Abstract
Attention-deficit hyperactivity disorder (ADHD) is a neurodevelopmental condition marked by difficulties with attention, increased activity levels, and impulsive behaviour, which can impact social, academic, and work-related performance. Its presence in adults is often overlooked and inadequately addressed. Emerging research suggests a link between ADHD and unhealthy lifestyles, including sedentary behaviour, substance use, and effort discounting, a decision-making process where individuals undervalue rewards requiring significant physical or cognitive effort. This study investigates the association between ADHD symptoms, physical effort discounting, and indicators of unhealthy lifestyles in young adults. We recruited 181 participants aged 18–33 years. They completed the Effort-Expenditure for Rewards Task (EEfRT) and a hypothetical effort-discounting task, alongside questionnaires assessing ADHD and developmental co-ordination disorder (DCD) symptoms, physical activity, alcohol, tobacco and drug use. A logistic mixed model was used to analyze effort-discounting decisions, while regression analyses assessed the influence of ADHD symptoms and effort discounting on unhealthy lifestyle indicators. EEfRT decisions were significantly influenced by reward probability, monetary value, and ADHD medication status, whereas choices in the hypothetical effort-discounting task were influenced by money, effort and ADHD symptoms. When exploring the association between all variables, ADHD symptoms were positively correlated with effort discounting in the hypothetical task, smoking, and DCD. Effort discounting was associated with a sedentary lifestyle while smoking correlated with higher BMI and alcohol consumption. Linear and logistic regressions suggested that ADHD symptoms and effort discounting were associated with a sedentary lifestyle, and smoking status was significantly explained by ADHD symptoms. These findings highlight the need for targeted interventions addressing both ADHD symptomatology and lifestyle factors to improve outcomes in affected individuals.
Similar content being viewed by others
Introduction
Attention-deficit hyperactivity disorder (ADHD) is a neurodevelopmental condition characterised by a persistent pattern of attentional impairments, as well as hyperactivity and impulsivity that interferes with social, academic or labour functioning1. Systematic reviews and meta-analyses point to an ADHD world prevalence between 5 and 7% in children and adolescents2. Even though symptoms persist during adulthood, adult ADHD is possibly under-recognised, under-diagnosed, and poorly treated3, with an estimated prevalence of 2.6–6.8%4. Recent research also suggests that ADHD is associated with unhealthy lifestyles, such as sedentary behaviours or tobacco, alcohol and drug consumption5,6,7,8. Further, an impairment in integrating effort costs in decision making in ADHD has been suggested9.
Effort discounting refers to the subjective cost of physical or cognitive effort in decision making. Recent research has assessed the affectation of mental effort in ADHD10,11. Our study is focused on physical effort. This factor, together with risk and delay12, tends to decrease the value of an expected reward. Such a decrease is frequently modelled as a hyperbolic discounting function in hypothetical decision-making tasks13. In these hypothetical tasks, volunteers have to select among two alternatives involving a monetary reward in exchange for a physical exercise, such as running on a treadmill. Importantly, due to their hypothetical nature, rewards and efforts are not effectively obtained or expended. Other tasks employed in the evaluation of effort discounting, such as the Effort Expenditure for Rewards Task (EEfRT)14, involve an actual effort performance (fast pushing of a key). In the context of ADHD research, hypothetical physical effort-discounting tasks have been studied in adolescents15, where no differences were found between diagnosed and control volunteers. To our knowledge, this construct has not been studied in relation to ADHD symptoms in adults. On the other hand, the EEfRT has been recently used in two samples (cannabis users and non-users) of college students, where ADHD symptoms were measured as a covariate16. The authors found that cannabis users were more prone to exert high effort levels, but its association with ADHD symptoms was not assessed.
ADHD has also been linked to multiple facets of unhealthy lifestyle. A recent systematic review found increased odd ratios of cannabis (1.27–2.19, weighted mean 1.89, 8 studies) and tobacco (0.61–3.01, weighted mean 1.50, 11 studies) use, sedentary behaviour (1.08–8.9, weighted mean 1.88, 10 studies) and diet quality (1.25–3.89, weighted mean 1.79, 7 studies) in ADHD patients17. According to the meta-analysis by Cortese and collaborators18, the pooled prevalence of obesity in adults with ADHD is about 70%, compared with 16% of non-ADHD adults. They suggest that this association could be due to abnormal eating patterns, decreased physical activity, or time spent watching TV. There is also meta-analytic evidence for the association of ADHD and substance use and dependence19. The putative association between a mental disorder such as ADHD and several harmful lifestyles is relevant because all these studies point to a poorer quality of life for adults with ADHD. Eventually, these could be contributing factors to a known fact: ADHD is associated with increased mortality rates20,21,22. Therefore, research on the relationship between decision-making features and negative lifestyles could shed some light on this disorder and eventually improve current therapeutic approaches.
In the present report, we investigate the association between ADHD symptoms, effort discounting –assessed by two different decision-making tasks– and potential indicators of unhealthy lifestyles –such as sedentary behaviour, obesity, alcohol, tobacco and drug consumption– in a sample of 181 young adults. Our results point to an association between ADHD symptoms, effort discounting and smoking habits. Also, a greater impact of effort in decision-making was associated with a sedentary lifestyle and smoking habits.
Methods
Sample
As explained below, this manuscript reports the effort-related findings of a larger project that investigates time, risk and effort-discounting and its association with ADHD symptoms and lifestyles. Since our primary interest is ADHD symptomatology rather than diagnosis, we followed a transdiagnostic, dimensional, approach instead of splitting our sample by diagnosis. Therefore, all participants were included in one single group for all analyses. However, this section explains the sample composition by diagnosis group to provide a more detailed description.
