Abstract
Cardiovascular disease (CVD) is a global health concern; however, its association with the posterior occlusal contact remains unexplored. This study investigated the association between posterior occlusal contact and CVD risk in a large Japanese cohort and examined whether the loss of posterior occlusal contact in individuals with at least 20 teeth was a distinct CVD risk factor. Using Japanese health insurance claims data from 1,209,997 adults aged ≥ 40 years without prior CVD history (April 2016–March 2022), participants were categorized using the Eichner classification to assess posterior occlusal contact. Over an average follow-up period of 36.2 months, 51,471 participants developed CVD. Compared with individuals with full occlusal contact (Eichner A), those with reduced contact (Eichner B and C) demonstrated significantly higher CVD risks, with hazard ratios of 1.25 (95% confidence interval [CI]: 1.19–1.32) and 1.31 (95% CI: 1.17–1.46), respectively. In a subgroup analysis of participants with ≥ 20 teeth, reduced occlusal contact from Eichner A2 to B2 was associated with an increased risk of CVD, especially in those aged 40–59 years. These findings suggest that reduced posterior occlusal contact may contribute to increased CVD risk, emphasizing the importance of preserving natural occlusal support for CVD prevention.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) includes a variety of conditions such as heart attack, chronic coronary artery disease, stroke, and peripheral artery disease. It is the leading cause of premature death worldwide and remains a major public health issue, with 90% of cases being preventable through the proper management of risk factors1. The well-established risk factors for CVD include high blood pressure, high cholesterol levels, diabetes, obesity, smoking, and physical inactivity2. Preventive strategies typically focus on these risk factors, promoting healthier behaviors such as improved diet, regular exercise, and smoking cessation, which can address multiple risks simultaneously3. However, despite advances in its prevention and treatment, a notable level of residual risk remains, indicating that people can still develop CVD despite controlling for these traditional factors4.
Recent studies have indicated a possible association between oral health and cardiovascular outcomes, particularly the impact of tooth loss on the risk of CVD5,6. Evidence has shown that individuals who lose more teeth than the median for their age group have a 28% higher risk of heart disease and a 12% higher risk of stroke compared to those with fewer tooth losses7. Tooth loss has also been linked to a higher risk of death from CVD and adverse cardiovascular events8, with some studies suggesting its association with coronary heart disease and a slight association with heart attacks9,10. Moreover, retaining more teeth has been associated with a 27% increase in survival owing to CVDs11. These findings suggest that poor oral health, especially tooth loss, is related to an increased risk of CVD; however, the mechanisms underlying this association require further investigation.
Assessing oral function based solely on the number of teeth does not fully capture the complexity of how food is chewed and its role in overall health12. Posterior occlusal contact is crucial for efficient chewing and for maintaining good dental health13,14,15. Studies have suggested that reduced chewing ability, indicated by a weaker bite force and fewer functional masticatory units (FMUs), is linked to a higher risk of CVD16,17,18. In contrast, individuals with at least five functional tooth units (FTUs) demonstrated better cardiovascular health, potentially due to healthier eating habits compared to those with fewer than five FTUs19.
Most studies have focused on measures such as bite force, FMUs, and FTUs, which account for both natural and prosthetic teeth. To the best of our knowledge, no study has specifically examined the long-term association between posterior occlusal contact loss, using only natural teeth, and the risk of CVD. To study this association, we applied the Eichner classification to assess the posterior occlusal contact exclusively in natural teeth to determine whether occlusal loss independently predicts CVD risk. By focusing on individuals with at least 20 remaining teeth, we investigated whether the specific loss of posterior occlusal contact is a distinct risk factor for CVD through a detailed analysis of the Eichner subcategories A1–B2.
Methods
Data source and study design
This retrospective observational study was conducted using the Japan Medical Data Center (JMDC) Claims Database, a comprehensive insurer-based resource in Japan that includes the medical and dental records of > 60 health insurers nationwide. The JMDC Claims Database provides detailed information on the diagnoses, procedures, medications, and annual health checkups of individuals enrolled in Japanese insurance plans, including those under the age of 75. The database primarily represents Japan’s working-age population and their dependents, covering approximately 7.6% of the total population. It does not include individuals over the age of 75 or those without insurance coverage. To maintain data security, the database includes encrypted personal identifiers along with demographic information such as age and sex. We investigated the association between posterior occlusal contacts and CVD risk using data collected between April 2016 and March 2022.
Study population
The participant selection process is illustrated in Fig. 1. Initially, 6,741,176 individuals with available health check-up data were identified as potential participants. Individuals < 40 years of age (N = 2,399,923) were excluded due to the low prevalence of CVD and the small number of missing teeth. Participants who did not have dental codes recorded for all 28 teeth within the year before obtaining the health checkup data were also excluded (N = 3,064,814). Missing values in the health check-up data were addressed using multiple imputation analyses performed with the “mice” package in R (R Foundation for Statistical Computing, Vienna, Austria), generating 10 imputed datasets. Additionally, individuals who had been diagnosed with CVD within the 12 months preceding the index diagnosis were excluded from the study (N = 66,442). After applying these criteria, the final study population consisted of 1,209,997 participants, each free from CVD at baseline and with complete dental and health check-ups. The cohort study design is shown in Fig. 2.
