Abstract
The triple combination elexacaftor-tezacaftor-ivacaftor (ETI) has provided unprecedented clinical benefits for people with cystic fibrosis (pwCF) and drastically transformed the outcome of this disease. We aimed to describe the evolution of lung bacterial colonization in 198 French adult pwCF taking into account the use of concomitantly respiratory treatment. We collected sputum cultures produced during the entire follow-up period starting 3 years before and ending 1 year after ETI initiation. All sputum cultures were centralized and analyzed at our bacteriological laboratory. Clinical data included pulmonary function, respiratory treatments, physiotherapy, number of IV antibiotics treatment, as well as inpatient stays. We observed a significant decrease in colonization prevalence by any CF pathogen after one year of treatment with ETI (p < 0.001). This decrease was confirmed for Pseudomonas aeruginosa, MRSA and MSSA, Stenotrophomonas maltophilia, Achromobacter spp. and nontuberculous mycobacteria (NTM). The maximal density of bacteria documented in sputum cultures decreased from 2.107 CFU/ml to 1.106 CFU/ml after one year of ETI. We also found a decrease in prevalence of Pseudomonas aeruginosa chronic colonization and in the density of Pseudomonas aeruginosa after one year of ETI. These results confirm the decrease in prevalence and bacterial density of lung colonisation for most of the CF pathogens, including Achromobacter spp, Stenotrophomonas maltophilia concomitantly to the clinical improvement. Further studies are needed to better understand the underlying mechanisms of these microbiological changes.
Similar content being viewed by others
Introduction
Typical cystic fibrosis (CF) pathogens include Pseudomonas aeruginosa (Pa), but also methicillin-susceptible Staphylococcus aureus (MSSA), methicillin-resistant Staphylococcus aureus (MRSA), Haemophilus influenzae (Hi), Stenotrophomonas maltophilia (Sm), Achromobacter spp. (Ach), Burkholderia cepacia complex species (Bcc) which can cause pulmonary exacerbations (PEx). In CF, nontuberculous mycobacteria (NTM) can cause significant lung damage and are challenging to treat.
The latest triple combination of elexacaftor-tezacaftor-ivacaftor (ETI), has led to unprecedented improvements in respiratory outcomes by restoring CFTR function, including lung function, risk of PEx, and respiratory symptoms, as well as nutritional status and other manifestations of CF1,2,3 in people with at least one F508del mutation.
The impressive clinical effectiveness of ETI on lung function raises the question of its microbiological repercussions on lung bacteriological colonization. In the PROMISE study, a prospective observational study on 236 patients treated with ETI, Nichols et al. described a significant decrease in density for all measured CF pathogens. However, total bacterial load in sputum as measured by 16 S ddPCR did not decrease during the first 6 months of treatment with ETI4. In another study, Schaupp et al. described a decrease in Pa relative abundance at 3 months and an increase in the microbiome alpha-diversity at 1, 3 and 12 months5 after ETI introduction. In this study, we aimed to describe more precisely the changes in bacterial prevalence and density of CF pathogens in 198 adult pwCF during the 12 months after ETI initiation taking into account their respiratory treatment (mucolytic agents, inhaled antibiotics, azithromycin), frequency of at home respiratory physiotherapy sessions.
Methods
Study design and population
We conducted an observational study including all adult pwCF followed at the CF center at the University Hospital of Lyon, France and starting ETI treatment between January 2020 and December 2021. Patients participating in Phase II or Phase III studies on triple CFTR modulator therapy and meeting those criteria were also included. Our local ethics committee (MR004 #22_5671; Comité Scientifique et Ethique CSE #22_671, Hospices Civils de Lyon) in accordance with national legislation and institutional requirements approved this study. Patients included received a written information leaflet about the study and confirmed informed consent for study participation. All methods were performed in accordance with the relevant guidelines and regulations.
