Abstract
The role of pre-treatment HBV DNA levels on the prognosis of hepatitis B virus-related decompensated cirrhosis is unclear. This study investigated the effects of pre-treatment HBV DNA and other determinants on short-term and long-term survival of chronic hepatitis B (CHB) patients with decompensated cirrhosis. A total of 278 cirrhotic decompensated CHB patients treated with entecavir or tenofovir disoproxil fumarate were retrospectively enrolled. Cox regression models were used to analyze factors associated with all-cause mortality. The median follow-up time was 17 months (IQR2.17–58.94), during which 132 patients (47.4%) either died or underwent liver transplantation. The cumulative incidence of all-cause mortality was 16%, 29%, 34%, 39%, and 51% at the 1-month, 3-month, 6-month, 1-year, and 5-year follow-ups, respectively. Risk factors associated with 3-month all-cause mortality were age, presence of ascites and hepatic encephalopathy, baseline hepatitis flares, pre-treatment HBV DNA levels, and MELD scores. In the subgroup analysis, for 3-month all-cause mortality, significant associations of age, baseline hepatitis flares, and MELD scores with pre-treatment HBV DNA levels were observed (p for interaction were 0.005, 0.032, and 0.030, respectively). Risk factors associated with 5-year all-cause mortality were age, the presence of ascites and hepatic encephalopathy, and MELD scores. Liver functional reserve and age played a critical role in the prognosis of CHB patients with decompensated cirrhosis. Pre-treatment HBV DNA levels had an impact on short-term all-cause mortality, but not on long-term all-cause mortality.
Similar content being viewed by others
Introduction
Hepatitis B virus ((HBV) infection poses a major public health problem, with an estimated approximately 296 million infected individuals worldwide1. HBV-related hepatic complications, including hepatic decompensation, liver cirrhosis (LC), and hepatocellular carcinoma (HCC) occurred in 15%-40% of chronic hepatitis B (CHB) patients2,3. An estimated 820,000 people died from HBV-related disease in 2019, with deaths related to HBV-related LC and HCC contributing to 52% and 38%, respectively1,4.
There are two natural progressions of hepatic decompensated cirrhosis from compensated cirrhosis. One is an acute episode of preceding hepatitis B flares, while the other follows a gradual deterioration pattern leading to end-stage liver conditions5,6. Patients with decompensated cirrhosis generally have a worse prognosis compared to those with compensated cirrhosis. The 1-year, 2-year, and 3-year cumulative survival rates were 100% and 81.2% , 98.5% and 75.6%, and 98.5% and 69.5% in patients with compensated cirrhosis and decompensated cirrhosis, respectively7. The 5-year survival rate without liver transplantation drops to 14% -35% in decompensated cirrhotic CHB patients6. Patients with decompensated cirrhosis have a higher risk of disease progression to acute on-chronic liver failure (ACLF), which is characterized by hepatic and extrahepatic organ failure(s)8,9. The 28-day transplant-free mortality rates in HBV-related decompensated cirrhotic patients and cirrhotic HBV-ACLF patients were 4.5% and 52.1%, respectively, with corresponding 90-day mortality rates of 7.1% and 69.7%10.
Thus, international hepatitis B virus associations recommend immediate treatment with antiviral agents for CHB patients with decompensated cirrhosis to prevent deterioration of hepatic decompensation11,12,13. The role of pre-treatment HBV DNA levels in the prognosis of HBV-related decompensated cirrhosis remain unclear. This study aimed to investigate the impact of pre-treatment HBV DNA levels and identify factors during hepatic decompensation that could determine clinical outcomes in decompensated cirrhotic CHB patients treated with entecavir (ETV) or tenofovir (TDF).
Materials and methods
Patients and study design
This study population consisted of patients from an observational retrospective cohort of decompensated cirrhotic CHB patients treated with ETV or TDF between June 2009 and October 2022 in Taichung Veterans General Hospital. Hepatic decompensation was defined as an increase in serum total bilirubin (T-Bil) level greater than 2 mg/dL, prolongation of prothrombin time (PT) ≥ 3 s, or an international normalized ratio (INR) > 1.5 with or without the presence of ascites and /or hepatic encephalopathy14. The definition of CHB was hepatitis B surface antigen seropositivity for 6 months. The diagnosis of cirrhosis was based on the characteristic findings from radiological tests (such as a shrunken liver, surface nodular pattern or splenomegaly) of ultrasonography, computed tomography or magnetic resonance imaging. We excluded patients aged younger than 18 years old, those with current coinfection with the hepatitis C virus, or human immunodeficiency virus, or a history of hepatic tumor or non-hepatic tumor.
