Abstract
The ciliary body (CB) has been proposed as a niche of neural stem cells because, in vitro, cells from this area are able to form neurospheres, proliferate and differentiate. Here, we explore the potential of CB cells to differentiate and replace degenerated retinal ganglion cells (RGCs) in vivo. CB cells and cells from the subventricular zone (SVZ) were isolated from adult or postnatal C57BL/6Tg(CAG-EGFP) mice, respectively, and intravitreally injected into intact retinas, immediately after optic nerve crush or 45 days after the lesion of adult C57/BL/6 mice. Retinas were analysed in whole mounts or cross sections at different time points. Controls were matched untreated retinas. Neither cell type caused gliosis or toxicity when injected into intact retinas. When CB or SVZ cells were injected right after axotomy, they formed an epimembrane without integrating in the retina. However, when CB cells were administered in retinas depleted of RGCs, they integrated into the ganglion cell layer and expressed RGC and neuronal markers. Although SVZ cells were also able to integrate into RGC depleted retinas they did so more slowly than CB cells. These results shed light in the long-standing question of whether cells in the CB have the potential to transdifferentiate in vivo and point to the CB as a suitable source of cells that could be used in cell-replacement therapies for neurodegenerative diseases of the retina.
Similar content being viewed by others
Introduction
Mammalian retinal neurons, being part of the central nervous system, are not replaced when they die1. Photoreceptors and retinal ganglion cells (RGCs) – the first and last neurons, respectively, in the retinal circuitry2– are the most sensitive to degeneration. The loss of these cells is the cause of many human diseases that lead to blindness, such as glaucoma and retinal dystrophies1,3,4.
Advanced cell therapies for retinal degeneration are currently the subject of extensive research and rely on two main mechanisms: neuroprotection and neuronal replacement. In this line, different therapeutical strategies have been tested, but the optimal source of stem/progenitor cells suitable for retinal transplants remains to be determined1. Many studies have reported neuroprotection of RGCs after intravitreal administration of adult stem/stromal cells (MSCs) from non-ocular sources, such as those derived from the bone marrow or perinatal derivates5,6. However, different authors have demonstrated that MSCs do not integrate in the retina after injection in the vitreous and can cause functional impairment, anatomical remodelling, gliosis, immune recognition and microglial activation7,8, regardless of the ontogenic origin of the cells9. Currently, the most promising candidates as a source of cells suitable for retinal transplants include induced pluripotent stem cells (iPS), and eye-derived multipotent cells located in the ciliary body (CB)10,11. However, some observations have shown that iPS may retain epigenetic memory of their somatic cells of origin12,13which may display still-unknown negative complications and it has been also shown that some tissues derived from iPS cells can be immunogenic14, which may limit one of the most prominent advantages or iPS cells over other stem cell types.
Pioneer studies on neurogenesis performed in fish and amphibians showed highly proliferative multipotent retinal stem cells located in the ciliary marginal zone (CMZ) in these animals. In addition to be a relatively superficial and accessible area, CMZ cells are a perpetual self-renewing source of proliferative cells that increase proliferation and neurogenesis after cell injury in these species15. Endogenous stem cells at the peripheral retina of fishes and amphibians can give rise to the full range of retinal neurons16, indicating stem cell plasticity in response to lesion. The peripheral retinal region in mammals, the CB, does not have the capacity to regenerate damaged retinal cells. However, the CB has been considered as the evolutionary reminiscence of the CMZ of lower vertebrates10,17,18. Interestingly, adult Royal College of Surgeons rats, an animal model for retinitis pigmentosa, show more proliferating progenitor cells in the CB than control rats, as well as an increase of dividing cells in response to RGCs induced-degeneration19. Moreover, CB cells are those with the longest telomeres in the adult retina, which suggests a strong proliferative potential since longest telomeres in specific tissues have been described as a signature of adult stem cell compartments20. These results strongly suggest that CB cells may hold the potential to regenerate retinal neurons following degeneration, and the CB was proposed as a niche of neural stem cells (NSCs). In fact, two independent groups identified quiescent retinal stem cells in the adult mammalian eye almost two decades ago21,22. Under culture conditions, these adult progenitor cells located in the CB, displayed signs of self-renewal forming neurospheres (NsCBCs) and generated new retinal neurons both in the presence and in the absence of endogenous growth factors21,22. In addition, the neurogenic potential of these CB cells, that are densely packed with pigment granules leading to a dark appearance of the tissue, is not compromised with the pigmentation per se10,22.
Based on these data, sphere-forming cells from the mammalian CB have been considered as a promising source of cells to treat retinal degeneration and damage. Experiments performed so far to test the potential of CB cells to generate different types of retinal cells (including photoreceptors and RGCs) have been performed in vitro, but have not been successful when the cells were transplanted into the subretinal space21,22,23.
Here, we evaluate the regenerative potential of primary adult mouse CB cells, and cells amplified from CB-derived neurospheres (Ns-CB) and compare them to other neural stem cells, such as those obtained from the subventricular zone (SVZ), in a well-established model of RGC degeneration (reviewed in24). We observed that primary and Ns-CB cells had different beneficial effects depending on the time of injection along the degenerative process. When the intravitreal injection was performed at the time of the axotomy, these cells exert a neuroprotective capacity on the degenerating neurons. In contrast, if they are delivered once RGCs have degenerated, they tend to integrate into the RGC-depleted layer and some of them start to express RGC markers, suggesting that they may hold the capacity of becoming ganglion cells. Strikingly, SVZ cells were also able to integrate into the retinas depleted of RGCs but at a slower pace.
Results
Effect of intravitreal injection of neural stem cells into axotomized retinas
To assess the potential of primary CB cells as a viable source of stem cells for regenerative therapies, we utilised a transgenic mouse model with ubiquitous GFP expression25. We initially examined the proliferative and differentiation capabilities of CB cells isolated from these reporter mice. Our findings confirmed their capacity to generate neurospheres (Ns-CB) (Fig. 1A), displaying a high proliferative ratio along the next seven days in culture (Fig. 1B). Remarkably, during the induction of differentiation, CB cells exhibited a loss of both pigmentation and GFP expression as they exited the neurosphere (Fig. 1C). In fact, a significant number of them started to express neuronal markers such as class III beta-tubulin (βIII-tubulin also known as Tuj1) or Calretinin indicating that they can initiate their differentiation to neurons (Fig. 1D).
