Abstract
Astrocytes act as immune cells that can produce a series of chemokines to attract large numbers of leucocytes to the lesion site, where they contribute to excessive inflammation following spinal cord injury (SCI). However, the relevant regulatory mechanism involved in chemokine production by astrocytes has not been fully elucidated. In the present study, we examined the correlation between C-C motif chemokine ligand 5 (CCL5) and high mobility group box-1 protein (HMGB1) in a T8–T10 spinal cord contusion model. Our results revealed that SCI-induced CCL5 protein levels increased synchronously with the increase in HMGB1. Administration of an HMGB1-neutralizing antibody significantly reduced the protein expression of CCL5 in the context of SCI. An in vitro study revealed that HMGB1 binding with TLR2/4 receptors potently facilitates the production of CCL5 by astrocytes by activating the intracellular ERK/JNK-mediated NF-κB pathway. Furthermore, the HMGB1-induced release of CCL5 from astrocytes is involved in promoting microglia/macrophage accumulation and M1 polarization. The inhibition of HMGB1 activity reduces microglia/macrophage infiltration by decreasing the expression of CCL5 and improves motor functional recovery following SCI. Our results provide insights into the new functions of HMGB1-mediated astrocytic CCL5 production, which elicits inflammatory cell recruitment to the site of injury; this recruitment is associated with excessive inflammation activation. These data may provide a new therapeutic strategy for central nervous system (CNS) inflammation.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a common neurologic insult worldwide that can result in high morbidity and disability1,2. The complex pathophysiological processes of SCI are attributed to initial mechanical injury followed by a secondary injury3. Inflammatory reactions after injury are considered a major contributor to secondary damage4. The inflammatory response is complex, driven by diverse types of infiltration of leukocytes and activated glia, and connected with the extent of tissue damage and functional changes5,6. The activation of excessive neuroinflammation from infiltrating or residential inflammatory cells has emerged as a key contributor to tissue homeostasis imbalances in the lesion milieu7,8. In addition to infiltrating leukocytes and activating microglia to initiate inflammatory responses in response to SCI, reactive astrocytes are recognized as crucial regulators of neuroinflammation9,10. Astrocytes are one of the first cell responders to SCI, following injury, damage-associated molecular patterns (DAMPs) promote astrocytes to release a series of proinflammatory substances by pattern recognition receptors (PRRs), and these astrocyte-derived proinflammatory mediators have a profound role in influencing the local inflammatory microenvironment, ultimately exacerbating the neuropathology progress of SCI3,11,12.
C-C motif chemokine ligand 5 (CCL5)/RANTES is a member of the CC chemokine family that plays a key role in the central nervous system (CNS), mostly as an inflammatory and chemoattractant molecule13,14. CCL5 expression is induced in astrocytes, microglia, and neurons in the lesion core after SCI, and astrocytes are significant sources of CCL513,15. Accumulating evidence shows that CCL5 is associated with the recruitment of microglia, monocytes, and T lymphocytes in conjunction with the chemokine C-C motif receptor 5 (CCR5)14,15. CC chemokine receptor 5 (CCR5) is a seven-transmembrane, G protein-coupled receptor (GPCR) that is expressed in astrocytes, microglia and neurons16,17. CCL5 participates in the recruitment and activation of immune cells to the inflammatory area after injury and contributes to the inflammatory process, which in turn may be a precursor to secondary damage18. Blocking of CCL5 expression in reactivated astrocytes hinders the expansion of the lesion and improves neurological function recovery by preventing secondary inflammatory injury following SCI19,20. Given that CCL5 production by astrocytes is an important factor in eliciting neuroinflammation following SCI, unveiling the regulatory mechanism that drives CCL5 production in the injured cord may serve as a potential therapeutic strategy for preventing the occurrence of damage cascade events. A growing body of evidence shows that viral infection, traumatic injury and inflammatory stimuli are associated with the expression of CCL5 in astrocytes and other cell types19,21,22. However, the key molecules that drive CCL5 expression in reactive astrocytes after SCI have not been fully characterized.
High mobility group box 1 (HMGB1), a ubiquitous and abundant nuclear protein, plays a critical role in nucleosome formation and DNA transcription23. HMGB1 is also an important DAMP that is involved in multiple inflammatory CNS pathologies including sclerosis and SCI24,25. HMGB1 is passively released from necrotic cells or actively secreted from activated astrocytes, microglia, and macrophages after CNS insult26,27,28. The SCI-induced expression of HMGB-1 promotes the release of inflammatory mediators including tumor necrosis factor (TNF)-α, interleukin (IL)-1β and IL-629. As a key promoter of neuroinflammation, HMGB1 mediates inflammatory mediator production through interactions with multiple receptors, such as toll-like receptor-2 (TLR2), TLR4, and receptor for advanced glycation end product (RAGE) in microglia, neurons, and astrocytes30,31,32. Thus, HMGB1, an inflammatory regulator, exacerbates secondary damage to the injured spinal cord, and blocking of HMGB1 is beneficial for alleviating inflammation and promoting the recovery of neurological function30,33. Furthermore, HMGB1 promotes persistent inflammation by recruiting leucocytes in multiple inflammatory diseases34,35. However, whether the recruitment of leukocytes to the site of tissue damage is mediated by the HMGB1-induced production of CCL5 in astrocytes following SCI has not been reported. Here, we analyzed the relationship between the expression of HMGB1 and CCL5 following rat spinal cord contusion. We further investigated the regulatory mechanisms of HMGB1-induced expression of astrocytic CCL5, as well as its effects on microglia/macrophage migration and polarization. Our results showed that HMGB1-induced astrocytic CCL5 expression facilitates the recruitment of inflammatory cells towards lesion sites, thereby driving neuroinflammation.
Materials and methods
Animals
Adult male Sprague–Dawley (SD) rats, weighing 180–220 g, a total of 156 rats were randomized into 4 groups, operation group, n = 54; operation + IgG group, n = 42; operation + HMGB1 Ab group, n = 42; operation + CCL5 Ab group, n = 18. Rats were obtained from Shanghai SIPPR-Bk Lab Animal Co., Ltd. and maintained in specific pathogen-free laboratory animal facilities of the Ninth People’s Hospital Affiliated with Shanghai Jiao Tong University School of Medicine. All animal experiments complied with the National Institutes of Health Guide for the Care and Use of Laboratory Animals and were reviewed and approved by the Institution of Animal Care and Use Committee (IACUC) of the Ninth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine (approval no. SH9H-2023-A197-SB). All the rats were housed in standard cages in an air-conditioned room at a controlled temperature (22 ± 2 °C) with a 12–12 h light-dark cycle and had free access to water and food. All the rats were deeply anaesthetized for euthanasia via the intraperitoneal injection of an overdose of sodium pentobarbital (120 mg/kg).
Establishment of the contusion SCI rat model
The animals subjected to surgical treatment after grouping as described above. The contusion SCI rat model was generated as previously described36. Briefly, the rats were anaesthetized via an intraperitoneal injection of sodium pentobarbital (35 mg/kg). The fur was shaved from the surgical site and the skin was disinfected with chlorhexidine. A 15-mm midline skin incision was made to expose the vertebral column. After the spinal thoracic region was exposed by separation of the dorsal muscles to the side, the spinous processes of the T8–T10 vertebrae were exposed. A laminectomy was performed at the vertebral level T9, with the dorsal cord surface exposed and the dura remaining intact. The exposed spinal cord segment (approximately 3 mm in length) received a 150-kilodyne spinal contusion injury via the IH-0400 Impactor (Precision Systems and Instrumentation) injury device as previous reported18. The impact rod was removed immediately, and the wound was irrigated. For drug delivery, 10 µl of HMGB1 (50 µg/kg, R&D Systems, cat. no. MAB16901), CCL5 neutralizing antibody (50 µg/kg, R&D Systems, cat. no. MAB478) or IgG control (50 µg/kg, R&D Systems, cat. no. 6-001-A) was then slowly injected (injection flow rate, 35 nl/s) intrathecally using the Hamilton syringe (needle size, 26 ga). Muscles and incisions were sutured using silk threads. Postoperative care included butorphanol administration twice a day for a 5-day period, as well as the administration of vitamins, saline, and enrofloxacin twice a day for a 7-day period. Manual expression of the bladders was performed twice a day until the animals recovered spontaneous voiding.
