Abstract
The study aimed to compare the effectiveness between Hiporfin-photodynamic therapy (PDT) and loop electrosurgical excision procedure (LEEP) in treating cervical high-grade squamous intraepithelial lesion (HSIL). We conducted a retrospective analysis of 104 women diagnosed with cervical HSIL at our hospital from April 2019 to July 2023. With 1:1 matched case-control, 52 cases received Hiporfin-PDT and 52 cases underwent LEEP. All PDT-treated cases received Hiporfin (2 mg/kg) I.V. and a diode laser at a wavelength of 630-nm. T-test, Chi-square test, Fisher’s exact test, and Yates’s correction for continuity were conducted for statistical. A P value < 0.05 was considered significant. The complete response (CR) post-PDT at 3rd-6th months,10th-12th months and 24th months was in 98.1% (51/52),100.0% (45/45) and 100.0% (22/22) patients respectively, compared to 98.1% (51/52), 100.0% (46/46) and 100.0% (24/24) patients respectively after LEEP. HPV clearance rates after PDT at 3rd-6th months,10th-12th months and 24th months was 76.9% (40/52), 88.9% (40/45) and 95.5% (21/22) respectively, compared to 69.2% (36/52), 93.5% (43/46) and 95.8% (23/24) respectively after LEEP, with no significant difference between the two groups (P = 0.508, P = 0.687 and P = 1.000, respectively). Postoperative complications in the PDT group were tolerable. The cure rates and HPV eradication of Hiporfin-PDT were comparable with that of LEEP in the management of cervical HSIL. Hiporfin-PDT may serve an alternative method for organ-saving in cervical HSIL.
Similar content being viewed by others
Cervical cancer is the sixth most common cancer in Chinese women, with approximately 110,000 new cases and 59,000 deaths occurring annually in China1. According to the 5th Edition of the World Health Organization (WHO) Classification of Female Genital Tract Tumors, cervical squamous intraepithelial lesions are categorized into two levels: low-grade squamous intraepithelial lesion (LSIL), which includes cervical intraepithelial neoplasia (CIN) I, and high-grade squamous intraepithelial lesion (HSIL), which encompasses CIN II and CIN III2. HPV is a significant factor in the development of cervical carcinoma, detected in about 70% of CIN cases3. HSIL known as cervical intraepithelial neoplasia is a pre-malignant state, without appropriate intervention, might progress to cervical cancer4,5,6. In recent years, the age of initial sexual activity is getting lower and the incidence of HSIL is increasing each year particularly in young women7,8,9.
Current treatment options for HSIL include LEEP, cold-knife coning (CKC), cryosurgery, laser surgery and thermocoagulation, etc., all of which are non-selective tissue removal treatments10. Despite positive effect on HSIL regression with LEEP, several severe side effects such as hemorrhages, cervical canal stenosis, scarring of the cervix and post-treatment infertility, early miscarriage and premature delivery, etc., which are unacceptable for patients willing to conceive later in the course of their life11. Thus, there is a pressing need within the global medical community to explore alternative treatments that minimize the impact on fertility.
PDT as a modern, highly selective and non-invasive procedure is based on the systemic or topical application of photosensitizers, that selectively accumulate in pathologic tissues and induce cellular oxidative stress through generation of reactive oxygen species by irradiation at a specific wavelength12. This effect can directly destroy tumor cells and indirectly cause ischemia and hypoxia in the tumor tissue by disrupting the tumor microvasculature. It also stimulates the host immune system. However, the base structure is not affected13,14. Thus, PDT has the effect of organ-saving. PDT is successfully employed in various medical fields and has shown promise in the treatment of CIN and cervical cancer15.
Hiporfin, the only one of hematoporphyrin derivatives (HpD) going through formal clinical trials and approved for oncological indications by Chinese State Food and Drug Administration (SFDA), has demonstrated efficacy in treating both precancerous lesions and cancers16,17,18,19,20,21. Due to the increasing incidence of cervical HSIL among younger women, there is a growing clinical demand for PDT. In comparison to surgical options like LEEP, an increasing number of patients are opting for conservative treatments to preserve the structural integrity of the cervix. Nevertheless, there is a lack of research comparing Hiporfin-PDT with LEEP in patients with cervical HSIL. Our study, therefore, seeks to address this gap by evaluating the clinical efficacy of Hiporfin-PDT as a novel treatment for cervical HSIL and comparing its effectiveness with that of LEEP.
