Abstract
Many observational studies and experiments have found a strong association between lipid levels and adipokines and multiple myeloma (MM), but the causal relationship between lipid levels, adipokines and MM remains to be determined. We performed a two-sample and multivariate MR analysis to investigate the causal relationship between lipid levels, adipokines and MM. Total cholesterol(TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG) were used to represent lipid levels, and adiponectin, leptin, and resistin were used to represent adipokines. Genetic data for each index and MM were obtained from the Integrated Epidemiology Unit (IEU) Genome-Wide Association Study (GWAS) database, and two-sample MR analyses were performed, as well as multivariate MR analyses of adipokines for causality of MM using BMI as an adjusting factor. In the analyzed results, no significant causal association was found between adipokines, lipid levels and multiple myeloma, and after adjusting for BMI, an association between adipokines and MM was still not found. The results of this MR study do not support an association between genetically predicted adipokines, lipid levels, and risk of MM, but we cannot rule out the existence of a weak association. The mechanisms need to be further investigated.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is a neoplastic disease characterized by the proliferation of clonal plasma cells. MM accounts for 1% of neoplastic diseases and is the second most common hematologic malignancy. The global incidence of multiple myeloma has increased by 126% as a result of population growth, the aging of the world’s population, and an increase in age-specific incidence rates1.Current treatments for MM include injections of proteasome inhibitors, oral immunomodulators and dexamethasone, treatment with monoclonal antibodies directed against myeloma cell surface antigens, and autologous hematopoietic stem cell transplantation when criteria are met, which improve the survival years of patients with MM but remain incurable2.Therefore, it is necessary to explore the causes and mechanisms of MM.
Obesity is strongly associated with the development of many cancers3. Many studies have shown that obesity is one of the risk factors for MM4 and that obesity may be an important pathway to the development of MM5. Obesity is one of the risk factors for MM. Lipid levels, adipokines and obesity are closely related. Some adipokines stimulate cancer progression through oncogenic signaling or indirect mechanisms6. Adipokines have been shown to be associated with cancer progression through carcinogenesis or indirect mechanisms. Many clinical studies have shown that adipokines are closely related to MM7,8,9,10. Meanwhile, recent studies have shown that blood lipid levels also play an important role in tumor development and metastasis11,12, which has a certain relationship with MM. However, the relationship between blood lipid levels, adipokines and MM still needs to be further explored.
Mendelian randomization (MR) is an analytical method designed to estimate whether an exposure is causally associated with a certain outcome by using the genetic variation of a given exposure as instrumental variables (IVs)13. In recent years, genome-wide association studies (GWAS) have accumulated millions of data points on associations between genetic variants and complex diseases or phenotypes14. In contrast to observational cohort studies, which are plagued by confounding and reverse causation bias, MR studies are based on instrumental variables (i.e., genetic variants) that are randomly distributed according to Mendelian laws of inheritance, mimicking the randomization process of randomized clinical trials. Thus, MR provides strong evidence to support causal inferences about the effects of specific exposures on outcomes13. The present study utilized this genetic variation as a tool to explore the relationship between lipid levels, adipokines, and MM and to consider BMI as a risk factor for the development of MM and its correlation with adiponectin levels15. Several studies have shown a significant positive correlation between BMI and the development of MM16,17,18, so we first performed a two-sample Mendelian analysis between BMI and MM to investigate the correlation and considered the role of BMI in the study of adipokines. In the study of the relationship between lipid levels and MM, we first performed a univariate MR analysis between the indicators and the outcomes and performed a multivariate analysis of lipid levels and the risk of MM development to clarify their independent effects on the outcomes.
The purpose of this study was to determine whether lipid levels and adipokines are causally related to the risk of developing MM by using a two-sample MR approach. We also performed multivariate MR to determine whether adipokines have a causal effect on the occurrence of MM independent of BMI and applied multivariate MR to analyze the results of the independent effects of lipid level indicators on MM.
Methods
Study design
This study followed the guidelines for using MR to enhance the reporting of observational epidemiologic studies19. It began with a two-sample MR on the causal relationship between lipid levels, adipokines, and MM, in which three main hypotheses were prerequisites. Hypothesis 1 was that genetic variation was significantly associated with lipid levels or adipokines. Hypothesis 2 was that genetic variants were not associated with any confounders of the exposure-outcome association. Hypothesis 3 was that genetic variants affect aneurysm risk only through lipid levels or adipokines. Then, we applied multivariate MR to assess whether BMI moderated the causal effect of adipokines on MM risk by including BMI as a moderator in the model.
Data sources
Adiponectin, circulating leptin levels, and resistin were chosen as indicators of adipokines, triglycerides, total cholesterol, HDL cholesterol, and LDL cholesterol as indicators of lipid levels, and multiple myeloma was chosen as the outcome of this study.
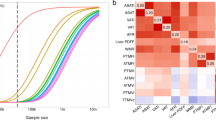
Genetic data for adiponectin, leptin, resistin, BMI, and MM were obtained from publicly available data in the Integrated Epidemiology Unit (IEU) Genome-Wide Association Study (GWAS) database (Medical Research Council, University of Bristol, UK) (https://gwas.mrcieu.ac.uk/)20, whose search codes were “ieu-a-1”, “ebi-a-GCST90007307”, “ebi-a-GCST90022034”, “ieu-b-40”, and “ieu-b-4957”. Genetic data for adiponectin were derived from genetic information containing 39,883 mixed-race participants, of which 14 out of 2,675,209 SNPs were selected as instrumental variables (p < 5 × 10−8). Genetic data for circulating leptin levels were obtained from a study containing genetic information from 56,802 mixed-race participants, of which 6 out of 231,001 SNPs were selected as instrumental variables (p < 5 × 10−8). Genetic data for resistin came from genetic information containing 21,758 participants from a European population, of which 13 out of 13,138,697 SNPs were selected as instrumental variables (p < 5 × 10−8). Genetic data for BMI came from genetic information containing 681,275 participants from a European population, of which 507 out of 2,336,260 SNPs were selected as instrumental variables (p < 5 × 10−8). Lipid-related indicators, including TC, HDL-C, LDL-C, and triglycerides, were GWAS data from a Global Lipids Genetics Consortium (GLGC) study on lipid levels involving 188,577 mixed-race participants21, in which, Eighty-two of the 2,446,982 SNPS of TC were selected as instrumental variables (p < 5 × 10−8), and 84 of the 2,447,442 SNPS of HDL-C were selected as instrumental variables (p < 5 × 10−8). 73 of 2,437,752 SNPS in LDL-C were selected as instrumental variables (p < 5 × 10−8). Out of 2,439,433 SNPS in triglycerides, 54 were extracted as instrumental variables (p < 5 × 10−8). Table 1 shows the relevant sources and information for each exposure or outcome factor (Table 1).