Cell culture and treatment
Astrocytes were prepared from the spinal cord of newborn Sprague–Dawley rats, 1–2 days after birth for maximum homogeneity, and the astrocytes were isolated and cultured according to previously described methods. Briefly, the cells were enzymatically dissociated using 0.25% trypsin (Gibco, cat. no. 25200056) for 6 min at 37 °C, and the suspension was then centrifuged at 1200 rpm for 5 min and cultured in 1:1 Dulbecco’s modified Eagle’s medium: Ham’s F-12 medium (Sigma, cat. no. FG4815) supplemented with 10% fetal bovine serum (FBS, Gibco, cat. no. 16140071), 0.224% NaHCO3, and 1% penicillin/streptomycin (Beyotime, cat. no. C0222) in the presence of 5% CO2. A monolayer of astrocytes was obtained 12–14 days after plating. Non-astrocytes were detached from the flasks by shaking and were removed by changing the medium. Third or fourth passage cells were rendered quiescent through incubation in medium containing 0.5% FBS for 4 days prior to the experiments. The astrocyte phenotype was confirmed by cells exhibiting a characteristic morphology and positive staining for the astrocytic marker glial fibrillary acid protein (GFAP, 1:400, Sigma, cat. no. G3893).
Western blot
Protein was extracted from cells with a buffer containing 1% SDS, 100 mM Tris-HCl, 1 mM PMSF, and 0.1 mM β-mercaptoethanol, following treatment with 0–2.5 µg/ ml rat recombinant HMGB1 (Biomatik, cat. no. RPC28181) protein for 24 h. Alternatively, protein was extracted from 1 cm segments of the injured site at 0 days, 1 days, 4 days, and 1 week following contusion (n = 6 at each time point). The protein concentration of each sample was measured by the Bradford method (Beyotime, cat. no. P0006C) to maintain the same load. Protein extracts were heat denatured at 95 °C for 5 min, electrophoretically separated via 10% SDS‒PAGE (Beyotime, cat. no. P0012A), and transferred to PVDF membranes (Beyotime, cat. no. FFP70). The membranes were subjected to a reaction with a 1:1000 dilution of primary antibodies in TBS buffer at 4 °C for 36 h, followed by a reaction with a secondary antibody conjugated with a goat anti-rabbit (Beyotime, cat. no. A0216) or goat anti-mouse HRP dilution of 1:1000 (Beyotime, cat. no. A0208) at room temperature for 2 h. After the membrane was washed, HRP activity was detected using an ECL kit (Beyotime, cat. no. P0018M). The images were scanned with a GS800 Densitometer Scanner (Bio-Rad), and the data were analyzed via PDQuest 7.2.0 software (Bio-Rad). β-actin was used as an internal control. The following antibodies were used for Western blotting. HMGB1 (1:500, Cayman Chemical, cat. no. 11515); p-ERK (1:1000, CST, cat. no. 4370 S); ERK (1:1000, CST, cat. no. 9102 L); p-JNK (1:1000, CST, cat. no. 9251 L); JNK (1:1000, CST, cat. no. 9252T); p-P38 (1:1000, CST, cat. no. 4511T); P38 (1:1000, CST, cat. no. 8690T); p-p65NF-κB (1:1000, CST, cat. no. 3033 S); p65NF-κB (1:1000, CST, cat. no. 8242T) and β-actin (1:5000, Proteintech, cat. no. 66009-1-Ig).
ELISA
Primary astrocytes were cultured in six-well plates (1.5 × 105 cells/well) for 24 h, followed by stimulation with 0–2.5 µg/ml recombinant rat HMGB1 for 24 h before the assay. For the use of a specific inhibitor of HMGB1-mediated astrocyte production of CCL5, astrocyte was treated with the selective RAGE inhibitor FPS-ZM1 (MCE, cat. no. HY-19370), the TLR2 inhibitor C29 (MCE, cat. no. 363600-92-4), the TLR4 inhibitor TAK-242 (sigma, cat. no. 614316), the P38 inhibitor B203580 (TOCRIS, cat. no. 1202), the JNK inhibitor SP600125 (TOCRIS, cat. no. 1496), the ERK inhibitor PD98059 (TOCRIS, cat. no. 1213), or the NF-κB inhibitor SN50 (MCE, cat. no. HY-P0151) for 24 h. Cell supernatants were harvested, and cells and tissue samples were lysed in buffer containing 1% SDS, 100 mM Tris-HCl, 1 mM PMSF, and 0.1 mM β-mercaptoethanol. The lysates were centrifuged at 12,000×g for 15 min. CCL5 levels (R&D systems, cat. no. MMR00) were assessed via ELISA kits according to the manufacturer’s directions. The plates were read via a 96-well plate reader (Biotek Synergy2) at a wavelength of 450 nm.
Tissue immunofluorescence staining
The vertebra segments were harvested from six experimental models at each time point, postfixed, and sectioned. The sections were blocked with 0.01 M PBS containing 3% BSA (Beyotime, cat. no. ST023), 0.1% Triton X-100 (Beyotime, cat. no. P0096), 10% normal goat serum (Bioss, cat. no. C-0005) and/or 10% normal donkey serum (Rockland Immunochemicals, Inc, cat. no. D120-00-0050) for 1 h at 37 °C. Thereafter, the sections were incubated with different primary antibodies against GFAP (1:400, Sigma), CCL5 (1:200, Bioss, cat. no. bs-1324R), IBA-1 (1:500, Wako, cat. no. 019-19741) or CD68 (1:200, Bioss, cat. no. bs-1324R) at 4 °C for 36 h. The sections were further incubated with the Cy3-labelled goat anti-rabbit IgG (1:400, Abcam, cat. no. ab97075) or the Alexa Fluor 488-labeled donkey anti-mouse IgG (1:400, Abcam, cat. no. ab150109) for 24 h at 4 °C. The sections were observed under a fluorescence microscope (ZEISS, axio image M2). Next, 10 fields of each section were randomly selected from one sample, and the intensity of immunolabeled cells in the spinal cord was analyzed using Image-Pro Plus 6.0 software (Media Cybernetics, Rockville, Md, USA).
Cell viability assay
The effects of FPS-ZM1, C29 or TAK-242 on astrocyte viability were assayed by a CCK8 (Dojindo, Kumamoto, Japan, cat. no. CK04) assay according to the manufacturer’s instructions. In brief, the astrocytes were seeded in 96-well plates at a density of 6 × 103 cells/well and cultured for 24 h. The cells were treated with different concentrations of inhibitors; subsequently, the culture medium was discarded, and 10 µl of CCK-8 solution was added to the 96-well plates for 2 h at 37 °C, and the absorbance was subsequently measured at 450 nm with a microplate reader (BioTek, Synergy2).
