Abstract
It remains unclear whether there is an independent association of paternal age with implantation failure (IF) in couples undergoing Assisted Reproductive Technology (ART) treatment. Little is known about the interactive effects of paternal age with maternal age, paternal smoking and alcohol consumption on IF. The Anhui Maternal-Child Health Cohort Study (AMCHS) interviewed 1910 infertile couples (paternal age ranged 22–57 years) to look for risk factors associated with IF. Implantation outcome was assessed using serum β-HCG between 0 and 25 IU/L 14 days post-embryo transfer. Odds ratios (ORs) for IF in relation to paternal age, and its interactions with maternal age, paternal smoking and alcohol consumption were evaluated using logistic regression models. The risk of IF (n = 735) increased with paternal age ≥ 35, while it remained similarly lower among males aged 22–34. After adjusting for socioeconomic status, paternal lifestyles and semen factors, the OR for IF was 1.50 (95%CI 1.16–1.93) at paternal age of 35-<40 years, 2.06 (1.34–3.16) at 40-<45 years and 3.80 (2.50–7.07) at ≥ 45 years in comparison to those aged < 35. With additional adjustments for maternal age and maternal factors including anovulation and antral follicle counting, the corresponding ORs were 1.19 (0.89–1.60), 1.31 (0.79–2.16) and 2.13 (1.06–4.29). The association remained significant in those with maternal age > 30, paternal smoking or alcohol consumption, but not in their counterparts, respectively. Among those with a paternal age ≥ 35, each additional year of smoking was associated with a 7.0% increased risk of IF (OR = 1.07, 95% CI: 1.01–1.14); however, no such association was observed in younger paternal age groups. Significant interaction effects were observed between advanced paternal age and maternal age, as well as paternal alcohol consumption. The AMCHS had demonstrated that paternal age ≥ 35 years elevates the risk of IF, with additional impacts from advanced maternal age and paternal alcohol consumption. The findings of the AMCHS highlight the need to consider paternal and maternal ages in fertility planning and suggest that IF can be reduced by stopping paternal smoking and alcohol consumption.
Similar content being viewed by others
Introduction
Infertility affects more than 14% of couples worldwide, with male factors accounting for approximately 30% of cases. As infertility rates rise, the demand for Assisted Reproductive Technology (ART) has been increasing1,2. However, the chance of conception per cycle remains relatively low and about 35% of euploid embryos suffer implantation failure (IF)3 which refers to the inability of a zona-free blastocyst to attach and subsequently penetrate the uterine lining4.
While advanced maternal age is a well-documented risk factor for IF5,6, the influence of paternal age on the outcome of ART remains unclear. Some studies7,8 have shown an inverse association between paternal age and IF, but others have not9,10. The reason for these inconsistent results remains unknown. They might stem from varied adjustments undertaken during data analysis or a specific paternal age threshold associated with increased risk of IF. Furthermore, although a significant positive correlation between paternal and maternal ages exists11, few studies have assessed to what extent maternal age interacts with and explains the association between advanced paternal age and risk of IF. In Japan, Kidera et al.12 showed that advanced paternal age decreased the normal fertilization rate when the maternal age was 35–39 and increased the miscarriage rate when maternal age was < 35 years, suggesting advanced parental age may jointly increase the risk of IF. The potential mediating role of maternal age in the relationship between advanced paternal age and IF remains to be quantified.
Previous studies have suggested associations of paternal smoking and alcohol consumption with an increased risk of IF13,14,15,16. However, the interaction between advanced paternal age, smoking and alcohol consumption on the increased of IF is unclear. It has been hypothesised that advanced paternal age, smoking and alcohol consumption could jointly increase oxidative stress and DNA damage in sperm15. In this paper, we carried out a prospective cohort study of women undergoing their first frozen embryo transfer (FET) in China17. The study aimed to elucidate if there was an independent association between paternal age and IF. Additionally, we assessed the interaction effects of paternal age with maternal age, paternal smoking, and alcohol consumption on the risk of IF.
