Abstract
Branched-chain amino acid transaminase 2 (BCAT2) encodes a crucial protein involved in the initial catalysis of branched-chain amino acid (BCAA) catabolism, with emerging evidence suggesting its association with tumor progression. This study explores BCAT2 in a pan-cancer multi-omics context and evaluates its prognostic significance. We utilized a multi-database approach, analyzing cBioPortal for genetic alterations, RNA-Seq data from TCGA and GTEx for expression patterns, and RSEM for transcript analysis. Protein expression and interaction networks were assessed using the Human Protein Atlas, UniProt, and STRING. Prognostic value was determined through Cox regression analysis of TCGA clinical survival data, while immune cell infiltration across various cancers was examined using TCGA data and the TIMER2 platform. Our results revealed that BCAT2 alterations are primarily amplifications and is upregulated in various tumors, correlating with poor survival rates in several tumor types, including GBMLGG, LGG, and UVM. Elevated BCAT2 protein levels were common in pan-cancer, interacting with a range of metabolic enzymes. Additionally, BCAT2 expression significantly influenced CD4+ T cells, CD8+ T cells, and Treg cells infiltration, with varied correlations across cancer types. These findings indicate BCAT2 as a potential biomarker for cancer diagnosis and therapy, potentially regulating key metabolic and immune factors to mediate tumor progression and the microenvironment.
Similar content being viewed by others
Introduction
Cancer remains a foremost cause of death and a substantial public health challenge worldwide, directly impacting both healthcare systems and the global economy1. Despite advancements in primary treatment strategies such as surgery, radiotherapy, and chemotherapy2, patients frequently face poor prognoses and survival, hindered by complications such as drug resistance and side effects3. This underscores the urgent need for novel biomarkers as therapeutic and diagnostic targets. Pan-cancer analysis, transcending traditional organ-specific approaches, offers a comprehensive perspective by integrating genomics data across various cancer types. This approach is crucial for identifying biomarker genes. By discovering and validating these biomarkers, pan-cancer analysis holds the potential to revolutionize cancer prognosis, treatment, and the understanding of cancer biology4.
Given these challenges, our study focuses on the metabolic pathways involving branched-chain amino acids (BCAAs), specifically examining the role of branched-chain amino acid transaminase 2 (BCAT2) within a pan-cancer framework. We hypothesize that BCAT2 could serve as a critical biomarker, offering new insights into cancer prognosis and therapeutic strategies.
Branched-chain amino acids (BCAAs)—leucine, valine, and isoleucine—are essential hydrophobic amino acids predominantly metabolized in muscle tissues5. Under normal circumstances, BCAAs participate in protein synthesis and molecular signal regulations by mediating the production of coenzyme A (CoA) and glutamate6. Recently, anomalous BCAAs metabolism was found in multiple tumors accompanied by disturbed nitrogen and carbon sources, leading tumor cells to obtain BCAAs from other circulation or peripheral tissues7,8. Emerging evidence highlights a significant correlation between dysregulated BCAA metabolism and increased cancer risk across various cancer types9.
Branched-chain amino acid transaminase (BCAT) plays a crucial role in the transamination of BCAAs, which is a reversible process to form branched-chain \(\alpha\)-keto acid (BCKA)10. After the oxidative decarboxylation conducted by branched-chain keto-acid dehydrogenase (BCKDH) complex, BCKA is transformed to the final metabolites with a regulatory function on energy production triggering tricarboxylic acid cycle (TCA)11. BCAT2, a member of the BCAT family, encodes a ubiquitously expressed enzyme that catalyzes BCAA metabolism12. Recent studies has illuminated the involvement of BCAT2 in tumor development, including its regulation by the proto-oncogene c-myc5 and its contribution to cancer progression through BCAA catabolism13. However, a comprehensive understanding of the role and mechanisms of BCAT2 in cancer remains elusive.
To elucidate the function and mechanism of BCAT2 in pan-cancer progression and to identify its potential as a valuable biomarker for cancer diagnosis and prognosis, this study is structured as follows. We first conducted a pan-cancer bioinformatics analysis of BCAT2, encompassing gene expression and genetic alterations, along with protein-level changes. Subsequently, we performed a pan-cancer survival analysis and investigated the association of BCAT2 with immune cell infiltration, integrating molecular findings with clinical implications.
