Abstract
To assess the circulating characteristics of common respiratory pathogens following the complete relaxation of non-pharmaceutical interventions (NPIs) and the cessation of the dynamic zero-COVID policy. The retrospective analysis was conducted from 14,412 patients with acute respiratory infections (ARIs) from January 24, 2020, to December 31, 2023, including Influenza A virus (IFV-A), Influenza B virus (IFV-B), Respiratory Syncytial Virus (RSV), Human Rhinovirus (HRV), Human Parainfluenza Virus (HPIV), Human Metapneumovirus (HMPV), Human Coronavirus (HCoV), Human Bocavirus (HBoV), Human Adenovirus (HAdV), and Mycoplasma pneumoniae (MP). Compared with 2020–2022, Joinpoint analysis indicated a monthly increase in overall pathogen activity in 2023, rising from an average of 43.05% to an average of 68.46%. The positive rates of IFV-A, IFV-B, HMPV, HPIV, HCoV, and MP increased, while those of HRV and RSV decreased, and no differences in HAdV and HBoV. The outbreak of IFV-A and MP was observed, the positive rate of MP has surpassed pre-COVID-19 pandemic levels and the spread of RSV was interrupted by IFV-A. Infants and toddlers were primarily infected by HRV and RSV, Children and adolescents exhibited a higher prevalence of infections with MP, IFV-A, and HRV, whereas Adults and the elderly were primarily infected by IFV-A. The incidence of co-infections rose from 4.25 to 13.73%. Restricted cubic spline models showed that the susceptible age ranges for multiple pathogens expanded. These changes serve as a reminder to stay alert in the future and offer clinicians a useful guide for diagnosing and treating.
Similar content being viewed by others
Introduction
Acute respiratory infections (ARIs) represent a substantial public health concern on a global scale1and are commonly caused by a variety of pathogens, including viruses, bacteria, and mycoplasmas. These pathogens typically infect respiratory cells, leading not only to self-limiting diseases confined to the upper respiratory tract with mild symptoms but also to the development of acute bronchiolitis, pneumonia, chronic lung diseases, and exacerbations of other systemic diseases2. Spread through droplets and aerosols, these pathogens are characterized by rapid transmission and a broad range3, capable of infecting large groups in a short period and impacting different demographics. For instance, Human Rhinovirus (HRV) can increase airway inflammation and the severity of clinical symptoms in asthma patients4, while Mycoplasma pneumoniaecan cause severe upper and lower respiratory tract infections in children and adults5. Influenza virus (IFV) related hospitalizations and serious complications pose a severe health threat to the elderly population6, and Respiratory Syncytial Virus (RSV) is among the most common and severe infections in infants and the elderly globally7, with immunocompromised adults also suffering significant consequences from RSV infections. Additionally, Human Parainfluenza Virus (HPIV), Human Metapneumovirus (HMPV), Human Adenovirus (HAdV), Human Bocavirus (HBoV), and Human Coronavirus (HCoV) are among the principal pathogens causing ARIs.
The COVID-19 pandemic has heightened awareness of the severe dangers posed by the transmission of respiratory pathogens8. Many countries have implemented non-pharmaceutical interventions (NPIs) to curb the spread of SARS-CoV-2. In China, varying levels of NPIs and the dynamic zero-COVID policy were enforced for nearly three years, leading to reduced transmission of influenza and other common respiratory pathogens, and a lower level of natural immunity in the population, thereby increasing susceptibility in the following seasons. With the relaxation of NPIs, countries like Israel reported a resurgence of respiratory viral infections in 20229, and Germany reported a sharp increase in severe respiratory infections associated with IFV and RSV towards the end of 202210. In December 2022, China announced the end of the dynamic zero-COVID policy and full relaxation of NPIs11, with domestic and international travel and cooperative exchanges fully reopened, and social activities no longer restricted, signaling new challenges for respiratory pathogen infections. In 2023, an increase in cases of influenza-like illnesses and pneumonia was monitored in Beijing, China12. However, the characteristics of respiratory pathogen infections are often influenced by regional, seasonal, demographic, and other factors, and there is a significant climatic difference between the northern and southern regions of China. To date, there has been no investigation into the circulating characteristics of common pathogens in this region following the complete relaxation of NPIs and the end of the dynamic zero-COVID policy.
This study involves a retrospective analysis of laboratory data from 14,412 ARIs patients at the Ningbo Medical Center, Li Hui Li Hospital, from January 24, 2020, to December 31, 2023, aimed at investigating the changes in the epidemiological patterns of common respiratory pathogens in Ningbo in 2023, providing a critical reference for future potential pathogen epidemics and formulating prevention and control strategies.
