Abstract
The aim of this study was to investigate the association between persistent nocturnal sleep duration patterns and carotid intima-media thickness (CIMT) in Chinese patients with type 2 diabetes mellitus (T2DM). From March 1, 2018 to August 31, 2023, a cross-sectional study was carried out at the National Metabolic Management Center of the First Affiliated Hospital of Ningbo University. Each patient completed a minimum of three sleep questionnaire assessments during the study period. Group-based trajectory modeling was employed to identify distinct groups of patients exhibiting different trajectories of nocturnal sleep duration. CIMT ≥ 1 mm was used to assess early atherosclerotic changes in arterial structure. Multiple logistic regression was used to assess the association between trajectories of nocturnal sleep duration and CIMT. Three trajectories of nocturnal sleep duration were identified: persistent short (6.44 h: n = 114, 13.5% of all subjects), persistent moderate (7.59 h: n = 500, 59.0%), and persistent long (8.69 h: n = 233, 27.5%). After adjusting for age, sex, education, body mass index, physical activity, current smoking, current alcohol drinking, hypertension, hyperlipidemia, and HbA1c, the odds of CIMT ≥ 1 mm were found to be higher in patients with persistent short nocturnal sleep duration (OR 3.03, 95%CI 1.15, 7.98). However, no significant association was found between persistent long sleep duration at night and CIMT ≥ 1 mm. Persistent short nocturnal sleep duration was associated with increased CIMT in Chinese patients with T2DM. Further longitudinal studies are warranted to fully elucidate this topic.
Similar content being viewed by others
Introduction
The prevalence of type 2 diabetes mellitus (T2DM) presents a significant public health challenge for China, with an estimated 140.9 million adults diagnosed in 20211. The number is expected to 174.4 million by 20451. This growing population faces a heightened risk of atherosclerotic cardiovascular diseases, including coronary artery disease, stroke, and peripheral vascular disease. These complications are major contributors to disability and mortality, accounting for approximately half of all deaths in patients with T2DM2.
Adequate sleep is vital for both physical and mental health, and the American Heart Association identifies the nocturnal sleep duration as one of eight essential components in achieving optimal cardiovascular health3. Studies have established a correlation between sleep duration and cardiovascular health, with both short and long sleep durations associated with increased cardiovascular mortality4,5,6. However, modern lifestyles have demonstrably altered sleep patterns globally, including China, where the average daily sleep duration decreased from 8.2 h in 2010 to 7.6 h in 20187. Notable, individuals with T2DM are more susceptible to sleep problems compared to the general population8,9.
Atherosclerosis is the primary pathological basis for the occurrence of cardiovascular disease (CVD)10. Atherosclerosis, a key contributor to cardiovascular disease (CVD), can manifest as structural changes in arterial walls or functional changes such as arterial stiffness11. Carotid intima-media thickness (CIMT), measured via ultrasound, is a well-established indicator of early atherosclerosis progression and future myocardial infarction or stroke12,13,14. Research findings have varied regarding the link between sleep duration and CIMT15,16,17,18,19,20,21. No study in China has investigated this association in patients with T2DM. Meanwhile, most existing studies on sleep duration and CIMT rely on single-point sleep data15,16,17,18,19,20,21, which may not accurately reflect participants’ long-term sleep habits.
Therefore, this study aimed to utilize trajectory models to explore the association between persistent sleep duration patterns and CIMT in Chinese T2DM patients, focusing on stable sleep categories derived from repeated measurements over three years. Since sleep duration is a modifiable and ubiquitous process, the findings may have practical implications for the prevention of CVD in patients with T2DM.
Materials and methods
Metabolic management center (MMC)
The MMC, led by Ruijin Hospital, provides standardized diagnosis and treatment for adults aged 18 to 75 with various metabolic disorders, including T2DM22. Patients under MMC management are required to attend annual check-ups. To date, over 1000 MMCs have been running across mainland China23. Established in 2018, the First Affiliated Hospital of Ningbo University is the largest branch in Ningbo and a provincial-level center for Zhejiang Province24. From March 1, 2018 to August 31, 2023, 5680 patients with T2DM were managed at this center.