Generation and characterization of neurospheres from mouse CB cells. (A) BrdU immunofluorescence (red) in 5 days neurospheres generated from cells isolated from the ciliary body of 2 months-old mice. Nuclei were counterstained with DAPI (blue). (B) Quantification of proliferation rate in growing neurospheres (growth Rate = diameter(t1)/diameter (t1-1 day) – 1) X 100). ***p < 0.001. (C) Upper panels show neurosphere derived cells from the ciliary body of GFP mice one and nine days after the induction of differentiation. Bottom panels show GFP fluorescence from the same image. Note that many cells in the neurosphere are pigmented and/or positive for GFP but they lose the pigment and/or GFP as they leave the neurosphere to differentiate. (D) Immunofluorescence for βIII-tubulin/Tuj1 and calretinin (red) in cells derived from CB-neurospheres 7 days after induction of differentiation. Nuclei were counterstained with DAPI (blue).
Given the proliferative potential of CB cells and their capacity to initiate differentiation, we assessed their regenerative potential in vivo. We also isolated neural stem cells from a non-retinal context, the subventricular zone (Ns-SVZ), to test whether stem-capable cells from a different niche, unrelated to the retina, could adapt and differentiate when transplanted into the retina (see Material and Methods) (Fig. 2A). We first analysed the survival, location and potential adverse effects or toxicity of injecting CB, Ns-CB and Ns-SVZ cells isolated from GFP reporter mice into the retina of adult wild type mice (Fig. 2B). The cells were monocularly injected into the vitreous and analysed 90 days later. In the three cases, GFP cells were detected 90 days after injection forming an epimembrane above the DAPI stained nuclei at the level of the ganglion cell layer (Fig. 2C). The quantification of the total number of DAPI nuclei in the RGC layer was similar in injected and intact retinas (Fig. 2D), suggesting that the number of astrocytes, microglial cells, endothelial cells and displaced amacrine cells was not affected by the injected cells.
We then used antibodies against the transcription factor Brn3a, which is encoded by the Pou4f1gene26,27,28, to quantify number of RGCs in flat-mounted retinas injected with GFP+cells and found no differences from intact retinas (Fig. 2E, F). In addition, immunodetection of GFAP (macroglia) and Iba-1 (microglia) in retinal sections did not show anatomical activation of either macroglia or microglia (Fig. S1) in the transplanted groups. Unlike what has been described when other cell types are injected into the vitreous8 we did not find microglial cells in the vitreous of the transplanted groups. Together, these results indicate that intravitreal injection of CB, Ns-CB cells and Ns-SVZ cells is not toxic for endogenous retinal neurons and does not induce glial activation.
CB, NS-CBC and NS SVZ survive long-term after intravitreal administration, do not integrate into the retina and are not detrimental to neurons in the ganglion cell layer. (A) Design of the primary ciliary body cells (CB), collection and cultivation process to form neurosphere-expanded CB (Ns-CB) and the obtention of neural stem cells from the subventricular zone (Ns-SVZ). (B) CB, Ns-CB or Ns-SVZ of C57/BL/6 Tg(CAG-EGFP) mice were intravitreally administered in intact retinas (toxicity analysis) of C57BL/6 mice. (C) Confocal images taken from the vitreous side of flat mounts of untreated and intravitreally transplanted intact retinas 90 days after the transplant. Transplanted cells (green) form an epimembrane above the ganglion cell layer (DAPI staining) without integrating into the retina (bottom row). (D) Scatter bar graph showing the mean total number ± SD of DAPI nuclei in the ganglion cell layer. (E) Scatter bar graph showing the mean total number ± SD Brn3a*RGCs in untreated and intravitreally transplanted intact retinas analysed at 45 and 90 days after transplantation (One-way ANOVA, Tukey’s multiple comparisons test). Data from one independent experiment. (F) Neighbour maps of untreated and intravitreally transplanted intact retinas analysed 90 days after the transplant showing the topographical distribution of Brn3a+ RGCs. Colour scale goes from 0–22 (purple) to ≥ 160 (red) neighbour RGCs in a radius of 0.11 mm. The bottom-right of each panel shows the number of RGCs counted in its corresponding retina. S: superior, N nasal.
Then, we injected CB, Ns-CB cells and Ns-SVZ cells into the retinas of mice unilaterally axotomized, which is a well-established model of RGC degeneration24,29,30,31. Each cell type was injected intravitreally immediately after optic nerve crush (ONC) and the retinas were analysed 5, 14 and 45 days later (Fig. 3A). All cell types formed an epimembrane above the RGC layer, as observed in intact retinas. Interestingly, the epiretinal membrane formed by SVZ cells had a different morphology than that formed by CB and Ns-CB cells, as cells were not as densely packed as in the retinas injected with CB cells, and they showed a more rounded soma with many processes (Fig. S2).
Neuroprotection of axotomized RGCs. (A) CB, Ns-CB or Ns-SVZ of C57/BL/6 Tg(CAG-EGFP) mice were intravitreally administered right after optic nerve axotomy (neuroprotection analysis) of C57BL/6 mice. (B) Left: Neighbour maps showing the distribution of Brn3a+RGCs in a representative retina from each group and time point. Below each map, a magnified view of Brn3a+ RGCs extracted from the dorso-temporal quadrant of the central retina is presented. (S, superior, N, nasal). Colour scale goes from 0–22 (purple) to ≥ 160 (red) neighbour RGCs in a radius of 0.11 mm. At the bottom right of each panel is shown the number of RGCs counted in its corresponding retina. Data from two independent experiments. Right: Scatter bar graph showing the mean total number of Brn3a+RGCs ± SD in untreated and transplanted axotomized retinas at 5, 14 and 45 days after the injury and transplant. At all time-points the number of RGCs was significantly higher in treated than in untreated retinas (One way ANOVA, Dunnett’s multiple comparisons test. *p < 0.05; **p < 0.01; ***p < 0.001). In addition, at 45 days, the number of RGCs was significantly higher in Ns-CBC retinas compared to the other two cell types (≠p < 0.05).
