Abstract
Background
The value of endoscopic septoplasty for patients with deviated nasal septum and allergic rhinitis has not been systematically summarized. This study aims to assess the impact of surgical intervention on quality of life through a meta-analysis.
Methods
We conducted a comprehensive search of PubMed, CNKI, EMBASE, and the Cochrane Library for studies on the treatment of patients with deviated nasal septum and allergic rhinitis up to 2024. Studies that were duplicates, lacked full text, had incomplete data, or involved animal experiments, commentaries, or systematic reviews were excluded. Meta-analysis was performed using STATA 16.0.
Results
The total nasal symptom score (TNSS) in patients who received endoscopic surgery was considerably reduced compared to those treated with spray therapy alone, indicating a significant improvement (SMD = -21.29, 95% CI: -26.26, -116.33). Classic symptoms of allergic rhinitis, including rhinorrhea (SMD=-9.97, 95% CI: -16.97, -2.98), nasal obstruction (SMD=-27.25, 95% CI: -41.12, -13.38), nasal itching (SMD=-10.32, 95% CI: -13.16, -7.48), and sneezing (SMD=-12.66, 95% CI: -14.99, -10.34), showed significant improvement. There was no significant difference in the incidence of complications between the two treatments (OR = 1.01, 95% CI: 0.49, 2.10).
Conclusion
Patients with a deviated nasal septum and allergic rhinitis benefit more from septoplasty. However, the procedure should be performed cautiously by experienced clinicians, taking into account the specific condition of the nasal septum.
Similar content being viewed by others
Introduction
Allergic rhinitis (AR) is one of the most prevalent global health concerns, currently affecting up to 30% of the population1, with its incidence steadily rising. The disease is often accompanied by complications that significantly diminish quality of life due to its chronic nature and recurrent episodes, making full recovery difficult for many patients. AR is a non-infectious inflammatory condition of the nasal mucosa, triggered by immune responses involving various active cells and cytokines upon allergen exposure2,3,4. Clinically, AR is characterized by paroxysmal sneezing, nasal congestion, and rhinorrhea, with nasal congestion being the most common and debilitating symptom. In severe cases, AR can also affect the eyes and paranasal sinuses, further impairing patients’ daily activities and overall well-being.
Deviated nasal septum (DNS) affects more than 70% of the general population to varying degrees5. DNS primarily manifests as nasal obstruction but can also lead to snoring, anxiety, headaches, mouth breathing, and sinusitis6,7, with nasal congestion being the most prominent complaint. Coexisting conditions, such as turbinate hypertrophy, AR, and chronic sinusitis, can exacerbate these symptoms, with AR being the most frequently associated comorbidity8.
Septoplasty (STP) is the standard surgical intervention for DNS and often yields satisfactory outcomes9,10,11. In cases of DNS combined with AR, the deviation can worsen AR by promoting antigen accumulation in the nasal cavity. Additionally, DNS may hinder the efficacy of nasal spray treatments, as the anatomical obstruction prevents proper drug distribution, limiting therapeutic effectiveness. Conservative management of AR includes allergen avoidance, pharmacotherapy (e.g., antihistamines, leukotriene inhibitors, or corticosteroids), and specific allergen immunotherapy. While these strategies can alleviate symptoms, some patients with refractory AR do not achieve adequate control with medication alone.
Managing patients with both DNS and AR remains a clinical challenge. Various treatment options have been explored, but none have consistently provided optimal results. The effectiveness of septoplasty in this population is still debated, with some studies reporting limited improvement in patients with both DNS and AR12.
The aim of this study is to evaluate the benefits of combining nasal septoplasty with pharmacotherapy for patients with DNS and AR. Outcome measures, including the total nasal symptom score (TNSS), symptom relief, and quality of life, will be used to assess the impact of this combined treatment approach13,14,15,16. Our findings will provide evidence to guide future treatment strategies.
Materials and methods
Search strategy
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines17. The protocol has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42024584093).We performed a comprehensive search of electronic databases, including PubMed, EMBASE, the Cochrane Library, and CNKI, for relevant studies published between 2000 and 2024. The search terms used were “septoplasty” or “nasal septal reconstruction” or “septectomy” combined with “allergic rhinitis” and “nasal septal deviation”. Additionally, we manually reviewed the reference lists of relevant studies to identify other eligible articles. Two researchers independently conducted the search process.
Inclusion and exclusion criteria
The inclusion criteria for the selected studies were as follows:
-
1.