Transwell migration assay
A transwell migration assay of BV2 microglia cells or RAW264.7 macrophages were performed using 6.5-mm transwell chambers with 8-µm pores (Costar, Cambridge, MA, cat. no. 3422). Briefly, the upper chamber was filled with 200 µl of BV2 microglia or RAW264.7 macrophages (3 × 105 cells/ml) in serum-free medium, the lower chamber was filled with 0.1 µg/ml rat recombinant CCL5 (rCCL5, PeproTech, cat. no. 400 - 13) or astrocyte-conditioned medium (ACM) for 48 h. Astrocytes were treated with 0.5 µg/ml rat recombinant HMGB1 for 24 h, and the supernatant was collected and incubated with 2.5 µg/ml IgG or CCL5 neutralizing antibody for 4 h to produce conditioned medium. After migration for 48 h, the upper surface of each membrane was cleaned with a cotton swab. The cells attached to the bottom surface of each membrane were stained with 0.1% crystal violet (Beyotime, cat. no. C0121), imaged using a DMR inverted microscope (Leica Microsystems, Bensheim, Germany) and counted using Image-Pro Plus 6.0 software (Media Cybernetics, Rockville, Md, USA). 6 random fields for each group were photographed for counting purposes. Experiments were performed three times independently.
Hematoxylin‑eosin (HE) staining
The tissues were cut into 20 μm thick sections and stained using the hematoxylin-eosin staining method according to the protocol (Beyotime, cat. no. C0105S). Briefly, the sections were stained with hematoxylin solution for 5 min followed by 5 dips in 1% acid ethanol (1% HCl in 70% ethanol) and then rinsed in distilled water. Then the sections were stained with eosin solution for 3 min followed by dehydration with graded alcohol and clearing in xylene. Thereafter, the sections were observed under a fluorescence microscope (ZAISS, axio image M2). The lesion area was analyzed using Image-Pro Plus 6.0 software.
Quantitative real-time polymerase chain reaction
Total RNA was prepared with Trizol (Gibco, cat. no. 15596018CN) from BV2 microglia cells or RAW264.7 macrophages treated with 0.1 µg/ml rat recombinant CCL5 or astrocytes conditioned medium (ACM) for 24 h. Astrocytes were treated with 0.5 µg/ml rat recombinant HMGB1 for 24 h, and the supernatant was collected and incubated with 2.5 µg/ml IgG or CCL5 neutralizing antibody for 4 h to produce a conditioned medium. The first-strand cDNA was synthesized using the reverse transcription Kit according to the manufacturer’s protocol (Vazyme, cat. no. R423). Then, qRT-PCR was performed using the SYBR Green Real-time PCR Master Mix Kit (Vazyme, cat. no. R423). The sequence-specific primers were designed, synthesized by Invitrogen (Shanghai, China), and listed in Table 1. The expression levels were normalized to an endogenous β-actin. The comparative cycle threshold (Ct) method (2−ΔΔCt) was used to calculate the relative expression of mRNA.
Behavioral testing
Hindlimb locomotor function recovery was assessed by the Basso, Beattie, and Bresnahan (BBB) scale as described previously37. The assessment was performed 0, 7, 14, 21 and 28 days after injury. Three well-trained investigators were invited to observe the behavior of the rats for 5 min. All the tests were performed by blinded observers. The BBB score ranges from 0 to 21 according to the rating scale. A score of 0 indicates no movement, whereas a score of 21 indicates normal movement without locomotor disorders. Every rat had a BBB score of 21 before surgery, and 0 to 1 after successful SCI.
Statistical analysis
All the data are presented as the mean ± SD and were analyzed using GraphPad Prism 8 software (San Diego, CA, USA). The statistical significance of differences between groups was analyzed by two-tailed unpaired Student’s t test, one-way or two-way analysis of variance (ANOVA) followed by Dunnett’s or Tukey’s post-hoc comparisons. Statistical significance was set to *P < 0.05.
Results
Activation of the chemokine CCL5 in astrocytes is regulated by HMGB1 expression following spinal cord contusion
To determine whether HMGB1 expression correlates with CCL5 production by astrocytes after SCI, we first measured the protein levels determination of CCL5 and HMGB1 in the contused spinal cord at different time points. The data revealed that the protein levels of CCL5 increased synchronously with the increase in HMGB1 at the lesion site from 1 d onwards, with a peak at 4 d after SCI (Fig. 1A–C). The administration of 10 µl of an HMGB1 neutralizing antibody (HMGB1 Ab, 50 µg/kg) to the lesion site resulted in a marked reduction in CCL5 production on various days (Fig. 1D). These data indicate that HMGB1 efficiently regulates CCL5 production following SCI.
As chemokines are primarily produced in astrocytes following CNS tissue damage13,21,38, we next analyzed the potential regulatory role of HMGB1 in the production of the astrocytic chemokine CCL5. Immunofluorescence staining revealed that CCL5 production was significantly increased in GFAP-positive cells at 4 d following SCI, whereas the injection of 10 µl of an HMGB1 neutralizing antibody at the lesion site markedly decreased the expression of CCL5 in astrocytes (Fig. 1E). These data indicate that SCI-induced expression of HMGB1 drives CCL5 production by astrocytes.
Changes in CCL5 and HMGB1 protein levels changes at lesion sites following rat SCI. (A) ELISA measurement of CCL5 protein levels at lesion sites following SCI at 0 d, 1 d, 4 d and 7 d, respectively. (B) Western blot analysis of HMGB1 expression following SCI at 0 d, 1 d, 4 d and 7 d. (C) Quantification data are shown in (B). Quantities were normalized to endogenous β-actin. (D) ELISA analysis of CCL5 protein levels at lesion sites at 0 d, 1 d, 4 d and 7 d following with or without intrathecal injection of 10 µl of an HMGB1 neutralizing antibody (HMGB1 Ab, 50 µg/kg). (E) Immunofluorescence staining revealed the colocalization of CCL5 with GFAP-positive astrocytes before or after SCI at 4 d with or without the intrathecal injection of 10 µl of HMGB1 Ab (50 µg/kg). The rectangle indicates the region magnified. Arrowheads indicate positive signals. n = 6. Scale bars, 50 μm in (E). The experiments were performed in triplicate. The error bars represent the standard deviation (*P < 0.05, **P < 0.01).
HMGB1 robustly facilitates the production of CCL5 from astrocytes through TLR2/4 receptors
To further investigate the regulatory relationship between HMGB1 and CCL5 in astrocytes, primary cultured astrocytes with a purity exceeding 90% were exposed to 0–2.5 µg/ml rat recombinant HMGB1 (rHMGB1) for 24 h. ELISA measurements of the cell supernatants and lysates revealed that cell treatment with various concentrations of HMGB1 robustly promoted the production of CCL5 from astrocytes in a dose-dependent manner (Fig. 2A–D). The treatment of astrocyte with 2.5 µg/ml HMGB1 Ab in the presence of 0.5 µg/ml rHMGB1 markedly reduced the production of CCL5 from astrocytes (Fig. 2E and F). These data indicate that HMGB1 promotes the production of CCL5 from astrocytes.
Examination of CCL5 production in astrocytes following stimulation with rHMGB1. (A, B) Purified primary astrocytes were stained with GFAP and Hoechst 33,342, and the purity was greater than 90%. Scale bar, 50 μm. (C, D) ELISA analysis of CCL5 in the lysates and supernatants of primary astrocytes following stimulation with 0–2.5 µg/mL rat recombinant HMGB1 (rHMGB1) for 24 h, respectively. (E, F) ELISA assay was used to determine the production of CCL5 in the lysates and supernatants following primary astrocyte treatment with 0.5 µg/ml rHMGB1 in the presence of 2.5 µg/ml HMGB1 Ab, respectively. The experiments were performed in triplicate. The error bars represent the standard deviation (*P < 0.05, **P < 0.01, ***P < 0.001).
