Abstract
The link between cardiometabolic markers and hepatic steatosis and liver fibrosis in non-hypertensive, non-diabetic populations remains unclear. A study was conducted using data from the National Health and Nutrition Examination Survey. Hepatic steatosis and liver fibrosis were assessed using vibration-controlled transient elastography. Logistic regression and restricted cubic splines (RCS) were used to evaluate the associations of cardiometabolic index (CMI), atherogenic index of plasma (AIP), triglyceride-glucose index (TyG), and estimated glucose disposal rate (eGDR) on hepatic steatosis and estimated fibrosis. Mediation analysis examined the role of insulin resistance (HOMA-IR) and liver enzymes. Among 1489 participants, 39.15% had hepatic steatosis and 2.82% had liver fibrosis. Higher CMI (OR = 3.967, 95%CI: 2.297, 6.851), AIP (OR = 3.255, 95%CI: 2.031, 5.216), TyG (OR = 3.689, 95%CI: 2.363, 5.760), and FLI (OR = 2.695, 95%CI: 1.997, 7.816) tertiles of Q3 were linked to increased hepatic steatosis odds, while eGDR reduced odds (OR = 0.217, 95%CI: 0.127, 0.373). The AUC values of these four cardiac markers were greater than FLI, among which eGDR showed the highest predictive value (AUC = 0.781). In the hepatic steatosis population, CMI (OR = 1.419, 95%CI: 1.033, 2.747), AIP (OR = 5.527, 95%CI: 1.082, 28.242), and TyG (OR = 2.345, 95%CI: 1.180, 4.661) were also showed significant association with liver fibrosis, while eGDR and FIB-4 were not associated with liver fibrosis. AIP had the highest discriminative ability for liver fibrosis (AUC = 0.798). Mediation analysis showed HOMA-IR mediated 25.50%~36.20% of cardiometabolic markers’ associations with hepatic steatosis, followed by liver enzymes. Cardiometabolic markers are strongly linked to hepatic steatosis and liver fibrosis in populations without traditional risk factors, even outperforming the established hepatic steatosis and the fibrosis marker, highlighting their potential for early liver disease risk identification in seemingly healthy individuals.
Similar content being viewed by others
Introduction
Non-alcoholic fatty liver disease (NAFLD), recently renamed as metabolic dysfunction-associated steatotic liver disease (MASLD), has emerged as a major public health challenge, affecting approximately 27.7% of the adult population in the United States1. The disease spectrum ranges from simple steatosis to liver fibrosis, which is characterized by excessive deposition of extracellular matrix components and persistent activation of inflammatory response2. Beyond its hepatic manifestations, NAFLD/MASLD is increasingly recognized as a multisystem disorder with significant cardiovascular implications34;, and there is heterogeneity in this relationship56;. Recent epidemiological studies have revealed particularly high disease burden in specific populations, with prevalence rates exceeding 40% among Mexican Americans1. Of particular concern, liver fibrosis has been identified as a major determinant for chronic liver disease progression and is strongly associated with increased risk of insulin resistance and metabolic complications7. The complex relationship between NAFLD/MASLD, liver fibrosis, insulin resistance, and cardiometabolic risk underscores the critical importance of early identification and intervention8.
Cardiometabolic markers, including the cardiometabolic index (CMI), atherogenic index of plasma (AIP), triglyceride-glucose index (TyG), and estimated glucose disposal rate (eGDR), have gained prominence in assessing metabolic health and predicting cardiovascular and liver diseases. CMI, which combines obesity and lipid parameters, has been used for risk assessment in diabetes and cardiovascular diseases9. AIP, the logarithm of the triglyceride-to-HDL cholesterol ratio, has shown a strong association with hepatic steatosis10. The TyG index, derived from triglycerides and fasting glucose, serves as a robust marker of insulin resistance and is linked to the development of non-alcoholic fatty liver disease (NAFLD), even in non-obese individuals11. eGDR, a measure of insulin sensitivity, is associated with liver stiffness and fibrosis in NAFLD patients12. These potential associations may be related to the fact that obesity and diabetes are important risk factors for hepatic steatosis and hepatic fibrosis1314;. Among all the components of metabolic syndrome, obesity and diabetes are the factors that have the most significant impact on the severity of fatty liver disease and liver fibrosis15. However, whether these metabolic indices are still associated with hepatic steatosis and fibrosis in populations without obesity and diabetes has not been clarified. Furthermore, it is also unclear whether these cardiometabolic markers are superior to established markers of hepatic steatosis, such as fatty liver index (FLI) and fibrosis, such as fibrosis-4 index (FIB-4). Investigating these markers in such populations is crucial, as they are perhaps at other risk for liver-related complications despite the absence of traditional risk factors like obesity and diabetes.