Adults (participants aged ≥ 18 years) diagnosed with allergic rhinitis and nasal septal deviation.
-
2.
At least one of the following surgical interventions: septoplasty, nasal septal reconstruction, or septectomy.
-
3.
A control group receiving non-surgical conservative treatment, including nasal corticosteroid sprays, oral or intravenous corticosteroids, intranasal decongestant sprays, or oral antihistamines.
-
4.
Data reported for at least one outcome, such as total effective rate, length of hospital stay, symptom scores, or complications.
-
5.
Randomized controlled trials (RCTs).
The exclusion criteria were as follows:
-
1.
Animal experiments, comments, abstracts, letters, or editorial materials.
-
2.
Studies lacking a clear diagnosis of both allergic rhinitis and nasal septal deviation in the participants.
-
3.
Inability to obtain full-text articles or extract relevant data.
Data extraction and quality assessment
Two researchers independently extracted key information from each study, including the first author’s name, publication year, sample size, mean patient age, gender ratio, surgical treatment plan, control strategy, follow-up duration, and primary outcomes. Full-text articles were retrieved when necessary to gather sufficient information, and any discrepancies were resolved by consulting the original authors. The methodological quality of the included studies was assessed using the Cochrane risk-of-bias tool.
Statistical analysis
Following the recommendations of the Cochrane Collaboration, we conducted a quantitative synthesis of the included study indicators. Meta-analyses were performed using STATA 16.0 software. For binary outcomes, we calculated the odds ratio (OR) with 95% confidence intervals (CI), while for continuous outcomes, we utilized the standardized mean difference (SMD) with 95% CI to assess the treatment effect. A random-effects model was employed to account for potential clinical heterogeneity. If I² exceeded 50%, subgroup analyses based on baseline characteristics, interventions, or sensitivity analyses (where studies were sequentially excluded) were performed to identify the source of heterogeneity18. Publication bias and small sample effects were assessed using funnel plots and statistical tests19.
Results
Basic characteristics of the included studies
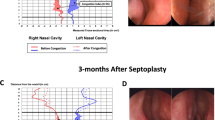
Following the predefined screening criteria, 15 randomized controlled trials were included in the analysis, as detailed in Fig. 120,21,22,23,24,25,26,27,28,29,30,31,32,33,34. The included studies involved a total of 709 patients who received nasal endoscopic surgery and/or spray therapy, and 707 patients who received conservative treatment alone. The participants’ ages ranged from 25 to 45 years. Although the specific population characteristics were not fully reported in all studies, the authors indicated that the treatment groups were comparable across studies. The follow-up period ranged from 6 to 12 months, during which improvements in patient symptoms were recorded. The study findings varied depending on the specific objectives of each trial. A comprehensive assessment of the methodological quality revealed that all studies had a low risk of bias. Further details can be found in Table 1; Fig. 2.
Main results
In 6 studies, the total nasal symptom score (TNSS) of patients treated with endoscopic surgery and/or spray therapy was evaluated23,25,27,28,29,34. Significant heterogeneity was found (I² = 98.8%, p < 0.001; Fig. 3), and the random-effects model was applied. Surgical treatment had significantly improvement in reducing TNSS compared to conservative therapy (SMD = -21.29, 95% CI: -26.26, -116.33). Sensitivity analysis indicated stable results, with no publication bias observed (p > 0.05). We also examined symptom improvement between the experimental and control groups, with precise scoring of symptoms. In three studies, rhinorrhea scores were reported for patients treated with endoscopic surgery and spray therapy23,27,29. Significant heterogeneity was found (I² = 98.4%, p < 0.001; Fig. 4a), and the random-effects model was applied. Surgical treatment was significantly more effective in reducing rhinorrhea compared to conservative therapy (SMD = -9.97, 95% CI: -16.97, -2.98). Sensitivity analysis indicated stable results, with no publication bias observed (p > 0.05).
For nasal obstruction, three studies provided data on patient scores23,27,29. Heterogeneity was present (I² = 98.7%, p < 0.001; Fig. 4b), and the random-effects model showed that surgical treatment was more effective in alleviating nasal obstruction than conservative spray therapy (SMD = -27.25, 95% CI: -41.12, -13.38). No instability was observed in the sensitivity analysis, and no publication bias was detected (p > 0.05).
Three studies assessed nasal itching scores23,27,29. The heterogeneity test found significant heterogeneity (I² = 89.4%, p < 0.001; Fig. 4c), and a random-effects model was applied. Surgical treatment significantly reduced nasal itching compared to conservative treatment (SMD = -10.32, 95% CI: -13.16, -7.48). The sensitivity analysis showed stable results, with no publication bias (p > 0.05).