Ethical declaration
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board and Ethics Committee of Taichung Veterans General Hospital (IRB: CE-18232A) and the Ethics Committee waived informed consent.
Assessment and follow-up evaluation
The baseline date was defined as the date when decompensated status was noted. Prescription of TDF or ETV was initiated upon recognition of the decompensated status. Patients’ baseline characteristics were assessed and laboratory tests were conducted, including age, sex, liver biochemical test, creatinine, serum HBV DNA, hepatitis B e antigen (HBeAg), and model for end-stage liver disease (MELD) scores. MELD scores were calculated at baseline according to the following equations: (0.378 * loge(bilirubin)) + (1.120*loge(INR)) + (0.957*loge(creatinine)) + 0.643 ) * 10 (if hemodialysis, value for creatinine is automatically set to 4.0)15. ALT normalization was defined as values within the upper limit of normal (ULN) and was set at 50 U/L for men and 35U/L for women according to the local laboratory reference. The definition of hepatitis flares was a rise of ALT levels to > 5 times ULN.
Patients with hepatic decompensation were followed-up closely every 1–2 weeks during the first 3 months and then every 3 months. The primary end-point was 3-month all-cause mortality and the secondary end-point was 5-year all-cause mortality. Patients who died or underwent liver transplantation were included in all-cause mortality categories during the period of follow-up.
Laboratory methods
HBV DNA levels were measured using a real-time PCR assay and Roche CobasTaqMan HBV Test, with a lower limit of quantification of 20 IU/mL (Roche Diagnostics, Branchburg, USA). The status of HBsAg was determined using a qualitative Architect assay (Abbott Laboratories, Chicago, Illinois, USA). Qualitative HBeAg was determined by commercial enzyme immunoassays (Roche Diagnostics, Mannheim, Germany).
Statistical analysis
Categorical variables were expressed as number of cases and compared by the Chi-squared test or Fisher’s exact test. Continuous variables were expressed as median ± interquartile range (IQR) and compared by the Mann–Whitney U test. The cumulative incidence of 3-month and 5-year all-cause mortality were calculated using the Kaplan–Meier method and compared using the log-rank test. Cox proportional hazards models were employed to assess factors associated with 3-month and 5-year all-cause mortality, adjusting for all independent variables with a p value < 0.05, which was considered statistically significant in the univariate analyses. Sensitivity analyses were conducted to explore the associations of pretreatment HBV DNA levels with 3-month and 5-year all-cause mortality. Statistical tests were performed using SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA).
Results
Patients’ characteristics
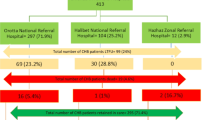
Figure 1 shows that a total of 278 decompensated cirrhotic CHB patients treated with ETV or TDF were included in this study. The median follow-up duration was 17 months (IQR2.17–58.94). Of these patients, with median age of 56.22 years (IQR 47.39–64.62), 223 (80.20%) were male and 37 (13.30%) were HBeAg-positive. Specifically, 230 patients (82.70%) received ETV, while 48 (17.30%) were treated with TDF (Table 1). Patients who died or underwent liver transplant had a higher percentage of the presence of ascites and hepatic encephalopathy (75.80% vs. 43.20%, p < 0.001; 22.70% vs. 3.40%, p < 0.001), lower albumin levels (2.8 g/dL vs. 3.1 g/dL, p < 0.001), higher bilirubin levels (7.85 mg/dl vs. 3.20 mg/dl, p < 0.001), prolonged prothrombin time (17.35 s vs. 13.7 s, p < 0.001), and high MELD scores (22.58 vs. 14.92, p < 0.001) compared to those who survived.