Methods
Study population and data sources
This retrospective study included patients with ARIs who were treated at the Medical Center LHL Hospital in Ningbo between January 24, 2020, and December 31, 2023. Relevant data were extracted from the hospital’s laboratory information system. Patients with incomplete clinical data were excluded from the study, resulting in a total cohort of 14,412 cases. (1124 cases in 2020, 2006 cases in 2021, 1976 cases in 2022, and 9306 cases in 2023).
Laboratory testing
Nasopharyngeal or throat swab samples were collected from patients for laboratory analysis. Various pathogens were detected using polymerase chain reaction (PCR) capillary electrophoresis technology including Influenza A virus (IFV-A), Influenza B virus (IFV-B), Respiratory Syncytial Virus (RSV), Human Rhinovirus (HRV), Human Parainfluenza Virus (HPIV), Human Metapneumovirus (HMPV), Human Coronavirus (HCoV), Human Bocavirus (HBoV), Human Adenovirus (HAdV), and Mycoplasma pneumoniae (MP). (HEALTH GENENTECH, Ningbo, China).
Statistical analysis
Statistical analysis was performed using R software (version 4.2.1, https://cran.r-project.org). Medians and interquartile ranges (IQRs) were reported for continuous variables, while categorical variables were represented as percentages ((n, %) and analyzed using the Wallis rank sum test or Pearson’s Chi-squared test. The interactions among pathogens are estimated by Spearman correlate analysis. Monthly changes in overall pathogen activity were analyzed using Joinpoint software(version 5.0, https://surveillance.cancer.gov/joinpoint). Non-linear associations between age and pathogen positivity rates were evaluated using a restricted cubic spline regression model(RCS), with four knots set at the 20th, 40th, 60th, and 80th percentiles. P-value < 0.05 was considered statistically significant.
Results
General data of the study population
This study included data from 14,412 cases, with cases increasing from 5,106 cases in 2020–2022 to 9,306 cases in 2023. Patients were divided into five age groups: Infants and toddlers (0–3 years, 4,009 patients, 27.82%), children (4–6 years, 3,094 patients, 21.47%), adolescents (7–17 years, 3,273 patients, 22.71%), adults (18–59 years, 2,136 patients, 14.82%), and the elderly (≥ 60 years, 1,900 patients, 13.18%). In 2023, there was a significant increase in the median age of patients and the proportion of females (P < 0.05). Additionally, the proportion of the Infants and toddler group significantly decreased, while the proportions of adolescents, adults, and the elderly increased (P < 0.001). The positive rates of IFV-A, IFV-B, HMPV, HPIV, HCoV, and MP increased, while those of HRV and RSV decreased(P < 0.05). No differences were observed in the detection rates of HAdV and HBoV(P > 0.05). (Table 1).
Monthly distribution characteristics of overall Pathogen activity
The detection rate of at least one pathogen infection within the study population was calculated monthly to assess the overall activity of the respiratory pathogens (Fig. 1). Using Joinpoint analysis, it was found that overall pathogen activity decreased from January 2020 to April 2020 (APC = −56.82), then rapidly increased until July 2020 (APC = 96.63). From July 2020 to January 2023, there was a slow decline (APC = −1.27), until it consistently rose from January 2023 to the end of the year (APC = 8.71). (P < 0.05). There were three significant turning points in the trend of pathogen activity, in April 2020, July 2020, and January 2023. Overall activity of the respiratory pathogens increased from an average of 43.05% in 2020–2022 to an average of 68.46% in 2023 (P < 0.001).
Joinpoint analysis of overall monthly pathogen activity from January 2020 to December 2023. Colored lines represent the fitting model for the red dots. The legend provides the Annual Percentage Change (APC) values for the fitting curve each month. *Indicates a significant difference from 0, with a two-sided P-value < 0.05.
Season characteristics of individual pathogens
Except for July 2022, IFV-A (Fig. 2A) was almost undetectable during 2020–2022, but reappeared in March-April 2023, with an outbreak beginning in October. IFV-B (Fig. 2B) experienced a similar period of low activity, lasting from July 2021 to April 2022, with few detections after that and a significant increase starting in November 2023.
Season Characteristics of Individual Pathogens from January 2020 to December 2023. (A) Influenza A virus; (B) Influenza B virus (C) Human Rhinovirus; (D) Human Adenovirus; (E) Human Parainfluenza virus; (F) Human Bocavirus; (G) Respiratory syncytial virus; (H) Human Metapneumovirus; (I) Human Coronavirus; (J) Mycoplasma pneumoniae.
HRV (Fig. 2C) was the first to rebound in June 2020, maintaining a high detection rate until November when it declined. HAdV (Fig. 2D), HPIV (Fig. 2E), and HBoV (Fig. 2F) began to rebound in November 2020. In 2023, with HRV detections decreasing, HPIV increasing, and no significant changes in HBoV and HAdV detections.
