Abstract
To investigate the ramifications of dose alterations and clinical outcomes linked to imperfect uterine tandem implantation within high dose rate brachytherapy (HDR-brachytherapy) for cervical cancer. A retrospective analysis was conducted on imperfect intrauterine insertion images from November 2020 to July 2021. The physicist reconfigured two-dimensions (2D) and three-dimensions (3D) plans based on prescription (6 Gy) for both the imperfection (IM) and perfect (PER) implantation. A paired t-test was employed to assess (reference volume of clinical target volume) CTVref, (reference isodose) Vref, (conformal index) COIN, (equivalent dose in 2-Gy fractions) EQD2 of (organs at risks) OARs, (tumor control probability) TCP, and (normal tissue complication probability) NTCP. Among 1742 brachytherapy insertions, 38 (2.18%) instances of imperfect images were identified in 24 out of 319 patients (7.52%). COIN > 0.64 met the prescribed requirements solely in the PER-3D group. For inadequate implantation, the IM-3D-group showed enhancements in EQD2 of OARs and NTCP for the rectum, sigmoid colon, and small intestine, whereas NTCP of the bladder was augmented in the IM-2D-group. Regarding anterior wall perforation, the IM-group exhibited increases in EQD2 and NTCP for the rectum and small intestine, along with EQD2 for the bladder in 3D. In the IM-2D-group demonstrated increases in EQD2 for the bladder, rectum, and small intestine, as well as NTCP for the sigmoid and small intestine. In cases of posterior wall perforation, the IM-3D-group showcased augmented EQD2 for the bladder and rectum, and NTCP for the rectum and sigmoid. Conversely, EQD2 was solely increased in the rectum in the 2D context. Finally, in instances of fundus perforation, the IM-group exhibited heightened EQD2 for the sigmoid. Imperfect uterine tube implantation leads to worse clinical outcomes and greater adverse reactions.
Similar content being viewed by others
Introduction
Cervical cancer remains a significant global health issue, ranking as the fourth most common malignancy among women globally, with an estimated 604,127 new cases and 341,831 deaths each year1. Particularly in China, the disease burden exhibits striking severity. According to 2022 epidemiological projections, there were 111,820 new diagnoses and 61,579 mortalities—figures that represent nearly 20% of global cervical cancer fatalities2,3. The clinical management approach for non-operable primary cervical cancer has evolved to prioritize definitive radiotherapy, with brachytherapy emerging as the cornerstone modality, delivering 40–60% of the total radiation dose to the tumor targets4.
The unique dosimetric advantages of brachytherapy stem from its capacity to deliver high-intensity radiation through intracavitary or interstitial applicators, achieving rapid dose fall-off gradients that spare adjacent critical structures. This radiobiological superiority, however, is exquisitely dependent on geometric precision. As dose distribution follows the inverse square law, millimeter-level deviations in applicator positioning can precipitate disproportionate dose perturbations—a 2 mm displacement may escalate rectal dose exposure by 15–20%, while simultaneously creating cold spots in tumor regions5. Clinical correlations substantiate these dosimetric observations: comparative analyses reveal a 50% improvement in 5-year survival rates between cohorts with optimal versus suboptimal implant geometry (60% vs 40%)6, underscoring the life-altering consequences of implantation accuracy.
Despite these critical implications, the current academic discourse reveals notable gaps in knowledge. Existing research predominantly focuses on macro-level complications, such as uterine perforation, which has a reported incidence ranging from 4.5 to 17.9%7,8, while overlooking the systematic assessment of more subtle implantation inaccuracies. The literature lacks comprehensive analyses of: (1) dosimetric variance patterns associated with specific error types (e.g., cervical os displacement, uterine axis deviation, tandem depth discrepancy); (2) consequent alterations in TCP and normal NTCP; (3) differential impacts between 2D and 3D image-guided treatment planning approaches.
Our investigation addresses these deficiencies through a dual analytical approach. First, we establish a novel classification system for uterine tandem malpositioning based on spatial deviation vectors. Second, by employing Monte Carlo simulation and biological modeling, we quantify how post-correction replanning in both 2D and 3D paradigms modulates dosimetric parameters (D90, D2cc) and their corresponding clinical endpoints. This methodology not only provides unprecedented insights into the radioclinical consequences of implantation inaccuracies but also establishes an evidence base for precision brachytherapy protocols.