HMGB1 has been demonstrated to participate in the production of multiple inflammatory mediators after CNS insults through several pattern-recognition receptors, including TLR-2, TLR-4 and RAGE31,32. To determine whether HMGB1-mediated CCL5 elevation is regulated by three receptors, the 2 µM RAGE inhibitor FPS-ZM1, the 10 µM TLR2 inhibitor C29 or the 2 µM TLR4 inhibitor TAK-242 inhibitor were added to the culture medium of astrocytes in the presence of 0.5 µg/ml rHMGB1 for 24 h. ELISA results revealed that the protein levels of CCL5 in the supernatants and lysates were markedly decreased following astrocyte treatment with C29 or TAK-242. However, astrocyte treatment with FPS-ZM1 did not affect the protein level of CCL5. A CCK-8 cell viability test revealed that the three inhibitors had no effect on astrocyte viability (Fig. 3). Collectively, these data indicate that HMGB1 can potently induce CCL5 production from astrocytes through TLR2/4 receptors.
Effects of RAGE, TLR-2, or TLR-4 interference on HMGB1-induced CCL5 production in astrocytes. (A, B) Cell lysates and supernatants were tested by ELISA for the production of CCL5, following astrocyte treatment with 0.5 µg/ml rHMGB1 in the presence of the RAGE inhibitor FPS-ZM1 (2 µM) for 24 h. (D, E) ELISA was used to determine CCL5 protein levels in lysates and supernatants from astrocytes after stimulation with 0.5 µg/ml rHMGB1 in the presence of the TLR2 inhibitor C29 (10 µM) for 24 h. (G, H) CCL5 levels in lysates and supernatants of astrocytes were determined by ELISA after the astrocytes were treated with the TLR4 inhibitor TAK-242 (2 µM) in the presence of 0.5 µg/ml rHMGB1 for 24 h. (C,F, I) CCK8 assay of the effects of FPS-ZM1, C29, or TAK-242 on the viability of astrocytes. The experiments were performed in triplicate. The error bars represent the standard deviation (*P < 0.05, **P < 0.01).
HMGB1-mediated CCL5 production in astrocytes is attributed to MAPK/NF‑κB pathway activation
The mitogen-activated protein kinase (MAPK)/NF-kappaB (NF-κB) pathway plays a critical role in the HMGB1-triggered inflammatory activation of astrocytes in the CNS39,40. To elucidate the mechanisms of HMGB1-induced CCL5 production from astrocytes. The MAPK/NF-κB pathway was analyzed following primary astrocyte treatment with 0–2.5 µg/ml rHMGB1 for 24 h. The results revealed that exposure of astrocytes to rHMGB1 efficiently promoted the phosphorylation of the ERK, P38, JNK kinase and p65NF-κB proteins in a dose-dependent manner (Fig. 4).
Determination of CCL5 synthesis-related protein levels in astrocytes following stimulation with rHMGB1. (A) Western blot analysis of the phosphorylation of the ERK, JNK, P38 kinase and p65NF-κB proteins after astrocytes were treated with 0–2.5 µg/mL rHMGB1 for 24 h. (B-E) Quantification data are shown in (A). Quantities were normalized to endogenous β-actin. The experiments were performed in triplicate. The error bars represent the standard deviation (*P < 0.05, **P < 0.01, ***P < 0.001).
To clarify whether HMGB1-induced activation of the MAPK/NF-κB pathway is involved in the production of CCL5 in astrocytes, a selective inhibitor of extracellular signal-regulated kinases (ERK, PD98059), c-Jun N-terminal kinase (JNK, SP600125) or P38 mitogen-activated protein kinase (P38, SB203580) was added to the culture medium of astrocytes in the presence of 0.5 µg/ml rHMGB1. The results revealed that 10 µM of the ERK inhibitor PD98059 or 10 µM of the JNK inhibitor SP600125 markedly decreased the HMGB1-induced production of CCL5, whereas 10 µM of the P38 inhibitor SB203580 had no effect (Fig. 5A and B). Accordingly, the phosphorylated activation of p65NF-κB was also markedly attenuated by the ERK or JNK inhibitors (Fig. 5C and D). The production of HMGB1-stimulated CCL5 in lysates and supernatants was also attenuated by 10 µM p65NF-κB inhibitor SN50 (Fig. 5E and F). These data indicate that ERK/JNK-mediated NF-κB activation is indispensable for HMGB1-induced astrocytic CCL5 production.
Effects of the inhibition of MAPK/NF-κB signaling on the HMGB1-induced production of CCL5 from astrocytes. (A, B) ELISA was used to determine the effects of 10 µM ERK inhibitor PD98059, 10 µM JNK inhibitor SP6001251 or 10 µM P38 inhibitor SB203580 in the presence of 0.5 µg/ml rHMGB1 for 24 h on CCL5 protein production levels in lysates and supernatants of astrocytes. (C) Western blot analysis of the activation of p65NFκB protein after astrocyte treatment with 10 µM ERK inhibitor PD98059 or 10 µM JNK inhibitor SP6001251 for 24 h in the presence of 0.5 µg/ml rHMGB1. (D) Quantification data are shown in (C). Quantities were normalized to endogenous β-actin. (E, F) ELISA analysis of CCL5 in the lysates and supernatants of primary astrocytes following challenge with 10 µM SN50 for 24 h in the presence of 0.5 µg/ml rHMGB1, respectively. The experiments were performed in triplicate. The error bars represent the standard deviation (*P < 0.05, **P < 0.01, ***P < 0.001).
HMGB1-mediated expression and release of CCL5 from astrocytes actively participate in the recruitment of microglia/macrophage
Chemokines, which are recognized as major contributors to driving the migration of microglia/macrophages migrates to sites of tissue damage, have been shown to play crucial roles in the CNS after injury12,41. To reveal the function of CCL5 on the in recruitment of inflammatory cells, a Transwell assay was performed to examine the migration of BV2 microglia or RAW 264.7 macrophage cells cocultured with 0.1 µg/ml rat recombinant CCL5 (rCCL5) for 48 h. Compared with the control cells, both BV2 and RAW 264.7 cells stimulated with rCCL5 exhibited increased migratory ability (Fig. 6A-D). To further elucidate the role of HMGB1-mediated CCL5 release by astrocytes in the recruitment of BV2 or RAW 264.7 cells, astrocyte-conditioned medium (ACM) was established by treating astrocytes with 0.5 µg/ml rHMGB1 for 24 h, after which the supernatant was collected and incubated with 2.5 µg/ml IgG or CCL5 Ab for 4 h. Transwell assays revealed that ACM, which was established with the CCL5 Ab in the presence of the collected supernatant, markedly inhibited HMGB1-induced BV2 and RAW 264.7 cells migration (Fig. 6E-H). These data indicate that HMGB1-mediated astrocytic CCL5 expression and release are involved in promoting the migration of microglia/macrophage.
Effects of HMGB1-mediated astrocytic CCL5 on the migration of BV2 microglia cells or RAW 264.7 macrophage cells in vitro. (A) Illustration of the BV2 or RAW 264.7 cells with rCCL5 coculture model. (B) Transwell assay analysis of migration the ability of BV2 or RAW 264.7 cells co-incubated with 0.1 µg/ml rCCL5 for 48 h. (C) and (D) Quantification data are shown in (B). (E) Illustration of the BV2 or RAW 264.7 cells and ACM coculture model. (F) Migration assay of BV2 or RAW 264.7 cells cocultured with ACM. ACM were prepared from astrocytes exposed to 0.5 µg/ml rHMGB1 for 24 h, followed by the supernatant was collected and incubated with 2.5 µg/ml IgG or CCL5 Ab for 4 h. (G) and (H) Quantification data are shown in (F). Scale bars, 100 μm in (B) and (F). The experiments were performed in triplicate. The error bars represent the standard deviation (*P < 0.05, **P < 0.01, ***P < 0.001).