Sneezing scores were reported in three studies. Heterogeneity was again present (I² = 76.2%, p = 0.015; Fig. 4d)23,27,29, and the random-effects model demonstrated a greater reduction in sneezing with surgical treatment compared to conservative treatment (SMD = -12.66, 95% CI: -14.99, -10.34). Sensitivity analysis indicated stable results, and no publication bias was observed (p > 0.05).
Lastly, complications were assessed in five studies24,25,27,32,33. No significant heterogeneity was found (I² = 0.0%, p = 0.591; Fig. 5), allowing the use of a fixed-effects model. The complication rate did not significantly differ between the surgical group and the conservative treatment group (OR = 1.01, 95% CI: 0.49, 2.10). Sensitivity analysis confirmed the robustness of the results, and no publication bias was found (p > 0.05).
Discussion
Nasal septal deviation primarily reduces nasal airflow due to alterations in bone and cartilage structures, making it one of the leading causes of nasal congestion in otolaryngology9,35. The reported incidence of nasal septal deviation varies widely, from 30.9 to 65%, depending on the criteria used to define it. This condition can have significant physical and social consequences, affecting patients’ quality of life, and septoplasty remains the most common surgical treatment36. The success of this surgery largely depends on the patient’s subjective satisfaction with functional outcomes. In patients with allergic rhinitis, mucosal hypertrophy further contributes to airway narrowing. While septoplasty increases the cross-sectional area of the nasal airway, its efficacy in alleviating symptoms of allergic rhinitis remains unclear.
Our study demonstrates that patients undergoing endoscopic nasal surgery achieve significantly improvement in reducing TNSS compared to those receiving conservative spray treatment. Symptom improvement, including relief from rhinorrhea, nasal obstruction, nasal itching, and sneezing, was consistently more pronounced following surgery compared to conservative spray treatment. The outcomes reflect the technical skill of the surgeons and the appropriateness of surgical indications. Importantly, no severe complications, such as nasal septal perforation, abscess formation, or nasal collapse, were observed. It is also crucial to emphasize the importance of addressing adenoid hypertrophy in children to prevent future complications.
The debate regarding the benefits of combining septoplasty with turbinate reduction surgery continues. While some studies, such as those by Stewart11 and Uppal37, found no significant difference between septoplasty with or without turbinate reconstruction, Hong38 reported better outcomes with combined surgery one-month post-operation, though the difference was no longer significant at three and six months. Hong’s findings suggest that the combination may provide faster and more consistent symptom relief. Similarly, Nilsen39 compared outcomes of septoplasty, inferior turbinate radiofrequency therapy (RFIT), and their combination, concluding that the combined approach resulted in reduced postoperative nasal congestion. Combining septoplasty with inferior turbinate surgery may also reduce the likelihood of requiring revision surgery40.
Our study indicates that septoplasty significantly improves nasal symptoms and quality of life. Allergic patients, on average, are more likely to experience persistent nasal congestion and facial pressure postoperatively than non-allergic patients, highlighting the need for careful postoperative management. Prior research has shown that patients with asthma are prone to more severe nasal congestion, which may necessitate aggressive nasal airway interventions to improve lower respiratory function41. Nasal blockage compromises the ability to cleanse, humidify, and warm inhaled air, potentially worsening asthma symptoms. However, in our study, there was no significant difference in postoperative symptom improvement between asthma and non-asthma patients, suggesting that both groups can achieve similar quality-of-life outcomes post-surgery.
Despite its strengths, this study has several limitations. A notable weakness is the reliance on Chinese literature, with limited inclusion of studies from other regions. While Chinese otolaryngology practices are well-established and based on extensive clinical experience, this may restrict the generalizability of our findings. Additionally, variations in medication regimens across patients due to differences in symptom severity and tolerance introduced heterogeneity among the studies. Future large-scale, multicenter randomized clinical trials with standardized treatment protocols are necessary to validate these findings.
Data availability
Data is provided within the manuscript or supplementary information files.
References
García-Paz, V. et al. Allergic rhinitis improvement after septorhinoplasty in a sample of allergic rhinitis patients with septal deviation: a quasi-experimental study. Sao Paulo Med. J. 140, 17–23 (2022).
