Abstract
Sodium-glucose co-transport protein 2 (SGLT2) inhibitors, a novel category of oral hypoglycemic agents, offer a promising outlook for individuals experiencing heart failure with reduced ejection fraction. Evidence is emerging that highlights their potential in alleviating myocardial fibrosis and oxidative stress. However, the precise mechanisms through which SGLT2 inhibitors influence myocardial fibrosis induced by angiotensin II (Ang II) or transforming growth factor-β1 (TGF-β1) are not fully understood. This study aims to explore the intricate mechanisms by which SGLT2 inhibitors ameliorate myocardial fibrosis, particularly focusing on the nuanced interplay within the SIRT6 signaling pathway. Primary cardiac fibroblasts were isolated from the hearts of 1-3-day-old neonatal KM mice, were stimulated with Ang II or TGF-β1 to establish an in vitro model of myocardial fibrosis. Treatment with 10 µM Empagliflozin (EMPA) and Dapagliflozin (DAPA) significantly curtailed the proliferation of cardiac fibroblasts, substantially reduced collagen expression induced by Ang II/TGF-β1, and mitigated the phenotypic transformation and oxidative stress response. SIRT6, which is closely associated with myocardial fibrosis, demonstrated that the suppression its expression attenuated the protective effects of EMPA and DAPA against myocardial fibrosis and oxidative stress. Our findings suggest that SGLT2 inhibitors markedly decrease the Ang II/TGF-β1-induced transformation of cardiac fibroblasts to a myofibroblast phenotype by upregulating SIRT6 protein expression, thereby inhibiting oxidative stress and ameliorating myocardial fibrosis.
Similar content being viewed by others
Introduction
Over the past decade, heart failure patients have experienced increased rates of hospitalization and mortality, leading to a growing financial burden1. Heart failure can result in impaired myocardial contractile function, often characterized by myocardial fibrosis, a common feature in various cardiac diseases. Myocardial fibrosis, influenced by factors like ischemia and oxidative stress, contributes to complications such as arrhythmias2,3,4. Currently, there is no specific treatment for myocardial fibrosis, and clinical interventions include ACE inhibitors, AT1 receptor blockers, and extracellular matrix (ECM) cross-linking enzyme inhibitors5. The renin-angiotensin-aldosterone system, particularly Angiotensin II (Ang II) and transforming growth factor-β1 (TGF-β1), plays a key role in inducing myocardial fibrosis through fibroblast activation and ECM protein synthesis. Oxidative stress and TGF-β1 further contribute to the pro-fibrotic pathway6,7,8,9.
Type 2 diabetes represents a significant risk factor for cardiovascular diseases, highlighting an urgent demand for efficacious therapeutic strategies. Sodium-glucose co-transporter 2 (SGLT2) inhibitors, a class of anti-hyperglycemic drugs, lower blood sugar levels by enhancing glycosuria, osmotic diuresis, and urinary sodium excretion. These inhibitors provide ancillary benefits that extend beyond glycemic control, such as promoting weight loss and reducing blood pressure, which suggest a cardiorenal protective effect in both diabetic and non-diabetic populations. Notable SGLT2 inhibitors used in China include Dapagliflozin (DAPA), Empagliflozin (EMPA), and Canagliflozin. Extensive cardiovascular trials have shown that SGLT2 inhibitors effectively control glucose without significantly increasing cardiovascular risks in diabetic patients. Furthermore, these medications have shown a significant capacity to reduce major adverse cardiovascular events (MACE) and decrease rehospitalization rates in heart failure patients. Recent research highlights the cardiovascular protective role of SGLT2 inhibitors, revealing their potential to alleviate oxidative stress, inflammation, and fibrosis. This evolving research area emphasizes the current importance and impact of SGLT2 inhibitors in cardiovascular studies10,11.
SIRT6, a nicotinamide adenine dinucleotide-dependent histone deacetylase primarily expressed in the heart, kidney, and brain, is renowned for its association with longevity. Studies have shown a reduction in SIRT6 expression levels in both animal models of heart failure and in vitro cellular models subjected to induction by surgical manipulation or stimulants such as Ang II and TGF-β1. This decrease in SIRT6 expression has been correlated with increased markers of myocardial fibrosis, resulting in impaired cardiac function12,13. Therefore, SIRT6 plays a negative regulatory role in cardiac diseases such as myocardial fibrosis and cardiac hypertrophy. Its cardioprotective effects are largely due to its anti-oxidative and anti-apoptotic characteristics. Recent studies have indicated that in diabetic atherosclerosis, which stems from diabetic lesions, the administration of SGLT2 inhibitors can upregulate SIRT6 expression levels. Similar findings have been observed in further in vitro experiments involving human aortic endothelial cell14. Hence, SIRT6 acts as a mediator for the beneficial effects of SGLT2 inhibitors. In light of these findings, we propose a hypothesis that SIRT6 might serve as a potential therapeutic target for SGLT2 inhibitors to mitigate myocardial fibrosis.
In summary, our study primarily focuses on the impact of the SGLT2 inhibitors, DAPA and EMPA, on the Ang II/TGF-β1-induced in vitro myocardial fibrosis model. We aim to investigate their protective effects and mechanisms on damaged myocardium, with oxidative stress response and the potential involvement of SIRT6 being crucial factors.