RSV (Fig. 2G) and HMPV (Fig. 2H) began to rebound towards the end of 2020. Except for a peak in RSV infections in September 2021, most peaks occurred in winter. From April 2023, the number of RSV cases and the detection rate continually rose, peaking in September, but sharply declined from October, while HMPV cases continued to increase from September.
HCoV (Fig. 2I) had lower detection numbers and rates in both phases, though slight peaks were in July or October. MP (Fig. 2J) was continuously detected from April 2022, with a stable number of detections each month until April 2023, when MP detection rates and numbers sharply increased, peaking from July to October.
Age characteristics of pathogen epidemiological patterns
From 2020 to 2022, HRV consistently exhibited the highest positive rates across all age groups. In 2023, a distinct shift in the pattern of pathogen detection was observed across various age demographics. In Infants and toddlers (Fig. 3A), notable increases were recorded in the positive rates of IFV-A, HBoV, HRV, HPIV, RSV, HMPV, and MP, (P < 0.05). HRV was predominant, detected at a rate of 24.76%, followed by RSV (17.18%) and MP (12.27%).
For the children’s group (Fig. 3B), notable rises were observed in the detection of IFV-A, HPIV, HCoV, HMPV, and MP (P < 0.05), with MP being most prevalent at a rate of 31.21%. This was followed by HRV (22.54%) and IFV-A (22.28%). In adolescents (Fig. 3C), increased detection was noted for IFV-A, IFV-B, HMPV, and MP, whereas RSV saw a reduction in positive rates (P < 0.05). MP was most frequently detected, occurring at a rate of 33.48%, with IFV-A (29.71%) and HRV (15.83%) trailing.
Within the Adults (Fig. 3D), there were rises in the positive rates of IFV-A, HCoV, HMPV, HAdV, and MP (P < 0.05), with IFV-A leading at a rate of 30.08%, followed by HRV (7.08%) and MP (5.49%). Lastly, in the elderly group (Fig. 3E), enhancements in the positive rates of IFV-A, HRV, HPIV, HCoV, HAdV, and MP were seen (P < 0.05). IFV-A had the highest positive rate at 13.47%, succeeded by HRV (6.37%) and HCoV (3.77%).
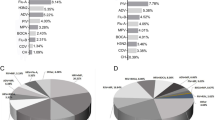
Single infection, co-infections, and the interactions between pathogens
From 2020 to 2022, 1,981 out of 5,106 cases (38.79%) were infected with one pathogen, with HRV being the most prevalent in single infections, accounting for 738 out of 5,106 cases (14.45%), followed by RSV with 302 cases (5.91%). Co-infections occurred in 217 out of 5,106 cases (4.25%) (Fig. 4A). In the co-infections (Fig. 4B), dual infections accounted for 210 out of 217 cases (96.77%), with the most common being HRV + HMPV and HRV + HAdV, each at 30 cases (13.82%), followed by HRV + RSV at 24 cases (11.06%) and HRV + HPIV) at 22 cases (10.44%). There were 5 cases of triple infections (2.30%) and 2 cases of quadruple infections (0.92%).
(A) Distribution of respiratory pathogen infection patterns in 2020–2022. (B) Co-infection proportions in 2020–2022. (C) Distribution of respiratory pathogen infection patterns in 2023. (D) Co-infection proportions in 2023. (E) The interactions between two pathogens. Positive interactions with P-value < 0.05 were denoted in red star and the negative interactions with P-value < 0.05 were denoted in black star.
In 2023, the positive rate of one pathogen and co-infections among the population increased(P < 0.05), with 5,093 out of 9,306 cases (54.72%) infected with one pathogen. IFV-A led the single infections with 1,687 out of 9,306 cases (18.13%), followed by MP with 1,206 cases (12.95%). There were 1,278 out of 9,306 cases (13.73%) with co-infections involving two or more pathogens (Fig. 4C). In these co-infections (Fig. 4D), dual infections dominated with 1,169 out of 1,278 cases (91.47%), the most common being HRV + MP at 286 cases (22.38%), followed by IFV-A + HRV at 161 cases (12.60%) and IFV-A + MP at 73 cases (5.71%). There were 104 cases of triple infections (8.14%), with MP + HRV + others being the most common in triple infections (3.21%), and 5 cases of quadruple infections (0.39%).