During the screening of instrumental variables, several approaches were used to ensure the quality of genetic variation associated with exposure factors in the pooled GWAS data. First, we applied a genome-wide significance threshold (p < 5 × 10−8) to select SNPs associated with the correct exposures. Second, we excluded SNPs showing total linkage disequilibrium (r2 ≥ 0.001 and 10 Mb). Third, we removed variants found in the PhenoScanner database that were associated with potential confounders (e.g., smoking and hypertension)22, thus satisfying Hypothesis 2. Fourth, we discarded variants identified as outliers by the Mendelian Randomized Polytomous Residuals and Outliers (MR- PRESSO) test. Finally, to avoid the effect of weak instrumental bias, we excluded SNPs with F-statistic values less than 1023.The research process of this study is shown in Fig. 1.
Major mendelian randomization analysis
This study was statistically analyzed using TwoSampleMR in R studio 4.1.1. First, effect values and standard errors were obtained by selecting IVs (instrumental variables) between IVs and exposure factors and IVs and outcome metrics, respectively. BMI, adiponectin, circulating leptin levels, resistin, triglycerides, TC, HDL-C and LDL-C, and MM-related GWAS data were imported into R software and assigned to the exposure and outcome groups. We performed single SNP analysis for each selected SNP, where MR estimates were calculated using the Wald ratio method. To confirm that effector alleles were associated with higher levels of exposure, we reconciled exposure and outcome GWAS data. The main analyses in this study were performed using the IVW and MR‒Egger methods; the IVW method is considered the most efficient due to its maximum statistical power; however, IVW is biased because it assumes the absence of any horizontal pleiotropy, i.e., the effect of the genetic tool on the outcome under consideration through pathways independent of exposure24. The MR‒Egger regression method modifies the IVW method to account for polyvalence bias25 to enhance the stability of the results. The effect sizes (β) and standard errors corresponded to one standard deviation at each exposure factor level. The significance threshold was set at a p value of less than 0.05. Scatter plots and trend lines for different two-sample MR methods were generated to analyze the exposure-outcome relationship, with the slope and direction of the trend line indicating the magnitude and direction of the causal estimate, respectively. Dominance ratios (ORs), 95% confidence intervals (95% CIs) and p values were derived using IVW and MR‒Egger regression. When the p value for IVW is less than 0.05 and the direction of the results obtained by MR‒Egger regression is the same as the direction of the IVW results, it can be determined that the exposure factor is significantly associated with the outcome.
Heterogeneity test
Due to data from many different GWAS cohort studies with potential differences between studies, the MR analysis method may be heterogeneous and lead to biased estimates of causal effects. Cochran’s Q test was therefore used to assess heterogeneity in IVW and MR‒Egger regression26. If the heterogeneity test result P > 0.05 was not statistically significant, heterogeneity did not affect the study results.
Sensitivity analysis
Additional sensitivity analyses were also conducted. We estimated intercepts and slopes for MR‒Egger regressions, where the intercepts indicate the average horizontal polytomies and the slopes indicate the polytomies-adjusted MR estimates. Statistically significant intercept values (p < 0.05) indicate the presence of horizontal polytropy27. To determine whether individual genetic variants contributed to the association between exposure and outcome, the study underwent an additional leave-one-out analysis. In leave-one-out analysis, MR was performed by excluding each SNP exclusion in turn. Horizontal pleiotropy in this study can also be tested by funnel plots, which, if relatively symmetrical, indicate that there is no significant horizontal pleiotropy.
Multivariate mendelian randomization analysis
Multivariate MR is an extension of MR that is capable of addressing genetic variation associated with multiple risk factors28. We applied multivariate MR to assess whether BMI modulates the causal effect of adiponectin, leptin, or resistin on MM risk, using BMI as a moderator. BMI-related data from the Integrated Epidemiology Unit (IEU) Genome-Wide Association Study (GWAS) database (Medical Research Council, University of Bristol, Bristol, UK) with code “ieu-b-40” in publicly available data were selected for multivariate MR analysis with adiponectin, leptin, and resistin to assess whether adipokines adjusted for BMI were causally associated with MM. Multivariate MR analysis was also used for the correlates of lipid indicators by adjusting for lipid indicators to clarify the independent effect of the correlates on MM. In all populations, separate multivariate MR analyses were performed using a “weighted regression-based approach”, which applies IVW to multivariate regression models28. The method applied IVW to the multivariate regression model.
Results
GWAS data
Table 1 shows the number of SNPs associated with each exposure factor that were genome-wide significant (p value < 5 × 10−8) after data for each metric were pooled. In univariate analyses, the F-statistics for all traits exceeded the standard threshold of 10, suggesting that associations of relevant phenotypes with MM are not affected by bias from weak instrumental variables.
The causal relationship between BMI and MM
Regarding the relationship between BMI and MM, we performed a one-way MR analysis (Table 2). The results showed a causal relationship between BMI and MM in the IVW method (OR = 1.001, 95%CI = 1.000-1.001, P = 0.039), and the results of the MR‒Egger method were also consistent (OR = 1.002, 95%CI = 1.000-1.004, P = 0.010). The scatterplot can visualize the above results (Fig. 2). Heterogeneity was assessed using Cochran’s Q-test, which showed no significant heterogeneity (p = 0.922), Egger’s intercept was used to indicate the reliability of the MR estimates, which showed no significant pleiotropy (p = 0.515), and funnel plots were also able to visualize the results in a way that demonstrated the absence of significant pleiotropy (Fig. 3). The leave-one-out method verified the reliability of the results by excluding a single SNP for testing, and the results also indicated the reliability of the existence of causality between BMI and MM (p = 0.039). Therefore, the reliability of the results of MR analysis was high.