Factors associated with 3-month all-cause mortality
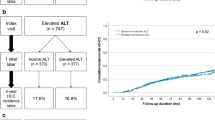
In total, 80 patients (28.80%) died or underwent liver transplantation, including 15 treated with TDF and 65 with ETV during the first 3 months. The cumulative incidence of all-cause mortality was 16%, 29%, 34%, 39% and 51% at the 1-month, 3-month, 6-month, 1-year, and 5-year follow-ups, respectively (Fig. 2A and 2B).
Factors associated with all-cause mortality within 3 months were analyzed by Cox regression analysis, and the choice of ETV or TDF was not found to be associated with 3-month all-cause mortality. In the multivariate Cox regression analysis, significant risk factors for all-cause mortality within 3 months included older age (hazard ratio [HR] = 1.037, 95%CI:1.014–1.061, p = 0.001), presence of ascites and hepatic encephalopathy (HR = 2.972, 95%CI:1.541–5.731, p = 0.001; and HR = 3.307, 95%CI:1.767–6.188, p < 0.001), ALT≧5 × ULN (HR = 2.094, 95%CI:1.088–4.030, p = 0.027), MELD scores (HR = 1.101, 95%CI: 1.058–1.146, p < 0.001), and pre-treatment HBV DNA levels (HR = 1.147, 95%CI: 1.004–1.312, p = 0.044) (Table 2).
In this study, 189 enrolled patients met APASL ACLF criteria9. Significant risk factors for 3-month all-cause mortality in patients who fulfilled the APASL ACLF criteria are detailed in Supplementary Table 1 (Table S1).
Hazard ratios for all-cause mortality within 3 months for patients across different patient subgroups based on levels of pre-treatment HBV DNA are shown in Fig. 3. The risk of 3-month all-cause mortality was significantly higher in patients with pre-treatment HBV DNA levels ≧ 4 Log10 IU/mL compared to those with pre-treatment HBV DNA levels < 4 Log10 IU/mL (HR = 2.354; 95%CI: 1.322–4.192; p = 0.004). Moreover, we observed significant interactions between pre-treatment HBV DNA levels with age, baseline hepatitis flares, and MELD score (p for interaction = 0.005, 0.032, and 0.030, respectively). The effect of pre-treatment HBV DNA levels ≧ 4 Log10 IU/mL was more pronounced in patients under 60 years of age, without baseline hepatitis flares, and those with MELD score ≧20 compared to their counterparts.
Sensitivity analyses for 3-months all-cause mortality for HBV-related decompensated cirrhotic patients with pre-treatment HBV DNA < 4 and ≧ 4 log10 IU/mL. HBeAg, hepatitis B e antigen ; ALT, alanine aminotransferase; MELD, Model for End-Stage Liver Disease; NUC, Nucleoside/nucleotide analogs; TDF, Tenofovir disoproxil fumarate; ETV, entecavir.
Figure 4 illustrates the combined effect of HBV DNA ≧4 Log10 IU/mL and MELD scores ≧ 20 on 3-month all-cause mortality, showing an adjusted HR of 2.795 (95% CI: 1.094–7.140, p = 0.032).
Factors associated with 5-year all-cause mortality
A total of 132 patients (47.5%) either died or underwent liver transplantation, including 20 treated with TDF and 112 with ETV over a period of 5 years. Among the 278 enrolled patients, 143 of them regained liver compensation, defined as having serum bilirubin levels < 2 mg/dL and an INR prolongation of < 3 s. Factors associated with 5-year all-cause mortality were analyzed using Cox regression analysis, and the choice of ETV or TDF was not associated with 5-year all-cause mortality. In the multivariate Cox regression analysis, significant risk factors for 5-year all-cause mortality were older age (HR = 1.021, 95% CI: 1.004–1.039, p = 0.017), presence of ascites and hepatic encephalopathy (HR = 2.519, 95% CI: 1.538–4.125, p < 0.001; and HR = 3.634, 95% CI: 2.167–6.094, p < 0.001), and MELD scores (HR = 1.071, 95% CI: 1.041–1.102, p < 0.001) (Table 3).
There were no significant differences or interactions in hazard ratios for 5-year all-cause mortality among patients with varying levels of pre-treatment HBV DNA across different subgroups. Additional details can be found in Supplementary Fig. 1.