The present study aimed to examine the associations of cardiometabolic markers (CMI, AIP, TyG, and eGDR) with hepatic steatosis and liver fibrosis in a population without obesity and diabetes from NHANES, and to compare them with established markers (FLI and FIB-4). Furthermore, we investigated the mediating effects of insulin resistance and liver function parameters in these relationships. Our findings could provide insights into the early pathophysiological mechanisms linking cardiometabolic dysfunction to liver disease and identify potential targets for early intervention.
Result
Patient characteristics
The baseline characteristics of the study population are presented in Table 1 and sTable 1. Among 1489 participants, 572 (39.15%) had hepatic steatosis and 41 (2.82%) had liver fibrosis. For hepatic steatosis, patients were older and male compared with controls (all P < 0.001). The CMI, AIP and TyG showed higher levels in hepatic steatosis when compared to control groups (all P < 0.001); while eGDR was lower in hepatic steatosis group (P < 0.001). For liver fibrosis, similar but more pronounced alterations in these indices were observed.
Cardiometabolic markers and liver steatosis
Table 2 presents the multivariable-adjusted associations between cardiometabolic markers and hepatic steatosis. After full adjustment in Model 3, CMI (OR = 3.877, 95%CI: 2.252, 6.674), AIP (OR = 5.261, 95%CI: 2.818, 9.819), TyG (OR = 2.738, 95%CI: 2.021, 3.710), and FLI (OR = 1.041, 95%CI: 1.028,1.054) showed positive associations with hepatic steatosis, while eGDR (OR = 0.771, 95%CI: 0.696, 0.854) demonstrated a negative association (all P < 0.001). Compared with the lowest tertiles(Q1), participants in the highest quartile (Q3) had significantly higher odds of hepatic steatosis for CMI (OR = 3.967, 95%CI: 2.297, 6.851), AIP (OR = 3.255, 95%CI: 2.031, 5.216), TyG (OR = 3.689, 95%CI: 2.363, 5.760), and FLI (OR = 2.695, 95%CI: 1.997,7.816) while showing lower odds for eGDR (OR = 0.217, 95%CI: 0.127, 0.373).
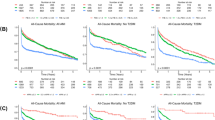
The receiver operating characteristic (ROC) curves (sFigure 1) demonstrated that the AUC values of these four cardiac markers were greater than FLI, among which eGDR showed the highest predictive value (AUC = 0.781). Restricted cubic spline analyses (Fig. 1) revealed linear associations of AIP and TyG with hepatic steatosis (P for nonlinearity > 0.05), while CMI and eGDR showed a nonlinear relationship (P for nonlinearity < 0.05).
Nonlinear associations of cardiometabolic markers with hepatic steatosis and liver fibrosis in population without obesity and diabetes. Nonlinear associations of CMI (A), AIP (C), TyG (E) and eGDR (G) with hepatic steatosis. Nonlinear associations of CMI (B), AIP (D), TyG (F) and eGDR (H) with hepatic fibrosis. CMI: Cardiac metabolic index; AIP: Atherogenic index of plasma; TyG: Triglyceride glucose index; eGDR: Estimated glucose disposal rate.
Cardiometabolic markers and liver fibrosis
The associations between cardiometabolic markers and liver fibrosis were examined in the overall population and hepatic steatosis subgroup (sTables 2 and 3). In the overall population, after fully adjusting for potential confounders in Model 3, the four cardiometabolic markers were not significant associated with liver fibrosis (sTable 2). In the hepatic steatosis population, CMI (OR = 1.419, 95%CI: 1.033, 2.747), AIP (OR = 5.527, 95%CI: 1.082, 28.242), and TyG (OR = 2.345, 95%CI: 1.180, 4.661) were showed significant association with liver fibrosis, while eGDR and FIB-4 were not associated with liver fibrosis. Compared with the lowest tertiles(Q1), only Q3 of AIP (OR = 5.331, 95%CI: 1.063, 26.734) show an association with liver fibrosis when compared to Q1. ROC curve analyses (sFigure 1) indicated that AIP had the highest discriminative ability for liver fibrosis (AUC = 0.798). The restricted cubic spline analyses (Fig. 1) revealed linear relationship between AIP and liver fibrosis (P for nonlinearity > 0.05), and nonlinear associations of CMI and TyG on liver fibrosis (P for nonlinearity < 0.05).
Subgroup analysis
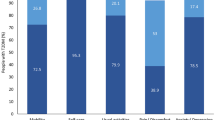
Stratified analyses were conducted to explore potential effect modifications in the associations between cardiometabolic markers and hepatic steatosis (sTable 3–6). For these cardiometabolic markers, stronger associations with hepatic steatosis were observed in patients aged 20–40 years, female, Non-Hispanic black, those with less than high school education, no married, former smokers, no drinking, and those with no physical activity.
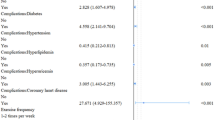
Mediation analysis
Mediation analyses were performed to explore potential mediating effects of insulin resistance (HOMA-IR), and liver enzymes (ALT, AST, GGT) in the associations between cardiometabolic markers and steatosis (Fig. 2, sTable 7–10). Mediation analysis identified HOMA-IR as the primary mediator linking cardiometabolic markers to hepatic steatosis, accounting for 25.50%~36.20% of the effects of (all P < 0.001). ALT further mediated 7.18%~12.45% of the effects of cardiometabolic markers on hepatic steatosis.