Adiponectin has no causal relationship with MM
To investigate the absence of a causal relationship between adiponectin and MM, adiponectin and MM were first analyzed in a one-way MR analysis (Table 2). The results showed that in the IVW method, adiponectin was not associated with the risk of MM (OR = 0.999, 95% CI = 0.998-1.000, P = 0.126), and the results of the MR‒Egger method also supported the above results (OR = 0.999, 95%CI = 0.997-1.000, P = 0.243). Scatterplots and forest plots were used to visualize the above results (Figs. 4 and 5). Cochran’s Q-test results show no significant heterogeneity (p = 0.518), Egger’s intercept indicates the reliability of MR estimation, and the results show no significant multiplicity (p = 0.767). Funnel plots also visualize the results in a way that shows that the results are not significantly multiplicative (Fig. 6). The leave-one-out method also verified the reliability of the results (p = 0.126). Therefore, the reliability of the results of the MR analysis was high.
In turn, we considered a multivariate MR analysis of BMI as a confounder (Table 3), and the results of the univariate analysis could be confirmed by the results of the multivariate MR analysis, which showed no significant causal effect of adiponectin on MR (p = 0.632, OR = 0.100, 95%CI = 0.999–1.001), similar to the results obtained from the univariate MR analysis.
No causal relationship between circulating leptin level and resistin and MM
Univariate MR Analysis of circulating leptin levels and MM showed no significant causal relationship, and univariate MR Analysis showed IVW results (OR = 1.000, 95%CI = 0.999–1.001, p = 0.164), the MR-Egger analysis is also consistent with the result (Table 2), the scatter-plot can be visually displayed (Fig. 7) and the forest map can be used to visualize the result (Fig. 9), and the subsequent sensitivity analysis also confirmed the stability of the result, while the Egger intercept is not significant (p = 0.781) and funnel plot results (Fig. 8) also suggest that pleiotropy is unlikely to bias the results, increasing the reliability of MR Estimates (Table 2). In addition, multivariate MR Analyses taking into account BMI did not provide evidence of a causal effect of circulating leptin levels on MM risk (OR = 1.000, 95%CI = 0.998–1.001, p = 0.987) (Table 3).
MR Analysis did not show the causal effect of resistin on MM risk (OR = 0.999, 95%CI = 0.999–1.001, p = 0.931). Scatter plots and forest plots were produced to visually show the results (Figs. 10 and 12). Sensitivity analysis confirmed that there was no causal relationship between resistin levels and MM risk. In addition, the Egger intercept (p = 0.198) indicated that there was no significant pleiotropy in the study results (Table 2), which could be represented by funnel plot (Fig. 11). In addition, multivariate MR Estimates did not support a causal effect of resistin levels on MM risk when accounting for BMI (OR = 0.100, 95%CI = 0.999-1.000, p = 0.345) (Table 3).
No causal link between TC and MM
The findings also showed no significant causal relationship between TC and the risk of MM. One-way MR analysis showed no causal relationship in IVW and MR‒Egger analysis (OR = 1.000, 95% CI = 0.999-1.000, p = 0.461; OR = 1.000, 95% CI = 0.999–1.001, p = 0.226). Then, a series of sensitivity analyses were conducted, and the heterogeneity test also showed no significant heterogeneity in the results (p = 0.233). Egger’s intercept (p = 0.329) also indicated that there was no significant multiplicity in the study results. The leave-one-out method and funnel plot also indicated that the results of this study were reliable (Figs. 13 and 14).
No causal relationship between HDL-C, LDL-C, TG and MM
The results of the study showed no significant causal relationship between HDL-C, LDL-C, TG and the risk of MM. One-way MR analysis showed no causal effect of HDL-C with MM (OR = 1.000, 95%CI = 0.999–1.001, P = 0.117), which was verified by MR‒Egger’s hair (OR = 1.000, 95%CI = 0.999–1.001, P = 0.361). The Q-test using Cochran showed no significant heterogeneity (p = 0.264), and the use of the Egger intercept showed no significant multiplicity of results (p = 0.921). The leave-one-out method and the funnel plot also showed that the results were reliable (Figs. 15 and 16).
The IVW results showed that LDL-C was not associated with the risk of MM (OR = 1.000, 95%CI = 0.999–1.001, p = 0.337), and MR-Mgger yielded corresponding results. Heterogeneity was not found using Cochran’s Q statistic (p = 0.815), the Egger intercept also showed no pleiotropy in the outcome (p = 0.949), and the results of the funnel plot and leave-one-out method also showed the reliability of the outcome (Figs. 17 and 18).
The results of the IVW and MR‒Egger methods showed no significant causal relationship between TG and the risk of MM (OR = 0.999, 95%CI = 0.999–1.001, p = 0.853; OR = 1.000, 95%CI = 0.999-1.000, p = 0.521). Then, a series of sensitivity analyses were performed using Cochran’s Q statistic (p = 0.173), which did not reveal heterogeneity, Egger’s intercept, which also showed that there was no multiplicity of outcomes (p = 0.353), and leave-one-out and funnel plots, which showed that the results were reliable (Figs. 19 and 20).
Multivariate MR of triglycerides, HDL-C, LDL-C, TC and MM
We also conducted multivariate MR analysis of the causal relationship between triglycerides, HDL-C, LDL-C, TC and MM, and after considering the role of each exposure factor in generating a relationship on the outcome, the results of the multivariate MR analysis still showed that there was no significant causality between each exposure factor and the risk of MM (p = 0.200, OR = 0.997, 95%CI = 0.994–1.001; p = 0.118, OR = 1.001, 95%CI = 0.999–1.003; p = 0.158, OR = 0.999, 95%CI = 0.999–1.005, p = 0.210, OR = 1.001, 95%CI = 0.999–1.002) (Table 4).
