratio = 2.546; 95% CI, 1.05–6.174; P = 0.039), and history of psychiatric disease (β = 1.568; odds ratio = 4.796; 95% CI, 1.276–18.026; P = 0.02) were the three independent risk factors for POD (Table 3).
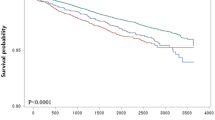
Predictive value of CAR for POD
The predictive value of preoperative CAR for POD was evaluated by ROC analysis. As shown in Fig. 2, the area under the curve of CAR for POD was 0.731, with a cutoff value of 3.69, sensitivity of 94.1%, and specificity of 43.9% (95% CI, 0.608–0.853; P = 0.004). The positive likelihood ratios (+ LR) and negative likelihood ratios (− LR) were 1.676 and 0.134, respectively, which of the Area Under the Curve (AUC) value of CAR (AUC: 0.731) were superior to those of CRP (AUC: 0.709) and ALB (AUC: 0.26). Based on a cutoff value of 3.69, patients were classified into a high CAR group (CAR ≥ 3.69) and a low CAR group (CAR < 3.69) (Table 4).
(A) Comparison of CARs between POD and non-POD groups. POD, postoperative delirium; CAR, C-reactive protein to albumin ratio. P < 0.05 was considered statistically significant. (B) The predictive value of CAR for POD by ROC curve analysis. The AUC of CAR for POD was 0.731, with a cut-off value of 3.69, a sensitivity of 94.1%, and a specificity of 43.9% (95% CI: 0.608–0.853, P = 0.004).
Discussion
In terms of basic characteristics and intraoperative parameters, SGA score, alcohol consumption, and history of psychiatric disorders differed significantly between POD and non-POD groups. In laboratory measurements, there were significant differences between POD and non-POD groups in CRP and ALB levels and CAR. There were no significant differences in other background factors. In the Tokyo Guideline, mortality, complication rates, bile duct injury rates, and open conversion rates were lower for early (72 h to 1 week) cholecystectomy for acute cholecystitis compared to standby surgery6. However, there was no significant difference in the time elapsed from the onset of acute cholecystitis to surgery between the two groups. Furthermore, patients were classified according to whether surgery was performed within 72 h, and there was no difference in the incidence of POD when surgery was performed within 72 h of onset.
The results of current study in the multivariate logistic regression model showed that the CAR and SGA score were higher in patients with POD than in those without. Furthermore, patients with psychiatric disorders were at higher risk of developing POD. Malnutrition and a history of neuropsychiatric disorders have been reported as significant risk factors for POD after chronic and acute cholecystitis7.
Neuroinflammatory changes in the central nervous system have been proposed as an explanatory mechanism for the background factors of POD11. CRP level is one of the most common biomarkers for systemic inflammation. Some studies have shown that the CRP level is an independent risk factor for POD after hip surgery12, vascular surgery13, and laparoscopic surgery for colon cancer14. Another study reported high serum CRP levels preoperatively and on postoperative day 2 as potential predictors of POD in elderly patients after major noncardiac surgery.15 ALB level is frequently used to assess the nutritional status of patients undergoing surgery. Previous studies have shown that hypoalbuminemia is significantly associated with an increased risk of POD16, 17. Several studies have reported that severe preoperative hypoalbuminemia is a predictor of POD and worse outcomes in patients undergoing noncardiac surgery18. CRP and ALB levels can also predict morbidity, mortality, and poor outcomes, such as longer hospitalization and intensive care unit (ICU) stays, respectively; elevated CRP levels are associated with malignancy, sepsis, and inflammatory disease; and decreased ALB levels are associated with pre-existing medical conditions, liver failure, renal failure, and malnutrition due to pre-existing hepatic, and renal conditions and malnutrition19, 20. Preoperative nutritional status correlates with postoperative complications, including POD, strongly suggesting the importance of improving nutritional status as much as possible before surgery.
