Abstract
Unilateral biportal endoscopic (UBE) surgery is an innovative minimally invasive technique for treating lumbar disc herniation. However, conventional surgical positioning, which combines preoperative surface localization with intraoperative fluoroscopy, has several limitations, including suboptimal accuracy, procedural complexity, and reduced operative efficiency. Additionally, incomplete decompression and over-decompression are common issues in UBE surgery, might leading to disastrous outcomes. However, determining the extent of laminectomy remain a significant challenge. This study explores the use of Kirschner Wire as a localization tool in UBE surgery to enhance localization precision and the the appropriate decompression range. This study included 78 patients diagnosed with lumbar disc herniation (LDH) and radicular pain who underwent UBE discectomy using Kirschner Wires as a localization tool. Another 73 patients with LDH underwent standard UBE discectomy without Kirschner Wires. We compared demographic data, surgical variables, postoperative complications, and health-related quality of life (HRQOL) between the two groups. Incorrect segmental localization occurred in 2 patients in the Kirschner Wire group and 11 patients in the standard UBE discectomy group, indicating a significant difference. The Kirschner Wire group demonstrated shorter total operation time, less time spent identifying the correct segment, fewer instances of radiology exposure, and reduced intraoperative blood loss. Additionally, less paraspinal muscle injury was observed in the Kirschner Wire group. Incomplete decompression was identified in 4 patients in the standard UBE discectomy group, all of whom required revision surgery, whereas no cases of incomplete decompression were observed in the Kirschner Wire group. The incidence of facet injury was higher in the standard UBE discectomy group due to the over-decompression. However, no significant differences were found between the groups in terms of dural tear, root injury, incision infection, and revision surgery. Both groups showed improvements in visual analog scale (VAS) scores for back pain, VAS scores for leg pain, and Oswestry Disability Index (ODI), with a more significant decrease in leg pain VAS scores observed in the Kirschner Wire group. Kirschner Wire is an effective localization tool in UBE discectomy, providing accurate segmental localization and aiding surgeons in determining the extent of laminectomy for decompression, thus reducing the likelihood of incomplete decompression or over-decompression. Additionally, the use of Kirschner Wire can decrease total operation time, radiation exposure, intraoperative blood loss, and paraspinal muscle injury. We recommend Kirschner Wire as localization tools in UBE discectomy to enhance surgical precision and outcomes.
Similar content being viewed by others
Introduction
Lumbar disc herniation (LDH) is one of the most common spine diseases, which is charasterised by low back pain with or without leg pain caused by the compression of the spinal nerve root from a protruded disc material1. Almost 70–85% of patients experience at least one episode of lower back pain with or without leg pain during their lives, severely influencing their health-related quality of life (HRQOL)1. For those who suffered from sever leg pain with no relief by conservative treatments or combined with neurological deficits, including sensory or motor problem, surgery is considered as an effective method. Lumbar inerbody fusion (LIF) in open approach is widely applied in treating LDH with good clinical outcomes and the majority of spinal surgeons are well trained and comfortable in performing it2. However, this conventional open surgery requires a large midline skin incision, extensive detachment and prolonged retraction of back muscles from the spinal processes, may leading to great volumes of intra-operative blood loss, postoperative low back pain, delay recovery and mobilization3. Therefore, many minimally tnvasive techniques and improved approaches have been proposed and used in treating LDH, such as minimally invasive lateral lumbar interbody fusions (LLIF) with percutaneous pedicle screws (PPS)4, percutaneous endoscopic discectomy1, and et al.
In recent years, unilateral biportal endoscopy (UBE) has emerged as a new minimally invasive spine technique with good visualization of the contralateral sublaminar and medial foraminal areas5. Furthermore, good cinical outcomes have been reported by many researchers, such as improving function, with the additional benefits of a significantly greater decrease in pain, postoperative recovery time, time to mobilization, and opioid use1,5,6,7. UBE is efectively employed in addressing various lumbar spine conditions, and our research team sucessfully completed the first UBE discectomy in our medical center in May 2023.