Material and methods
Patient selection and applicator insertion
Cervical cancer patients treated with intracavitary brachytherapy (ICBT) in our hospital from November 2020 to July 2021 were included in this study. All patients received pelvic external beam radiotherapy (EBRT) 45 Gy, according to the situation and a supplementary dose of 5–10 Gy to parametrial or 10–15 Gy to residual enlarged lymph nodes and HDR-BT 6 Gy × 5–6 F. During EBRT, single-agent cisplatin (40 mg/m2) was given weekly for 5–6 times. BT was performed after completion of EBRT, and the entire radiotherapy course was completed within 8 weeks. All patients underwent pelvic gynecological examination and pelvic Magnetic Resonance Imaging (MRI)/Computed Tomography (CT) imaging, both performed at the time of diagnosis and before brachytherapy. Segedin et al. identified several risk factors including " necrotic cervical tumor, cervical polyp, submucosal fibroid, stenosis, or distortions of the cervical canal (particularly due to prior conization), and a retroflexed or extremely anteflexed uterus," all of which are associated with a higher incidence of uterine perforation. However, in the article by M Parvath ES9 additional uterine pathology was not significantly associated with uterine perforation during brachytherapy. In this study, the anatomical location of the uterus before brachytherapy was classified into the following types, as delineated in the literature by Chakrabarti B7and illustrated in Fig. 1.
All patients were placed with CT compatible applicators under intravenous anesthesia (Fletcher-Suit style tandem-ovoid intracavitary applicators). A CT scan with a slice thickness of 3 mm was conducted using a Philips CT simulator (Philips Healthcare, Andover, MA), covering the range from the vulva to 5 cm above the uterus. The acquired CT scan images were subsequently transferred to the Oncentra Brachytherapy planning system (Version 4.6.0) for 3D treatment planning. At our institution, in the event of imperfect applicator implantation during brachytherapy, re-implantation would be undertaken by a different gynecologic oncologist. If immediate correction was not feasible, the re-implantation procedure was scheduled 72 h later, with all applicator implantation images retained. For this study, all saved image sets from the designated study phase were reviewed to identify and categorize types of intrauterine tube implantation imperfections.
Imperfection implantation was defined based on four conditions observed on CT scan (Fig. 2): (1) Anterior Wall Perforation: perforation of the uterine tube from the anterior ventral side of the uterine axis; (2) Posterior Wall Perforation: perforation of the uterine canal from the dorsal side of the uterine axis; (3) Inadequate Implantation: the uterine tube did not exceed the isthmus of the cervix or was in the uterine cavity and did not exceed 1 cm above the upper edge of the lesion or was more than 2 cm from the bottom of the uterine cavity; (4) Fundus Perforation: visual confirmation of the applicator tip extension beyond the uterine serosa on CT scan. The differences brought about by the various types of applicator implantation dissatisfaction in 2D and 3D plans were analyzed, and clinical records were maintained for each patient.
Intrauterine tube implantation imperfect classification was defined as four conditions on CT scan: (A) Anterior Wall Perforation: perforation of the uterine tube from the anterior ventral side of the uterine axis; (B) Posterior Wall Perforation: perforation of the uterine canal from the dorsal side of the uterine axis; (C) Inadequate Implantation: the uterine tube did not exceed the isthmus of the cervix or was in the uterine cavity and did not exceed 1 cm above the upper edge of the lesion or was more than 2 cm from the bottom of the uterine cavity; (D) Fundus Perforation: visual confirmation of the applicator tip extension beyond the uterine Serosa on CT scan.
Contouring and treatment planning
The perfect/imperfect positioning CT images were re-transmitted to the Oncentra Brachytherapy planning system (Version 4.6.0). Gynecologic oncologists delineated the high-risk clinical target volume (HR-CTV) and OARs based on gynecological physical examination, MRI/CT images at diagnosis and before BT. Target volume definition and reporting were adhered to Gynaecological (GYN) GEC-ESTRO recommendations, with mandatory contouring of organs at risk and dose-volume parameter reporting (e.g., the minimal dose to 90% of the clinical target volume [D90], the minimal dose to the most exposed 2 cm3 of the respective organ [D₂cc])10,11. The target volume and OARs were delineated according to IBS-GEC ESTRO-ABS recommendations12. HR-CTV encompassed all cervical and residual tumors, verified through gross examination, physical examination, imaging, and pathology, while OARs included the bladder, rectum, sigmoid colon and small intestine. The bladder was defined as the entire outer wall, with its lower boundary at the beginning of the urethra. The rectum encompassed the entire outer wall, with its lower boundary 1 cm above the anus and upper boundary at the rectosigmoid junction. The sigmoid colon was delineated from the level of flexion of the rectum and sigmoid colon to the level of disappearance of the corpus uteri. Small intestine included the intestinal canal and mesentery, with its lower boundary at the flexion level of the rectum and sigmoid colon, and upper boundary at the disappearance level of the uterine body.
