Abstract
Chronic kidney disease-mineral and bone disorder (CKD-MBD) are recognized as a systemic disease affecting the prognosis of patients with CKD. Proper management of CKD-MBD is important to improve the prognosis of patients with CKD. Although proteinuria is recognized as a poor prognostic factor in these patients, few reports have examined its association with CKD-MBD. We examined the association between proteinuria and CKD-MBD using data from the Japan Chronic Kidney Disease Database Extension (J-CKD-DB-Ex). Among the patients registered in the J-CKD-DB-Ex, 30,977 with CKD stages G2–G5 who had serum creatinine, albumin, calcium, and phosphate concentrations measured at least once and urinalysis performed were included. The patients were divided into four groups (negative, 1+, 2+, and 3+) according to the degree of proteinuria. The association between proteinuria and CKD-MBD was examined by a logistic regression analysis. In a model adjusted for age, sex, diabetes, and the estimated glomerular filtration rate (eGFR), the odds ratio of the 3 + group compared with the negative group significantly increased to 2.67 (95% confidence interval, 2.29–3.13) for hyperphosphatemia, 2.68 (1.94–3.71) for hypocalcemia, and 1.56 (1.24–1.98) for hypomagnesemia. Proteinuria is associated with hyperphosphatemia, hypocalcemia, and hypomagnesemia in patients with CKD independently of eGFR.
Similar content being viewed by others
Introduction
Disturbances in mineral and bone metabolism are widespread in chronic kidney disease (CKD). These disturbances are an important cause of morbidity, extraskeletal calcification, and are associated with increased cardiovascular mortality1,2,3. Disturbances in mineral and bone metabolism have traditionally been referred to as renal osteodystrophy and classified based on a bone biopsy. Subsequently, mineral metabolism disorders associated with CKD became recognized as systemic diseases, and the concept of CKD-mineral and bone disorder (CKD-MBD) was proposed to describe broader clinical manifestations4. This concept has been adopted internationally and has contributed to the global development of evidence-based clinical practice guidelines. These guidelines recommend target ranges for managing serum concentrations of calcium, phosphate, and parathyroid hormone (PTH), which are the main parameters in CKD-MBD. Appropriate management of these disorders is important to improve the prognosis of patients with CKD5. Recently, the importance of magnesium in managing CKD-MBD has also been recognized6.
Proteinuria is a highly sensitive marker of various kidney diseases and vascular endothelial disorders, and is recognized as a risk factor for CKD progression and mortality in patients with CKD7,8. CKD-MBD and proteinuria are important factors associated with a poor prognosis in patients with CKD, but few studies have examined their association. This study was performed to clarify the relationship between CKD-MBD (especially dysmetabolism of calcium, phosphate, and magnesium) and proteinuria in patients with CKD using data from the Japan Chronic Kidney Disease Database Extension (J-CKD-DB-Ex).
Materials and methods
Study design and population
The J-CKD-DB-Ex is a longitudinal extension of the existing Japan Chronic Kidney Disease Database (J-CKD-DB) (UMIN trial number, UMIN000026272). The J-CKD-DB-Ex is a multicenter, automatically extracted comprehensive database of patients with CKD from 21 Japanese university hospitals9,10. In this study, we used data on patients with CKD from four university hospitals from which we collected prior data. The J-CKD-DB was initiated in December 2014, and this database contains information on all inpatient and outpatient encounters, prescriptions, diagnostic codes, and laboratory measurements. J-CKD-DB inclusion criteria were as follows: (1) age ≥ 18 years; (2) proteinuria ≥ 1+ (dipstick test), and/or estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m29. The facilities participating in the J-CKD-DB were required to have electronic health record systems that incorporated Standardized Structured Medical Information eXchange 2 (SS-MIX2) storage and a structured data entry function that could transfer data to the SS-MIX2 storage system11. Patient records were anonymized and informed consent was obtained in an opt-out method on the website of each participating university hospital in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan. The J-CKD-DB-Ex study was conducted in accordance with the principles of the Declaration of Helsinki under the supervision of the Ethics Committee of Kawasaki Medical School. The J-CKD-DB-Ex was supported by grants from the Japan Agency for Medical Research and Development, Practical Research Project for Life-Style related Diseases including Cardiovascular Diseases and Diabetes Mellitus.