So far, nearly 180 UBE discectomies have been sucessfully performed in our center, and some experiences have been achieved and summarized. During the performance of UBE discectomy, we found that the location of correct surgical segment was the key to success of the surgery. However, compared with traditional open surgery, the surgical visualization in UBE is significantly smaller, and it is easier for the surgeons to locate the wrong surgical segment, namely the disorientation under endoscopic visualization, which needs more time to be re-located the correct segments, then might increasing the operation time and the incidence of postoperative complications. Intraoperative fluoroscopy could be used to locate the surgical segment in UBE discectomy; however, unlike traditional open surgery, location at wrong surgical segments could also happen even if intraoperative fluoroscopy used in UBE discectomy since the limited surgical visualization. To our knowledge, no studies have reported how to increase the accuracy of location of surgical segments.
In addition, incomplete decompression is a common issue in UBE surgery, especially for young surgeons who are just learning this technique and determining the extent of laminectomy and minimizing the risk of incomplete decompression remain significant challenges8. Due to the limited surgical view under the UBE endoscope, determining the laminectomy decompression range poses a significant challenge. If the decompression range is small, postoperative symptom relief is minimal, leading to poor surgical outcomes. If the decompression range is large, it may result in postoperative spinal instability and symptoms like low back pain. Therefore, determining the appropriate decompression range is crucial for UBE surgery. To the best of our knowledge, there is currently no literature reporting on how to determine the decompression range in UBE surgery, especially for young surgeons who are just learning this technique.
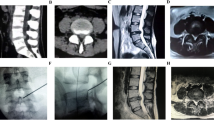
Based on our experiences, to minimize the number of intraoperative fluoroscopy and radiology exposure, and to achieve sufficient decompression while avoiding over-decompression in UBE surgery, we first introduced Kirschner Wire as a location tool in UBE discectomy (Firgure 1), which might provide us the anatomical informations to identify the vertebral plate and intervertebral space, avoiding the disorientation under endoscopic visualization, finding the correct surgical segment quickly and correctly, and determining the appropriate decompression range as well.
Therefore, we performed this study, aming to explore the application of Kirschner Wire as a location tool in UBE discectomy.
Methods
Subjects
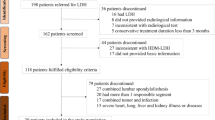
A toal of 151 patients diagnosed as LDH with radicular pain who underwent UBE discectomy between May 2023 and July 2024 were enrolled in this study. 78 patients received UBE discectomy with application of Kirschner Wire as a location tool by two surgeons (Dr. Qiulin Zhang and Dr. Changwei Yang); while another 73 patients received regular UBE discectomy without Kirschner Wire by two surgeons (Dr. Ningfang Mao and Dr. Xiaolong Li).
The inclusion criteria were: (1) back or radiating pain related to single-segment LDH; (2) symptom persistence of more than 4 weeks; (3) magnetic resonance (MR) images corre-lated to the symptoms; and (4) sufficient data, including demographic data, surgical variables, complications and assessments of HRQOL.
The exclusion criteria were as follows: (1) foraminal or extraforaminal disc involvement; (2) more than 2 segments needs be performed; (3) recurred LDH; (4) motion instability (defined as > 3 mm translation or > 5o angulation); (5) spondylolisthesis more than Meyerding grade II; (6) cauda equine syndrome; (7) comorbid tumorous or infectious conditions. In addition, those who lacked sufficient data in the follow-ups were excluded from this study.
This study was approved by the Institutional Review Board, and all patients in our study provided written informed consent for the study and surgery. Due to the retrospective nature of the study, (Review Board of Changhai Hospital, Navy Medical University) waived the need of obtaining informed consent. All methods were performed in accordance with the relevant guidelines and regulations required by the journal.