Materials and methods
Study design
Our hospital granted approval to initiate photodynamic therapy (PDT) as a novel technology project for treating gynecological tumors from April 2019 with ethical approval (XJS20190004). All methods were performed in accordance with relevant guidelines and regulations. This retrospective analysis included 104 patients with morphologically proven diagnosis of CINII and III from April 2019 to July 2023. The number of patients in the group that implemented PDT and LEEP was the same, 52 in each group. Written informed consent was obtained from all participants, providing comprehensive details about the main objectives of the study, treatment protocol, and potential complications. Patients who desired organ preservation were assigned to the PDT group. Each PDT case was matched with a control patient from the LEEP group with the same age group (Every 5-year-old represents an age group. For example, 21–25 years old, 26–30 years old, and so on.), the same lesion degree (CINII/CINIII), and the closest diagnosis time (an interval of less than 3 months).
The inclusion criteria were as follows: cervical HSIL. The exclusion criteria were as follows: concurrent vaginal and/or vulvar HSIL, a history of cervical HSIL surgery, or suspected invasive carcinoma of cervix; an allergy to Hiporfin or known porphyria (the PDT group); menstruation, pregnancy or lactation; significant abnormal liver function, coagulation dysfunction, serious uncontrolled medical complications, acute inflammatory period, active of general infectious disease; high-dose usage of antithrombotic or antiplatelet agglutination drugs.
Initial clinical examination before treatment involved bacteriological analysis of vaginal and cervical secretions, HPV testing (Cobas 4800), liquid-based cytology (AutoCyte thin-layer cytology test), colposcopy, pathological examination of cervical biopsy samples, blood routine examination, coagulation function, hepatorenal function tests, human chorionic gonadotropin (HCG) detection, electrocardiogram. Colposcopy was performed by experienced colposcopists.
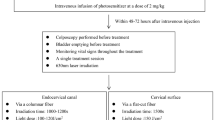
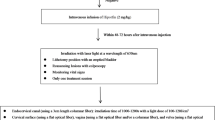
Photodynamic therapy
In all 52 patients of PDT group, a photosensitizer (Hiporfin; Chongqing Milelonge Biopharmaceutical Co., Ltd, China) was injected intravenously at a dose of 2 mg/kg in a room blocked by uv light after hospitalization. Illumination with red laser light at a wave length of 630 nm (PDT630 semiconductor laser treatment machine: Shenzhen Laser Medical Technology Co., Ltd, China) was applied to the surface of uterine cervix and the endocervical canal 48–72 h after injection of the photosensitizer. Two types of optical fiber were utilized: flat cut fiber and columnar fiber (Shenzhen Laser Medical Technology Co., Ltd, China).
Bladder emptying before treatment. PDT was administered with the patient in the lithotomy position and vital signs were monitored throughout. Colposcopy was conducted before treatment to determine the location and size of lesions with the application of acetic acid. Treatment session was only once. Laser light was applied via a columnar fiber inserted in the endocervical canal with an irradiation time of 1000–1200 s and a light dose of 100–120 J/cm2. Flat cut fiber was positioned and irradiated at the surface of the cervix with an irradiation time of 1500s and a light dose of 150 J/cm2. The size and number of irradiation fields were determined by the extent of the pathologic lesions. For HSIL lesions not exceeding 4 cm in diameter, a single irradiation field was used, overlapping the lesion by at least 5 mm at the edges. If the lesion spanned more than 4 cm in any direction, two or three irradiation fields of 4 cm diameter each were used, ensuring overlap between fields to prevent missed lesions and inadequate treatment (Figs. 1 and 2).
After PDT, patients were advised to protect their skin and eyes from light exposure, particularly sunlight, for approximately 4–6 weeks due to the photosensitizer’s potential to cause light sensitivity. This precaution aimed to prevent systemic side effects. However, patients’ daily life such as using telephone or computer was not affected. Patients were asked to use contraception until the results of the 3rd to 6th-month follow-up were obtained.