Discussion
This study is the first to explore the causal relationship between BMI, adipokines, and lipid levels and MM based on MR analysis. The results of this study respond to the long-term effects of genetically controlled BMI, adipokines, and lipid levels on MM, which are not influenced by short-term or other confounding factors. The present MR study found that there is a causal relationship between BMI and MM, but there are no data to support a causal relationship between adipokines, lipid levels and MM.
Obesity is strongly associated with the development of many malignant tumors3, as studies have shown. Obesity is one of the important predisposing factors of MM4,17,29,30,31. Monoclonal gammopathy of undetermined significance (MGUS) is a precancerous plasma cell malignancy that occurs before MM32. Studies have shown that patients with MM have a higher cross-sectional area of abdominal adipose tissue and higher metabolic activity of adipose tissue than patients with MGUS, implying that adipose tissue plays a role in the progression of MGUS to MM33. Moreover, some studies have found that obesity increases the mortality rate of MM34,35. Currently, obesity is mainly measured by metrics such as BMI. Elevated BMI is associated with the progression of MM and its high mortality rate5,36. However, some scholars still hold different opinions on the correlation between the two37,38. In this study, MR analysis was performed again to investigate the relationship.
The mechanisms underlying the correlation between obesity and MM have not been established39. The role of adipokines is one of the mechanisms by which obesity affects cancer, and adipose tissue hypoxia triggers changes in adipokine levels that may be associated with the progression of various cancers40,41. Adipose tissue is the largest known endocrine organ and can secrete more than 50 adipokines42. Adipose tissue is the largest known endocrine organ, secreting more than 50 adipokines. It has been shown that adipocytes support the survival of MM cells and promote migration. This effect is mainly associated with the level of adipokines secreted by adipocytes43,44. The study of whether adipokines are the cause of MM is still in the exploratory stage. In this study, adiponectin, leptin, and resistin were selected to investigate whether adipokines are causally involved in the development of MM.
Adiponectin is the most abundant adipokine secreted by adipose tissue, with higher secretion by bone marrow adipose tissue, and may be promoted to increase in many adverse conditions45. Adiponectin binds to receptors and is involved in physiopathological processes such as insulin sensitization, lipid metabolism, energy regulation, inflammation and cancer development46 and is often considered a beneficial adipokine. Studies have shown that adiponectin is associated with the development of MM47. Hofmann7 found in a pooled study of seven cohorts that patients with MM had lower serum adiponectin levels than controls. In addition, they stratified the samples according to BMI and observed that adiponectin levels in overweight subjects or obese subjects were negatively associated with MM risk. Related mechanistic findings revealed that AKT is an enzyme critical for MM cell proliferation and survival and that adiponectin induces the proliferation and apoptosis of MM cells through the PKA/AKT pathway48. Moreover, enhanced adipogenic activity is essential for maintaining cell membrane integrity in rapidly proliferating cancer cells49. Inhibition of adipogenesis by adiponectin mediates the antiproliferative effects of adiponectin in MM cells. Adiponectin is PKA/AMPK-dependent and exerts its antiproliferative effects by downregulating the key lipogenic enzyme ACC through this pathway to induce cell cycle arrest and apoptosis in MM cells48. In addition, adiponectin activates AMPK in several cell lines by increasing p53 and p21 expression, and AMPK interferes with cell growth signaling through mTOR, thereby inhibiting cancer progression50. AMPK interferes with cell growth signaling through mTOR, thus inhibiting cancer progression. In summary, decreased adiponectin levels may be associated with an increased risk of MM development. However, this study found no significant causal relationship between adiponectin and MM. Instead, studies have shown that elevated BMI is associated with an increased risk of MM5. There was a negative correlation between serum adiponectin and BMI, and after considering the modifying effect of BMI, there was still no causal relationship between adiponectin and MM risk. The mechanism of the relationship between adiponectin and MM still needs to be further explored, and medullary tumor type, different stages, risk stratification and tumor heterogeneity may be the reasons for the inconsistent results.
Leptin has an important role in the control of many physiological processes, including hormone production, blood pressure, reproduction, osteogenesis, hematopoiesis, angiogenesis, and immunity51. Leptin has direct and indirect biological effects on the regulation of cancer proliferation, metastasis, angiogenesis and chemoresistance51. Existing studies on the relationship between leptin and MM remain contradictory, and a study that included 14 patients with MM and 25 healthy controls showed that serum leptin levels were higher in the MM group (than in healthy controls)52. Liu et al.53 conducted a meta-analysis in 2021 showing higher leptin concentrations in MM patients than in controls. However, Hofmann et al.54 studied serum leptin levels in 174 patients (10.01 ± 2.64 ng/mL) and 348 controls (9.60 ± 2.71 ng/mL) in the United States between 1993 and 2001 and found that the difference was not statistically significant. Studies on the mechanisms associated with leptin and MM have shown that upregulation of leptin levels stimulates the proliferation of MM cells and reduces the antitumor effects of chemotherapy through activation of the AKT/STAT 3 pathway55. It also promotes the expression of autophagy proteins through the IAK/STAT 3 pathway and exerts antiapoptotic effects in MM cells56. It can also promote the expression of autophagy proteins through the IAK/STAT3 pathway and exert antiapoptotic effects in MM cells. An in vitro experiment showed that leptin induced modification of gene expression, which enhanced the growth and viability of MM cells10. In an in vitro experiment, leptin was shown to induce modifications in gene expression, thereby enhancing MM cell growth and viability. However, the present study showed no obvious causal relationship between leptin and MM, and the correlation between the two remains to be further explored. The mechanism of leptin’s effect on MM is more in the reduction of the effect of chemotherapy, so it is related to the progression of MM and has less effect on the development of MM.
The present study also did not find a causal relationship between resistin levels and MM. Resistin is highly expressed in bone marrow and is involved in insulin resistance, inflammation, immune regulation and cancer development57. A study including 73 MM patients and 73 controls showed that low circulating resistin concentrations were associated with MM risk8. However, a meta-analysis of seven studies including 367 MM patients and 524 controls53 showed no significant difference in circulating resistin levels between the two groups. The role of resistin in MM is complex, with some studies suggesting that it is a protective adipokine, and Pang et al.58 found that resistin abrogates chemotherapy-induced apoptosis in myeloma cells by inhibiting chemotherapy-induced cysteine asparaginase cleavage, thereby enhancing multidrug resistance in MM. However, low resistin levels may also increase the risk of MM development8. Although research on the relationship between resistin and MM is still in its infancy, drugs targeting resistin may be a potential way to prevent or overcome multidrug resistance in multiple myeloma59.