Treatment employed a 192Ir source in Flexitron HDR brachytherapy set-up (Nucletron, an Elekta company, Stockholm, Sweden). Utilizing the Oncentra treatment planning system (Elekta AB, Stockholm, Sweden, version 4.6.0), both 2D and 3D brachytherapy plans were conducted on perfect/imperfect images of the intrauterine implantation, with a prescription dose of 6 Gy in a single fraction. The 2D plans aimed to compare normalization at point A, defined as the point located 2 cm lateral to the central canal of the uterus and 2 cm from the mucous membrane of the lateral fornix in the axis of the uterus. 3D plans were designed to deliver at least 100% of the prescribed dose to 90% volume CTV (HR-CTV D90), with optimization carried out to ensure CTV coverage and reduce dose to OARs as necessary. For patients, the EBRT and HDR-BT radiation doses need to meet specific dose constraints: HR-CTV D90 ≥ 85–90 Gy EQD2, rectum D2cc ≤ 65–75 Gy EQD2, sigmoid D2cc ≤ 70–75 Gy EQD2, and bladder D2cc ≤ 80–90 Gy EQD2, ensuring that two gray equivalent doses (EQD2) (α/β = 10) were delivered to the 100% isodose curve passing through this point. All 2D plans and imperfect 3D plans for intrauterine implantation were solely utilized for dose analysis in this study and were not implemented clinically. Only corrected 3D plans were implemented for the patients.
Parameters calculation
We use a COIN13 to evaluate implant quality and dose specification in brachytherapy.
In the formula, CTVref represents HR-CTV volume covered by the 100% prescription dose line, CTV represents the HR-CTV volume, and represents the total volume covered by the 100% prescription dose line. COIN is commonly utilized to quantify the degree of agreement between the prescribed dose line (plane) and the target volume in brachytherapy. An ideal COIN value = 1, with clinical treatment typically requiring COIN > 0.6413.
Regarding OARs, doses at volumes of 2 cc and 1 cc, and the maximum dose for all OARs (rectum, bladder, sigmoid, and intestines), were evaluated. Specifically, doses were assessed on a 2 cc volume to allow for direct comparison with dose tolerance thresholds outlined in the work of GYN-GECESTRO11. Both the physical dose and EQD2 of the OARs were calculated for D2cc using Eq. (2).
Based on the concept of equivalent uniform dose (EUD), Gay, H. A14 proposed the TCP / NTCP model Mathematical models of NTCP and TCP have been proposed for better optimization and evaluation of HDR BT plans. We used the published code of TCP / NTCP, which takes into account the total dose of radiation therapy (EBRT 45 Gy + BT 6 Gy × 5 fractions)15.
Vi is a unitless partial volume, Di is the dose received by the voxel volume at i, and the sum of all partial volumes Vi values equals to 1. atumor = − 10, abladder = 2, arectum = 8.33, aintestines = 6, asigmoid = 615. TCD50 is the irradiation dose received at a tumor control rate of 50%, γ50 = 3; TD50 is the dose tolerated by normal tissue at a complication rate of 50% for OARs (the bladder, rectum, sigmoid and intestines), γ50 = 416.
Statistical analysis
IBM® SPSS® Statistics software version 23 was used for data analysis. Paired sample t test was used to compare parameters generated with or without normalization for intrauterine tandem implantation, both imperfect and corrected perfect, across the two plans. A significance level of 0.05 was used, and p ≤ 0.05 was considered statistically significant. EQD2 calculations were performe using linear quadratic (LQ) spreadsheet available at American Brachytherapy Society’s http://www.americanbrachytherapy.org/guidelines/LQ_spreadsheet.xls website.