Loop electrosurgical excision procedure
LEEP procedures were conducted under local anesthesia in the outpatient operating room. Patients assumed the position necessary for bladder lithotomy. Prior to treatment, a colposcopic evaluation was carried out. Following the administration of local anesthesia, the cervix was fully exposed, and acetic acid was applied to delineate the lesion area. A LEEP knife was then utilized to execute a cone-shaped resection, starting 5 mm outside the lesion boundary, with a resection depth according to the type of cervical transformation zone. To immediately halt bleeding, the wound surface was electrocoagulated. In cases where the lesion was extensive, additional cuts were made in stages. Post-operatively, the excised specimens were labeled and sent for pathological examination.
Follow-up and statistical analysis
The efficacy of PDT was assessed by gynecological examinations at 3rd-6th and 10th-12th months after treatment, and annually thereafter. We used WeChat to contact the patients for follow-up at the scheduled time, and all patients demonstrated good compliance. The evaluations included clinical examination, HPV testing, liquid-based cytology testing; colposcopy; cervical biopsy. Currently, there are no definitive criteria for remission in PDT. The final assessment of the PDT efficacy was based on postoperative cytology, colposcopy and morphological findings, irrespective of HPV infection status. The criteria used were as follows: complete response (CR) (cytology, colposcopy and cervical biopsy pathology indicated no high-grade lesions); stabilization (residual HSIL); progression (cervical biopsy pathology confirmed invasive carcinoma).
The final assessment of LEEP efficacy was based on postoperative cytology, HPV test, and colposcopy pathological findings. The follow-up time was determined according to the pathology of the LEEP surgical margins. If the margins were negative, combined cytology and HPV testing were conducted at 6th months postoperatively. If the cytology indicated atypical squamous cell of undetermined significance (ASCUS) or a higher-grade lesion and/or HPV positivity, colposcopy and cervical biopsy were performed. In cases where the surgical margin was positive for HSIL, combined cytology and HPV testing were done at 3rd-6th months postoperatively. If the cytology indicated ASCUS or a higher-grade lesion and/or HPV positive, colposcopy and cervical biopsy were performed.
A cure for cervical HSIL by LEEP was defined by any of the following: negative LEEP surgical margin pathology, with negative cytology and HPV testing at 6th months postoperatively; HSIL confirmed at the surgical margin but negative cytology and HPV testing at 3rd-6th months postoperatively; HSIL confirmed at the surgical margin with positive HPV testing at 3rd-6th months postoperatively, but cytology, colposcopy, and histopathological examination showed no high-grade lesions.
Treatment-related side effects including vaginal hemorrhage, infection, pelvic pain, vaginal discharge and photosensitivity was evaluated in accordance with Common Terminology Criteria for Adverse Events (CTCAE) Ver. 5.0.
All statistical analyses were performed using SPSS 27.0 software. The t-test, Chi-square test, Yates’s correction for continuity, and Fisher’s exact test were employed for the analyses. The follow-up period and age between the two groups were compared using a t-test. Categorical data were compared using the Chi-square test, Yates’s correction for continuity, or Fisher’s exact test, as appropriate. Specifically, the Chi-square test was used when the total sample size of the two groups was n ≥ 40 and the expected count of all cells (theoretical number, T) was ≥ 5. Yates’s correction for continuity was applied when n ≥ 40 but 1 ≤ T ≤ 5. Fisher’s exact test was used when n < 40 or T < 1. A P-value of less than 0.05 was considered statistically significant.
Results
Characteristics of patients
The average age of patients was comparable between the PDT and LEEP groups, at 30.8 ± 8.1 years (range, 21–69 years) and 31.8 ± 7.1 years (range, 23–67 years), respectively (P = 0.48). The follow-up periods were also similar, with the PDT group at 25.4 ± 14.9 months (range, 7–58 months) and the LEEP group at 29 ± 14.7 months (range, 7–57 months) (P = 0.182). Pre-treatment, infection rates of HPV were all 100% in both groups. Before treatment, there were no significant statistical differences in HPV substyle and cytological examination of cervical smears between the two groups (P = 0.192 and P = 0.21, respectively). Meanwhile, the incidence of CIN II and CIN III was identical in both groups, with 32 cases of CIN II and 20 cases of CIN III, respectively. The rates of cervical gland involvement and endocervix involvement all showed no statistical difference between two groups (P = 1.000 for both) (Table 1).