A sample of 183 participants was recruited. Two of them lacked crucial information and were excluded. Thus, the final sample included 181 volunteers (96 male, 85 female; mean age 21.76, standard deviation, SD = 2.87, 18–33). Fifty-eight participants had a current clinical diagnosis of ADHD (25 male, 33 female; mean age 22.48, SD = 3.43, 18–32), demonstrated by the research project’s clinicians or a signed clinical report. One hundred twenty-three participants lacked a clinical diagnosis of ADHD (71 male, 52 female; mean age 21.38, SD = 2.47, 18–33). The medication status of ADHD-diagnosed participants was diverse: 30 of them were medicated under prescription (either methylphenidate, lisdexamfetamine dimesylate or atomoxetine), whereas 27 were non-medicated (1 missing value). Our research goal was to evaluate participants in two visits: in the case of medicated ADHD volunteers, we planned to assess them in their usual medication status during one of the visits, whereas we asked them to take the medication after evaluation in the other visit. By doing so, we expected to analyse the effect of medication on decision-making tasks. However, we could not pursue this goal due to dropouts and a limited number of medicated participants. Due to this initial plan, 7 participants included in this report were assessed without taking their habitual medication the day of the assessment. Thus, they were off medication between 12 and 24 h before the experiment. According to the pharmacokinetics of these drugs, the effect of methylphenidate lasts a maximum of 8–12 h in the extended-release preparations23. A recent report showed negligible levels in plasma after 6 h of consuming lisdexamfetamine24. As for atomoxetine, it has a plasma half-life of 5.2 hours25. For simplicity and statistical power, we coded medication status as 0 for controls, 1 for medicated ADHD participants, and 2 for non-medicated ADHD participants (including volunteers who usually did not take medication and the 7 participants who were requested to delay their administration until finishing the assessment).
Procedure
After an initial telephone screening, volunteers attended the laboratory individually or in small groups (2 to 6 persons per group) to receive detailed information about the project. The overall project involved two visits to engage in the same decision-making tasks and complete a set of psychometric questionnaires. Since a large number of participants missed the second visit, the results reported here pertain to the first assessment. After signing the informed consent form, volunteers completed the decision-making tasks explained below in a randomised order (about 45 min overall). Then, they were individually assessed with the MINI International Neuropsychiatric Interview (5.0, Spanish version), Global Physical Activity Questionnaire (GPAQ), Systematic Inventory of Alcohol Consumption (SIAC) and some general health questions (i.e., weight, height, dexterity, number of cigarettes per day, driving licence, habitual medication) (see below for a description of the assessment tools). Subsequently, they self-administered a set of questionnaires to assess ADHD symptomatology, self-regulation, impulsivity, risk-taking and self-harm behaviours, developmental co-ordination disorder (DCD), study habits, and a set of sociodemographic questions, including previous diagnoses of neurological or psychiatric conditions.
Participants received a fixed reward of 10 € per visit, which could be increased by randomly selecting one or two decisions of some of the decision-making tasks (average money won = 11.29 €, range 10–17.65 €).
Decision-making tasks
Participants completed six decision-making tasks to assess time-, risk- and physical effort-discounting. Three involved an immediate reward in exchange for the corresponding discounting factor, and the remaining were hypothetical (no actual rewards, delays, risks, or efforts were involved). In this paper, we report the results of the effort-discounting immediate and hypothetical tasks.
We used the Effort-Expenditure for Rewards Task (EEfRT)14 to assess immediate physical effort discounting. We programmed it in Cogent 2000, developed by the Cogent 2000 team at the FIL and the ICN and Cogent Graphics developed by John Romaya at the LON at the Wellcome Department of Imaging Neuroscience, which runs in Matlab (The MathWorks, Inc., Natick, MA, USA), following published descriptions of the EEfRT. In each trial, participants had to decide between a low-reward (1 €) low-effort (30 spacebar presses in 7 s with the index finger of the dominant hand) alternative and a higher reward (1.85, 1.88, 2.26, 2.53, 2.55, 3.03, 3.60, 3.66 or 4.15 €) in exchange of a harder effort (100 spacebar presses in 21 s with the little finger of the non-dominant hand). As in the original version of the task, irrespective of choice and effort completion, rewards were not guaranteed: for each trial, the initial screen showed both reward/effort alternatives and also the probability of obtaining the reward in case of successful completion of the demanded effort: 12%, 50% or 88%. Thus, participants had to trade-off between effort expenditure and probability. Trials were pseudo-randomised during task programming in ten blocks of 9 trials, each including every probability and money mentioned above (see Supplementary Table S1 for all trial blocks). Volunteers were instructed to choose the easy or hard alternative within 5 s; otherwise, the selection would be random. If participants were unsuccessful in completing the required effort on time, a screen was presented with the following text: “Time out! You have not completed the task. You have not won any money”. They were explicitly told the three probability levels but not the reward amounts; also, they were informed that they would be playing for 15 min and that the program would randomly choose two of their selections to the sum of which constituted their earnings. This random selection was automatically carried out by the Matlab code of the task.
The ‘hypothetical’ physical effort-discounting task followed the well-known design of this kind of paradigm12, as described elsewhere13. Participants faced 50 decision-making trials that involved an effortless alternative (paired with a reward lower than 20 €) and 20 € in exchange for a hypothetical effort (x minutes running on a treadmill, 5 < x < 75 min). Instead of using fixed effort levels for all participants, we used Ed Vul and collaborators’ Functional Adapting Sequential Tool (Fast v1.0) (www.evullab.org/pdf/s6.pdf). This algorithm starts from a set of fixed values and progressively finds the optimal indifference points to estimate the hyperbolic discounting curve of each participant through Bayesian inference. More precisely, the effortful alternative was randomly presented on the left or right, showing “20 €” on top and the proposed effort (automatically selected by the stepwise algorithm between 5 and 75 min) under it. The effortless alternative entailed “0 min” running, and the program automatically selected an amount of money lower than 20 €. Hence, the effortless alternative involved rewards close to 20 €, and the effortful alternative entailed lower effort levels for effort-averse participants. The opposite happened for effort-seeking volunteers. In any case, the algorithm found the indifference points (those decisions where the volunteer hesitated between the effortful and the effortless alternatives) and estimated the discounting constant (k) defining each participant’s hyperbolic decaying curve. The constant k ranges from 0 to 1, with lower values indicating lower effort discounting. In this task, decisions were not time-constrained, and the overall duration was about 5 min. Participants were informed about this approximate duration but not the exact number of trials. They were told that rewards and efforts were hypothetical in this task.