Mediating proportions of insulin resistance, and liver function in the association of cardiometabolic markers with hepatic steatosis. Mediating proportions of insulin resistance, liver function, and inflammatory response in the association of CMI (A), AIP (B), TyG (C) and eGDR (D) with hepatic steatosis. CMI: Cardiac metabolic index; AIP: Atherogenic index of plasma; TyG: Triglyceride glucose index; eGDR: Estimated glucose disposal rate; HOMA-IR: Homeostasis model assessment of insulin resistance; ALT: Alanine transaminase; AST: Aspartate transaminase; GGT: Gamma-glutamyl transferase; hsCRP: High-sensitivity C-reactive protein. *P < 0.05,**P < 0.001.
Sensitive analysis
The robustness of our findings was verified through several sensitivity analyses (sTable 12-sTable 19). After imputation of missing values, exclusion of participants with ASCVD, use of CBPS method and application of unweighted logistic regression, the associations between cardiometabolic markers and hepatic outcomes remained largely consistent with our primary analyses. Specifically, in all sensitivity analyses, higher levels of CMI, AIP, and TyG maintained significant positive associations with hepatic steatosis, while higher eGDR consistently showed inverse associations. Similar patterns were observed for the assocations of eGDR with liver fibrosis.
Discussion
In this large population-based study of individuals without obesity and diabetes, we comprehensively evaluated the associations of cardiometabolic markers (CMI, AIP, TyG, and eGDR) on hepatic steatosis and liver fibrosis. We found that elevated levels of CMI, AIP, and TyG were significantly associated with increased risk of hepatic steatosis, while higher eGDR showed protective effects. Moreover, in this specific population, the correlation of these four cardiometabolic markers with hepatic steatosis was stronger than that of the established hepatic steatosis marker, FLI. Additionally, in the non-obese and non-diabetic population with hepatic steatosis, CMI, AIP, and TyG were significantly associated with hepatic fibrosis, while this relationship was not observed with the known fibrosis marker FIB-4. This is the first study to evaluate these cardiometabolic markers in relation to hepatic steatosis and estimated fibrosis in a population without traditional risk factors, providing valuable insights into early liver disease risk identification in apparently healthy individuals.
Our findings are both consistent with and extend beyond previous studies examining cardiometabolic markers in liver disease. Recent cross-sectional studies have shown that elevated CMI was independently associated with NAFLD and liver fibrosis in the general population1617;. Similarly, several studies have demonstrated that elevated AIP was significantly associated with increased NAFLD risk1819;. A meta-analysis by Wang et al.20 revealed that TyG index exhibited good diagnostic performance for MAFLD with an area under ROC curve of 0.75 (0.71–0.79). For eGDR, Song et al.21reported its inverse association with mortality risk in NAFLD patients (Q4 vs. Q1, HR = 0.65, 95%CI 0.48–0.89). However, our study makes several novel contributions. First, while previous research mainly focused on general populations or those with established metabolic disorders2223;, we specifically investigated a population without traditional risk factors (obesity and diabetes), providing insights into early identification of liver disease risk. Second, compared to studies examining individual markers, we comprehensively evaluated multiple cardiometabolic markers simultaneously and found that eGDR demonstrated the strongest and most consistent association with hepatic steatosis and estimated fibrosis in this specific population. Third, we found that the predictive value of cardiometabolic markers on hepatic steatosis and fibrosis was superior to that of the established hepatic steatosis marker (FLI) and the fibrosis marker (FIB-4), in population without obesity and diabetes.
Our study demonstrated significant associations between cardiometabolic markers and liver pathology in individuals without traditional risk factors, with substantial mediating effects through insulin resistance and liver enzymes. The mediation analysis revealed that HOMA-IR accounted for 25.50%~36.20% of these associations, while liver enzymes contributed 7.18%~12.45%. These findings align with recent evidence from metabolic pathway studies. Insulin resistance has been recognized as a central mediator, accounting for up to 85% of the association between metabolic disorders and NAFLD development24. Insulin resistance, even in individuals without diabetes or hypertension, is a critical aspect of metabolic syndrome2526;. Therefore, in individuals without obesity and diabetes, cardiometabolic indicators also influence the occurrence and progression of fatty liver disease and liver fibrosis through insulin resistance. The metabolic dysregulation triggers a cascade of pathophysiological changes, primarily through insulin signaling disruption and liver enzymes release2728;. The molecular mechanisms underlying these associations involve complex cellular and signaling pathways. At the cellular level, metabolic stress initiates mitochondrial dysfunction and oxidative stress, leading to increased production of reactive oxygen species (ROS) and persistent activation of inflammatory response29. This process is mediated through endoplasmic reticulum stress, which directly affects liver function and insulin resistance30. Recent studies have identified key mechanistic pathways: regulatory T cells produce amphiregulin (Areg) that promotes liver fibrosis through EGFR signaling on hepatic stellate cells while exacerbating insulin resistance via IL-6-dependent pathways31; the liver-gut axis interacts with mitochondrial stress to accelerate disease progression32; and redox-dependent pathways maintain pro-inflammatory and pro-fibrotic signaling in hepatic stellate cells through various transcription factors including NF-κB33. These pathological changes are further complicated by alterations in systemic inflammation markers and adipocytokines34, creating a complex network of metabolic and inflammatory perturbations that can initiate and perpetuate liver damage even before the development of traditional cardiovascular risk factors.