In the PDT group, 45 patients completed their follow-up at 10th-12th months, and 22 patients at 24 months. The incomplete follow-up for some patients was due to the follow-up period not yet being reached, rather than loss to follow-up. HPV eradication rate in the PDT group was 76.9% (40/52), 88.9% (40/45) and 95.5% (21/22) at 3rd-6th months,10th-12th months and 24th months respectively. Patients with persistent HPV showed no HSIL recurrences during the long-time follow-up period. Before treatment, cervical smear test greater than or equal to ASCUS was 73.1% (38/52) and negative conversion rate of cytology was 89.5% (34/38), 97.0% (32/33) and 100.0% (22/22) at 3rd-6th months, 10th-12th months and 24th months respectively. The CR rate of HSIL in the PDT group was 98.1% (51/52),100.0% (45/45) and 100.0% (22/22) respectively at 3rd-6th months,10th-12th months and 24th months. One patient with a residual lesion at the 3rd-6th month follow-up declined further surgical intervention and the lesion resolved by the 10th-12th months. Post-treatment colposcopy revealed lesion site removal (Fig. 3). All cervical canal lesions were completely resolved. The negative conversion rate of cervical gland involvement was 100.0% (25/25).
Colposcopic images showing application of PDT in the cervix. CINIIwith cervical gland involvement in the cervix before PDT, showing lesion site at both cervical surface and cervical canal with acetowhitening (A); 3 months after PDT, showing residual lesion site at 6 o’clock of cervical surface with acetowhitening (C); 6 months after PDT, showing residual lesion site still at 6 o’clock of cervical surface with acetowhitening (C); 12 months after PDT, there was no evidence of HSIL lesions with acetowhitening (D).
In the LEEP group, 6 patients had positive resection margins. 46 patients completed their follow-up at 10th-12th months and 24 patients at 24 months. HPV eradication rate was 69.2% (36/52), 93.5% (43/46) and 95.8% (23/24) at 3rd-6th months,10th-12th months and 24th months respectively. Pre-treatment, cervical smears greater than or equal to ASCUS was 61.5% (32/52) and negative conversion rate of cytology was 75.0% (24/32), 100.0% (27/27) and 100.0% (24/24) respectively at 3rd-6th months,10th-12th months and 24th months. The CR rates were 98.1% (51/52) at 3rd-6th months, 100.0% (46/46) at 10th-12th months, and 100.0% (24/24) at 24 months. One LEEP patient of group with residual lesions at the 3rd-6th month follow-up underwent a hysterectomy.
There was no statistical difference between the two groups in terms of HPV substyle eradication rate, HPV infection clearance, negative conversion rate of cytology or cure rate between two groups (Table 2; Fig. 4).
Post-PDT, all patients’ cervixes appeared normal and their menstrual cycles remained unchanged after PDT. During the long-term follow-up period, eight patients who were actively trying to conceive successfully achieved pregnancies, including one spontaneous abortion, 4 term pregnancies, and 3 ongoing pregnancies. Three women delivered vaginally and one delivered by C-section at term. No fetal loss occurred due to cervical incompetence. Two cases of ongoing pregnancy have reached their second trimester, and one case has reached the third trimester. Prenatal examination showed no abnormality. Children have no important abnormalities in their physical growth.
Adverse effects
The procedure was tolerable in the PDT group. There were no serious adverse effects in 52 patients during and after PDT. No vaginal hemorrhage or infection occurred in all treated women. Additionally, there was no effect on sexual life after PDT. Several patients noted mild (grade 1) pelvic pain and vaginal discharge within the first 10 days post-illumination without need for intervention. Mild photosensitivity, characterized by slight edema and a burning sensation on sun-exposed skin was observed in a few patients, likely due to insufficient sun protection education. After guidance, the allergic symptoms improved within 5–7 days after treating with oral loratadine and ice.
In the LEEP group, some women reported mild (grade1) pelvic pain and vaginal discharge, which also did not necessitate treatment. Vaginal hemorrhage (grade 2) occurred in 5.8% (3/52) by packing hemostasis with gauze compression.