All patients starting ETI were included, including patients participating in Phase II or III studies on triple CFTR modulator therapy. Demographic data extracted from medical files included patients’ age, sex, genotype, body mass index (BMI), percentage of predicted forced expiratory volume in one second (ppFEV1%), respiratory treatment (mucolytic agents, inhaled antibiotics, azithromycin), any prior treatment with CFTR modulator (ivacaftor (IVA), ivacaftor/lumacaftor (IVA/LUM), tezacaftor/lumacaftor (TEZ/LUM)), number of inpatients per year and length of hospitalisations for any respiratory reason. Inpatients were defined as patients hospitalised for at least 24 h during the year of interest.
For each patient, sputum data were retrospectively extracted from all sputum cultures collected during the defined follow-up period of 3 years before and 1 year after ETI initiation. This included sputum collected during routine visits taking place every three months or during PEx. When collected from routine visits, some sputum samples were induced by the inhalation of hypertonic saline solution. No swabs were performed for any of the patients. All sputum cultures had been centralised at our bacteriological laboratory. Cultures were analysed using French national guidelines REMIC recommendations6, detection thresholds were as follow : 102 CFU/ml for Pa, MRSA and MSSA, Sm, Ach, Bcc; 107 CFU/ml for Hi. Bacterial densities in sputum were also collected at 4 different points closest to the one-year interval from ETI initiation namely Y-2 (mean ± SD): -25.6 ± 1.6 months, Y-1: -13.6 ± 1.7 months, Y0: -0.9 ± 2.1 months and Y + 1: 9.5 ± 2.8 months.
According to the recommendations, PEx was defined as increased cough or sputum production, shortness of breath and lung function decline, associated with loss of weight or appetite, chest pain, fever7; leading to antibiotic therapy initiation.
Colonisation definitions
Colonisation was defined as positive if at least one sputum culture per year was positive. Positivity threshold was 102 CFU/ml for Pa, MSSA and MRSA, Sm, Ach, Bcc, and 107CFU/ml for Hi. The status of Pa colonisation was defined according to the Leeds criteria8. When Pa had never been documented, patients were defined as never colonised. Colonisation was considered as chronic when more than half the sputum cultures were positive during a year, with a minimum of two sputum cultures, and as intermittent otherwise. Patients were considered as free if none of their sputum cultures was positive for a whole year if previously colonised (cleared from Pa).
Statistical analysis
Bacterial colonisation prevalences were assessed each year as the proportion of patients with at least one positive sputum culture during the year. The 95% confidence intervals were built using the Wilson method. Logistic mixed models with a random intercept were carried out to test the treatment effect on colonisation. A linear mixed model was carried out to quantify ETI effect on ppFEV1 change over time. Patients were divided into three groups depending on ETI effect on ppFEV1 change (high, moderate and low), according to the terciles of the random effects on the treatment effect. They were also divided into four groups according to the age quartiles and to ppFEV1 at Y0. Colonisation prevalences during Y + 1 were compared between the groups using a chi-square test to test the existence of an association between ETI effect on colonisation and age, severity of lung damage or ETI effect on ppFEV1 change. P-values were corrected using the Holm method to take into account the test multiplicity. All the analyses were carried out using the statistical software R, version 4.3.19. Statistical significance was defined by a p-value < 0.05.
Results
Clinical characteristics of the population
One hundred ninety-eight adult pwCF were included with a median age of 28.8 years at ETI introduction and a higher male proportion (n = 120, 61%). Among them, 24 patients were participating in Phase II or III studies on triple CFTR modulator therapy. One hundred twenty-two patients (62%) were homozygous for F508del. One hundred seven patients (54%) had received treatment with a prior CFTR modulator, mainly lumacaftor-ivacaftor, before starting ETI. Median ppFEV1 was 65% at ETI introduction (Table 1).
One hundred ninety-six patients completed a full year of ETI. Of the 2 patients who did not complete a full year of treatment, one patient died of an abdominal surgery unrelated to CF, and one patient moved out of the region. All 198 patients were analysed within the cohort.
During the 3 years before ETI introduction, mean ppFEV1 was respectively 65.4% ± 20.0, 63.8% ± 20.3, 60.1% ± 21.6 at Y-2, Y-1 and Y0 and improved at Y + 1 to 77.4% ± 22.5 (Fig. 1A).