Lipids play an important role in cell growth and proliferation, and evidence suggests that abnormal lipid metabolism promotes cancer development, invasion, and metastasis through multiple signaling pathways60,61. Serum lipid levels are associated with future cancer risk, including breast and prostate cancer62. Therefore, lipid metabolism has emerged as a new target for cancer prevention and treatment. However, the significance of altered lipid metabolism in MM pathophysiology is unclear. There is a link between cholesterol metabolism and cancer63. Some studies have shown that MM patients have significantly lower levels of TC, LDL-C, HDL-C and TG64,65,66,67. Sato et al.68 demonstrated that cholesterol is needed for the growth of mouse myeloma cells under serum-free conditions. In another study, Li et al.69 also confirmed this finding. In a clinical study, Scolozzi et al.70 found a negative correlation between TC and MM stage in 41 patients with MM. Quesney Huneeus V71 found that mevalonate, a precursor of cholesterol, provides the structural cholesterol that allows cells to pass through the G1 phase to the S phase in the cell cycle, which is essential for malignant cell proliferation. However, the specific mechanism of cholesterol and MM has not been clearly investigated. In hematologic malignancies, there is an interaction between chronic low-grade inflammation morbidity, dyslipidemia, and oxidative stress. The decreased levels of HDL-C in patients with MM may be due to the protective effect of HDL-C against MM through antioxidant and anti-inflammatory properties72. Inflammatory pathways activated by immune factors and genetic alterations affecting oncogenes are part of the mechanism leading to carcinogenesis73. HDL-C may inhibit myeloproliferation and leukocytosis by reducing the proliferation of granulocyte-monocyte progenitor cells and interleukin-3 in bone marrow cells74,75. HDL-C can inhibit bone marrow proliferation and leukocytosis by reducing the proliferation of granulocyte-monocyte progenitors and interleukin-3 in bone marrow cells. It has been observed that76 LDL-C has an antimyeloma cell apoptotic effect in MM patients. Meanwhile, Hungria et al.67 using cholesterol-rich microemulsions demonstrated increased plasma LDL clearance in MM patients, which in turn led to low LDL-C and TC. Yavasoglu et al.77 also found hypocholesterolemia in MM patients due to increased LDL clearance and cholesterol utilization by myeloma cells. This evidence suggests that LDL-C may have a role in the development of MM. In contrast, the present study found no significant causal relationship between TC, HDL-C, LDL-C, TG and MM after MR analysis based on univariate and multivariate lipid levels. This may be related to the correlation between cholesterol levels and MM staging, in which hypocholesterolemia has been considered more as a consequence than a cause of MM in existing studies78, which was laterally confirmed in the present study.
This MR analysis adequately assesses the validity of each MR hypothesis. The consistency of the results of different MR statistical methods reveals the robustness of our conclusions. In this study, we did not manually scan selected SNPs in PhenoScanner for potential secondary phenotypes. The small number of SNPs in adipokines after extraction and harmonization made the reliability of the results slightly thin. Moreover, the pathogenesis and etiology of MM is complex and has not been fully elucidated. Therefore, excluding SNPs that may be associated with other traits may result in a large bias. In this case, the analysis of all selected IVs was considered credible based on previous similar studies and opinions79,80. Although the exclusion restriction hypothesis could not be fully tested, it could be partially verified by multiple sensitivity analysis methods. We did not observe any evidence of heterogeneity or horizontal pleiotropy. Therefore, the likelihood of violating the MR hypothesis was low in our study. In addition, we still did not find a clear causal relationship after considering the adjusting role of BMI in this context. Regarding the study of lipid levels, after performing univariate MR analysis, we performed multivariate MR analysis to clarify the independent effects of each exposure factor on MM, but the results still did not find that a causal relationship existed.
In this study, in addition to the limitation that only a few SNPs were selected as IVs, most genetic variants had a relatively limited effect on specific exposures, such as adipokine levels, as they may only explain a small portion of the variance in that exposure. It is important to note that there are other factors besides BMI that affect adipokine levels, such as diet, exercise, and lipid levels81,82. However, BMI is the main determinant because the above factors are correlated with BMI. In addition, BMI can be easily measured in large cohorts, and there is a large amount of GWAS data available. BMI was also chosen based on its major relevance as a known risk factor for MM. In studies of lipid levels and MM, the results are more reliable because of the larger GWAS data. However, both univariate and multivariate MR analyses showed no significant causal relationship. It is possible that the etiology and mechanisms of MM are too complex and that the several phenotypes studied thus far do not act directly on MM to produce a causal effect. Therefore, the exploration of the etiology and risk factors for MM still needs to be continued.
Conclusions
The evidence provided in this study suggests that adipokines (adiponectin, leptin, resistin) and lipid levels (TC, HDL-C, LDL-C, TG) may not have a causal effect on MM at the genetic level, and these studies help us to objectively validate previous observational studies. However, this result is not completely conclusive, and the above findings should be verified by more studies. This study further deepens the exploration and understanding of the pathogenesis and etiology of MM.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
van de Donk, N., Pawlyn, C. & Yong, K. L. Multiple myeloma. Lancet397, 410–427. https://doi.org/10.1016/s0140-6736(21)00135-5 (2021).
Cowan, A. J. et al. Diagnosis and management of multiple myeloma: A review. Jama327, 464–477. https://doi.org/10.1001/jama.2022.0003 (2022).
Lauby-Secretan, B. et al. Body fatness and Cancer–viewpoint of the IARC Working Group. N. Engl. J. Med.375, 794–798. https://doi.org/10.1056/NEJMsr1606602 (2016).
Teras, L. R. et al. Body size and multiple myeloma mortality: A pooled analysis of 20 prospective studies. Br. J. Haematol.166, 667–676. https://doi.org/10.1111/bjh.12935 (2014).