Methods and materials
Animals
The study is reported in accordance with ARRIVE guidelines. It received approval and oversight from the Laboratory Animal Resource Center at Dalian Medical University (Approval No. AEE24002), adhering to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85–23, revised 1996). Neonatal KM mice (1–3 days old) were sourced from the animal center at Liaoning Changsheng Biotechnology Co., Ltd.
KM neonatal mice cardiac fibroblasts culture and treatment
Cardiac fibroblasts (CFs) were isolated from 1 to 3 day old KM neonatal mice. Before rapid cardiac excision, animals were anesthetized with 4% isoflurane inhalation, and the adequacy of anesthesia was monitored by the absence of reflexes. Subsequently, the mice were humanely euthanized by cervical dislocation. The extraction process began with an overnight enzymatic breakdown using 0.25% trypsin at 4℃ for 12 h. This was followed by further enzymatic disintegration with 0.8% type II collagenase at 37℃ for 1 h. Afterward, the cell mixtures were centrifuged, and the resulting sediments were resuspended in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin. Following 1 h of differential adhesion, cardiomyocytes and CFs were separated.
When the CF density reached approximately 90%, trypsin digestion was applied for 3–5 min, followed by centrifugation at 1000 rpm for 5 min at room temperature. The cells were then resuspended and seeded into 6-well plates at a density of 2.5 × 105 cells/mL. After 24 h of growth, the cells were treated with Ang II (No.A1042; APE×BIO) for 48 h and TGF-β1 (#AF-100–21 C; PeproTech, Rock Hill, NJ) for 24 h, respectively. Prior to Ang II and TGF-β1 treatment, 10 µM EMPA (#HY-15409; MedChemExpress) and DAPA (#HY-10450; MedChemExpress) were applied to CFs 1 h before.
MTT assay
The MTT kit (#E-CK-A341; Elabscience) was employed to assess the viability and proliferation rate of CFs. CFs were seeded at a density of 5 × 104 cells/mL in 96-well plates and allowed to grow to confluence. Subsequently, they were treated with varying concentrations of Ang II (0.01, 0.1, 1 µM) and TGF-β1 (1, 5, 10 ng/mL). After pretreatment, 50 µL of MTT reagent was added to each well, and the cells were further incubated at 37℃ for 4 h. After aspirating the supernatant, 150 µL of DMSO was introduced to each well to dissolve the formazan crystals formed by viable cells. The optical density (OD) of each well was measured at a wavelength of 570 nm using a microplate reader (Molecular Devices, USA), providing a quantitative assessment of cell viability and proliferation.
Western blot analysis
Total protein was extracted from CFs using RIPA lysis buffer containing protease inhibitors. The BCA working solution was prepared to quantifiy the extracted protein groups, which were then denatured by heating, separated by SDS-PAGE electrophoresis, and transferred to a PVDF membrane. The membrane was blocked with 5% skim milk for 1 h. Subsequently, the membranes were incubated overnight at 4 °C with the following primary antibodies: GAPDH (1:10000), COL1 (1:1000), COL3 (1:500), TGF-β1 (1:500), NOX4 (1:500), and SIRT6 (1:500). Afterward, the membranes were incubated with secondary antibodies at room temperature for 1 h. Immunoreactive protein bands were detected using the ECL Plus Kit (180–5001, Tanon, China) and the ChemiDoc XRS + system (Bio-Rad, USA). The protein intensities were quantitatively measured using ImageJ software, with GAPDH serving as the internal reference protein.
Measurement of oxidative stress markers and reactive oxygen species (ROS) generation
The levels of reactive oxygen species (ROS) in CFs were assessed using DCFH-DA fluorescent probes. The collected samples were incubated with DCFH-DA at 37 ℃ for 45 min in a light-protected, humidified chamber. After rinsing with PBS, images were captured using an ortho-fluorescence microscope (Leica DM68 THUNDER). For each biological sample, three to five fields of view were selected, maintain consistent exposure time, gain, and offset settings. The fluorescence signals were analyzed using ImageJ software. The ROS expression levels in CFs from each group were determined using flow cytometry. The activities of glutathione peroxidase (GSH, Solarbio) and malondialdehyde (MDA, S0131S, Beyotime) were measured using commercial assay kits according to the manufacturer’s instructions.
Immunofluorescent staining
Immunofluorescence staining of α-smooth muscle actin (α-SMA) (ABclonal; A17910) in cultured CFs was performed. Cells were fixed in 4% paraformaldehyde for 15 min and permeabilized with 0.5% TritonX-100 for 20 min at room temperature. After blocking with 5% BSA for 1 h at room temperature, the cells were incubated with the primary antibody α-SMA at 4 ℃ overnight. The cells were then washed three times with PBST and incubated with secondary antibodies (ABclonal; AS007) for 1 h at room temperature in the dark. Finally, the cells were rinsed three times and incubated in DAPI (Beyotime, P0131). Images were visualized by using a fluorescence microscope.
Small interference RNA (siRNA) transfection
CFs were seeded into 6-well plates at a density of 2.5 × 105 cells/mL, and transient knockdown assays were conducted using Lipofectamine 2000. The siRNA targeting SIRT6 was procured from GenePharma (Shanghai, China). The sequence of the SIRT6 siRNA was as follows:
Sense: 5′-GCUGCACGGAAACAUGUUUTT-3′.