As previously reported (reviewed in24), the quantification of Brn3a+RGCs in flat-mounted retinas following ONC revealed a stark decline, with approximately 50% of RGCs dying by day 5, escalating to 85% by day 14, and a mere 4% surviving after 45 days in the control group, which included non-injected animals and those injected with vehicle media, since none of the vehicles elicited neuroprotection (Fig. S3A). In contrast, retinas injected with CB, Ns-CB, or Ns-SVZ cells exhibited a significantly higher count of Brn3a+ cells compared to control retinas. In comparison to axotomized retinas, where only 53% of Brn3a+cells survived at day 5 and 3.8% at day 45, the percentage of Brn3a cells in injected retinas surpassed 60% at day 5 and remained above 6% at day 45 (Fig. 3B). Interestingly, the highest density of Brn3a+ cells was detected close to the location of the injected CB cells (Fig. 4).
RGC neuroprotection is enhanced in the vicinity of CB pigmented cells. (A) Retinal photomontage acquired with transmitted light 45 days after CB transplant. CB pigmented cells are observed mostly in the infero-nasal quadrant (opposite to the injection site, dorso-temporal, white arrow). (B) Neighbour maps showing the co-topography of surviving Brn3a+RGCs and pigmented-CBCs in the same flat-mounts at 5, 14 or 45 days post-injection and ONC. Colour scale has been adjusted for each time point to better visualise the colocalization of Brn3a+RGCs and pigmented-CB cells, and it goes from 0–22 (purple) to ≥ 120 (red) at 5 days, 0–7 to ≥ 56 at 14 days, and from 0–4/≥32 at 45 days neighbour RGCs or pigmented-CBCs in a radius of 0.11 mm. The number of RGCs or pigmented-CB cells counted in the corresponding retina is shown at the bottom of each panel. S: superior, N: nasal.
These interesting results showed an increase in the number of Brn3a+ cells in the retinas transplanted with neural stem cells. However, as shown in our in vitro assays, CB cells lose the GFP expression as they undergo differentiation and consequently, we cannot confirm the visualisation of differentiating cells. Thus, we faced uncertainty regarding whether the observed surge in Brn3a+cells post-transplant is attributed to neuroprotection of axotomized RGCs or the outcome of neural stem cells differentiation upon injection.
Transplantation of ciliary body cells into RGC-depleted retinas results in an increased number of cells expressing ganglion cell markers
To distinguish whether transplanted neural stem cells induce neuroprotection of axotomized RGCs or are differentiating, we injected the CB, Ns-CB or Ns-SVZ cells 45 days after ONC, once the majority of RGCs and their axons have already degenerated, and then analysed the retinas at two time points (30 and 90 days) after transplantation (Fig. 5A). As in the previous assay, GFP cells formed an epimembrane at the retina surface. However, this time we also observed GFP signal into the layer normally occupied by Brn3a cells in the retinas injected with CB or Ns-CB cells, and in the inner nuclear layer in the retinas injected with Ns-SVZ cells (Fig. 5B). In the later case, GFP cells showed a branched morphology not observed in the retinas injected with CB cells (Fig. 5C).
The analysis of flat-mounted retinas revealed a significantly higher number of Brn3a+ cells in transplanted retinas both 30 and 90 days after cell administration compared to retinas at the time of injection. In fact, the number of Brn3a+cells was 2-fold higher in CB and Ns-CB-transplanted retinas 30 days after cell administration and almost 3-fold higher than the number of RGCs found in axotomized controls 90 days after cell transplantation, indicating de novo acquisition of Brn3a -expressing cells and thus suggesting that CB cells, either primary or expanded (Ns-CB), are likely differentiating to RGCs (Fig. 5D-E).
In the retinas injected with Ns-SVZ, the number of Brn3a+cells did not significantly increase 30 days after injection compared to the retinas at the time of injection, but they showed 2.3 times more Brn3a+cells than untreated controls 90 days after cell administration (Fig. 5D-E).
Strikingly, in the case of retinas injected with CB cells, the higher density of Brn3a+cells coincided again with the location of pigmented cells (Fig. 5F). These results suggested that CB, Ns-CB and Ns-SVZ cells have the capacity to express Brn3a when injected in vivo, but it takes longer for Ns-SVZ than for CB cells.
RGC depleted retinas transplanted with CBC, Ns-CB or Ns-SVZ have a higher number of Brn3a cells than untreated retinas. (A) CB, Ns-CB or Ns-SVZ from Tg(CAG-EGFP) mice were intravitreally administered in control RGC depleted retinas (45 days after ONC, integration and replacement analysis). (B) Vitreous side of flat mounted RGC depleted retinas analysed 90 days after CB, Ns-CB or Ns-SVZ cells transplantation. Brn3a cells (purple) and GFP signal (green) from transplanted cells is detected. Magnifications acquired from the central retina in the dorso-temporal quadrant. (C) Left: Vitreous side of flat mounted RGC depleted retinas analysed 90 days after Ns-SVZ transplant. Right, confocal magnification focused on the INL showing a Ns-SVZ cells integrate into the INL. (D) The scatter bar graph illustrates the total mean number ± SD of Brn3a+cells in depleted retinas, assessed at two time points: 45 days after optic nerve crush (ONC), (time 0) and 90 days post-ONC (135 days after ONC), following RGC depletion alone or in combination with intravitreal administration of CB, Ns-CB, or Ns-SVZ. In untreated retinas, Brn3a+cells are RGCs that survived the optic nerve axotomy. There is no difference between time 0 and time 90 after depletion between untreated retinas. However, retinas treated with each type of neural stem cell have significantly more Brn3a+cells than the untreated ones (One-way ANOVA, Holm-Šídák’s multiple comparisons test. vs. 0 d after treatment: *p < 0.05, **p < 0.01; ***p < 0.001. vs. 30 d after treatment: ##p < 0.01; ###p < 0.001. vs. 90 d after treatment: aaap<0.001). (E) Neighbour maps showing the distribution of Brn3a+ cells in a representative retina from each group and time point. S: superior, N: nasal. (F) Neighbour maps showing the co-topography of Brn3a+ cells and CB pigmented cells in the same depleted retinas at 30 and 90 days after the transplant. Colour scale (top left map) goes from 0–6 (purple) to ≥ 32 (red) neighbour RGCs in a radius of 0.11 mm. The number of RGCs in the corresponding retina is shown at the bottom of each panel. Data from two independent experiments. S: superior, N: nasal.