Results
The genetic alteration of BCAT2
Understanding that genetic alterations and epigenetic modifications can trigger abnormal gene expression, we began our analysis with BCAT2 alterations across different cancer types using the cBioPortal platform. Our findings revealed a notably high frequency of BCAT2 alterations in adrenocortical carcinoma (4.47%), primarily characterized by gene amplification. This was followed by patients with endometrial cancer exhibiting various alterations including amplification, deep deletion, multiple alterations, and mutations (Fig. 1A).
To delve deeper into the nature of these alterations, the lollipop diagram (Fig. 1B) of mutations indicated that there existed 59 missenses, 5 splices, 2 truncating sties and 2 fusion sites in the gene structure of BCAT2, with the highest mutation frequency occurred at the missense site E153K. Complementing these findings, we employed RSEM14 for quantitative transcript analysis, revealing that the highest transcript expression of BCAT2 occurred in the amplification group on average (Fig. 1C).
The expression analysis of BCAT2 in pan-cancer
Building on our genetic analysis, we next explored BCAT2 gene expression across various cancer types using the TCGA pan-cancer database. Our results revealed that after multiple testing adjustment, BCAT2 was upregulated in 12 tumor types compared to normal tissues, including BLCA, BRCA, CESC, CHOL, GBM, HNSC, KICH, KIRP, LIHC, PRAD, STAD, and UCEC. Notably, higher BCAT2 expression was observed in HPV-positive HNSC compared to HPV-negative HNSC, and in metastatic SKCM relative to primary SKCM tumors. Conversely, BCAT2 expression was downregulated in COAD, PCPG, and THCA tumors (Fig. 2A).
BCAT2 expression profile in pan-cancer. (A) The expression of BCAT2 in normal and tumor tissues from TCGA database. (B) BCAT2 expression in paired normal and tumor tissues from TCGA database. (C) Pan-cancer expression of BCAT2 between tumor tissues from TCGA database and normal tissues from GTEx database. *q-value < 0.05; **q-value < 0.01; ***q-value < 0.001.
To strengthen these findings, we examined BCAT2 expression in paired tumor and normal tissues. This analysis indicated elevated BCAT2 levels in BRCA, CHOL, HNSC, KIRP, LIHC, PRAD, and STAD tumors, whereas lower levels were observed in LUAD, READ, and THCA tumors (Fig. 2B).
Further validation was achieved by integrating data from both the TCGA and GTEx databases, comparing BCAT2 expression in normal and tumor tissues. This comprehensive comparison showed increased BCAT2 expression in 10 tumor types: BRCA, CHOL, DLBC, GBM, HNSC, KICH, KIRP, LIHC, PRAD, and THYM. In contrast, decreased expression was noted in ACC, ESCA, KIRC, LAML, LGG, LUAD, LUSC, OV, PAAD, PCPG, READ, SKCM, STAD, TGCT, THCA, and UCS compared to their respective normal tissues (Fig. 2C).
Combining these analysis, we concluded that BCAT2 is consistently upregulated in BRCA, CHOL, HNSC, KIRP, LIHC, and PRAD tumors, while it is downregulated in THCA tumors. These expression difference between tumor and normal samples further underscored the potential role of BCAT2 as tumor progression biomarker. The upregulation of BCAT2 in multiple cancer types aligns with previous findings on its role in metabolic reprogramming15, where cancer cells rely on BCAA metabolism to support their growth and survival. BCAT2 promotes BCAA uptake and sustains BCAA catabolism, providing essential nutrients and energy for tumor progression. This suggests that these tumors may depend heavily on BCAA metabolism for their advancement16. However, the mechanism underlying BCAT2 downregulation in THCA tumors has not been well characterized, and its potential role in thyroid cancer progression remains to be verified, indicating a need for further investigation.
The protein abundance of BCAT2
Having investigated the genetic alterations and gene expression of BCAT2, we next proceeded to analyze its protein abundance across various tissues. The distribution of BCAT2 protein abundance was initially examined (Fig. 3A). Notably, high BCAT2 expression was observed in a broad range of tissues, with particularly elevated levels in the adrenal gland, bladder, nerve, ovary, and prostate, whereas blood exhibited lower expression.