Discussion
The cumulative incidence of all-cause mortality was 16%, 19%, 34%, 39%, and 51% at the 1-month, 3-month, 6-month, 1-year, and 5-year follow-ups, respectively. ETV or TDF was not an independent factor of the prognosis in CHB patients with decompensated cirrhosis regardless of whether assessing 3-month or 5-year all-cause mortality. Age, presence of ascites and hepatic encephalopathy, and higher MELD scores were predictors of both 3-month and 5-year all-cause mortality. Higher levels of HBV DNA and hepatitis flares at baseline were also independent predictors of 3-month all-cause mortality, but not 5-year all-cause mortality.
In concordance with findings from other studies, our study demonstrated that the choice of antiviral therapy was not an independent factor of all-cause mortality in CHB -patients with decompensated cirrhosis14,16. The severity and prognosis of decompensated cirrhosis has been associated with pre-existing liver disease and baseline liver function reserve. TCF-Yip et al. reported younger age, as well as lower baseline MELD scores and ALT levels were predictors of 6-month transplantation-free survival in CHB cirrhotic patients with baseline MELD scores≧1517. In a Taiwan 8-year cohort study, the presence of hepatic encephalopathy and baseline MELD score were independent predictors of both 3-month and 8-year liver-related morality in decompensated CHB patients14. In our study, older age, the presence of ascites and hepatic encephalopathy, and higher baseline MELD scores were predictors of both 3-month and 5-year all-cause mortality.
The key finding in the present study is that higher levels of HBV DNA and hepatitis flares at baseline were also predictors of 3-month all-cause mortality, but not 5-year all-cause mortality. Ying Zhu report that HBV reactivation exhibited a higher risk of 90-day mortality in cirrhotic patients compared to those without cirrhosis18. This could be explained by the fact that HBV-triggered flares could cause hepatocytes damage induced by interactions between a vigorous host immune response and a high viral load. Such conditions increase the risk of developing liver failure, leading to a higher short-term mortality rate in cirrhotic CHB patients19. In sensitivity analyses, the effects of pre-treatment HBV DNA ≧4 Log10 IU/mL and 3-month all-cause mortality were more pronounced in patients under 60 years of age and in those without baseline hepatitis flares compared to their counterparts. A possible explanation for these findings is the prolonged presence of high HBV DNA levels in serum, which can cause more severe liver fibrosis and accelerate the progressive deterioration of cirrhosis in younger cirrhotic decompensated CHB patients without high levels of ALT20,21. Furthermore, ETV and TDF, the first-line treatment options for CHB, achieved undetectable HBV DNA in 82.9% and 71.4% of treatment-naïve CHB patients, respectively, after one year of antiviral therapy22,23. This implies that due to their high potency and low resistance of TDF and ETV against HBV replication, long-term antiviral therapy could lead to sustained viral suppression, stabilizing liver function over time and improving long-term survival12,16. These factors help explain why baseline HBV DNA had less impact on 5-year all-cause mortality.
Our findings have clinical implications as we identified risk factors associated with all-cause mortality in patients with hepatitis B virus-related decompensated cirrhosis. The initial 3–6 months following the diagnosis of decompensation status appear to be crucial for determining whether liver reserve can recover or stabilize for patients with hepatitis B virus-related decompensated cirrhosis5. Our study observed a sharp rapid increase in all-cause mortality within the first 3-months, with independent factors, including age, baseline HBV DNA levels, ALT levels, MELD scores, the presence of ascites and hepatic encephalopathy, contributing to 3-month all-cause mortality. Interestingly, baseline HBV DNA levels were found to be associated with short-term all-cause mortality, but not long-term all-cause mortality, suggesting a critical role in initial disease progression. The MELD score, validated as one of the criteria for allocation of liver transplantation in patients with end-stage liver disease24, also demonstrated that the combination of MELD score ≧20 and HBV DNA ≧4 log10 IU/mL contributed to a joint effect in the 3-month all-cause mortality. This underscores the heightened risk of short-term all-cause mortality for HBV-mediated liver decompensation and liver failure in patients with poor liver reserve at baseline. Additionally, our findings indicate that aggressive treatment with antiviral therapy to suppress HBV viral replication in CHB patients with cirrhosis is crucial to reduce the HBV-triggered persistent damage in liver reserve. Antiviral therapy to achieve HBV suppression is essential to improve long-term survival if patients can recover from the crisis of acute liver decompensation or liver failure16. Clinicians can potentially use these insights to predict unfavorable outcomes and determine the likelihood of the need for liver transplantation, as the process of hepatic decompensation could be irreversible despite antiviral therapy for suppressing HBV viral load.