Our stratified analyses revealed significant effect modifications in the associations between cardiometabolic markers and hepatic outcomes. The stronger associations of cardiometabolic markers with hepatic steatosis in younger participants (aged 20–40 years) may reflect earlier onset of metabolic dysfunction in this age group, as supported by Jung et al.24 who identified age-specific patterns in metabolic regulation. The pronounced gender differences, particularly stronger associations of cardiometabolic markers in females, align with findings from Arefhosseini et al.34 demonstrating distinct inflammatory profiles between sexes in early-stage liver disease. These findings emphasize the need for targeted screening strategies in specific demographic subgroups, particularly among younger individuals, females, and those with obesity, even in the absence of traditional cardiovascular risk factors.
Our study provides novel insights into the relationship between cardiometabolic markers and liver disease progression in individuals without traditional risk factors.
This study has significant public health implications. It highlights the importance of cardiometabolic markers in identifying early liver disease risk among individuals who are seemingly healthy but may be at risk due to underlying cardiometabolic abnormalities, and may be superior to the established hepatic steatosis marker (FLI) and the fibrosis marker (FIB-4). In the general population, many people may not be aware that they are at risk of liver diseases such as hepatic steatosis and fibrosis, especially if they do not have obvious risk factors like obesity and diabetes. The findings suggest that routine screening of cardiometabolic markers could help in early detection of hepatic steatosis and potentially fibrosis, allowing for timely interventions to prevent disease progression. This is particularly important because early-stage liver diseases are often asymptomatic, and by the time symptoms appear, the condition may have advanced significantly. Our findings contribute to the growing evidence supporting the use of non-invasive biomarkers in MASLD diagnosis, addressing the need for reliable screening tools beyond liver biopsy35. The integration of these findings into clinical practice could transform our approach to early disease detection in apparently healthy populations.
The present study has several notable strengths. First, our innovative focus on individuals without established metabolic disorders provides unique insights into the early pathophysiological changes that may precede clinical manifestations of liver disease. This approach is particularly valuable as it helps identify potential intervention windows before the development of more severe metabolic complications. Second, our comprehensive assessment of multiple cardiometabolic markers provides a more nuanced understanding of the metabolic perturbations associated with liver disease progression. Third, we employed validated non-invasive markers for liver disease assessment, which as highlighted by Abdelhameed et al.30, are increasingly recognized as reliable tools for population-based studies.
Several limitations of our study should be acknowledged. First, the cross-sectional design prevents us from establishing causal relationships between cardiometabolic markers and liver disease progression. Based on the cross-sectional design of the study and other limitations (e.g. lack of precise phenotyping), we cannot imply that insulin resistance (systemic and/or hepatic) is promoting hepatic steatosis and fibrosis, as MASLD also induces/worsens insulin resistance36. Second, while we utilized well-validated non-invasive markers, the lack of liver biopsy confirmation remains a limitation, as current non-invasive methods may not fully capture the complexity of liver pathology37. In the absence of liver biopsy data, VCTE, as a non-invasive diagnostic method, has been recommended by multiple studies for the non-invasive assessment of hepatic steatosis and fibrosis. One of the main reasons for the lower accuracy of VCTE is obesity. In obese individuals, the thick subcutaneous fat can interfere with the propagation of shear waves, leading to inaccurate measurement results. In our study, however, focused on a non-obese and non-diabetic population, which effectively addressed this limitation. Third, our study population, although large, may not be fully representative of all ethnic and demographic groups, potentially limiting the generalizability of our findings. Additionally, we could not account for all potential confounding factors, such as detailed dietary patterns and genetic variations, which might influence both cardiometabolic markers and liver disease development. Future longitudinal studies incorporating more diverse populations and additional environmental and genetic factors are needed to validate our findings and establish temporal relationships between these markers and liver disease progression.
In conclusion, our study demonstrates that cardiometabolic markers are significantly associated with hepatic steatosis and liver fibrosis in individuals without obesity and diabetes, even outperforming the established hepatic steatosis marker and the fibrosis marker, highlighting the importance of early metabolic screening even in apparently healthy populations. These findings extend current understanding of MASLD pathogenesis by revealing that metabolic perturbations may precede clinically evident disease, supporting the recent paradigm shift in fatty liver disease conceptualization.