Discussion
Our study has demonstrated that PDT with Hiporfin presents an effective and promising therapeutic option with comparable results to LEEP for patients with cervical HSIL since its simplicity of the procedure, a low risk of severe systemic complications, organ-saving as well as its high therapeutic efficacy. No new disease development or recurrence during the median follow-up of 25.4 months. Given the higher sensitivity of HPV testing for CINII–III detection relative to colposcopy or cytology22,23, regular post-treatment HPV testing is crucial for the early identification of persistent or recurrent CINII–III23,24. The HPV eradication rate at 10th-12th months after PDT was 88.9%, showing no statistical difference compared to the LEEP group. Patients with persistent HPV had no HSIL recurrences during the long follow-up period. These results indicate that the PDT has the great therapeutic potential in HPV-positive precancerous diseases. The results of anti-viral efficacy demonstrate its effectiveness in preventing disease relapse. There was no occurrence of serious complications compared to LEEP. As such, PDT, as a treatment for cervical HSIL, does not lag behind the existing methods in terms of therapeutic effectiveness and minimizes the destruction of the cervical stroma.
In recent years, there has been a notable increase in uterine cervical neoplasia among young women. In the childbearing age group, oncologists face challenges about necessity for both high cervical neoplasia cure rate and fertility protection25,26. PDT is an alternative organ-saving therapeutic approach in the treatment of oncological diseases without damaging the cervical stroma. It is based on the combination of the selective accumulation of a photosensitizer in cells with fast metabolic speed and specific damaging action of the laser light targeting pre-malignant or malignant tissue. This photodynamic reaction is characterized by the photochemical generation of singlet oxygen, leading to both cellular and vascular necrosis27. PDT with multifactorial mechanisms makes many advantages; less invasive, sparing organ function, enhancing quality of life, high selectivity to tumor sites, being compatible with other therapeutic or adjuvant therapy and repeatability, etc13,14,28.
Photosensitizers including systemic and topical application of photosensitizers are critical for PDT. A pivotal issue regarding PDT with topical application of photosensitizer such as 5-aminolaevulinic acid (5-ALA) for CIN is the maximum depth of necrosis caused by this method. In skin tumors, the maximum depth of necrosis by PDT is 1.3 mm29. If the maximum depth of necrosis is 1.0–1.3 mm, as seen in tumors of the oral cavity and the gastrointestinal tract after 5-ALA PDT, we conclude that PDT with 5-ALA remains too superficial to reach all of the CIN lesions. Moreover, the limited success of PDT in the treatment of CIN may be due to inadequate treatment of the cervical canal because of locally applied topical forms of photosensitizers30. However, more promising results were achieved by systemic administration of photosensitizers for the CIN treatment by PDT. Muroya et al.31reported that they have performed PDT with Photofrin on 131 cases (31 cervical dysplasia, 1 vulva dysplasia, 95 cervical carcinoma in situ (CIS), 3 squamous cell carcinomas, microinvasion, and 1 CIS + endocervical adenocarcinoma, microinvasion). Of these cases, 127 became CR (127/131, 96.9%). The first CR case was 10 years ago and no recurrence has been observed yet. According to In Istomin’s results30, CR was in 23/24 (95.83%) patients with CIN2 and in 81/88 (92.05%) patients with CIN3 after PDT with Photolon. Lee et al.32 found that 26 young patients with CIN (4 CIN1, 1 CIN2 and 21 CIN3) were treated via PDT with Photogem, resulting in a 92.3% cure rate for CIN and an 83.3% HPV eradication rate. In the patients treated via LEEP (1 CIN1, 6 CIN2 and 19 CIN3), cure rate was 96.0% and HPV eradication rate was 81%. They concluded that the cure rates and eradication of HPV infection of PDT were comparable with that of LEEP therapy in the management of CIN. Similarly, in our research, 52 patients with cervical HSIL (32 CIN2, 20 CIN3) were treated with Hiporfin-PDT, CR was 100.0% and the HPV eradication rate was 95.5% at 10th-12th months. In the patients treated via LEEP (32 CIN2, 20 CIN3), CR was 100.0% and the HPV eradication rate was 95.8% at 10th-12th months. The CR and clearance rate of HPV infection of Hiporfin-PDT were comparable to that of LEEP in the management of cervical HSIL. No recurrence of cervical HSIL was observed at 24th months after Hiporfin-PDT. A longer follow-up period is necessary to confirm the durability of Hiporfin-PDT.
Creasman and Di Saia33 reported that the surgical treatment including electrocautery, cold-knife excision, freezing and laser ablation achieved high success rates between 90% and 98%. Baser et al. reported 21.2% high-risk HPV persistence 12 months after cold-knife conization on 113 women in Turkey34. Among 358 women in China, HR-HPV persistence was 24.3% 3-months after LEEP35. Our results were comparable with the above reports. Therefore, Hiporfin-PDT may be an alternative treatment for cervical HSIL in clinic.