Analysis of all pathogen interactions (Fig. 4E) revealed negative interactions between IFV-A and all other pathogens, MP and other eight pathogens (excluding HCoV), and RSV and other seven pathogens (excluding HBoV and HAdV). Positive interactions were observed between IFV-B and HMPV, and between HRV and HBoV. (P < 0.05)
Non-linear relationship between age and pathogen positivity rate
A restricted cubic spline (RCS) regression model (P-nonlinear < 0.001) was used to evaluate the non-linear relationship between age and the risk of infection by various pathogens in two 2020–2022 and 2023 respectively, age-risk trends in the two stages were consistent, we observed that the odds ratios (ORs) associated with IFV-A, IFV-B, HRV, HMPV, HAdV, and MP infections first increase with age and then decrease (Fig. 5A, B, C, D, E and F respectively), reaching their peak at ages 24, 27, 3, 4, 5, and 8 years, respectively. For HPIV, RSV, and HBoV, age-related OR values decreased with increasing age, peaking in groups under 1 year of age (Fig. 5G, H and I). HCoV (Fig. 5J) showed a pattern of initial decrease followed by an increase in OR with age, with the highest OR values in groups under 1 year and over 90 years. Data indicate that the age-related OR values for IFV-A, IFV-B, HRV, HMPV, HAdV, MP, HPIV, and HCoV were higher in 2023, within a certain range of susceptible ages.
Non-linear associations between age and the risk of respiratory pathogen infections were estimated by the restricted cubic spline regression model. (A) Influenza A virus; (B) Influenza B virus (C) Human Rhinovirus; (D) Human Metapneumovirus; (E) Human Adenovirus; (F) Mycoplasma pneumoniae; (G) Respiratory syncytial virus; (H) Human Parainfluenza virus; (I) Human Bocavirusx; (J) Human Coronavirus.
Defining an OR value > 1 as indicative of a higher risk of infection, no age range with OR > 1 was observed for IFV-A, MP, and HCoV in 2020–2022. In 2023, their age ranges with OR values > 1 were 6–46 years for IFV-A, 7–8 years for MP, and under 6 or over 26 years for HCoV. For IFV-B, HRV, HMPV, HAdV, HPIV, RSV, and HBoV, the age ranges with OR > 1 were as follows: in 2020–2022, 10–45 years, under 6 years, 3–5 years, under 7 years, under 3 years, under 7 years, and under 5 years or over 78 years, respectively; in 2023, 7–48 years, under 8 years, 1–7 years, under 8 years, under 7 years, under 7 years, and under 6 years or over 70 years, respectively. Compared to 2020–2022, the susceptible age ranges expanded for IFV-B, HRV, HMPV, HAdV, HPIV, and HBoV (with increases in the width of 6, 2, 4, 1, 4 and 9 years, respectively), while remaining unchanged for RSV.
Discussion
Since the onset of the COVID-19 pandemic, the deployment of NPIs globally has significantly decreased the incidence of most seasonal respiratory pathogens. In December 2022, China announced a complete relaxation of NPIs and the termination of the dynamic zero-COVID policy. The Jionpoint13 analysis was used to establish piecewise regression according to the time characteristics of patients with infection. The month was divided into different intervals through several connection points, and trend fitting and optimization were carried out for each interval to analyze the turning point of trend change.The data indicated that January 2023 marked a turning point in overall pathogen activity, which increased progressively month by month, from an average of 43.05% in 2020–2022 up to 68.46% in 2023, accompanied by an increase in the proportion of adolescents, adults, and the elderly, differing from the Infants and toddlers and Children-dominant infection pattern observed from 2020 to 2022.
During 2020–2022, the seasonal prevalence of IFV-A and IFV-B was abbreviated or even absent, with only brief, minor rebounds occurring, consistent with reports from other regions in China14. However, in 2023, IFV-A exhibited a typical bimodal activity pattern in spring and autumn-winter, with a nearly 30% positive rate in adults and adolescents. A similar double-peak pattern of influenza was observed in Northern China15, where the community infection rate was higher, possibly due to the colder and drier climate favoring the transmission of IFV-A. Our results align with the pre-2020 IFV-A prevalence patterns in Eastern China16, suggesting that IFV-A may have regained its dominant position and typical seasonal characteristics in the region’s respiratory virus landscape, but has not returned to pre-pandemic levels. while IFV-B detection significantly increased in December. However, due to limited observation time, trends in IFV-B require ongoing surveillance.
The global incidence of MP was reduced from 8.61 to 1.69% in 2020 following the introduction of NPIs17. A 2023 study from Spain did not indicate an increase in the severity of MP infections18, yet concerns about MP outbreaks remain in other countries19. We observed a rapid rise in MP infections from April to June 2023, with a fluctuating positivity rate of 27.6-32.6% between July and October, exceeding the 25.4% reported in Beijing, China20. This aligns with pre-COVID-19 seasonal characteristics of MP in our region reported by Jiang Q21but with a higher positive rate in our study. The reasons behind this MP epidemic remain unclear but may be associated with the lifting of restrictions. Additionally, reports suggested that this MP epidemic was predominantly caused by macrolide-resistant MP (MRMP), accounting for over 90% of cases20. Infections with MRMP often present with more severe clinical symptoms, resulting in prolonged illness and increased treatment difficulty, highlighting the need for enhanced prevention measures against MP infections.
