Abstract
This study aims to evaluate sociodemographic information, lifestyle, physical and mental health status, and otological symptoms factors associated with the accuracy of the Hearing Handicap Inventory for the Elderly Screening version (HHIE-S) in older people, which helps to increase the efficiency of hearing screening. Participants aged over 60 years who had not undergone professional hearing examinations were recruited from July 2023 to November 2024. The assessments consisted of age, sex, body mass index, living alone, education background, occupation, history of smoking, alcohol consumption, noise exposure, hypertension, diabetes, coronary heart disease, cerebrovascular disease, cognitive function, anxiety, depression, tinnitus and vertigo, along with HHIE-S and pure tone audiometry. The rate of total accuracy, total inaccuracy, false negative, and false positive were calculated, and factors associated with the false negatives and false positives of the HHIE-S were analyzed via multivariate logistic regression analysis. The results revealed that 773 participants (aged 60–93 years) were included, and the total inaccuracy rate of the HHIE-S was 33.11%. Among individuals with normal hearing, the false positive rate of the HHIE-S was 13.64%, while the false negative rate was 36.35% among individuals with hearing loss. Tinnitus (OR = 24.77, 95% CI 4.91–124.89) was the main factor contributing to false positives of HHIE-S. However, the significantly associated factors with false negatives of HHIE-S were living alone (OR = 1.96, 95% CI 1.21–3.17), smoking (OR = 1.83, 95% CI 1.23–2.70), cognitive decline (OR = 1.54, 95% CI 1.11–2.16), anxiety (OR = 1.51, 95% CI 1.02–2.22) and hypertension (OR = 0.65, 95% CI 0.46–0.91). Therefore, even when the HHIE-S ≤ 8 during hearing screening for the older people, there is still a possibility of hearing loss. Vigilance should be maintained associated factors such as living alone, smoking, cognitive decline and anxiety.
Similar content being viewed by others
Introduction
Hearing loss is the most common sensory disorder in older people, and the proportion of individuals experiencing any degree of hearing loss exceeds 42.0% among those aged above 60 years1. Globally, the prevalence of moderate to severe hearing loss increases exponentially with age, increasing from 15.4% among individuals in their sixth decade of life to 58.2% among those aged more than ninety years1. Untreated hearing loss not only affects communication and interaction but also has adverse effects on various aspects of the aged population, including frailty, falls, gout and cognitive decline2,3,4. Furthermore, the Lancet Commission on Dementia Prevention, Intervention, and Care recognized hearing loss as one of the modifiable risk factors for dementia in 20175. Although the population attributable fraction (PAF) of hearing loss has decreased from 9.1 to 7.0% with further research, hearing loss still ranks first among the 14 modifiable risk factors in 20246. Therefore, early detection of hearing loss through screening in older people is essential so that timely interventions can be facilitated and the occurrence of adverse events can be mitigated7.
The Hearing Handicap Inventory for the Elderly Screening version (HHIE-S) is the most commonly used tool among numerous available modalities of hearing screening for older people8. It was developed by Ventry and Weinstein in 1982 and has gained popularity because of its cost-effectiveness and accessibility9. Compared with the whisper test and the single question test, the HHIE-S had a stronger correlation with hearing thresholds and quality of life10,11. A study had shown that the HHIE-S has greater sensitivity for the assessment of hearing loss than other scales, such as the Speech, Spatial, and Qualities of Hearing Scale-12 (SSQ12)12. Furthermore, HHIE-S results had been used to represent the actual hearing status of the older population in some studies13. In 2021, the World Health Organization (WHO) recommended the use of the HHIE-S as the first step in hearing screening to understand hearing status and assess whether daily hearing difficulties are experienced by older adults14. At present, the HHIE-S had been translated into multiple languages, including Italian and Chinese, and all versions have been proven to be satisfactory in hearing assessment15,16.