Method
Study design and participants
We conducted a cross-sectional study using data from the National Health and Nutrition Examination Survey (NHANES) 2017–2020. NHANES is a nationally representative survey of the civilian, non-institutionalized U.S. population, designed to assess the health and nutritional status of adults and children. Data were collected through personal interviews, health examinations at mobile examination centers, and laboratory analyses (https://www.cdc.gov/nchs/nhanes/index.html). The study was approved by the National Center for Health Statistics Ethics Review Board, and informed written consent was obtained from all participants.
Our study focused on adults aged 20 years or older who were free from obesity and diabetes. The diagnostic criteria for diabetes are38: being told by a doctor that you have diabetes, an HbA1c level of ≥ 6.5%, a fasting glucose level of ≥ 7.0 mmol/L, a random blood glucose level of ≥ 11.1 mmol/L, a two - hour OGTT blood glucose level of ≥ 11.1 mmol/L, or the use of diabetes medication or insulin. Obesity is defined as a BMI of ≥ 30 kg/m239. A total of 5170 participants were excluded (2504 people were obesity but had no diabetes, 698 people were not obesity but had diabetes, 1030 people were both had obesity diabetes, and 938 had no enough information to determine obesity or diabetes), and 4458 individuals met these criteria. From this group, we excluded participants: (1) who lacked sufficient information to calculate the cardiometabolic markers (CMI, AIP, TyG, eGDR); (2) missing data on LSM and CAP; (3) with missing fasting blood glucose or those with a weight of 0; (4) with viral hepatitis, autoimmune hepatitis, liver tumors, other liver diseases; (5) missing covariates. The participant selection process is depicted in Fig. 3.
Cardiometabolic biomarker calculations
Cardiometabolic biomarker consisted of CMI, AIP, TyG, and eGDR. FLI and FIB-4, as established markers of liver steatosis and fibrosis, were also included in the analysis. Then, these indices were grouped according to tertiles.
CMI=(TG/HDL-C)×(waist circumference/height)9.
AIP = log10[TG (mmol/L)/HDL-C (mmol/L)]10.
TyG = ln[fasting TG (mg/dL)×fasting glucose (mg/dL)/2]11.
eGDR = 21.158−(0.09×waist circumference)−(3.407×hypertension)−(0.551×HbA1c)12.
FLI = e(0.953×ln(TG)+0.139×BMI+0.718×ln(GGT)+0.053×waist circumference−15.745)/(1 + e(0.953×ln(TG)+0.139×BMI+0.718×ln(GGT)+0.053×waist circumference−15.745))×10040.
FIB-4=(Age×AST))/(blood platelet count×√ALT)41.
Hepatic steatosis and liver fibrosis
VCTE was performed using FibroScan (Echosens, Paris, France) by trained technicians following standardized protocols. LSM and CAP were obtained simultaneously during each examination. Hepatic steatosis was defined as CAP ≥ 248 dB/m based on previous validation studies42. This cutoff value has shown good diagnostic accuracy for detecting moderate-to-severe hepatic steatosis, with an area under the ROC curve of 0.8243. Significant liver fibrosis was defined as LSM ≥ 8.2 kPa4445;. This threshold has been validated in multiple studies and demonstrates high sensitivity and specificity for detecting advanced fibrosis46.
Mediator
Insulin resistance and liver function were evaluated as potential mediators. Insulin resistance was assessed using the homeostasis model assessment of insulin resistance (HOMA-IR), calculated as: [fasting glucose (mmol/L) × fasting insulin (µU/mL)]/22.5. Liver function was evaluated using serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), and gamma-glutamyl transferase (GGT).
Covariates
Sociodemographic characteristics included age, sex, race/ethnicity (Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black, Other), education level (< high school, high school graduate, > high school), marital status, and family income-to-poverty ratio. Lifestyle factors included smoking status (never, former, current), alcohol consumption (none, mild-to-moderate), and physical activity level (none, moderate, vigorous). Clinical measurements included body mass index (BMI), waist circumference, height, blood pressure, and laboratory parameters: fasting blood glucose, insulin, HbA1c, liver enzymes (ALT, AST, GGT), kidney function markers (creatinine, uric acid, blood urea nitrogen), lipid profile (triglycerides, total cholesterol, HDL cholesterol), and high-sensitivity C-reactive protein. Medical history information was collected on cardiovascular disease, chronic kidney disease, and cancer.
Statistical analyses
Baseline characteristics were presented as median (interquartile range) for continuous variables and number (percentage) for categorical variables. The Shapiro-Wilk test was used to assess normality of continuous variables. Between-group differences were compared using the Mann-Whitney U test for continuous variables and chi-square test or Fisher’s exact test for categorical variables as appropriate.