Methods
Study population and data collection
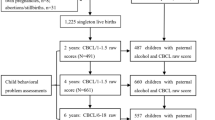
In 2017, the Anhui Maternal-Child Health Cohort Study (AMCHS) was set up in Anhui China, to investigate the ART outcomes and their influencing factors. The AMCHS methods have been fully described in our previous paper17. In brief, the AMCHS enrolled 2,198 infertile couples consecutively, undergoing FET for the first time treatment with autologous gametes from May 2017 to April 2021 at a large university-affiliated infertility center in China. In this study, the focus was FET, therefore couples having preimplantation genetic diagnosis technology (PGT) and fresh embryo transfers were not included. Informed consent was obtained from each participant. The primary interview instrument was a comprehensive questionnaire addressing general health and risk factors, details of which have been previously published17.
This study was approved by the Ethics Committee of Anhui Medical University (No. 20160270) and complied with the Helsinki Declaration.
Ovarian stimulation protocol, embryo quality assessment and frozen embryo transfer protocol
Controlled ovarian stimulation was achieved using a standard long pituitary downregulation in the luteal phase or a short protocol with an antagonist to treat infertility. In the AMCHS, ejaculated spermatozoa were used. Semen was separated through pure sperm density gradient or swim-up sperm preparation. All semen samples were analysed according to the World Health Organization criteria18. Either standard IVF or Intracytoplasmic Sperm Injection (ICSI) was employed to fertilize oocytes in the fertilization medium. A good-quality blastocyst was defined as B3–B4 or B5 embryo ≥ BB based on the Gardner standard19. Two or fewer embryos were transferred depending on their quality on day 5 or 6 after oocyte retrieval in compliance with national regulations. All participants had a serum hCG level done on day 14 after embryos transfer and an ultrasound scan examination was undertaken on thirty days after embryos transfer to confirm the presence of a fetal sac.
Outcome measurement
Implantation failure was defined as, a serum β-HCG (Beckman Coulter Inc., Fullerton, CA, USA) below 25 IU/L on 14 days post-embryo transfer and the absence of a fetal sac at the ultrasound examination.
Statistics analysis
The analysis included data from 1,910 couples after excluding those with missing paternal age (n = 6), withdrawals (n = 78), blastocyst cultivation failures (n = 28), low responses to controlled ovarian hyperstimulation (n = 19), natural pregnancies occurring mid-treatment (n = 5), and unavailable outcome data (n = 152). Their characteristics were described using means ± SD for continuous variables and numbers and % for categorical variables. Differences between the two groups, implantation success and implantation failure, were examined using t-tests for continuous variables and Chi-square tests for categorical variables. Binary logistic regression models were employed to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for the implantation failure in relation to paternal age. Using logistic regression analysis, we adjusted for different sets of confounders to examine the effect sizes of different factors from the paternal and maternal sides, on the association of advanced paternal age with IF. In model 1, we adjusted for socioeconomic status (residential location and family income), paternal smoking habits and alcohol consumption. In model 2, we further adjusted for paternal mental status (depression and anxiety), histories of any serious illness, and semen volume and morphology. In model 3, maternal age was additionally adjusted to examine how great the residual effect of maternal age could have on the association of advanced paternal age with IF. Finally, in model 4, we included other factors from females as adjustments, including female lifestyles, body mass index (BMI), mental status, infertility type, infertility duration, ovulation disorder and antral follicle count.
In addition, we investigated the interaction effects of paternal age with maternal age, paternal smoking and alcohol consumption respectively, using the terms of advanced paternal age, advanced maternal age, smoking, or alcohol consumption in the multiple adjusted regression models. We also stratified the data analysis by advanced maternal age (or paternal smoking and alcohol consumption, respectively) to examine the differences in the association of advanced paternal age with IF (additive effect) between two groups using the methods in our previous studies20. All analyses were performed using SPSS version 29.0 (IBM Co., Armonk, NY, USA).
Results
Table 1 shows the characteristics of male participants. Of the 1910 male participants, their average age was 32.3 years (SD 5.1), with a range of 22–57 years. 40.3% had an educational level of ≥ university, 51.9% were current- or former- smokers and 71.3% consumed alcohol in different amounts. Compared to those with implantation success, men who had implantation failure were more likely to be older and living in urban areas (Table 1). There were no significant differences between the two groups for implantation success and failure in the other characteristics (Table 1). However, the data of their spouses showed that women with implantation failure were more likely to be older, suffer from anxiety, have secondary infertility, higher oestradiol levels, < 10 antral follicles count and were less likely to be anovulatory (data on request). As expected there was a significant correlation between paternal age and maternal age (r = 0.789, p < 0.001).