Flow diagram of participant selection. This flowchart illustrates the stepwise selection process for the study participants from the Japan Medical Data Center Claims Database. The initial dataset comprised of 6,741,176 individuals with health checkup data. The exclusion criteria were as follows: individuals < 40 years of age (N = 2,399,923), those without dental codes for all 28 teeth within 1 year prior to the health check-up (N = 3,064,814), and those with a diagnosis of CVD within 12 months prior to the index date (N = 66,442).
CVD definition and assessment
The CVDs selected for this study, myocardial infarction, angina pectoris, stroke, heart failure, atrial fibrillation, and pulmonary embolism, were chosen based on the Framingham Heart Study, which is a widely recognized cohort study. The primary outcome was the new onset of CVD, defined as a composite endpoint that included myocardial infarction (ICD-10 codes: I210–I214 and I219), angina pectoris (ICD-10 codes: I200, I201, I208, and I209), stroke (ICD-10 codes: I600–I616, I619, I629, I630–I639, and G459), heart failure (ICD-10 codes: I500, I501, I509, and I110), atrial fibrillation (ICD-10 codes: I480–I484 and I489), and pulmonary embolism (ICD-10 codes: I260 and I269). CVD diagnoses were defined using the following criteria: (i) candidates were identified as those with recorded diagnoses of myocardial infarction, angina pectoris, stroke, heart failure, atrial fibrillation, or pulmonary embolism in their medical claims data during the follow-up period (April 2016–March 2022) and (ii) those with suspected flagging of these diagnoses were excluded. Follow-up ended on the date of diagnosis, date of death, or end of the study period.
Occlusal status classification
Posterior occlusal status, classified using the Eichner classification, was the primary explanatory variable. Although the JMDC Claims Database does not provide the number of teeth present, it records dental visits for disease management (e.g., periodontal examinations and mechanical tooth cleaning). Dental codes for all teeth were included, and if multiple codes were available, the most recent one was used. As reported previously, the number of teeth present was determined using these codes20,21. Additionally, the number of supporting zones, defined as pairs of opposing teeth in occlusal contact (including premolars and molars on both the right and left sides), was recorded and categorized into 0–4 support zones. As shown in Fig. 3, the Eichner classification system evaluates the dental occlusal support by assessing the presence and distribution of support zones22. Class A includes individuals with all support zones intact: A1 indicates complete contact across all support zones, A2 indicates missing teeth in either the upper or lower arch, and A3 indicates missing teeth in both arches but presence of all posterior support zones. Class B includes individuals with partial support zones: B1 indicates presence of three support zones, B2 indicates presence of two support zones, B3 indicates presence of only one support zone, and B4 indicates the absence of molar support zones, with occlusal contacts limited to the anterior region. Class C includes individuals with the absence of functional support zones: C1 indicates teeth in both arches but absence of occlusal contact, C2 indicates teeth only in one arch, and C3 indicates fully edentulous, lacking teeth in both arches.
Categorization of dental occlusal support according to the Eichner classification, based on the presence and location of remaining teeth. Class A includes individuals with full support zones: A1 indicates complete contact across all areas, A2 indicates missing teeth in either the upper or lower arch, and A3 indicates missing teeth in both arches while maintaining posterior support. Class B includes individuals with partial occlusal support zones; B1 indicates three support zones, B2 indicates two support zones, B3 indicates only one support zone, and B4 indicates absence of opposing molar support and occlusal contacts limited to the front teeth. Class C includes individuals with the absence of functional occlusal support: C1 indicates teeth in both arches but without occlusal contact, C2 indicates teeth in only one arch, and C3 indicates complete edentulism, with no teeth in either arch.
Other variables
Several risk factors of CVD have been identified3. In our study, we adjusted for demographic factors, health behaviors, and comorbidities that were likely to be associated with CVD and were accessible through the claims data. The demographic variables included insurance status (independent or dependent), age, and sex (male or female). Age was calculated by subtracting the date of birth from the date of medical checkup. The participants were categorized into two age groups: 40–59 and 60–75 years. Health behaviors included obesity, smoking, alcohol consumption, and physical activity. Self-reported smoking habits, alcohol consumption, and physical activities were recorded. Obesity was defined as a body mass index (BMI) of ≥ 25 kg/m². Current smokers were identified as individuals who had smoked more than five packs (100 cigarettes) in their lifetime and smoked daily or occasionally within the last 28 days. Alcohol use was categorized based on consumption frequency, and current drinkers were defined as those who consumed alcohol daily or occasionally. Physical activity was assessed using a standardized questionnaire, with ideal physical activity defined as engaging in at least 30 min of exercise twice weekly or walking for at least 1 h daily. The number of teeth, excluding the third molars, was classified into two groups, < 20 and ≥ 20 teeth, based on previous studies indicating that at least 20 teeth were sufficient to ensure adequate masticatory function23. Comorbidities evaluated included hypertension, diabetes, and dyslipidemia. Hypertension was defined as a systolic blood pressure (SBP) ≥ 140 mmHg, diastolic blood pressure (DBP) ≥ 90 mmHg, or the use of blood pressure-lowering medications. Diabetes was defined as a fasting glucose level ≥ 126 mg/dL or the use of glucose-lowering medications. Dyslipidemia was defined as a low-density lipoprotein (LDL) cholesterol level ≥ 140 mg/dL, high-density lipoprotein (HDL) cholesterol level < 40 mg/dL, triglyceride level ≥ 150 mg/dL, or the use of lipid-lowering medications.