Remarkably, the sensitivity of the HHIE-S varies considerably among different studies, ranging from 51.0 to 86.4%, and the specificity spanned from 72.4–100.0%16,17. Many studies had shown that the consistency between HHIE-S scores and pure tone average hearing threshold varies by the degree of hearing loss, age, sex, ethnicity, and other factors10,18. Additionally, older adults, who experience a gradual decline in physical functioning, have a multimorbidity prevalence rate ranging from 55.0–98.0%19. Many studies have shown that factors such as noise exposure, hypertension, and depression may affect the accuracy of self-reported hearing loss18,20. However, the effects of physical and mental health status, otological symptoms on the results of the HHIE-S remain unknown. In this context, it is crucial to explore sociodemographic information, lifestyle, physical and mental health status, and otological symptoms factors associated with the accuracy of the HHIE-S. Understanding the impact of various factors can help healthcare professionals optimize the use of the HHIE-S and enhances the efficiency of hearing screenings and facilitates early interventions. Ultimately, these efforts can reduce adverse outcomes associated with hearing loss.
Methods
Study participants
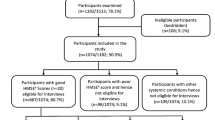
Participants were recruited through social media notices and community activities in a community from July 2023 to November 2024 in Beijing, China. Individuals aged over 60 years who had not undergone professional hearing examinations were included. Individuals who were either incapable of cooperating with the questionnaire survey or hearing test due to severe illness or not willing to complete it were excluded from the study. Approval for this research was granted by Beijing Tongren Hospital, Capital Medical University (TREC2023-KY075). All procedures adhered to the approvals, and all participants provided their consent through signed informed consent forms. All the processes were performed in accordance with the Declaration of Helsinki.
Evaluation of associated factors
Some possible factors associated with the accuracy of the HHIE-S were selected, including the following: (1) sociodemographic and lifestyle factors, including age, sex, body mass index (BMI), living alone, education background, occupation, history of smoking, alcohol consumption and noise exposure; and (2) physical and mental health status and otological symptoms, including a history of hypertension, diabetes, coronary heart disease, cerebrovascular disease, cognitive function, anxiety, depression, tinnitus and vertigo.
The criteria were as follows: (1) Sociodemographic and lifestyle factors were obtained through direct inquiry of the participants, with BMI was calculated as weight divided by the square of height. Noise exposure referred to occupational noise, meaning exposure to steady noise with a noise rating of 85 dB for eight hours per day for five days per week for one years21. (2) Hypertension was diagnosed as persistent or three or more occasions on different days with a seated systolic blood pressure ≥ 140 mmHg and/or a diastolic blood pressure ≥ 90 mmHg22. (3) Diabetes was diagnosed on the basis of a hemoglobin A1c level ≥ 6.5%, a fasting plasma glucose value ≥ 126 mg/dL, a 2-hour plasma glucose value ≥ 200 mg/dL during a 75-g oral glucose tolerance test, a random glucose value ≥ 200 mg/dL, or classic hyperglycemic symptoms/crisis criteria23. (4) Coronary heart disease and cerebrovascular disease: participants were asked about heart and cerebrovascular diseases diagnosed by a specialist doctor. (5) Tinnitus was the perception of sound without an external source within one month, and vertigo was defined as a sensation of false movement within one month. (6) Cognitive function was assessed by the Montreal Cognitive Assessment (MoCA), which has a maximum score of 30 points. If the subject had 12 years or less of education, 1 point was added to the result, and a score of less than 26 was considered to indicate cognitive decline. (7) Anxiety and depression were assessed by the Generalized Anxiety Disorder-7 (GAD-7) scale and the Patient Health Questionnaire-9 (PHQ-9), respectively. The GAD-7 has a total score of 21, and a score greater than 5 indicates that anxiety has already affected quality of life in some aspects. The PHQ-9 has a total score of 27, and a score greater than 4 suggests the possibility of mild depression.
Although hearing loss may affect the results of questionnaires related to information acquisition, cognitive function, and emotions by influencing verbal communication, researchers employed methods such as increasing the volume of the conversation or using visual-textual aids to ensure that participants could accurately understand the assessment content and respond accordingly.
Assessment of the HHIE-S
First, each participant received general instructions for the HHIE-S from the trained physician. There were 10 items in total and two subscales, the Social Subscale and the Emotional Subscale. The items were then administered through a single round of face-to-face questioning. If the participant did not understand a question, appropriate explanations were provided. The interviewer recorded the participant’s first response and assigned a score of 0 for “no” responses, 2 for “sometimes” responses, and 4 for “yes” responses. The total scores were calculated as the sum of all the item scores, and the score range was 0–40. The total scores of the HHIE-S above 8 (HHIE-S > 8) were indicative of “hearing loss”. Conversely, a total HHIE-S score of 8 or less (HHIE-S ≤ 8) indicated “normal hearing”.