There were several limitations in this study. First, this was a retrospective study with an insufficient number to perform propensity score matching, which could reduce baseline confounding variables between patients treated with ETV and TDF. Second, data on HBV genotype were unavailable, and different HBV genotypes (such as genotype B and C, which are strongly associated with development of cirrhosis and HCC25) could influence disease progression differently. Therefore, we did not adequately elucidate the impact of HBV genotype on the outcomes in decompensated cirrhotic CHB patients. Third, a liver biopsy was not performed for all enrolled patients due to coagulopathy to confirm the severity of cirrhotic status. Fibroscan and elastography were also not available before decompensated status and during the period of follow-up. Baseline non-invasive laboratory-based tests (e.g., Fibrosis-4 Index, aspartate aminotransferase-to-platelet ratio index) might be affected in the setting of acute decompensated status initially. The diagnosis of cirrhosis was based on the discretion of gastroenterologists interpreting radiological findings, which may not always be sufficient for an accurate diagnosis. Additionally, it is challenging to confirm the presence of hepatic steatosis without liver biopsies in our study. Forth, data on Serum GGT were not available for all patients. Therefore, we did not adequately elucidate the impact of GGT on the outcomes in decompensated cirrhotic CHB patients. Fifth, details regarding daily alcohol consumption were not always documented in our retrospective study, so we were unable to confirm whether patients consumed alcohol (> 20 g/day) or not. Finally, in analyzing risk factors for mortality among our participants, we did not account for non-liver related mortality as a competing risk in assessing the association of liver-related mortality and independent variables. Instead, we used all-cause mortality as the study endpoint because the number of cases of non-liver related mortality was small.
In conclusion, hepatic reserve and age were associated with both 3-month and 5-year all-cause mortality in decompensated cirrhotic CHB patients. Additionally, higher levels of baseline HBV DNA and hepatitis flares were predictors of 3-month, but not 5-year all-cause mortality, suggesting that flares mediated by high HBV viral load play a crucial role in the short-term survival of CHB patients with decompensated cirrhosis.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Jeng, W. J., Papatheodoridis, G. V. & Lok, A. S. F. Hepatitis B. Lancet 401(10381), 1039–1052 (2023).
Lai, C. L. & Yuen, M. F. The natural history and treatment of chronic hepatitis B: a critical evaluation of standard treatment criteria and end points. Ann. Intern. Med. 147(1), 58–61 (2007).
Suzuki, T. et al. Development of hepatocellular carcinoma from various phases of chronic hepatitis B virus infection. PLoS One. 16(12), e0261878 (2021).
World Health Organization. Hepatitis B. 2023; https://www.who.int/news-room/fact-sheets/detail/hepatitis-b. Accessed Aug 10, 2023.
Chang, M. L., Cheng, J. S., Chien, R. N. & Liaw, Y. F. Hepatitis flares are associated with better outcomes than no flare in patients with decompensated cirrhosis and chronic hepatitis B virus infection. Clin. Gastroenterol. Hepatol. 18(9), 2064-2072.e2062 (2020).
Peng, C. Y., Chien, R. N. & Liaw, Y. F. Hepatitis B virus-related decompensated liver cirrhosis: benefits of antiviral therapy. J. Hepatol. 57(2), 442–450 (2012).
Lin, C. L., Tseng, K. C., Chen, K. Y., Liao, L. Y. & Kao, J. H. Factors predicting outcomes of hepatitis B-related cirrhosis patients with long-term antiviral therapy. J. Formos. Med. Assoc. 119(10), 1483–1489 (2020).
Shalimar, et al. Acute on chronic liver failure because of acute hepatic insults: Etiologies, course, extrahepatic organ failure and predictors of mortality. J. Gastroenterol. Hepatol. 31(4), 856–864 (2016).
Sarin, S. K. et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol. Int. 13(4), 353–390 (2019).
Wu, T. et al. Development of diagnostic criteria and a prognostic score for hepatitis B virus-related acute-on-chronic liver failure. Gut. 67(12), 2181–2191 (2018).