As expected, although we detected GFP cells in the vitreous and in deep layers of the neural retina 90 days after cell transplantation (Fig. 5A), we did not find co-localization of GFP with Brn3a, RBPMs or βIII-tubulin positive cells, in agreement with the previous observation that CB cells from the GFP reporter mouse line lose the GFP expression during in vitro differentiation (Fig. 1).
The retinas that underwent transplantation were subsequently incubated with antibodies targeting two well-established markers of RGCs, namely RBPMS and βIII-tubulin (reviewed in26). Analysis of flat-mounted retinas demonstrated a notable increase in the number of cells positive for both RBPMS and βIII-tubulin in retinas injected with CB and Ns-CB cells compared to control retinas (Fig. 6A-D). These findings strongly suggest that both primary CB and Ns-CB cells possess the capability to express RGC markers when introduced into retinas lacking these neurons, indicating their potential to differentiate and potentially replace degenerated RGCs over an extended period. Moreover, under the same experimental conditions, SVZ cells transplanted into retinas expressed early RGC markers (βIII-tubulin or Brn3a) but did not exhibit mature RGC markers (RBPMS). This observation implies that SVZ cells may also have the ability to differentiate into neurons in vivo, albeit requiring a prolonged duration for the maturation process.
The number of cells expressing mature RGCs markers is higher in depleted retinas transplanted with CB, Ns-CB or Ns-SVZ than in control retinas. (A) Neighbour maps showing the distribution of RBPMS+cells in each group at day 90 after depletion/transplant. The number of cells counted in its corresponding retina and underneath a magnification of RBPMS immunodetection is shown at the bottom of each panel. (B) The scatter bar graph illustrates the total mean number ± SD of RBPMS+cells in depleted retinas, assessed at two time points: 45 days after ONC (time 0) and 90 days post-ONC (135 days after ONC), following RGC depletion alone or in combination with intravitreal administration of CB, Ns-CB, or Ns-SVZ. In untreated retinas, RBPMS+cells are RGCs that have survived the optic nerve axotomy. There is no difference between time 0 and time 90 after depletion between untreated retinas. However, retinas treated with each type of neural stem cell have significantly more RBPMS+cells than the untreated ones (One-way ANOVA, Holm-Šídák’s multiple comparisons test. ***p < 0.001). (C) Neighbour maps showing the distribution of βIII-tubulin+cells in each group at day 90 after depletion/transplant. At the bottom of each panel is shown the number of cells counted in its corresponding retina and underneath a magnification of βIII-tubulin immunodetection. Neighbour map colour scale goes from 0–6 (purple) to ≥ 32 (red) neighbour RGCs in a radius of 0.11 mm. Magnifications were acquired from the central-medial retina in the dorso-temporal quadrant S: superior, N: nasal. (D) The scatter bar graph illustrates the total mean number ± SD of βIII-tubulin+cells in depleted retinas, assessed at two time points: 45 days after ONC (time 0) and 90 days post-ONC (135 days after ONC), following RGC depletion alone or in combination with intravitreal administration of CB, Ns-CB, or Ns-SVZ. In untreated retinas, βIII-tubulin+cells are RGCs that have survived the optic nerve axotomy. No difference is observed between time 0 and time 90 after depletion in untreated retinas. However, retinas treated with each type of neural stem cell have significantly more βIII-tubulin+cells than the untreated ones. (One-way ANOVA, Holm-Šídák’s multiple comparisons test. *p < 0.05; **p < 0.01, ***p < 0.001).
Discussion
Here we show that both primary and in vitro expanded CB cells have the ability to express RGC markers in retinas depleted of this specific population. Neural stem cells derived from the brain, rather than the eye, also appear to exhibit the capacity to differentiate and express neuronal markers but their behaviour differs from that of CB cells.
Our experiments showed that when injected into intact retinas, immediately after ONC or long-term after ONC, both CB and SVZ cells survive in the vitreous much longer than other adult stem cells, such as mesenchymal stromal cells, which were not detected 90 days after implantation6,7,32. This indicates that neural stem cells do not induce a host-graft rejection response as the one observed after injection of other types of stem cells (for a detailed review see33).
To investigate potential beneficial effects of CB cells in pathological conditions, we carried out two different approaches. In the first one, we performed cell transplantation at the same time than axotomy induction. In a second assay, cells were transplanted once most RGCs had degenerated. In both cases, we found an increase in the number of Brn3a cells compared to non-transplanted controls, confirming that injection of neural stem cells has a positive effect in injured retinas. In the first scenario, we could not undoubtedly distinguish whether the increase in the number of Brn3a+cells was due to a delay in the degeneration of axotomized RGCs or to the differentiation of injected cells. Given the result of the second assay and taking into account that the additional number of Brn3a+cells is similar in both assays, it is likely that injected cells have engaged the differentiation process in both paradigms. However, we cannot discard that in the first assay, neural stem cells are also exerting a neuroprotective effect on axotomized RGCs. Strikingly, when CB and SVZ cells were injected into retinas depleted of RGCs, the number of cells expressing RGC markers 30 or 90 days after CB or SVZ administration was significantly higher than in depleted retinas at the time of injection. In other words, CB and SVZ cells hold the capacity to differentiate into neurons. Given that RGCs from the transgenic GFP donor lose GFP expression, we cannot be certain that CB and SVZ cells differentiate into RGCs and cannot exclude the possibility that they induce RGC differentiation from Müller glia, for example. However, the observation that SVZ cells migrating into the INL do not express RGC markers and still retain GFP expression, whereas new Brn3a+ cells in CB-injected retinas are not positive for GFP, supports the idea that CB and SVZ cells have differentiated into RGCs.