HMGB1-regulated astrocytic CCL5 promotes M1 polarization of microglia/macrophage
Microglia/macrophage polarization state changes between pro-inflammatory phenotype (M1) and anti-inflammatory (M2) have been suggested as a huge factor in inflammatory responses in SCI pathophysiology42,43. To reveal the impact of HMGB1-induced astrocytic CCL5 on microglia/macrophage polarization, qRT-PCR was conducted to assess the polarization of BV2 microglia or RAW 264.7 macrophage cells cocultured with 0.1 µg/ml rat recombinant CCL5 (rCCL5) or ACM for 24 h. The results demonstrated that rCCL5 greatly induced M1 polarization in both BV2 and RAW 264.7 cells (Fig. 7A and B). Furthermore, the presence of CCL5 Ab in ACM notably reduced HMGB1-induced M1 polarization in BV2 and RAW 264.7 cells (Fig. 7C and D). The data indicate that HMGB1-induced astrocytic CCL5 enhances M1 polarization of microglia/macrophage.
Effects of HMGB1-induced astrocytic CCL5 on microglia/macrophage polarization. (A) and (B) qRT-PCR was used to determine the expression of M1 markers (CD86, iNOS and TNF-a) and M2 markers (CD206, Arg1 and Ym1) after BV2 or RAW 264.7 cells incubated with 0.1 µg/ml rCCL5 for 24 h. (C) and (D) The expression levels of M1 and M2 markers were determined by qRT-PCR following BV2 or RAW 264.7 cells cocultured with ACM for 24 h. ACM was prepared by astrocytes challenge with 0.5 µg/ml rHMGB1 for 24 h, after which the supernatant was collected and incubated with 2.5 µg/ml IgG or CCL5 Ab for 4 h. The experiments were performed in triplicate. The error bars represent the standard deviation (*P < 0.05, **P < 0.01, ***P < 0.001).
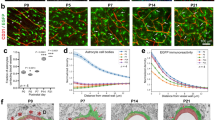
Administration of a HMGB1- or CCL5-neutralizing antibody reduces microglia/macrophage infiltration and improves motor functional recovery following SCI
To further elucidate the role of HMGB1-induced CCL5 in the migration of microglia/macrophages following SCI, 10 µl of neutralizing antibodies HMGB1 (HMGB1 Ab, 50 µg/kg) or CCL5 (CCL5 Ab, 50 µg/kg) was intrathecally injected into the lesion site immediately after spinal cord contusion. Immunofluorescence staining revealed that blocking HMGB1 or CCL5 significantly reduced the intensity of IBA1-labeled microglia/macrophages or CD68- labeled macrophages at the lesion area at 4 d after SCI (Fig. 8A-C).
To assess the influences of HMGB1 or CCL5 on lesion size and functional recovery. HE staining was first performed to observe the lesion area in the damaged cord tissues, and the data revealed that HMGB1 Ab or CCL5 Ab treatment remarkedly reduced the lesion size of the cord at 21 d post-injury in comparison with the vehicle (Fig. 8D and E). Subsequently, hindlimb locomotor function was evaluated by BBB scores after the blockade of HMGB1 or CCL5 activity in SCI rats. Compared with vehicle treatment, the application of HMGB1 Ab or CCL5 Ab significantly improved the hindlimb locomotor function of the rats from 7 d onwards compared with the vehicle group (Fig. 8F). These data indicate that the inhibition of HMGB1-mediated CCL5 production decreases the recruitment of microglia/macrophages at the lesion site and improves motor function following rat SCI.
Immunofluorescence of microglia/macrophage and locomotor function assessment after the inhibition of HMGB1 or CCL5 by neutralizing antibodies in rat SCI. (A) Immunofluorescence of IBA1- or CD68-positive cells at 4 d following SCI after neutralizing antibody application by intrathecal injection of 10 µl of neutralizing antibodies (HMGB1 Ab, 50 µg/kg), CCL5 (CCL5 Ab, 50 µg/kg) or normal rabbit IgG (IgG, 50 µg/kg). n = 6. Scale bars, 50 μm. (B, C) Quantitative analysis of the intensity of IBA1- or CD68-labeled cells in (A), respectively. (D) HE staining of the injured spinal cord at 21 d after administration of 10 µl of HMGB1, CCL5 neutralizing antibodies or normal rabbit IgG. n = 6. Scale bars, 500 μm. (E) Quantification data are shown in (D). (F) Basso, Beattie, and Bresnahan (BBB) locomotor scale scores for hindlimb motor function in rats at 0 d, 7 d, 14 d, 21 d and 28 d following the intrathecal administration of the HMGB1 Ab, CCL5 Ab or normal rabbit IgG. n = 6. The experiments were performed in triplicate. The error bars represent the standard deviation (*P < 0.05, **P < 0.01, ***P < 0.001).
Discussion
The secondary phase of traumatic SCI usually initiates a cascade of pathophysiological events, including neuroinflammation, ischemia, excitotoxicity, free radical formation, and edema, which results in tissue loss and neurological function disorders44,45. Multiple biological events and cellular mechanisms are involved in pathological processes44,46, among which neuroinflammation is a key determinant of secondary due to the regions associated with injury involve the activation and infiltration of many inflammatory cells3,45. Resident microglia and infiltrating immune cells act as key regulators of the inflammatory cascades by releasing a variety of inflammatory mediators after SCI47. Interestingly, microglia/macrophage activation and infiltration are mediated by astrocyte-induced chemokine expression48. Chemokine expression is upregulated within minutes to hours, and lasts for hours to days, depending on the severity of the injury12,49, and activated astrocytes have been suggested to be responsible for the expression of chemokines13,17,21. In this study, we found that CCL5 expression was rapidly induced in astrocytes in the injured spinal cord, and that the astrocyte-derived chemokine CCL5 can tune the inflammatory microenvironment by recruiting leukocytes to damaged tissue following SCI.
After SCI, microglia/macrophages play a dual role in promoting both secondary injury and repair processes, which can be attributed to distinct subsets of those cells42,43. Two main subsets have been characterized: pro-inflammatory (M1) or anti-inflammatory (M2) cells. In vitro, M1 microglia/macrophages were induced by lipopolysaccharide (LPS) or interferon-gamma (IFN-gamma). While IL-4 or IL-13 promotes an M2 phenotype42,43,50. The activated M1 microglia/macrophages produce pro-inflammatory cytokines, including IL-1β, IL-6, IL-12, and IL-23, as well as cytotoxic mediators such as reactive oxygen species (ROS). This contributes to secondary tissue damage and axonal retraction after SCI. Conversely, M2 polarization may underlie the protective effects in axon growth and angiogenesis by releasing IL-10 and transforming growth factor-beta (TGF-β)42,43,51. Of note, in the early stages after injury, the microenvironment favored the M1 polarization phenotype, and only a small number of M2 macrophages were present42,52. Neuroinflammation induced by M1 microglia/macrophages is a significant pathological manifestation after SCI. In this study, we found that HMGB1-induced astrocytic CCL5 promotes M1 polarization of microglia/macrophages in vitro. Additionally, sexual dimorphism in immune responses leads to differences in incidence rates in autoimmune disease between males and females53,54. Whether the immune response is sex-dependent after SCI is not completely clear and is partly controversial55,56. Herein, we only used male rats as an experimental model, the effects of sex on immune cells after SCI which need further research.
The chemokine CCL5 is widely present in astrocytes, and neurons of the CNS and plays an important role in regulating immune cell differentiation and migration, and maintaining inflammatory reactions13,21. CCL5 is dramatically induced within a variety of cell types to recruit macrophages, monocytes, and T cells to the site of inflammation accelerating CNS inflammation and consequently increasing the severity of damage14,18. In the present study, our in vivo and in vitro data suggested that CCL5 primarily facilitates the migration of microglia/macrophages. These data indicate that CCL5 activity inhibition is a therapeutic target in neuroinflammatory diseases. CCL5 expression is induced by multiple proinflammatory cytokines. The expression of CCL5 is increased following the stimulation of astrocytes with the cytokines TNF-a and IL-1β in the CNS57. Lipopolysaccharide-induced astrocyte activation also promotes the expression and secretion of CCL5 after SCI in vivo19. In the present study, we showed that SCI-induced HMGB1 is a potent inducer of CCL5 production in astrocytes.