LEEP result in substantial cervical stroma destruction, posing a risk of potential cervical incompetence. However, PDT does not harm the base structure of cervix and preserves cervical integrity. In our research, there were no instances of fetal loss due to cervical incompetence. Screening tests for cervical cancer, including HPV and cytological examinations, were all normal before and after pregnancy. No PDT-related complications were reported during pregnancy and delivery, and children show no significant abnormalities in their physical growth36. For the young age group, PDT serves as a conservative therapeutic option for fertility preservation, offering hope, especially when HSIL involves the cervical canal.
For patients with a body weight of 50 kg, the cost of once treatment session with Hiporfin-PDT is approximately 15,000RMB. The cost of Hiporfin-PDT is slightly higher than that of LEEP. As a result of the positive effects of Hiporfin-PDT, such as a high cure rate, preservation of organ integrity, and the absence of serious adverse reactions, an increasing number of patients are choosing to invest in this treatment instead of opting for LEEP. Meanwhile, many hospitals in China utilize Hiporfin-PDT to treat various precancerous and cancerous conditions, including Paget’s disease, precancerous lesions of the lower genital tract, basal cell carcinoma, advanced obstructive esophageal cancer, malignant airway tumors, gastric cancer, unresectable hilar cholangiocarcinoma, and others16,17,18,36,37,38,39,−40. We anticipate that the price of photosensitizers can be reduced to benefit more patients.
This study stands out as one of the first reports in English literature comparing the application of PDT with LEEP for treating cervical HSIL, with a focus on fertility preservation and organ conservation. However, it had the following limitations, including a single-arm trial design, a small sample size, and a relatively young average age of patients. In the future we need to conduct multi-center studies with larger sample sizes. Additionally, patients of older age, those with concurrent vaginal and/or vulvar HSIL, and individuals with a history of cervical HSIL surgery will be included to demonstrate the efficacy of Hiporfin-PDT, aiming to benefit a broader range of patients. We also expect that PDT can be performed without any hospitalization and less side effects using new photosensitizers.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Sung, H. et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. https://doi.org/10.3322/caac.21660 (2021).
Cree, I. A., White, V. A., Indave, B. I. & Lokuhetty, D. Revising the WHO classification: female genital tract tumours. Histopathology 76, 151–156. https://doi.org/10.1111/his.13977 (2020).
Tsuda, H. et al. Relationship between HPV typing and abnormality of G1 cell cycle regulators in cervical neoplasm. Gynecol. Oncol. 91, 476–485. https://doi.org/10.1016/j.ygyno.2003.08.019 (2003).
Gustafsson, L. & Adami, H. O. Natural history of cervical neoplasia: consistent results obtained by an identification technique. Br. J. Cancer 60, 132–141. https://doi.org/10.1038/bjc.1989.236 (1989).
Peto, J., Gilham, C., Fletcher, O. & Matthews, F. E. The cervical cancer epidemic that screening has prevented in the UK. Lancet 364, 249–256. https://doi.org/10.1016/s0140-6736(04)16674-9 (2004).
Tainio, K. et al. Clinical course of untreated cervical intraepithelial neoplasia grade 2 under active surveillance: systematic review and meta-analysis. Bmj 360, k499. https://doi.org/10.1136/bmj.k499 (2018).
Xavier-Júnior, J. C., Dufloth, R. M., Vale, D. B., Lima, M. T. & Zeferino, L. C. Early age at First Sexual Intercourse is Associated with higher prevalence of high-grade squamous intraepithelial lesions (HSIL). Rev. Bras. Ginecol. Obstet. 39, 80–85. https://doi.org/10.1055/s-0036-1597973 (2017).
Reissing, E. D., Andruff, H. L. & Wentland, J. J. Looking back: the experience of first sexual intercourse and current sexual adjustment in young heterosexual adults. J. Sex. Res. 49, 27–35. https://doi.org/10.1080/00224499.2010.538951 (2012).
Sýkorová, K. & Flegr, J. Faster life history strategy manifests itself by lower age at menarche, higher sexual desire, and earlier reproduction in people with worse health. Sci. Rep. 11, 11254. https://doi.org/10.1038/s41598-021-90579-8 (2021).
in WHO Guidelines for Treatment of Cervical Intraepithelial Neoplasia 2–3 and Adenocarcinoma in situ: Cryotherapy, Large Loop Excision of the Transformation Zone, and Cold Knife Conization (World Health Organization Copyright © World Health Organization 2014). (2014).