Ghosh, S. K., Dutta, M. & Haldar, D. Role of bilateral Inferior Turbinoplasty as an Adjunct to Septoplasty in improving nasal obstruction and subjective performance in patients with deviated nasal Septum Associated with allergic rhinitis: an interventional, prospective study. Ear Nose Throat J. 102, 445–452 (2023).
Kirmaz, C. et al. Effects of allergen-specific immunotherapy on functions of helper and regulatory T cells in patients with seasonal allergic rhinitis. Eur. Cytokine Netw. 22, 15–23 (2011).
Al-Rasheedi, A. N. et al. Changes in serum hypoxia-inducible factor-1α and erythropoietin in allergic rhinitis patients: correlation with the th inflammatory profile and disease comorbidities. Int. J. Immunopathol. Pharmacol. 37, 3946320231196745 (2023).
Clark, D. W., Del, S. A., Raithatha, R. & Senior, B. A. Nasal airway obstruction: prevalence and anatomic contributors. Ear Nose Throat J. 97, 173–176 (2018).
Ma, Q., Su, K., Fu, Z., Wang, P. & Shi, H. Anxiety and depression in patients with nasal septal deviation. Am. J. Otolaryngol. 41, 102450 (2020).
Deveci, I. et al. Impact of nasal septal surgery on Sleep Quality and Attention-Deficit/Hyperactivity disorder. J. Craniofac. Surg. 29, e632–e635 (2018).
Salo, P. M. et al. Prevalence of allergic sensitization in the United States: results from the National Health and Nutrition Examination Survey (NHANES) 2005–2006. J. Allergy Clin. Immunol. 134, 350–359 (2014).
Bugten, V. et al. Quality of life and symptoms before and after nasal septoplasty compared with healthy individuals. BMC Ear Nose Throat Disord. 16, 13 (2016).
Hytönen, M., Blomgren, K., Lilja, M. & Mäkitie, A. A. How we do it: septoplasties under local anaesthetic are suitable for short stay surgery; the clinical outcomes. Clin. Otolaryngol. 31, 64–68 (2006).
Stewart, M. G. et al. Outcomes after nasal septoplasty: results from the nasal obstruction septoplasty effectiveness (NOSE) study. Otolaryngol. Head Neck Surg. 130, 283–290 (2004).
Karatzanis, A. D. et al. Septoplasty outcome in patients with and without allergic rhinitis. Rhinology 47, 444–449 (2009).
Bernstein, J. A., Bernstein, J. S., Makol, R. & Ward, S. Allergic rhinitis: a review. JAMA 331, 866–877 (2024).
Torres, M. I. et al. Intranasal Versus Oral Treatments for Allergic Rhinitis: A Systematic Review with Meta-Analysis. J Allergy Clin Immunol Pract. S2213-2198(24)00888-2. Advance online publication. (2024). https://doi.org/10.1016/j.jaip.2024.09.001
Corren, J. et al. Effects of Combination Treatment with Tezepelumab and Allergen Immunotherapy on Nasal Responses to Allergen: a Randomized Controlled Trial. J. Allergy Clin. Immunol. 151, 192–201 (2023).
Kasemsuk, N. et al. Local nasal immunotherapy for allergic rhinitis: a systematic review and Meta-analysis. Int. Forum Allergy Rhinol. 12, 1503–1516 (2022).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6, e1000097 (2009).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Duval, S. & Tweedie, R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455–463 (2000).
Pan, J. & Shihong, Y. Clinical analysis of nasal endoscopic surgery in the treatment of allergic Rhinitis. China Continuing Med. Educ. (in Chinese). 8, 90–92 (2016).
Hua, L. & Zheng, T. Submucous Correction of Nasal Septum in treating perennial allergic rhinitis with nasal septum deviation. J. Yichun Coll. (in Chinese). 36, 65–67 (2014).
Baisheng, L. Surgical Treatment of allergic rhinitis with nasal septum deviation: a Clinical Observation of 100 cases. J. Med. Theory Pract. (in Chinese). 28, 1498–1499 (2015).
Ping, L. Surgical Treatment Effect of deviation of nasal septum with allergic Rhinitis. Chin. Foreign Med. Res. (in Chinese). 17, 50–51 (2019).
Yiming, L. Clinical Observation of nasal septum correction under nasal endoscope for allergic Rhinitis. J. Clin. Med. Literature (in Chinese). 5, 1–2 (2018).
Zhicheng, S. Analyze the clinical Effect and Rehabilitation Status of Surgical Treatment of nasal septum deviation with allergic Rhinitis. Chin. Med. Digest: Otorhinolaryngol. (in Chinese). 36, 48–50 (2021).