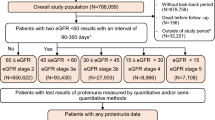
The study population comprised 34,628 patients from the J-CKD-DB-Ex registry with CKD stages G2–G5 who had serum creatinine, albumin, calcium, and phosphate concentrations measured at least once and urinalysis. Of the 34,628 patients, 1,012 were excluded from our study because of taking phosphate binders and/or vitamin D receptor activators. In addition, to minimize the impact of acute kidney injury (AKI) on the results, 2,639 patients with onset of AKI were excluded. The criteria for AKI were an increase in serum creatinine concentration of 0.3 mg/dL or more within 48 h or an increase of 1.5 times the basal value, based on the KDIGO classification12. We enrolled the remaining 30,977 patients in this cross-sectional study. The flowchart of patients enrolled in this study is shown in Fig. 1. When extracting the data used in this study from the database, patients with simultaneous measurements of four laboratory parameters (i.e., serum creatinine, albumin, calcium, and phosphate) were selected, and the lowest eGFR point was used as the reference point when multiple data were available for the same patient as performed in the previous study13. Inpatients and outpatients were included, and patients undergoing kidney replacement therapy (i.e., hemodialysis, peritoneal dialysis, and kidney transplantation) were not excluded. This study protocol was approved by the Clinical Research Ethics Committee of the Institutional Review Board at Kyushu University (Approval Number: 21166–02).
Outcomes and covariates
The primary outcome of the study was the presence of the following mineral metabolism disorders (i.e., hyperphosphatemia, hypophosphatemia, hypercalcemia, and hypocalcemia), and the secondary outcome of the study was the presence of abnormal magnesium metabolism (i.e., hypermagnesemia, and hypomagnesemia). Mineral metabolism disorders were defined as follows. Hyperphosphatemia and hypophosphatemia were defined as serum phosphate concentrations ≥ 4.5 mg/dL and < 2.5 mg/dL, respectively13,14,15. Hypercalcemia and hypocalcemia were defined as serum corrected calcium concentrations ≥ 10.3 mg/dL and < 8.4 mg/dL, respectively13,14. Hypermagnesemia and hypomagnesemia were defined as serum magnesium concentrations ≥ 2.5 mg/dL and < 1.8 mg/dL, respectively6,16. The serum corrected calcium concentration was calculated using the serum albumin concentration based on Payne’s formula: corrected calcium = serum calcium + (4 − serum albumin), only when the serum albumin concentration is < 4 g/dL17.
The primary exposure was the degree of proteinuria by the dipstick test. A urinalysis by the dipstick method was performed on spot urine specimens. The urine dipstick results were interpreted by the medical staff in each hospital and recorded as negative, 1+, 2+, and 3+. In accordance with the policy of the Japanese Committee for Clinical Laboratory Standards (https://www.jccls.org/), the urine dipstick results are manufactured to be displayed according to urine protein concentrations as follows: 0–29 mg/dL for negative, 30–99 mg/dL for 1+, 100–299 mg/dL for 2+, and ≥ 300 mg/dL for 3+. More precisely, the Japanese Committee for Clinical Laboratory Standards defines a urine protein concentration ≥ 1,000 mg/dL as 4+. However, the J-CKD-DB defines ≥ 300 mL/dL as 3 + because some urine test paper manufacturers do not have a 4 + setting. The patients were divided into four groups according to the degree of proteinuria: negative (n = 20,504), 1+ (n = 6,114), 2+ (n = 2,893), and 3+ (n = 1,466). The presence or absence of diabetes was obtained from the medical records. Serum PTH concentrations were measured using whole or intact PTH assays. The values measured by the two different assays were converted using the following formula: intact PTH (pg/mL) = 1.7 × whole PTH (pg/mL)18.