Ethics approval and consent to participate
This study was approved by the ethics committee of the Chongqing University Cancer Hospital Review Board (Approval ID:CZLS2023085-A). Informed consent was obtained from all participants and/or their legal guardians. All methods were carried out in accordance with relevant guidelines and regulations.
Results
In our study, among 319 patients undergoing brachytherapy (total 1742 insertions), imaging imperfections were observed in 24 cases (7.52% of patients), corresponding to 38 individual insertion events (2.18% of all procedures) in Table 1. The characteristics of the 24 patients included in the study analysis are shown in Table 2.
Anatomical location of uterus before brachytherapy
Among the 24 patients with imperfect uterine tube implantation, the retroverted uterus accounted for 45.83% (11/24), the acutely anteflexed uterus accounted for 37.5% (9/24), and the small uterus accounted for 16.67% (4/24). Additionally, there were five patients with obstructing cervical masses, none of whom had this condition in isolation: one patient had a retroverted uterus, three had an acutely anteflexed uterus, and one had a small uterus.
Radiotherapy parameters
In all patients with an imperfect uterine tube placement, there was good agreement in VOI (p > 0.05), and CTVref was less than VOI. CTVref was smaller in PER-3D group than in PER-2D group. The Vref in the PER-3D group exhibited the smallest magnitude, significantly differing from that in the PER-2D group (p < 0.05); COIN values exceeding 0.64 were exclusively observed in the PER-3D group, contrasting with values below this threshold in other groups. Particularly, the smallest COIN value was recorded in the imperfect 2D (IM-2D) group.
These findings indicate that only the PER-3D group meets the clinical requirements for COIN, achieving target coverage by encapsulating the smallest feasible volume, while the remaining groups attained target coverage by expanding the dose coverage range, as shown in Table 3.
Inadequately implanted
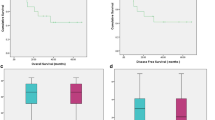
In 38 cases of imperfect intrauterine tube implantation, the proportion of inadequate intrauterine tube implantation was 31.58% (12/38), in Table 1. Inadequate intrauterine tandem implantation increased EQD2 of rectum, sigmoid and small intestine in 3D plans (p < 0.05); however, there was no statistically significant difference in EQD2 of OARs in 2D plans (p > 0.05). as depicted in Table 3A and Fig. 3A. In Table 4 we observed that inadequately implanted reduced TCP, which was more significant in the 2D plans; the NTCP of OARs in the IM-3D group was significantly higher than that in the PER-3D group, with the exception of the bladder (p < 0.05); additionally, the NTCP of the bladder in the IM-2D group was lower compared to the PER-2D group (p < 0.05).
Anterior wall perforation
Anterior uterine wall perforation accounted for 28.95% of the 38 cases of imperfect intrauterine implantation, in Table 1. When Anterior uterine wall perforation occurred, EQD2 in the rectum, small intestine, and bladder was significantly increased in 3D plans (p < 0.05). EQD2 was also significantly higher in the small intestine in the 2D plans (p < 0.05), while EQD2 of rectum and sigmoid colon in the 2D plans decreased, especially for sigmoid colon (p < 0.05), as shown in Table 3B and Fig. 3B. As depicted in Table 4, anterior wall perforation resulted in a reduction of TCP, with the impact being particularly pronounced in the 3D plan.
Posterior wall perforation
Posterior Wall Perforation occurred in 9 patients, accounting for 23.68% (9/38) of the 38 cases of imperfect intrauterine implantation, in Table 1. When posterior wall perforation occurred in the concatemat uteri, the EQD2 of OARs increased in both 2D and 3D plans, except for a reduction of EQD2 in bladder in the 2D plans,. Notably, significant increases in EQD2 were observed for both rectum and bladder in the 3D plans, and for rectum in the 2D plans (p < 0.05). For details, refer to Table 3C and Fig. 3C.
Fundus perforation
Fundusperforation was observed in 6 patients, constituting 15.79% (6/38) of the 38 cases of imperfect intrauterine implantation, as detailed in Table 1. Table 3D and Fig. 3D show that EQD2 of sigmoid colon was increased when axis perforation occurred (p < 0.05), and Table 4 shows that when axis perforation occurred, TCP of patients was decreased (p < 0.05) and NTCP of OARs was increased (p > 0.05).