Went, M. et al. Search for multiple myeloma risk factors using Mendelian randomization. Blood Adv.4, 2172–2179. https://doi.org/10.1182/bloodadvances.2020001502 (2020).
Khandekar, M. J., Cohen, P. & Spiegelman, B. M. Molecular mechanisms of cancer development in obesity. Nat. Rev. Cancer11, 886–895. https://doi.org/10.1038/nrc3174 (2011).
Hofmann, J. N. et al. Low levels of circulating adiponectin are associated with multiple myeloma risk in overweight and obese individuals. Cancer Res.76, 1935–1941.. https://doi.org/10.1158/0008-5472.Can-15-2406 (2016).
Dalamaga, M. et al. Low circulating adiponectin and resistin, but not leptin, levels are associated with multiple myeloma risk: A case-control study. Cancer Causes Control CCC20, 193–199. https://doi.org/10.1007/s10552-008-9233-7 (2009).
Santo, L. et al. Circulating resistin levels and risk of multiple myeloma in three prospective cohorts. Br. J. Cancer117, 1241–1245. https://doi.org/10.1038/bjc.2017.282 (2017).
Reseland, J. E. et al. Abnormal adipokine levels and leptin-induced changes in gene expression profiles in multiple myeloma. Eur. J. Haematol.83, 460–470. https://doi.org/10.1111/j.1600-0609.2009.01311.x (2009).
Luo, X. et al. Emerging roles of lipid metabolism in cancer metastasis. Mol. Cancer16, 76. https://doi.org/10.1186/s12943-017-0646-3 (2017).
Santos, C. R. & Schulze, A. Lipid metabolism in cancer. FEBS J.279, 2610–2623. https://doi.org/10.1111/j.1742-4658.2012.08644.x (2012).
Emdin, C. A., Khera, A. V. & Kathiresan, S. Mendelian randomization. Jama318, 1925–1926. https://doi.org/10.1001/jama.2017.17219 (2017).
Richmond, R. C. & Davey Smith, G. Mendelian randomization: Concepts and scope. Cold Spring Harbor Perspect. Med.12https://doi.org/10.1101/cshperspect.a040501 (2022).
Ouchi, N., Parker, J. L., Lugus, J. J. & Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol.11, 85–97. https://doi.org/10.1038/nri2921 (2011).
Ugai, T. et al. Association of BMI, smoking, and Alcohol with multiple myeloma mortality in asians: A pooled analysis of more than 800,000 participants in the Asia Cohort Consortium. CCancer Epidemiol. Biomark. Prev.28, 1861–1867. https://doi.org/10.1158/1055-9965.Epi-19-0389 (2019).
Wallin, A. & Larsson, S. C. Body mass index and risk of multiple myeloma: A meta-analysis of prospective studies. Eur. J. Cancer47, 1606–1615. https://doi.org/10.1016/j.ejca.2011.01.020 (2011).
Renehan, A. G., Tyson, M., Egger, M., Heller, R. F. & Zwahlen, M. Body-mass index and incidence of cancer: A systematic review and meta-analysis of prospective observational studies. Lancet371, 569–578. https://doi.org/10.1016/s0140-6736(08)60269-x (2008).
Skrivankova, V. W. et al. Strengthening the reporting of observational studies in epidemiology using Mendelian randomization: The STROBE-MR statement. Jama326, 1614–1621. https://doi.org/10.1001/jama.2021.18236 (2021).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife7https://doi.org/10.7554/eLife.34408 (2018).
Willer, C. J. et al. Discovery and refinement of loci associated with lipid levels. Nat. Genet.45, 1274–1283. https://doi.org/10.1038/ng.2797 (2013).
Kamat, M. A. et al. PhenoScanner V2: An expanded tool for searching human genotype-phenotype associations. Bioinformatics35, 4851–4853. https://doi.org/10.1093/bioinformatics/btz469 (2019).
Burgess, S. & Thompson, S. G. Avoiding bias from weak instruments in Mendelian randomization studies. Int. J. Epidemiol.40, 755–764. https://doi.org/10.1093/ije/dyr036 (2011).
Burgess, S. et al. Guidelines for performing mendelian randomization investigations: Update for summer 2023. Wellcome Open. Res.4https://doi.org/10.12688/wellcomeopenres.15555.3 (2019). 186.
Burgess, S. & Thompson, S. G. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur. J. Epidemiol.32, 377–389. https://doi.org/10.1007/s10654-017-0255-x (2017).
Li, Q. et al. Mendelian randomization study of heart failure and stroke subtypes. Front. Cardiovasc. Med.9, 844733. https://doi.org/10.3389/fcvm.2022.844733 (2022).
Bowden, J., Davey Smith, G. & Burgess, S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol.44, 512–525. https://doi.org/10.1093/ije/dyv080 (2015).
Burgess, S. & Thompson, S. G. Multivariable Mendelian randomization: The use of pleiotropic genetic variants to estimate causal effects. Am. J. Epidemiol.181, 251–260. https://doi.org/10.1093/aje/kwu283 (2015).
Carson, K. R., Bates, M. L. & Tomasson, M. H. The skinny on obesity and plasma cell myeloma: A review of the literature. Bone Marrow Transplant.49, 1009–1015. https://doi.org/10.1038/bmt.2014.71 (2014).
De Pergola, G. & Silvestris, F. Obesity as a major risk factor for cancer. J. Obes.2013 291546. https://doi.org/10.1155/2013/291546 (2013).
Birmann, B. M., Giovannucci, E., Rosner, B., Anderson, K. C. & Colditz, G. A. Body mass index, physical activity, and risk of multiple myeloma. Cancer Epidemiol. Biomark. Prev.16, 1474–1478. https://doi.org/10.1158/1055-9965.Epi-07-0143 (2007).
Mouhieddine, T. H., Weeks, L. D. & Ghobrial, I. M. Monoclonal gammopathy of undetermined significance. Blood133, 2484–2494. https://doi.org/10.1182/blood.2019846782 (2019).
Veld, J. et al. Abdominal adipose tissue in MGUS and multiple myeloma. Skelet. Radiol.45, 1277–1283. https://doi.org/10.1007/s00256-016-2425-4 (2016).