Additional measures
ADHD symptoms
We used the 18-item Adult ADHD Self-Report Scale (ASRS) version 1.126. This is a Likert-style (0 = never, 4 = very often) screening tool in which respondents are asked about their feelings and behaviour in the past six months. The first nine items constitute the inattention scale, whereas the following nine pertain to hyperactivity-impulsivity symptoms, following the DSM-5 criteria. We calculated the score for each subscale although in most analyses we only considered the overall score for simplicity.
GPAQ
The Global Physical Activity Questionnaire (GPAQ) is a tool developed by the World Health Organisation to assess physical activity during a normal week in three domains: at work, for leisure, and for travelling27. Volunteers were interviewed about the number of days and minutes per day that they do intense and/or moderate activities in each domain. The final score was the amount of metabolic equivalents (METs)-minutes per week. One MET was equivalent to a consumption of 1 kcal/kg/hour and corresponded to the energy cost of sitting quietly. Intense and moderate activities were assigned 8 and 4 METs per minute, respectively. Thus, the final score was the sum of all intense activities (in minutes) multiplied by 8 and all moderate activities (including travelling) multiplied by 4. Values below 600 did not meet WHO recommendations.
SIAC
The Systematic Inventory of Alcohol Consumption (SIAC)28 is a short interview to assess alcohol consumption. Participants were asked about the number of days and amount of alcoholic drinks they consume in a typical week. This was quantified as ‘standard units’ (SU) such as, for example, one glass of beer (200 cc) corresponded to 1 SU, one glass of a distilled drink (i.e., whiskey, 50 cc) corresponded to 2 SU, and one shot was 0.5 SU. We provided one single score per participant, collapsing drinking habits in weekdays and weekends.
DCD
DCD and ADHD co-occur in approximately 50% of cases29,30. Conceivably, it could mediate the relationship between ADHD, physical activity and obesity. Moreover, it could also be related to specific patterns of response in the EEfRT, where a fine motor output is required. We used the Adult Developmental Coordination Disorder/Dyspraxia Checklist-ADC 31 translated into Spanish by our research team. This is a Likert-scale questionnaire with 4 alternatives (0 = never, 3 = always) divided into two sections: (1) a 10-item assessment of developmental coordination disorder (as described in DSM-5) during childhood; (2) a 30-item exploration of current motor impairment in everyday activities. Higher values indicate more DCD symptoms.
Body-mass index (BMI) and smoking habits
Participants were asked about their height and weight. BMI was calculated as weight in kg divided by the square of height in meters. We also asked them the number of cigarettes, if any, smoked in a typical day.
Drug use in MINI
We assessed volunteers with the MINI International Neuropsychiatric Interview 32. Their responses on the use of illicit drugs (module K) were coded as 0 if they had not used any illicit substance in the last 12 months or 1 if they answered positively any question in module K.
Statistical analyses
We performed two independent sets of analyses. First, we explored specific patterns of responses in the effort-related tasks (EEfRT and hypothetical effort-discounting task) in relation to the factors of interest of this research: ADHD symptomatology and lifestyles. Thus, we used two logistic mixed models (one for each task) to estimate effort-related decisions from task- and subject-specific variables. Second, we pursued the overall goal of assessing the relationship between ADHD symptoms, effort discounting, and indicators of unhealthy habits. For this purpose, we selected one indicator for each effort-discounting task (proportion of effortful decisions in the EEfFRT, discounting constant k in the hypothetical task), and employed pairwise correlations and regression analyses.
The logistic mixed models assessed which task- and subject-specific variables explained effort-related decisions. The two effort-discounting tasks had singular characteristics that led to slightly different analyses. In the EEfRT task, the same trials were presented to every subject in the same order. Thus, decisions were non-independent (there were several decisions per subject and each task item was answered by several participants), and therefore we analysed responses with a crossed-effects logistic mixed model to assess which task features and subject-specific traits explained the selection of the high reward-high effort alternative. Choice was coded as 1 in the trials where that alternative was selected and 0 when participants chose the low effort alternative. The main hypothesis was that decisions would depend on the money and probability involved in each trial, and between-subject variables such as ADHD symptoms and physical activity might influence choices. Thus, the fixed effects of the model included trial-specific features (money and probability), trial number to examine fatigue, physical activity (GPAQ in Met-min) and ADHD symptoms (ASRS-18). As subject-specific covariates, we tested sex (0 = male, 1 = female), medication status (0 = controls, 1 = medicated ADHD, 2 = non-medicated ADHD), DCD symptoms, effort discounting (k from the hypothetical task), BMI and smoker (0 = no, 1 = yes). Crossed random effects were included for subjects and trials as recommended by other authors, for example33. Once included the variables of interest in the model (money and probability of the trial, trial number, GPAQ and ADHD symptoms, as well as the crossed random effects), we added the covariates one by one in an arbitrary order and tested whether they improved the goodness-of-fit of the model. This was quantified using the Bayesian Information Criteria (BIC; lower values indicate better goodness of fit). According to the standard interpretation34, when comparing two models, a difference (ΔBIC) between 0 and 2 indicates that both models are similar; a ΔBIC between 2 and 6 points to a significant difference, and a ΔBIC greater than 6 indicates that the model with the lower value is strongly better than the other. The logistic mixed model for the hypothetical effort-discounting task was similar except for the random effects: in this case, trials were different for every subject since they were automatically ‘selected’ by the algorithm. Therefore, only subjects were included as random effects. Concerning the dependent variable, the selection of the effortful option (20 € in exchange for certain amount of minutes running in a treadmill) was coded as 1, whereas the effortless option (certain amount of money with no effort involved) was coded as 0. In this case, the fixed-effects independent variables were the effort involved in the effortful alternative, the money involved in the effortless alternative, trial number (even though we did not expect an effect of fatigue in this case), and subject-specific traits such as ADHD and DCD symptomatology, and lifestyle indicators as mentioned above. The best models are explained in detail in the Results section.