Surgical technique
UBE discectomy with application of Kirschner wire
The patient was positioned prone on a Jackson table under general anesthesia. The surgical approach was determined based on the symptomatic side. The procedure was as follows:
Preoperative Localization: C-arm fluoroscopy was used to identify the surgical segment, including the upper and lower pedicles and intervertebral space (Fig. 1A). A Kirschner Wire (K-wire) was then inserted (Fig. 1B), and a second C-arm fluoroscopy was performed (Fig. 1C and D) to confirm the target segment. The K-wire was ideally positioned at the lower lamina of the upper vertebra and the medial aspect of the facet joints, marking the boundary of the lamina to be resected. In the sagittal plane, the K-wire should align with the center of the target intervertebral disc. If misplaced, the K-wire was repositioned and fluoroscopy repeated.
The application of Kirschner Wire as the location tool before the UBE discectomy. (A) The first fluoroscopy by C-arm to locate the the surgical segment, including the upper and lower pedicles and intervertebral space. (B) Input the Kirschner Wire. C and D. The second fluoroscopy to explore the location of the Kirschner Wire.
Portal Establishment: After confirming the K-wire position, incisions for the endoscopic portal and surgical portal were made. The endoscopic portal was placed 1–1.5 cm lateral to the K-wire, within the facet joint, with a length of 3–5 cm. The surgical portal was positioned 1–1.5 cm medial to the K-wire, with a length of 4–7 cm. The endoscopic portal facilitated continuous irrigation and visualization, while the surgical portal allowed instrument manipulation and removal of herniated disc material.
Decompression Procedure: Under endoscopic guidance, the K-wire was identified (Fig. 2), clarifying the lamina boundaries to prevent disorientation. The hypertrophic ligamentum flavum and abnormal fatty hyperplasia were removed to expose the dural edge and ipsilateral traversing nerve root. Protruded disc fragments were extracted using pituitary forceps and Kerrison punches. After removal, nerve root mobility was assessed with a hook dissector.
Closure: Annulus fibrosis repair was performed in all patients (Fig. 3). Wounds were closed using 3 − 0 absorbable sutures and skin adhesives.
Regular UBE discectomy without Kirschner wire
73 patients received regular UBE discectomy without Kirschner Wire by two surgeons (Dr. Ningfang Mao and Dr. Xiaolong Li). The surgery was performed according to the procedures reported by Kim et al.1.
C-arm fluoroscopy was first performed to locate the surgical segment. After the placement of endoscopic portal) and surgical portal, C-arm fluoroscopy was performed again to relocate the position of two portals and target segment (Fig. 4). If the surgeons did not find the target intervertebral space during the procedure of decompression, intraoperative C-arm fluoroscopy was performed to relocate. Annulus fibrosus suture was performed in all patients and wound closure was performed using 3:0 absorbable sutures and skin adhesives.
Data collection
Demographic data were collected, including age, gender, BMI, duration of hospitalization and surgical segment. Several surgical variables were also collected and compared, including total operation time, time used to find the correct segment, number of radiology exporsure, number of incorrect segment location and intraoperative blood loss. Cross-sectional area (CSA) of the paraspinal muscles based on MRI scans performed preoperatively and postoperatively9, which was measured at the disc level using MRI using ImageJ software (NIH, Bethesda, MD, USA). The ratio of muscle CSA variation (RCV) was calculated according to the following formula: Last CSA/preoperative CSA*100%. The degree of paravertebral muscle atrophy was calculated using the following formula: 100%-RCV.
Complications were also compared between two groups. In addition, patients’ HRQOL. Visual Analog Scale (VAS) was used to assess the back pain and leg pain. Clinical outcomes were assessed by the Oswestry Disability Index (ODI). Improvement of VAS or ODI was defined as [(Postoperative-Preoperative)/Preoperative*100%]. All data was measured by two independent reviewers.
Statistical analysis
Statistical analyses were performed using SPSS 21.0 statistics software (SPSS Inc, Chicago, IL). Descriptive statistics were listed in the form of mean and standard deviation (SD). A χ2 test was used to compare the categorical variables, such as gender, number of incorrect segment location and et al. The independent-samples t test was carried out for surgical variables, degree of paraspinal muscle injur, improvement of HRQOL and et al. P < 0.05 was selected as significant level.
