Abstract
This observational investigation aimed to explore potential risk factors for anemia in pregnancy. Firstly, a cross-sectional study was conducted, encompassing a review of clinical data of 43,201 pregnant women admitted to the Hainan Women and Children’s Medical Center between January 2017 and December 2020. Comparison between women with and without anemia in pregnancy revealed significant differences between the two groups concerning age, gestational diabetes, hypothyroidism, hyperthyroidism, chronic hepatitis B virus infection, syphilis infection, and human immunodeficiency virus infection. Multivariable logistic regression analysis showed that chronic hepatitis B virus infection was significantly associated with anemia during pregnancy (AOR 2.97, 95% CI 2.57–3.44, p < 0.0001). Subsequently, a retrospective cohort comprising 86 cases with chronic hepatitis B virus infection and 129 control subjects recruited from the Hainan Women and Children’s Medical Center from November 2021 and January 2023 was examined. Results of the examination revealed a corroborative association between chronic hepatitis B virus infection and anemia in pregnancy (OR 2.13, 95% CI 1.20–3.79, p = 0.0092), particularly manifesting in the third trimester of gestation. Further analysis unveiled distinctive hematological alterations among cases with chronic hepatitis B virus infection, characterized by diminished erythrocyte size and reduced levels of corpuscular hemoglobin. Collectively, these findings underscore a positive association of chronic hepatitis B virus infection with anemia during pregnancy.
Similar content being viewed by others
Introduction
Anemia in pregnancy, characterized by a hemoglobin (Hb) concentration below 11 g/dl in pregnant women, affects nearly 50% of pregnancies on a global scale1. Its association with maternal morbidity, mortality, and adverse fetal outcomes underscores its status as a significant public health concern worldwide, particularly prevalent in developing nations1,2. The etiology of pregnancy-related anemia is multifaceted, with iron deficiency representing a primary causal factor alongside with various other contributors including malnutrition, thalassemia, and infectious diseases such as hookworm infection or malaria3,4,5,6,7. In this observational study, we sought to identify potential risk factors associated with anemia during pregnancy. To achieve this, we conducted both a cross-sectional analysis and a retrospective cohort study, with anemia in pregnancy defined as the primary outcome variable.
Methods
Subjects and data collection
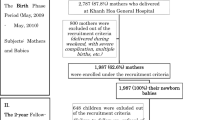
The cross-sectional study encompassed a review of demographic and clinical records pertaining to pregnant women admitted to the Hainan Women and Children’s Medical Center (HNWCMC) between January 2017 and December 2020. Exclusion criteria were applied to eliminate patients under 18 years old, cases of stillbirth, and individuals admitted for reasons other than delivery. Anonymized data including age, diagnosis of gestational diabetes, anemia in pregnancy, hypothyroidism, hyperthyroidism, chronic hepatitis B virus (HBV) infection, syphilis infection, and human immunodeficiency virus (HIV) infection, were extracted from the electronic medical records system. All patients were well characterized for all abovementioned clinical and demographic data. To identify factors associated with anemia, anemia in pregnancy was treated as the dependent variable, while age, gestational diabetes, hyperthyroidism, chronic HBV infection, syphilis infection, and HIV infection were considered as independent variables.
The retrospective cohort included 86 HBV cases and 129 controls who were admitted to the HNWCMC between November 2021 and January 2023. Serum samples were prepared by allowing 5 ml peripheral blood to clot at room temperature for 30 min. Afterwards, the samples were centrifuged at 3000 rpm for 10 min, and supernatant was collected for further analysis. Serum samples were utilized for serological assessment to determine the status of HBV infection. The presence of HBsAg, anti-HBsAg, HBeAg, anti-HBeAg, and anti-HBcAg was determined utilizing the iFlash 3000 chemiluminescence immunoassay analyzer in conjunction with the iFlash anti-HBcAg kit (YHLO Biotech, Co., Ltd. Shenzhen, China). Chronic HBV infection was defined as the presence of HBsAg for at least six months during the pregnancy. Serum levels of alanine transaminase (ALT) and aspartate aminotransferase (AST) were quantified utilizing specific kits (XinChuangYuan Biotech, Co., Ltd. Beijing, China), adhering strictly to the manufacturers’ instructions. The 86 HBV cases tested positive for HBsAg either before pregnancy (n = 7) or during the first trimester of pregnancy (n = 79), and all retained positive HBsAg results in a subsequent test conducted at least 6 months later. In contrast, the 129 controls were negative for HBsAg throughout the pregnancy. Hematological parameters for all HBV cases and controls were assessed during the first, second, and third trimesters to diagnose anemia in pregnancy using either the BC-6100Plus Analyzer (Mindray, USA) or the Sysmex XN-1000 Analyzer (Sysmex, Japan). Parameters pertaining to red blood cells, encompassing red blood cell count (RBC), hemoglobin concentration (HGB), hematocrit (HCT), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), red blood cell distribution width-standard deviation (RDW-SD), and RDW-coefficient of variation (RDW-CV), were subjected to analysis. The diagnosis of anemia in pregnancy was established in accordance with World Health Organization (WHO) criteria, defining anemia as hemoglobin levels below 11.0 g/dL during the pregnancy8. All studied subjects in the retrospective cohort were characterized for RBC-associated parameters in all three trimesters of pregnancy and assessed for chronic HBV infection.