Table 2 displays the number, rate and crude odds ratio of implantation failure in paternal age groups. There were significant differences in implantation failure rate across six paternal age groups at 22-<25, 25-<30, 30-<35, 35-<40, 40-<45, and ≥ 45–57 years (p < 0.001), and the implantation failure increased with paternal age (trend p < 0.001). Taking the largest number of participants in the paternal age group of 30-<35 years as a reference group for analysis, we found that crude ORs of implantation failure in the age groups of 22-<25 and 25-<30 years were not significantly different from that the age group of 30-<35 years, but increased in the age groups of 35-<40 years (1.56, 95%CI 1.20–2.04), in 40-<45 years (2.07, 1.35–3.18) and in ≥ 45–57 years (4.07, 2.21–7.50) (Table 2).
Table 3 shows the adjusted odds ratio and 95%CIs of implantation failure in relation to advanced paternal age using different sets of adjustments for analysis. As there were no significant differences in the risk of IF among the age groups of 22-<25, 25-<30 and 30-<35 in all model analyses, we combined these groups into one group as a reference for analysis. Adjusting for urban-rurality living, annual family income, paternal smoking and alcohol consumption (Model 1), ORs of implantation failure in the age groups of 35-<40, 40-<45 and 45–57 compared to all in 22-<35 years were 1.53 (1.19–1.96), 2.04 (1.34–3.11) and 4.00 (2.17–7.38) respectively. Further adjustments for paternal depression, anxiety, history of any serious diseases, semen volume and morphology showed similar ORs to those in Model 1, except for reduction in the OR in the age group of 45–57 years older (adjusted OR 3.80, 2.50–7.07). Adding maternal age to the adjustment analysis (Model 3) made further reductions in the ORs in the age groups of 35-<40, 40-<45 and 45–57 years compared to those in Model 2; the corresponding ORs were 1.18 (0.89–1.57), 1.32 (0.81–2.16) and 2.24 (1.13–4.60) respectively, but the increased OR in the age group of 45–57 years remained significant. Additional adjustments for other factors from females (Model 4) showed similar ORs to those in Model 3.
Separate data analysis by maternal age of 20-<30 years and ≥ 30 years (which was around a median of maternal age at 30.2 years in this study population of ART couples) showed a significant association of advanced paternal age with implantation failure in women aged ≥ 30 years, but not in younger maternal age groups. There were significant differences in the OR between the two groups (Table 4). Interaction effect analysis in the fully adjusted logistic regression model, also showed a significant interaction of advanced paternal age with maternal age on IF (Model 4 multiple adjusted OR 1.67, 95%CI 1.30–2.13, p = < 0.001, with paternal age ≥ 35 and maternal age ≥ 30). We further examined the risk of IF among men aged ≥ 35 years versus those aged 22-<35 years in each of three groups of maternal ages 20-<30, 30-<35 and 35–47 years, respectively (suppl Table 1). In the maternal age groups of both 30-<35 and 35–47 years, the increased risk of IF in men aged ≥ 35 years was significant, but not significant for the maternal age group of 20-<30, which further supported the interaction effect of advanced paternal age and maternal age on IF.
Separate data analysis by smoking status revealed that there was a significant association of advanced paternal age with implantation failure in men who smoked, but not in those who never-smoked (Table 5). The differences in the OR between these two groups approached conventional statistical significance (ROR 1.51, p = 0.084) (Table 5). In the multiple adjusted logistic regression model analysis, the interaction effect of advanced paternal age with smoking on IF was not significant (fully adjusted OR 1.19, 95%CI 0.82–1.73, p = 0.371, at paternal age ≥ 35 and smoking, data not shown in the tables). The three groups of paternal ages < 30, 30-<35 and ≥ 35 years showed borderline significant differences in the OR of implantation failure between the two groups, smoking and never-smoking, in the paternal age group ≥ 35 years (ROR 1.75, p = 0.071), following a non-significant increased ROR at the paternal age of 30-<35 years (1.17, p = 0.277). In addition, the duration of smoking cessation (in months) and total years of smoking were further analysed in Model 4 to examine their associations with IF risk. In the group of paternal age ≥ 35 years, each additional year of smoking was associated with 7.0% increased odds of IF (OR = 1.07, 95% CI: 1.01–1.14), whereas no association was observed in the younger paternal age group (OR = 0.99, 95% CI: 0.96–1.03). The difference in ORs between these two age groups was significant (ROR = 1.08, p = 0.014). However, the duration of smoking cessation (in months) was not significantly associated with IF in either age group, probably due to the smaller number of former smokers in the current AMCHS dataset, which could not provide enough study power in analysis for this.