The mean number of PEx was respectively 3.0, 2.5 and 2.8 per patient per year at Y-2, Y-1 and Y0 and decreased to 0.7 at Y + 1 (Fig. 1B). Respiratory physiotherapy was performed at a mean frequency of 4.0, 3.8, 3.8 times per week at Y-2, Y-1 and Y0 and decreased to a mean frequency of 2.2 times a week at Y + 1 (Fig. 1B).
The proportion of patients using respiratory treatment decreased during follow-up. Patients using mucolytic agents (dornase alpha or hypertonic saline solution) decreased from 89%, 90%, 92% at Y-2, Y-1 and Y0 to 72% at Y + 1. Patients using inhaled antibiotic decreased from 69%, 68%, 65 at Y-2, Y-1 and Y0 to 37% at Y + 1 (tobramycin from 40%, 38%, 37–20%; colistin from 42%, 34%, 31–18%; aztreonam from 26%, 31%, 30–10%). Patients using oral azithromycin decreased from 32%, 37%, 42% at Y-2, Y-1 and Y0 to 11% at Y + 1 (Fig. 1C).
The number of inpatients per year was 45 (23%), 47 (24%) and 56 (28%) for a mean length of stay of 18 days ± 12.7, 19 days ± 11.1, 21 days ± 15.5 at Y-2, Y-1, Y0, and decreased to 6 (3%) for a mean length of stay of 11 days ± 2.1 at Y + 1 (Fig. 1D).
Sputum cultures
The number of patients able to produce at least one sputum culture was 194, 196, 198 at Y-2, Y-1 and Y0, and 179 at Y + 1. Seventeen patients did not provide any sputum culture at Y + 1 due to lack of productive cough despite sputum induction with inhaled hypertonic saline. The mean number of sputum cultures per year for each patient able to produce sputum was stable for the 3 years before ETI and decreased at Y + 1 (Table 2).
Prevalence of bacterial colonisation
Results are summarised in Table 2. Almost all patients were classified as colonised by one of the seven CF pathogens of interest of the study (at least one positive sputum culture per year) for each of the three years before ETI initiation (99%, n = 193; 99%, n = 194; 98%, n = 195). The number of colonised patients significantly decreased to 161 patients (90%) at Y + 1, p < 0.001.
The prevalence of patients positive for Pa, MRSA, MSSA, Sm and Ach was stable from Y-2 to Y0 and significantly decreased at Y + 1 (p < 0.05).
There was no significant change in Hi and Bcc prevalences during follow-up.
The prevalence of patients positive for NTM was 7.2% (n = 14), 8.7% (n = 17) and 10% (n = 20) during the three years before ETI and decreased significantly to 1.7% (n = 3) at Y + 1, p < 0.001. Considering the three patients remaining positive after ETI initiation, 2 were positive for M. avium and one for M. intracellulare. All the patients colonised at Y0 with M. abscessus (n = 6) and M. chimerae (n = 3) cleared their sputum at Y + 1.
Summed CF pathogens culture density
Summed bacterial density, defined as the concentration of all cultured bacteria in sputum cultures, also decreased after the initiation of ETI, from a median of 2.107 CFU/ml, 1.107 CFU/ml, 2.107 CFU/ml during the three years before ETI introduction, to a median of 1.106 CFU/ml at Y + 1 (See Supplementary Fig. 1).
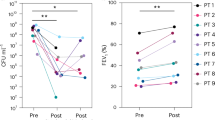
Mean bacterial density for each CF pathogens of interest
Due to instability of mean bacterial densities in sputum cultures during the 3-year period before ETI for MSSA, Hi, Ach and Bcc, no comparison test with the period after ETI was performed. We observed a decreasing tendency of mean bacterial densities of each CF pathogens of interest after ETI, except for Hi. (Fig. 2).
Focus on Pseudomonas aeruginosa
For Pa colonisation, we considered the following groups: patients never colonised, chronically and intermittently colonised patients, and patients considered as free (cleared from Pa). The prevalence of Pa chronic colonisation decreased from 65% (n = 129) at Y0 to 51% (n = 91) at Y + 1. The prevalence of Pa intermittent colonisation remained stable. This stability was explained by the conversion from chronic colonisation to intermittent colonisation (n = 11) and from intermittent colonisation to free (n = 8). There was no new colonisation with Pa after ETI initiation (Fig. 3).