The associations between cardiometabolic markers and hepatic steatosis/fibrosis were examined using multivariable logistic regression models. Three models were constructed with progressive adjustment for potential confounders: Model 1 adjusted for age, gender, race, and education; Model 2 additionally adjusted for smoke, alcohol, and activity; Model 3 further adjusted for hypertension, ASCVD, CKD, and Cancer. Results were expressed as odds ratios (ORs) with 95% confidence intervals (CIs). Restricted cubic spline analyses with 3 knots were performed to evaluate potential non-linear relationships between cardiometabolic markers and hepatic steatosis and estimated fibrosis. The likelihood ratio test was used to assess non-linearity by comparing models with linear and spline terms.
Mediation analyses using the bootstrap method with 1000 resamples were performed to assess whether insulin resistance (HOMA-IR) and liver enzymes (ALT, AST, GGT) mediated the associations between cardiometabolic markers and hepatic steatosis. The proportion of mediation was calculated as the ratio of indirect effect to total effect.
Stratified analyses were conducted according to prespecified subgroups including age, sex, race, education, marital status smoke, alcohol, and activity. Several sensitivity analyses were conducted: (1) imputation of missing values; (2) exclusion of ASCVD; (3) using unweighted logistic regression; and (4) using covariate balancing propensity score (CBPS) method to balance covariates47.
All statistical analyses were performed using R version 4.3.3 (R Foundation for Statistical Computing, Vienna, Austria). Two-sided P-values < 0.05 were considered statistically significant.
Data availability
The data were publicly available from NHANSE (https://www.cdc.gov/nchs/nhanes/).
References
Pan, J. et al. Prevalence of Nafld, Mafld, and Masld: Nhanes 1999–2018. Diabetes Metab. 50 https://doi.org/10.1016/j.diabet.2024.101562 (2024).
Parola, M. & Pinzani, M. Liver fibrosis in Nafld/Nash: from pathophysiology towards diagnostic and therapeutic strategies. Mol. Aspects Med. 95 https://doi.org/10.1016/j.mam.2023.101231 (2024).
Ktenopoulos, N. et al. Non-Alcoholic fatty liver disease and coronary artery disease: A bidirectional association based on endothelial dysfunction. Int. J. Mol. Sci. https://doi.org/10.3390/ijms251910595 (2024).
Targher, G., Byrne, C. D., Tilg, H. & Masld A systemic metabolic disorder with cardiovascular and malignant complications. Gut 73, 691–702. https://doi.org/10.1136/gutjnl-2023-330595 (2024).
Stefan, N., Yki-Jarvinen, H. & Neuschwander-Tetri, B. A. Metabolic Dysfunction-Associated steatotic liver disease: heterogeneous pathomechanisms and effectiveness of Metabolism-Based treatment. Lancet Diabetes Endocrinol. 13, 134–148. https://doi.org/10.1016/S2213-8587(24)00318-8 (2025).
Stefan, N. & Targher, G. Clusters of metabolic Dysfunction-Associated steatotic liver disease for precision medicine. Nat. Rev. Gastroenterol. Hepatol. https://doi.org/10.1038/s41575-025-01048-w (2025).
Zhang, W. et al. Metabolic Dysfunction-Associated steatotic liver disease-Related hepatic fibrosis increases risk of insulin resistance, type 2 diabetes, and chronic kidney disease. Eur. J. Gastroenterol. Hepatol. 36, 802–810. https://doi.org/10.1097/MEG.0000000000002767 (2024).
Fabris, L., Campello, E., Cadamuro, M. & Simioni, P. The evil relationship between liver fibrosis and cardiovascular disease in metabolic Dysfunction-Associated fatty liver disease (Mafld): looking for the culprit. Biochim. Biophys. Acta Mol. Basis Dis. 1870, 166763 https://doi.org/10.1016/j.bbadis.2023.166763). (2024).
Wakabayashi, I. & Daimon, T. The cardiometabolic index as a new marker determined by adiposity and blood lipids for discrimination of diabetes mellitus. Clin. Chim. Acta. 438, 274–278. https://doi.org/10.1016/j.cca.2014.08.042 (2015).
Dobiasova, M. Atherogenic index of plasma [Log(Triglycerides/Hdl-Cholesterol)]: theoretical and practical implications. Clin. Chem. 50, 1113–1115. https://doi.org/10.1373/clinchem.2004.033175 (2004).
Irace, C. et al. Markers of insulin resistance and carotid atherosclerosis. A comparison of the homeostasis model assessment and triglyceride glucose index. Int. J. Clin. Pract. 67, 665–672. https://doi.org/10.1111/ijcp.12124 (2013).
Yao, J. et al. Association between estimated glucose disposal rate control level and stroke incidence in Middle-Aged and elderly adults. J. Diabetes. 16, e13595. https://doi.org/10.1111/1753-0407.13595 (2024).
Forouzesh, P., Kheirouri, S. & Alizadeh, M. Predicting hepatic steatosis degree in metabolic Dysfunction-Associated steatotic liver disease using obesity and Lipid-Related indices. Sci. Rep. 15, 8612. https://doi.org/10.1038/s41598-024-73132-1 (2025).