Clinical outcomes
During the process of uterine tandem implantation, neither the patients nor the doctors reported any obvious perforation. The possibility of re-perforation was evaluated after perforation was detected via positioning CT scans, and experienced doctors were tasked with re-implanting the uterine tandem. There were no instances of bleeding or damage to surrounding organs during or within 2 h after the operation, and no symptoms of pelvic infection were reported within 1 week after operation.
At the three-month follow-up after treatment, one patient was lost to follow-up, while 18 patients exhibited local complete response and five showed partial response. At the two-year follow-up post-treatment, four patients were lost to follow-up, 18 patients remained in local complete remission, and one patient experienced recurrence and continuous progression.
Discussion
Brachytherapy stands as an indispensable modality for the radical radiotherapy of cervical cancer. The technical precision of brachytherapy implantation has been demonstrated to significantly influence treatment outcomes7,17,18,19. Sandun et al.20 emphasized the clinical significance of even minor shifts in intracavitary (IC) and combined intracavitary/interstitial (IC/IS) applicator positions in cervical cancer treatment. Uterine perforation represents the most studied applicator location in brachytherapy8,18,21,22. However, no prior study has classified uterine position before brachytherapy, categorized dissatisfaction with intrauterine implantation, and conducted dosimetric and clinical outcome predictions.
Literature review indicates that the incidence of uterine perforation following applicator placement assisted by CT scan ranges from 2.8 to 13.7%23,24,25. The rate of uterine perforation per insertion varies between 4.56 and 6.4%, while the rate per patient spans from 7.39 to 17.9%18,26. In our study, the rate of uterine perforation was 2.18% (38/1742) per insertion and 7.52% (24/319) per patient, both of which lower than previous reports. Currently, in addition to CT and MRI, ultrasound is used to guide applicator implantation. With intraoperative US guidance, the reported incidence of perforation was reduced to 0.9–1.4%27,28. It is recommended that ultrasound-guided intrauterine tube implantation should be selected according to the patient’s uterine position in order to reduce the incidence of uterine perforation. Real-time intraoperative ultrasound guidance may be useful to reduce uterine perforation rates and thus increase brachytherapy use. Ultrasound can assist in performing not only intracavitary brachytherapy but also interstitial brachytherapy29,30.
It’s likely that reported incidence rates underestimate the actual occurrence due to underreporting by surgeons. Otter S et al.31, highlighted older age, larger tumors, retroverted uterus, and stenotic cervical as predisposing factors for uterine perforation. Other studies identified factors such as age over 60 years24,32,33, history of prior conization21,32, physician inexperience7, scarring or distortion of the cervical34, and increasing tumor size as risk factors for uterine perforation. A novel scoring system for predicting the risk of uterine perforation: uterine position was included in the risk factors, with sensitivity of 46% and 66.7%, Specificity of 96% and 73% in the test and validation columns, respectively (P < 0.05). Additional uterine pathology was not a risk factor for uterine perforation9. Pre-planning by imaging is required before insertion to assess uterine cavity length, orientation, and position, as well as to determine the location of any residual cervical mass. This pre-planning reduces the likelihood of imperfect brachytherapy implantation7. The study by Onal et al. revealed that preoperative MRI planning reduced the incidence of perforation to 4% from 11% without pre-planning31. The pre-BT MRI image details were utilized for scoring the patients prior to BT9, of the patients in this study, 91.7% underwent MRI before BT treatment.
The anatomical positions of the cervix and uterus before brachytherapy were classified based on pre-planning images, and the types of uterine perforation were manually categorized. Onal C31 enrolled 200 patients and concluded that the most frequent perforation site was the posterior uterine wall (4%), followed by the fundus (2.5%) and anterior wall (2%). In our study of 319 patients, the most common cause of imperfect uterine tube insertion was inadequate uterine tube insertion, followed by anterior uterine perforation. The larger sample size in our cohort may provide more robust data compared to earlier studies.
In our study, different types of intrauterine tube implantation imperfections during brachytherapy were investigated. COIN was utilized to evaluate the degree of conformality in target area13. A COIN value above 0.64 meets clinical requirements and signifies optimal treatment quality. Analysis of radiobiological parameters across all groups revealed that only the PER-3D group achieved a COIN value > 0.64, meeting clinical requirements. These results indicate that 3D plan is the optimal choice for brachytherapy.