The second set of analyses addressed the main objective of our study: to determine the relationship between ADHD symptoms, effort discounting and lifestyles. Consequently, the variables included were the following: (1) sociodemographic and general information: age, sex, medication status (as explained above); (2) symptom questionnaires: ASRS-18 and DCD; (3) physical effort discounting: EEfRT (overall fraction of high effort choices per participant) and hyperbolic k in the hypothetical task; (4) unhealthy habits and features: BMI, GPAQ, SIAC, smoker, number of cigarettes, drug consumption (from MINI). Most variables were positively skewed and kurtosis was very high (Table 1; Figure S1), so they were transformed by using the Box-Cox transformation. Since interpretability is difficult with transformed variables, we performed all analyses both in transformed and, as a sensitivity analysis, in the raw data. Individual associations between variables were evaluated through pair-wise correlations. Then, we used regression equations to answer whether ADHD symptoms and effort discounting (operationalized by either the EEfRT or the hypothetical task) had an effect on any unhealthy habit. Thus, each lifestyle indicator (weekly physical activity, alcohol consumption, smoking and drug use) was fitted to two regression models (including either EEfRT or k effort) with ADHD symptoms and effort discounting as independent variables, and sex and BMI as covariates. We repeated the main analyses using clinical diagnosis instead of ADHD symptoms in the Supplementary Information as a sensitivity analysis.
All statistical analyses were carried out in Stata 16.1 (StataCorp LLC, USA).
Results
Logistic mixed models to explain effort discounting decisions.
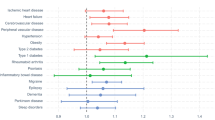
Regarding the EEfRT task, the best model (lowest BIC; Wald’s χ2(10) = 623.64, p < 0.0001) included the following fixed factors: money and probability involved in each decision, trial number, medication status of the participants, DCD symptoms, physical activity (GPAQ), smoking status and interaction between probability and medication status (Table 2). The crossed random effects included subject and trial number. Note that DCD symptoms improved the model with respect to ADHD symptoms. A list of all candidate models is shown in Table S2 (included in the Supplementary Information). Within this model, the variables that significantly explained decisions were probability, money, trial number, medication status and the interaction between medication status and probability (Fig. 1; see Table 2 for statistics). The explanatory role of the remaining variables was not significant. The variance inflation factor (VIF) of this model was low (mean VIF = 2.27), pointing to a low multicollinearity of predictors. Random effects were significant (χ2(2) = 1442.97, p < 0.0001), including the contribution of trial and volunteer. Thus, the probability and money involved in the trial influenced participants’ decisions. They were also affected by the medication status of participants (medicated participants selected the effortful alternative more often than controls), and the interaction of this variable with the probability of the trial (negative interaction in ADHD medicated and non-medicated participants with respect to controls). This shows that medicated ADHD volunteers were more prone to select the high effort alternative in low probability trials. Finally, there was a clear effect of fatigue (trial number), since volunteers tended to choose the high effort alternative less often through the course of the experiment (Fig. 1).
Effect of predictors on EEfRT decisions after the logistic mixed model. (A) Participants tended to choose the effortful alternative when money increased, but strongly depending on trial probability. Note that effortful choices for low probability trials (12%) were always below 0.5 irrespective of the money at stake, whereas they were above 0.7 in high probability trials, even for small rewards. (B) The effect of fatigue is apparent for all trial types: chances to select the effortful alternative decreased with trial number in all cases. (C) The probability of choosing the effortful alternative with respect to trial probability followed a nearly sigmoid shape for undiagnosed participants and medicated ADHD volunteers. However, the curve was less steep for medicated participants, whose preference for the effortful alternative was higher than the other groups in low-probability trials but similar to them in high-probability trials.
Regarding the hypothetical effort-discounting task, two models explained the data equally well (ΔBIC = 1). The only difference between them was the inclusion of ADHD symptomatology as independent variable, so we discuss this (see Table S2, in the Supplementary Information, for a list of all tested models). The model included the following fixed factors: money involved in the effortless option, effort involved in the effortful option, the interaction between these variables, response time, and ASRS-18 (Wald’s χ2(5) = 1381.25, p < 0.0001, BIC = 10,381). All variables significantly explained decisions: overall, selection of the effortful alternative was negatively explained by the money of the effortless alternative and the effort of the effortful one, and positively explained by the interaction between them and response time (Table 2). As expected, this interaction indicated that participants tended to avoid the effortful alternative when the money involved in the effortless one approached to 20 €, and when the effort proposed in the effortful alternative was high (see Fig. 2). Regarding ADHD symptoms, they were negatively associated with the selection of the effortful option. Multicollinearity of this model was also low (VIF = 4.53). Random effects included volunteers, and were also significant (χ2(1) = 789.29, p < 0.0001).
Effect of money of the effortless alternative and effort level (prospective minutes running) of the effortful alternative on decisions in the hypothetical effort discounting task. For all money amounts, the probability of choosing the high effort alternative was very low when approaching to the maximum effort level. However, as expected, this probability was higher in low effort decisions. In these cases, the money involved in the effortless alternative was the main factor to guide decisions. Note that the money offered in the effortful option was always 20 €. CI, Confidence Interval.
In conclusion, volunteers’ decisions in both tasks were adequately explained by task parameters. More precisely, the EEfRT task was more sensitive to DCD symptoms, fatigue, medication status and lifestyle indicators (sedentarism and smoking), whereas decisions in the hypothetical task were only explained by ADHD symptoms, in addition to task parameters.
Association between ADHD symptoms, physical effort discounting and lifestyles.