Statistical analysis
Continuous variables and categorical data are described as the median (interquartile range) and percentage, respectively. The distribution of the baseline characteristics stratified by the degree of proteinuria was compared using the following trend analyses. The Cochran–Armitage and Jonckheere–Terpstra tests were used for categorical and continuous variables, respectively. Age, sex, diabetes, and the eGFR were selected as confounding factors. Unadjusted and adjusted logistic regression models were used to estimate the odds ratio (OR) and 95% confidence interval (CI) for the outcomes. A two-tailed P-value < 0.05 was considered statistically significant in all analyses. Several subgroup sensitivity analyses were performed, including stratifying patients according to the presence or absence of diabetes because this has a major effect on proteinuria. Additionally, analyses in which patients were stratified by CKD stages were performed to examine the effect of kidney function. Finally, subgroup analyses were performed with PTH, a factor with high missing value, added as a confounding factor. Statistical analyses were performed with JMP pro version 17.0 (SAS Institute, Cary, USA) and EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R version 3.6.2 (www.r-project.org)19.
Results
Baseline characteristics according to the degree of proteinuria
The median age of the 30,977 patients was 71 years and 56.8% were men. The baseline characteristics of this study population stratified by the degree of proteinuria are shown in Table 1. Patients with higher levels of proteinuria showed the following: (1) younger age; (2) higher proportion of men and diabetes; (3) higher serum concentrations of creatinine and phosphate; (4) lower serum concentrations of albumin, corrected calcium and magnesium; and (5) a lower eGFR.
Distribution of mineral metabolism disorders according to the degree of proteinuria
The distribution of mineral metabolism disorders according to the degree of proteinuria is shown in Fig. 2. In particular, 26.1% (382/1,466) of patients with proteinuria 3 + had hyperphosphatemia. The proportion of patients with each mineral metabolism disorder tended to increase as proteinuria increased in hyperphosphatemia, hypercalcemia, hypocalcemia, hypermagnesemia, and hypomagnesemia.
Association of the degree of proteinuria with mineral metabolism disorders
The ORs and 95% CIs using the unadjusted and adjusted logistic regression models for mineral metabolism disorders according to the degree of proteinuria are shown in Table 2. In the model adjusted for age, sex, diabetes, and the eGFR, the ORs for the 3 + group compared with the negative group were significantly increased to 2.67 (95% CI, 2.29–3.13) for hyperphosphatemia, 2.68 (1.94–3.71) for hypocalcemia, and 1.56 (1.24–1.98) for hypomagnesemia. Adjusted ORs and 95% CIs for every one-category increase in proteinuria were 1.40 (1.33–1.46) for hyperphosphatemia, 1.17 (1.11–1.24) for hypophosphatemia, 1.43 (1.30–1.58) for hypocalcemia, and 1.25 (1.18–1.33) for hypomagnesemia. In hypophosphatemia, ORs for the 1 + and 2 + group compared with the negative group were significant; however, the significant difference disappeared for the 3 + group, which had ORs of 0.79 (0.59–1.04) compared with the negative group. In contrast, no consistent associations were found for hypercalcemia or hypermagnesemia. Adjusted ORs for the 3 + group compared with the negative group were 1.18 (0.93–1.49) for hypercalcemia and 1.06 (0.83–1.34) for hypermagnesemia; adjusted ORs and 95% CIs for every one-category increase in proteinuria were 1.06 (0.99–1.13) for hypercalcemia and 1.06 (0.99–1.13) for hypermagnesemia. The ORs and 95% CIs for mineral metabolism disorders for each confounding factor are shown in Supplementary Table 3.