In contrast to changes in CRP and ALB levels alone, which are nonspecific as each is associated with multiple pathologies, CAR correlates with prognostic potential by more accurately reflecting the severity of nutrient deprivation and inflammation19,20,21. Previous studies have demonstrated the predictive ability of the CAR for morbidity, mortality, and other outcomes in various patients, including critically ill19, pre-transplant or cirrhotic22,23,24, postoperative20, 25, 26, and oncological patients.27, 28 The CAR has also been reported as a preoperative predictive indicator of POD in total knee29, 30 and hip30, 31 arthroplasty surgeries in elderly patients. In the present study, a preoperative CAR of 3.69 or higher was a risk factor for POD in acute cholecystitis with surgery.
POD occurs on postoperative days 2–53, 16 and prolongs hospital stay by 2–3 days and intensive care unit stay by 2 days32, 33 POD is associated with 7–10% surgery-related mortality, but has been reported to be 1% in patients without delirium34. In the POD group, all patients experienced disease onset within 24 h. In our study, there was no difference in surgery-related mortality, complications, or length of hospital stay. There were no cases of rehospitalization in either group. However, because early detection of POD is expected to reduce medical resources and increase patient well-being, a new preoperative evaluation of CAR may be beneficial as an assessment measure of the risk factor for the development of POD. Since CRP and ALB are common items in preoperative blood tests for patients with acute cholecystitis, we believe that there is a significant advantage to adding CAR as a preoperative evaluation item, as there is no direct burden on the patient or additional medical resources. For patients predicted to develop POD based on the calculated CAR values, multidisciplinary POD countermeasures from preoperative to immediate postoperative period may contribute to the reduction of factors that promote POD.
POD is caused by multiple factors and presents with various clinical syndromes and pathophysiological changes. Our understanding of delirium captures only a subset of these symptoms. Although many previous studies show an association between POD and inflammation indices, few have been disease-limited studies. By limiting the disease, specific background factors included in previous studies can be excluded. And since there is no literature on POD in only acute cholecystitis. To our knowledge, this is the first study to report preoperative CAR as a predictor of POD in patients undergoing cholecystectomy. A limitation of this study is that it was a retrospective, single-center study that needs to be validated in a prospective, multicenter study. Furthermore, the predictors were measured only preoperatively, ignoring their relationship with the longitudinal improvement or worsening of delirium for each patient. Some residual confounding factors (for example, sample selection bias and preoperative comorbidities) cannot be completely excluded. In particular, CRP may contribute to the improvement or worsening of delirium, as it may increase or decrease between the preoperative and postoperative periods. We improved the clinical pathway starting in 2022 to standardize the schedule of blood draws and items to observe the course of POD and biomarker variability. And by adding new blood collection items, we plan to conduct a more in-depth study for the next report. It would be interesting to investigate the dynamic changes in the CAR after surgery in future studies to investigate POD outcomes and CAR dynamics. On the other hand, the application of CAR to other acute diseases and hepatobiliary-pancreatic surgery with highly invasive may contribute by adding new depth to existing literature. Because this study was retrospective, the definition and severity of delirium may not have been accurately identified. The patients with low-activity delirium were included in the non-delirium group. It is unclear whether CAR in combination with other variables (such as IL-6 and TNF-α) can predict the risk of POD, and further studies are needed to validate the same. As both CRP and ALB are synthesized in the liver, an improved assessment of the exact relationship between liver dysfunction and serum CAR levels in acute cholecystitis is also a topic for future study.
Conclusions
In conclusion, preoperative CAR, preexisting psychiatric disorders, and SGA score may be promising predictors of POD after cholecystectomy for acute cholecystitis. In particular, the new preoperative evaluation of CAR may be beneficial as an assessment measure of the risk factor for the development of POD.
Data availability
The authors affirm that all the data are true and valid. The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- POD:
-
Postoperative delirium
- CAR:
-
C-reactive protein/albumin ratio
- SGA:
-
Subjective global assessment
- CCI:
-
Charlson comorbidity index
- BMI:
-
Body mass index
- PNI:
-
Prognostic nutritional index
- TLC:
-
Total lymphocyte count
- ASA-PS:
-
American society of anesthesiologists physical status
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- CVD:
-
Cardiovascular disease
- CVA:
-
Cerebrovascular disease
- BZD:
-
Benzodiazepine
- WBC:
-
White blood cells
- CRP:
-
C-reactive protein
- AST:
-
Aspartate transaminase
- ALT:
-
Alanine transaminase
- ALB:
-
Albumin
- DSM-5:
-
Diagnostic and statistical manual of mental disorders, 5th Edition
- SD:
-
Standard deviation
- ROC:
-
Receiver Operating Characteristic
- CI:
-
Confidence interval
- + LR:
-
Positive likelihood ratios
- − LR:
-
Negative likelihood ratios
- AUC:
-
Area under the curve
References
Bai, J. et al. Association between postoperative delirium and mortality in elderly patients undergoing hip fractures surgery: a meta-analysis. Osteoporos Int.31, 317–326 (2020).