The protein expression level of BCAT2 in pan-cancer. (A) The protein level of BCAT2 in normal tissues from GTEx database. (B,C) The protein expression of BCAT2 in tumor and normal tissues from HPA database. (D) BCAT2 location in the substructure of cells obtained from from UniProt database. (E) Interaction relationship of BCAT2 protein.
Further analysis using the Human Protein Atlas (HPA) database revealed that BCAT2 expression was highest in colorectal cancer, prostate cancer, breast cancer, endometrial cancer, and ovarian cancer (Fig. 3B). This widespread expression pattern was also consistent across various tissues, with the exception of bone marrow, caudate, cerebellum, hippocampus, skeletal muscle, smooth muscle, and adipose tissues, where BCAT2 was not expressed (Fig. 3C), suggesting that its function is more relevant in specific tissue environments and less critical in others, particularly those with lower proliferative activity.
Exploring the subcellular localization of BCAT2 through the UniProt database, we found its presence in both the mitochondrion and nucleoplasm (Fig. 3D). This subcellular localization suggests roles in both energy metabolism and nuclear processes. The presence of BCAT2 in the mitochondria suggests its role in enhancing the utilization of BCAA, which directly supports mitochondrial respiration by providing crucial metabolites for energy production16. In the nucleoplasm, BCAT2 participates in regulatory processes that influence gene expression or nuclear signaling pathways, potentially linking metabolic status to nuclear functions involved in tumor cell proliferation and survival17,18.
Finally, our analysis of the protein-protein interaction (PPI) network indicated that BCAT2 interacts with multiple metabolic proteins, such as GCLC and BCK (Fig. 3E). These interactions highlight the potential involvement of BCAT2 in key metabolic pathways, further supporting its role in cancer metabolism and progression.
The correlation of BCAT2 with pan-cancer prognosis
After conducting an in-depth bioinformatics analysis of BCAT2, we further analyzed the significance of BCAT2 in pan-cancer clinical prognosis. Initially, we scrutinized the BCAT2 gene expression across different stages of tumors, guided by WHO cancer staging criteria. BCAT2 exhibited decreased expression in later stages of BLCA (P = 0.009, Fig. 4A), in contrast to increased expression in advanced stages of UVM and HNSC (P = 0.035 and 0.040 respectively, Fig. 4B,D). For THCA tumors, a unique expression pattern was observed: BCAT2 gene expression levels increased in stage II (P = 0.009) but decreased in advanced stages (P = 0.004 and 0.008 respectively, Fig. 4C). After adjusting the p-values, we still observed a significant expression pattern indicating progression in both THCA and HNSC. Additionally, we fitted a linear regression for UVM, revealing a significant increasing linear trend (P = 0.0044), indicating that as the tumor progressed, BCAT2 expression steadily increased.
We then aimed to elucidate the relationship between BCAT2 gene expression and the survival of cancer patients, after leveraging significant findings from prior research and using available data from relevant databases. The top three quartiles of BCAT2 gene expression were defined high expression category19. The divergence in survival outcomes across different cancers suggests that BCAT2 may play contrasting roles, either as a pro-survival factor or as a driver of tumor progression, depending on the cancer type. For instance, the association between high BCAT2 expression and better OS in KIRP and PAAD could indicate that BCAT2 supports metabolic processes that sustain tumor homeostasis without driving aggressive tumor behavior. In contrast, poorer OS in GBMLGG, LGG, and UVM patients with high BCAT2 expression suggests that BCAT2 may contribute to a more aggressive tumor phenotype in these cancer types, possibly through enhanced BCAA metabolism and cell proliferation (Fig. 5).
Delving deeper, univariate Cox regression analysis using TCGA data linked high BCAT2 expression with decreased OS in LGG, PCPG, and UVM patients, but a favorable OS in BLCA, BRCA, KIRP, and PAAD cases (Fig. 6A). Disease-specific survival (DSS) analysis classified high BCAT2 expression as a protective biomarker for BLCA, KIRP, and PAAD, and as a risk marker for LGG, PCPG, PRAD, THCA, THYM, and UVM (Fig. 6B). Disease-free interval (DFI) assessments, defined as time from treatment completion to disease recurrence or death, showed BCAT2 acting as a contributor in DLBC, LGG, PCPG, and UVM and as an inhibitor in BLCA, KIRP, and PAAD (Fig. 6C). Additionally, BCAT2 was established as a protective factor for KIRP patients in progression-free interval (PFI), defined as time from the start of treatment to disease progression or death, reflecting treatment effectiveness, analysis (Fig. 6D).