Subgroup analyses
Subgroup analyses were performed by stratifying patients according to the presence or absence of diabetes. The ORs and 95% CIs using the adjusted logistic regression models for mineral metabolism disorders according to the degree of proteinuria stratified by the presence or absence of diabetes are shown in Table 3. A significant association was observed between proteinuria and hypercalcemia and hypermagnesemia in the group without diabetes, while this association disappeared in the group with diabetes. The results for the other mineral metabolism disorders were generally consistent with the main analysis of all subjects.
ORs and 95% CIs using adjusted logistic regression models for mineral metabolism disorders according to the degree of proteinuria stratified by CKD stage are shown in Supplementary Table 1. We focused on hyperphosphatemia, hypocalcemia, and hypomagnesemia, which were shown to have significant results in Table 2. In hyperphosphatemia, the results were similar to those shown in Table 2, except for CKD stages G3b and G4. In hypocalcemia, the number of patients in the 3 + group could not be adequately analyzed because stratification considerably reduced the number in this group. In hypomagnesemia, stratification by kidney function eliminated any significant association, suggesting that kidney function may have a significant impact on the association between proteinuria and hypomagnesemia.
Additional analyses were performed to determine the effect of PTH on mineral metabolism disorders (Supplementary Table 2). However, the number of subjects available for this analysis decreased from 30,977 to 1,062 because of the large number of missing PTH values. The extremely low number of outcomes may have destabilized the statistical model when multivariate analysis was performed.
Discussion
In this cross-sectional study of patients from the J-CKD-DB-Ex registry, we showed that the proportion of patients with mineral metabolism disorders tended to increase as proteinuria increased. In logistic regression models adjusted for age, sex, and the eGFR, we found that the increase in proteinuria was significantly associated with hyperphosphatemia, hypocalcemia, and hypomagnesemia. In this analysis using real-world data from the J-CKD-DB-Ex, we were able to show an association between proteinuria and CKD-MBD, both of which are risk factors for progression and mortality in patients with CKD.
Among the mineral metabolism disorders found in this study, hyperphosphatemia is a strong predictor of mortality and cardiovascular events, and an association between hyperphosphatemia and proteinuria has been reported. A cross-sectional study of 1,738 patients with CKD reported that albuminuria was significantly associated with higher plasma phosphate concentrations independent of the GFR20. To understand the mechanisms underlying these observations, the authors of this previous study conducted experiments using puromycin aminonucleoside (PAN)-induced nephrosis rats, which is a model that shows high levels of proteinuria. The expression of NaPi-IIa, a sodium–phosphate cotransporter in proximal tubules, was increased in PAN rats, which suggested that phosphate reabsorption in the tubules was enhanced. PAN rats also showed decreased phosphorylation of fibroblast growth factor (FGF) receptor substrate 2a, which is a major FGF-23 receptor substrate. This finding suggested that the urinary excretion of phosphate by FGF-23 may have been suppressed. Another cohort study also reported that proteinuria was associated with decreased FGF-23 biological activity and increased serum phosphate concentrations21. These previous results support our findings.
An association between proteinuria and the serum vitamin D status has been observed, which may explain the associations between proteinuria and hypocalcemia and hypomagnesemia. In experiments using PAN rats, vitamin D binding protein, to which the most serum vitamin D is bound, leaked into the urine as proteinuria, resulting in a decrease in serum 25-hydroxyvitamin D concentrations22. Similarly, a multicenter, cross-sectional study of patients with CKD reported that patients with a high amount of proteinuria were at higher risk of having low serum 25-hydroxyvitamin D concentrations23. Decreased 25-hydroxyvitamin D may result in decreased production of active vitamin D in the kidneys. The reduced action of active vitamin D suppresses calcium and magnesium absorption from the gastrointestinal tract, resulting in hypocalcemia and hypomagnesemia. Another cross-sectional study reported that proteinuria led to renal magnesium wasting through tubular injuries24. Because serum vitamin D is also involved in phosphate absorption, the aforementioned decrease in active vitamin D may explain the trend toward higher hypophosphatemia with increased proteinuria observed in this study.