This study was performed in line with the principles of the Declaration of Helsinki9. Approval for the study protocol was obtained from the Ethics Committee of the HNWCMC (Approval No.: HNWCMC-2023-80). Given the exclusively anonymized nature of the data utilized in this study and no more than minimal risk to the subjects, the requirement for informed consent was waived by the Institutional Review Board.
Detection of thalassemia genetic variations
For genomic analysis, DNA extraction from peripheral blood leukocytes was performed utilizing the Nucleic Acid Extraction or Purification Kit (Guangzhou Ruineng Medical Technology Co., Ltd. Guangzhou, China), following the manufacturer’s protocols. Common thalassemia mutations were identified utilizing the polymerase chain reaction-reverse dot blot hybridization technique, as previously described10.
Statistical analyses
All statistical analyses were meticulously conducted using GraphPad Prism Software (version 10.0.2). The Kolmogorov-Smirnov test was utilized to assess the normal distribution of variables. The student’s t-test was utilized to assess statistical significance for normally distributed quantitative data, while the Mann–Whitney U test was employed for non-normally distributed data. For binary variables, the chi-squared test or Fisher’s exact test was employed to ascertain statistical significance and odd ratios (ORs). Additionally, multivariable logistic regression analysis was executed to evaluate the predictive capacity of multiple independent variables on a binary outcome, and adjusted odd ratios (AORs) were calculated to quantify these associations. A p-value less than 0.05 was considered statistically significant.
Results
Association between chronic HBV infection and anemia in pregnancy in a cross-sectional study
A total of 43,201 pregnant women admitted to HNWCMC between January 2017 and December 2020 were screened. After applying the exclusion criteria, 38,180 pregnant women, with a mean age of 29.3 years, were included in the cross-sectional study (Supplementary Fig. 1, Table 1). Among the 38,180 cases, 7357 (19.27%) were diagnosed with anemia in pregnancy, 2548 (6.67%) developed gestational diabetes, 344 (0.90%) showed hypothyroidism, and 60 (0.16%) exhibited hyperthyroidism. The frequencies of chronic HBV infection, syphilis infection, and HIV infection were recorded at 2.10, 0.21, and 0.026%, respectively. (Table 1)
To determine potential risk factors for anemia in pregnancy, the pregnant women were stratified into two groups: 7,353 cases with anemia and 30,823 individuals without anemia. Subsequent analysis revealed significant disparities between the two groups concerning age, gestational diabetes, hypothyroidism, hyperthyroidism, chronic HBV infection, syphilis infection, and HIV infection. Multivariable logistic regression analysis was then employed, revealing that advanced maternal age (AOR 1.01, 95% CI 1.00-1.01, p < 0.0001), gestational diabetes (AOR 2.19, 95% CI 2.00-2.39, p < 0.0001), hypothyroidism (AOR 2.56, 95% CI 2.05–3.19, p < 0.0001), hyperthyroidism (AOR 1.95, 95% CI 1.12–3.30, p = 0.015), chronic HBV infection (AOR 2.97, 95% CI 2.57–3.44, p < 0.0001), and syphilis infection (AOR 1.74, 95% CI 1.06–2.79, p = 0.025) were each associated with an elevated risk of anemia in pregnancy (Table 2). Consequently, in addition to reaffirming the previously established associations between anemia in pregnancy and gestational diabetes11, hypothyroidism and hyperthyroidism12, this cross-sectional study revealed a robust positive association between chronic HBV infection and anemia in pregnancy.