Ha, A. et al. A contemporary population-based analysis of the incidence, cost, and outcomes of postoperative delirium following major urologic cancer surgeries. Urol Oncol. 36, 341 e315–341 e322 (2018).
Witlox, J. et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA.304, 443–451 (2010).
Rudolph, J. L. & Marcantonio, E. R. Review articles: postoperative delirium: acute change with long-term implications. Anesth Analg.112, 1202–1211 (2011).
Pisani, M. A., Murphy, T. E., Araujo, K. L. & Van Ness, P. H. Factors associated with persistent delirium after intensive care unit admission in an older medical patient population. J Crit Care.25(540), e541-547 (2010).
Okamoto, K. et al. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci.25, 55–72 (2018).
Park, Y. M. et al. Postoperative delirium after cholecystectomy in older patients: A retrospective study. Ann Hepatobiliary Pancreat Surg.27, 301–306 (2023).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis.40, 373–383 (1987).
Detsky, A. S. et al. What is subjective global assessment of nutritional status?. JPEN J Parenter Enteral Nutr.11, 8–13 (1987).
Sun, K., Chen, S., Xu, J., Li, G. & He, Y. The prognostic significance of the prognostic nutritional index in cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol.140, 1537–1549 (2014).
Maldonado, J. R. Neuropathogenesis of delirium: review of current etiologic theories and common pathways. Am J Geriatr Psychiatry.21, 1190–1222 (2013).
Lee, H. J. et al. Early assessment of delirium in elderly patients after hip surgery. Psychiatry Investig.8, 340–347 (2011).
Pol, R. A. et al. C-reactive protein predicts postoperative delirium following vascular surgery. Ann Vasc Surg.28, 1923–1930 (2014).
Xiang, D., Xing, H., Tai, H. & Xie, G. Preoperative C-Reactive Protein as a Risk Factor for Postoperative Delirium in Elderly Patients Undergoing Laparoscopic Surgery for Colon Carcinoma. Biomed Res Int.2017, 5635640 (2017).
Vasunilashorn, S. M. et al. High C-Reactive Protein Predicts Delirium Incidence, Duration, and Feature Severity After Major Noncardiac Surgery. J Am Geriatr Soc.65, e109–e116 (2017).
Rudolph, J. L. et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation.119, 229–236 (2009).
Karas, P. L., Goh, S. L. & Dhital, K. Is low serum albumin associated with postoperative complications in patients undergoing cardiac surgery?. Interact Cardiovasc Thorac Surg.21, 777–786 (2015).
Zhang, Y. et al. TNIP1 alleviates hepatic ischemia/reperfusion injury via the TLR2-Myd88 pathway. Biochem Biophys Res Commun.501, 186–192 (2018).
Park, J. E. et al. The C-Reactive Protein/Albumin Ratio as a Predictor of Mortality in Critically Ill Patients. J Clin Med. 7 (2018).
Saito, H. et al. Prognostic Significance of the Preoperative Ratio of C-Reactive Protein to Albumin and Neutrophil-Lymphocyte Ratio in Gastric Cancer Patients. World J Surg.42, 1819–1825 (2018).
Park, J. et al. Predictive utility of the C-reactive protein to albumin ratio in early allograft dysfunction in living donor liver transplantation: A retrospective observational cohort study. PLoS One.14, e0226369 (2019).
Oikonomou, T. et al. The significance of C-reactive protein to albumin ratio in patients with decompensated cirrhosis. Ann Gastroenterol.33, 667–674 (2020).