Our study had two main strengths. First, the data used in this study were automatically extracted from medical records and are real-world data from actual clinical practice. Second, this study used a larger data set than previous studies20,25, increasing the possibility of generating better quality medical evidence regarding the association between proteinuria and CKD-MBD. Although urinalysis is frequently performed in clinical practice, it is rare to investigate mineral metabolism disorders, especially serum phosphate and magnesium disorders, in departments other than nephrology. However, given that this study has demonstrated an association between proteinuria and CKD-MBD, it may be advisable to evaluate patients with positive proteinuria using blood tests for hidden disorders in serum calcium, phosphate, and magnesium to help with early detection.
Our study also had several limitations. First, this study was conducted on patients at university hospitals, which may have led to selection bias and may not be widely applicable to patients with CKD. Second, of the data collected in the J-CKD-DB-Ex, some factors had high missing values (e.g., PTH) and some potential confounding factors were not collected (e.g., alkaline phosphatase). These factors could not be used in the multivariate analysis and their effect on the results could not be verified. Third, this was a cross-sectional study and causal relationships could not be discussed. Finally, unmeasured or unknown confounding factors could lead to a null hypothesis. Despite these limitations, we believe that the present observational study provides useful insights into proteinuria and mineral metabolism disorders in patients with CKD.
Conclusion
This study shows that proteinuria is associated with hyperphosphatemia, hypocalcemia, and hypomagnesemia in patients with CKD. Hopefully, the associations shown in this study will lead to further research and ultimately to further improvements in the management of proteinuria and CKD-MBD.
Data availability
The data analyzed in this study are not publicly available, but are available from the corresponding author on reasonable request.
References
Reiss, A. B. et al. CKD, arterial calcification, atherosclerosis and bone health: Inter-relationships and controversies. Atherosclerosis. 278, 49–59 (2018).
Yamada, S. & Nakano, T. Role of chronic kidney disease (CKD)-mineral and bone disorder (MBD) in the pathogenesis of cardiovascular disease in CKD. J. Atheroscler Thromb. 30, 835–850 (2023).
Magagnoli, L. et al. Association between CKD-MBD and mortality in older patients with advanced CKD-results from the EQUAL study. Nephrol. Dial Transpl. 38, 2562–2575 (2023).
Moe, S. et al. Definition, evaluation, and classification of renal osteodystrophy: A position statement from kidney disease: Improving global outcomes (KDIGO). Kidney Int. 69, 1945–1953 (2006).
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 clinical practice Guideline Update for the diagnosis, evaluation, Prevention, and treatment of chronic kidney disease–Mineral and Bone Disorder (CKD-MBD). Kidney Int. Suppl. 7, 1–59 (2017).
Sakaguchi, Y. The emerging role of magnesium in CKD. Clin. Exp. Nephrol. 26, 379–384 (2022).
Matsushita, K. et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: A collaborative meta-analysis. Lancet. 375, 2073–2081 (2010).
Inker, L. A. et al. Early change in proteinuria as a surrogate end point for kidney disease progression: An individual patient meta-analysis. Am. J. Kidney Dis. 64, 74–85 (2014).
Nakagawa, N. et al. J-CKD-DB: A nationwide multicentre electronic health record-based chronic kidney disease database in Japan. Sci. Rep. 10, 7351 (2020).
Nagasu, H. et al. Kidney outcomes Associated with SGLT2 inhibitors Versus other glucose-lowering drugs in real-world clinical practice: The Japan chronic kidney Disease Database. Diabetes Care. 44, 2542–2551 (2021).
Kimura, M. et al. SS-MIX: A ministry project to promote standardized healthcare information exchange. Methods Inf. Med. 50, 131–139 (2011).