Cox regression analysis of BCAT2. (A–D) The univariate Cox regression of BCAT2 for the OS, DSS, DFI and PFI in TCGA pan-cancer patients was presented by forest maps. After adjusting for p-values, we still observe significant correlations between OS and BCAT2 expression in KIRP, LGG, PAAD, and UVM. For DSS, significant correlations are found in KIRP, LGG, PAAD, PCPG, THCA, THYM, and UVM. No significant correlations were observed for DFI, while for PFI, significant associations remain for LGG, KIRP, PAAD, PCPG, and UVM.
Overall, these findings highlight a complex, cancer-type-specific role for BCAT2, underscoring the need for a deeper understanding of its mechanisms in different cancer types. Further studies are necessary to explore the biological underpinnings of these associations, particularly the metabolic and signaling pathways that BCAT2 regulates in distinct tumor environments. Understanding these mechanisms will be crucial for developing targeted therapies that could modulate BCAT2 activity in a context-dependent manner.
Analysis of BCAT2 and immune cell infiltration
Building on our previous investigations, we conducted a correlation analysis using the TIMER2 database to evaluate the association between BCAT2 expression and immune cell infiltration across various cancer types. Our analysis revealed diverse interactions between BCAT2 expression and different subsets of immune cells.
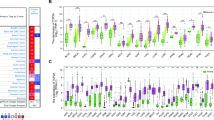
Immune infiltration analysis of BCAT2. (A) The expression of BCAT2 was correlated with CD4+ T cell infiltration by analyzing on TIMER2 database. (B) The correlation between BCAT2 expression and the infiltration of CD8+ T cells on TIMER2 database. (C) BCAT2 expression was associated to Treg cells infiltration in pan-cancer using data from TIMER2 database. *P < 0.05; **P < 0.01; ***P < 0.001.
Specifically, BCAT2 expression positively correlated with naïve CD4+ T cells in BLCA, SKCM, and THCA; with both CD4+ T cells and CD4+ Th cells in HNSC; and with CD4+ Th cells in LGG, SARC, and READ. Conversely, a negative correlation was observed with non-regulatory CD4+ T cells in GBM; with CD4+ Th cells in BLCA and TGCT; and with CD4+ memory cells in BRCA, KIRC, and THCA (Fig. 7A). Regarding CD8+ T cells, BCAT2 expression exhibited a significant positive correlation in CESC, HNSC-HPV(+), and UVM. However, negative correlations were identified in BRCA, KIRC, KIRP, PCPG, SKCM, and THYM (Fig. 7B). In the context of Treg cells, BCAT2 expression was positively associated with Treg cells in HNSC-HPV(+), LUAD, and TGCT, but negatively correlated with Treg cells in KIRP and THCA (Fig. 7C).
These findings underscore the complex role of BCAT2 in modulating the immune microenvironment across different cancer types. By influencing the infiltration and activity of various immune cell subsets, BCAT2 may play a pivotal role in tumor immunity and progression. This highlights the importance of further investigating the mechanisms of BCAT2 in immune regulation to better understand its potential as a therapeutic target in cancer.
Discussion
Early identification and successful therapy are crucial factors in enhancing the outcomes in cancer patients. The accumulation of diverse genetic changes that manifest novel antigens on cancer cell surfaces is critical to tumor development. By conducting pan-cancer analysis, we can uncover the commonalities and distinctions among various types of cancer, offering valuable insights for crafting tailored strategies for cancer prevention and personalized treatment. Recent studies have increasingly concentrated on multi-omics pan-cancer analysis to uncover gene mutations, RNA alterations, and cancer-promoting genes linked to cancer initiation and progression. These findings are important in facilitating early cancer detection and pinpointing influential biomarkers.