Statistics
All the analyses were performed using R Studio, version 4.0.4. Statistical significance was set at p < 0.05.
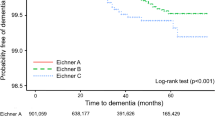
Descriptive statistics were used to summarize the demographic and clinical characteristics of study participants. Continuous variables are reported as means with standard deviations, and categorical variables as frequencies and percentages. Baseline characteristics among the three Eichner classifications and between the non-CVD and CVD groups were compared using the chi-squared test for categorical variables. Since the Anderson–Darling test indicated that all continuous variables (age, number of teeth, BMI, SBP, DBP, fasting glucose level, LDL, HDL, and triglycerides) did not follow a normal distribution (p < 0.001), analysis of variance and the Mann–Whitney U test were used to compare the groups with continuous variables. Kaplan–Meier curves were generated to compare the incidence rates of CVD across the Eichner classifications during the study period, and the log-rank test was used to evaluate the differences between groups. Log-log plots were used to verify the assumptions of the Cox proportional hazards model.
The primary analysis used a multivariable Cox proportional hazards model to evaluate the association between the Eichner classifications and CVD risk. The hazard ratio (HR) and corresponding 95% confidence interval (CI) were calculated for both an unadjusted model and a model adjusted for covariates such as age group, teeth group, sex, insurance status, smoking, alcohol use, obesity, hypertension, diabetes, dyslipidemia, and physical activity. We conducted three sensitivity analyses to assess the robustness of the findings. First, analyses were conducted using only complete cases, without applying multiple imputation, to address missing health check-up data (BMI, SBP, DBP, fasting glucose levels, LDL, HDL, triglycerides, use of blood pressure-lowering medications, use of glucose-lowering medications, use of lipid-lowering medications, smoking, alcohol consumption, and physical activity), resulting in a total of 883,584 subjects included in the analysis. Second, continuous values for the number of teeth, BMI, SBP, fasting glucose level, and LDL cholesterol were used instead of tooth group, obesity, hypertension, diabetes, and dyslipidemia in the multivariable model. Third, we applied induction periods of 6 and 12 months, meaning that participants who developed CVD within these time frames after the baseline were excluded from the analysis. After applying these criteria, the final study populations consisted of 1,110,228 and 994,801 subjects, respectively.
The subgroup analysis focused on individuals with ≥ 20 teeth and examined the relationship between the Eichner subcategories (A1–B2) and newly diagnosed CVD cases. This emphasis on subcategories A1 and B2 was based on an analysis that compared the Eichner subcategories (A1–C2) and their average number of teeth, revealing that categories B3 and below had significantly < 20 teeth (Table S1). The HRs and 95% CIs were calculated for a model adjusted for age, sex, insurance status, smoking, alcohol use, obesity, hypertension, diabetes, dyslipidemia, and physical activity. To further explore the impact of occlusal support within this subgroup, analyses stratified by sex (695,964 males and 514,033 females) and age (40–59 years, N = 1,106,776; 60–75 years, N = 103,221) were conducted. Additionally, the E-values were calculated to estimate the minimum strength of association that an unmeasured confounder would need with both the exposure and outcome, conditional on the measured covariates, to fully explain the observed association.
Ethics
This study used anonymized data sourced from the JMDC Claims Database, a commercially available resource, in compliance with Japan’s Act on the Protection of Personal Information. As the data were anonymized, informed consent was not required for their collection or use. Anonymization followed the standards outlined in the Next-Generation Medical Infrastructure Act. In line with Japan’s ethical guidelines for clinical research, studies that use anonymized information do not require approval from ethics review boards. This study adhered to the principles of the Declaration of Helsinki.
Result
Participant demographics
The analysis included 1,209,997 participants with a mean age of 49.0 ± 6.7 years (695,964 males and 514,033 females), resulting in a total observation period of 3,646,412 person-years. Over an average follow-up period of 36.2 months, 51,471 individuals (mean age: 51.4 ± 7.3 years; 33,221 males and 18,250 females) were newly diagnosed with CVD. Table 1 summarizes the baseline clinical characteristics according to the Eichner classification: Eichner A (N = 1,170,278), Eichner B (N = 31,591), and Eichner C (N = 8,128). The proportion of CVD cases was significantly higher in the Eichner B and C than in the Eichner A group (p < 0.001). Dependent, alcohol consumption, physical inactivity, and HDL levels were notably lower whereas the other variables were substantially higher in the Eichner B and C than in the Eichner A group.