Sharma, A. et al. Obesity increases the risk of hepatic fibrosis in young adults with type 2 diabetes mellitus: the need to screen. Obes. (Silver Spring). 32, 1967–1974. https://doi.org/10.1002/oby.24130 (2024).
Suwala, S. & Junik, R. Assessment of the Liver Steatosis and Fibrosis Risk in Metabolic Syndrome and its Individual Components, Considering the Varying Definitions Used in Clinical Practice Throughout Time: A Retrospective Cross-Sectional Study. Biomedicines. (2024). https://doi.org/10.3390/biomedicines12081739(
Yan, L., Hu, X., Wu, S., Cui, C. & Zhao, S. Association between the cardiometabolic index and Nafld and fibrosis. Sci. Rep. 14, https://doi.org/10.1038/s41598-024-64034-3(2024).
Xu, M. et al. Non-Linear associations between cardiovascular metabolic indices and metabolic-Associated fatty liver disease: A Cross-Sectional study in the Us population (2017–2020). Open. Life Sci. 19 https://doi.org/10.1515/biol-2022-0947 (2024).
Li, K., Li, J., Cheng, X., Wang, J. & Li, J. Association between the atherogenic index of plasma and New-Onset Non-Alcoholic fatty liver disease in Non-Obese participants. Front. Endocrinol. (Lausanne). 13 https://doi.org/10.3389/fendo.2022.969783 (2022).
Chen, Y., Lu, C., Ju, H., Zhou, Q. & Zhao, X. Elevated Aip is associated with the prevalence of Mafld in the Us adults: evidence from Nhanes 2017–2018. Front. Endocrinol. (Lausanne). 15 https://doi.org/10.3389/fendo.2024.1405828 (2024).
Wang, J. et al. The diagnostic and prognostic value of the Triglyceride-Glucose index in metabolic Dysfunction-Associated fatty liver disease (Mafld): A systematic review and Meta-Analysis. Nutrients 14 https://doi.org/10.3390/nu14234969 (2022).
Song, J., Ma, R. & Yin, L. Associations between estimated glucose disposal rate and arterial stiffness and mortality among Us adults with Non-Alcoholic fatty liver disease. Front. Endocrinol. (Lausanne). 15 https://doi.org/10.3389/fendo.2024.1398265 (2024).
Zeng, P., Cai, X., Yu, X. & Gong, L. Markers of insulin resistance associated with Non-Alcoholic fatty liver disease in Non-Diabetic population. Sci. Rep. 13, https://doi.org/10.1038/s41598-023-47269-4(2023).
Karaaslan, H. et al. Comparison of Triglyceride-Glucose index and anthropometric obesity indices in predicting severe grades of hepatic steatosis in nonalcoholic fatty liver disease among Non-Diabetic obese individuals. Hepatol. Forum. 5, 113–119. https://doi.org/10.14744/hf.2023.2023.0049 (2024).
Jung, I., Koo, D. J. & Lee, W. Y. Insulin resistance, Non-Alcoholic fatty liver disease and type 2 diabetes mellitus: clinical and experimental perspective. Diabetes Metab. J. 48, 327–339. https://doi.org/10.4093/dmj.2023.0350 (2024).
Cankurtaran, M. et al. Insulin resistance and metabolic syndrome in patients with Nafld but without diabetes: effect of a 6 month regime intervention. Acta Gastroenterol. Belg. 70, 253–259 (2007).
Fan, Y. et al. Beta-Cell function or insulin resistance was associated with the risk of type 2 diabetes among women with or without obesity and a history of gestational diabetes. BMJ Open. Diabetes Res. Care. https://doi.org/10.1136/bmjdrc-2019-001060 (2020).
Zhou, S. L. et al. The relationship between Endoplasmic reticulum stress and liver function, insulin resistance and vascular endothelial function in patients with Non-Alcoholic fatty liver disease. Eur. Rev. Med. Pharmacol. Sci. 24, 11707–11715 https://doi.org/10.26355/eurrev_202011_23816(2020).
Mohamad, J., Amedeo, L. & Perspective Article Determinants and assessment of cardiovascular risk in steatotic liver disease owing to metabolic Dysfunction-Addressing the challenge. Metabolism Target. Organ. Damage. 4 https://doi.org/10.20517/mtod.2024.34 (2024).
Zhao, Y. et al. Mitochondrial dysfunction in metabolic dysfunction fatty liver disease (Mafld). Int. J. Mol. Sci. https://doi.org/10.3390/ijms242417514 (2023).
Abdelhameed, F. et al. Non-Invasive scores and serum biomarkers for fatty liver in the era of metabolic Dysfunction-Associated steatotic liver disease (Masld): A comprehensive review from Nafld to Mafld and Masld. Curr. Obes. Rep. 13, 510–531. https://doi.org/10.1007/s13679-024-00574-z (2024).
Savage, T. M. et al. Amphiregulin from regulatory T cells promotes liver fibrosis and insulin resistance in Non-Alcoholic steatohepatitis. Immunity 57, 303–318 https://doi.org/10.1016/j.immuni.2024.01.009(2024).