Previous reports have shown that major barriers to cell engraftment in the retina are inflammation, glial activation and an intact inner limiting membrane34,35,36,36,37. It is widely believed that neuroprotective mechanisms share a common ground that different cell therapies can achieve by modulating inflammation, trophic factor secretion, and addressing neuroinflammation and trophic factor withdrawal, which are the underlying causes of all neurodegenerative processes38. The protocol of performing axotomy and cell injection at the same time has been used to investigate neuroprotection conferred by other types of stem cells that actually exert a neuroprotective effect under the same circumstances5,7,32. We observed an average of approximately 6000 and 3000 more Brn3a+cells in the transplanted retinas than in the controls 5 and 14 days after implantation, respectively. Since these timeframes seem to be too short for the injected cells to begin differentiating and expressing markers of ganglion cells, it is likely that neural stem cells may also have a neuroprotective effect on degenerating RGCs. Notably, CB, Ns-CB and Ns-SVZ differ from other cell-based neuroprotective therapies in that they do not induce gliosis, microglial activation and migration into the vitreous, or retinal detachment, which are adverse effects observed with other adult cells, such as MSCs even in syngeneic transplantation5,6,8,32. We believe that, in addition to starting differentiation at longer time points, neural stem cells exert a neuroprotective effect on degenerating cells and appear to be safer than other adult stem cells reported to have neuroprotective properties.
In conclusion, CB and SVZ cells emerge as promising sources for potential replacement therapies in neurodegenerative diseases affecting RGCs. Their sustained neuroprotective properties, even after in vitro expansion, make them relevant to consider them for applications in patients with degenerative retinal pathologies. Their immune-tolerant nature positions neural stem cells as better candidates for neuroprotection than non-neural origin stem cells. Moreover, CB and Ns-SVZ cells exhibit potential to differentiate into RGCs following RGC loss, offering hope for future treatments in patients with existing RGC damage. In addition, CB cells, either primary or expanded in vitro (Ns-CB), show greater efficacy than SVZ cells, suggesting that stem cell niches from the degenerating areas are more suitable for areas are better suited for neuronal restoration. The advantage of Ns-CB cells over primary CB cells is that their in vitro expansion allows the creation of cell banks for clinical use. Finally, further studies are needed to evaluate the in vivo stimulation of endogenous CB cells for retinal therapy and to extend the investigation to other retinal neurons.
Materials and methods
Animal handling
Adult pigmented C57BL/6 male mice (30 g ± 4 mean weight) were obtained from the University of Murcia breeding colony. Previously reported mice C57BL/6 Tg(CAG-EGFP) (Hadjantonakis et al., 1999) were breed in the Alicante animal facility. Only males were used because in the model of RGC degeneration used here, optic nerve crush, there are no differences in the progression of RGC loss except at 3 days post-lesion, a time point that is not relevant in this study.
All animals were treated in compliance with the European Union guidelines for Animal Care and Use for Scientific Purpose (Directive 2010/63/EU), the guidelines from the Association for Research in Vision and Ophthalmology (ARVO) Statement for the Use of Animals in Ophthalmic and Vision Research and ARRIVE and our institutional guidelines. All procedures were approved by the Ethical and Animal Studies Committee of the University of Murcia, and the Instituto de Neurociencias de Alicante.
Animals were randomly allocated to each experimental group, and none was excluded from the study. The experimental design is summarised in the corresponding figures. Cells isolated from C57/BL/6 Tg(CAG-EGFP were injected intravitreally into C57/BL/6 mice in three groups: intact, immediately after optic nerve crush (ONC) or 45 days after ONC. Retinas were analysed in whole mounts or cross sections at different time points. Controls were matched untreated retinas. The number of retinas per group, cell type and time point are shown in each graph (n = 3–12).
Animals undergoing surgery were anaesthetized by intraperitoneal injection of a mixture of ketamine (60 mg/kg; ketolar, Pfizer, Alcobendas, Madrid, Spain) and xylazine (10 mg/kg; Rompum, Bayer, Kiel, Germany). Analgesia was provided by subcutaneous administration of buprenorphine (0.1 mg/kg; Buprex, Buprenorphine 0.3 mg/mL; Schering-Plough, Madrid, Spain). During and after surgery, the eyes were covered with an ointment (Tobrex; Alcon S. A., Barcelona, Spain) to prevent corneal desiccation.
Cell isolation
The protocol used for CB isolation is a modification from39. Isolation of the retinal stem cells was performed in a specific sterile room dedicated to primary culture experiments. Mice were sacrificed by cervical dislocation and eyes were removed and cleaned removing hair, blood vessels and ocular muscle in a 60 mm dish containing Hank’s balanced salt solution (HBSS). Eyes were transferred into a new 60 mm dish with HBSS supplemented with glucose 8%, Hepes 2%, penicillin/streptomycin 0.5% and gentamicin 0.1%. Using curved micro-dissecting scissors eyes were cut in half and the cornea and iris removed away from the ciliary margin. Then, ciliary margin was removed from the RPE and transferred into a 35 mm Petri dish with HBSS supplemented. All the ciliary margins were collected into a 35 mm dish containing 2 mL of Dispase and incubated during 10 min at 37 °C. Next, the medium was replaced with a solution containing Kynurenic Acid 2 mg, Trypsin-EDTA 0.25% and Hyaluronidase 6.7 mg and DNAse 1µL/mL and put at 37 °C during 30 min. Then, the ciliary epithelium was gently scraped from the sclera and transferred into a 15 mL tube where it was pipetted 30 times up and down to break apart the epithelial cells and then centrifuged for 5 min at 1500 RPM. The supernatant was replaced with Trypsin inhibitor (1.5 mL) and titrated and centrifuged 5 min at 1500 RPM. The supernatant was replaced with supplemented media (Neurobasal, L-glutamine 0.1%, B27 0.1% and penicillin/streptomycin 0.1%) and titrated in a single cell suspension and filtered using a Cell Strainer 40 μm. It was centrifuged 5 min at 1500 RPM. At this point, we took the CB cells to be subsequently injected.