Results
We enrolled 78 patients who underwent UBE discectomy with application of Kirschner Wire and 73 patients who received regular UBE discectomy, respectively. The patients’ demographic characteristics were shown in Table 1. There was no significant difference of age, gender, BMI and surgical segment between two groups (P > 0.05). The duration of hospitalization in UBE discectomy with Kirschner Wire group was significantly shorter than it in regular UBE group (4.40 ± 1.59 vs. 5.55 ± 3.74, P = 0.014).
The total operation time in UBE discectomy with Kirschner Wire group was 91.86 ± 26.47 minuts, which was significantly shorter than it (111.36 ± 33.25 mintus) in regular UBE group with the P value of < 0.001 (Table 2). Dut to the use of Kirschner Wire, surgeons could find the correct segment more easily with less time (13.96 ± 6.08 vs. 27.51 ± 9.82 mintus, P < 0.001) and less numbers of radiology exposure (2.03 ± 0.16 vs. 2.26 ± 0.47, P < 0.001) compared with regular UBE discectomy (Table 2). In regular UBE group, incorrect surgical segment was located in 11 patients (15.07%), and surgeons were lost the position under endoecope, which required intraoperative fluoroscopy again. However, disorientation under endoscopic visualization only happened in 2 patients in UBE discectomy with Kirschner Wire (2.56%), with significant difference (P = 0.006, Table 2). In addition, the intraoperative blood loss was significantly less in UBE discectomy with Kirschner Wire group than that in regular UBE group (56.92 ± 49.04 ml vs. 87.12 ± 74.17 ml, P = 0.003). The degree of paraspinal muscle injury in UBE discectomy with Kirschner Wire group and regular UBE group was 5.37 ± 2.40 and 8.09 ± 5.82, respectively, with significantly difference (P < 0.001, Table 2).
As to the complications, 2 and 2 cases of dural tear occurred in UBE discectomy with Kirschner Wire group and regular UBE group, respectively, which were treated with conservative treatment including bed rest and fluid replacement. No signficant difference of incidence of dural tear was observed between two groups (P = 0.946, Table 2). Incomplete decompression was identified in 4 patients in the regular UBE discectomy group, all of whom required revision surgery, whereas no cases of incomplete decompression were observed in the Kirschner Wire group. The symptoms of these patients were not relieved after conservative treatment and all of them received revision surgery eventually. There was significant difference of the incidence of incomplete decompression and revision surgery between two groups (P = 0.041, Table 2). Root injury occurred in 1 and 2 patients with postsurgical numbness and pain in the lower limbs without muscle strength and reflex abnormalities in UBE discectomy with Kirschner Wire group and regular UBE group, respectively, without significantly difference (P = 0.521, Table 2), and they recovered within 1 month after treatment with low-dose methylprednisolone combined with a pregabalin capsule and methycobal. 1 and 1 patients experienced incision infection and the wound returned to normal after the treatment of antibiotics (P = 0.962). However, we found that there was significant difference of facet injury between two groups with 1 case in UBE discectomy with Kirschner Wire group and 6 cases in regular UBE group (P = 0.043, Table 2).
In both groups, postoperative back and leg pain and ODI were significantly improved (Table 1). Improvemeng of leg pain was found to be significantly freater in UBE discectomy with Kirschner Wire group than that in regular UBE group (91.53 ± 11.37 vs. 84.59 ± 20.00, P = 0.009, Table 2); however, no significant difference of improvemeng of back pain and ODI was observed between two groups (P = 0.161 and P = 0.566, respectively. Table 2).
Discussion
In recent years, unilateral biportal endoscopic (UBE) discectomy has gained significant traction in managing degenerative lumbar pathologies, particularly lumbar disc herniation and spinal stenosis. This minimally invasive approach demonstrates distinct advantages over conventional open procedures, notably attenuated iatrogenic soft tissue trauma, abbreviated hospitalization durations, and accelerated functional recovery10. In contrast to traditional microscopic techniques that constrain surgical visualization to extradural spaces while restricting instrument maneuverability2, UBE establishes dual interdependent portals: an endoscopic observation channel and an instrument manipulation channel. This biportal architecture synergistically yields an expansive visual field encompassing both intraspinal and foraminal regions10, thereby enhancing anatomical discernment critical for precise decompression.