We also investigated the association between chronic HBV infection and other pregnancy-related complications. As summarized in Supplementary Table 1, chronic HBV infection was positively associated with gestational diabetes and hypothyroidism, but no significant association was found between chronic HBV infection and hyperthyroidism. Furthermore, while both chronic HBV infection and gestational diabetes were independently associated with anemia during pregnancy, no cumulative effect of these factors on anemia was observed (Supplementary Table 2).
Association between chronic HBV infection and anemia in pregnancy in a retrospective cohort
To confirm the association between chronic HBV infection and anemia in pregnancy, a retrospective cohort study was subsequently conducted. The cohort comprised 86 pregnant women who tested positive for HBsAg either before conception or during the first trimester, while 129 age-matched pregnant women, testing negative for HBsAg, constituted the control group. The HBV cases exhibited markedly elevated serum levels of alanine transaminase (ALT) and aspartate aminotransferase (AST), consistent with the profile of chronic HBV infection (Table 3).
Throughout the entirety of pregnancy, both HBV cases and controls were monitored for the onset of anemia. During the first trimester, 12.8% (11 out of 86) of HBV cases developed anemia, a proportion significantly higher than the 4.7% observed in control subjects (OR 3.01, 95% CI 1.07–8.47, p = 0.303). Interestingly, no discernible difference in the prevalence of anemia emerged between the two groups during the second trimester (50% vs. 41.1%, OR 1.39, 95% CI 0.80–2.40, p = 0.24). However, a notable discrepancy in the prevalence of anemia resurfaced in the third trimester, with 60.5% of HBV cases and 41.1% of control subjects exhibiting anemia (OR 2.19, 95% CI 1.25–3.83, p = 0.0054). Cumulatively considering anemia across any trimester, 69.1% of HBV cases and 51.9% of control subjects were affected during pregnancy (OR 2.13, 95% CI 1.20–3.79, p = 0.0092), thereby corroborating the positive association between chronic HBV infection and anemia in pregnancy (Table 3).
No correlation between chronic HBV infection and thalassemia
To ascertain whether the observed association between chronic HBV infection and anemia in pregnancy might be confounded by the presence of thalassemia, a prevalent risk factor for anemia in pregnancy in the Hainan population2,10, a genetic analysis was conducted. Specifically, the cohort of 86 HBV cases and 129 controls was genotyped for common genetic variations of α and β thalassemia. Table 4 presents the prevalence of carriers of thalassemia genetic variations among HBV cases, which is 32.6% (28 out of 86), similar to the prevalence observed among the control group (32.6%; 42 out of 129). When the patients were subdivided based on specific subtypes of thalassemia, the stratified analysis revealed no significant association between chronic HBV infection and any subtype of thalassemia. Consequently, these findings suggest that there is no discernible association between HBV infection and thalassemia.
Association between chronic HBV infection and erythrocytes parameters
To gain insight into the positive association between chronic HBV infection and anemia in pregnancy, we explored the relationship between the presence of HBsAg and various erythrocyte parameters beyond HGB, including RBC, HCT, MCV, MCH, MCHC, RDW-SD and RDW-CV. No significant disparities were observed between HBV cases and controls in RBC, HCT, RDW-SD, or RDW-CV across any trimester. However, discernible differences were noted between the two groups in MCV, MCH, and MCHC. Although both HBV cases and control subjects exhibited similar trajectories in these parameters throughout pregnancy, HBV cases consistently demonstrated a tendency toward decreased MCV, MCH, and MCHC compared to control subjects. Specifically, significant differences in MCV during the third trimester, MCH in the first and third trimesters, and MCHC in the first trimester were observed (Fig. 1, Supplementary Table 3).
Association between chronic hepatitis B virus (HBV) infection and MCV, MCH and MCHC. Comparison of mean corpuscular volume (MCV) (A), mean corpuscular hemoglobin (MCH) (B), and mean corpuscular hemoglobin concentration (MCHC) (C) between HBV cases and control subjects during three trimesters of pregnancy. Data are presents as mean ± SEM (standard error of mean). Statistical significance between control subjects and HBV cases was determined using unpaired students T test. *p < 0.05, ****p < 0.0001.