Kidney Disease. Improving global outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute kidney Injury. Kidney Int. Suppl. 2, 1–138 (2012).
Sofue, T. et al. Prevalences of hyperuricemia and electrolyte abnormalities in patients with chronic kidney disease in Japan: A nationwide, cross-sectional cohort study using data from the Japan chronic kidney Disease Database (J-CKD-DB). PLoS One. 15, e0240402 (2020).
Fukagawa, M. et al. Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Ther. Apher Dial. 17, 247–288 (2013).
Bozic, M. et al. Independent effects of secondary hyperparathyroidism and hyperphosphataemia on chronic kidney disease progression and cardiovascular events: An analysis from the NEFRONA cohort. Nephrol. Dial Transpl. 37, 663–672 (2022).
Haider, D. G. et al. Hypermagnesemia is a strong independent risk factor for mortality in critically ill patients: Results from a cross-sectional study. Eur. J. Intern. Med. 26, 504–507 (2015).
Payne, R. B. et al. Interpretation of serum calcium in patients with abnormal serum proteins. Br. Med. J. 4, 643–646 (1973).
Kazama, J. J. Japanese Society of Dialysis Therapy treatment guidelines for secondary hyperparathyroidism. Ther. Apher Dial. 11, S44–S47 (2007).
Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 48, 452–458 (2013).
de Seigneux, S. et al. Proteinuria increases plasma phosphate by altering its tubular handling. J. Am. Soc. Nephrol. 26, 1608–1618 (2015).
Kim, H. et al. The effect of interactions between proteinuria, activity of fibroblast growth factor 23 and serum phosphate on renal progression in patients with chronic kidney disease: a result from the KoreaN cohort study for Outcome in patients with chronic kidney Disease study. Nephrol. Dial Transpl. 35, 438–446 (2020).
Matsui, I. et al. Active vitamin D and its analogue, 22-oxacalcitriol, ameliorate puromycin aminonucleoside-induced nephrosis in rats. Nephrol. Dial Transpl. 24, 2354–2361 (2009).
Hamano, T. et al. Guideline-practice gap in the management of predialysis chronic kidney disease mineral bone disorder in Japan. Ther. Apher Dial. 15, 2–8 (2011).
Oka, T. et al. Proteinuria-associated renal magnesium wasting leads to hypomagnesemia: A common electrolyte abnormality in chronic kidney disease. Nephrol. Dial Transpl. 34, 1154–1162 (2019).
Yap, Y. S. et al. Hyperphosphatemia is associated with overt proteinuria in non-diabetic patients with late-stage chronic kidney disease: A cross-sectional study. Int. Urol. Nephrol. 45, 163–172 (2013).
Acknowledgements
We thank Ellen Knapp, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
Sho Shimamoto: Conceptualization, Methodology, Formal analysis, Visualization, Writing- Original draft preparation. Takako Nakahara: Investigation, Data curation, Visualization, Writing- Reviewing and Editing. Shunsuke Yamada: Validation, Writing- Reviewing and Editing. Hajime Nagasu: Data curation, Writing- Reviewing and Editing. Seiji Kishi: Data curation, Validation. Naoki Nakashima, Kazuhiko Tsuruya, Hirokazu Okada, Kouichi Tamura, Ichiei Narita, Shoichi Maruyama, Yuichiro Yano, Takashi Yokoo, Takashi Wada, Jun Wada, Eiichiro Kanda, Hiromi Kataoka, and Masaomi Nangaku: interpretation of data, final approval of the submitted manuscript. Naoki Kashihawa: Project administration. Toshiaki Nakano: Conceptualization, Validation, Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shimamoto, S., Nakahara, T., Yamada, S. et al. Association between proteinuria and mineral metabolism disorders in chronic kidney disease: the Japan chronic kidney disease database extension (J-CKD-DB-Ex). Sci Rep 14, 27481 (2024). https://doi.org/10.1038/s41598-024-79291-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-79291-5