Abstract
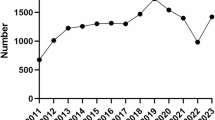
The China National HIV Study (CNHS) on the surgical patient population aimed to investigate the preoperative HIV positive rate and secular trends in the surgical patient population of China. The CNHS included a nationally representative sample of participants who were diagnosed with HIV infection between 2009 and 2018 during preoperative screening selected from 27 comprehensive hospitals in nine provinces using a stratified random sampling methodology. The preoperative HIV positive rate was estimated according to age, sex, occupation, urbanization, and hospital level. An ARIMA model was developed to predict HIV trend from 2019 to 2023. A total of 4,753,874 patients, including 2,830,307 males with an average age of 45·3 years, participated in the CNHS. HIV infection was diagnosed in 2,858 individuals (6·0 per 10,000), and increased from 19·5 (14·4–24·6) per 100,000 in 2009 to 84.8(77.2–92.3) in 2016, decreased from 75.2 (68.3–82.0) in 2017 to 74·3 (67·7–81·0) in 2018. Compared to 2009, the annual growth rate of preoperative HIV positive rate in 2018 was 381%, with most patients being male (567%), aged ≥ 50 years (423%), official staff (1508%), and unemployed (1153%). The predicted HIV positive rate from 2019 to 2023 showed an overall decreasing trend in ARIMA(2,1,3)(1,1,2)4 model. The first time preoperative HIV positive rate in the surgical patient population with a ten-year secular trend was report. Increasing trend was seen from 2009 to 2016 with a slight decreasing from 2017, which implied a positive comment on the current HIV prevention programs.
Similar content being viewed by others
Introduction
There were 38.4 million [33.9–43.8 million] people living with HIV/AIDS worldwide by the end of 2021, and 1.5 million [1.1–2.0 million] people were newly infected1 The positive rate of HIV infection is an important indicator for monitoring the spread of the epidemic and the effectiveness of prevention and control algorithms. National HIV surveillance is commonly undertaken using sentinel monitoring sites among high-risk groups in China2,3 However, sentinel surveillance sites mainly cover high-risk groups such as drug users, among commercial sex workers (CSWs) and men who have sex with men (MSM) in designated hospitals, and there is a lack of monitoring of the surgical patient population in comprehensive hospitals4,5,6,7 Individuals with undiagnosed HIV infection in the surgical patient population, particularly those who are unaware of their HIV infection status in comprehensive hospitals, pose a risk of HIV transmission.
In order to reduce iatrogenic infections, provide early intervention for infected people, protect medical staff and reduce medical disputes, hospitals in China have routinely formulated an infectious disease preoperative screening (including HBsAg, Anti-HBs, HBeAg, Anti-HBe, Anti-HBc, Anti-HCV, Anti-HIV, Anti-TP). Therefore, the medical records of preoperative HIV screening extracted using population-based sampling methods and clinic-based data during the epidemiological survey were analyzed. The China National HIV Study (CNHS) of surgical patient population was designed and undertaken to provide an up-to-date national dataset of preoperative HIV positive rate in comprehensive hospitals and describe the secular trend in the surgical patient population of China.
Methods
Sampling methods
During the main sampling phase, 31 provinces (municipalities or autonomous regions) in mainland China were categorized into three regions (high, moderate, and low HIV endemic areas) according to the classification standard of the epidemic area2,8,9,10 A total of nine provinces and municipalities were initially selected by stratified random sampling (three from highly, four from moderately, and two from lowly endemic areas) (Fig. 1). Hospital selection within each province was further stratified by hospital reputation in HIV-related care, research capacity, and patient volume. Provincial health bureaus provided updated lists of comprehensive hospitals, from which one provincial, one city-level, and one county-level hospital were selected using probability proportional to size (PPS) sampling. In cases of refusal, replacement hospitals were chosen via a modified Kish grid prioritizing institutions with comparable bed counts and service scope.11 Finally, nine provincial, nine city-level, and nine county-level hospitals were selected. Although no formal sample - size calculation was carried out, the inclusion of 4,753,874 patients in this study has ensured sufficient statistical power to detect minor differences among subgroups. According to the standards of epidemiological research, large sample sizes usually yield reliable results.
This flow chart shows the overall nationwide sampling process. Nine provinces and municipalities were first selected by stratified random sampling. The sampling was performed separately in each province using the multistage stratified cluster random sampling method. The data were collected and the national preoperative HIV positive rates were then estimated for the overall population and for subgroups of interest.
Data extraction
The medical records of all eligible patients in the selected hospitals, who had undergone preoperative screening between January 1, 2009, and December 31, 2018, were collected through the medical reports checking system by trained research teams. Duplicate reports of selected patients were excluded using the unique identification (ID) number in the medical record system. The extracted data included age, sex, occupation, residence, HIV test results, hospital level, and departments where patients visited. The hospital departments were divided into high-risk departments with more patients visiting HIV infection and low-risk departments. High-risk departments included the departments of dermatology, urology, and anorectal surgery, while others were regarded as low-risk departments.