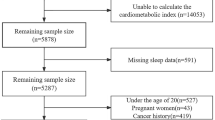
Study design and analytic sample
This cross-sectional study utilized data from the MMC at the First Affiliated Hospital of Ningbo University between March 1, 2018, and August 31, 2023. Patients were eligible for this study if they met the 1999 WHO criteria for T2DM25 and the following additional criteria: (1) Completed the annual sleep questionnaire at least three times; and (2) Had carotid ultrasound examination with CIMT data available at the time of the last sleep questionnaire. Among the 5680 patients with T2DM under MMC management, 847 completed the annual sleep questionnaires at least three times, and 786 underwent carotid ultrasounds with CIMT data. Subsequently, sleep data from 847 patients were used for sleep duration trajectory analysis, and 786 eligible patients were analyzed to explore the association between nocturnal sleep duration trajectories and CIMT (Fig. 1).
Data collection and study variables
Trained nurses conducted in-person interviews using standardized MMC questionnaire to collect data on demographics, behavioral vascular risk factors, and medical history22. Trained hospital staff assessed anthropometric and biochemical parameters following the MMC standardized protocol22. Specifically, the following data were extracted for this study:
-
(1)
Self-reported demographics:
-
(a)
Age.
-
(b)
Sex (male or female).
-
(c)
Education level (below high school, or high school or above).
-
(a)
-
(2)
Self-reported behavioral vascular risk factors.
-
(a)
Current smoking (yes or no; assessed at the time of the last sleep questionnaire).
-
(b)
Current alcohol drinking (yes or no; assessed at the time of the last sleep questionnaire).
-
(c)
Physical activity (low, or moderate/high; assessed at the time of the last sleep questionnaire using the International Physical Activity Questionnaire-Short26).
-
(d)
Nocturnal sleep duration (Assessment conducted during the first MMC visit and at each subsequent annual follow-up. The questionnaire contains the following questions: 1) How did you rate your sleep over the past seven days? Good, bad, or requiring medication for sleep? 2) What were your typical bedtime and wake up times over the past seven days? 3) Did you nap during the past seven days? If so, how long was each nap? Nocturnal sleep duration was obtained by calculating the interval between bedtime and wake-up time).
-
(a)
-
(3)
Medical history.
-
(a)
High blood pressure (yes or no; defined as blood pressure reading on the day of the last sleep data collection of at least 140mmHg systolic and/or 90mmHg diastolic, measured while seated using an automated Omron HBP-1100U monitor27).
-
(b)
Hyperlipidemia (yes or no; defined as meeting any of the following criteria on the day of the last sleep data collection: total cholesterol ≥ 4.5mmol/L and/or triglycerides ≥ 1.7mmol/L (AU5400, Beckman Coulter, USA)28).
-
(a)
-
(4)
Anthropometric and biochemical parameters.
-
(a)
Body mass index (BMI) (< 24 kg/m2, 24 to < 28 kg/m2, or ≥ 28 kg/m229; BMI was calculated by dividing weight in kilograms by the square of height in meters. Weight and height were measured at the time of the last sleep data collection in a standing position with light clothes and without shoes. Weight and height were measured to the nearest 0.1 kg and 0.5 cm, respectively, using calibrated digital scale (HNH-318, Omron, Japan)).
-
(b)
Glycosylated hemoglobin (HbA1c, < 7% or ≥ 7%28; determined at the time of the last sleep data collection using the high-performance liquid chromatographic method on a D-10 Hemoglobin Analyzer (Bio-Rad, USA)).
-
(c)
CIMT (< 1 mm or ≥ 1 mm30; assessed at the time of the last sleep questionnaire using B-mode ultrasound (Resona R9T, Mindray China) by an ultrasound doctor. In a longitudinal view, CIMT appeared as a double line pattern between the intima-lumen and media-adventitia interfaces of the carotid wall. To minimized interindividual variability, measurements were taken on a plaque-free segment (usually distal common carotid artery) at least 5 mm below the carotid bifurcation. To ensure high-quality images for CIMT measurement, a lateral probe position with a 90° insonation angle was used. CIMT was measured three times on a 10 mm segment, preferably on the posterior wall, and the average value was recorded for both left and right sides).