Assessment of pure tone audiometry
After the interview with the HHIE-S questionnaire, the individual was referred for further examination by pure tone audiometry, mostly on the same day as the initial interview. Pure tone audiometry was carried out in a quiet room with background noise less than 35 dB(A) after otoscopy. Air-conducted thresholds at 0.5, 1, 2, and 4 kHz for each ear were obtained with Danish International Hearing’s Conera Diagnostic Sound Level Meter. In accordance with the WHO (2021), hearing loss was defined as the pure tone average (PTA) at 0.5, 1, 2 and 4 kHz of air-conducted (PTA0.5–4 kHz) in the better ear being greater than or equal to 20 dB HL or more than or equal 35 dB HL in the worse ear1. Conversely, individuals with a PTA0.5–4 kHz of less than 20 dB in the better ear and less than 35 dB in the worse ear were classified as having normal hearing.
Following the PTA0.5–4 kHz, the participants were divided into those with normal hearing and those with hearing loss. Among individuals with normal hearing, older people who score 8 points or less on the HHIE-S were classified into the normal hearing accuracy group (NH accuracy group), while those scoring more than 8 points were placed in the false positive group. Among individuals with hearing loss, older people who score more than 8 points on the HHIE-S were categorized into the hearing loss accuracy group (HL accuracy group), and those scoring 8 points or less were assigned to the false negative group.
Statistical analysis
The total accuracy rate is equal to the sum of the number of individuals with normal hearing and an HHIE-S score of 8 points or less, and those with hearing loss and an HHIE-S score greater than 8 points, divided by the total number of participants (n = 773). Conversely, the total inaccuracy rate is equal to the sum of the number of individuals with normal hearing and an HHIE-S score greater than 8 points, and those with hearing loss and an HHIE-S score of 8 points or less, divided by the total number of participants (n = 773). The false positive rate is equal to the number of individuals with normal hearing and an HHIE-S score greater than 8 points divided by the number of individuals with normal hearing (n = 110). The false negative rate is equal to the number of individuals with hearing loss and an HHIE-S score of 8 points or less divided by the number of individuals with hearing loss (n = 663). (Table 1)
The Shapiro-Wilk test was used to test the normality of the quantitative data. Quantitative data were expressed as mean ± standard deviation (SD) if normally distributed, and median (25%, 75% quartile) if not. Categorical data were expressed as frequencies and proportions. Comparisons were made between quantitative data and count data of the NH accuracy group and the false positive group among the normal hearing populations, as well as between the HL accuracy group and the false negative group among the hearing loss populations, using t-tests, chi-square tests, or Fisher’s exact tests. Bonferroni test for multiple comparisons was conducted for “BMI”, “Occupation”, and “Education Background”. To avoid potentially missing the influence of important variables, variables that exhibited a significance level of P < 0.10 in the univariable analysis were subsequently included in a multivariate logistic regression model. “Age” was a continuous variable, and for “education background”, “less than high school education"=0, “high school education"=1, and “more than high school education"=2. Other independent variables were assigned “No"=0 and “Yes"=1. The Hosmer–Lemeshow test was used as a postestimation tool to demonstrate the goodness of fit of the logistic regression models. A dependent variable assigned a value of 1 indicated that the HHIE-S score was greater than 8 points in the normal hearing population and less than or equal to 8 points in the hearing loss population; otherwise, it was assigned a value of 0. The odds ratio (OR) and its corresponding 95% confidence interval (95% CI) were calculated via multiple logistic regression.
All the statistical analyses were performed via SPSS 25.0 (IBM SPSS Statistics 25.0; IBM, Redmond, WA, USA) and GraphPad Prism 8.0 (GraphPad Prism 8.0; Inc., San Diego, CA, USA). Statistical significance was set at P < 0.05 and all P values were two-sided tests.