In this study, we identified that BCAT2 was significantly upregulated in several cancer types, including BRCA, CHOL, HNSC, KIRP, LIHC, and PRAD, while it was notably downregulated in THCA tumors. The upregulation of BCAT2 in these cancers may reflect its critical role in metabolic reprogramming, where cancer cells rely on BCAA metabolism to fuel tumor growth and survival. By promoting BCAA catabolism, BCAT2 supports mitochondrial respiration and provides essential metabolites for energy production, which may be particularly important in metabolically active tumors like BRCA and HNSC17,20. Conversely, the downregulation of BCAT2 in THCA suggests a distinct metabolic dependency in thyroid cancers, possibly indicating a unique regulatory mechanism that warrants further investigation.
Additionally, our findings align with previous studies showing that BCAT2 overexpression is linked to poorer prognosis in some cancer types20, such as GBMLGG, LGG, and UVM, likely due to its role in enhancing tumor cell proliferation and invasiveness through increased metabolic activity. However, we also observed a contrasting trend in other cancer types21, like KIRP and PAAD, where high BCAT2 expression was associated with improved survival, suggesting a more regulatory or protective role in these tumors, potentially supporting tumor homeostasis. These contrasting outcomes highlight the cancer-type-specific role of BCAT2, and further mechanistic investigation is needed to clarify how BCAT2 contributes to tumor progression and prognosis across different cancers.
Previous research has focused on the role of BCAT2 in PAAD. For example, Li et al. demonstrated that BCAT2 stabilization contributed to PAAD development in mice22, and other studies hightlighted that degradation of BCAT2 could inhibit PAAD tumor growth6,13. This prior evidence points to BCAT2 acting as an oncogene in PAAD progression. However, our findings, showing BCAT2 as a positive prognostic factor in PAAD, suggest a more complex role that needs further investigation.
Moreover, our study aligns with some aforementioned works. Samuel and colleagues found that inhibiting BCAT2 impaired the progression of GBM23. High BCAT2 expression in estrogen receptor-positive BRCA was associated with poor survival outcomes24, and Zhang et al. reported that BCAT2 downregulation correlated with a worse prognosis in patients with STAD25. These findings are consistent with our results, inhibiting BCAT2 expression will contribute to the diagnosis and therapy of pan-cancer.
We further explored the interaction between BCAT2 and tumor microenvironment (TME), which encompasses a sophisticated arrangement of tumor cells, noncancerous cells, blood vessels, extracellular matrix, and other substances26. Intriguingly, our study showed that BCAT2 correlates significantly with the infiltration of CD4+ T cells, CD8+ T cells, and regulatory T (Treg) cells across various cancers, which suggests its potential role in modulating immune responses within the TME. This aligns with existing research and underscores the importance of BCAT2 as a promising biomarker in cancer immunotherapy, guiding the development of more effective and personalized treatment strategies27,28.
In conclusion, our comprehensive study validated that BCAT2 expression was dramatically altered in pan-cancer and had a significant correlation with cancer progression and survival outcomes. Additionally, BCAT2 showed obvious association with the infiltrations of CD4+ T cells, CD8+ T cells and Treg cells, suggesting its potential involvement in modulating the immune microenvironment. While these findings highlight BCAT2 as a promising biomarker for cancer prognosis and immune-targeted therapies, it is important to acknowledge that our analysis is primarily based on correlations. Therefore, further investigation into the causal relationships and detailed mechanistic studies are necessary to validate these findings and fully understand the role of BCAT2 in cancer progression.
Methods
Data sources
In total, we included 32 cancer types for this study. The expression profile of BCAT2 and clinical information of pan-cancer patients were sourced from The Cancer Genome Atlas (TCGA)29 and Genotype-Tissue Expression (GTEx)30 databases, utilizing the Genomic Data Commons platform (GDC)31 for data retrieval. The cBioPortal database32 was employed to analyze BCAT2 genetic alterations.
To explore BCAT2 protein abundance and its subcellular localization in tumor versus normal tissues, we utilized resources from The Human Protein Atlas database33, along with the String database34 for protein-protein interaction (PPI) analysis, and the Uniprot platform35 to determine the subcellular structure of BCAT2.
Along with TIMER2 database36, the information of immune cell infiltration from TCGA cohorts were collected and used to analyze the correlation with BCAT2 expression in pan-cancer patients.