Discussion
In the retrospective cross-sectional study encompassing 38,180 pregnant women, we observed a prevalence of anemia in pregnancy amounting to 19.27%. Notably, this finding aligns closely with the prevalence (17.78%) reported in a previous study involving 18 million Chinese pregnant women nationwide13. Such congruence lends credence to the reliability of our findings. However, in the retrospective cohort recruited from the same center in this study, the prevalence of anemia in pregnancy exceeded 50%. This substantial disparity is likely attributable to more meticulous follow-up procedures implemented in the retrospective cohort compared to the cross-sectional study. This discrepancy underscores a notable limitation inherent in retrospective cross-sectional studies, namely the potential for underestimation of prevalence due to less rigorous surveillance.
Notably, the cross-sectional study revealed a positive association of chronic HBV infection with anemia in pregnancy, and the association was confirmed in a retrospective cohort. Consequently, through the amalgamation of a cross-sectional study and a retrospective cohort analysis, this investigation furnishes compelling evidence supporting an association between chronic HBV infection and an elevated risk of anemia in pregnancy. Both anemia during pregnancy and hepatitis B virus (HBV) infection pose significant public health challenges in the developing world. However, the potential link between the two pathogenic conditions remains uncertain. Recent observational studies have yielded conflicting evidence on this matter. By reviewing of medical records encompassing 16,727 pregnant women, Deng et al. reported a higher prevalence of anemia among HBsAg cases compared to controls in southern China14, suggesting a positive association between HBV infection and anemia in pregnancy. However, such an association was not confirmed by two other retrospective observational studies, each with comparable sample sizes15,16. Therefore, the results of our study resolve the discordance evident in prior observational studies concerning this issue14,15,16. One possible explanation for the discrepancy might be missing data, which is a common limitation of retrospective studies17. Consequently, the findings of this study advocate for a cautious interpretation of observations derived from cross-sectional studies. Ideally, such findings should be validated through complementary observational studies to ensure robustness and reliability.
Despite the significant reduction in the prevalence of HBV infection following the introduction of the HBV vaccine, over 1.5 million new HBV infections continue to occur annually18,19. This persistence is largely attributed to the substantial variation in HBV vaccination coverage globally20. It is estimated that over 300 million individuals across the world live with chronic HBV infection19. Additionally, approximately 4.5 million women with chronic HBV infection give birth annually21. Consequently, identifying the association between chronic HBV infection and anemia in pregnancy carries substantial public health implications, particularly in developing countries.
Given that HBV infection often precedes the development of anemia during pregnancy, the observed positive association between the two conditions suggests that HBV infection may contribute to the development of anemia in pregnancy. This potential relationship and its underlying mechanisms warrant further investigation. Notably, subsequent analyses revealed distinct hematological characteristics, notably reduced erythrocyte size and corpuscular volume in HBV cases compared to control subjects. This finding suggests that chronic HBV infection may confer the risk of anemia in pregnancy by influencing the volume of erythrocytes and levels of corpuscular hemoglobin, rather than impacting the quantity or size variability of erythrocytes. Iron deficiency stands as the most prevalent cause of microcytic and hypochromic anemia22. While thalassemia represents another common etiology of microcytic and hypochromic anemia, particularly prevalent in tropical and subtropical regions23. Given the exclusion of an association between chronic HBV infection and thalassemia in our study, it is conceivable that HBV infection may elevate the risk of anemia in pregnancy by influencing iron metabolism. This hypothesis finds support in observations of iron metabolism disorders occurring in individuals with HBV-related liver diseases24. Consequently, the evaluation of iron supplementation necessity for HBV cases during pregnancy may emerge as a clinically consideration.
Interestingly, the current study confirms two previous established associations: the association between gestational diabetes and anemia in pregnancy11 and the association between chronic HBV infection with gestational diabetes25,26. Given that both chronic HBV infection and gestational diabetes are positively associated with anemia during pregnancy, it is conceivable that these factors might have an accumulative or synergistic effect on anemia. However, the present study found no evidence of such an accumulative or synergistic effect. This finding suggests the presence of an unknown interaction among these three conditions, which warrants further investigation.