Calle, E. E., Rodriguez, C., Walker-Thurmond, K. & Thun, M. J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N. Engl. J. Med.348, 1625–1638. https://doi.org/10.1056/NEJMoa021423 (2003).
Khan, M. M. et al. Risk factors for multiple myeloma: Evidence from the Japan Collaborative Cohort (JACC) study. Asian Pac. J. Cancer Prev. APJCP7, 575–581 (2006).
Kleinstern, G. et al. Body mass index associated with monoclonal gammopathy of undetermined significance (MGUS) progression in Olmsted County, Minnesota. Blood Cancer J.12, 67. https://doi.org/10.1038/s41408-022-00659-9 (2022).
Fernberg, P. et al. Tobacco use, body mass index, and the risk of leukemia and multiple myeloma: A nationwide cohort study in Sweden. Cancer Res.67, 5983–5986. https://doi.org/10.1158/0008-5472.Can-07-0274 (2007).
Pylypchuk, R. D., Schouten, L. J., Goldbohm, R. A., Schouten, H. C. & van den Brandt, P. A. Body mass index, height, and risk of lymphatic malignancies: A prospective cohort study. Am. J. Epidemiol.170, 297–307. https://doi.org/10.1093/aje/kwp123 (2009).
Zipori, D. The hemopoietic stem cell niche versus the microenvironment of the multiple myeloma-tumor initiating cell. Cancer Microenviron.3, 15–28. https://doi.org/10.1007/s12307-009-0034-7 (2010).
Divella, R., De Luca, R., Abbate, I., Naglieri, E. & Daniele, A. Obesity and cancer: The role of adipose tissue and adipo-cytokines-induced chronic inflammation. J. Cancer7, 2346–2359. https://doi.org/10.7150/jca.16884 (2016).
Tarasiuk, A., Mosińska, P. & Fichna, J. The mechanisms linking obesity to colon cancer: An overview. Obes. Res. Clin. Pract.12, 251–259. https://doi.org/10.1016/j.orcp.2018.01.005 (2018).
Deng, T., Lyon, C. J., Bergin, S., Caligiuri, M. A. & Hsueh, W. A. Obesity, inflammation, and cancer. Annu. Rev. Pathol.11, 421–449. https://doi.org/10.1146/annurev-pathol-012615-044359 (2016).
Caers, J. et al. Neighboring adipocytes participate in the bone marrow microenvironment of multiple myeloma cells. Leukemia21, 1580–1584. https://doi.org/10.1038/sj.leu.2404658 (2007).
Bullwinkle, E. M. et al. Adipocytes contribute to the growth and progression of multiple myeloma: Unraveling obesity related differences in adipocyte signaling. Cancer Lett.380, 114–121. https://doi.org/10.1016/j.canlet.2016.06.010 (2016).
Cawthorn, W. P. et al. Bone marrow adipose tissue is an endocrine organ that contributes to increased circulating adiponectin during caloric restriction. Cell Metabol.20, 368–375. https://doi.org/10.1016/j.cmet.2014.06.003 (2014).
Fang, H. & Judd, R. L. Adiponectin regulation and function. Compr. Physiol.8, 1031–1063. https://doi.org/10.1002/cphy.c170046 (2018).
Hofmann, J. N. et al. Circulating adiponectin levels differ between patients with multiple myeloma and its Precursor Disease. Obesity25, 1317–1320. https://doi.org/10.1002/oby.21894 (2017).
Nigro, E. et al. New insight into adiponectin role in obesity and obesity-related diseases. Biomed. Res. Int.2014 (658913). https://doi.org/10.1155/2014/658913 (2014).
Mashima, T., Seimiya, H. & Tsuruo, T. De novo fatty-acid synthesis and related pathways as molecular targets for cancer therapy. Br. J. Cancer100, 1369–1372. https://doi.org/10.1038/sj.bjc.6605007 (2009).
Medina, E. A. et al. PKA/AMPK signaling in relation to adiponectin’s antiproliferative effect on multiple myeloma cells. Leukemia28, 2080–2089. https://doi.org/10.1038/leu.2014.112 (2014).
Lin, T. C. & Hsiao, M. Leptin and Cancer: Updated functional roles in carcinogenesis, therapeutic niches, and Developments. Int. J. Mol. Sci.22https://doi.org/10.3390/ijms22062870 (2021).
Pamuk, G. E. et al. Leptin and resistin levels in serum of patients with hematologic malignancies: Correlation with clinical characteristics. Exp. Oncol.28, 241–244 (2006).
Liu, R., Gao, D., Lv, Y., Zhai, M. & He, A. Importance of circulating adipocytokines in multiple myeloma: A systematic review and meta-analysis based on case-control studies. BMC Endocr. Disorders22https://doi.org/10.1186/s12902-022-00939-2 (2022).
Hofmann, J. N. et al. A prospective study of circulating adipokine levels and risk of multiple myeloma. Blood120, 4418–4420. https://doi.org/10.1182/blood-2012-06-438606 (2012).
Yu, W. et al. Adipocytes secreted leptin is a pro-tumor factor for survival of multiple myeloma under chemotherapy. Oncotarget7, 86075–86086. https://doi.org/10.18632/oncotarget.13342 (2016).
Liu, Z. et al. Mature adipocytes in bone marrow protect myeloma cells against chemotherapy through autophagy activation. Oncotarget6, 34329–34341. https://doi.org/10.18632/oncotarget.6020 (2015).
Patel, L. et al. Resistin is expressed in human macrophages and directly regulated by PPAR gamma activators. Biochem. Biophys. Res. Commun.300, 472–476. https://doi.org/10.1016/s0006-291x(02)02841-3 (2003).
Pang, J. et al. Resistin induces multidrug resistance in myeloma by inhibiting cell death and upregulating ABC transporter expression. Haematologica102, 1273–1280. https://doi.org/10.3324/haematol.2016.154062 (2017).
Tentolouris, A., Ntanasis-Stathopoulos, I. & Terpos, E. Obesity and multiple myeloma: Emerging mechanisms and perspectives. Semin Cancer Biol.92, 45–60. https://doi.org/10.1016/j.semcancer.2023.04.003 (2023).