HMGB1, also known as amphotericin or HMG1, is a chromosomal nonhistone protein named for its high electrophoretic mobility in polyacrylamide gels23,25. It is involved in several inflammatory pathological conditions such as ischemic stroke, traumatic brain injury, Alzheimer’s disease, and multiple sclerosis25,58. After SCI, HMGB1 is rapidly expressed and released by astrocytes, neurons, and microglia/macrophages, which in turn activates microglial and astrocytic inflammatory responses in autocrine and paracrine manners27,30. HMGB1 mediates proinflammatory cytokine production contributing to an inflammatory microenvironment29,59. Several lines of evidence have shown that HMGB1 recruits leukocytes to the site of tissue damage via the formation of a heterocomplex with the homeostatic chemokine CXCL12 in other CNS diseases34,35. Furthermore, HMGB1 mediates monocyte transendothelial migration in an autocrine/paracrine manner60. Interestingly, HMGB1 not only recruits but also inhibits migration in some cells. For example, in pulmonary hypertension, HMGB1 inhibits human pulmonary artery endothelial cell migration61. In the present study, we revealed that HMGB1 indirectly induced the migration of immune cells to lesion sites by promoting the production of CCL5 by astrocytes in an early stage following SCI. Besides the pro-inflammatory effects of SCI, HMGB1 also plays a crucial role in promoting angiogenesis during the recovery phase following SCI in adult zebrafish and stroke in rats62,63. Therefore, it can be inferred that HMGB1 may contribute to nervous system regeneration, at least partially, by facilitating angiogenesis during the post-recovery stage of SCI.
Different receptor systems have been reported to interact with extracellular HMGB1, and only TLR2/4 and RAGE have been confirmed to act as specific HMGB1 receptors31,32,59. TLR2/4 and RAGE are expressed in astrocytes, macrophages/microglia, and neurons of the CNS64,65. HMGB1 is elevated and released from reactive astrocytes, which induces proinflammatory cytokine production in microglia and astrocytes by TLR2, TLR4 and/or RAGE after CNS injury64,65,66. The interaction of HMGB1 with TLR2, TLR4 and/or RAGE results in the activation of the ERK, JNK, and p38 MAPK kinases and downstream NF-κB pathways67,68,69,70,71, thereby leading to an inflammatory response. In this study, we not only investigated the roles of receptors in HMGB1-induced astrocytic CCL5 expression but also explored the regulatory mechanism involved. We demonstrated that HMGB1-induced CCL5 production in astrocytes is regulated by ERK/JNK-mediated NF-κB pathway activation, and depends on TLR2/4 receptors. In addition, CCL5 may also be induced by HMGB1 in microglia, as these cells can activate the NF-κB pathway and express the TLR2 and TLR4 receptors59,66. These findings suggest the functional significance of the TLR2/4 receptor and MAPK/NF-κB signaling pathways in HMGB1-induced proinflammatory mediator production.
Conclusion
As shown in Fig. 9, SCI-induced HMGB1 binds to TLR2/4 receptors to facilitate CCL5 production from astrocytes via intracellular ERK/JNK-mediated NF-κB pathway activation, which in turn promotes the recruitment of microglia/macrophages and exacerbates the inflammatory milieu. Inhibition of HMGB1 or CCL5 immediately after SCI decreases the accumulation of microglia/macrophages at the lesion site, thereby contributing to ameliorating locomotor functional deficits in rats.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CNS:
-
Central nervous system
- SCI:
-
Spinal cord injury
- DAMP:
-
Damage-associated molecular pattern
- HMGB1:
-
High mobility group box 1
- CCL5:
-
C-C motif Chemokine Ligand 5/RANTES
- TLR4:
-
Toll-like receptor 4
- RAGE:
-
Receptor for advanced glycation end product
- PRRs:
-
Pattern-recognition receptors
- MAPK:
-
Mitogen-activated protein kinases
- NF-κB:
-
Nuclear factor kappa-B
- ANOVA:
-
Analysis of variance
- GFAP:
-
Glial fibrillary acid protein
References
Eli, I., Lerner, D. P. & Ghogawala, Z. Acute traumatic spinal cord injury. Neurol. Clin.39, 471–488. https://doi.org/10.1016/j.ncl.2021.02.004 (2021).
Alexander, M. Pandemics, climate change, and disability related to SCI. Spinal Cord Ser. Cases. 6, 36. https://doi.org/10.1038/s41394-020-0285-6 (2020).
Hellenbrand, D. J. et al. Inflammation after spinal cord injury: a review of the critical timeline of signaling cues and cellular infiltration. J. Neuroinflamm.18, 284. https://doi.org/10.1186/s12974-021-02337-2 (2021).
Ding, Y. & Chen, Q. The NF-kappaB pathway: a focus on inflammatory responses in spinal cord injury. Mol. Neurobiol.60, 5292–5308. https://doi.org/10.1007/s12035-023-03411-x (2023).
Taoka, Y. & Okajima, K. Role of leukocytes in spinal cord injury in rats. J. Neurotrauma17, 219–229. https://doi.org/10.1089/neu.2000.17.219 (2000).
Rice, T., Larsen, J., Rivest, S. & Yong, V. W. Characterization of the early neuroinflammation after spinal cord injury in mice. J. Neuropathol. Exp. Neurol.66, 184–195. https://doi.org/10.1097/01.jnen.0000248552.07338.7f (2007).
Gadani, S. P., Walsh, J. T., Lukens, J. R. & Kipnis, J. Dealing with danger in the CNS: the response of the immune system to injury. Neuron87, 47–62. https://doi.org/10.1016/j.neuron.2015.05.019 (2015).
Faden, A. I., Wu, J., Stoica, B. A. & Loane, D. J. Progressive inflammation-mediated neurodegeneration after traumatic brain or spinal cord injury. Br. J. Pharmacol.173, 681–691. https://doi.org/10.1111/bph.13179 (2016).
Colombo, E., Farina, C. & Astrocytes Key regulators of neuroinflammation. Trends Immunol.37, 608–620. https://doi.org/10.1016/j.it.2016.06.006 (2016).
Linnerbauer, M., Wheeler, M. A. & Quintana, F. J. Astrocyte crosstalk in CNS inflammation. Neuron108, 608–622. https://doi.org/10.1016/j.neuron.2020.08.012 (2020).
Carpentier, P. A. et al. Differential activation of astrocytes by innate and adaptive immune stimuli. Glia49, 360–374. https://doi.org/10.1002/glia.20117 (2005).
Gyoneva, S. & Ransohoff, R. M. Inflammatory reaction after traumatic brain injury: therapeutic potential of targeting cell-cell communication by chemokines. Trends Pharmacol. Sci.36, 471–480. https://doi.org/10.1016/j.tips.2015.04.003 (2015).
Julian-Villaverde, F. J., Serrano-Ponz, M., Ramalle-Gomara, E. & Martinez, A. Ochoa-Callejero, L. CCL5 levels predict stroke volume growth in acute ischemic stroke and significantly diminish in hemorrhagic stroke patients. Int. J. Mol. Sci.23https://doi.org/10.3390/ijms23179967 (2022).
de Nadai, P. et al. CCR5 usage by CCL5 induces a selective leukocyte recruitment in human skin xenografts in vivo. J. Investig Dermatol.126, 2057–2064. https://doi.org/10.1038/sj.jid.5700369 (2006).
Tavares, L. P. et al. ACKR2 contributes to pulmonary dysfunction by shaping CCL5:CCR5-dependent recruitment of lymphocytes during influenza A infection in mice. Am. J. Physiol. Lung Cell. Mol. Physiol.318, L655–L670. https://doi.org/10.1152/ajplung.00134.2019 (2020).