Neurosphere generation
To generate neurospheres and the group that we have called Ns-CBCs we continued by replacing the supernatant with plating media (Neurobasal with EGF 20 ng/mL, FGF2 20 ng/mL and Heparin 2 µg/mL at a density of 20 cells/µL). Once every two days, add to the culture media FGFb, EGF and Heparin 2µL/each well. After 7 days, the neurospheres generated were spin down 5 min at 800 RPM. We removed the supernatant and incubated the neurospheres 10 min at 37 °C with 1 mL of Accutase. After that, the solution was pipetted 50 times to dissociate the neurospheres, and then centrifuged for 5 min at 1000 RPM. The supernatant was replaced with Neurobasal to inject the cells.
To generate neurospheres from SVZ cells (Ns-SVZ), we followed the instructions published by40. To dissociate the neurospheres generated we followed the next steps, they neurospheres were collected by centrifugation during 7 min at 800 RPM from the culture medium. Then, the pellet was incubated with 200 µL of Accutase during 10 min at room temperature. After that, the solution was centrifuged 10 min at 1500 RPM. The supernatant was replaced with its medium without growth factors to be injected.”
In vitro differentiation of cells from ciliary body derived neurospheres (CB-NS)
To differentiate cells from CB-NS, we promoted differentiation in a medium supplemented with 4% fetal bovine serum in the absence of growth factors (EGF and FGF2) and plated them on a polylysine-coated coverslip. When incubated under differentiation conditions, the cells began to concentrically migrate from the neurosphere and the neurosphere usually disappeared after 9–10 days in culture.
Optic nerve crush (ONC)
The left optic nerve crushed following previously described methods41,42. In brief, to access the optic nerve at the back of the eye, an incision was made in the skin overlying the superior orbital rim, the dorso-external orbital contents were dissected, and the superior and external rectus muscles were sectioned. Then, the optic nerve was crushed at 0.5 mm from the optic disc during 10 s using watchmakers forceps. Before and after the procedure, the eye fundus was observed through the operating microscope to assess the integrity of the retinal blood flow.
Intravitreal injections
Intravitreal injections were done following standard procedures7,42,43. Briefly, the needle of a Hamilton microsyringe (26G; Hamilton 701 N, Esslab, Benfleet, UK) was introduced through the supratemporal sclera into the vitreous and the cells (5,000/eye) or vehicles were injected in a final volume of 2.5 µl.
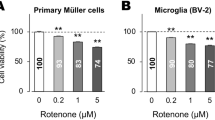
To determine the cell dose for intravitreal injections, we injected 5,000 CB or 12,500 CB into the vitreous of intact retinas. After 45 days, the total number of RGCs immunolabelled with Brn3a was automatically quantified in flat-mounts. In the group treated with 12,000 CB there was a significant loss of RGCs (Fig. S3B), suggesting that this dose was harmful for RGCs. We performed all subsequent experiments with the lower dose for all cell types, as the number of CBs isolated from a mouse is small and the higher dose was close to the toxic dose.
Tissue processing
Animals were euthanised by a lethal intraperitoneal injection of pentobarbital (Dolethal Vetoquinol®, Especialidades Veterinarias, S.A., Alcobendas, Madrid, Spain) and then, they were perfused transcardially with saline and 4% paraformaldehyde in 0.1 M phosphate buffer (pH 7.4). Eyes were enucleated and post fixed for 1 extra hour in the same fixative. Retinas were dissected as flattened whole-mounts as previously described41,42,43.
For cross sections, eyes were cryoprotected in serial concentrations of sucrose, and sagittal sections of 14 μm thickness are then made using a cryostat (Leica, Jung CM3000, Germany).
Immunodetection
Immunodetection was carried out as reported41,42,43. RGCs were detected with mouse α-Brn3a (1:300; MAB1585, Merck Millipore), rabbit anti RBPMS (1:750, GTX118619, Genetex) or mouse anti βIII tubulin (1:500, 801201, Biolegend). Microglial cells, with rabbit α-Iba1 (1:500; ab178846, Abcam), and macroglial cells with rabbit α-GFAP (1:500; Sigma Aldrich). Secondary detection was carried out with donkey α-mouse IgG1-Alexa fluor 594 or donkey α-rabbit Alexa 594 (1:500; Molecular Probes; Thermo Fisher Scientific). Retinas or cross sections were mounted with antifading medium containing DAPI (Vectashield with DAPI, Vector laboratories Palex Medica).
To detect BrdU, we add BrdU to the culture medium (at a concentration of 28 µM) and subsequent staining with an anti-BrdU antibody (rat anti BrdU 1:1000; ab6326, Abcam). Quantification of the proliferation rate of the neurospheres, indicating their increase in size over time (growth Rate = current diameter/past diameter(1/days in culture)−1)X100).
Image acquisition and analysis
Retinal photomontages were imaged using an epifluorescence microscope (Axioscop 2 Plus; Zeiss Mikroskopie, Jena, Germany) equipped with a computer-driven motorised stage (ProScan H128 Series; Prior Scientific Instruments) controlled by image analysis software (Image-Pro Plus, IPP 5.1 for Windows; Media Cybernetics). Each photomontage was reconstructed from 154 (11 × 14) individual images43,44. For high-resolution detail capture and for 3D reconstruction of retina, individual images are acquired with the confocal microscope (Leica TCS SP8 Confocal Microscope). Confocal microscope features four lasers: 405 nm ultraviolet continuous wave laser; 458, 476, 488, and 514 nm multiline Argon lasers; a 561 nm DPSS yellow laser; and a 633 nm HeNe red laser.
The equipment is controlled by software (Leica Application Suite X (LAS X), Leica Microsystems), allows Z-Stack image capture, and subsequent 3D reconstruction of the captured tissue block, as well as cleaner images and the ability to distinguish signal colocalizations.
Quantifications
The total number of Brn3a+RGCs or DAPI nuclei in the ganglion cell layer was automatically quantified on flat mounts using a computer subroutine previously developed in our laboratory41,44.
Pigmented cells, RBPMS and βIII tubulin positive cells in the GCL were manually dotted on the photomontage using Adobe Photoshop® CS 8.0.1 image editing software. The dotted photomontages were saved in tiff format for further quantification and distribution analysis.