Antisense: 5′-AAACAUGUUUCCGUGCAGCTT-3′.
After transfection, the transfection reagent was removed, and 2 mL of complete medium was added to sustain the culture. The experiment was categorized into four groups: SIRT6 siRNA, NC siRNA, SIRT6 siRNA post-EMPA pretreatment, and NC siRNA post-EMPA pretreatment with Ang II treatment.
Statistical analysis
All experimental data were analyzed using GraphPad Prism 9. Student’s t-test and one-way ANOVA were applied, as appropriate, to assess differences between and among groups. Post-hoc pairwise comparisons were conducted using Dunnett’s t-test or Fisher’s protected least significant difference test. Unless otherwise indicated, the data are presented as the mean ± SD. The threshold for statistical significance was established at p < 0.05.
Results
Observation of the morphology of primary cardiac fibroblasts
Primary cardiac fibroblasts were obtained by isolating the hearts of neonatal mice aged 1–3 days. These cells were carefully cultured in flasks an examined under a microscope after a 6 h incubation period. The observation revealed that the fibroblasts, predominantly exhibited spindle or stellate shapes, indicative of their flattened structures within the culture environment (Supplemental Fig. 1).
Construction of Ang II/TGF-β1-induced myocardial fibrosis model
To determine the optimal dosage of Ang II for inducing myocardial fibrosis in CFs, MTT and Western blot experiments were conducted. Ang II concentrations of 0.01, 0.1, and 1 µM were selected to treat CFs over periods of 24 and 48 h, followed by measuring the optical density in each group. The results indicated that, compared to the control group, there was no significant change in cell proliferation at the 24-hour mark with Ang II treatment. However, whereas a marked increase in proliferation was observed after 48 h at the 1 µM concentration (Fig. 1A,B). Western blot analysis revealed that the signal intensities for TGF-β1, COL1, and COL3 were notably increased in CFs treated with 1 µM Ang II for 48 h (Fig. 1C–C3). Consequently, a 48-hour treatment period with a 1 µM concentration of Ang II was established as optimal for subsequent experiments.
Construction of Ang II/TGF-β1-induced myocardial fibrosis model in vitro. (A, B) The effect of varying Ang II concentrations (0.01, 0.1, 1 µM) on cardiac fibroblasts (CFs) proliferation rates at 24 h and 48 h post-induction. (C-C3) Strip plots illustrating the levels of TGF-β1, COL1, and COL3 proteins following 48 h of Ang II induction at concentrations of 0.01, 0.1, and 1 µM, accompanied by statistical analysis. (D) The influence of different TGF-β1 concentrations (1, 5, 10 ng/mL) on CFs proliferation rates after a 24 h induction period. (E-E3) Strip plots and statistical analysis of TGF-β1, COL1, and COL3 proteins induced by CFs for 24 h with varying TGF-β1 concentrations (1, 5, and 10 ng/mL). Each experiment was conducted three times (n = 3) for reproducibility. *P < 0.05, **P < 0.01, ***P < 0.001 vs. CN group. Of note, CN control. Original blots are presented in Supplementary Information for Western blot Original Data.
To further induce myocardial fibrosis, cells were exposed to TGF-β1 at varying concentrations of 1, 5, and 10 ng/mL for 24 h. MTT assay results demonstrated a significant increase in cell proliferation in the 10 ng/mL TGF-β1 group (Fig. 1D). Western blot findings corroborated this, showing substantial elevation in the signal intensities of TGF-β1, COL1, and COL3 proteins after 24 h of treatment with 10 ng/mL TGF-β1 in CFs (Fig. 1E–E3). Therefore, for the construction of the in vitro model in subsequent experiments, CFs were induced with 10 ng/mL TGF-β1 for 24 h.
Empagliflozin and Dapagliflozin suppress Ang II-induced proliferation and phenotypic transformation of CFs
CFs were exposed to various concentrations of EMPA and DAPA (0.5, 2, 10, 25, and 50 µmol/L) for 24 h to evaluate cell viability in the presence of SGLT2 inhibitors. The findings indicated that concentrations of 0.5, 2, and 10 µM of EMPA and DAPA did not significantly affect the viability of CFs (Fig. 2A, B). However, treatment with EMPA and DAPA notably inhibited the proliferation rate of Ang II-induced cells (Fig. 2C,D). Western blot analysis showed that 10 µM EMPA and DAPA significantly reduced the expression of COL1 and COL3 in Ang II-induced CFs (Fig. 2E,F). Immunofluorescence staining for α-SMA expression revealed that EMPA and DAPA suppressed the differentiation of Ang II-induced fibroblasts (Fig. 2G).
Empagliflozin and Dapagliflozin suppress Ang II-induced proliferation and phenotypic transformation of CFs. (A-B) Effect of EMPA and DAPA on the viability of CFs. (C-D) Effect of EMPA and DAPA pretreatment on the proliferation rate of Ang II-induced CFs. (E-F) Western blot analysis of protein expression levels in CFs following Ang II induction and pretreatment with EMPA/DAPA. (G) Immunofluorescence detection of α-SMA expression in CFs induced by Ang II after pretreatment with 10 μM EMPA/DAPA. Each experiment was conducted three times (n = 3) for reproducibility. *P < 0.05, ***P < 0.001 vs. CN group, #P < 0.05, ##P < 0.01, ###P < 0.001 vs. Ang II group. Of note, CN control, EMPA empagliflozin, DAPA dapagliflozin. Original blots are presented in Supplementary Information for Western blot Original Data.