Suboptimal placement of the applicator can result in uterine perforation, inadequate dose to the target and excess dose to adjacent normal tissues. The dose variation caused by uterine perforation varies significantly depending on the perforation location. Optimal placement of the tandem and ovoids is essential for an acceptable brachytherapy plan35. Failure to perform a brachytherapy boost correlates with increased local failure risk in patients with cervix cancer, whereas tandem malposition does not correlate with increased risk. In Manon Kissel’s study18, even with suboptimal brachytherapy implantation, optimization prevented inadequate dose coverage or poorer local control. In cases with obstructive cervical mass, good subsequent insertion is possible with acceptable dose volume parameters, if planned dose can be delivered to its 60% volume. Indian institutional experience documented by Chakrabarti et al. revealed that analyzes dosimetric variations after imperfect brachytherapy insertions7. Insertion of adequate length of tandem aligned to uterine axis is warranted for adequate tumor coverage. In the Bikramjit study, anterior perforation resulted in a high bladder dose in 40% of cases and a high rectal dose in 20% cases7. When inserted in the retroverted direction in a retroverted uterus, the tandem generates acceptable dose-volume parameters. Acute anteflexion and mobile retroversion should be corrected whenever detected.
TCP and NTCP radiobiological parameters were used to predict tumor control probability and normal tissue complication probability. The advantage of NTCP and TCP radiobiology lies in their ability to predict and evaluate the ultimate therapeutic effect of a specific treatment regimen, with prediction conclusions aligning closely with clinical observations22,36. When intrauterine tube implantation was imperfect, the varying positions of the uterine tube had distinct dose effects on OARs across different plans, resulting in reduced TCP and increased NTCP for different OARs (see Tables 3, 4). In conclusion, regardless of the site of intrauterine canal implantation imperfection, EQD2 and NTCP of OARs were increased to varying degrees, while TCP was decreased. This underscores the impact of brachytherapy implant quality on patients’ disease-free survival, aligning with conclusions from prior studies17.
One investigation demonstrated that patients diagnosed with cervical cancer at Stages III/IV experienced a reduction of approximately 1% in local tumor control per day of treatment delay beyond 30 days. Moreover, Petereit et al. observed a notable decline in 5-year survival rate from 65 to 54%, when treatment duration exceeded 55 days37,38. A recent study echoed these findings, reporting a 3-year local tumor control rate of over 94% when total radiation therapy was administered within a 7-week timeframe39. Due to the rapid doubling time of cancer cells, current evidence strongly advocates against treatment interruptions during standard therapy protocols. This underscores the critical need to address delays caused by uterine perforation during brachytherapy, as such events may compromise treatment efficacy and survival outcomes. In our study, all cases of uterine perforation were promptly corrected without clinically significant complications. Similar findings have been reported in other studies, where patients completed treatment without significant delay or further complications after correct reinsertion of the tandem21,32,34. Thus, immediate evaluation for possible reinsertion should be pursued upon identifying uterine perforation. Our study demonstrates that prompt correction of applicator placement is feasible and safe in cases of uterine perforation, allowing patients to proceed with brachytherapy without undue delay, thus potentially optimizing treatment efficacy and patient outcomes8.
Conclusions
Compared to the IMP group and the PER-2D group, the PER-3D group demonstrated clinical superiority in cervical cancer brachytherapy with a COIN value exceeding 0.64. When suboptimal placement of the uterine canal occurs, the resulting dose to organs at risk (OARs) fails to meet clinical standards, and the rise in NTCP (Normal Tissue Complication Probability) comes at the expense of a decreased TCP (Tumor Control Probability). Immediate correction of the uterine canal position is strongly recommended to avoid damage to other organs. For patients with abnormal cervix and uterine body positions, ultrasound-guided uterine tube placement is advised to enhance accuracy. Most importantly, the incidence of uterine perforation is significantly lower in patients undergoing image-guided intracavitary insertion for cervical cancer.
Data availability
The datasets used and analysed from the current study are available from the corresponding author on reasonable request.
References
Singh, D. et al. Global estimates of incidence and mortality of cervical cancer in 2020: A baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob. Health 11(2), e197–e206 (2023).
Qi, J. et al. National and subnational trends in cancer burden in China, 2005–20: An analysis of national mortality surveillance data. Lancet Public Health 8(12), e943–e955 (2023).