During the procedures of UBE discectomy performed in our center, how to find the correct segments that need to be decompressed under the endoscope remains a great challenge although the surgical portal could provide a broad and clear surgical field of view. The incorrect segment location ratio in your classical approach was reported to be 15.07% (11/73), which was significantly greater than it in Kirschner Wire group. Few researchers reported the incorrect segment location ratio in UBE surgery. The incidence of incorrect segment location and disorientation under endoscopic visualization was only repotred by researchers in academic conferences, ranging from 2.4 to 16.6%. However, some reasons might be contributors to this high ratio. First, many patients we selected were from the early stages when we first began performing this type of surgery. At the begining of carrying out this new technique, we found it was difficult to find out the anatomy of laminae and intervertebral space due to the lack of experiences. Consequently, more time need be spared. This relative inexperience in the early stages resulted in incorrect segmental localization for many patients during the initial surgical procedure. However, as the number of surgeries increased and experience accumulated, the accuracy of segmental localization has progressively improved. Nevertheless, due to the inclusion of early cases, the overall rate of incorrect segmental localization has remained elevated, reported as high as 15.07%. Second, to cultivate young surgeons, we routinely grant them autonomy in performing UBE surgery. During their initial training phase, these surgeons independently conduct preoperative localization, though inexperience frequently contributes to elevated error rates in segment identification during early UBE cases, which might also result in our high incorrect segment location ratio in classical approach. However, longitudinal analysis demonstrates progressive improvement in localization accuracy as procedural experience accumulates, and overall localization accuracy gradually improves. Therefore, the selection of these early cases resulted to the high incorrect segment location ratio in your classical approach, which was also a limitation of this study.
To handle this disadvantage, we first introduced Kirschner Wire as a location tool at UBE discectomy (Firgure 1), and this study reported the effectiveness of Kirschner Wire as a location tool in UBE discectomy.
In this study, Kirschner Wire was input at the beginning of the surgery to provide surgeons accurate anatomy of laminae and intervertebral space under the endoscope. With the help of Kirschner Wire, we could easily determine the surgical segments that need to be decompressed. As a result, only 2 cases of incorrect segment location occurred in UBE discectomy with Kirschner Wire group, while 11 cases occurred in regular UBE discectomy. These 2 cases in UBE discectomy with Kirschner Wire group occurred at the beginning of this new technique with less surgical experiences. With the number of performances of UBE discectomy, we could find Kirschner Wire in surgical field faster and more easily. Consequently, less total operation time and time used to find the correct segment was spared, which was an advantage of Kirschner Wire. In addition, uncertain about the anatomy under the endoscope needed more times of radiology exposure to determine the surgical sgment, which could also be decreased by using of Kirschner Wire during the UBE discectomy. Furthermore, with the help of Kirschner Wire as a location tool, surgeons were certained about which muscles needed to be exposed and which segment needed to be decompressed. As a result, less intraoperative blood loss and degree of paraspinal muscle injury was observed in UBE discectomy with Kirschner Wire group compared with regular UBE discectomy with significant difference. Consequently, less less intraoperative blood loss and degree of paraspinal muscle injury resulted in shorter duration of hospitalization, which was another advantage of use of Kirschner Wire as a location tool in UBE discectomy.
Despite its favorable clinical outcomes, such as reduced blood loss and shorter hospitalization, UBE discectomy carries potential complications, including epidural hematoma, dural injury, and compression of the outlet nerve root10. In this study, we also reported the incidence of complications in UBE discectomy with Kirschner Wire group and regular UBE discectomy group. The total complication rate was 8.9% and 20.5% in UBE discectomy with Kirschner Wire group and regular UBE discectomy group, respectively, which was consistent with previous studies11. There were 2 and 2 cases of dural tear occurred in UBE discectomy with Kirschner Wire group and regular UBE discectomy group, respectively, which was higher than it in traditional surgery12. UBE surgery is performed with endoscopy and has a steeper learning curve than traditional open surgery; this is the reason for the high number of dural tear. During endoscopic surgery, it is not easy to control the distance, and it is easy to puncture and damage the dural membrane. Besides, adhesion between intervertebral disc and dural sac due to the prolonged duration of intervertebral disc herniation might also contributed to the higher rate of dural tear. Incomplete decompression was also one of the common complications in UBE discectomy, which was also reported in previous studies13,14. Long-term traditional surgery can produce muscle memory in the surgeon, while UBE discectomy is a new technqiue with short application in clinics.