Statistical analysis
The statistical analysis was performed using R software, version 3.6.2. We employed Student’s t-test to compare groups, considering a P value of less than 0.05 as statistically significance. Additionally, the Benjamini-Hochberg procedure was applied to adjust p-values when performing multiple testing to control for false discovery rates. Data were presented as means ± standard deviation (SD). For survival analysis, we utilized the Kaplan–Meier method and univariate Cox regression analysis. Furthermore, we used the RSEM tool, version 1.3.314, for accurate quantification of gene and isoform expression from RNA-Seq data. Across all tumors in the TCGA dataset, we utilized the Tumor Immune Estimation Resource 2.0 (TIMER2.0, http://timer.cistrome.org/) to analyze the partial Spearman’s correlations between BCAT2 expression and various immune cell populations, including CD4+ T cells, CD8+ T cells, and Treg cells. Multiple estimation algorithms were employed for this analysis, including TIMER, EPIC, TIDE, CIBERSORT, CIBERSORT-ABS, QUANTISEQ, XCELL, and MCPCOUNTER.
Data availability statement
BCAT2 expression and clinical data across various cancers were sourced from The Cancer Genome Atlas (TCGA, https://www.cancer.gov/tcga) and Genotype-Tissue Expression (GTEx, http://commonfund.nih.gov/GTEx), via the Genomic Data Commons (GDC, https://gdc.cancer.gov/). BCAT2 genomic alterations data were obtained from the cBioPortal database (http://www.cbioportal.org/). Protein expression analysis, including interaction networks and subcellular localization, was conducted using The Human Protein Atlas (https://www.proteinatlas.org/), STRING database (https://cn.string-db.org/), and UniProt (https://www.uniprot.org/).
References
Sung, H. et al. Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Chen, G. et al. Gpc2 is a potential diagnostic, immunological, and prognostic biomarker in pan-cancer. Front. Immunol. 13, 857308 (2022).
Feng, Z. et al. Pan-cancer and single-cell analysis reveals CENPL as a cancer prognosis and immune infiltration-related biomarker. Front. Immunol. 13, 916594 (2022).
Lai, G., De Grossi, F., Catusi, I., Pesce, E. & Manfrini, N. Dissecting the puzzling roles of FAM46C: A multifaceted pan-cancer tumour suppressor with increasing clinical relevance. Cancers 16, 1706 (2024).
Nong, X. et al. The mechanism of branched-chain amino acid transferases in different diseases: Research progress and future prospects. Front. Oncol. 12, 988290 (2022).
Lei, M.-Z. et al. Acetylation promotes BCAT2 degradation to suppress BCAA catabolism and pancreatic cancer growth. Signal Transduct. Target. Ther. 5, 70 (2020).
Li, T. et al. Defective branched-chain amino acid catabolism disrupts glucose metabolism and sensitizes the heart to ischemia-reperfusion injury. Cell Metab. 25, 374–385 (2017).
Hattori, A. et al. Cancer progression by reprogrammed BCAA metabolism in myeloid leukaemia. Nature 545, 500–504 (2017).
Katagiri, R. et al. Increased levels of branched-chain amino acid associated with increased risk of pancreatic cancer in a prospective case-control study of a large cohort. Gastroenterology 155, 1474–1482 (2018).
Yin, M. & Lei, Q.-Y. BCAT2-BCKDH metabolon maintains BCAA homeostasis. Nat. Metab. 4, 1618–1619 (2022).
Vargas-Morales, J. M. et al. Association of BCAT2 and BCKDH polymorphisms with clinical, anthropometric and biochemical parameters in young adults. Nutr. Metab. Cardiovasc. Dis. 31, 3210–3218 (2021).
Dimou, A., Tsimihodimos, V. & Bairaktari, E. The critical role of the branched chain amino acids (BCAAS) catabolism-regulating enzymes, branched-chain aminotransferase (bcat) and branched-chain \(\alpha\)-keto acid dehydrogenase (bckd), in human pathophysiology. Int. J. Mol. Sci. 23, 4022 (2022).
Li, J.-T. et al. BCAT2-mediated BCAA catabolism is critical for development of pancreatic ductal adenocarcinoma. Nat. Cell Biol. 22, 167–174 (2020).
Li, B. & Dewey, C. N. RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinform. 12, 1–16 (2011).
Cai, Z. et al. BCAT2 shapes a noninflamed tumor microenvironment and induces resistance to anti-PD-1/PD-L1 immunotherapy by negatively regulating proinflammatory chemokines and anticancer immunity. Adv. Sci. 10, 2207155 (2023).