-
(a)
Statistics analyses
All statistical analyses were performed using Python 3.11.5 and Stata 17 for Mac. Group-based trajectory modeling (GBTM) was employed to delineate subgroups of patients exhibiting persistent patterns of nocturnal sleep duration, based on 3–5 annual measurements collected at the first MMC visit and subsequent follow-ups between March 1, 2018, and August 31, 2023, with intervals of approximately one year. The GBTM approach posits the presence of unobserved subpopulations or distinct groups defined by their developmental trajectories across time. This methodology facilitates the estimation of an individual’s likelihood of belonging to a specific group, while also approximating the distribution of trajectories among subpopulations. From a statistical perspective, GBTM involves simultaneously estimating multiple regression models and integrating the information derived from these models to determine the highest probability of an individual’s inclusion within a particular trajectory group. The analysis was conducted using Stata 17, fitting finite (discrete) mixture models to longitudinal data to identify clusters of individuals displaying similar progressions in behavior or outcomes over time. The models utilized the Censored Normal distribution with a cubic polynomial type (order ≤ 3) assigned to each group trajectory in Stata31.
Categorical data were presented as numbers and percentages, while normally distributed continuous variables were presented as means and standard deviations (SD). Inter-group comparisons were conducted using either one-way ANOVA or Chi-square tests, as appropriate. To investigate the association between sleep duration trajectories and CIMT, the following models were employed: (1) Unadjusted model: Simple logistic regression analyses were conducted, with CIMT (≥ 1 mm or < 1 mm) as the dependent variable and sleep duration trajectories as the primary independent variable; (2) Adjusted model: Multiple logistic regression analyses were performed. Model 1 was adjusted for age and sex, while Model 2 included additional adjustments for education, BMI, physical activity, current smoking, and current alcohol drinking. Model 3 further incorporated adjustments for hypertension, hyperlipidemia, and HbA1c. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for each model. Analyses excluded missing data on adjusted variables. Statistical significance was defined as a p-value ≤ 0.05. Sensitivity analyses were conducted as follows: (1) Subgroup analyses were performed by stratifying the fully adjusted Model 3 by sex. (2) CIMT was analyzed as a continuous variable (in millimeters) using multiple linear regression, with sleep duration trajectories as the primary independent variable and the moderate sleep duration group as the reference, adjusted for the same covariates as in Model 3.
Ethics
The study was granted ethical approval by the Research Ethics Committee of the First Affiliated Hospital of Ningbo University (2019-R057). All methods were carried out in accordance with current guidelines and all procedures complied with the requirements of the Declaration of Helsinki. Written informed consent was obtained from all patients, permitting the use of routinely collected data for research purpose.
Results
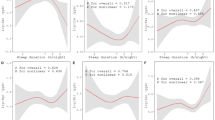
The optimal model eventually identified three trajectories of nocturnal sleep duration: group 1 (persistent short), group 2 (persistent moderate), and group 3 (persistent long). The persistent short nocturnal sleep duration group consisted of 114 patients (13.5%), with an average sleep duration of 6.44 h (SD ± 1.01); the persistent moderate nocturnal sleep duration group consisted of 500 patients (59.0%), with an average sleep duration of 7.59 h (SD ± 0.84); and the persistent long nocturnal sleep duration group consisted of 233 patients (27.5%), with an average sleep duration of 8.69 h (SD ± 0.71). The trajectories of nocturnal sleep duration of the three groups remained relatively stable over time (Fig. 2).
Table 1 reports the comparison of characteristics among the different nocturnal sleep duration trajectories. The mean age was 48.6 years (SD ± 11.8), and 66.7% were male, and 4.3% of them had CIMT ≥ 1 mm. The ages of the patients in the three groups were 49.8 years (SD ± 10.4), 48.3 years (SD ± 11.3), and 48.7 (SD ± 13.5), respectively. There were no significant differences in the constituent ratio of sex, education, BMI, physical activities, current smoking, current alcohol drinking, hypertension, hyperlipidemia, HbA1c, and CIMT across the group.