This study has three notable limitations. Firstly, although HBV infection preceded the development of anemia during pregnancy in the majority of HBV cases in the retrospective cohort, for the small number of cases where anemia developed in the first trimester, it is challenging to determine whether HBV infection or anemia occurred first. This limitation may affect the validity of the findings from the retrospective cohort. Secondly, since the observational studies were conducted at a single center in Hainan, China, caution is needed when generalizing the results to other populations. Thirdly, age is a significant factor that could influence pregnancy-related complications, including anemia27,28, as reflected in our cross-sectional study. Given that the median age of the participants was approximately 30 years, the findings may not be generalizable to populations of different age groups. Further research is needed to confirm the association across diverse age groups.
In summary, our study delineates a discernible association between chronic HBV infection and an escalated susceptibility to anemia in pregnancy, as evidenced by rigorous cross-sectional and retrospective cohort investigations. These findings hold public health implications for clinical practice, particularly for developing countries with high prevalence of HBV infection.
Data availability
Data is provided within the manuscript.
References
Shand, A. W. & Kidson-Gerber, G. L. Anaemia in pregnancy: a major global health problem. Lancet 401 (10388), 1550–1551. https://doi.org/10.1016/S0140-6736(23)00396-3 (2023).
Petrakos, G., Andriopoulos, P. & Tsironi, M. Pregnancy in women with thalassemia: challenges and solutions. Int. J. Womens Health 8, 441–451. https://doi.org/10.2147/IJWH.S89308 (2016).
Stephen, G. et al. Anaemia in pregnancy: Prevalence, risk factors, and adverse perinatal outcomes in Northern Tanzania. Anemia 1846280. https://doi.org/10.1155/2018/1846280 (2018).
Msuya, S. E. et al. Anaemia among pregnant women in Northern Tanzania: prevalence, risk factors and effect on perinatal outcomes. Tanzan. J. Health Res. 13 (1), 33–39. https://doi.org/10.4314/thrb.v13i1.60881 (2011).
McClure, E. M. et al. The association of parasitic infections in pregnancy and maternal and fetal anemia: a cohort study in coastal Kenya. PLoS Negl. Trop. Dis. 8 (2), e2724. https://doi.org/10.1371/journal.pntd.0002724 (2014).
Georgieff, M. K. Iron deficiency in pregnancy. Am. J. Obstet. Gynecol. 223 (4), 516–524. https://doi.org/10.1016/j.ajog.2020.03.006 (2020).
Brooker, S., Hotez, P. J. & Bundy, D. A. Hookworm-related anaemia among pregnant women: a systematic review. PLoS Negl. Trop. Dis. 2 (9), e291. https://doi.org/10.1371/journal.pntd.0000291 (2008).
Organization, W. H. & Anemia. https://www.who.int/data/nutrition/nlis/info/anaemia (2024).
World Medical, A. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310 (20), 2191–2194. https://doi.org/10.1001/jama.2013.281053 (2013).
Wang, M. et al. Prevalence and genetic analysis of thalassemia in childbearing age population of Hainan, the free trade Island in Southern China. J. Clin. Lab. Anal. 36 (3), e24260. https://doi.org/10.1002/jcla.24260 (2022).
Hayashi, I. et al. Association of a pro-inflammatory diet and gestational diabetes mellitus with maternal anemia and hemoglobin levels during pregnancy: a prospective observational case-control study. Nutr. Res. 115, 38–46. https://doi.org/10.1016/j.nutres.2023.05.003 (2023).
Yang, Y. et al. Maternal thyroid dysfunction and gestational anemia risk: Meta-analysis and new data. Front. Endocrinol. (Lausanne) 11, 201. https://doi.org/10.3389/fendo.2020.00201 (2020).
Shi, H. et al. Severity of anemia during pregnancy and adverse maternal and fetal outcomes. JAMA Netw. Open 5 (2), e2147046. https://doi.org/10.1001/jamanetworkopen.2021.47046 (2022).
Deng, Q. et al. Prevalence of hepatitis B virus infection among pregnant women in the mountainous regions of southern China: a retrospective single-center study. J. Clin. Lab. Anal. 37 (2), e24837. https://doi.org/10.1002/jcla.24837 (2023).
Bierhoff, M. et al. Maternal hepatitis b infection burden, comorbidity and pregnancy outcome in a low-income population on the Myanmar-Thailand border: a retrospective cohort study. J. Pregnancy 2019, 8435019. https://doi.org/10.1155/2019/8435019 (2019).