The transmission of HRV, HAdV, and HBoV has not changed significantly but continues to be detectably persistent. Notably, HRV maintained a high positivity rate without clear seasonality, similar to reports from South Korea22. This could be due to the lack of a viral envelope and HRV’s strong environmental stability. Additionally, rhinoviruses grow faster than other viruses and are less likely to be inactivated by alcohol-based disinfectants. RSV exhibited varying seasonal characteristics. In 2020 and 2022, it peaked during the winter, whereas in 2021, a late-summer peak was observed—a phenomenon also noted in Australia, Japan, and Shanghai, China23,24,25. However, in 2023, RSV showed a new seasonal pattern, starting to increase significantly in April and abruptly declining in October, and although the total positive rate of RSV in 2023 was lower than that in 2020–2022, the number of infections did not decrease. While the peak activity of IFV-A happened to be in March-April and October-December, RSV activity suddenly dropped with the rebound of influenza, and Kunming, China, also detected the same epidemic characteristics as ours26. Reports in 2016 from the Netherlands have noted interruptions in RSV peaks due to the IFV-A infections27. Additionally, HMPV displayed a seasonal pattern similar to RSV, whereas HPIV and HCoV showed atypical seasonal fluctuations.
Analysis of infection patterns by age group revealed that the pathogens with notable change varied across demographics in 2023. Infants and toddlers had a higher detection of HRV and RSV, particularly RSV, which was significantly higher than in other groups. However, as the number of other age groups increased, the proportion of infants and toddlers decreased significantly in 2023, which also contributed to the decrease in the overall positive rate of HRV and RSV.In children and adolescents, MP was most frequently detected. Children had a lower positive rate for IFV-A compared to adolescents but a higher rate for HRV. In adults and the elderly, IFV-A was most prevalent. Previous research had confirmed the higher susceptibility of Infants and toddlers to HRV, RSV, HAdV, and HPIV28,29,30, linked to their immature immune systems. The age pattern for MP also aligns with other reports31,32. IFV-A infection spaned all age groups and, in Chinese households, cohabitation of elderly individuals with their children and grandchildren may exacerbate the spread of influenza within domestic settings33,34, which in turn, may drive community transmission. Notably, infants and the elderly are at a higher risk of related complications35, highlighting the importance of enhancing transmission prevention measures across different social settings, including frequent handwashing, avoiding touching the face, wearing masks, and receiving flu vaccinations, all of which help reduce the risk of respiratory pathogen infections.
Comparing 2020–2022, the rate of co-infections rose from 4.25 to 13.73%. The proportion of co-infections involving HRV combined with HMPV/HAdV/RSV/HPIV decreased. With HRV, IFV-A, and MP combinations predominating, HRV was involved in over 50% of co-infection cases. J.Z et al36.found that the co-infection rate of respiratory pathogens in Shandong Province, China, decreased from 7.05% in 2019 to 4.69% in 2020–2021. A comparison of our data suggests that co-infections appeard to be more frequent after the full relaxation of NPIs. Analysis of interactions between pathogens showed mostly negative interactions with each other, particularly those involving IFV-A. Several studies conducted in the United States have indicated a competitive interaction between IFV-A and HRV37, with M.D. et al.‘s study38 further highlighting a potential rejection effect of most seasonal respiratory viruses. Therefore, the decrease in RSV and HRV transmission rates in 2023, may be associated with early outbreaks of IFV-A. Nonetheless, whether the severity of clinical symptoms associated with co-infections remains to be further studied.
Lastly, RCS models39was used to analyze this nonlinear regression model to evaluate the relationship between age and infection outcomes with different pathogens, dividing age into 5 intervals at 4 knots and applying a cubic polynomial analysis at each interval to fit the data points and producing a smooth curve. Comparing 2020–2022, 2023 data suggested an increase in infection risk for most pathogens within a certain range of susceptible ages and a widening age range of susceptibility for most pathogens. This means that when NPIs ended, more people became susceptible to these pathogens. Hu et al. and Jiang et al40. also reported that the age range of susceptible groups for RSV and MP increased respectively in 2023. The prevailing view for this change was partly related to long-term immune dysfunction41following the COVID-19 infection wave in early 2023. Other reports42also say this was a phenomenon of “immunity debt”, highlighting the broad-spectrum effectiveness of public measures.The implementation of NPIS was accompanied by inadequate immune system stimulation and reduced natural immunity levels, but there was no immediate and significant recovery in national immunization during the epidemic43. wang et al44. also confirmed that the influenza pandemic in South China, North China and the United States in 2022–2023 was caused by the increase in population susceptibility, and believed that viruses whose activity decreased significantly during the COVID-19 pandemic45also had the potential for large-scale outbreaks. Our study suggested while NPIs offer effective short-term solutions for controlling the spread of these pathogens, their long-term use has unintended consequences that can reduce the immunity of the population.