Rema, P. et al. Effectiveness and safety of loop electrosurgical excision procedure in a low-resource setting. Int. J. Gynaecol. Obstet. 103, 105–110. https://doi.org/10.1016/j.ijgo.2008.06.020 (2008).
Rogers, L., Sergeeva, N. N., Paszko, E., Vaz, G. M. & Senge, M. O. Lead structures for applications in photodynamic therapy. 6. Temoporfin Anti-inflammatory conjugates to target the Tumor Microenvironment for in Vitro PDT. PLoS One 10, e0125372. https://doi.org/10.1371/journal.pone.0125372 (2015).
Brown, S. B., Brown, E. A. & Walker, I. The present and future role of photodynamic therapy in cancer treatment. Lancet Oncol. 5, 497–508. https://doi.org/10.1016/s1470-2045(04)01529-3 (2004).
Huang, Z. A review of progress in clinical photodynamic therapy. Technol. Cancer Res. Treat. 4, 283–293. https://doi.org/10.1177/153303460500400308 (2005).
Dolmans, D. E., Fukumura, D. & Jain, R. K. Photodynamic therapy for cancer. Nat. Rev. Cancer 3, 380–387. https://doi.org/10.1038/nrc1071 (2003).
Zeng, R. et al. Clinical efficacy of HiPorfin Photodynamic Therapy for Advanced Obstructive Esophageal Cancer. Technol. Cancer Res. Treat. 19, 1533033820930335. https://doi.org/10.1177/1533033820930335 (2020).
Liao, C., Shi, L., Wang, D. & Wang, X. Bimodal photodynamic therapy for treatment of a 91-year-old patient with locally advanced cutaneous basal cell carcinoma and postoperative scar management. Photodiagnosis Photodyn Ther. 36, 102553. https://doi.org/10.1016/j.pdpdt.2021.102553 (2021).
Li, L. et al. Treatment of perianal Paget’s disease using photodynamic therapy with assistance of fluorescence examination: case report. Lasers Med. Sci. 24, 981–984. https://doi.org/10.1007/s10103-009-0653-8 (2009).
Huang, Z. An update on the regulatory status of PDT photosensitizers in China. Photodiagnosis Photodyn Ther. 5, 285–287. https://doi.org/10.1016/j.pdpdt.2009.01.005 (2008).
Huang, Z. Photodynamic therapy in China: over 25 years of unique clinical experience part two-clinical experience. Photodiagnosis Photodyn Ther. 3, 71–84. https://doi.org/10.1016/j.pdpdt.2006.03.001 (2006).
Huang, Z. Photodynamic therapy in China: over 25 years of unique clinical experience Part one-history and domestic photosensitizers. Photodiagnosis Photodyn Ther. 3, 3–10. https://doi.org/10.1016/s1572-1000(06)00009-3 (2006).
Costa, S. et al. Performance of HPV DNA testing in the follow-up after treatment of high-grade cervical lesions, adenocarcinoma in situ (AIS) and microinvasive carcinoma. Ecancermedicalscience 9, 528. https://doi.org/10.3332/ecancer.2015.528 (2015).
Cuschieri, K., Bhatia, R., Cruickshank, M., Hillemanns, P. & Arbyn, M. HPV testing in the context of post-treatment follow up (test of cure). J. Clin. Virol. 76 (Suppl 1), S56–s61. https://doi.org/10.1016/j.jcv.2015.10.008 (2016).
Nagai, Y., Maehama, T., Asato, T. & Kanazawa, K. Persistence of human papillomavirus infection after therapeutic conization for CIN 3: is it an alarm for disease recurrence? Gynecol. Oncol. 79, 294–299. https://doi.org/10.1006/gyno.2000.5952 (2000).
Hopper, C. Photodynamic therapy: a clinical reality in the treatment of cancer. Lancet Oncol. 1, 212–219. https://doi.org/10.1016/s1470-2045(00)00166-2 (2000).
Tao, X. H. et al. Efficacy and safety of photodynamic therapy for cervical intraepithelial neoplasia: a systemic review. Photodiagnosis Photodyn Ther. 11, 104–112. https://doi.org/10.1016/j.pdpdt.2014.02.012 (2014).