Cumulative CVD risk according to the Eichner classification
Figure 4 displays the Kaplan–Meier curves for cumulative CVD risk stratified according to the Eichner classifications A, B, and C. Significant differences in CVD incidence were observed among the three groups, as confirmed by a statistically significant log-rank test (p < 0.001). Cox proportional hazards analyses were conducted to evaluate the impact of the Eichner classification on CVD development, adjusting for demographic factors, health behaviors, comorbidities, and the number of teeth. After controlling for these variables, the Eichner classification remained a major predictor of CVD risk (Table 2). Compared with the Eichner A group, the Eichner B group exhibited a 1.25-fold increased risk of CVD (HR: 1.25, 95% CI: 1.19–1.32, p < 0.001), and the Eichner C group showed a 1.31-fold increased risk of CVD (HR: 1.31, 95% CI: 1.17–1.46, p < 0.001).
Sensitivity analyses were performed to validate these findings. First, analyses were conducted using only complete cases without applying multiple imputation to handle missing health check-up data. These results are consistent with those of the primary analysis (Table S2). Second, continuous values were used instead of categorical variables for the number of teeth, obesity, hypertension, diabetes, and dyslipidemia in the multivariable model, yielding similar HRs (Table S3). Third, induction periods of 6 and 12 months were used to exclude individuals with latent CVD at baseline. The results remained stable, demonstrating the robustness of the observed associations over the different induction periods (Table S4). Fourth, the E-value analysis indicated that an unmeasured confounder would need a minimum strength of association of 1.81 (lower confidence limit: 1.67) for Eichner B and 1.95 (lower confidence limit: 1.62) for Eichner C with both the exposure and outcome (Table S5). Overall, these sensitivity analyses corroborated the initial findings, demonstrating the robustness of the results across various methodological adjustments and population subgroups.
Cumulative CVD risk according to the Eichner subclassifications in the ≥ 20 teeth group
Table 3 compares the Eichner subclassifications between the non-CVD (N = 1,140,302) and CVD group (N = 49,756) among the participants with ≥ 20 teeth. Figure 5 shows the results of the Cox proportional hazards analysis for CVD, stratified according to the Eichner subclassifications A1–B2, in the group with ≥ 20 teeth. Compared with Eichner A1, Eichner A2, A3, B1, and B2 were associated with a significant increase in CVD risk. The risk increased progressively with subclassifications from A2 (HR: 1.10, 95% CI: 1.06–1.15) to B2 (HR: 1.25, 95% CI: 1.14–1.38).
Subgroup analyses were performed to examine the association between the Eichner subcategories and CVD risk stratified by sex and age (Figures S1 and S2). For males, the Eichner classifications A2, B1, and B2 were associated with a significant increase in CVD risk compared with the Eichner classification A1, with HRs ranging 1.10–1.27. In females, significant associations were observed with Eichner A2, A3, B1, and B2, with HRs ranging 1.09–1.38. Among females, Eichner A3 demonstrated the strongest association (HR: 1.38, 95% CI: 1.07–1.78) compared with the other classifications. Age-stratified analyses revealed that individuals in the 40–59 year age group exhibited a higher CVD risk linked to Eichner subclassifications, with significant associations observed for Eichner classifications A2, A3, B1, and B2. Conversely, in the 60–75 age group, only Eichner B1 and B2 were significantly associated with increased CVD risk, with an HR of 1.12 (95% CI: 1.01–1.25) and 1.25 (95% CI: 1.10–1.42), respectively.
Discussion
In this large-scale retrospective observational study involving 1,209,997 participants, we investigated the relationship between posterior occlusal contact and risk of CVD. Our results indicated that participants with reduced posterior occlusal contact had a notably higher risk of developing CVD than those with full occlusal support. These associations remained robust across various sensitivity analyses, underscoring the potential clinical relevance of the posterior occlusal contact in assessing CVD risk. In the group with ≥ 20 teeth, subgroup analyses by sex provided additional insights; among males, the classifications A2, B1, and B2 were significantly associated with increased CVD risk. In contrast, the classifications A2–B2, and particularly A3, showed the strongest associations with females. These findings suggest that even moderate occlusal loss may increase the risk of CVD in females. Age-stratified analyses further indicated that the classifications A2–B2 were significantly associated with elevated CVD risk in individuals aged 40–59 years, indicating that early occlusal deterioration may have a more pronounced impact on CVD risk in middle-aged individuals. In contrast, only Eichner B1 and B2 were significantly associated with CVD risk in the 60–75 age group, suggesting that although reduced occlusal function remains a risk factor in older adults, its impact may be masked or outweighed by other age-related CVD risk factors. In particular, physiological changes associated with aging, such as vascular aging, atherosclerosis progression, and metabolic alterations, may reduce the influence of occlusal function on CVD risk. As the first study to use claims data to explore this association, our findings suggest that maintaining or restoring natural occlusal support in the premolar and molar regions may serve as modifiable targets for CVD prevention.