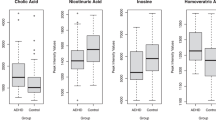
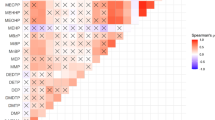
To have an initial, exploratory, assessment of the relationship between all variables of interest, we built a correlation matrix that included ADHD symptoms, the EEfRT main outcome variable (overall fraction of high effort choices), the main outcome of the effort-discounting hypothetical task (hyperbolic k), DCD symptoms, GPAQ Met-mins, BMI, SIAC, smoker, number of cigarettes and drug use according to MINI. The matrix is shown in Table 3 and Table S3 for transformed and raw variables, respectively. ADHD symptoms were positively correlated with k effort, DCD and smoker. In addition, the outcome variables of both effort-discounting tasks were negatively correlated. This negative correlation was expected because, whereas higher k values indicate more effort discounting (or a greater cost of effort), the EEfRT variable was the proportion of effortful choices, and therefore inversely proportional to effort discounting. Also, GPAQ results negatively correlated with k effort, showing that volunteers with higher effort discounting (higher k) followed a more sedentary lifestyle (lower Met-mins). Finally, smoking was positively associated with BMI and alcohol consumption (see Fig. 3). All correlations held for raw variables except those involving k effort, likely due to its extremely asymmetric and skewed distribution. Differences in ADHD symptoms, BMI and alcohol consumption by smoking status of participants were confirmed by t-tests in transformed variables (ASRS-18: two-tailed t(164) = − 2.16, p = 0.0322, Cohen’s d = − 0.37, 95% CI (− 0.71, − 0.03); BMI: two-tailed t(159) = − 2.07, p = 0.0398, Cohen’s d = − 0.36, 95% CI (− 0.71, − 0.02); SIAC: two-tailed t(130) = − 4.37, p < 0.0001, Cohen’s d = − 0.81, 95% CI (− 1.19, − 0.43)), and Mann–Whitney U tests in raw variables (ASRS-18: z = − 2.197, p = 0.028, Cohen’s d 95% CI after bootstrapping (− 0.69, − 0.03); BMI: z = − 1.871, p = 0.0613, Cohen’s d (− 0.71, − 0.02); SIAC: − 4.48, p < 0.0001, Cohen’s d (− 1.14, − 0.30)) (see Fig. 4).
Scatter plots showing the significant association between effort discounting (k effort) and ADHD symptoms (ASRS-18) (A), ADHD and developmental co-ordination disorder (DCD) symptoms (B), the hypothetical (k effort) and immediate (EEfRT) effort discounting tasks used in this study (C), and hypothetical effort discounting and a sedentary lifestyle (GPAQ) (D). All variables but EEfRT (proportion of effortful choices throughout the task) were transformed as explained in the text. The linear fit prediction with 95% confidence interval is shown for each plot.
In summary, ADHD symptoms were associated with effort discounting, DCD symptoms and smoking. Also, effort discounting was correlated with a sedentary lifestyle. Finally, smoking was associated with two other indicators of negative lifestyles, namely BMI and alcohol consumption.
Finally, we asked whether each indicator of unhealthy lifestyles was associated with ADHD symptoms and effort discounting. We ran two regressions for each lifestyle indicator (GPAQ, SIAC, smoking and drug use), including ASRS-18, effort-discounting (either EEfRT or hypothetical task) and their interaction as independent variables of interest. In all cases, sex and BMI were included as covariates. Regarding weekly physical activity, the model was only significant when the hypothetical task was included (F(5,152) = 3.02, p = 0.0125, Adjusted R2 = 0.06). ASRS-18 and its interaction with effort-discounting significantly explained the data (see Table 4), suggesting that a sedentary lifestyle (lower GPAQ values) was associated with higher ADHD symptoms, and this effect was reinforced by effort discounting (higher k values) (Fig. 5). Since ASRS-18 and k were correlated (see Table 3), the VIF of this model was moderately high (mean VIF = 12.75). As recommended by some experts35, since standard errors of the coefficients were low, we did not take any measure to reduce collinearity.
Interaction of ADHD symptoms and effort discounting (hypothetical task) on weekly physical activity (GPAQ). The graph shows that, for participants with low ADHD symptoms (10th percentile), effort discounting was weakly associated with physical activity. However, for participants with high ADHD symptoms (90th percentile), effort discounting strongly predicted a sedentary lifestyle (low GPAQ levels).
About alcohol use, including the same covariates, none of the regression equations was significant, and sex was the only significant predictor within the model (pointing to a higher alcohol consumption in male even when controlling by BMI). The logistic regression on smoking was significant with both effort-discounting indicators (EEfRT: LR χ2(5) = 11.29, p = 0.046, Pseudo R2 = 0.06; hypothetical task: LR χ2(5) = 12.81, p = 0.025, Pseudo R2 = 0.067). When including EEfRT, no independent variable reached statistical significance (see Table S4), and collinearity was lower (mean VIF = 9.78). Setting the hypothetical task as predictor, the effect of ASRS-18 was slightly more substantial (p = 0.031), suggesting an explanatory impact of ADHD symptoms on smoking when controlling for the rest of the variables (see Table 4). This regression also had high VIF values, but collinearity did not seem to affect the analysis due to the relatively low standard errors of coefficients. The models including drug use as dependent variable were also non-significant. See Table S4 for all non-significant models.
In conclusion, the regression models revealed an effect of ADHD symptoms and physical effort discounting on a sedentary lifestyle, and an influence of ADHD symptoms on smoking when controlling by the other variables.
Discussion
Our study shows an association between ADHD symptomatology in adults, the impact of physical effort on decision making, and negative lifestyles: ADHD symptoms were associated with effort discounting, a sedentary lifestyle and smoking. The EEfRT was not associated with any ecological measure of lifestyle or symptoms scale, but its main outcome (fraction of effortful choices) correlated with the effort-discounting hypothetical task. According to the EEfRT results, medicated participants diagnosed with ADHD had a blunted perception of probability, since they tended to choose the effortful alternative more frequently (with respect to controls and non-medicated ADHD) in low-probability trials.