Neighbour maps (nearest neighbour analyses)
Cell distribution was assessed by neighbour maps using previously reported methods44. These maps depict, using a colour scale, the number of neighbours around a given cell in a radius of 0.11 mm. All maps were plotted using SigmaPlot (SigmaPlot 9.0 for Windows; Systat Software, Inc., Richmond, CA, USA).
Statistics
There was no blinding in this study as the experimental animals and transplanted retinas were easily identifiable and the quantification methods were automatised. Data were analysed and plotted with GraphPad Prism v.7 (GraphPad San Diego, USA). Tests applied are detailed in results or figure legends. Differences were considered significant when p < 0.05. Data are presented in scatter dot plots showing independent samples and the mean ± standard deviation (SD).
Data availability
All data generated or analysed during this study are included in this published article, or if absent are available from the corresponding authors upon reasonable request.
Abbreviations
- BrdU:
-
Bromodeoxyuridine
- Brn3a:
-
Brain-specific homeobox/POU domain protein 3 A
- CB:
-
Ciliary body
- GFAP:
-
Glial fibrillary acidic protein
- GFP:
-
Green fluorescent protein
- Ns:
-
Neurosphere
- RBPMS:
-
RNA-binding protein with multiple splicing
- RGC:
-
Retinal ganglion cell
- SVZ:
-
Subventricular zone
References
Jin, Z. B. et al. Stemming retinal regeneration with pluripotent stem cells. Prog Retin Eye Res. 69, 38–56 (2019).
Ramon & Cajal y S. La Retina de Los Vertebrados. (Consejo Superior de Investigaciones Científicas, Madrid, Spain, (2021).
You, W. et al. A time window for rescuing dying retinal ganglion cells. Cell. Commun. Signal. 22, 88 (2024).
Cui, N., Jia, J. & He, Y. Glaucomatous retinal ganglion cells: death and protection. Int. J. Ophthalmol. 18, 160–167 (2025).
Mesentier-Louro, L. A. et al. Long-term neuronal survival, regeneration, and transient target reconnection after optic nerve crush and mesenchymal stem cell transplantation. Stem Cell. Res. Ther. 10, 121 (2019).
Millán-Rivero, J. E. et al. Human Wharton’s jelly mesenchymal stem cells protect axotomized rat retinal ganglion cells via secretion of anti-inflammatory and neurotrophic factors. Sci. Rep. 8, 16299 (2018).
Norte-Muñoz, M. et al. Neuroprotection and axonal regeneration induced by bone marrow mesenchymal stromal cells depend on the type of transplant. Front. Cell. Dev. Biol. 9, 772223 (2021).
Norte-Muñoz, M. et al. Immune recognition of syngeneic, allogeneic and xenogeneic stromal cell transplants in healthy retinas. Stem Cell. Res. Ther. 13, 430 (2022).
Muñoz, M. N. et al. Effect of olfactory ensheathing glia clone TEG3 on neuroprotection, microglial activation and gene expression profile of allotransplanted retina with and without immunosuppression. Acta Ophthalmol. 100, (2022).
Fernández-Nogales, M., Murcia-Belmonte, V., Chen, H. Y. & Herrera, E. The peripheral eye: A neurogenic area with potential to treat retinal pathologies? Prog Retin Eye Res. 68, 110–123 (2019).
Lamba, D. A. et al. Generation, purification and transplantation of photoreceptors derived from human induced pluripotent stem cells. PLoS One. 5, e8763 (2010).
Aldiri, I. et al. The dynamic epigenetic landscape of the retina during development, reprogramming, and tumorigenesis. Neuron 94, 550–568e10 (2017).
Polo, J. M. et al. Cell type of origin influences the molecular and functional properties of mouse induced pluripotent stem cells. Nat. Biotechnol. 28, 848–855 (2010).
Jiang, Z., Han, Y. & Cao, X. Induced pluripotent stem cell (iPSCs) and their application in immunotherapy. Cell. Mol. Immunol. 11, 17–24 (2014).
Ail, D. & Perron, M. Retinal degeneration and Regeneration-Lessons from fishes and amphibians. Curr. Pathobiol Rep. 5, 67–78 (2017).
Casarosa, S. et al. Xrx1 controls proliferation and multipotency of retinal progenitors. Mol. Cell. Neurosci. 22, 25–36 (2003).
Moshiri, A., Close, J. & Reh, T. A. Retinal stem cells and regeneration. Int. J. Dev. Biol. 48, 1003–1014 (2004).
Nishiguchi, K. M., Kaneko, H., Nakamura, M., Kachi, S. & Terasaki, H. Identification of photoreceptor precursors in the Pars plana during ocular development and after retinal injury. Invest. Ophthalmol. Vis. Sci. 49, 422–428 (2008).
Jian, Q. et al. Activation of retinal stem cells in the proliferating marginal region of RCS rats during development of retinitis pigmentosa. Neurosci. Lett. 465, 41–44 (2009).
Flores, I. et al. The longest telomeres: a general signature of adult stem cell compartments. Genes Dev. 22, 654–667 (2008).
Ahmad, I., Tang, L. & Pham, H. Identification of neural progenitors in the adult mammalian eye. Biochem. Biophys. Res. Commun. 270, 517–521 (2000).
Tropepe, V. et al. Retinal stem cells in the adult mammalian eye. Science 287, 2032–2036 (2000).
Cicero, S. A. et al. Cells previously identified as retinal stem cells are pigmented ciliary epithelial cells. Proc. Natl. Acad. Sci. U S A. 106, 6685–6690 (2009).
Vidal-Sanz, M. et al. Shared and differential retinal responses against optic nerve injury and ocular hypertension. Front. Neurosci. 11, 235 (2017).
Hadjantonakis, A. K., Pirity, M. & Nagy, A. Cre recombinase mediated alterations of the mouse genome using embryonic stem cells. Methods Mol. Biol. 97, 101–122 (1999).
Nadal-Nicolás, F. M. et al. Pan-retinal ganglion cell markers in mice, rats, and rhesus macaques. Zool. Res. 44, 226–248 (2023).