Zheng, R. S. et al. Cancer incidence and mortality in China, 2022. Zhonghua Zhong Liu Za Zhi 46(3), 221–231 (2024).
Viswanathan, A. N. et al. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part II: High-dose-rate brachytherapy. Brachytherapy 11(1), 47–52 (2012).
Tanderup, K. et al. Consequences of random and systematic reconstruction uncertainties in 3D image based brachytherapy in cervical cancer. Radiother. Oncol. 89(2), 156–163 (2008).
Pötter, R. et al. MRI-guided adaptive brachytherapy in locally advanced cervical cancer (EMBRACE-I): A multicentre prospective cohort study. Lancet Oncol. 22(4), 538–547 (2021).
Chakrabarti, B. et al. Clinical and dosimetric consequences of imperfect applicator insertion in cervical cancer brachytherapy. J. Contemp. Brachyther. 10(4), 321–336 (2018).
Small, W. Jr. et al. Uterine perforation during brachytherapy for cervical cancer: Complications, outcomes, and best practices for forward treatment planning and management. Brachytherapy 20(3), 557–564 (2021).
ES, M.P., et al. Development and validation of a novel scoring system to predict the risk of uterine perforation during intracavitary brachytherapy for cervical cancer. J. Gynecol. Oncol. 35(3), e35 (2024).
Haie-Meder, C. et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): Concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother. Oncol. 74(3), 235–245 (2005).
Pötter, R. et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): Concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother. Oncol. 78(1), 67–77 (2006).
Mahantshetty, U. et al. IBS-GEC ESTRO-ABS recommendations for CT based contouring in image guided adaptive brachytherapy for cervical cancer. Radiother. Oncol. 160, 273–284 (2021).
Baltas, D. et al. A conformal index (COIN) to evaluate implant quality and dose specification in brachytherapy. Int. J. Radiat. Oncol. Biol. Phys. 40(2), 515–524 (1998).
Gay, H. A. & Niemierko, A. A free program for calculating EUD-based NTCP and TCP in external beam radiotherapy. Phys. Med. 23(3–4), 115–125 (2007).
Wen, A. et al. Radiobiological and dosimetric comparison of 60Co versus 192Ir high-dose-rate intracavitary-interstitial brachytherapy for cervical cancer. Radiat. Oncol. 17(1), 206 (2022).
Sukhikh, E. S. et al. Dosimetric and radiobiological comparison of simultaneous integrated boost and sequential boost of locally advanced cervical cancer. Phys. Med. 73, 83–88 (2020).
Viswanathan, A. N. et al. The quality of cervical cancer brachytherapy implantation and the impact on local recurrence and disease-free survival in radiation therapy oncology group prospective trials 0116 and 0128. Int. J. Gynecol. Cancer 22(1), 123–131 (2012).
Kissel, M. et al. Impact of suboptimal tandem implantation on local control and complications in intracavitary brachytherapy for cervix cancer. Brachytherapy 18(6), 753–762 (2019).
Wu, A. et al. Comparison of the dosimetric influence of applicator displacement on 2D and 3D brachytherapy for cervical cancer treatment. Technol. Cancer Res. Treat. 20, 15330338211041200 (2021).
Jayarathna, S. et al. Dosimetric impact of applicator displacement on three-dimensional image-guided high-dose-rate brachytherapy treatments for cervical cancer. J. Contemp. Brachyther. 15(5), 334–343 (2023).
Verma, M. et al. An audit of uterine perforation and its effect on the final outcome in an academic research medical center: An optimized balance between overall treatment time and medical crisis. J. Contemp. Brachyther. 15(2), 130–133 (2023).
Kaur, G. et al. Dosimetric and radiobiological evaluation of treatment plan for cervical cancer high-dose-rate intracavitary brachytherapy. J. Contemp. Brachyther. 14(3), 253–259 (2022).
Irvin, W. et al. Uterine perforation at the time of brachytherapy for carcinoma of the cervix. Gynecol. Oncol. 90(1), 113–122 (2003).
Barnes, E. A. et al. Prospective comparison of clinical and computed tomography assessment in detecting uterine perforation with intracavitary brachytherapy for carcinoma of the cervix. Int. J. Gynecol. Cancer 17(4), 821–826 (2007).