We demonstrate that a ‘laboratory tool’ to measure the impact of physical effort in decision making is associated with an ecological indicator of a sedentary lifestyle. This confirms previous findings of our group in smaller samples13,36. In addition, ADHD symptoms interacted with this association, suggesting that the effect of physical effort discounting on low levels of daily physical activity is increased by ADHD symptoms. Unexpectedly, this association was not present when using the EEfRT to measure effort-based decision making. To our knowledge, the relationship between EEfRT and a sedentary lifestyle has not been analysed in previous reports, although several studies have found a performance impairment in this task in relation to mood conditions that can lead to sedentarism. For instance, EEfRT-related decisions co-varied with amotivation in schizotypy individuals37, participants with high anhedonia chose less often the high effort alternative with respect to controls38, and a similar effect occurred in depression39,40. Also, a recent study showed a negative correlation between BMI and the proportion of high-effort choices in the EEfRT41. The reason why a hypothetical effort-discounting task is more sensitive to correlate with ecological measures than the EEfRT may be the motivation induced by immediate monetary rewards. Also, the type of effort involved in this task could be perceived as more accessible to people with a sedentary lifestyle, whereas the physical exercise proposed in the effort-discounting task (minutes running on a treadmill), albeit hypothetical, could be more demanding.
Furthermore, we prove an association between physical effort discounting and ADHD symptoms in young adults. Rather than splitting our sample by diagnosis, we followed a transdiagnostic approach and found that symptoms explained the effort-discounting constant k. Although previous studies suggested the affectation of effort processing in ADHD42,43,44, this is the first proof to link symptoms with a higher cost of physical effort in decision making. As we explained in the Introduction, a transdiagnostic approach minimises the under-diagnosis of this disorder and could be more adequate for conditions that clearly show a continuum in the general population rather than a clear-cut dichotomous characterisation. In this respect, ADHD symptoms strongly correlated with DCD symptoms. The association between executive functions and motor skills may underlie this correlation, as initially suggested by Barkley45. Recent research shows that DCD increases the risk of showing executive dysfunction29,46,47. Children with ADHD often present difficulties in tasks with a high demand for motor skills48. Our study suggests that this could also be the case in adults.
Regarding ADHD and negative lifestyles, symptoms were associated with the probability of participants being smokers. Note that participants were asked about cigarette use, but not vaping: this is a limitation of this part of the study. The link between ADHD symptoms and smoking habits was previously demonstrated in adolescents49 and young adults50. Rhodes and collaborators51 showed that young adults with a previous ADHD diagnosis were more likely to become smokers. Recent research suggests the putative genetic component of this link52, pointing to impulsivity-related single-nucleotide polymorphisms. McClernon and Kollins53 modelled the increased risk of ADHD and smoking co-occurrence as the merge of genetic predisposition, in turn related to aberrant dopamine functioning, increased novelty-seeking and impulsivity, deficits in impulse control, and various social factors. In our study, smoking also correlated with other possible indicators of negative lifestyles, such as BMI and alcohol consumption. Therefore, based on this set of indirect associations, a hypothesis to be tested in the future is whether smoking could be the gate for people with high ADHD symptoms to enter other negative lifestyles, such as harmful alcohol consumption or obesity.
The main limitation of our research is the inability to control for the different kinds of medication taken by ADHD-diagnosed participants. The initial intention of our overall project was to assess participants in two visits; in the case of medicated ADHD volunteers, they were asked to take the treatment as usual in one of the visits and delay its administration after the other assessment since most ADHD medications do not need a washout period. However, we could not achieve this objective due to dropouts for the second session and the limited number of medicated participants.
Another possible limitation is that we did not collect subjective ratings of effort by the participants in any of the physical effort-discounting tasks. Asking participants about their actual experience on effort expenditure during the EEfRT, or their prospective subjective feeling about the hypothetical task, could have helped interpreting the relationship between the variables of interest of our experiment. To mitigate this, the constant estimated after the hypothetical effort-discounting task (k) is usually understood as a subjective proxy of effort cost54,55; therefore, even though we did not explicitly ask participants about their subjective feeling with respect to effort, the actual subjective cost could have been captured by this task. The approach we used for the hypothetical effort discounting task could not capture a feature that has been reported in temporal discounting56: in some cases, participants have been shown to be willing to pay extra money now than a lower amount after several months. These volunteers were tagged as “debt averse” by the researchers. Applied to physical effort discounting, some participants would be willing to choose an effortless alternative, paying some extra money, instead of choosing to make an effort and a lower payment. Indeed, this was not captured by our task, but it is relevant for daily activities: many of us prefer driving for 10 min to the city centre instead of walking for 30 min, even though we would have to pay for the gas and the parking. Regarding the lifestyle indicators included in the study, we selected one directly related to effort discounting (i.e., sedentary lifestyle) and those potentially associated with it, such as smoking, alcohol, and drug use. There are other indicators that could have been included, such as education, employment markers, time watching TV or use of other substances, for instance.
Our research suggests new lines of research. Since ADHD symptoms are associated with effort-discounting and unhealthy habits indicators, the causal processes underlying these relationships should be addressed. Are genetic determinants, neural substrates, and behavioural and/or social factors mediating these associations? How should therapeutic approaches to ADHD deal with these issues? Can medication protect from the development of unhealthy habits, or should they be treated through psychotherapy?
Conclusions
Our research shows that ADHD symptoms in young adults are related to an increased sensitivity to the cost of physical effort in decision making and to unhealthy habits such as a sedentary lifestyle and smoking. Further, smoking is associated with BMI and alcohol consumption. Overall, this points to an underlying structure that may explain why ADHD patients are more prone to harmful lifestyles.
Data availability
We provide as supplementary materials the two databases produced by this project and the Stata logs pertaining to all analyses.
Abbreviations
- ADHD:
-
Attention deficit/hyperactivity disorder
- ASRS:
-
ADHD self-report scale
- BIC:
-
Bayesian information criteria
- BMI:
-
Body-mass index
- DCD:
-
Developmental co-ordination disorder
- EEfRT:
-
Effort expenditure for rewards task
- GPAQ:
-
Global physical activity questionnaire
- MINI:
-
MINI international neuropsychiatric interview
- SD:
-
Standard deviation
- SIAC:
-
Systematic inventory of alcohol consumption
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. (American Psychiatric Publishing, Inc., 2013). https://doi.org/10.1176/appi.books.9780890425596
Thomas, R., Sanders, S., Doust, J., Beller, E. & Glasziou, P. Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics 135, e994–e1001 (2015).
Asherson, P. et al. Mainstreaming adult ADHD into primary care in the UK: Guidance, practice, and best practice recommendations. BMC Psychiatry 22, 640 (2022).