Results
Population characteristics
A total of 773 people aged between 60 and 93 (mean age: 70.90 ± 7.37) years were included in the study. The study population consisted of 333 (43.08%) males and 440 (56.92%) females. 43.47% (n = 336) of the individuals had HHIE-S scores of 8 or below, whereas 56.53% (n = 437) had HHIE-S scores above 8. According to the PTA0.5–4 kHz, 14.23% (n = 110) of the individuals had normal hearing, and the remaining 85.77% (n = 663) had varying degrees of hearing loss.
Total accuracy rate, total inaccuracy rate, false positive rate, and false negative rate
The total accuracy rate of the HHIE-S was 66.89% among all individuals, whereas the total inaccuracy rate was 33.11%. On the other hand, the false positive rate of the HHIE-S was 13.64% among individuals with normal hearing. In the population with hearing loss, the false negative rate was 36.35% (Table 1).
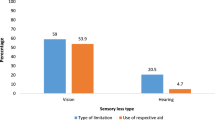
Factors associated with false positives on the HHIE-S in populations with normal hearing
The results of the univariate analysis are shown in Table 2. Compared with the NH accuracy group, older individuals with PTA0.5–4 kHz<20 dB HL in the false positive group had a greater rate of tinnitus (x2 = 28.72, P < 0.001).
In order to avoid omitting important potential factors and accomplish the regression analysis, with hypertension (P = 0.06), coronary heart disease (P = 0.07), cerebrovascular disease (P = 0.08), and tinnitus (P < 0.001) as the independent variables, the results of univariate logistic regression analysis revealed that tinnitus (OR = 24.77, 95% CI 4.91–124.89) was related to false positives in the HHIE-S (Fig. 1).
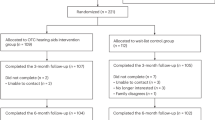
Factors associated with false negatives of the HHIE-S in a population with hearing loss
The univariate analysis results suggested that the individuals in false negative group were younger than the HL accuracy group (t = 3.05, P = 0.01). The participants in the false negative group had higher rates of living alone (x2 = 5.68, P = 0.02), smoking (x2 = 10.40, P = 0.01), cognitive decline (x2 = 6.44, P = 0.01) and anxiety (x2 = 4.90, P = 0.03) but a lower rate of hypertension (x2 = 8.53, P =0.003) (Table 2).
The logistic regression model revealed that the significant factors associated with increased false negatives of the HHIE-S included living alone (OR = 1.96, 95% CI 1.21–3.17), smoking (OR = 1.83, 95% CI 1.23–2.70), cognitive decline (OR = 1.54, 95% CI 1.11–2.16) and anxiety (OR = 1.51, 95% CI 1.02–2.22). However, hypertension (OR = 0.65, 95% CI 0.46–0.91) potentially enhanced the accuracy of the HHIE-S (Fig. 2).
Forest plot of a multivariate logistic regression analysis to explain the factors associated with the false negatives of the HHIE-S in the older population with hearing loss.
OR, odds ratio; CI, confidence interval. a The control group was composed of individuals with an education background of “less than high school education”.
Discussion
In this study, we observed that living alone, smoking, hypertension, cognitive decline, and anxiety were potentially associated with the false negatives of the HHIE-S among older individuals experiencing hearing loss. Notably, the purpose of hearing screening is to help older individuals who are unaware of hearing loss discern hearing abnormalities24. Therefore, missed screening may delay the diagnosis and intervention of hearing loss. Some studies had demonstrated that individuals with hypertension had a greater incidence of hearing loss and worse hearing thresholds25,26,27. Moderately severe hearing loss is easily perceived due to its impact on daily communication and life28. Therefore, older individuals who had hearing loss with hypertension were more likely to have hearing abnormalities through the subjective questionnaire. Although hypertension may enhance the credibility of HHIE-S results, greater attention should be paid to the hearing condition of aged people with hypertension. Regular re-screening should be conducted even if their HHIE-S score is 8 or less. Additionally, smoking can affect sensory gating and temporarily normalize the auditory gating deficit by the event-related potential P5029. This resulted in their inability to recognize hearing loss in cases of mild hearing loss, which may contribute to increasing the false negative rate of the HHIE-S among older individuals with hearing loss who also smoke30.