Table 2 reports the results of the single logistic regression analysis. Without adjustment and considering a significance level of p ≤ 0.05, CIMT ≥ 1 mm was found to be associated with age, sex, current smoking, current alcohol drinking, hypertension, hyperlipidemia, HbA1c, and nocturnal sleep duration trajectories.
Table 3 reports the multiple logistic regression results of nocturnal sleep duration trajectories (with persistent moderate nocturnal sleep duration group as the reference) and CIMT ≥ 1 mm in patients with T2DM. After adjusting for age and sex (model 1), the odds of CIMT ≥ 1 mm were found to be higher in patients with persistent short nocturnal sleep duration (OR 2.78, 95%CI 1.10 to 7.02). With additional adjustments in Model 2 for education, BMI, physical activity, current smoking, and current alcohol drinking, the odds of CIMT ≥ 1 mm were found to be higher in patients with persistent short nocturnal sleep duration (OR 2.84, 95%CI 1.10, 7.32). The fully adjusted Model 3 yielded similar results (OR 3.03, 95%CI 1.15, 7.98). However, no significant association was observed between persistent long nocturnal sleep duration and CIMT ≥ 1 mm.
The results of the sensitivity analyses were consistent with the primary analysis. In sex-stratified subgroup analyses (fully adjusted Model 3), the OR of CIMT ≥ 1 mm in the persistent short nocturnal sleep duration group (with persistent moderate nocturnal sleep duration group as reference) was 2.50 (95% CI 1.02 to 6.15) among men and 3.88 (95% CI 0.37 to 40.98) among women. For the persistent long nocturnal sleep duration group, the OR was 2.11 (95% CI 0.94 to 4.77) in men and 2.09 (95% CI 0.30 to 14.56) in women. When treating CIMT as a continuous variable (in millimeters), the persistent short nocturnal sleep duration group showed a significant association with higher CIMT (β = 0.0477, 95% CI 0.013 to 0.082), whereas the persistent long nocturnal sleep duration group did not (β = 0.0028, 95% CI − 0.023 to 0.029).
Trajectories of nocturnal sleep duration of the total participants. The solid lines are the predicted nocturnal sleep duration trajectory, and the dashed lines are the 95% confidence interval. Group 1 indicates persistent short nocturnal sleep duration (114 individuals, 13.5%); group 2, persistent moderate nocturnal sleep duration (500 individuals, 59.0%); and group 3, persistent long nocturnal sleep duration (233 individuals, 27.5%).
Discussion
Using longitudinal data with repeated measurement of sleep duration, three heterogeneous trajectories of nocturnal sleep duration were identified. We observed that a trajectory of persistent short nocturnal sleep duration, compared to moderate sleep duration, was associated with a greater likelihood of having CIMT ≥ 1 mm in patients with T2DM. Conversely, no significant association was found between a trajectory of persistent long sleep duration and CIMT ≥ 1 mm.
Previous researches have demonstrated a correlation between sleep duration and CIMT in the non-diabetic population, but limited data are available for patients with T2DM. Our results in patients with T2DM, a population with a high prevalence of sleep disturbances and increased risk of cardiovascular disease2,8,9, are consistent with previous studies. A cross-sectional association between short sleep duration and greater CIMT in middle-aged adults in the US18, older adults (≥ 65 years) in Japan19, and adolescents in Hongkong17, has been established. Another study in the Greek community found that those who slept < 6 h had maximum CIMT among all subjects15. In our study, a persistent average sleep duration of 6.44 h was associated with CIMT ≥ 1 mm. CIMT is one of the quantitative indicators reflecting early atherosclerosis and can effectively predict the occurrence of future cardiovascular events32. Our findings suggest that even a small but persistent reduction in persistent sleep duration may contribute to the progression of early atherosclerosis. This has been supported by a recent study from Thurston et al., who reported an increased risk of cardiovascular disease associated with persistent short sleep duration (≤ 5 h) over 20 years33.