This study has limitations. First, being a single-center study may limit the generalizability of our results. Second, as a retrospective study that only included individuals tested for all pathogens, it may not represent all those seeking healthcare. Additionally, pathogen testing in this study began on January 24, 2020, which might not fully reflect the actual pathogen detection characteristics for that month. Lastly, while we reported only a limited number of pathogens, the prevalence of MP and IFV is currently significant; therefore, establishing a multicenter, prospective, and comprehensive pathogen surveillance system is necessary.
Conclusions
Following the complete relaxation of NPIs and the cessation of the dynamic zero-COVID policy. the prevalence of common respiratory pathogens exhibited a notable increase, particularly with regard to the outbreaks of IFV-A and MP. The transmission of RSV may have been prematurely interrupted by the IFV-A outbreaks, while the positive rate of MP has surpassed pre-COVID-19 pandemic levels. Additionally, there has been a significant rise in co-infections and a broadening of the age range of individuals susceptible to various pathogens. underscoring the need for ongoing monitoring of dynamic respiratory pathogens to assist healthcare providers in implementing targeted preventive measures.
Data availability
All key information data generated or analyzed during this study are included in this article.
References
Global burden of 369 diseases. and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019.
Narasimhan, H., Wu, Y., Goplen, N. P. & Sun, J. Immune determinants of chronic sequelae after respiratory viral infection. Sci. Immunol. 7, eabm7996. https://doi.org/10.1126/sciimmunol.abm7996 (2022).
Leung, N. H. L. Transmissibility and transmission of respiratory viruses. Nat. Rev. Microbiol. 19, 528–545. https://doi.org/10.1038/s41579-021-00535-6 (2021).
Padayachee, Y., Faiez, T. S., Singanayagam, A., Mallia, P. & Johnston, S. L. Asthma and viruses: a focus on rhinoviruses and SARS-CoV-2. J. Allergy Clin. Immunol. 147, 1648–1651. https://doi.org/10.1016/j.jaci.2021.03.011 (2021).
Ren, Y. et al. Development and validation of a nomogram for predicting Mycoplasma pneumoniae pneumonia in adults. Sci. Rep. 12, 21859. https://doi.org/10.1038/s41598-022-26565-5 (2022).
McElhaney, J. E. et al. The immune response to influenza in older humans: beyond immune senescence. Immun. Ageing: I a. 17. https://doi.org/10.1186/s12979-020-00181-1 (2020).
Mazur, N. I. et al. The respiratory syncytial virus vaccine landscape: lessons from the graveyard and promising candidates. Lancet Infect. Dis. 18, e295–e311. https://doi.org/10.1016/s1473-3099(18)30292-5 (2018).
Koh, H. K., Geller, A. C. & VanderWeele, T. J. Deaths from COVID-19. Jama. 325, 133–134. https://doi.org/10.1001/jama.2020.25381 (2021).
Amar, S., Avni, Y. S., O’Rourke, N. & Michael, T. Prevalence of common infectious diseases after COVID-19 Vaccination and Easing of Pandemic restrictions in Israel. JAMA Netw. Open. 5, e2146175. https://doi.org/10.1001/jamanetworkopen.2021.46175 (2022).
Singer, R. et al. The increase in invasive bacterial infections with respiratory transmission in Germany, 2022/2023. Deutsches Arzteblatt Int. 121, 114–120. https://doi.org/10.3238/arztebl.m2023.0261 (2024).
The Lancet Regional Health- & Western, P. The end of zero-COVID-19 policy is not the end of COVID-19 for China. Lancet Reg. Health West. Pac. 30, 100702. https://doi.org/10.1016/j.lanwpc.2023.100702 (2023).
Gong, C. et al. Increase of respiratory illnesses among children in Beijing, China, during the autumn and winter of 2023. Euro. Surveillance: Bull. Europeen sur les maladies Transmissibles = Eur. Commun. Disease Bull. 29. https://doi.org/10.2807/1560-7917.Es.2024.29.2.2300704 (2024).
Wang, X. et al. Unraveling the global burden of inflammatory bowel disease (1990–2019): a Joinpoint regression analysis of divergent trends in 10–24 and 50–69 age cohorts. Autoimmun. rev. 103586. https://doi.org/10.1016/j.autrev.2024.103586 (2024).
Liu, P. & Xu, J. Resurgence of influenza virus activity during COVID-19 pandemic in Shanghai, China. J. Infect. https://doi.org/10.1016/j.jinf.2022.09.025 (2022).
Li, Y. et al. Cocirculation and coinfection of multiple respiratory viruses during autumn and winter seasons of 2023 in Beijing, China: a retrospective study. J. Med. Virol. 96, e29602. https://doi.org/10.1002/jmv.29602 (2024).