Unlike the traditional open surgery, it is not easy to control the distance and determine whether the decompression is enough or not, leading to incomplete decompression consequently. Therefore, incomplete decompression is a great challenge for UBE surgery, especially for young surgeons who are just learning this technique and determining the extent of laminectomy, which might result in persisting postoperative symptoms of lower limb radicular pain and numbness, and some patients may even experience exacerbation of lower limb symptoms. In our study, incomplete decompression was identified in 4 patients in the regular UBE discectomy group. These patients received conservative treatments such as low-dose methylprednisolone combined with a pregabalin capsule and methycobal; however, back pain and leg pain were still not significantly relieved. Therefore, revision surgery of tradition open fusion suregery was performed. However, no cases of incomplete decompression were observed in the Kirschner Wire group since Kirschner Wire could provides us a range for decompression under endoscopy to estimating the extent of laminectomy and reduce the likelihood of incomplete decompression. Besides, if the decompression range is large, it may result in postoperative spinal instability and symptoms like low back pain. In regular UBE discectomy, we were confused about the boundary of decompresion, and too many bones and soft tissues might be ground off, leading to the facet injury, instability of the lumbar spine, greater intraoperative blood loss and degree of paraspinal muscle injury mentioned abrove. With the help of Kirschner Wire, we could not only determine the decompression range intraoperatively to ensure effective decompression but also prevent over-decompression, thereby avoiding facet joint damage and postoperative altered stress distribution. The results showed a significant difference in facet injury between the two groups: 1 case in the UBE discectomy with Kirschner Wire group versus 6 cases in the regular UBE group (P = 0.043, Table 2). Therefore, Kirschner Wire is recommended as a location tool to provide us the anatomy of laminae and bony boundary need to be ground off.
Root injury was also observed in both groups, which was transient since these patients recovered within 1 month after treatment with low-dose methylprednisolone combined with a pregabalin capsule and methycobal. The initial learning curve during surgery might be the important contributor to transient root injury. In our experiences, with the increasing unmbers of UBE discectomy, incidence of dural tear, Incomplete decompression and root injury could be significantly decreased by mastering the endoscopic technique, and overccoming the learning curve. Although the operation time was significantly longer in regular UBE discectomy, there was no significant difference of incision infection between two groups. Compared with tradition open surgery, there was no fixation system implaced in UBE discectomy, which was another advantage of UBE discectomy.
In both groups, postoperative back and leg pain and ODI were significantly improved, verifing that UBE discectomy was an effective surgery for lumbar disc hernitation15. We found that the improvement of leg VAS score was signfiicantly greater in UBE discectomy with Kirschner Wire group than that in regular UBE discectomy group. The higher incidence of Incomplete decompression and revision surgery might be contributed to this. However, there was no significant difference of improvement of back VAS score and ODI between two groups.
The limitations of this study are its retrospective nature, small sample size, and short follow-up period. Many patients we selected were from the early stages when we first began performing this type of surgery. This relative inexperience in the early stages resulted in incorrect segmental localization ratio for many patients in classical approach during the initial surgical procedure, which was also a limitation of this study. In addition, because of the nature of retrospective studies, selection bias seems to be intrinsic by patients’ preferences and the surgeon’s experience may be influenced the outcomes. Adequate randomized prospective studies for UBE discectomy with Kirschner Wire is required to verify the present results.