Our study found no significant association between persistent long sleep duration and CIMT ≥ 1 mm in Chinese patients with T2DM, unlike some previous observational studies that reported an association between long sleep duration and increased CIMT among adults in Germany21, community residents in Japan20, and police officers in New York34. These differences may stem from variations in study populations and methodological approaches. Unlike prior studies, which often involved non-diabetic populations and relied on single-point sleep duration measurements, our study focused on T2DM patients and utilized trajectory modeling to capture persistent sleep patterns over three years. Additionally, the definition of long sleep duration in our study (8.69 h) was lower than thresholds used in some prior research (e.g., 11–12 h in the study conducted in Germany), and our reference group (mean 7.59 h) aligns with current sleep recommendations35, potentially reducing the contrast with long sleep duration compared to studies using shorter reference durations (e.g., 6 h in the Japanese community residents study20).
The biological mechanisms linking short nocturnal sleep duration and CIMT in patients with T2DM remain unclear. Studies have shown that short sleep duration is associated with obesity36, hypertension37, dyslipidemia38, and poor glycemic control39, which are all traditional risk factors for atherosclerosis. Therefore, these factors may mediate the relationship between short sleep duration and CIMT. However, even after adjusting for these factors, persistent short sleep duration remained significantly associated with CIMT. This suggests that the relationship between short sleep duration and CIMT may be partially explained by these traditional atherosclerosis risk factors. Short sleep duration may also impact CITM through other pathways. Researches have indicated that short sleep duration can lead to chronic, system low-grade inflammation40, impair endothelial function41,42, and increased nocturnal catecholamine concentrations43. Additionally, there is evidence suggesting that sleep deprivation can lead to significant metabolic and neuroendocrine alterations, including elevated evening cortisol and thyrotropin levels44. These physiological mechanisms, not assessed in the present study, warrant consideration in future research.
A key strength of this study is the use of GBTM to identify persistent sleep duration patterns in T2DM patients based on repeated measurements. Although sleep duration remained relatively stable within groups, these repeated assessments confirmed the consistency of habitual sleep behavior in this population, enhancing the reliability of our classifications and highlighting their potential relevance to chronic outcomes like atherosclerosis. To the best knowledge of authors, this is the first study in China to investigate the relationship between sleep duration trajectories and CIMT among patients with T2DM. However, our study has certain limitations. First, our analyses are cross-sectional, which limits our ability to infer the directionality or causality of any relationship between sleep duration and CIMT. Second, this study is based on data from a single MMC center, limiting the generalizability of its findings. Future research should consider utilizing data from all MMCs across China to clarify the association between sleep duration and atherosclerosis. Third, the current study did not consider the influence of other features of sleep, such as sleep regularity, efficiency, quality, and sleep-disordered breathing, and these need to be further explored. Finally, our study did not adjust for the use of certain medications, such as hypnotics that could influence sleep duration, as well as antidiabetic agents (e.g., GLP-1 receptor agonists), antihypertensives, antiplatelet and statins that could influence CIMT, due to regimen changes over the 3-5-year period, which precluded reliable classification. Future studies with detailed, time-updated medication data could further explore these effects45,46.
Conclusions
Our study of Chinese patients with T2DM revealed an association of persistent short sleep duration with elevated CIMT. Further longitudinal study is warranted to fully elucidate this topic.
Data availability
The dataset will be available upon request unless there are legal or ethical reasons for not doing so. Study data are available on reasonable request to the corresponding author.
References
Sun, H. et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119 (2022).
Einarson, T. R., Acs, A., Ludwig, C. & Panton, U. H. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc. Diabetol. 17 (1), 83 (2018).
Lloyd-Jones, D. M. et al. Life’s essential 8: updating and enhancing the American heart association’s construct of cardiovascular health: a presidential advisory from the American heart association. Circulation 146 (5), e18–e43 (2022).
Jin, Q. et al. Association of sleep duration with all-cause and cardiovascular mortality: a prospective cohort study. Front. Public. Health. 10, 880276 (2022).
Han, H. et al. Sleep duration and risks of incident cardiovascular disease and mortality among people with type 2 diabetes. Diabetes Care. 46 (1), 101–110 (2023).
Tao, F. et al. Associations of sleep duration and quality with incident cardiovascular disease, cancer, and mortality: a prospective cohort study of 407,500 UK biobank participants. Sleep. Med. 81, 401–409 (2021).