Illness perception domains are related to health behaviors in patients with various physical and mental conditions31. Older adults who live alone frequently exhibit emotional disturbances, including loneliness, social isolation, and depression32. On the one hand, personality traits significantly influence self-perception of hearing loss. Individuals with anxiety potentially experience heightened sensitivity to emotional difficulties, thereby neglecting their attention to auditory difficulties33. On the other hand, anxiety symptoms predict an increase in auditory looming bias and consequently lead to misunderstandings of hearing conditions34. Furthermore, the relationship between cognitive decline and hearing loss is relatively complex. Perception is a part of cognitive function, and impaired perceptive function may lead to hearing agnosia35. Moreover, many studies have shown that declines in spatial working memory and sustained attention are prevalent in older adults and are correlated with self-reported hearing loss36. Smoking, and anxiety can exacerbate cognitive decline and lead to misperceptions of subjective hearing status37. However, in this cross-sectional study, the possibility that cognition decline was a result of other factors cannot be excluded. In general, when the HHIE-S ≤ 8 in hearing screening among older people, attention should be given to factors such as living alone, smoking, cognitive decline, and anxiety in older people to avoid depriving them of the opportunity for hearing assessments.
Although age appeared to influence the accuracy of the univariate analysis, it was not a significant predictor in the logistic regression model. A study revealed that the sensitivity of the HHIE-S gradually decreased with increasing age. The results showed the highest sensitivity of 77.6% in people under 60 years of age, which decreased to 71.4% in those over 60 years of age18. This may be attributed to the normalization of hearing loss as an aspect of aging, which thereby reduces the perception of hearing problems as a treatable condition.
Only tinnitus was associated with the false positives of the HHIE-S in both the univariate analysis and logistic regression model among individuals with normal hearing. However, this result was not observed among those with hearing loss. In the general older population, tinnitus was observed in approximately one-fifth of the them38. Like individuals who are experiencing stress, those who suffer from tinnitus are prone to anxiety and display heightened sensitivity39. Moreover, individuals with tinnitus might find themselves in a state of confusion concerning their hearing ability. The intensity of tinnitus can sometimes overwhelm authentic sounds, thereby creating a misleading perception of their auditory status40. Furthermore, even tinnitus patients who exhibit normal results on an audiogram may have underlying hearing loss, which may not be immediately proven41. Therefore, during hearing screening, it was recommended to inquire about the presence of tinnitus in individuals with HHIE-S>8 and to conduct a comprehensive assessment subsequently.
In addition, we also observed that the total inaccuracy rate of the HHIE-S was approximately 33.11% in older adults. Specifically, the false positive rate among individuals with normal hearing was about 13.64%, while the false negative rate among those with hearing loss reached approximately 36.35%. A study in northeastern China suggested that the sensitivity of the HHIE-S in detecting hearing loss was only 60.5%, and its specificity was 71.7%15. However, a multicenter study revealed that the probability that a person was affected by hearing loss when HHIE-S > 8 was 90.21%42. There was considerable variation in the accuracy of the HHIE-S across different studies. The HHIE-S is a subjective questionnaire that assesses hearing status in older people on the basis of whether they have difficulty hearing in a specific scene and emotional state12. Therefore, the accuracy of the HHIE-S may be associated with various factors, such as sociodemographic information, lifestyle, physical and mental health status, otological symptoms in older people. During the process of hearing screening, it is meaningful to incorporate inquiries about medical history like tinnitus and screening for cognitive function.
In summary, various factors, such as lifestyle habits, tinnitus, and the physical and mental health of older people, can affect the accuracy of the HHIE-S. When using the HHIE-S to conduct hearing screening among the older people, even if the score is 8 or less, hearing loss may still occur. Factors such as living alone, smoking, cognitive decline, and anxiety should be given attention, and they can be incorporated into the screening process when necessary. Increasing the efficiency of using the HHIE-S can prevent adverse consequences caused by hearing loss in older adults.