Sorce, S. et al. Increased brain damage after ischaemic stroke in mice lacking the chemokine receptor CCR5. Br. J. Pharmacol.160, 311–321. https://doi.org/10.1111/j.1476-5381.2010.00697.x (2010).
Knerlich-Lukoschus, F. & Held-Feindt, J. Chemokine-ligands/receptors: multiplayers in traumatic spinal cord injury. Mediat. Inflamm.2015 (486758). https://doi.org/10.1155/2015/486758 (2015).
He, B. et al. Sustainable inflammatory activation following spinal cord injury is driven by thrombin-mediated dynamic expression of astrocytic chemokines. Brain Behav. Immun.116, 85–100. https://doi.org/10.1016/j.bbi.2023.11.035 (2024).
Lin, M. S. et al. Curcumin attenuates the expression and secretion of RANTES after spinal cord injury in vivo and lipopolysaccharide-induced astrocyte reactivation in vitro. J. Neurotrauma28, 1259–1269. https://doi.org/10.1089/neu.2011.1768 (2011).
Brambilla, R. et al. Inhibition of astroglial nuclear factor kappaB reduces inflammation and improves functional recovery after spinal cord injury. J. Exp. Med.202, 145–156. https://doi.org/10.1084/jem.20041918 (2005).
McTigue, D. M. et al. Selective chemokine mRNA accumulation in the rat spinal cord after contusion injury. J. Neurosci. Res.53, 368–376 (1998).
Gangwani, M. R., Noel, R. J. Jr., Shah, A., Rivera-Amill, V. & Kumar, A. Human immunodeficiency virus type 1 viral protein R (vpr) induces CCL5 expression in astrocytes via PI3K and MAPK signaling pathways. J. Neuroinflamm.10, 136. https://doi.org/10.1186/1742-2094-10-136 (2013).
Takeda, T. et al. The combination of a nuclear HMGB1-positive and HMGB2-negative expression is potentially associated with a shortened survival in patients with pancreatic ductal adenocarcinoma. Tumour Biol.35, 10555–10569. https://doi.org/10.1007/s13277-014-2328-8 (2014).
Andersson, A. et al. Pivotal advance: HMGB1 expression in active lesions of human and experimental multiple sclerosis. J. Leukoc. Biol.84, 1248–1255. https://doi.org/10.1189/jlb.1207844 (2008).
Paudel, Y. N. et al. HMGB1: a common biomarker and potential target for TBI, neuroinflammation, epilepsy, and cognitive dysfunction. Front. Neurosci.12, 628. https://doi.org/10.3389/fnins.2018.00628 (2018).
Hayakawa, K. et al. High-mobility group box 1 from reactive astrocytes enhances the accumulation of endothelial progenitor cells in damaged white matter. J. Neurochem.125, 273–280. https://doi.org/10.1111/jnc.12120 (2013).
Kigerl, K. A., Lai, W., Wallace, L. M., Yang, H. & Popovich, P. G. High mobility group box-1 (HMGB1) is increased in injured mouse spinal cord and can elicit neurotoxic inflammation. Brain Behav. Immun.72, 22–33. https://doi.org/10.1016/j.bbi.2017.11.018 (2018).
Rovere-Querini, P. et al. HMGB1 is an endogenous immune adjuvant released by necrotic cells. EMBO Rep.5, 825–830. https://doi.org/10.1038/sj.embor.7400205 (2004).
Chen, K. B. et al. High mobility group box-1 serves a pathogenic role in spinal cord injury via the promotion of pro-inflammatory cytokines. J. Leukoc. Biol.110, 1131–1142. https://doi.org/10.1002/JLB.3MA0721-007R (2021).
Papatheodorou, A. et al. High-mobility group box 1 (HMGB1) is elevated systemically in persons with acute or chronic traumatic spinal cord injury. J. Neurotrauma34, 746–754. https://doi.org/10.1089/neu.2016.4596 (2017).
Park, J. S. et al. Involvement of toll-like receptors 2 and 4 in cellular activation by high mobility group box 1 protein. J. Biol. Chem.279, 7370–7377. https://doi.org/10.1074/jbc.M306793200 (2004).
Wang, J. et al. HMGB1 participates in LPS–induced acute lung injury by activating the AIM2 inflammasome in macrophages and inducing polarization of M1 macrophages via TLR2, TLR4, and RAGE/NF–kappaB signaling pathways. Int. J. Mol. Med.45, 61–80. https://doi.org/10.3892/ijmm.2019.4402 (2020).
Yang, J. et al. Hyperbaric oxygen alleviates experimental (spinal cord) injury by downregulating HMGB1/NF-kappaB expression. Spine38, E1641–E1648. https://doi.org/10.1097/BRS.0000000000000005 (2013).
Venereau, E., Schiraldi, M., Uguccioni, M. & Bianchi, M. E. HMGB1 and leukocyte migration during trauma and sterile inflammation. Mol. Immunol.55, 76–82. https://doi.org/10.1016/j.molimm.2012.10.037 (2013).
Venereau, E. et al. HMGB1 as biomarker and drug target. Pharmacol. Res.111, 534–544. https://doi.org/10.1016/j.phrs.2016.06.031 (2016).
Zhang, Y. et al. Macrophage migration inhibitory factor facilitates prostaglandin E(2) production of astrocytes to tune inflammatory milieu following spinal cord injury. J. Neuroinflamm.16, 85. https://doi.org/10.1186/s12974-019-1468-6 (2019).
Basso, D. M., Beattie, M. S. & Bresnahan, J. C. A sensitive and reliable locomotor rating scale for open field testing in rats. J. Neurotrauma12, 1–21. https://doi.org/10.1089/neu.1995.12.1 (1995).
Hayashi, M., Luo, Y., Laning, J., Strieter, R. M. & Dorf, M. E. Production and function of monocyte chemoattractant protein-1 and other beta-chemokines in murine glial cells. J. Neuroimmunol.60, 143–150. https://doi.org/10.1016/0165-5728(95)00064-9 (1995).
Pedrazzi, M. et al. Selective proinflammatory activation of astrocytes by high-mobility group box 1 protein signaling. J. Immunol.179, 8525–8532. https://doi.org/10.4049/jimmunol.179.12.8525 (2007).
Gaikwad, S. et al. Tau oligomer induced HMGB1 release contributes to cellular senescence and neuropathology linked to Alzheimer’s disease and frontotemporal dementia. Cell. Rep.36, 109419. https://doi.org/10.1016/j.celrep.2021.109419 (2021).
Biber, K., Vinet, J. & Boddeke, H. W. Neuron-microglia signaling: chemokines as versatile messengers. J. Neuroimmunol.198, 69–74. https://doi.org/10.1016/j.jneuroim.2008.04.012 (2008).
Kigerl, K. A. et al. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J. Neurosci.29, 13435–13444. https://doi.org/10.1523/JNEUROSCI.3257-09.2009 (2009).
David, S. & Kroner, A. Repertoire of microglial and macrophage responses after spinal cord injury. Nat. Rev. Neurosci.12, 388–399. https://doi.org/10.1038/nrn3053 (2011).
Sterner, R. C. & Sterner, R. M. Immune response following traumatic spinal cord injury: pathophysiology and therapies. Front. Immunol.13, 1084101. https://doi.org/10.3389/fimmu.2022.1084101 (2022).
Chio, J. C. T., Xu, K. J., Popovich, P., David, S. & Fehlings, M. G. Neuroimmunological therapies for treating spinal cord injury: evidence and future perspectives. Exp. Neurol.341, 113704. https://doi.org/10.1016/j.expneurol.2021.113704 (2021).