Godoy, H. et al. Photodynamic therapy effectively palliates gynecologic malignancies. Eur. J. Gynaecol. Oncol. 34, 300–302 (2013).
Allison, R. R. et al. PD/PDT for gynecological disease: a clinical review. Photodiagnosis Photodyn Ther. 2, 51–63. https://doi.org/10.1016/s1572-1000(05)00033-5 (2005).
Hillemanns, P. et al. Photodynamic therapy in women with cervical intraepithelial neoplasia using topically applied 5-aminolevulinic acid. Int. J. Cancer. 81, 34–38. (1999).
Istomin, Y. P., Lapzevich, T. P., Chalau, V. N., Shliakhtsin, S. V. & Trukhachova, T. V. Photodynamic therapy of cervical intraepithelial neoplasia grades II and III with Photolon. Photodiagnosis Photodyn Ther. 7, 144–151. https://doi.org/10.1016/j.pdpdt.2010.06.005 (2010).
Muroya, T. et al. Application of PDT for Uterine Cervical Cancer. Diagn. Ther. Endosc 5, 183–190. https://doi.org/10.1155/dte.5.183 (1999).
Chan Lee, J. K. & Jeong, C. H. Young Jeong Na, In Ho Kim, Sun Young Lee, Seung Jo Kim. Photodynamic therapy in the management of cervical intraepithelial neoplasia. Korean J Gynecol Oncol Colposc 15, 85–91, doi: https://doi.org/10.3802/kjgoc.2004.15.2.85 (2004).
Di Saia, P. J. C. W. Preinvasive disease of the cervix.Clinical gynecological oncology. 4th ed. St. Louis (MO): Mosby Year Book. 1–36 (1992).
Baser, E. et al. Risk factors for human papillomavirus persistence among women undergoing cold-knife conization for treatment of high-grade cervical intraepithelial neoplasia. Int. J. Gynaecol. Obstet. 125, 275–278. https://doi.org/10.1016/j.ijgo.2013.12.012 (2014).
Wu, J., Jia, Y., Luo, M. & Duan, Z. Analysis of Residual/Recurrent disease and its risk factors after Loop Electrosurgical Excision Procedure for High-Grade Cervical Intraepithelial Neoplasia. Gynecol. Obstet. Invest. 81, 296–301. https://doi.org/10.1159/000437423 (2016).
Liu, Y., Wu, R., Li, C., Wei, L. & Li, R. Successful pregnancy and delivery after HiPorfin photodynamic therapy for cervical high-grade squamous intraepithelial lesion. Photodiagnosis Photodyn Ther. 46, 104062. https://doi.org/10.1016/j.pdpdt.2024.104062 (2024).
Jin, F. et al. Clinical application of photodynamic therapy for malignant airway tumors in China. Thorac. Cancer 11, 181–190. https://doi.org/10.1111/1759-7714.13223 (2020).
Li, Z. et al. Long-term results of ERCP- or PTCS-directed photodynamic therapy for unresectable hilar cholangiocarcinoma. Surg. Endosc. 35, 5655–5664. https://doi.org/10.1007/s00464-020-08095-1 (2021).
Liu, Y. et al. HiPorfin photodynamic therapy for vaginal high-grade squamous intraepithelial lesion. Arch. Gynecol. Obstet. https://doi.org/10.1007/s00404-024-07600-4 (2024).
Zhu, J. et al. Photodynamic therapy may salvage chemotherapy failure in gastric cancer: a case report and a literature review. Photodiagnosis Photodyn Ther. 46, 104038. https://doi.org/10.1016/j.pdpdt.2024.104038 (2024).
Acknowledgements
We thank all the participants and researchers who collaborated on the execution of this research.
Author information
Authors and Affiliations
Contributions
Y.L. performed data analysis and drafted the manuscript. R.Z.L., C.Z.L. and Z.H.L. revised the manuscript. L.F.D., L.N.G., Q.Y.H. and J.H. collected the data. L.H.W. and R.F.W. conceived, designed and supervised the study. All of the authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Y., Li, R., Li, C. et al. Photodynamic therapy compared with loop electrosurgical excision procedure in patients with cervical high-grade squamous intraepithelial lesion. Sci Rep 14, 27090 (2024). https://doi.org/10.1038/s41598-024-78445-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-78445-9