This study demonstrated a notable association between reduced posterior occlusal contact and CVD even after adjusting for the number of teeth. Previous studies have shown that reduced masticatory ability, including the loss of FMUs and reduced maximum bite force, particularly among females, is linked to an increased risk of CVD-related mortality16,24,25. The indicators of chewing function were also negatively correlated with vascular health26, highlighting a possible link between chewing ability and cardiovascular health. Most previous studies have included both natural and prosthetic teeth to assess occlusal function16,17,18,19. In contrast, our study uniquely focused on the role of posterior occlusal contact with only natural teeth using the Eichner classification. This approach highlights the specific contribution of natural occlusal support to cardiovascular health and suggests that maintaining natural posterior occlusion may play a crucial role in CVD prevention. Evaluating the posterior occlusal contact using solely natural teeth is important because natural and prosthetic teeth differ in their abilities to exert and transmit chewing forces. For instance, the biting forces in fixed partial, removable partial, and complete denture wearers were 80%, 35%, and 11%, respectively, of those with natural dentition27. Natural teeth accurately convey sensations and pressures and effectively distribute forces through the periodontal ligament, whereas prosthetic teeth may lack this feedback and force distribution abilities28. This difference may influence vascular health and metabolism owing to the physiological effects of occlusal function and mastication.
The association between reduced posterior occlusal contact and increased CVD risk may be mediated, in part, by dietary habits and their effects on cardiovascular health. Posterior occlusal support is essential for effective mastication and has a considerable impact on dietary choice and nutrient intake29. Participants in the Eichner B or C group who had reduced chewing function tended to avoid hard-to-chew foods in favor of softer, easier-to-chew options30,31. This dietary shift often results in a decrease in fiber and vitamin intake, and an increase in carbohydrate consumption32,33,34. The effects of this altered dietary pattern are well documented, with studies consistently showing that a reduced intake of fiber, fruits, and vegetables is associated with a higher risk of atherosclerosis and cardiometabolic diseases35,36,37. Conversely, diets rich in vegetables, antioxidant vitamins, and fiber are associated with a reduced CVD incidence38,39. Recent research has demonstrated a dose-response relationship between the number of occlusal support areas and individuals’ perceived ability to consume fruits and vegetables, reinforcing the notion that posterior occlusal contact influences dietary quality40. Our study demonstrated that moderate occlusal loss (A2, A3, B1, and B2) was associated with an increased risk of CVD, suggesting that partial posterior contact with some degree of mastication may be insufficient for maintaining an optimal diet. Beyond dietary implications, occlusal changes may affect psychosocial factors, such as psychological stress and depression, which contribute substantially to CVD risk41. For instance, reduced chewing ability can lead to dissatisfaction with one’s ability to chew, which, in turn, can affect social interactions and self-confidence42,43. Our analysis revealed a notable increase in CVD risk within the 40–59 age group, especially for those with Eichner classifications A2–B2. These findings suggest that, in midlife, when individuals are often actively engaged in both social and professional settings, oral health issues may have a heightened psychosocial impact. Psychological stress and anxiety are known risk factors for CVD41, while low social support in the workplace has been linked to higher CVD prevalence44. Furthermore, our results suggest sex-specific trends in the association between occlusal status and CVD risk, with females in the Eichner A3 group showing a particularly strong association with CVD even with preserved occlusal support areas. This difference may be due to heightened psychosocial stress responses to oral health challenges among females, which can disrupt social interactions, dietary habits, and stress management practices, potentially leading to an elevated CVD risk45. This pattern has been observed not only in Japan but also in other countries, such as the UK and the US, suggesting a broader, cross-cultural phenomenon46,47,48. Therefore, future studies should explore the impact of specific tooth loss patterns on cardiovascular outcomes to clarify how different occlusal changes affect dietary intake, psychosocial well-being, and physiological stress responses. Such investigations could yield valuable insights into targeted preventive strategies and interventions to address oral health and cardiovascular risks.
Each CVD event was analyzed separately, and individuals with reduced posterior occlusal support exhibited an elevated risk of several CVDs, including angina pectoris, stroke, heart failure, atrial fibrillation, and pulmonary embolism (Table S6). This result aligns with those of prior research suggesting that diminished bite force may be a considerable risk factor for coronary heart disease and stroke16. Notably, studies have indicated that patients with a history of myocardial infarction often exhibit poor oral health with fewer occlusal contacts in the intercuspal position, highlighting a potential link between compromised occlusal health and an increased risk of myocardial infarction49. However, our analysis did not identify a significant association between the absence of occlusal contact (Eichner B and C) and incidence of myocardial infarction specifically (Table S7). This unexpected outcome may be partly due to the limited number of myocardial infarction cases in the study cohort, potentially affecting the statistical power. Moreover, the association between reduced occlusal support and myocardial infarction was insignificant after adjusting for the number of teeth, suggesting that the number of remaining teeth plays a critical role in this relationship. Unlike that with other CVDs, where occlusal support independently influences risk, the risk of myocardial infarction appears to be more sensitive to the presence of retained teeth. This finding suggests that, while occlusal function affects overall cardiovascular health, maintaining a greater number of teeth may be particularly important for mitigating the risk of myocardial infarction.