Huang, S. S. et al. C-reactive protein-to-albumin ratio is a predictor of hepatitis B virus related decompensated cirrhosis: time-dependent receiver operating characteristics and decision curve analysis. Eur J Gastroenterol Hepatol.29, 472–480 (2017).
Amygdalos, I. et al. Clinical value and limitations of the preoperative C-reactive-protein-to-albumin ratio in predicting post-operative morbidity and mortality after deceased-donor liver transplantation: a retrospective single-centre study. Transpl Int.34, 1468–1480 (2021).
Haruki, K. et al. The C-reactive Protein to Albumin Ratio Predicts Long-Term Outcomes in Patients with Pancreatic Cancer After Pancreatic Resection. World J Surg.40, 2254–2260 (2016).
Ito, T. et al. Impact of the Preoperative C-reactive Protein to Albumin Ratio on the Long-Term Outcomes of Hepatic Resection for Intrahepatic Cholangiocarcinoma. Asian Pac J Cancer Prev.21, 2373–2379 (2020).
Kinoshita, A. et al. The C-Reactive Protein/Albumin Ratio, a Novel Inflammation-Based Prognostic Score, Predicts Outcomes in Patients with Hepatocellular Carcinoma. Annals of Surgical Oncology.22, 803–810 (2014).
Cui, X., Jia, Z., Chen, D., Xu, C. & Yang, P. The prognostic value of the C-reactive protein to albumin ratio in cancer: An updated meta-analysis. Medicine (Baltimore). 99, e19165 (2020).
Zhao, X. et al. EphA2 Promotes the Development of Cervical Cancer through the CXCL11/PD-L1 Pathway. J Oncol.2022, 4886907 (2022).
Peng, J., Wu, G., Chen, J. & Chen, H. Preoperative C-Reactive Protein/Albumin Ratio, a Risk Factor for Postoperative Delirium in Elderly Patients After Total Joint Arthroplasty. J Arthroplasty.34, 2601–2605 (2019).
Kim, H. J. et al. Association of C-reactive protein to albumin ratio with postoperative delirium and mortality in elderly patients undergoing hip fracture surgery: A retrospective cohort study in a single large center. Exp Gerontol.172, 112068 (2023).
Brown, C. H. t. et al. The Impact of Delirium After Cardiac Surgical Procedures on Postoperative Resource Use. Ann Thorac Surg. 101, 1663–1669 (2016).
Scholz, A. F., Oldroyd, C., McCarthy, K., Quinn, T. J. & Hewitt, J. Systematic review and meta-analysis of risk factors for postoperative delirium among older patients undergoing gastrointestinal surgery. Br J Surg.103, e21-28 (2016).
Raats, J. W., van Eijsden, W. A., Crolla, R. M., Steyerberg, E. W. & van der Laan, L. Risk Factors and Outcomes for Postoperative Delirium after Major Surgery in Elderly Patients. PLoS One.10, e0136071 (2015).
Acknowledgements
We would like to thank Editage (www.editage.com) for the English language editing.
Funding
This work was supported by JSPS KAKENHI Grant Number 23K08203.
Author information
Authors and Affiliations
Contributions
Conception and design of study: RN, YT; Acquisition of data: RN, TF, YK, MI; Analysis and interpretation of data: RN, TF, YK; Drafting of the manuscript: RN, TF, YK, TO, MK, HK. All authors critically revised the manuscript, agree to be fully accountable for ensuring the integrity and accuracy of the work, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that there are no conflicts of interest.
Ethics approval and consent
This retrospective study was approved by the Institutional Review Board of Kansai medical university medical center (approval number: 2022016). Due to the retrospective nature of the study, the Institutional Review Board of Kansai medical university medical center waived the need of obtaining informed consent’ in the manuscript. The study was performed in accordance with the ethical guidelines of the 1964 Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nakatake, R., Funatsuki, T., Koshikawa, Y. et al. C reactive protein albumin ratio as a new predictor of postoperative delirium after cholecystectomy for acute cholecystitis. Sci Rep 14, 21704 (2024). https://doi.org/10.1038/s41598-024-72856-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-72856-4
Keywords
This article is cited by
-
Clinical biomarkers of perioperative neurocognitive disorder: initiation and recommendation
Science China Life Sciences (2025)