Subsequently, we investigated the impact of EMPA and DAPA on the proliferation rate of TGF-β1-induced CFs. EMPA and DAPA were observed to significantly inhibit the proliferation of TGF-β1-induced cells, as depicted in Fig. 3A,B. Additionally, 10 µM EMPA and DAPA markedly reduced the expression of COL1 and COL3 in TGF-β1-induced CFs (Fig. 3C,D). Consistent with these findings, immunofluorescence staining for α-SMA expression indicated that EMPA and DAPA inhibited the activation of fibroblasts induced by TGF-β1 (Fig. 3E).
Empagliflozin and Dapagliflozin suppress TGF-β1-induced proliferation and phenotypic transformation of CFs. (A-B) Effect of EMPA and DAPA pretreatment on the proliferation rate of TGF-β1-induced CFs. (C-D) Western blot analysis of protein expression levels in CFs following pretreatment with EMPA/DAPA and subsequent induction by TGF-β1. (E) Immunofluorescence detection of α-SMA expression in CFs induced by TGF-β1 after pretreatment with 10 μM EMPA/DAPA. Each experiment was repeated three times (n = 3). *P < 0.05, ***P < 0.001 vs. CN group, #P < 0.05, ##P < 0.01, ###P < 0.001 vs. TGF-β1 group. Of note, CN control, EMPA empagliflozin, DAPA dapagliflozin. Original blots are presented in Supplementary Information for Western blot Original Data.
Empagliflozin and Dapagliflozin suppresses Ang II/TGF-β1-induced oxidative stress injury in CFs
Previous research has established a strong association between myocardial fibrosis and oxidative stress injury. The fluorescence intensity of ROS, labeled with the DCFH-DA probe, was assessed using fluorescence microscopy and flow cytometry. The data revealed that 10 µM EMPA and DAPA markedly reduced ROS production induced by Ang II/TGF-β1 in CFs, as evidenced in Fig. 4A-D. Additionally, the results showed that compared to the control group, the MDA content was increased and the GSH content was decreased in the Ang II group. However, after 10 µM EMPA/DAPA pretreatment, the MDA content decreased and the GSH content increased. Similar results were observed in the TGF-β1 group (Fig. 4E-H). While Ang II/TGF-β1 treatment significantly upregulated NOX4 protein expression in CFs, pretreatment with 10 µM EMPA and DAPA led to a substantial decrease in NOX4 expression (Fig. 4I-L). These findings indicate that EMPA and DAPA effectively attenuate oxidative stress in CFs triggered by Ang II/TGF-β1.
Empagliflozin and Dapagliflozin suppress Ang II/TGF-β1-induced oxidative stress injury in CFs. (A, B) Fluorescent microscopy to visualize reactive oxygen species (ROS) generation after 10 µM EMPA/DAPA pretreatment, with subsequent quantification of ROS levels. (C-D) Statistical analysis of ROS levels, as measured by flow cytometry, following 10 µM EMPA/DAPA pretreatment. (E-H) Assessment of malondialdehyde (MDA) and glutathione (GSH) activity levels, indicating oxidative stress. (I-L) Western blot analysis to determine the expression of NOX4 protein induced by Ang II/TGF-β1, post 10 µM EMPA/DAPA pretreatment, complemented by statistical graph. Each experiment was conducted three times (n = 3) for reproducibility. *P < 0.05, **P < 0.01, ***P < 0.001 vs. CN group, #P < 0.05, ##P < 0.01, ###P < 0.001 vs. Ang II or TGF-β1 group. Of note, CN control, EMPA empagliflozin, DAPA dapagliflozin. Original blots are presented in Supplementary Information for Western blot Original Data.
Empagliflozin and Dapagliflozin regulate SIRT6 to inhibit Ang II/ TGF-β1-induced proliferation and phenotypic transformation of CFs.
SIRT6 is known to be associated with myocardial fibrosis. To investigate the effect of SGLT2 inhibitors on SIRT6 expression, we examined SIRT6 protein levels using Western blot analysis. The results showed that treatment with 10 µM EMPA and DAPA significantly increased SIRT6 expression compared to the Ang II/TGF-β1 group (Fig. 5A,B).
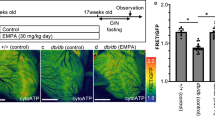
Empagliflozin and Dapagliflozin regulate SIRT6 to inhibit Ang II/ TGF-β1-induced proliferation and phenotypic transformation of CFs. (A, B) Western blot analysis depicting SIRT6 protein expression in CFs subjected to Ang II/TGF-β1 induction following 10 µM EMPA/DAPA pretreatment, accompanied by statistical graphs. (C, D) Utilization of the MTT assay to evaluate the impact on CFs proliferation rate subsequent to transfection. (E, F) Immunofluorescence assay to ascertain the expression level of α-SMA in transfected CFs, complemented by their respective statistical graphs. Each experiment was conducted three times (n = 3) for reproducibility. *P < 0.05, **P < 0.01 vs. CN group, #P<0.05, ##P<0.01 vs. Ang II or TGF-β1 group. Of note, CN control, NC negative control, A Ang II, T TGF-β1, SI-S6 si SIRT6, E empagliflozin, D dapagliflozin. Original blots are presented in Supplementary Information for Western blot Original Data.