Association between colonisation prevalence and clinical features (table 3)
The colonisation prevalence during the year following the treatment introduction (Y + 1) was significantly different according to the age quartile (p = 0.03), with a trend to a decrease in younger patients. The colonisation prevalence decrease during Y + 1 seemed to be higher for patients with less severe lung damage estimated by ppFEV1 at Y0, but this trend did not reach statistical significance (p = 0.06). No link was identified between treatment effect on ppFEV1 change and treatment effect on colonisation prevalence (p = 0.88).
Discussion
This study showed a significant prevalence reduction in lung bacterial colonisation by typical CF pathogens, from 99 to 90%, and a decrease in the maximum bacterial density in sputum after one year of ETI treatment, in a context of reduced use of respiratory treatment (mucolytic agents, azithromycin) and of respiratory physiotherapy sessions. This reduction is greater in younger adults with better pulmonary function.
The samples analysed in this study were sputum cultures performed as recommended in current routine clinical practices10. Sputum cultures are considered the best method to reflect lung colonisation in adults while maintaining a favorable balance between convenience, tolerability and sufficient specificity and sensitivity11. Treatment with ETI induced a dramatic reduction in sputum but we obtained sputum analysis for 179 patients.
Our study displays several strengths. First, our population size is important, with a time of follow-up extending over one year after ETI introduction. Furthermore, our results are consistent with existing data on clinical improvement following ETI initiation available in other trials12,13in terms of lung function improvement. Our study also reports real-world data on PEx and hospitalisations, the decrease in therapeutic burden, i.e. a reduction in the number of patients using mucolytic agents, long-term inhaled (tobramycin, colistin, aztreonam) or oral (azithromycin) antibiotics and also in the frequency of weekly physiotherapy sessions. These results have not been reported in other real-world studies. The decrease in most CF pathogens density described in this study seemed to have started before ETI introduction. This could be explained by the large number of patients already treated with ivacaftor/ lumacaftor, but also the decrease of routine visits during Covid pandemic. We confirmed the reduction in lung bacterial colonization during the year after ETI introduction despite the reduction in the use of respiratory treatments already practiced in real life by pwCF. Several studies investigating changes in the pulmonary microbiota under ETI treatment corroborate our findings5,14,15. Migliorisi et al. reported nearly 45% of sputum cultures becoming negative after a year of treatment with ETI in a small cohort of 26 patients16. In a case-control study on 24 patients, Sosinski et al. found a ratio decrease in typical CF pathogens in the first sputum culture collected after ETI introduction14. Pallenberg et al. found a decrease in total bacterial density in 31 patients after 14 and 50 weeks of treatment with ETI15, also corroborating our results. In contrast, Schaupp et al. found no change in total bacterial density on 79 patients after 1 year of treatment with ETI5.
Focusing on Pa, our results confirmed those of other studies both in terms of prevalence decrease4,13,15,17,18and in terms of bacterial density decrease4,19. There are few data on the evolution of Pa colonisation status. Nichols et al. showed a trend towards a lower eradication rate in patients with colonisation defined as chronic or mucoid Pa, although this trend was not significant4. In our study, almost a third of patients with chronic Pa colonisation before ETI modified their status under ETI, either towards intermittent colonisation, remission or the absence of sputum.
The prevalence of both MSSA and MRSA significantly decreased after one year of treatment, confirming existing results for MRSA13,15,18and for MSSA15.
Changes in Sm prevalence were reported in a single other study4, describing 16 of 25 previously Sm-positive patients becoming culture negative after 6 months of treatment with ETI. A previous study describing Ach colonisation did not show any change in Ach prevalence during treatment with ETI4. On contrary, our study showed a decrease in Ach prevalence. The only study focusing NTM prevalence is a retrospective study on 15 patients describing a decrease in NTM prevalence, particularly species from the M. abscessuscomplex, after one year of ETI treatment20.