Chu, Y. et al. Temporal trends in sleep pattern among Chinese adults between 2010 and 2018: findings from five consecutive nationally representative surveys. Public. Health. 225, 360–368 (2023).
Narisawa, H. et al. Prevalence, symptomatic features, and factors associated with sleep disturbance/insomnia in Japanese patients with type-2 diabetes. Neuropsychiatr Dis. Treat. 13, 1873–1880 (2017).
Maimaitituerxun, R. et al. Sleep quality and its associated factors among patients with type 2 diabetes mellitus in Hunan, China: a cross-sectional study. BMJ Open. 14 (2), e078146 (2024).
Veerasamy, M. et al. Association of aging, arterial stiffness, and cardiovascular disease: a review. Cardiol. Rev. 22 (5), 223–232 (2014).
Palombo, C. & Kozakova, M. Arterial stiffness, atherosclerosis and cardiovascular risk: pathophysiologic mechanisms and emerging clinical indications. Vascul Pharmacol. 77, 1–7 (2016).
Grobbee, D. E. & Bots, M. L.Carotid artery intima-media thickness as an indicator of generalized atherosclerosis. J. Intern. Med. 236 (5), 567–573 (1994).
Ou, Q., Zhang, J., Wen, X., Yang, L. & Tao, L. Clinical significance of carotid intima-media thickness and plasma homocysteine in acute ST-segment elevation myocardial infarction. Cardiovasc. Diagn. Ther. 13 (6), 917–928 (2023).
Kumar, P. et al. CIMT as a risk factor for stroke subtype: A systematic review. Eur. J. Clin. Invest. 50 (11), e13348 (2020).
Oikonomou, E. et al. The impact of sleeping duration on atherosclerosis in the community: insights from the corinthia study. Sleep. Breath. 25 (4), 1813–1819 (2021).
Suzuki, S. et al. Self-reported sleep duration and subclinical atherosclerosis in a general population of Japanese men. J. Atheroscler Thromb. 25 (2), 186–198 (2018).
Li, J. W. S. et al. Short sleep duration is weakly associated with carotid intima-media thickness in adolescents. J. Pediatr. 195, 80–84 (2018).
Sands, M. R. et al. Short sleep duration is associated with carotid intima-media thickness among men in the coronary artery risk development in young adults (CARDIA) study. Stroke 43 (11), 2858–2864 (2012).
Nakazaki, C. et al. Association of insomnia and short sleep duration with atherosclerosis risk in the elderly. Am. J. Hypertens. 25 (11), 1149–1155 (2012).
Abe, T., Aoki, T., Yata, S. & Okada, M. Sleep duration is significantly associated with carotid artery atherosclerosis incidence in a Japanese population. Atherosclerosis 217 (2), 509–513 (2011).
Wolff, B. et al. Relation of self-reported sleep duration with carotid intima-media thickness in a general population sample. Atherosclerosis 196 (2), 727–732 (2008).
Zhang, Y., Wang, W. & Ning, G. Metabolic management center: an innovation project for the management of metabolic diseases and complications in China. J. Diabetes. 11 (1), 11–13 (2019).
National Metabolic Management Center. MMC Breaks Through 1000 Milestone. http://national-mmc.com/ (2022).
The First Affiliated Hospital of Ningbo University. Hospital has been Awarded the Honorary title of Provincial-Level National Metabolic Management Center and Provincial-Level Model Center. http://www.nbdyyy.com/art/2021/11/4/art_80_633223.html (2021).
Alberti, K. G. & Zimmet, P. Z. .Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. 15 (7), 539–553 (1998).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35 (8), 1381–1395 (2003).
Liu, J. Highlights of the 2018 Chinese hypertension guidelines. Clin. Hypertens. 26, 8 (2020).
Jia, W. et al. Standards of medical care for type 2 diabetes in China 2019. Diabetes Metab. Res. Rev. 35 (6), e3158 (2019).
Pan, X. F., Wang, L. & Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 9 (6), 373–392 (2021).
Naqvi, T. Z. & Lee, M. S. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc. Imaging. 7 (10), 1025–1038 (2014).
NaginD. S. Group-based trajectory modeling: an overview. Ann. Nutr. Metab. 65 (2-3), 205–210 (2014).