Patel, F. D. et al. Optimization of high-dose-rate intracavitary brachytherapy schedule in the treatment of carcinoma of the cervix. Brachytherapy 10(2), 147–153 (2011).
Sapienza, L. G. et al. Decrease in uterine perforations with ultrasound image-guided applicator insertion in intracavitary brachytherapy for cervical cancer: A systematic review and meta-analysis. Gynecol. Oncol. 151(3), 573–578 (2018).
Akbas, T. et al. Intraoperative sonographic guidance for intracavitary brachytherapy of cervical cancer. J. Clin. Ultrasound 46(1), 8–13 (2018).
Schaner, P. E. et al. Intraoperative ultrasound guidance during intracavitary brachytherapy applicator placement in cervical cancer: The University of Alabama at Birmingham experience. Int. J. Gynecol. Cancer 23(3), 559–566 (2013).
Pareek, V. et al. A phase III randomised trial of trans-abdominal ultrasound in improving application quality and dosimetry of intra-cavitary brachytherapy in locally advanced cervical cancer. Gynecol. Oncol. 160(2), 375–378 (2021).
Addley, S. et al. Combined direct hysteroscopic and real-time ultrasound guidance facilitating safe insertion of intra-uterine brachytherapy applicator for locally advanced cervical cancer with significant endocervical stenosis: A novel collaborative approach. Gynecol. Oncol. Rep. 47, 101178 (2023).
Onal, C. et al. Uterine perforation during 3-dimensional image-guided brachytherapy in patients with cervical cancer: Baskent University experience. Int. J. Gynecol. Cancer 24(2), 346–351 (2014).
Jhingran, A. & Eifel, P. J. Perioperative and postoperative complications of intracavitary radiation for FIGO stage I–III carcinoma of the cervix. Int. J. Radiat. Oncol. Biol. Phys. 46(5), 1177–1183 (2000).
Rangarajan, R. Incidence of suboptimal applicator placement and the resulting dosimetric impact in image-based intracavitary brachytherapy. J. Med. Phys. 43(3), 168–172 (2018).
Bahadur, Y. A. et al. Uterine perforation and its dosimetric implications in cervical cancer high-dose-rate brachytherapy. J. Contemp. Brachytherapy 7(1), 41–47 (2015).
Otter, S. et al. Improving the efficiency of image guided brachytherapy in cervical cancer. J. Contemp. Brachytherapy 8(6), 557–565 (2016).
Singh, G., et al. Dosimetric analysis of cervical cancer stage IIB patients treated with volumetric modulated arc therapy using plan uncertainty parameters module of Varian Eclipse treatment planning system. Biomed. Phys. Eng. Express. 7(3) (2021).
Chen, S. W. et al. The adverse effect of treatment prolongation in cervical cancer by high-dose-rate intracavitary brachytherapy. Radiother. Oncol. 67(1), 69–76 (2003).
Gillen, J. M. et al. Association of financial assistance programs and time to completion of therapy in women receiving chemoradiation for cervical cancer. Gynecol. Oncol. Rep. 34, 100660 (2020).
Tanderup, K. et al. Effect of tumor dose, volume and overall treatment time on local control after radiochemotherapy including MRI guided brachytherapy of locally advanced cervical cancer. Radiother. Oncol. 120(3), 441–446 (2016).
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Chongqing Technology Innovation and Application Development Special Project-Key project (No. CSTB2022TIAD-KPX0152), Chongqing Innovative Medical Device Application Demonstration Project (No. CQEIC2024MDAD-057), and Scientific and Technological Research Program of Chongqing Municipal Education Commission (No. KJQN202300132).
Author information
Authors and Affiliations
Contributions
Xiujuan Zhao reviewed the literature, target delineation, data collection, wrote the manuscript, critical analysis, drafting/final editing; Haiyan wu mainly carried out planning and design, data collection, critical analysis, drafting/final editing; Ruotong yi mainly translated and polished the article; Duke Chen contributed to writing, made statistical analysis; Ying Tang critically reviewed the manuscript conten. Dongling Zou and Qi Zhou critically reviewed the manuscript content; all other authors provided supporting funds for the study. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, X., Wu, H., Yi, R. et al. Dosimetric and clinical outcomes study of occult uterine tandem imperfect implantation in HDR-brachytherapy for cervical cancer. Sci Rep 15, 24681 (2025). https://doi.org/10.1038/s41598-025-02779-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02779-1