To further investigate the role of SIRT6 in the amelioration of myocardial fibrosis by SGLT2 inhibitors, CFs were transfected with SIRT6 siRNA. The cell proliferation rate in the Ang II/TGF-β1 + SIRT6 siRNA group was significantly higher compared to the Ang II/TGF-β1 + NC siRNA group. Additionally, the proliferation rate of cells in the Ang II/TGF-β1 + EMPA/DAPA + SIRT6 siRNA group was significantly higher compared to the Ang II/TGF-β1 + EMPA/DAPA + NC siRNA group (Fig. 5C,D). Moreover, knockdown of SIRT6 increased Ang II/TGF-β1-induced α-SMA expression and also attenuated the protective effects of SGLT2 inhibitors against cell damage (Fig. 5E,F).
Effects of Empagliflozin and Dapagliflozin on oxidative stress in CFs after inhibition of SIRT6 expression
We further explored whether Empagliflozin and Dapagliflozin could egulate ROS levels in each group after transfection. The results indicated that the Ang II/TGF-β1 + SIRT6 siRNA group produced increased levels of ROS compared to the model Ang II/TGF-β1 + NC siRNA group. ROS levels were significantly increased in the Ang II/TGF-β1 + EMPA/DAPA + SIRT6 siRNA group compared to the Ang II/TGF-β1 + EMPA/DAPA + NC siRNA (Fig. 6A,B). Consistently, Western blot analysis showed that the Ang II/TGF-β1 + EMPA/DAPA + SIRT6 siRNA group upregulated the expression of NOX4 protein compared to the Ang II/TGF-β1 + EMPA/DAPA + NC siRNA group (Fig. 6C,D). These results revealed that knockdown of SIRT6 increased Ang II/TGF-β1-induced oxidative stress injury in cells and attenuated the protective effects of SGLT2 inhibitors on myocardial fibrosis.
Effects of Empagliflozin and Dapagliflozin on oxidative stress in CFs after inhibition of SIRT6 expression. (A, B) Flow cytometry assessment and quantification of ROS production in the Ang II/TGF-β1 group following transfection. (C-D) Western blot detection of SIRT6 and NOX4 protein expression in the Ang II/TGF-β1 group post-transfection, with accompanying statistical graphs. Each experiment was conducted three times (n = 3) for reproducibility. *P < 0.05, **P < 0.01, ***P < 0.01, ****P < 0.001. Of note, CN control, NC negative control, A Ang II, T TGF-β1, SI-S6 si SIRT6, E empagliflozin, D dapagliflozin. Original blots are presented in Supplementary Information for Western blot Original Data.
Discussion
In this study, we demonstrated that the SGLT2 inhibitors Empagliflozin (EMPA) and Dapagliflozin (DAPA) protect against Ang II/TGF-β1-mediated proliferation of cardiac fibroblasts (CFs) by upregulating SIRT6 protein expression. This upregulation ameliorates myocardial fibrosis and protects the myocardium by inhibiting oxidative stress.
Myocardial fibrosis is a prevalent pathological alteration seen in various myocardial diseases. It hyper-activates the body’s reparative mechanisms, leading to cardiac remodeling, as outlined by Frangogiannis5. One key inducer of myocardial fibrosis is oxidative stress, characterized by increased production of reactive oxygen species (ROS). This excess ROS disrupts normal cellular functions, damages DNA structures, and precipitates cellular aging, apoptosis, and necrosis15. Most anti-fibrotic treatments currently employed in clinical practice target early lesions, resulting in a lack of effective therapies for advanced cases. SGLT2 inhibitors have gained significant attention as promising therapeutic agents in heart failure management, associated with a reduced risk of sudden death in heart failure patients, demonstrating a protective effect on the cardiovascular system. Despite these benefits, our analysis did not show a reduction in the incidence of arrhythmic events (including both atrial and ventricular arrhythmias) in patients treated with SGLT2 inhibitors16. This suggests that while SGLT2 inhibitors may contribute positively to overall cardiovascular health, their impact on arrhythmias remains unclear and warrants further investigation. Increasing clinical trial data, such as findings from the DAPA-HF and EMPA-TROPISM trials, indicate that SGLT2 inhibitors not only improve heart failure with reduced ejection fraction (HFrEF) but also curb interstitial fibrosis and diminish the expression of inflammatory markers17,18. Experimental studies at the animal and cellular levels further support the cardioprotective effects of SGLT2 inhibitors, including EMPA and DAPA. These agents mitigate oxidative stress induced by diabetic cardiomyopathy, enhance cardiac function, and inhibit myocardial fibrosis19,20. Furthermore, these cardiac benefits may be independent of their glucose-lowering activity18,21.
In our study, Ang II/TGF-β1 was employed to induce myocardial fibrosis. The findings revealed that EMPA and DAPA significantly reduced the expression of COL1, COL3, and α-SMA in CFs, and attenuated the levels of ROS and NOX4 expression compared to the model group. Consequently, EMPA and DAPA can ameliorate the phenotypic transformation associated with myocardial fibrosis, diminish oxidative stress injuries, and confer protection to myocardial tissue.