While no change in Hi prevalence was evident after ETI introduction, a trend towards increasing Hi density was observed in our study. Similar results were reported by Pallenberg et al., showing an increase in DNA detection at 14 and 50 weeks post-ETI in 6 patients who were Hi-negative before ETI initiation15and also by Heltshe SL in G551D pwCF treated with ivacaftor21. Hi is usually detected early in the disease course. Its growth has been described as inhibited by the production of pyocyanin by Pa22. An increased density could be an indirect indicator confirming the eradication of Pa in the lungs of pwCF.
The reduction of summed CF culture density highlight the complex microbial dynamics in CF lungs with interactions inbetwwen species, which can influence the immune response and the chronicity of infections. Our results regarding bacterial prevalence decrease should be interpreted with caution. Even though we obtained a mean number of 3.1 sputum per patient, many pwCF treated with ETI have lowered frequency of expectorations along with poor sputum quality. Moreover, the absence of pathogen documentation in sputum is not a proof of its eradication and may reflect its presence under a threshold of detection.
The contrast between the major clinical improvement and the moderate decrease in lung bacterial colonisation reported in this study and in current literature questions the underlying mechanisms influencing either of those parameters. Acquired lung damage, such as bronchiectasis, can encourage chronic colonisation and take part in a reduced efficacy in bacterial eradication23. In a previous study on the effects of ivacaftor, Heltshe et al. found no correlation between the decrease in Pa frequency and age nor FEV1 at baseline, but with the improvement of FEV1 when Pa culture positivity was analysed as a continuous variable based on the proportion of positive cultures21. Our study was conducted with adult patients, thus more likely to have structural lung damage24, while change in colonisation status during treatment with ETI seemed to be associated with a younger age and better ppFEV1 at introduction.
Much remains to be elucidated to better understand the pathophysiological mechanisms underlying the clinical respiratory improvement and the evolution of pulmonary colonisation in patients treated with ETI. In this context, the question of antibiotic strategies needs to be reconsidered. Antibiotics have been used to eradicate bacteria early after lung colonisation, to control pathogens during chronic colonisation as a maintenance therapy,and to recover from PEx7,25. Therapeutic de-escalation must be carried out with great care, as the benefits of antibiotics in the course of CF disease remain central and as pathogen identification during follow-up is becoming less reliable as patients expectorate less frequently and less abundantly when treated with ETI. In this study,chronic antibiotic discontinuation was usually due to the patient’s decision. In addition to SIMPLIFY26, further studies will be needed to confirm the safety of stopping treatments. On top of these new challenges, classic challenges regarding antibiotic therapy persist : selection of antibiotic-resistant bacteria, adverse events with tissue or organ damage,and lack of microbial selectivity and therefore unwanted effect on bronchial and digestive microbiota27. New techniques for the detection of lung infectious diseases,better management of antibiotic adverse effect and simplification of treatment burden are 3 of the top 10 updated priorities highlighted by the James Lind Alliance in order to help clinicians take on the new therapeutic challenges raised by the HEMT era28.
Conclusion
Our study confirms the decrease both in sputum bacterial density and in the prevalence of lung colonisation by most CF pathogens, in association with clinical respiratory improvement in adult pwCF after one year of treatment with ETI and in a context of respiratory treatment reduction. These microbiological changes highlight the need for CF medical care guidelines updating for sputum monitoring and antibiotic strategies for PEx.
Evolution of clinical features. (A) evolution of lung function before and after ETI, ppFEV1%. (B) Evolution of respiratory symptoms, estimated by the frequency of weekly physiotherapy sessions and the number of PEx per patient per year. (C) Evolution of treatment load, focusing on pulmonary treatments: mucolytic agents, inhaled antibiotics, azithromycin. (D) Evolution of number of inpatients per year and length of stay hospitalisations stay.
Change of Pseudomonas aeruginosa colonisation status from Y0 (at ETI initiation) to Y + 1 (one year after ETI initiation). Colonisation was considered as chronic if more than half the sputum cultures were positive during the year; as intermittent if less than half the sputum cultures were positive during the year and patient was considered as free if previously colonised and no Pa was documented during the year. A minimum of 2 sputum cultures per year was required.
Data availability
the datasets used and/or analysed during the current study are available form the corresponding author on reasonable request.