Separate data analysis examining alcohol consumption found a significant association of advanced paternal age with implantation failure among men who consumed alcohol consumption regularly, but no such association was observed in those who did not consume alcohol. There were significant differences in the association between the two groups of consuming alcohol and not consuming alcohol (Table 6). Interaction effect analysis in the multiple adjusted regression model also showed a highly significant interaction of advanced paternal age with alcohol consumption on IF (fully adjusted OR 10.71, 95%CI 2.92–39.34, p = < 0.001, in the paternal age ≥ 35 with alcohol consumption, data not shown in the table).
Discussion
Our cohort study examined (1) the association between paternal age and implantation failure; (2) the interaction effects of advanced paternal age with maternal age, paternal smoking and alcohol consumption on implantation failure. We found that the risk of IF started to increase with a paternal age ≥ 35 years and there appears to be a dose-responsive relationship, while at the paternal ages of 22–34 there was no significant increase in IF. The association of advanced paternal age (≥ 45 years) with IF was independent of other factors but was moderated by advanced maternal age reducing the association. It was significantly pronounced at a maternal age above 30 years. Our study also demonstrated that while advanced paternal age was correlated with a heightened risk of IF among male smokers, this pattern did not extend to never-smokers. There was also a strong interactive effect between advanced paternal age and alcohol consumption on the risk of IF.
Previous studies showed inconsistent findings in the association between advanced paternal age and IF. For instance, Kaarouch et al.22 recruited 83 couples with female partners aged ≤ 39 undergoing IVF treatment in France and found no significant differences in IF between younger (< 40 years) and older (≥ 40 years) paternal age groups. The findings of their study were limited by the small sample size and lack of adjustment for additional factors. In the USA, conducting a retrospective cohort study of 2063 couples at a single academic reproductive medicine centre from 2012 to 2018, Kasman et al. (2021)10 also reported no significant effect of advanced paternal age on IF. In contrast, other studies showed significant association of advanced paternal age with IF. de La Rochebrochard et al. (2006)7 extracted data from 59 centres in the French National IVF Registry to examine 1938 couples with bilateral tubal obstruction and found that the adjusted odds ratio of failure to conceive was 1.52 (95% CI 1.08–2.14) at a paternal age 30–34 years, 1.32 (0.92–1.89) at 35–39 years, and 1.70 (1.14–2.52) at paternal age ≥ 40 years versus < 30 years. Coban et al. (2022) conducted a retrospective cohort study including 4930 fresh oocyte donation cycles from 3995 couples who had fresh embryo transfers at British Cyprus IVF Hospital from April 2005 to February 2020 and found that pregnancy rates (as defined by β-HCG) were significantly different among the paternal age groups of ≤ 29 years old (81%), 30–34 (71.8%), 35–39 (68.3%), 40–44 (71%), 45–49 (60.7%) and ≥ 50 (61.4%)23 These conflicting findings possibly stem from inadequate adjustment analysis for confounding factors in some studies24, particularly the absence of adjustment for maternal age and lifestyle factors (such as paternal smoking and alcohol consumption)21,22,25. Omitting maternal age from analyses exploring the impact of paternal age on ART outcomes, leads to analytical problems due to the high correlation between paternal and maternal ages, raising concerns about collinearity. In our analysis, maternal age was considered after adjustment for all paternal factors (Model 3) to determine the extent to which maternal age mediated the association between paternal age and IF. Even after including maternal age in our adjustments, the positive association of paternal age with IF persisted, albeit with reduced magnitude. Our study’s comprehensive adjustments for confounding variables, including maternal mental health, infertility specifics and biological aspects of both males and females, established a significant positive relationship between paternal age and IF.