With respect to study limitations, first, the cross-sectional analyses did not allow for causal or temporal relationships among the factors associated with the accuracy of the HHIE-S. In addition, considering the objectivity of the assessment, fewer factors were included in the study. In the future, multiple factors can be considered together. Finally, the current conclusions have not yet been validated in hearing screens, and we will update our findings subsequently.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- GAD-7:
-
Generalized Anxiety Disorder-7
- HHIE-S:
-
Hearing Handicap Inventory for the Elderly Screening version
- HL:
-
Hearing loss
- MoCA:
-
Montreal Cognitive Assessment
- NH:
-
Normal hearing
- OR:
-
Odds ratio
- PAF:
-
Population attributable fraction
- PHQ-9:
-
Patient Health Questionnaire-9
- PTA:
-
Pure tone average
- PTA0.5–4 kHz :
-
Pure tone average at 0.5, 1, 2 and 4 kHz of air-conducted
- SSQ12:
-
Speech, Spatial, and Qualities of Hearing Scale-12
- WHO:
-
World Health Organization
References
World Report on Hearing. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO. (2021).
Fu, X. et al. Association between hearing loss and gout based on National health and nutrition examination survey and Mendelian randomization analysis. Sci. Rep. 14 (1), 1–10 (2024).
Zheng, M. et al. Worsening hearing was associated with higher β-amyloid and Tau burden in age-related hearing loss. Sci. Rep. 12 (1), 1–7 (2022).
Assi, S. et al. The association of hearing loss with frailty among community-dwelling older adults: findings from the National health and aging trends study. BMC Geriatr. 23 (1), 1–10 (2023).
Livingston, G. et al. Dementia prevention, intervention, and care. Lancet 390 (10113), 2673–2734 (2017).
Livingston, G. et al. Dementia prevention, intervention, and care: 2024 report of the lancet standing commission. Lancet 404 (10452), 572–628 (2024).
Tsai Do, B. S. et al. Clinical practice guideline: Age-Related hearing loss. Otolaryngology–Head Neck Surg. 170 (S2), S1–S54 (2024).
Feltner, C. et al. Screening for hearing loss in older adults. Jama 325 (12), 1202–1215 (2021).
Ventry, I. M. et al. The hearing handicap inventory for the elderly: a new tool. Ear Hear. 3 (3), 128–134 (1982).
Purnami, N. et al. Score of hearing handicap inventory for the elderly (HHIE) compared to whisper test on presbycusis. Indian J. Otolaryngol. Head Neck Surg. 74 (Suppl 1), 311–315 (2022).
Tomioka, K. et al. The hearing handicap inventory for Elderly-Screening (HHIE-S) versus a single question: reliability, validity, and relations with quality of life measures in the elderly community, Japan. Qual. Life Res. 22 (5), 1151–1159 (2013).
Ferrán, S. et al. Early detection of hearing loss among the elderly. Life 14 (4), 1–15 (2024).
Gopinath, B. et al. Hearing and vision impairment and the 5-year incidence of falls in older adults. Age Ageing. 45 (3), 409–414 (2016).
Hearing screening: considerations for implementation. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO. (2021).
Wang, Y. et al. Analysing use of the Chinese HHIE-S for hearing screening of elderly in a Northeastern industrial area of China. Int. J. Audiol. 56 (4), 242–247 (2016).
Apa, E. et al. Italian validation of the hearing handicap inventory for Elderly - Screening version (HHIE-S-It). Acta Otorhinolaryngol. Ital. 43 (4), 262–272 (2023).
Diao, M. et al. Comparison between Self-Reported hearing and measured hearing thresholds of the elderly in China. Ear Hear. 35 (1), e228–e232 (2014).
Dillard, L. K. et al. Agreement between audiometric hearing loss and self-reported hearing difficulty on the revised hearing handicap inventory differs by demographic factors. J. Epidemiol. Community Health. 78 (8), 529–535 (2024).
Marengoni, A. et al. Aging with Multimorbidity: A systematic review of the literature. Ageing Res. Rev. 10 (4), 430–439 (2011).
Eikelboom, R. et al. Discrepancy between self-assessed hearing status and measured audiometric evaluation. PLoS One. 12 (8), e0182718 (2017).
Moore, B. C. J. et al. Guidelines for diagnosing and quantifying Noise-Induced hearing loss. Trends Hear. 26 (1), 1–21 (2022).
McEvoy, J. W. et al. 2024 ESC guidelines for the management of elevated blood pressure and hypertension. Eur. Heart J. 45 (38), 3912–4018 (2024).