Widerstrom-Noga, E. Neuropathic pain and spinal cord injury: management, phenotypes, and biomarkers. Drugs. 83, 1001–1025. https://doi.org/10.1007/s40265-023-01903-7 (2023).
Brockie, S., Hong, J. & Fehlings, M. G. The role of microglia in modulating neuroinflammation after spinal cord injury. Int. J. Mol. Sci.22, 706. https://doi.org/10.3390/ijms22189706 (2021).
Tanuma, N., Sakuma, H., Sasaki, A. & Matsumoto, Y. Chemokine expression by astrocytes plays a role in microglia/macrophage activation and subsequent neurodegeneration in secondary progressive multiple sclerosis. Acta Neuropathol.112, 195–204. https://doi.org/10.1007/s00401-006-0083-7 (2006).
Jaerve, A. & Muller, H. W. Chemokines in CNS injury and repair. Cell. Tissue Res.349, 229–248. https://doi.org/10.1007/s00441-012-1427-3 (2012).
Shapouri-Moghaddam, A. et al. Macrophage plasticity, polarization, and function in health and disease. J. Cell. Physiol.233, 6425–6440. https://doi.org/10.1002/jcp.26429 (2018).
Busch, S. A., Horn, K. P., Silver, D. J. & Silver, J. Overcoming macrophage-mediated axonal dieback following CNS injury. J. Neurosci.29, 9967–9976. https://doi.org/10.1523/JNEUROSCI.1151-09.2009 (2009).
Zhang, Q. et al. Targeting of MALT1 may improve functional recovery and attenuate microglia M1 polarization-mediated neuroinflammation during spinal cord injury. Mol. Neurobiol.60, 2632–2643. https://doi.org/10.1007/s12035-023-03208-y (2023).
Gal-Oz, S. T. et al. ImmGen report: sexual dimorphism in the immune system transcriptome. Nat. Commun.10, 4295. https://doi.org/10.1038/s41467-019-12348-6 (2019).
Gold, S. M., Willing, A., Leypoldt, F., Paul, F. & Friese, M. A. Sex differences in autoimmune disorders of the central nervous system. Semin. Immunopathol.41, 177–188. https://doi.org/10.1007/s00281-018-0723-8 (2019).
Stewart, A. N. et al. Acute inflammatory profiles differ with sex and age after spinal cord injury. J. Neuroinflamm.18https://doi.org/10.1186/s12974-021-02161-8 (2021).
Skinnider, M. A. et al. Single-cell and spatial atlases of spinal cord injury in the Tabulae Paralytica. Nature631, 150–163. https://doi.org/10.1038/s41586-024-07504-y (2024).
Guo, H. et al. Regulation of beta-chemokine mRNA expression in adult rat astrocytes by lipopolysaccharide, proinflammatory and immunoregulatory cytokines. Scand. J. Immunol.48, 502–508. https://doi.org/10.1046/j.1365-3083.1998.00422.x (1998).
Taverna, S. et al. High mobility Group Box 1: Biological functions and relevance in oxidative stress related chronic diseases. Cells11, 849. https://doi.org/10.3390/cells11050849 (2022).
Chen, K. B. et al. High-mobility group box-1 and its receptors contribute to proinflammatory response in the acute phase of spinal cord injury in rats. Spine36, 2122–2129. https://doi.org/10.1097/BRS.0b013e318203941c (2011).
Rouhiainen, A. et al. Regulation of monocyte migration by amphoterin (HMGB1). Blood. 104, 1174–1182. https://doi.org/10.1182/blood-2003-10-3536 (2004).
Bauer, E. M., Shapiro, R., Billiar, T. R. & Bauer, P. M. High mobility group Box 1 inhibits human pulmonary artery endothelial cell migration via a toll-like receptor 4- and interferon response factor 3-dependent mechanism(s). J. Biol. Chem.288, 1365–1373. https://doi.org/10.1074/jbc.M112.434142 (2013).
Fang, P. et al. HMGB1 contributes to regeneration after spinal cord injury in adult zebrafish. Mol. Neurobiol.49, 472–483. https://doi.org/10.1007/s12035-013-8533-4 (2014).
Hayakawa, K., Pham, L. D., Katusic, Z. S., Arai, K. & Lo, E. H. Astrocytic high-mobility group box 1 promotes endothelial progenitor cell-mediated neurovascular remodeling during stroke recovery. Proc. Natl. Acad. Sci. U.S.A.109, 7505–7510. https://doi.org/10.1073/pnas.1121146109 (2012).
Al-Ofi, E. A. & Al-Ghamdi, B. S. High-mobility group box 1, an endogenous ligand of toll-like receptors 2 and 4, induces astroglial inflammation via nuclear factor kappa B pathway. Folia Morphol. (Warsz.)78, 10–16. https://doi.org/10.5603/FM.a2018.0068 (2019).
Ding, B. et al. Tanshinone IIA attenuates neuroinflammation via inhibiting RAGE/NF-kappaB signaling pathway in vivo and in vitro. J. Neuroinflamm.17https://doi.org/10.1186/s12974-020-01981-4 (2020).
Fan, H. et al. Inhibiting HMGB1-RAGE axis prevents pro-inflammatory macrophages/microglia polarization and affords neuroprotection after spinal cord injury. J. Neuroinflamm.17https://doi.org/10.1186/s12974-020-01973-4 (2020).
Gunasekaran, M. K. et al. TLR4-dependant pro-inflammatory effects of HMGB1 on human adipocyte. Adipocyte5, 384–388. https://doi.org/10.1080/21623945.2016.1245818 (2016).
Liang, Y. et al. HMGB1 binding to receptor for advanced glycation end products enhances inflammatory responses of human bronchial epithelial cells by activating p38 MAPK and ERK1/2. Mol. Cell. Biochem.405, 63–71. https://doi.org/10.1007/s11010-015-2396-0 (2015).
Yuk, J. M. et al. A dual regulatory role of apurinic/apyrimidinic endonuclease 1/redox factor-1 in HMGB1-induced inflammatory responses. Antioxid. Redox Signal.11, 575–588. https://doi.org/10.1089/ars.2008.2196 (2009).
Wang, X. et al. Pharmacological network analysis of the functions and mechanism of kaempferol from Du Zhong in intervertebral disc degeneration (IDD). J. Orthop. Transl.39, 135–146. https://doi.org/10.1016/j.jot.2023.01.002 (2023).
Takagi, M. et al. Danger of frustrated sensors: role of toll-like receptors and NOD-like receptors in aseptic and septic inflammations around total hip replacements. J. Orthop. Transl.10, 68–85. https://doi.org/10.1016/j.jot.2017.05.004 (2017).
Acknowledgements
We would like to thank the grant involved in this study and Nature Research Editing Service for its linguistic assistance in this manuscript.
Funding
This study is supported by the Research Fund at the Hospital Level of Hanzhong Central Hospital in Shaanxi Province (YK1801); the Shaanxi Province Health Hanzhong Area Fracture and Osteopathy Treatment Research Innovation Platformthe (2024PT-16); the Natural Science Foundation of Shanghai (22ZR1437600); the Hainan Provincial Natural Science Foundation of China (823QN364); the Science and Technology Committee of Fengxian District, Shanghai (FK20201501).
Author information
Authors and Affiliations
Contributions
G Chi, J Lu, and T He contributed to conception, design, data acquisition, and analysis, drafted the manuscript; Y Wang and X Zhou contributed to data acquisition and analysis; Y Zhang and LS Qiu contributed to conception, supervision, critically revised the manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chi, G., Lu, J., He, T. et al. High mobility group box-1 protein promotes astrocytic CCL5 production through the MAPK/NF-κB pathway following spinal cord injury. Sci Rep 14, 22344 (2024). https://doi.org/10.1038/s41598-024-72947-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-72947-2