Tauil, R. B. et al. Metabolic-Associated fatty liver disease: the influence of oxidative stress, inflammation, mitochondrial dysfunctions, and the role of polyphenols. Pharmaceuticals (Basel). https://doi.org/10.3390/ph17101354 (2024).
Bellanti, F., Mangieri, D. & Vendemiale, G. Redox biology and liver fibrosis. Int. J. Mol. Sci. https://doi.org/10.3390/ijms25010410 (2023).
Arefhosseini, S., Aghajani, T., Tutunchi, H. & Ebrahimi-Mameghani, M. Association of systemic inflammatory indices with anthropometric measures, metabolic factors, and liver function in Non-Alcoholic fatty liver disease. Sci. Rep. 14, https://doi.org/10.1038/s41598-024-63381-5(2024).
Chen, T., Qin, X., Jiang, J. & He, B. Diagnostic indicators and lifestyle interventions of Metabolic-Associated fatty liver disease. Front. Nutr. 11, 1424246. https://doi.org/10.3389/fnut.2024.1424246 (2024).
Stefan, N., Schick, F., Birkenfeld, A. L., Haring, H. U. & White, M. F. The role of hepatokines in Nafld. Cell. Metab. 35, 236–252 https://doi.org/10.1016/j.cmet.2023.01.006(2023).
Wei, S., Wang, L., Evans, P. C. & Xu, S. Nafld and Nash: etiology, targets and emerging therapies. Drug Discov Today. 29 https://doi.org/10.1016/j.drudis.2024.103910 (2024).
2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes Care. 44, (2021). https://doi.org/10.2337/dc21-S002
Brittain, E. L. et al. Physical activity and incident obesity across the spectrum of genetic risk for obesity. JAMA Netw. Open. 7, e243821. https://doi.org/10.1001/jamanetworkopen.2024.3821 (2024).
Bedogni, G. et al. The fatty liver index: A simple and accurate predictor of hepatic steatosis in the general population. Bmc Gastroenterol. 6 https://doi.org/10.1186/1471-230X-6-33 (2006).
Sterling, R. K. et al. Development of a simple noninvasive index to predict significant fibrosis in patients with Hiv/Hcv coinfection. Hepatology 43, 1317–1325. https://doi.org/10.1002/hep.21178 (2006).
Karlas, T. et al. Individual patient data Meta-Analysis of controlled Attenuation parameter (Cap) technology for assessing steatosis. J. Hepatol. 66, 1022–1030. https://doi.org/10.1016/j.jhep.2016.12.022 (2017).
Mikolasevic, I. et al. Accuracy of controlled Attenuation parameter and liver stiffness measurement in patients with Non-Alcoholic fatty liver disease. Ultrasound Med. Biol. 47, 428–437. https://doi.org/10.1016/j.ultrasmedbio.2020.11.015 (2021).
Engin, A. Nonalcoholic fatty liver disease and staging of hepatic fibrosis. Adv. Exp. Med. Biol. 1460, 539–574. https://doi.org/10.1007/978-3-031-63657-8_18( (2024).
Testino, G. Liver Steatosis Assessment. Minerva Gastroenterol (Torino). 69, (2023). https://doi.org/10.23736/S2724-5985.23.03506-4
Zhong, H. et al. Non-Alcoholic fatty liver disease: pathogenesis and models. Am. J. Transl Res. 16, 387–399. https://doi.org/10.62347/KMSA5983 (2024).
Christian, F., Chad, H. & Kosuke, I. Covariate balancing propensity score for a continuous treatment: application to the efficacy of political advertisements. Annals Appl. Stat. 12, 156–177. https://doi.org/10.1214/17-AOAS1101 (2018).
Acknowledgements
We expressed gratitude to NHANES for data collection and quality control.
Funding
This research was supported by the National Natural Science Foundation of China (No. 82371597), the Natural Science Foundation of Hubei Province (No.2023AFB609) and Health Commission of Hubei Province Project (No.WJ2023M150).
Author information
Authors and Affiliations
Contributions
ZF contributed to Conceptualization, Data curation, Formal analysis, Funding acquisition and Writing–original draft. CY and XZ contributed to Formal analysis, Investigation, and Writing–original draft. JZ contributed to Conceptualization, Project administration, Supervision, and Writing–review & editing. All authors had full access to all the data in the study and the final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All survey protocols were approved by the institutional review board of the National Center for Health Statistics. All participants provided written informed consent before participation.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fan, Z., Yang, C., Zhao, X. et al. Association of cardiometabolic markers with hepatic steatosis and liver fibrosis in population without obesity and diabetes. Sci Rep 15, 15695 (2025). https://doi.org/10.1038/s41598-025-01003-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01003-4
Keywords
This article is cited by
-
The association between cardiometabolic index (CMI) and metabolic dysfunction-associated steatotic liver disease (MASLD): a systematic review and meta-analysis
Diabetology & Metabolic Syndrome (2025)