Previous studies in western countries showed that paternal age of around ≥ 40 years would significantly increase the risk of IF in ART settings. Our AMCHS study found that advanced paternal age could be associated with increased IF from ≥ 35 years, which was younger than those in western countries7,26,27,28, potentially indicating population-specific cut-offs that may differ due to racial or environmental factors. The significant interaction effect between paternal and maternal ages on IF could be attributed to a compromised oocyte repair capacity. During embryogenesis, oocytes can repair sperm-derived DNA damage. However, advanced paternal age increases the extent of such damage, which may not be fully compensated for when maternal age exceeds 3029. The evidence from our study underscores the importance of considering paternal age in family planning. Future research should aim to unravel the mechanisms underlying paternal and maternal age thresholds, which may vary by race and environmental exposure. There is established evidence that paternal smoking increases the risk of implantation failure14,30 Tobacco smoke constituents directly interact with spermatozoa, potentially leading to DNA damage, which in turn may precipitate implantation failure31,32. Our AMCHS corroborates this by demonstrating a significant elevation in the risk of IF associated with advanced paternal age in individuals who were current and former smokers, compared to never-smokers. This suggests that paternal smoking may exacerbate the adverse effect of advancing paternal age on IF among couples undergoing ART treatments. Moreover, our data demonstrated a possible cumulative effect of tobacco exposure in the advanced paternal age group. It is possible that prolonged smoking with advanced paternal age could compound sperm DNA damage and oxidative stress over time33. More studies are needed to elucidate the different impacts of smoking on sperm quality in paternal age < 35 and ≥ 35 years, considering both genetic and epigenetic factors.
Rossi et al. suggested that paternal alcohol consumption increases the risk of IF (OR 1.36, 95%CI 1.04–1.78)34. Our research identified a substantial interaction between advanced paternal age and paternal alcohol consumption on IF. This is in line with previous studies34,35 indicating the detrimental effects of excessive alcohol consumption on semen quality and its consequent association with implantation failure. For example, conducting a prospective cohort study of 965 male patients Borges et al.36 found that alcohol consumption significantly influenced sperm count/ml (B: −12.527, slope: 42.255, p = 0.040) and sperm DNA fragmentation (B: 5.833, slope: 9.680, p = 0.002), which may lead to IF32. Therefore, it was not surprising that we observed the interactive effect between advanced paternal age and alcohol consumption on IF. The additive effect observed in our study, where advanced paternal age significantly intensified the risk of IF among regular alcohol consumers, but not among abstainers, underscores the importance of avoiding alcohol for men aged ≥ 35 years in ART settings to enhance implantation success. It is imperative that paternal smoking and alcohol consumption are considered critical covariates when evaluating the impact of advanced paternal age on male infertility and ART outcomes.
Strengths and limitations of the study
The main contribution of this study, beyond the intrinsic importance of studying the impact of advanced paternal age on IF, lies in what it tells us about the paternal age cut-off point increasing the risk of IF with a maternal age contribution, factors influencing this association and its interactive effects with maternal age, paternal smoking and alcohol consumption. As far as we know, our study is the first to report differences in the impact of advanced paternal age on IF between smokers and never-smokers, and between men who consumed alcohol and those who did not, addressing that men with adverse lifestyles had a greater risk of IF and worsening the impact of advanced paternal age on IF. Our study included important co-variables for adjustment such as female age, reasons for infertility, male sperm quality and couples’ socioeconomic status, thus the confounding effect is minimised. Different sets of confounding adjustments would allow us to identify factors influencing the association. Furthermore, in our study infertile couples were consecutively recruited and a completed baseline questionnaire before the first FET to avoid selection bias. The study has limitations. First, all participants in the cohort were from the areas of Hefei, Anhui, China, and caution should be exercised when generalizing the findings to all infertile couples across the whole of China who received ART treatment. Second, the number of participants in the current cohort study was not large so that when we examined the interactive effects of paternal age with maternal age, paternal smoking and alcohol consumption, the 95%CIs were wide. In the future, large cohort studies are required to examine the interactions between different paternal age levels and these confounding factors.