Conclusions
Kirschner Wire is an effective localization tool in UBE discectomy, providing accurate segmental localization and aiding surgeons in determining the extent of laminectomy for decompression, thus reducing the likelihood of incomplete decompression or over-decompression. Additionally, the use of Kirschner Wire can decrease total operation time, radiation exposure, intraoperative blood loss, and paraspinal muscle injury. We recommend Kirschner Wire as a localization tool in UBE discectomy to enhance surgical precision and outcomes.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Kim, S. K., Kang, S. S., Hong, Y. H., Park, S. W. & Lee, S. C. Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: a multicenter, retrospective analysis. J. Orthop. Surg. Res. 13 (1), 22 (2018).
Mobbs, R. J., Phan, K., Malham, G., Seex, K. & Rao, P. J. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J. Spine Surg. 1 (1), 2–18 (2015).
Lee, C. S. et al. How does back muscle strength change after posterior lumbar interbody fusion? J. Neurosurg. Spine. 26 (2), 163–170 (2017).
Kameyama, K. et al. Radiological assessment of postoperative paraspinal muscle changes after lumbar interbody fusion with or without minimally invasive techniques. Global Spine J. 13 (2), 295–303 (2023).
Hwa Eum, J., Hwa Heo, D., Son, S. K. & Park, C. K. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J. Neurosurg. Spine. 24 (4), 602–607 (2016).
Mobbs, R. J., Li, J., Sivabalan, P., Raley, D. & Rao, P. J. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical Article. J. Neurosurg. Spine. 21 (2), 179–186 (2014).
Heo, D. H., Son, S. K., Eum, J. H. & Park, C. K. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg. Focus. 43 (2), E8 (2017).
Peng, J. et al. Learning curve insights in unilateral biportal endoscopic (UBE) spinal procedures: proficiency cutoffs and the impact on efficiency and complications. Eur. Spine J. 34 (3), 954–973 (2025).
Tan, B. et al. Unilateral biportal endoscopy vs. open decompression for lumbar epidural lipomatosis-cohort study using a prospective registry. Front. Neurol. 15, 1366357 (2024).
Yu, Z., Ye, C., Alhendi, M. A. & Zhang, H. Unilateral biportal endoscopy for the treatment of lumbar disc herniation. J Vis. Exp. 202 (2023).
Li, Y. S., Chen, C. M., Hsu, C. J. & Yao, Z. K. Complications of unilateral biportal endoscopic lumbar discectomy: A systematic review. World Neurosurg. 168, 359–68.e2 (2022).
Yu, X., Yue, H., Wei, H., Li, Q. & Li, Z. Comparative study of unilateral biportal endoscopic and traditional open surgery in the treatment of lumbar disc herniation. Altern. Ther. Health Med. 29 (5), 370–374 (2023).
Torudom, Y. & Dilokhuttakarn, T. Two portal percutaneous endoscopic decompression for lumbar spinal stenosis: preliminary study. Asian Spine J. 10 (2), 335–342 (2016).
Park, S. M. et al. Learning curve for lumbar decompressive laminectomy in biportal endoscopic spinal surgery using the cumulative summation test for learning curve. World Neurosurg. 122, e1007–e13 (2019).
Wang, B., He, P., Liu, X., Wu, Z. & Xu, B. Complications of unilateral biportal endoscopic spinal surgery for lumbar spinal stenosis: A systematic review of the literature and Meta-analysis of Single-arm studies. Orthop. Surg. 15 (1), 3–15 (2023).
Funding
This study was supported by Shanghai Yiyuan Xinxing Youth Medical Talent Development and Funding Program (SHWSRS(2025)_071).
Author information
Authors and Affiliations
Contributions
Changwei Yang, Guangzhu Yan, Mingyuan Yang and Kai Luo wrote the main manuscript text Xiaolomg Li and Ninfang Mao prepared figuressMingyuan Yang and Kai collected the data and conducted the ststistical analysisYushu Bai and Qiulin Zhang supervise the research.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Approval statement
This study was approved by the Institutional Review Board of Changhai Hospital, Navy Medical University”.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, C., Yan, G., Luo, K. et al. Kirschner wire as an effective localization tool in UBE discectomy: enhancing segmental localization accuracy and optimizing decompression margins. Sci Rep 15, 22588 (2025). https://doi.org/10.1038/s41598-025-03811-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03811-0