SIRT6 has been identified as a negative regulator of myocardial fibrosis, inhibiting Ang II and TGF-β1-induced proliferation of CFs and their differentiation into myofibroblasts22. Our experiments corroborated SIRT6’s role in negatively regulating myocardial fibrosis. Prior studies suggest synergistic effects between SIRT6 and another family member, SIRT1, with analogous functions23. SGLT2 inhibitors can directly affect cardiac function through the upregulation of SIRT1 and downstream mediators like PGC-1α and FGF21. The inhibition of AMPK and SIRT1 expression has been shown to diminish the cardioprotective effects of SGLT2 inhibitors24,25. Research by Yumei Ye et al. has demonstrated that Dapagliflozin can attenuate the expression of the Na+/H+ exchanger (NHE-1) through the activation of AMPK26. Furthermore, Empagliflozin exerts cardioprotective effects through the inhibition of the NHE127,28. These findings provide valuable insights into the mechanisms by which Empagliflozin and Dapagliflozin regulate SIRT6 that the inhibition of NHE1 by SGLT2 inhibitors may lead to alterations in intracellular pH and ion homeostasis, which might affect the activity and function of SIRT6. These speculations are predicated on existing research, necessitating additional experimental investigations to elucidate the detailed underlying mechanisms.
Elevated expression of SIRT6 following SGLT2 inhibitor pretreatment has been demonstrated in endothelial cell models under high glucose treatment, also leading to inhibited SGLT2 expression14. However, it remains unreported whether SGLT2 inhibitors ameliorate myocardial fibrosis by modulating SIRT6. Additionally, SIRT6 can confer cardioprotection by attenuating oxidative stress across various cardiovascular disease models. Conversely, inhibiting SIRT6 activity increases ROS production and sensitizes the heart to injury. SIRT6 has been reported to regulate the antioxidant gene transcription activator FOXO3 by activating AMPK, which in turn offers protection from ischemia-reperfusion injury29. FOXO3, a downstream target of SIRT1, modulates oxidative stress and autophagy by influencing FOXO3 expression. FOXO, a nuclear transcription factor, is regulated through post-translational modifications such as phosphorylation and acetylation30. SIRT6 possesses multiple enzymatic activities, including histone deacetylation. In the liver, FOXO3 recruits SIRT6 to downregulate SREBP-2, thus maintaining cholesterol homeostasis31. SIRT6 also impacts antitumor drug resistance by modulating the acetylation of FOXO3a and P53 proteins32. The influence of SGLT2 inhibitors on the SIRT6-FOXO3 signaling pathway in improving myocardial fibrosis remains to be experimentally validated. Our study’s findings suggest that SGLT2 inhibitors, including EMPA and DAPA, can mitigate oxidative stress injury by upregulating SIRT6, inhibiting CF phenotypic transformation and proliferation, reducing ROS levels, and suppressing NOX4 expression (Fig. 7).
A working model of EMPA/DAPA-mediated cardioprotection in Ang II/TGF-β1 induced oxidative stress by inhibiting SIRT6 signaling. This illustration delineates the underlying molecular mechanisms by which SGLT2 inhibitors, Empagliflozin (EMPA) and Dapagliflozin (DAPA), provide protective effects against myocardial fibrosis induced by Angiotensin II (Ang II) and Transforming Growth Factor-β1 (TGF-β1) in neonatal KM mouse primary cardiac fibroblasts. These inhibitors significantly curtail the proliferation of cardiac fibroblasts and reduce collagen expression induced by Ang II/TGF-β1. They also suppress the phenotypic transformation of fibroblasts into myofibroblasts and ameliorate the oxidative stress response. Central to this pathway is SIRT6, the expression of which is upregulated by the SGLT2 inhibitors, leading to the attenuation of myocardial fibrosis and oxidative stress.
This study casts a spotlight on the cardioprotective and antioxidative effects of SGLT2 inhibitors, underscoring their potential in addressing heart health. However, our enthusiasm is tempered by the recognition of certain limitations that require attention. The detailed regulatory mechanisms of these inhibitors and their complex molecular interactions with SIRT6—encompassing both upstream and downstream targets—remain only partially understood. Furthermore, our observations on the attenuation of cardiac fibrosis and oxidative stress by these inhibitors are currently limited to cell-based assays. Looking ahead, it’s imperative that we extend our investigations to in vivo models. Such a transition will unlock a more profound comprehension of the mechanisms by which SGLT2 inhibitors interface with SIRT6, allowing us to explore their therapeutic synergy within the complex tapestry of physiological systems.
Conclusion
SGLT2 inhibitors, a novel category of anti-hyperglycemic agents, have demonstrated cardioprotective effects in addition to their glucose-lowering properties. Accumulating evidence from clinical trials, including DAPA-HF and EMPA-TROPISM, supports the therapeutic potential of SGLT2 inhibitors in heart failure management, particularly for cases with reduced ejection fraction. Our cellular-level findings reinforce the promising outlook for these inhibitors, suggesting that SGLT2 inhibitors could play a crucial roal in the clinical management of heart failure. In summary, this study not only highlights potential targets through which SGLT2 inhibitors may confer cardioprotection but also introduces new strategies and concepts for the clinical treatment of myocardial fibrosis.
Data availability
All relevant data are presented within the paper or supplementary information files.
References
Roger, V. L. Epidemiology of Heart failure: a contemporary perspective. Circ. Res. 128, 1421–1434. https://doi.org/10.1161/CIRCRESAHA.121.318172 (2021).