Conclusion
In the context of ART in China, our study discovered that paternal age ≥ 35 years is correlated with an augmented risk of IF. Notably, this risk is compounded when both partners are of advanced age. Paternal smoking and alcohol consumption exacerbate the risk of IF alongside advancing paternal age. These findings underscore the necessity of emphasizing the implications of delayed childbearing in public health communications, as such delays significantly contribute to heightened IF risks among ART patients. Smoking cessation and the avoidance of alcohol by prospective fathers aged ≥ 35 years can mitigate the adverse effects of increased paternal age on IF, thereby improving the prospects of implantation success in ART treatments.
Data availability
All data supporting the findings of this study are available within the paper and its Supplementary Information. Potential collaborators are invited to contact the corresponding author (caoyunxia5972@ahmu.edu.cn).
References
eClinicalMedicine. The current status of IVF: are we putting the needs of the individual first? eClinicalMedicine 2023, 65 (2023).
Tatum, M. China’s fertility treatment boom. Lancet 396 (10263), 1622–1623 (2020).
Pirtea, P. et al. Recurrent implantation failure: reality or a statistical Mirage?? Consensus statement from the July 1, 2022 Lugano workshop on recurrent implantation failure. Fertil. Steril. 120 (1), 45–59 (2023).
Zegers-Hochschild, F. et al. The international glossary on infertility and fertility care, 2017. Hum. Reprod. 32 (9), 1786–1801 (2017).
Attali, E. & Yogev, Y. The impact of advanced maternal age on pregnancy outcome. Best Pract. Res. Clin. Obstet. Gynecol. 70, 2–9 (2021).
Vitagliano, A., Paffoni, A. & Viganò, P. Does maternal age affect assisted reproduction technology success rates after euploid embryo transfer? A systematic review and meta-analysis. Fertil Steril (2023).
de La Rochebrochard, E., de Mouzon, J., Thépot, F. & Thonneau, P. Fathers over 40 and increased failure to conceive: the lessons of in vitro fertilization in France. Fertil. Steril. 85 (5), 1420–1424 (2006).
Horta, F. et al. Male ageing is negatively associated with the chance of live birth in IVF/ICSI cycles for idiopathic infertility. Hum. Reprod. (Oxford England). 34 (12), 2523–2532 (2019).
Bellver, J., Garrido, N., Remohí, J., Pellicer, A. & Meseguer, M. Influence of paternal age on assisted reproduction outcome. Reprod. Biomed. Online. 17 (5), 595–604 (2008).
Kasman, A. M., Li, S., Zhao, Q., Behr, B. & Eisenberg, M. L. Relationship between male age, semen parameters and assisted reproductive technology outcomes. Andrology 9 (1), 245–252 (2021).
Du, J. et al. Association between parental age, brain structure, and behavioral and cognitive problems in children. Mol. Psychiatry. 27 (2), 967–975 (2022).
Kidera, N., Ishikawa, T., Kawamura, T. & Miyasaka, N. Impact of paternal age on IVF and pregnancy outcomes with only normal sperm parameters. Taiwan. J. Obstet. Gynecol. 61 (6), 1015–1020 (2022).
Klonoff-Cohen, H. Female and male lifestyle habits and IVF: what is known and unknown. Hum. Reprod. Update. 11 (2), 179–203 (2005).
Zitzmann, M. et al. Male smokers have a decreased success rate for in vitro fertilization and intracytoplasmic sperm injection. Fertil. Steril. 79 (Suppl 3), 1550–1554 (2003).
Mínguez-Alarcón, L., Chavarro, J. E. & Gaskins, A. J. Caffeine, alcohol, smoking, and reproductive outcomes among couples undergoing assisted reproductive technology treatments. Fertil. Steril. 110 (4), 587–592 (2018).
Ma, J., Gao, W. & Li, D. Recurrent implantation failure: a comprehensive summary from etiology to treatment. Front. Endocrinol. (Lausanne). 13, 1061766 (2022).
Yin, J. et al. Cohort profile: Anhui Maternal–Child health study in China. BMJ Open. 12 (6), e060091 (2022).
World Health Organization. WHO laboratory manual for the examination and processing of human semen, sixth edition. (World Health Organization, 2021). https://www.who.int/publications/i/item/9789240030787.
Gardner, D. K. & Schoolcraft, W. B. Culture and transfer of human blastocysts. Curr. Opin. Obstet. Gynecol. 11 (3), 307–311 (1999).
Chen, A. et al. Impact of older age adiposity on incident diabetes: a Community-Based cohort study in China. Diabetes Metabolism J. 46 (5), 733–746 (2022).