There are a few limitations of this study that must be considered when interpreting the data. First, it is important to acknowledge that the diagnoses recorded in the insurance claims databases are typically not rigorously validated, which introduces uncertainty regarding its accuracy. Consequently, although this retrospective observational study suggests a potential association between the Eichner classification and incidence of CVD, the findings do not definitively establish this relationship. Further research using rigorously validated prospective cohort studies is required to confirm these findings. Second, because this database mainly includes Japan’s working-age population and its dependents, it does not include individuals aged > 75 years. This exclusion limits our ability to evaluate the association between risk factors and CVD in older adults. The database includes data from major enterprises across Japan; however, its geographical distribution may not fully capture the demographic or regional variations across the entire country. Additionally, the emphasis of the JMDC Claims Database on a relatively younger population has led to a low incidence of CVD events being documented. However, the rate of CVD events recorded in this database aligns with the findings of other epidemiological studies in Japan50,51. Third, claims data typically include only diagnoses associated with medical treatments, which may result in underreporting of CVD cases among individuals who do not seek medical attention. Conversely, participants with multiple risk factors such as obesity, hypertension, and diabetes were more likely to be diagnosed with CVD because they tended to utilize medical services more frequently. Increased use of healthcare services can potentially enhance the likelihood of detecting CVD. Fourth, although adjustments were made for conventional confounding factors available in the database, some residual confounding variables, such as income level, educational attainment, and occupational type, may still influence the relationship between reduced posterior occlusal contact and the subsequent development of CVD5. Socioeconomic status has been shown to affect access to healthcare, including dental services52. Since the JMDC database does not provide information on socioeconomic status, it is possible that the association between occlusal contact and CVD could have been exaggerated due to the failure to account for these factors. Although residual confounding from unmeasured factors like income and education cannot be ruled out, the E-value of 1.95 for Eichner C and CVD (Table S5) exceeds the reported effects of socioeconomic status on CVD (HR = 1.44) and tooth loss (odds ratio = 1.66)53,54, suggesting minimal impact. Fifth, this study did not consider the duration of posterior occlusal support loss, which is crucial for understanding its potential impact on CVD. Knowing the length of time that the participants experienced this condition would provide valuable insights. Additionally, the study did not account for the presence or severity of periodontitis, despite its known association with the inflammatory processes and immune responses involved in the development of CVD55. Future research should address these gaps by including a broader range of participants and conducting more detailed assessments.
Conclusion and implications
This study demonstrated a notable association between reduced natural posterior occlusal contact and increased CVD risk, highlighting the importance of considering oral health, particularly natural occlusal support, as a key factor in CVD risk assessment. Our findings suggest that early intervention, including the provision of tailored prosthetic solutions, such as fixed or removable dentures, based on the extent of posterior occlusion loss and patient demographics (age and sex), could serve as an effective public health strategy in reducing CVD risk. Together, the study findings underscore the importance of integrating dental health into broader preventive healthcare frameworks to potentially improve cardiovascular outcomes.
Data availability
Data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Flora, G. D. & Nayak, M. K. A brief review of cardiovascular diseases, associated risk factors and current treatment regimes. Curr. Pharm. Des. 25, 4063–4084 (2019).
Adhikary, D., Barman, S., Ranjan, R. & Stone, H. A systematic review of major cardiovascular risk factors: A growing global health concern. Cureus 14, e30119 (2022).
Atnett, D. et al. (ed, K.) 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: A report of the American college of cardiology/american heart association task force on clinical practice guidelines. Circulation 140 e596–e646 (2019).
Sucato, V., Comparato, F., Ortello, A., Galassi, A. R. & Novo, G. Residual cardiovascular risk: role of remnants cholesterol, monocyte/hdl ratio and lipoprotein ratios on personalized cardiovascular prevention. J. Pers. Med. 14, 460 (2024).
Hardan, L. et al. Association between dental and cardiovascular diseases: A systematic review. Rev. Cardiovasc. Med. 24, 159 (2023).
Botelho, J. et al. An umbrella review of the evidence linking oral health and systemic noncommunicable diseases. Nat. Commun. 13, 7614 (2022).
Abnet, C. C. et al. Tooth loss is associated with increased risk of total death and death from upper Gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort. Int. J. Epidemiol. 34, 467–474 (2005).
Vedin, O. et al. Tooth loss is independently associated with poor outcomes in stable coronary heart disease. Eur. J. Prev. Cardiol. 23, 839–846 (2016).
Vedin, O. et al. Associations between tooth loss and prognostic biomarkers and the risk for cardiovascular events in patients with stable coronary heart disease. Int. J. Cardiol. 245, 271–276 (2017).