Wang, Y., Wang, M., Samuel, C. S. & Widdop, R. E. Preclinical rodent models of cardiac fibrosis. Br. J. Pharmacol. 179, 882–899. https://doi.org/10.1111/bph.15450 (2022).
Frangogiannis, N. G. Cardiac fibrosis: cell biological mechanisms, molecular pathways and therapeutic opportunities. Mol. Aspects Med. 65, 70–99. https://doi.org/10.1016/j.mam.2018.07.001 (2019).
Piek, A., Sillje, H. H. W. & de Boer, R. A. The vicious cycle of arrhythmia and myocardial fibrosis. Eur. J. Heart Fail. 21, 492–494. https://doi.org/10.1002/ejhf.1421 (2019).
Frangogiannis, N. G. Cardiac fibrosis. Cardiovasc. Res. 117, 1450–1488. https://doi.org/10.1093/cvr/cvaa324 (2021).
Sadoshima, J., Xu, Y., Slayter, H. S. & Izumo, S. Autocrine release of angiotensin II mediates stretch-induced hypertrophy of cardiac myocytes in vitro. Cell 75, 977–984. https://doi.org/10.1016/0092-8674(93)90541-w (1993).
Shah, A. K., Bhullar, S. K., Elimban, V. & Dhalla, N. S. Oxidative stress as a mechanism for functional alterations in Cardiac Hypertrophy and Heart failure. Antioxid. (Basel). 10. https://doi.org/10.3390/antiox10060931 (2021).
Desmouliere, A., Geinoz, A., Gabbiani, F. & Gabbiani, G. Transforming growth factor-beta 1 induces alpha-smooth muscle actin expression in granulation tissue myofibroblasts and in quiescent and growing cultured fibroblasts. J. Cell. Biol. 122, 103–111. https://doi.org/10.1083/jcb.122.1.103 (1993).
Zhao, W., Zhao, T., Chen, Y., Ahokas, R. A. & Sun, Y. Oxidative stress mediates cardiac fibrosis by enhancing transforming growth factor-beta1 in hypertensive rats. Mol. Cell. Biochem. 317, 43–50. https://doi.org/10.1007/s11010-008-9803-8 (2008).
Lee, T. M., Chang, N. C. & Lin, S. Z. Dapagliflozin, a selective SGLT2 inhibitor, attenuated cardiac fibrosis by regulating the macrophage polarization via STAT3 signaling in infarcted rat hearts. Free Radic Biol. Med. 104, 298–310. https://doi.org/10.1016/j.freeradbiomed.2017.01.035 (2017).
Kolijn, D. et al. Empagliflozin improves endothelial and cardiomyocyte function in human heart failure with preserved ejection fraction via reduced pro-inflammatory-oxidative pathways and protein kinase galpha oxidation. Cardiovasc. Res. 117, 495–507. https://doi.org/10.1093/cvr/cvaa123 (2021).
Tian, K. et al. Sirtuin-6 inhibits cardiac fibroblasts differentiation into myofibroblasts via inactivation of nuclear factor kappaB signaling. Transl Res. 165, 374–386. https://doi.org/10.1016/j.trsl.2014.08.008 (2015).
Zeng, Z. et al. Qishen granule attenuates cardiac fibrosis by regulating TGF-beta /Smad3 and GSK-3beta pathway. Phytomedicine 62, 152949. https://doi.org/10.1016/j.phymed.2019.152949 (2019).
D’Onofrio, N. et al. Sodium-glucose co-transporter2 expression and inflammatory activity in diabetic atherosclerotic plaques: effects of sodium-glucose co-transporter2 inhibitor treatment. Mol. Metab. 54, 101337. https://doi.org/10.1016/j.molmet.2021.101337 (2021).
Sack, M. N., Fyhrquist, F. Y., Saijonmaa, O. J., Fuster, V. & Kovacic, J. C. Basic biology of oxidative stress and the cardiovascular system: part 1 of a 3-Part series. J. Am. Coll. Cardiol. 70, 196–211. https://doi.org/10.1016/j.jacc.2017.05.034 (2017).
Oates, C. P. et al. SGLT2 inhibitors reduce sudden cardiac death risk in heart failure: Meta-analysis of randomized clinical trials. J. Cardiovasc. Electrophysiol. 34, 1277–1285. https://doi.org/10.1111/jce.15894 (2023).
McMurray, J. J. V. et al. A trial to evaluate the effect of the sodium-glucose co-transporter 2 inhibitor dapagliflozin on morbidity and mortality in patients with heart failure and reduced left ventricular ejection fraction (DAPA-HF). Eur. J. Heart Fail. 21, 665–675. https://doi.org/10.1002/ejhf.1432 (2019).
Requena-Ibanez, J. A. et al. Mechanistic insights of Empagliflozin in nondiabetic patients with HFrEF: from the EMPA-TROPISM study. JACC Heart Fail. 9, 578–589. https://doi.org/10.1016/j.jchf.2021.04.014 (2021).
Li, C. et al. SGLT2 inhibition with empagliflozin attenuates myocardial oxidative stress and fibrosis in diabetic mice heart. Cardiovasc. Diabetol. 18, 15. https://doi.org/10.1186/s12933-019-0816-2 (2019).