Abbreviations
- Ach:
-
Achromobacter
- ATP:
-
adenosin triphosphate
- Bcc:
-
Burkholderia cepacia complex
- CF:
-
cystic fibrosis
- CFTR:
-
cystic fibrosis transmembrane conductance regulator
- ETI:
-
elexacaftor-tezacaftor-ivacaftor
- FCV:
-
forced vital capacity
- HEMT:
-
highly effective modulator therapy
- Hi:
-
Haemophilus influenzae
- IVA:
-
ivacaftor
- IVA/LUM:
-
ivacaftor/lumacaftor
- MRSA:
-
methicillin-resistant Staphylococcus aureus
- MSSA:
-
methicillin-susceptible Staphylococcus aureus
- NTM:
-
nontuberculous mycobacteria
- Pa:
-
Pseudomonas aeruginosa
- PEx:
-
pulmonary exacerbation
- ppFEV1:
-
percentage of predicted forced expiratory volume in one second
- pwCF:
-
patients with CF
- Sa:
-
Staphylococcus aureus
- Sm:
-
Stenotrophomonas maltophilia
- TEZ/LUM:
-
tezacaftor/lumacaftor
References
Keating, D. et al. VX-445-tezacaftor-ivacaftor in patients with cystic fibrosis and one or two Phe508del alleles. N Engl. J. Med.379 (17), 1612–1620 (2018).
Barry, P. J. et al. Triple therapy for cystic fibrosis Phe508del-Gating and -residual function genotypes. N Engl. J. Med.385 (9), 815–825 (2021).
Sutharsan, S. et al. Efficacy and safety of elexacaftor plus tezacaftor plus ivacaftor versus tezacaftor plus ivacaftor in people with cystic fibrosis homozygous for F508del-CFTR: a 24-week, multicentre, randomised, double-blind, active-controlled, phase 3b trial. Lancet Respir Med.10 (3), 267–277 (2022).
Nichols, D. P. et al. Pharmacologic improvement of CFTR function rapidly decreases sputum pathogen density, but lung infections generally persist. J. Clin. Invest.133 (10), e167957 (2023).
Schaupp, L. et al. Longitudinal effects of elexacaftor/tezacaftor/ivacaftor on sputum viscoelastic properties, airway infection and inflammation in patients with cystic fibrosis. Eur. Respir J.62 (2), 2202153 (2023).
VG Librairies [Internet]. [cited 2023 Dec 4]. REMIC: référentiel en microbiologie médicale. Société française de microbiologie médicale. (2022). https://www.vg-librairies.fr/sciences-fondamentales/8653-remic-referentiel-en-microbiologie-medicale.html
Flume, P. A. et al. Cystic fibrosis pulmonary guidelines: treatment of pulmonary exacerbations. Am. J. Respir Crit. Care Med.180 (9), 802–808 (2009).
Lee, T. W. R., Brownlee, K. G., Conway, S. P., Denton, M. & Littlewood, J. M. Evaluation of a new definition for chronic Pseudomonas aeruginosa infection in cystic fibrosis patients. J. Cyst. Fibros.2 (1), 29–34 (2003).
R Core Team. R A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna. - References - Scientific Research Publishing [Internet]. [cited 2023 Nov 30]. (2022). https://www.scirp.org/(S(lz5mqp453ed%20snp55rrgjct55))/reference/referencespapers.aspx?referenceid=3456808
Saiman, L. & Siegel, J. Infection control recommendations for patients with cystic fibrosis: Microbiology, important pathogens, and infection control practices to prevent patient-to-patient transmission. Am. J. Infect. Control. 31 (3), S6–62 (2003).
Jung, A. et al. Sequential genotyping of Pseudomonas aeruginosa from upper and lower airways of cystic fibrosis patients. Eur. Respir J.20 (6), 1457–1463 (2002).
Miller, A. C. et al. The Rapid reduction of infection-related visits and antibiotic use among people with cystic fibrosis after starting Elexacaftor-Tezacaftor-Ivacaftor. Clin. Infect. Dis.75 (7), 1115–1122 (2022).