Wilson, K. et al. Poor oral health and risk of incident myocardial infarction: A prospective cohort study of Swedish adults, 1973–2012. Sci. Rep. 8, 11479 (2018).
Janket, S. J. et al. Number of teeth, C-reactive protein, fibrinogen and cardiovascular mortality: a 15-year follow-up study in a Finnish cohort. J. Clin. Periodontol. 41, 131–140 (2014).
Naka, O., Anastassiadou, V. & Pissiotis, A. Association between functional tooth units and chewing ability in older adults: a systematic review. Gerodontology 31, 166–177 (2014).
Delwel, S. et al. Chewing efficiency, global cognitive functioning, and dentition: A Cross-sectional observational study in older people with mild cognitive impairment or mild to moderate dementia. Front. Aging Neurosci. 12, 225 (2020).
Kosaka, T. et al. Factors influencing the changes in masticatory performance: the suita study. JDR Clin. Trans. Res. 3, 405–412 (2018).
Ueno, M., Yanagisawa, T., Shinada, K., Ohara, S. & Kawaguchi, Y. Masticatory ability and functional tooth units in Japanese adults. J. Oral Rehabil. 35, 337–344 (2008).
Hashimoto, S. et al. A lower maximum bite force is a risk factor for developing cardiovascular disease: the suita study. Sci. Rep. 11, 7671 (2021).
Chatzopoulou, E. et al. Poor masticatory capacity and blood biomarkers of elevated cardiovascular disease risk in the community: the Paris prospective study III. Arterioscler. Thromb. Vasc Biol. 41, 2225–2232 (2021).
Chun, H., Oh, J. & Doo, M. The risk of cardiovascular disease according to chewing status could be modulated by healthy diet in Middle-Aged Koreans. Nutrients 14, 3849 (2022).
Rangé, H. et al. Chewing capacity and ideal cardiovascular health in adulthood: A cross-sectional analysis of a population-based cohort study. Clin. Nutr. 39, 1440–1446 (2020).
Tamada, Y. et al. Validity of claims-based definition of number of remaining teeth in Japan: results from the longevity improvement and fair evidence study. PLoS One. 19, e0299849 (2024).
Miyano, T. et al. Association between reduced posterior occlusal contact and Alzheimer’s disease onset in older Japanese adults: results from the LIFE study. J. Alzheimers Dis. 97, 871–881 (2024).
Eichner, K. Renewed examination of the group classification of partially edentulous arches by Eichner and application advices for studies on morbidity statistics]. Stomatol. DDR. 40, 321–325 (1990).
Somsak, K. & Kaewplung, O. The effects of the number of natural teeth and posterior occluding pairs on the oral health-related quality of life in elderly dental patients. Gerodontology 33, 52–60 (2016).
Ansai, T. et al. Association of chewing ability with cardiovascular disease mortality in the 80-year-old Japanese population. Eur. J. Cardiovasc. Prev. Rehabil. 15, 104–106 (2008).
Darnaud, C., Thomas, F., Danchin, N., Boutouyrie, P. & Bouchard, P. Masticatory capacity and mortality: the preventive and clinical investigation center (IPC) cohort study. J. Dent. Res. 99, 152–158 (2020).
Testa, S. et al. Low drug levels and thrombotic complications in high-risk atrial fibrillation patients treated with direct oral anticoagulants. J. Thromb. Haemost. 16, 842–848 (2018).
Miyaura, K., Morita, M., Matsuka, Y., Yamashita, A. & Watanabe, T. Rehabilitation of biting abilities in patients with different types of dental prostheses. J. Oral Rehabil. 27, 1073–1076 (2000).
Weinberg, L. A. The biomechanics of force distribution in implant-supported prostheses. Int. J. Oral Maxillofac. Implants. 8, 19–31 (1993).
Kosaka, T. et al. A multifactorial model of masticatory performance: the suita study. J. Oral Rehabil. 43, 340–347 (2016).
Ritchie, C. S., Joshipura, K., Hung, H. C. & Douglass, C. W. Nutrition as a mediator in the relation between oral and systemic disease: associations between specific measures of adult oral health and nutrition outcomes. Crit. Rev. Oral Biol. Med. 13, 291–300 (2002).
Wakai, K. et al. Tooth loss and intakes of nutrients and foods: a nationwide survey of Japanese dentists. Community Dent. Oral Epidemiol. 38, 43–49 (2010).
Inomata, C. et al. Significance of occlusal force for dietary fibre and vitamin intakes in independently living 70-year-old Japanese: from SONIC study. J. Dent. 42, 556–564 (2014).
Iwasaki, M. et al. Longitudinal association of dentition status with dietary intake in Japanese adults aged 75 to 80 years. J. Oral Rehabil. 43, 737–744 (2016).
Yoshida, M. et al. Correlation between dental and nutritional status in community-dwelling elderly Japanese. Geriatr. Gerontol. Int. 11, 315–319 (2011).
Marr, J. W. & Morris, J. N. Dietary intake and the risk of coronary heart disease in Japanese men living in Hawaii. Am. J. Clin. Nutr. 34, 1156–1157 (1981).