Li, J.-T. et al. BCAT2-mediated BCAA catabolism is critical for development of pancreatic ductal adenocarcinoma. Nat. Cell Biol. 22, 167–174 (2020).
Wang, J., Wang, W., Zhu, F. & Duan, Q. The role of branched chain amino acids metabolic disorders in tumorigenesis and progression. Biomed. Pharmacother. 153, 113390 (2022).
Lee, J. H. et al. Branched-chain amino acids sustain pancreatic cancer growth by regulating lipid metabolism. Exp. Mol. Med. 51, 1–11 (2019).
Shichiri, K., Oshi, M., Ziazadeh, D., Endo, I. & Takabe, K. High mIR-200C expression is associated with suppressed epithelial-mesenchymal transition, TGF-\(\beta\) signaling and better survival despite enhanced cell proliferation in gastric cancer patients. Am. J. Cancer Res. 13, 3027 (2023).
Wang, C.-Y. et al. Gene signatures and potential therapeutic targets of amino acid metabolism in estrogen receptor-positive breast cancer. Am. J. Cancer Res. 10, 95 (2020).
Zhang, Y. et al. Identification of 14 differentially-expressed metabolism-related genes as potential targets of gastric cancer by integrated proteomics and transcriptomics. Front. Cell Dev. Biol. 10, 816249 (2022).
Li, J.-T. et al. Diet high in branched-chain amino acid promotes PDAC development by usp1-mediated bcat2 stabilization. Natl. Sci. Rev. 9, nwab212 (2022).
McBrayer, S. K. et al. Transaminase inhibition by 2-hydroxyglutarate impairs glutamate biosynthesis and redox homeostasis in glioma. Cell 175, 101–116 (2018).
Wang, C.-Y. et al. Gene signatures and potential therapeutic targets of amino acid metabolism in estrogen receptor-positive breast cancer. Am. J. Cancer Res. 10, 95 (2020).
Zhang, Y. et al. Identification of 14 differentially-expressed metabolism-related genes as potential targets of gastric cancer by integrated proteomics and transcriptomics. Front. Cell Dev. Biol. 10, 816249 (2022).
Hong, F. et al. Single-cell analysis of the pan-cancer immune microenvironment and sctime portal. Cancer Immunol. Res. 9, 939–951 (2021).
Nakamura, I. Impairment of innate immune responses in cirrhotic patients and treatment by branched-chain amino acids. World J. Gastroenterol. WJG 20, 7298 (2014).
Cai, Z. et al. BCAT2 shapes a noninflamed tumor microenvironment and induces resistance to anti-PD-1/PD-L1 immunotherapy by negatively regulating proinflammatory chemokines and anticancer immunity. Adv. Sci. 10, 2207155 (2023).
Weinstein, J. N. et al. The cancer genome atlas pan-cancer analysis project. Nat. Genet. 45, 1113–1120 (2013).
Lonsdale, J. et al. The genotype-tissue expression (GTEX) project. Nat. Genet. 45, 580–585 (2013).
Heath, A. P. et al. The NCI genomic data commons. Nat. Genet. 53, 257–262 (2021).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 6, pl1–pl1 (2013).
Uhlén, M. et al. Tissue-based map of the human proteome. Science 347, 1260419 (2015).
Szklarczyk, D. et al. The string database in 2023: protein-protein association networks and functional enrichment analyses for any sequenced genome of interest. Nucleic Acids Res. 51, D638–D646 (2023).
Consortium, U. Uniprot: the universal protein knowledgebase in 2023. Nucleic Acids Res. 51, D523–D531 (2023).
Li, T. et al. Timer2.0 for analysis of tumor-infiltrating immune cells. Nucleic Acids Res. 48, W509–W514 (2020).
Author information
Authors and Affiliations
Contributions
Q.C. and J.F. curated the data, analyzed the results, and created the visualization. Q.C. wrote the original draft. J.Z. and W.W. reviewed and edited the manuscript and supervised the project.
Corresponding authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cao, Q., Fan, J., Zou, J. et al. Multi-omics analysis identifies BCAT2 as a potential pan-cancer biomarker for tumor progression and immune microenvironment modulation. Sci Rep 14, 23371 (2024). https://doi.org/10.1038/s41598-024-74441-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-74441-1