Long, J. et al. Lipid metabolism and carcinogenesis, cancer development. Am. J. cancer Res.8, 778–791 (2018).
Lu, C. W. et al. VLDL and LDL, but not HDL, promote breast cancer cell proliferation, metastasis and angiogenesis. Cancer Lett.388, 130–138. https://doi.org/10.1016/j.canlet.2016.11.033 (2017).
Kitahara, C. M. et al. Total cholesterol and cancer risk in a large prospective study in Korea. J. Clin. Oncol.29, 1592–1598. https://doi.org/10.1200/jco.2010.31.5200 (2011).
Ding, E. L. & Hu, F. B. Cancer and cholesterol: Understanding the V-shaped association in patients with diabetes. CMAJ179, 403–404. https://doi.org/10.1503/cmaj.081069 (2008).
Choi, T. et al. Lipid level, lipid variability, and risk of multiple myeloma: A Nationwide Population-based study of 3,527,776 subjects. Cancers13https://doi.org/10.3390/cancers13030540 (2021).
Pedersen, K. M., Çolak, Y., Bojesen, S. E. & Nordestgaard, B. G. Low high-density lipoprotein and increased risk of several cancers: 2 population-based cohort studies including 116,728 individuals. J. Hematol. Oncol.13, 129. https://doi.org/10.1186/s13045-020-00963-6 (2020).
Jeong, S. M. et al. Association between high-density lipoprotein cholesterol level and risk of hematologic malignancy. Leukemia35, 1356–1364. https://doi.org/10.1038/s41375-020-01081-5 (2021).
Hungria, V. T. et al. Metabolism of a cholesterol-rich microemulsion (LDE) in patients with multiple myeloma and a preliminary clinical study of LDE as a drug vehicle for the treatment of the disease. Cancer Chemother. Pharmacol.53, 51–60. https://doi.org/10.1007/s00280-003-0692-y (2004).
Sato, J. D., Kawamoto, T. & Okamoto, T. Cholesterol requirement of P3-X63-Ag8 and X63-Ag8.653 mouse myeloma cells for growth in vitro. J. Exp. Med.165, 1761–1766. https://doi.org/10.1084/jem.165.6.1761 (1987).
Li, J. L. et al. Cholesterol requirement for growth of IR983F and P3X63-Ag8-U1 myeloma cells in serum-free medium. Cytobios68, 15–22 (1991).
Scolozzi, R. et al. Hypocholesterolemia in multiple myeloma. Inverse relation to the component M and the clinical stage. Minerva Med.74, 2359–2364 (1983).
Quesney-Huneeus, V. et al. The dual role of mevalonate in the cell cycle. J. Biol. Chem.258, 378–385 (1983).
Negre-Salvayre, A. et al. Antioxidant and cytoprotective properties of high-density lipoproteins in vascular cells. Free Radic. Biol. Med.41, 1031–1040. https://doi.org/10.1016/j.freeradbiomed.2006.07.006 (2006).
Giles, F. J., Krawczyk, J., O’Dwyer, M., Swords, R. & Freeman, C. The role of inflammation in leukaemia. Adv. Exp. Med. Biol.816, 335–360. https://doi.org/10.1007/978-3-0348-0837-8_13 (2014).
Zhu, X. & Parks, J. S. New roles of HDL in inflammation and hematopoiesis. Annu. Rev. Nutr.32, 161–182. https://doi.org/10.1146/annurev-nutr-071811-150709 (2012).
Yvan-Charvet, L. et al. ATP-binding cassette transporters and HDL suppress hematopoietic stem cell proliferation. Science328, 1689–1693. https://doi.org/10.1126/science.1189731 (2010).
Tirado-Vélez, J. M., Benítez-Rondán, A., Cózar-Castellano, I., Medina, F. & Perdomo, G. Low-density lipoprotein cholesterol suppresses apoptosis in human multiple myeloma cells. Ann. Hematol.91, 83–88. https://doi.org/10.1007/s00277-011-1246-8 (2012).
Yavasoglu, I. et al. Cholesterol levels in patients with multiple myeloma. Ann. Hematol.87, 223–228. https://doi.org/10.1007/s00277-007-0375-6 (2008).
Liu, X. et al. Cholesterol levels provide prognostic information in patients with multiple myeloma. Clin. Lab.66https://doi.org/10.7754/Clin.Lab.2019.190824 (2020).
Grinde, K. E. et al. Illustrating, quantifying, and correcting for Bias in Post-hoc Analysis of Gene-based rare variant tests of Association. Front. Genet.8, 117. https://doi.org/10.3389/fgene.2017.00117 (2017).
Fan, J. et al. Causal association of adipokines with osteoarthritis: A Mendelian randomization study. Rheumatology60, 2808–2815. https://doi.org/10.1093/rheumatology/keaa719 (2021).
Kozłowska, L. et al. Adiponectin, resistin and leptin response to dietary intervention in diabetic nephropathy. J. Ren. Nutr.20, 255–262. https://doi.org/10.1053/j.jrn.2010.01.009 (2010).
Becic, T., Studenik, C. & Hoffmann, G. Exercise increases adiponectin and reduces leptin levels in prediabetic and diabetic individuals: Systematic review and meta-analysis of randomized controlled trials. Med. Sci.6https://doi.org/10.3390/medsci6040097 (2018).
Acknowledgements
We thank the Integrated Epidemiology Unit (IEU) Genome-Wide Association Study (GWAS) database for providing the data.
Author information
Authors and Affiliations
Contributions
Y.D.: Performed the literature search, selected the articles and themes, drew schematic fgures, and wrote and edited the fnal manuscript. Y.Z.: Revision in papers. X.Z.: Grammar correction in papers. M.S. and F.D.: Data Collation and proofreading.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ding, Y., Zhang, Y., Zhang, X. et al. Association of lipid levels, adipokines and multiple myeloma: a two-sample multivariate Mendelian randomization study. Sci Rep 14, 25961 (2024). https://doi.org/10.1038/s41598-024-74838-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-74838-y