Zhu, A. Q., Li, Z. J. & Zhang, H. J. Spatial timing of circulating seasonal influenza A and B viruses in China from 2014 to 2018. Sci. Rep. 13, 7149. https://doi.org/10.1038/s41598-023-33726-7 (2023).
Meyer Sauteur, P. M. & Beeton, M. L. Mycoplasma pneumoniae: gone forever? Lancet Microbe. 4, e763. https://doi.org/10.1016/s2666-5247(23)00182-9 (2023).
Urbieta, A. D. et al. Mycoplasma pneumoniae at the rise not only in China: Rapid increase of Mycoplasma pneumoniae cases also in Spain. Emerg. Microbes Infect. 2332680. https://doi.org/10.1080/22221751.2024.2332680 (2024).
Wreghitt, T. Mycoplasma pneumoniae: current outbreak. Epidemiol. Infect. 1–3. https://doi.org/10.1017/s0950268824000293 (2024).
Yan, C. et al. Current status of Mycoplasma pneumoniae infection in China. World J. Pediatrics: WJP. https://doi.org/10.1007/s12519-023-00783-x (2024).
Jiang, Q., Yang, F., Peng, Y., Dong, X. & Ge, Y. Epidemiology and molecular identification of mycoplasma pneumoniae associated with respiratory infections in Zhejiang Province, China, 2008–2017. J. Clin. Lab. Anal. 34, e23460. https://doi.org/10.1002/jcla.23460 (2020).
Kim, H. M. et al. Impact of coronavirus disease 2019 on respiratory surveillance and explanation of high detection rate of human rhinovirus during the pandemic in the Republic of Korea. Influenza Other Respir. Viruses. 15, 721–731. https://doi.org/10.1111/irv.12894 (2021).
Saravanos, G. L. et al. RSV epidemiology in Australia before and during COVID-19. Pediatrics. 149. https://doi.org/10.1542/peds.2021-053537 (2022).
Jia, R. et al. Resurgence of respiratory syncytial virus infection during COVID-19 pandemic among children in Shanghai, China. Front. Microbiol. 13, 938372. https://doi.org/10.3389/fmicb.2022.938372 (2022).
Ujiie, M., Tsuzuki, S., Nakamoto, T. & Iwamoto, N. Resurgence of respiratory Syncytial Virus infections during COVID-19 pandemic, Tokyo, Japan. Emerg. Infect. Dis. 27, 2969–2970. https://doi.org/10.3201/eid2711.211565 (2021).
Zhang, G. et al. Epidemiological changes in respiratory pathogen transmission among children with acute respiratory infections during the COVID-19 pandemic in Kunming, China. BMC Infect. Dis. 24, 826. https://doi.org/10.1186/s12879-024-09733-y (2024).
van Asten, L. et al. Early occurrence of influenza A epidemics coincided with changes in occurrence of other respiratory virus infections. Influenza Other Respir. Viruses. 10, 14–26. https://doi.org/10.1111/irv.12348 (2016).
Kieninger, E., Fuchs, O., Latzin, P., Frey, U. & Regamey, N. Rhinovirus infections in infancy and early childhood. Eur. Respir. J. 41, 443–452. https://doi.org/10.1183/09031936.00203511 (2013).
Billard, M. N. & Bont, L. RSV immunisation: lessons from the COVID-19 pandemic. Lancet Child. Adolesc. Health. 7, 147–149. https://doi.org/10.1016/S2352-4642(22)00377-7 (2023).
Li, L., Jia, R., Zhang, Y., Sun, H. & Ma, J. Changes of parainfluenza virus infection in children before and after the COVID-19 pandemic in Henan, China. J. Infect. https://doi.org/10.1016/j.jinf.2023.02.009 (2023).
Lee, K. L. et al. Severe Mycoplasma pneumoniae pneumonia requiring intensive care in children, 2010–2019. J. Formos. Med. Association = Taiwan. Yi Zhi. 120, 281–291. https://doi.org/10.1016/j.jfma.2020.08.018 (2021).
Lee, E. et al. Annual and seasonal patterns in etiologies of pediatric community-acquired pneumonia due to respiratory viruses and Mycoplasma pneumoniae requiring hospitalization in South Korea. BMC Infect. Dis. 20, 132. https://doi.org/10.1186/s12879-020-4810-9 (2020).
Iyengar, P. et al. Case-ascertained study of household transmission of seasonal influenza - South Africa, 2013. J. Infect. 71, 578–586. https://doi.org/10.1016/j.jinf.2015.09.001 (2015).
Emanuels, A. et al. Remote Household Observation for Noninfluenza respiratory viral illness. Clin. Infect. Diseases: Official Publication Infect. Dis. Soc. Am. 73, e4411–e4418. https://doi.org/10.1093/cid/ciaa1719 (2021).