Willeit, P. et al. Carotid intima-media thickness progression as surrogate marker for cardiovascular risk: meta-analysis of 119 clinical trials involving 100 667 patients. Circulation 142 (7), 621–642 (2020).
Thurston, R. C. et al. Trajectories of sleep over midlife and incident cardiovascular disease events in the study of women’s health across the Nation. Circulation 149 (7), 545–555 (2024).
Ma, C. C. et al. Associations of objectively measured and self-reported sleep duration with carotid artery intima media thickness among Police officers. Am. J. Ind. Med. 56 (11), 1341–1351 (2013).
Watson, N. F. et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American academy of sleep medicine and sleep research society. Sleep 38 (6), 843–844 (2015).
Chaput, J. P. et al. The role of insufficient sleep and circadian misalignment in obesity. Nat. Rev. Endocrinol. 19 (2), 82–97 (2023).
Li, C. & Shang, S. Relationship between sleep and hypertension: findings from the NHANES (2007–2014). Int. J. Environ. Res. Public. Health. 18 (15), 7867 (2021).
Liang, Y. Y. et al. Association between sleep duration and metabolic syndrome: linear and nonlinear Mendelian randomization analyses. J. Transl Med. 21 (1), 90 (2023).
Lee, S. W. H., Ng, K. Y. & Chin, W. K. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: A systematic review and meta-analysis. Sleep. Med. Rev. 31, 91–101 (2017).
Besedovsky, L., Lange, T. & Haack, M. The sleep-immune crosstalk in health and disease. Physiol. Rev. 99 (3), 1325–1380 (2019).
Cherubini, J. M., Cheng, J. L., Williams, J. S. & MacDonald, M. J. Sleep deprivation and endothelial function: reconciling seminal evidence with recent perspectives. Am. J. Physiol. Heart Circ. Physiol. 320 (1), H29–35 (2021).
Bain, A. R. et al. Insufficient sleep is associated with impaired nitric oxide-mediated endothelium-dependent vasodilation. Atherosclerosis 265, 41–46 (2017).
Irwin, M., Thompson, J., Miller, C., Gillin, J. C. & Ziegler, M. Effects of sleep and sleep deprivation on catecholamine and interleukin-2 levels in humans: clinical implications. J. Clin. Endocrinol. Metab. 84 (6), 1979–1985 (1999).
Spiegel, K., Leproult, R. & Van Cauter, E. Impact of sleep debt on metabolic and endocrine function. Lancet 354 (9188), 1435–1439 (1999).
Morrison, A. M., Sullivan, A. E. & Aday, A. W. Atherosclerotic disease: pathogenesis and approaches to management. Med. Clin. North. Am. 107 (5), 793–805 (2023).
Wilt, T. J. et al. Pharmacologic treatment of insomnia disorder: an evidence report for a clinical practice guideline by the American college of physicians. Ann. Intern. Med. 165 (2), 103–112 (2016).
Acknowledgements
The authors thank Yanshu Chen and Miao Chen for managing the data.
Funding
This work was supported by the Medical Health Science and Technology Project of Zhejiang Province (Grant No. 2024KY1506), Ningbo Key Clinical Specialty (Endocrinology) (Grant No. 2022-B07), and Ningbo Top Medical and Health Research Program (Grant No.2023020713).
Author information
Authors and Affiliations
Contributions
JL and XP designed the study. MX cleaned the dataset. XP analyzed the data. XM and JL wrote the first draft of the manuscript. XM, XP, MX, LL and JL revised the article critically for important intellectual content and approved the final version. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was granted ethical approval by the Research Ethics Committee of the First Affiliated Hospital of Ningbo University (2019-R057). All methods were carried out in accordance with current guidelines and all procedures complied with the requirements of the Declaration of Helsinki. Written informed consent was obtained from all patients, permitting the use of routinely collected data for research purpose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, X., Pan, X., Xu, M. et al. Association between persistent nocturnal sleep duration patterns and carotid intima-media thickness in Chinese patients with type 2 diabetes. Sci Rep 15, 16573 (2025). https://doi.org/10.1038/s41598-025-00785-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-00785-x