Murugesu, S. et al. Does advanced paternal age affect outcomes following assisted reproductive technology? A systematic review and meta-analysis. Reprod. Biomed. Online. 45 (2), 283–331 (2022).
Kaarouch, I. et al. Paternal age: negative impact on sperm genome decays and IVF outcomes after 40 years. Mol. Reprod. Dev. 85 (3), 271–280 (2018).
Coban, O. et al. Effect of paternal age on assisted reproductive outcomes in ICSI donor cycles. Andrology 11 (3), 515–522 (2023).
Capelouto, S. M. et al. Impact of male partner characteristics and semen parameters on in vitro fertilization and obstetric outcomes in a frozen oocyte donor model. Fertility Sterilit. 110 (5), 859–869 (2018).
Wu, Y., Kang, X., Zheng, H., Liu, H. & Liu, J. Effect of paternal age on reproductive outcomes of in vitro fertilization. PloS One. 10 (9), e0135734 (2015).
Campos, I. et al. Effects of men and recipients’ age on the reproductive outcome of an oocyte donation program. J. Assist. Reprod.Genet. 25 (9–10), 445 – 542 (2008).
Marsidi, A. M., Kipling, L. M., Kawwass, J. F. & Mehta, A. Influence of paternal age on assisted reproductive technology cycles and perinatal outcomes. Fertil. Steril. 116 (2), 380–387 (2021).
Luna, M. et al. Paternal age and assisted reproductive technology outcome in ovum recipients. Fertil. Steril. 92 (5), 1772–1775 (2009).
Winship, A. L., Stringer, J. M., Liew, S. H. & Hutt, K. J. The importance of DNA repair for maintaining oocyte quality in response to anti-cancer treatments, environmental toxins and maternal ageing. Hum. Reprodouction Update. 24 (2), 119–134 (2018).
Klonoff-Cohen, H., Natarajan, L., Marrs, R. & Yee, B. Effects of female and male smoking on success rates of IVF and gamete intra-Fallopian transfer. Hum. Reprod. 16 (7), 1382–1390 (2001).
Zenzes, M. T. Smoking and reproduction: gene damage to human gametes and embryos. Hum. Reprod. Update. 6 (2), 122–131 (2000).
Borges, E. Jr. et al. Jr. Sperm DNA fragmentation is correlated with poor embryo development, lower implantation rate, and higher miscarriage rate in reproductive cycles of non-male factor infertility. Fertil. Steril. 112 (3), 483–490 (2019).
Sharma, R., Harlev, A., Agarwal, A. & Esteves, S. C. Cigarette smoking and semen quality: a new Meta-analysis examining the effect of the 2010 world health organization laboratory methods for the examination of human semen. Eur. Urol. 70 (4), 635–645 (2016).
Rossi, B. V. et al. Effect of alcohol consumption on in vitro fertilization. Obstet. Gynecol. 117 (1), 136–142 (2011).
Jensen, T. K. et al. Habitual alcohol consumption associated with reduced semen quality and changes in reproductive hormones; a cross-sectional study among 1221 young Danish men. BMJ Open. 4 (9), e005462 (2014).
Borges, E. Jr. et al. Paternal lifestyle factors in relation to semen quality and in vitro reproductive outcomes. Andrologia 50 (9), e13090 (2018).
Acknowledgements
We thank the study participants for their commitment to the AMCHS program. We appreciate the research coordinators for their hard work on the project to help collect the data. JY is supported by the China Scholarship Council.
Funding
The National Key Research and Development Program of China Grant number: 2021YFC2700604.
Author information
Authors and Affiliations
Contributions
RC, JY and YC set up the concept of this research paper. JY and RC performed the data analysis and drafted the manuscript. CL, XP, ZZ helped to collect the database and performed the data quality control. PG, HZ, DC, WZ, WJ commented and revised the manuscript. YC is PI for the AMCHS program. RC is responsible for the overall content of this research paper as guarantor. All authors made comments and revisions on the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yin, J., Chen, R., Churchill, D. et al. Effects of paternal age and interaction with smoking, alcohol consumption and maternal age on implantation failure in women undergoing ART. Sci Rep 15, 23452 (2025). https://doi.org/10.1038/s41598-025-03651-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03651-y