American Diabetes Association Professional Practice Committee. 2. Diagnosis and classification of diabetes: standards of care in Diabetes—2024. Diabetes Care. 47 (Suppl. 1), S20–S42 (2024).
Krist, A. H. et al. Screening for hearing loss in older adults. Jama 325 (12), 1196–1201 (2021).
Reed, N. S. et al. Association of midlife hypertension with Late-Life hearing loss. Otolaryngology–Head Neck Surg. 161 (6), 996–1003 (2019).
Quadri, O. R. et al. Sensorineural hearing loss among hypertensives. West. Afr. J. Med. 38 (2), 125–130 (2021).
Hara, K. et al. Association between hypertension, dyslipidemia, and diabetes and prevalence of hearing impairment in Japan. Hypertens. Res. 43 (9), 963–968 (2020).
Smith, S. et al. Age-related hearing loss and provider-patient communication across primary and secondary care settings: a cross-sectional study. Age Ageing. 49 (5), 873–877 (2020).
Wang, D. M. et al. Smoking affects the association between cognitive impairment and P50 Inhibition defects in patients with chronic schizophrenia: A case-control study. Asian J. Psychiatry. 79 (1), 1–7 (2023).
Land, S. R. et al. Associations of daily versus nondaily smoking, tobacco-Related risk perception, and Cancer diagnosis among adults in the population assessment of tobacco and health (PATH) study. Nicotine Tob. Res. 24 (10), 1540–1547 (2022).
Sawyer, A. T. et al. Illness perception and high readmission health outcomes. Health Psychol. Open. 6 (1), 1–7 (2019).
Mykyta, L. Living alone and feelings of depression among adults age 18 and older. Natl. Health Stat. Rep. 199 (1), 1–6 (2024).
Saniasiaya, J. et al. Hearing loss and psychosocial outcomes: influences of social emotional aspects and personality. PLoS One. 19 (6), e0304428 (2024).
Riskind, J. H. et al. Influence of anxiety, depression and looming cognitive style on auditory looming perception. J. Anxiety Disord. 28 (1), 45–50 (2014).
Coebergh, J. F. et al. Auditory agnosia for environmental sounds in Alzheimer’s disease: not hearing and not listening?? J. Alzheimers Dis. 73 (4), 1407–1419 (2020).
Miller, A. A. et al. Self-reported hearing loss is associated with faster cognitive and functional decline but not diagnostic conversion in the ADNI cohort. Alzheimer’s Dement. 20 (11), 7847–7858 (2024).
Fabrizi, E. et al. The Italian guideline on diagnosis and treatment of dementia and mild cognitive impairment. Age Ageing. 53 (11), 1–26 (2024).
Oosterloo, B. C. et al. Prevalence of tinnitus in an aging population and its relation to age and hearing loss. Otolaryngology–Head Neck Surg. 164 (4), 859–868 (2020).
Epp, B. et al. Increased intensity discrimination thresholds in tinnitus subjects with a normal audiogram. J. Acoust. Soc. Am. 132 (3), EL196–EL201 (2012).
Musleh, A. et al. Psychological impact and quality of life in adults with tinnitus: A Cross-Sectional study. Cureus 16 (1), e51976 (2024).
Vasilkov, V. et al. Evidence of cochlear neural degeneration in normal-hearing subjects with tinnitus. Sci. Rep. 13 (1), 1–19 (2023).
Kovalova, M. et al. The importance of screening for hearing loss in the elderly. Otolaryngol. Pol. 76 (3), 32–38 (2021).
Funding
This project is funded by the National Key Research and Development Program (2020YFC2005200) and the Key Medical Development Program of Beijing Tongren Hospital (trzdyxzy201802).
Author information
Authors and Affiliations
Contributions
X Z, X F and Y Z proposed paper ideas, collected data, organized data, and wrote papers; J Z, Y C and B L developed assessment indicators, controlled the overall study, and reviewed papers.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study received ethical approval from Beijing Tongren Hospital, Capital Medical University (TREC2023-KY075).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, X., Fu, X., Zhang, Y. et al. Optimization of utilizing the HHIE-S for hearing screening in older people: a cross-sectional study of associated factors. Sci Rep 15, 18080 (2025). https://doi.org/10.1038/s41598-025-02567-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-02567-x