Joshipura, K. J. et al. Fruit and vegetable intake in relation to risk of ischemic stroke. JAMA 282, 1233–1239 (1999).
Tada, A. & Miura, H. Systematic review of the association of mastication with food and nutrient intake in the independent elderly. Arch. Gerontol. Geriatr. 59, 497–505 (2014).
Steffen, L. M. et al. Associations of whole-grain, refined-grain, and fruit and vegetable consumption with risks of all-cause mortality and incident coronary artery disease and ischemic stroke: the atherosclerosis risk in communities (ARIC) study. Am. J. Clin. Nutr. 78, 383–390 (2003).
Okuda, N. et al. Fruit and vegetable intake and mortality from cardiovascular disease in Japan: a 24-year follow-up of the NIPPON DATA80 study. Eur. J. Clin. Nutr. 69, 482–488 (2015).
Lin, Y. C. et al. Association between the dental occlusion and perceived ability to eat foods of Taiwanese older adults. J. Oral Rehabil. 48, 817–826 (2021).
Neylon, A. et al. A global perspective on psychosocial risk factors for cardiovascular disease. Prog Cardiovasc. Dis. 55, 574–581 (2013).
Locker, D. Changes in chewing ability with ageing: a 7-year study of older adults. J. Oral Rehabil. 29, 1021–1029 (2002).
Locker, D., Clarke, M. & Payne, B. Self-perceived oral health status, psychological well-being, and life satisfaction in an older adult population. J. Dent. Res. 79, 970–975 (2000).
Johnson, J. V. & Hall, E. M. Job strain, work place social support, and cardiovascular disease: a cross-sectional study of a random sample of the Swedish working population. Am. J. Public. Health. 78, 1336–1342 (1988).
Tanveer, S. A. et al. Association of Self-Perceived psychological stress with the periodontal health of socially deprived women in shelter homes. Int. J. Environ. Res. Public. Health. 18, 5160 (2021).
Sekiguchi, A. et al. Association between high psychological distress and poor oral health-related quality of life (OHQoL) in Japanese community-dwelling people: the Nagasaki Islands study. Environ. Health Prev. Med. 25, 82 (2020).
Alsoghier, A., Riordain, R. N., Fedele, S. & Porter, S. Psychosocial impacts of oral epithelial dysplasia. J. Oral Pathol. Med. 50, 700–707 (2021).
An, J. et al. Effects of depression and stress on oral self-care among perinatal women in appalachia: A longitudinal study. Community Dent. Oral Epidemiol. 52, 871–879 (2024).
Szerszeń, M., Górski, B. & Kowalski, J. Clinical condition of the oral cavity in the adult Polish population below 70 years of age after myocardial Infarction-A Case-Control study. Int. J. Environ. Res. Public. Health. 19, 7265 (2022).
Saito, I. et al. Association between mortality and incidence rates of coronary heart disease and stroke: the Japan public health Center-based prospective (JPHC) study. Int. J. Cardiol. 222, 281–286 (2016).
Miura, K. et al. Four blood pressure indexes and the risk of stroke and myocardial infarction in Japanese men and women: a meta-analysis of 16 cohort studies. Circulation 119, 1892–1898 (2009).
McMaughan, D. J., Oloruntoba, O. & Smith, M. L. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Front. Public. Health. 8, 231 (2020).
Wang, T., Li, Y. & Zheng, X. Association of socioeconomic status with cardiovascular disease and cardiovascular risk factors: a systematic review and meta-analysis. J. Public. Health. 32, 385–399 (2024).
Seerig, L. M. et al. Tooth loss in adults and income: systematic review and meta-analysis. J. Dent. 43, 1051–1059 (2015).
Lockhart, P. B. et al. Periodontal disease and atherosclerotic vascular disease: does the evidence support an independent association? A scientific statement from the American heart association. Circulation 125, 2520–2544 (2012).
Acknowledgements
We acknowledge the valuable contributions of other researchers, staff, and participants in the study using the JMDC database. We would like to thank Editage (www.editage.jp) for editing.
Funding
This study was funded by Grants-in-Aid for Scientific Research (22H03299, 23 K24557) from the Japan Society for the Promotion of Science (JSPS) KAKENHI and Health and Labor Sciences Research Grants (23 FA1022) from the Ministry of Health, Labor, and Welfare.
Author information
Authors and Affiliations
Contributions
All authors satisfy the authorship criteria outlined in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals. TM, YT, TK, KO, and KT contributed to the study’s concept and design. KT carried out data acquisition, while TM, YT, TK, KO, and KT were responsible for analyzing and interpreting the data. TM prepared the initial draft of the manuscript, with YT, TK, KO, and KT providing critical revisions to enhance the manuscript’s intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Miyano, T., Tamada, Y., Kusama, T. et al. Impact of posterior occlusal contact loss on cardiovascular disease using a Japanese claims database. Sci Rep 15, 16693 (2025). https://doi.org/10.1038/s41598-025-01846-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-01846-x