Weng, M. et al. Effects of HBsAg carriers on pregnancy complications in pregnant women: a retrospective cohort study. Front. Med. (Lausanne) 10, 1166530. https://doi.org/10.3389/fmed.2023.1166530 (2023).
Burton, A. & Altman, D. G. Missing covariate data within cancer prognostic studies: a review of current reporting and proposed guidelines. Br. J. Cancer 91 (1), 4–8. https://doi.org/10.1038/sj.bjc.6601907 (2004).
Al-Busafi, S. A. & Alwassief, A. Global perspectives on the hepatitis b vaccination: challenges, achievements, and the road to elimination by 2030. Vaccines (Basel) 12 (3). https://doi.org/10.3390/vaccines12030288 (2024).
Collaborators, G. B. D. H. B. Global, regional, and national burden of hepatitis B, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Gastroenterol. Hepatol. 7 (9), 796–829. https://doi.org/10.1016/S2468-1253(22)00124-8 (2022).
Pujol, F. H. et al. Hepatitis B eradication: vaccine as a key player. Am. J. Transl Res. 15 (8), 4971–4983 (2023).
Terrault, N. A. et al. Viral hepatitis and pregnancy. Nat. Rev. Gastroenterol. Hepatol. 18 (2), 117–130. https://doi.org/10.1038/s41575-020-00361-w (2021).
Camaschella, C. Iron deficiency. Blood 133 (1), 30–39. https://doi.org/10.1182/blood-2018-05-815944 (2019).
Kattamis, A., Kwiatkowski, J. L., Aydinok, Y. & Thalassaemia Lancet 399 (10343) 2310–2324. https://doi.org/10.1016/S0140-6736(22)00536-0 (2022).
Gao, Y. H. et al. Iron metabolism disorders in patients with hepatitis B-related liver diseases. World J. Clin. Cases 6 (13), 600–610. https://doi.org/10.12998/wjcc.v6.i13.600 (2018).
Paramasivam, S., Krishnaswamy, S. & Giles, M. L. Unravelling the mechanisms by which chronic hepatitis B infection is associated with an increased risk of gestational diabetes. Front. Glob. Womens Health 4, 1184090. https://doi.org/10.3389/fgwh.2023.1184090 (2023).
Zhao, M. et al. Hepatitis B virus infection and increased risk of gestational diabetes regardless of liver function status: a Xiamen area population-based study. Front. Physiol. 13, 938149. https://doi.org/10.3389/fphys.2022.938149 (2022).
Alem, A. Z. et al. Prevalence and factors associated with anemia in women of reproductive age across low- and middle-income countries based on national data. Sci. Rep. 13 (1), 20335. https://doi.org/10.1038/s41598-023-46739-z (2023).
Horwich, T. B. et al. Cardiac troponin I is associated with impaired hemodynamics, progressive left ventricular dysfunction, and increased mortality rates in advanced heart failure. Circulation 108 (7), 833–838. https://doi.org/10.1161/01.CIR.0000084543.79097.34 (2003).
Acknowledgements
The work was funded by the Natural Science Foundation of Hainan Province, China (823QN359), the Major Science and Technology Project of Hainan Province (ZDKJ2021037), the Excellent Talent Team of Hainan Province (QRCBT202121), Hainan Province Clinical Medical Center (QWYH202175) and the German Ministry of Education and Research (BMBF) via the German Center for Lung Research (DZL4.0).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
X. Y and Q.Z. designed and supervised research; R.H., X.L., J.X., D.L., Y.F., Y.L., X. L., performed research; Z.L. and D. Z. collected data; R.H. and X.Y analyzed and interpreted data; FP and XY wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Human ethics and consent to participate declarations
Approval for the study protocol was obtained from the Ethics Committee of the HNWCMC (Approval No.: HNWCMC-2023-80). Given the exclusively anonymized nature of the data utilized in this study and no more than minimal risk to the subjects, the requirement for informed consent was waived by the Institutional Review Board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, R., Lu, Z., Li, X. et al. Positive association between chronic hepatitis B virus infection and anemia in pregnancy in Southern China. Sci Rep 15, 1980 (2025). https://doi.org/10.1038/s41598-024-84927-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-84927-7