Xing, Y. J. et al. A SGLT2 inhibitor Dapagliflozin alleviates Diabetic Cardiomyopathy by suppressing high glucose-Induced oxidative stress in vivo and in vitro. Front. Pharmacol. 12, 708177. https://doi.org/10.3389/fphar.2021.708177 (2021).
Santos-Gallego, C. G. et al. Empagliflozin ameliorates diastolic dysfunction and left ventricular Fibrosis/Stiffness in nondiabetic heart failure: a multimodality study. JACC Cardiovasc. Imaging. 14, 393–407. https://doi.org/10.1016/j.jcmg.2020.07.042 (2021).
Olson, E. R., Naugle, J. E., Zhang, X., Bomser, J. A. & Meszaros, J. G. Inhibition of cardiac fibroblast proliferation and myofibroblast differentiation by resveratrol. Am. J. Physiol. Heart Circ. Physiol. 288, H1131–1138. https://doi.org/10.1152/ajpheart.00763.2004 (2005).
Meng, F. et al. Synergy between SIRT1 and SIRT6 helps recognize DNA breaks and potentiates the DNA damage response and repair in humans and mice. Elife 9 https://doi.org/10.7554/eLife.55828 (2020).
Packer, M. Cardioprotective effects of Sirtuin-1 and its downstream effectors: potential role in mediating the heart failure benefits of SGLT2 (sodium-Glucose cotransporter 2) inhibitors. Circ. Heart Fail. 13, e007197. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007197 (2020).
Packer, M. Critical reanalysis of the mechanisms underlying the cardiorenal benefits of SGLT2 inhibitors and reaffirmation of the nutrient deprivation signaling/autophagy hypothesis. Circulation 146, 1383–1405. https://doi.org/10.1161/CIRCULATIONAHA.122.061732 (2022).
Ye, Y., Jia, X., Bajaj, M. & Birnbaum, Y. Dapagliflozin attenuates na(+)/H(+) Exchanger-1 in Cardiofibroblasts via AMPK activation. Cardiovasc. Drugs Ther. 32, 553–558. https://doi.org/10.1007/s10557-018-6837-3 (2018).
Baartscheer, A. et al. Empagliflozin decreases myocardial cytoplasmic na(+) through inhibition of the cardiac na(+)/H(+) exchanger in rats and rabbits. Diabetologia 60, 568–573. https://doi.org/10.1007/s00125-016-4134-x (2017).
Chen, S. et al. Empagliflozin mitigates cardiac hypertrophy through cardiac RSK/NHE-1 inhibition. Biomed. Pharmacother. 174, 116477. https://doi.org/10.1016/j.biopha.2024.116477 (2024).
Wang, X. X. et al. SIRT6 protects cardiomyocytes against ischemia/reperfusion injury by augmenting FoxO3alpha-dependent antioxidant defense mechanisms. Basic. Res. Cardiol. 111, 13. https://doi.org/10.1007/s00395-016-0531-z (2016).
Kodani, N. & Nakae, J. Tissue-specific metabolic regulation of FOXO-Binding protein: FOXO does not act alone. Cells 9 https://doi.org/10.3390/cells9030702 (2020).
Tao, R., Xiong, X., DePinho, R. A., Deng, C. X. & Dong, X. C. Hepatic SREBP-2 and cholesterol biosynthesis are regulated by FoxO3 and Sirt6. J. Lipid Res. 54, 2745–2753. https://doi.org/10.1194/jlr.M039339 (2013).
Khongkow, M. et al. SIRT6 modulates paclitaxel and epirubicin resistance and survival in breast cancer. Carcinogenesis 34, 1476–1486. https://doi.org/10.1093/carcin/bgt098 (2013).
Acknowledgements
This project was supported by the National Natural Science Foundation of China (82204387) and Dalian Science and Technology Innovation Fund (2023RQ010) to DW; Dalian Medical Science Research Project (22Z12006) and Dalian Key Field Innovation Team Project (2021RT14) to HYL.
Author information
Authors and Affiliations
Contributions
HXM: Conceptualization, Methodology, Investigation, Writing – original draft. KW: Conceptualization, Methodology, Investigation, Writing – review & editing. FHD: Investigation, Writing – review & editing. BKC: Investigation, Writing – review & editing. DW: Conceptualization, Methodology, Investigation, Writing – review & editing, Project administration and Funding acquisition. HYL: Investigation, Writing – review & editing, Project administration and Funding acquisition. All authors have read and approved the final manuscript, and therefore, have full access to all the data in the study and take responsibility for the integrity and security of the data.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, Hx., Wu, K., Dong, Fh. et al. Effects of Empagliflozin and Dapagliflozin in alleviating cardiac fibrosis through SIRT6-mediated oxidative stress reduction. Sci Rep 14, 30764 (2024). https://doi.org/10.1038/s41598-024-80829-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-80829-w
Keywords
This article is cited by
-
Impact of sodium–glucose transport protein-2 (SGLT2) inhibitors on the inflammasome pathway in acute myocardial infarction in type 2 diabetes mellitus: a comprehensive review
Cardiovascular Diabetology (2025)
-
Impact of dapagliflozin administration on remodeling marker and clinical outcomes of stemi patients with diabetes mellitus: a controlled clinical trial
Future Journal of Pharmaceutical Sciences (2025)
-
Sirtuins as Endogenous Regulators of Cardiac Fibrosis: A Current Perspective
Cardiovascular Toxicology (2025)