Qiuju, T. Analysis of nasal septum correction in the treatment of nasal septum deviation complicated with allergic Rhinitis. China Health Standard Manage. (in Chinese). 7, 63–65 (2016).
Chunhui, W. Analysis of Surgical Treatment of nasal septal deviation and allergic Rhinitis. Syst. Med. (in Chinese). 5, 37–39 (2020).
Enfu, W. Clinical effect of Surgical Treatment of patients with allergic rhinitis with nasal septum deviation. China Foreign Med. Treat. (in Chinese). 39, 67–69 (2020).
Hao, W. Surgical Treatment Effect of nasal septum deviation with allergic Rhinitis. Chin. J. Mod. Drug Application (in Chinese). 15, 70–72 (2021).
Juntao, W., Yumin, Y., Quangui, Y. & Delong, Y. Endoscopic septoplasty for the treatment of deviated nasal septum with allergic Rhinitis. Practical Clin. Med. (in Chinese). 16, 79–80 (2015).
Wei, Y. Observation on Prognosis of patients with deviation of nasal septum and allergic Rhinitis treated by surgery. Chin. Foreign Med. Res. (in Chinese). 17, 126–127 (2019).
Qinggen, Y., Juncai, C. & Hui, W. Efficacy Observation of Corrective Therapy of Nasal Septum Deviation for 58 cases of allergic Rhinitis. China Practical Med. (in Chinese). 12, 23–24 (2017).
Chaoguan, Z., Yunkai, Z. & Zi, L. Therapeutic effect of modified septoplasty for allergic rhinitis with nasal septum deviation. Chin. J. Otorhinolaryngology-Skull Base Surg. (in Chinese). 23, 168–170 (2017).
Shiming, Z. Analysis on the Effect of Surgical correction of nasal septum deviation for the treatment of allergic Rhinitis complicated with nasal septum deviation. Clin. Med. Eng. (in Chinese). 24, 217–218 (2017).
Hsu, D. W. & Suh, J. D. Anatomy and physiology of nasal obstruction. Otolaryngol. Clin. North. Am. 51, 853–865 (2018).
Alanazy, S. et al. Patterns of allergic rhinitis among adults in Qassim region, Saudi Arabia: a cross sectional study. Pan Afr. Med. J. 40, 70 (2021).
Uppal, S., Mistry, H., Nadig, S., Back, G. & Coatesworth, A. Evaluation of patient benefit from nasal septal surgery for nasal obstruction. Auris Nasus Larynx. 32, 129–137 (2005).
Hong, S. D. et al. Predictive factors of subjective outcomes after septoplasty with and without turbinoplasty: can individual perceptual differences of the air passage be a main factor? Int. Forum Allergy Rhinol. 5, 616–621 (2015).
Nilsen, A. H., Helvik, A. S., Thorstensen, W. M. & Bugten, V. A comparison of symptoms and quality of life before and after nasal septoplasty and radiofrequency therapy of the inferior turbinate. BMC Ear Nose Throat Disord. 18, 2 (2018).
Karlsson, T. R., Shakeel, M., Supriya, M., Ram, B. & Ah-See, K. W. Septoplasty with concomitant inferior turbinate reduction reduces the need for revision procedure. Rhinology 53, 59–65 (2015).
Thorstensen, W. M. et al. Sino-nasal characteristics in asthmatic patients. Otolaryngol. Head Neck Surg. 147, 950–957 (2012).
Acknowledgements
Supported by National Natural Science Foundation of China NO.82071031 and the Natural Science Foundation of Jilin Province NO.YDZJ202301ZYTS030.
Author information
Authors and Affiliations
Contributions
Yu Wu and Shengrui Gao designed the study and developed the retrieve strategy. Yu Wu and Tingting Yu executed the systematic evaluation as the first and second reviewers, searching and screening the summaries and titles, assessing the inclusion and exclusion criteria, generating data collection forms and extracting data, and evaluating the quality of the study. Yu Wu and Zhenyu Zhang performed meta-analysis. Yu Wu drafted the article, which was reviewed and revised by Xin Wang and Shengrui Gao.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This is a systematic review and meta-analysis, ethics approval and consent to participate are not applicable.
Consent for publication
Not applicable. This study does not involve human participants.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, Y., Yu, T., Zhang, Z. et al. The benefits of septoplasty for patients with deviated nasal septum and allergic rhinitis: a meta-analysis. Sci Rep 14, 28855 (2024). https://doi.org/10.1038/s41598-024-80377-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-80377-3