Chaulagain, A. et al. A systematic meta-review of systematic reviews on attention deficit hyperactivity disorder. Eur. Psychiatry 66, e90 (2023).
Björk, A., Rönngren, Y. & Våge, L. Adult Persons with ADHD and Their Lifestyle. In Clinical Handbook of ADHD Assessment and Treatment Across the Lifespan. Autism and Child Psychopathology Series (ed. Matson, J.) 161–182 (Springer, 2023). https://doi.org/10.1007/978-3-031-41709-2_7
Weissenberger, S. et al. ADHD and lifestyle habits in Czech adults, a national sample. Neuropsychiatr. Dis. Treat. 14, 293–299 (2018).
Upadhyaya, H. P. & Carpenter, M. J. Is attention deficit hyperactivity disorder (ADHD) symptom severity associated with tobacco use?. Am. J. Addict. 17, 195–198 (2008).
Anker, E., Haavik, J. & Heir, T. Alcohol and drug use disorders in adult attention-deficit/hyperactivity disorder: Prevalence and associations with attention-deficit/hyperactivity disorder symptom severity and emotional dysregulation. World J. Psychiatry 10, 202–211 (2020).
Mitchell, S. H. & Sevigny-Resetco, D. Effort-related decision-making in ADHD. J. Psychiatry Brain Sci. 5, e200027 (2020).
Wagner, D., Mason, S. G. & Eastwood, J. D. The experience of effort in ADHD: a scoping review. Front. Psychol. 15, 1349440 (2024).
Orhan, I., Corr, P. J. & Krupić, D. ADHD and the avoidance of mental effort: The role of response inhibition and avoidance motivation. J. Clin. Exp. Neuropsychol. 45, 537–552 (2023).
Green, L. & Myerson, J. A discounting framework for choice with delayed and probabilistic rewards. Psychol. Bull. 130, 769–792 (2004).
Bernacer, J. et al. Brain correlates of the intrinsic subjective cost of effort in sedentary volunteers. Prog. Brain Res. 229, 103–123 (2016).
Treadway, M. T., Buckholtz, J. W., Schwartzman, A. N., Lambert, W. E. & Zald, D. H. Worth the ‘EEfRT’? The effort expenditure for rewards task as an objective measure of motivation and anhedonia. PLoS ONE 4, e6598 (2009).
Mies, G. W., Ma, I., de Water, E., Buitelaar, J. K. & Scheres, A. Waiting and working for rewards: Attention-Deficit/Hyperactivity Disorder is associated with steeper delay discounting linked to amygdala activation, but not with steeper effort discounting. Cortex 106, 164–173 (2018).
Acuff, S. F., Simon, N. W. & Murphy, J. G. Effort-related decision making and cannabis use among college students. Exp. Clin. Psychopharmacol. 31, 228–237 (2023).
Johnstad, P. G. Unhealthy behaviors associated with mental health disorders: a systematic comparative review of diet quality, sedentary behavior, and cannabis and tobacco use. Front. public Heal. 11, 1268339 (2023).
Cortese, S. et al. Association between ADHD and obesity: A systematic review and meta-analysis. Am. J. Psychiatry 173, 34–43 (2016).
Lee, S. S., Humphreys, K. L., Flory, K., Liu, R. & Glass, K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clin. Psychol. Rev. 31, 328–341 (2011).
Dalsgaard, S., Østergaard, S. D., Leckman, J. F., Mortensen, P. B. & Pedersen, M. G. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: A nationwide cohort study. Lancet (London, England) 385, 2190–2196 (2015).
London, A. S. & Landes, S. D. Attention deficit hyperactivity disorder and adult mortality. Prev. Med. (Baltim) 90, 8–10 (2016).
Barbaresi, W. J. et al. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: A prospective study. Pediatrics 131, 637–644 (2013).
Wolraich, M. L. & Doffing, M. A. Pharmacokinetic considerations in the treatment of attention-deficit hyperactivity disorder with methylphenidate. CNS Drugs 18, 243–250 (2004).
Adler, L. A., Alperin, S., Leon, T. & Faraone, S. V. Pharmacokinetic and pharmacodynamic properties of lisdexamfetamine in adults with attention-deficit/hyperactivity disorder. J. Child Adolesc. Psychopharmacol. 27, 196–199 (2017).
Sauer, J.-M., Ring, B. J. & Witcher, J. W. Clinical pharmacokinetics of atomoxetine. Clin. Pharmacokinet. 44, 571–590 (2005).
Kessler, R. C. et al. The world health organization adult ADHD self-report scale (ASRS): A short screening scale for use in the general population. Psychol. Med. 35, 245–256 (2005).
Roman-Viñas, B. et al. International physical activity questionnaire: Reliability and validity in a Spanish population. Eur. J. Sport Sci. 10, 297–304 (2010).
Gual, A., Contel, M., Segura, L., Ribas, A. & Colom, J. The ISCA (Systematic Interview of Alcohol Consumption), a new instrument to detect risky drinking. Med. Clin. (Barc) 117, 685–689 (2001).
Blank, R. et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Dev. Med. Child Neurol. 61, 242–285 (2019).
Goulardins, J. B., Marques, J. C. B. & De Oliveira, J. A. Attention deficit hyperactivity disorder and motor impairment. Percept. Mot. Skills 124, 425–440 (2017).
Kirby, A., Edwards, L., Sugden, D. & Rosenblum, S. The development and standardization of the Adult Developmental Co-ordination Disorders/Dyspraxia Checklist (ADC). Res. Dev. Disabil. 31, 131–139 (2010).
Sheehan, D. V. et al. The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry (1998). https://doi.org/10.1016/S0924-9338(99)80239-9
Baayen, R. H., Davidson, D. J. & Bates, D. M. Mixed-effects modeling with crossed random effects for subjects and items. J. Mem. Lang. 59, 390–412 (2008).
Kass, R. E. & Raftery, A. E. Bayes factors. J. Am. Stat. Assoc. 90, 773–795 (1995).