Gushue, C. et al. Impact of Elexacaftor–Tezacaftor–Ivacaftor on lung disease in cystic fibrosis. Pediatr. Pulmonol.58 (8), 2308–2316 (2023).
Sosinski, L. M., Neugebauer, H. C. M., Ghuneim, K. A., Guzior, L. A. J. & Castillo-Bahena, D. V. A restructuring of microbiome niche space is associated with Elexacaftor-Tezacaftor-Ivacaftor therapy in the cystic fibrosis lung. J. Cyst. Fibros.21 (6), 996–1005 (2022).
Pallenberg, S. T. et al. Impact of Elexacaftor/Tezacaftor/Ivacaftor Therapy on the cystic fibrosis Airway Microbial Metagenome. Microbiol. Spectr.10 (5), e01454–e01422 (2022).
Migliorisi, G. et al. Elexacaftor-Tezacaftor-Ivacaftor as a final Frontier in the treatment of cystic fibrosis: definition of the clinical and microbiological implications in a case-control study. Pharmaceuticals. 15 (5), 606 (2022).
Beck, M. R., Hornick, D. B., Pena, T. A., Singh, S. B. & Wright, B. A. Impact of elexacaftor/tezacaftor/ivacaftor on bacterial cultures from people with cystic fibrosis. Pediatr. Pulmonol.58 (5), 1569–1573 (2023).
Sheikh, S. et al. Impact of elexacaftor–tezacaftor–ivacaftor on bacterial colonization and inflammatory responses in cystic fibrosis. Pediatr. Pulmonol.58 (3), 825–833 (2023).
Casey, M. et al. Effect of elexacaftor/tezacaftor/ivacaftor on airway and systemic inflammation in cystic fibrosis. Thorax. 78 (8), 835–839 (2023).
Wiesel, V. et al. Eradication of Nontuberculous Mycobacteria in people with cystic fibrosis treated with Elexacaftor/Tezacaftor/Ivacaftor: a Multicenter Cohort Study. J. Cyst. Fibros. ;S1569199323001339. (2023).
Heltshe, S. L. et al. Pseudomonas aeruginosa in cystic fibrosis patients with G551D-CFTR treated with ivacaftor. Clin. Infect. Dis. Off Publ Infect. Dis. Soc. Am.60 (5), 703–712 (2015).
Welp, A. L. & Bomberger, J. M. Bacterial community interactions during chronic respiratory disease. Front. Cell. Infect. Microbiol.10, 213 (2020).
Ratjen, F. et al. Cystic fibrosis. Nat. Rev. Dis. Primer. 1 (1), 15010 (2015).
Grasemann, H. & Ratjen, F. Cystic fibrosis. N Engl. J. Med.389 (18), 1693–1707 (2023).
Castellani, C. et al. ECFS best practice guidelines: the 2018 revision. J. Cyst. Fibros.17 (2), 153–178 (2018).
Mayer-Hamblett, N. et al. Discontinuation versus continuation of hypertonic saline or dornase alfa in modulator treated people with cystic fibrosis (SIMPLIFY): results from two parallel, multicentre, open-label, randomised, controlled, non-inferiority trials. Lancet Respir Med.11 (4), 329–340 (2023).
Nelson, M. T. et al. Maintenance tobramycin primarily affects untargeted bacteria in the CF sputum microbiome. Thorax. 75 (9), 780–790 (2020).
Rowbotham, N. J. et al. A refresh of the top 10 research priorities in cystic fibrosis. Thorax. 78 (8), 840–843 (2023).
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
L.M., A.DJ., Q.R. contributed to the design of the studyL.M., Q.R., L.B. contributed to the management and analysis of the dataL.M., A.DJ., M.R., Q.R. took the lead in writing the manuscriptAll authors provided critical feedback and helped shape the research, analysis and manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mianowski, L., Doléans-Jordheim, A., Barraud, L. et al. One year of ETI reduces lung bacterial colonisation in adults with cystic fibrosis. Sci Rep 14, 29298 (2024). https://doi.org/10.1038/s41598-024-77246-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-77246-4
Keywords
This article is cited by
-
Progress of personalized medicine of cystic fibrosis in the times of efficient CFTR modulators
Molecular and Cellular Pediatrics (2025)