Sarin, S. K. et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol. Int. 10(1), 1–98 (2016).
Lampertico, P. et al. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J. Hepatol. 67(2), 370–398 (2017).
Terrault, N. A. et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 67(4), 1560–1599 (2018).
Lee, K. C., Cheng, J. S., Chang, M. L., Chien, R. N. & Liaw, Y. F. Comparable outcomes of decompensated chronic hepatitis B patients treated with entecavir or tenofovir: an 8-year cohort study. Hepatol. Int. 16(4), 799–806 (2022).
Huo, T. I. et al. Evaluation of the increase in model for end-stage liver disease (DeltaMELD) score over time as a prognostic predictor in patients with advanced cirrhosis: risk factor analysis and comparison with initial MELD and Child-Turcotte-Pugh score. J. Hepatol. 42(6), 826–832 (2005).
Jang, J. W. et al. Effects of virologic response to treatment on short- and long-term outcomes of patients with chronic hepatitis B virus infection and decompensated cirrhosis. Clin. Gastroenterol. Hepatol. 16(12), 1954-1963.e1953 (2018).
Yip, T. C. et al. Factors associated with improvement in MELD score after antiviral treatment in patients with chronic hepatitis B. J. Gastroenterol. Hepatol. 35(9), 1610–1618 (2020).
Zhu, Y. et al. Hepatitis b virus reactivation increased the risk of developing hepatic failure and mortality in cirrhosis with acute exacerbation. Front. Microbiol. 13, 910549 (2022).
Liang, J. et al. Hepatitis B-related acute-on-chronic liver failure induced by hepatotropic viral insult is associated with worse prognosis than that induced by non-virus insult. BMC Infect. Dis. 21(1), 1273 (2021).
Iloeje, U. H. et al. Predicting cirrhosis risk based on the level of circulating hepatitis B viral load. Gastroenterology. 130(3), 678–686 (2006).
Kumar, M. et al. Virologic and histologic features of chronic hepatitis B virus-infected asymptomatic patients with persistently normal ALT. Gastroenterology. 134(5), 1376–1384 (2008).
Jung, S. K. et al. Tenofovir disoproxil fumarate monotherapy for nucleos(t)ide analogue-naïve and nucleos(t)ide analogue-experienced chronic hepatitis B patients. Clin. Mol. Hepatol. 21(1), 41–48 (2015).
Seto, W. K. et al. Changes of HBsAg and HBV DNA levels in Chinese chronic hepatitis B patients after 5 years of entecavir treatment. J. Gastroenterol. Hepatol. 29(5), 1028–1034 (2014).
Karvellas, C. J. et al. AASLD Practice guidance on Acute-on-chronic liver failure and the management of critically Ill patients with cirrhosis. Hepatology. https://doi.org/10.1097/HEP.0000000000000671 (2023).
Lin, C. L. & Kao, J. H. The clinical implications of hepatitis B virus genotype: Recent advances. J. Gastroenterol. Hepatol. 26(Suppl 1), 123–130 (2011).
Acknowledgements
We thank the Biostatistics Task Force of Taichung Veterans General Hospital for their statistical assistance.
Author information
Authors and Affiliations
Contributions
Conceptualization: Y.-J.H. and T.-C.L.; methodology: Y.-J.H., T.-C.L. and C.-H.C. (Cheng-Hsu Chen); formal analysis: Y.-J.H. and T.-C.L.; resources: Y.-J.H., C.-H.C. (Chung-Hsin Chang), S.-C.L., Y.-C.P., S.-W.L. and T.-Y.L.; investigation: Y.-J.H. and T.-C.L.; writing—original draft: Y.-J.H., T.-C.L.; writing—review and editing: C.-H.C. (Cheng-Hsu Chen), C.-H.C. (Chung-Hsin Chang), S.-C.L., Y.-C.P., S.-W.L., T.-Y.L., J.-S.W., T.-C.L.; supervision: T.-C.L. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board and Ethics Committee of Taichung Veterans General Hospital (IRB: CE-18232A) and the Ethics Committee waived informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, YJ., Wang, JS., Chen, CH. et al. Determinants of outcomes in patients with hepatitis B virus-decompensated cirrhosis. Sci Rep 15, 562 (2025). https://doi.org/10.1038/s41598-024-84413-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84413-0