O’Brien, R. M. A caution regarding rules of thumb for variance inflation factors. Qual. Quant. 41, 673–690 (2007).
Bernacer, J. et al. An amygdala-cingulate network underpins changes in effort-based decision making after a fitness program. Neuroimage 203, 116181 (2019).
Chu, R. S. T. et al. Effort-based decision making in schizotypy and its relationship with amotivation and psychosocial functioning. Front. Psychiatry 14, 1123046 (2023).
Slaney, C. et al. Objective measures of reward sensitivity and motivation in people with high versus low anhedonia. Psychol. Med. 53, 4324–4332 (2023).
Yang, X.-H. et al. Motivational deficits in effort-based decision making in individuals with subsyndromal depression, first-episode and remitted depression patients. Psychiatry Res. 220, 874–882 (2014).
Treadway, M. T., Bossaller, N. A., Shelton, R. C. & Zald, D. H. Effort-based decision-making in major depressive disorder: A translational model of motivational anhedonia. J. Abnorm. Psychol. 121, 553–558 (2012).
Mansur, R. B. et al. Effort-based decision-making is affected by overweight/obesity in major depressive disorder. J. Affect. Disord. 256, 221–227 (2019).
Sonuga-Barke, E. J. The dual pathway model of AD/HD: An elaboration of neuro-developmental characteristics. Neurosci. Biobehav. Rev. 27, 593–604 (2003).
Sergeant, J. A. Modeling attention-deficit/hyperactivity disorder: A critical appraisal of the cognitive-energetic model. Biol. Psychiatry 57, 1248–1255 (2005).
Chong, T.T.-J., Fortunato, E. & Bellgrove, M. A. Amphetamines improve the motivation to invest effort in attention-deficit/hyperactivity disorder. J. Neurosci. 43, 6898–6908 (2023).
Barkley, R. A. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychol. Bull. 121, 65–94 (1997).
Tal Saban, M., Ornoy, A. & Parush, S. Executive function and attention in young adults with and without developmental coordination disorder—A comparative study. Res. Dev. Disabil. 35, 2644–2650 (2014).
Schott, N. & Holfelder, B. Relationship between motor skill competency and executive function in children with Down’s syndrome. J. Intellect. Disabil. Res. 59, 860–872 (2015).
Papadopoulos, N., McGinley, J. L., Bradshaw, J. L. & Rinehart, N. J. An investigation of gait in children with attention deficit hyperactivity disorder: A case controlled study. Psychiatry Res. 218, 319–323 (2014).
Gudjonsson, G. H., Sigurdsson, J. F., Sigfusdottir, I. D. & Young, S. An epidemiological study of ADHD symptoms among young persons and the relationship with cigarette smoking, alcohol consumption and illicit drug use. J. Child Psychol. Psychiatry 53, 304–312 (2012).
van Amsterdam, J., van der Velde, B., Schulte, M. & van den Brink, W. Causal factors of increased smoking in ADHD: A systematic review. Subst. Use Misuse 53, 432–445 (2018).
Rhodes, J. D. et al. Cigarette smoking and ADHD: An examination of prognostically relevant smoking behaviors among adolescents and young adults. Psychol. Addict. Behav. 30, 588–600 (2016).
Treur, J. L. et al. Investigating causality between liability to ADHD and substance use, and liability to substance use and ADHD risk, using Mendelian randomization. Addict. Biol. 26, e12849 (2021).
McClernon, F. J. & Kollins, S. H. ADHD and smoking. Ann. N. Y. Acad. Sci. 1141, 131–147 (2008).
Seaman, K. L. et al. Subjective value representations during effort, probability and time discounting across adulthood. Soc. Cogn. Affect. Neurosci. 13, 449–459 (2018).
Chong, T.T.-J. et al. Neurocomputational mechanisms underlying subjective valuation of effort costs. PLOS Biol. 15, e1002598 (2017).
Myerson, J., Baumann, A. A. & Green, L. Individual differences in delay discounting: Differences are quantitative with gains, but qualitative with losses. J. Behav. Decis. Mak. 30, 359–372 (2017).
Acknowledgements
We thank Irati García, Patricia Díaz and Anaemilia Miño for their excellent technical assistance and all the undergraduate students who assisted in the assessments. We are also indebted to Nerea Crespo, Maite Aznárez, Pilar de Castro, María Vallejo, Carlos García-Roda, David Ramírez, César Soutullo, Azucena Díez, Irene Alústiza, David Brugos and Ignacio Gaínza for their participation in different stages of the project.
Funding
This study is supported by the Spanish Ministerio de Economía, Industria y Competitividad – Agencia Estatal de Investigación, including FEDER funds (ref. no. PSI2017-86763-P). It is also funded by Fundación Tatiana. GA is supported by a grant RYC2020‐030744‐I funded by MCIN/AEI/https://doi.org/10.13039/501100011033 and by “ESF Investing in your future”. SM is supported by a grant RYC-2017-22060 funded by MCIN/AEI/ and by PID2020–119328GA-I00 AEI Proyectos I + D + i funded by MCIN/AEI.
Author information
Authors and Affiliations
Contributions
J.B. and G.A. conceived the project. J.B., L.G., S.M. and G.A. participated in data collection. J.B., L.G., D.R.-R., M.E.C, S.M. and G.A. participated in data curation and analysis. J.B. and D.R.-R. prepared the first draft of the manuscript, which was extensively revised and approved by L.G., M.E.C, S.M. and G.A.
Corresponding author
Ethics declarations
Competing interest
The authors declare an absence of competing interests, either financial or non-financial.
Ethical approval and consent to participate
All procedures were revised and approved by the Committee of Ethics in Research of the University of Navarra (protocol number 2018.040). All participants signed the informed consent form after reading the information sheet and an oral project explanation. The research complies with the Helsinki Declaration of Human Rights (revised in Seoul in 2008).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bernacer, J., Gambra, L., Rodriguez-Romero, D. et al. Association between ADHD symptoms, physical effort discounting, and unhealthy lifestyles in adults. Sci Rep 15, 17255 (2025). https://doi.org/10.1038/s41598-025-02024-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02024-9