Quina, L. A. et al. Brn3a-expressing retinal ganglion cells project specifically to thalamocortical and collicular visual pathways. J. Neurosci. 25, 11595–11604 (2005).
Badea, T. C., Cahill, H., Ecker, J., Hattar, S. & Nathans, J. Distinct roles of transcription factors brn3a and brn3b in controlling the development, morphology, and function of retinal ganglion cells. Neuron 61, 852–864 (2009).
Berkelaar, M., Clarke, D. B., Wang, Y. C., Bray, G. M. & Aguayo, A. J. Axotomy results in delayed death and apoptosis of retinal ganglion cells in adult rats. J. Neurosci. 14, 4368–4374 (1994).
Cheng, L., Sapieha, P., Kittlerova, P. & Hauswirth, W. W. Di Polo, A. TrkB gene transfer protects retinal ganglion cells from axotomy-induced death in vivo. J. Neurosci. 22, 3977–3986 (2002).
Pernet, V. et al. Neuronal Nogo-A upregulation does not contribute to ER stress-associated apoptosis but participates in the regenerative response in the axotomized adult retina. Cell. Death Differ. 19, 1096–1108 (2012).
Mesentier-Louro, L. A. et al. Distribution of mesenchymal stem cells and effects on neuronal survival and axon regeneration after optic nerve crush and cell therapy. PLoS One. 9, e110722 (2014).
Norte-Muñoz, M., García-Bernal, D., García-Ayuso, D., Vidal-Sanz, M. & Agudo-Barriuso, M. Interplay between mesenchymal stromal cells and the immune system after transplantation: implications for advanced cell therapy in the retina. Neural Regen Res. 19, 542–547 (2024).
Johnson, T. V., Bull, N. D. & Martin, K. R. Identification of barriers to retinal engraftment of transplanted stem cells. Invest. Ophthalmol. Vis. Sci. 51, 960–970 (2010).
Zhang, K. Y., Aguzzi, E. A. & Johnson, T. V. Retinal ganglion cell transplantation: approaches for overcoming challenges to functional integration. Cells 10, 1426 (2021).
Zhang, K. Y. et al. Role of the internal limiting membrane in structural engraftment and topographic spacing of transplanted human stem Cell-Derived retinal ganglion cells. Stem Cell. Rep. 16, 149–167 (2021).
Peynshaert, K., Devoldere, J., Minnaert, A. K., De Smedt, S. C. & Remaut, K. Morphology and composition of the inner limiting membrane: Species-Specific variations and relevance toward drug delivery research. Curr. Eye Res. 44, 465–475 (2019).
Wareham, L. K. et al. Solving neurodegeneration: common mechanisms and strategies for new treatments. Mol. Neurodegener. 17, 23 (2022).
Coles, B. L. K. & van der Kooy, D. Isolation of retinal stem cells from the mouse eye. J. Vis. Exp. 2209 https://doi.org/10.3791/2209 (2010).
Vernerey, J., Magalon, K. & Durbec, P. Primary culture of SVZ-derived progenitors grown as neurospheres. Bio Protoc. 3, (2013).
Galindo-Romero, C. et al. Axotomy-induced retinal ganglion cell death in adult mice: quantitative and topographic time course analyses. Exp. Eye Res. 92, 377–387 (2011).
Sánchez-Migallón, M. C., Valiente-Soriano, F. J., Nadal-Nicolás, F. M., Vidal-Sanz, M. & Agudo-Barriuso, M. Apoptotic retinal ganglion cell death after optic nerve transection or crush in mice: delayed RGC loss with BDNF or a caspase 3 inhibitor. Invest. Ophthalmol. Vis. Sci. 57, 81–93 (2016).
Lucas-Ruiz, F. et al. Systemic and intravitreal antagonism of the TNFR1 signaling pathway delays Axotomy-Induced retinal ganglion cell loss. Front. Neurosci. 13, 1096 (2019).
Galindo-Romero, C. et al. Number and Spatial distribution of intrinsically photosensitive retinal ganglion cells in the adult albino rat. Exp. Eye Res. 108, 84–93 (2013).
Funding
Spanish Ministry of Economy and Competitiveness, Instituto de Salud Carlos III, Fondo Europeo de Desarrollo Regional “Una Manera de Hacer Europa” PI19/00071, PI24/00040 (MAB). Fundació La Marató de TV3 20142130 (EH) and 20142131 (MAB). The laboratory of E. H. is supported by grants from the Valencia Regional Government (PROMETEO/2020/007), the Spanish Government (PID2022-138245 NB-I00), Fundacion La Caixa (HR21-00824) and Fundacion ICAR (CelMa-ENVEJECE). E. H. laboratory is located at the Instituto de Neurociencias which is a Severo Ochoa Excellence Center CEX2021-001165-S.
Author information
Authors and Affiliations
Contributions
Conceptualization, E.H., M.A-B; Methodology, F.L-R., M.F-N., FJ V-S, M.H, F.M. N-N.; Data analysis and representation, F.L-R., M.F-N., E.H, M.A-B.; Writing, Review & Editing, E.H., M.A-B; Supervision, E.H., M.A-B.; Funding, E.H., M.A-B. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Ethics approval: All animals were treated in compliance with the European Union guidelines for Animal Care and Use for Scientific Purpose (Directive 2010/63/EU), the guidelines from the Association for Research in Vision and Ophthalmology (ARVO) Statement for the Use of Animals in Ophthalmic and Vision Research and ARRIVE and our institutional guidelines. All procedures were approved by the Ethical and Animal Studies Committee of the University of Murcia (approval number: A1320140704, approved the 7 th of May 2014, renewed the 4 th of June 2018, and the 30 th of July 2022, valid until 30 th July 2027) or the Instituto de Neurociencias de Alicante (approval number: 2023-VSC-PEA-0159, approved the 6 th of July 2023).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lucas-Ruiz, F., Fernández-Nogales, M., Valiente-Soriano, F.J. et al. Restorative potential of ciliary body cells in a retinal ganglion cell degeneration model. Sci Rep 15, 15503 (2025). https://doi.org/10.1038/s41598-025-00283-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-00283-0