Thomas, C. M. et al. Early and increased influenza activity among Children - Tennessee, 2022-23 influenza season. MMWR Morb. Mortal. Wkly Rep. 72, 49–54. https://doi.org/10.15585/mmwr.mm7203a1 (2023).
Zhang, J., Yang, T., Zou, M., Wang, L. & Sai, L. The epidemiological features of respiratory tract infection using the multiplex panels detection during COVID-19 pandemic in Shandong province, China. Sci. Rep. 13, 6319. https://doi.org/10.1038/s41598-023-33627-9 (2023).
Nickbakhsh, S. et al. Virus-virus interactions impact the population dynamics of influenza and the common cold. Proc. Natl. Acad. Sci. U.S.A. 116, 27142–27150. https://doi.org/10.1073/pnas.1911083116 (2019).
Weidmann, M. D., Green, D. A., Berry, G. J. & Wu, F. Assessing respiratory viral exclusion and affinity interactions through co-infection incidence in a pediatric population during the 2022 resurgence of influenza and RSV. Front. Cell. Infect. Microbiol. 13, 1208235. https://doi.org/10.3389/fcimb.2023.1208235 (2023).
Gauthier, J., Wu, Q. V. & Gooley, T. A. Cubic splines to model relationships between continuous variables and outcomes: a guide for clinicians. Bone Marrow Transplant. 55, 675–680. https://doi.org/10.1038/s41409-019-0679-x (2020).
Jiang, M. et al. Influence of non-pharmaceutical interventions on epidemiological characteristics of Mycoplasma pneumoniae infection in children during and after the COVID-19 epidemic in Ningbo, China. Front. Microbiol. 15, 1405710. https://doi.org/10.3389/fmicb.2024.1405710 (2024).
Phetsouphanh, C. et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat. Immunol. 23, 210–216. https://doi.org/10.1038/s41590-021-01113-x (2022).
Zhu, W. & Gu, L. Resurgence of seasonal influenza driven by A/H3N2 and B/Victoria in succession during the 2023–2024 season in Beijing showing increased population susceptibility. J. Med. Virol. 96, e29751. https://doi.org/10.1002/jmv.29751 (2024).
Li, K. et al. Temporal shifts in 24 notifiable infectious diseases in China before and during the COVID-19 pandemic. Nat. Commun. 15, 3891. https://doi.org/10.1038/s41467-024-48201-8 (2024).
Wang, Q. et al. Increased population susceptibility to seasonal influenza during the COVID-19 pandemic in China and the United States. J. Med. Virol. 95, e29186. https://doi.org/10.1002/jmv.29186 (2023).
Chow, E. J., Uyeki, T. M. & Chu, H. Y. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat. Rev. Microbiol. 21, 195–210. https://doi.org/10.1038/s41579-022-00807-9 (2023).
Acknowledgements
Thanks to all my colleagues in the laboratory.
Funding
This study was supported by grants from Medical and Health Research Project of Zhejiang Province (Grant No.2021KY304).
Author information
Authors and Affiliations
Contributions
Q.S. and M.J. drafted the initial manuscript and contributed to manuscript editing. Z. L. and M.J. collected the data from patients. Y.T. contributed to manuscript editing. Y.T. and Q. L. devised the conceptual ideas and contributed to the discussion and interpretation of the results. All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional Review Board Statement
This study was conducted following the principles of the Helsinki Declaration and obtained approval from the Ethics Committee of Li Huili Hospital, Ningbo City (Approval No.KY2024SL070-01).
Informed consent
The Patient informed consent was waived which is approved by ‘the Ethics Committee of Li Huili Hospital, Ningbo City’ due to the retrospective electronic medical information system.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, Q., Liu, Z., Jiang, M. et al. The circulating characteristics of common respiratory pathogens in Ningbo, China, both before and following the cessation of COVID-19 containment measures. Sci Rep 14, 25876 (2024). https://doi.org/10.1038/s41598-024-77456-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-77456-w
This article is cited by
-
Epidemiology and clinical characteristics of human rhinovirus in hospitalized children and adolescents with acute respiratory infections: a longitudinal study in Shenzhen, China (2019–2024)
Virology Journal (2025)
-
Human parainfluenza virus: an important but overlooked respiratory pathogen
World Journal of Pediatrics (2025)
-
Interpretation of pathogenicity and clinical features of multiple pathogens in pediatric lower respiratory tract infections by tNGS RPTM analysis
European Journal of Clinical Microbiology & Infectious Diseases (2025)
-
Epidemiological analysis of pediatric respiratory pathogens in Hunan, China: a retrospective multicenter study from 2022 to 2024
BMC Infectious Diseases (2025)