The CNHS was approved by the Institutional Review Board of the 3rd Hospital of Hebei Medical University (Sects. 2019-017-1), and as the study was a retrospective review of hospital records the requirement for informed consent was waived. The study protocol was registered with the Chinese Clinical Trial Registry (Chi-CTR-1900026185).
HIV testing followed China CDC’s National HIV Testing and Diagnosis Technical Guidelines (2021). All hospitals used ELISA for initial screening, confirmed by Western blot. Quality control included biannual proficiency testing, technician certification, and external audits by CDC-accredited labs. Sensitivity analyses confirmed consistency across institutions (Supplementary Table 3).
Modeling process
The auto-regressive integrated moving average (ARIMA) model is used for time series analysis by modeling an approximate description of the time-varying incidence series.
Sequence stabilization
The stabilization of the series was determined based on the trend graph of total HIV positive rate change from spring 2009 to winter 2018, autocorrelation analysis, partial autocorrelation analysis, and further verified by Augmented Dickey–Fuller test.
Model identification and parameter Estimation
The seasonality and stability of the sequence were analyzed, and the d, D, and S parameters were determined to identify and order the model.
Model test
The residual sequence, autocorrelation function (ACF), and partial ACF (PACF) images of the fitting model were tested.
Prediction
The fitted model was used to predict the HIV positive rate from 2019 to 2023.
Statistical analysis
Preoperative positive rate of HIV infection were estimated for the overall population and subgroups by age, sex, occupation, urbanization, and hospital level. We further examined the preoperative positive rate by high-risk and low-risk departments. The difference in positive rate between categories of nominal variables was tested using the Rao–Scott χ2 test. All statistical analyses were performed using SAS version 9·3 (SAS Institute Inc., Cary, NC, USA).
Results
General characteristics of participants
A total of 4,753,874 patients (96% of screened individuals) were included, with a male predominance (59.5%) and mean age of 45.3 years. Demographic details are summarized in Table 1.
Preoperative HIV positive rate in the surgical patient population
HIV infection was identified in 2,858 patients (6.0 per 10,000), with males accounting for 76.7% of cases. The overall annual HIV-positive rate from 2009 to 2018 was 60.1 per 100,000 (Table 1).
The preoperative HIV positive rate was also analyzed based on individual characteristics and regions (Table 1). Males had a higher preoperative HIV positive rate than females in each age group over 16 years; females had a higher rate than males in the age group ≤ 15 years. Males living in urban areas had a higher rate than those in rural areas. When stratified by occupation, business service personnel, and seamen, fishermen and long-distance drivers [497·2 (428·8–565·6) and 284·3 (177·2–391·4) per 100,000 population, respectively] had the highest positive rates. According to endemic areas, high-endemic areas had the highest positive rate. When stratified by hospital level, city-level and county-level hospitals [72·4 (68·2–76·7) and 72·6 (66·0–79·1) per 100,000 population, respectively] had a higher positive rate than provincial hospitals [49·4 (46·7–52·1) per 100,000 population] (Table 2).
Trends in preoperative HIV infection prevalence in the surgical patient population
summarize the trends in the preoperative HIV positive rate by sex, age, urbanization, classification of endemic area, and hospital level in the surgical patient population. The HIV-positive rate rose significantly from 19.5 to 74.3 per 100,000 between 2009 and 2018, with a striking 281% overall annual growth rate. Males experienced a 5.7-fold increase, surpassing females’1.5-fold rise (Table 1).
Figure 2 National preoperative HIV positive rate in China between 2009 and 2018. (A) National preoperative HIV positive rate in China by sex. (B) National preoperative HIV positive rate in China by age. (C) National preoperative HIV positive rate in China by urbanization. (D) National preoperative HIV positive rate in China by classification of endemic area. (E) National preoperative HIV positive rate in China by hospital level.
The annual growth rate in the 16-to-49-year age group (361%) was lower than that in the ≥ 50-year age group (423%); that in the urban area (449%) was faster than that in the rural area (331%); and that in the moderately endemic area (2758%) was faster than that in the highly endemic area (345%). The annual growth rate in provincial hospitals was 427%, followed by city-level hospitals (412%) and county-level hospitals (234%). According to occupation, the annual growth rate of official staff was 1508%, followed by that of unemployed (1153%), business services (503%), teachers (311%), workers (305%), retirees (275%), farmers (262%), and others (177%).
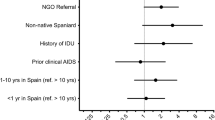
Table 3 summarizes the results of the risk factors of patients visiting high-risk departments. Male sex and the period from 2014 to 2018 were identified as strong risk factors for HIV infection. When compared with farmers, manual workers and retired workers had a higher risk of visiting high-risk departments. Compared with highly endemic areas, moderately and lowly endemic areas were protective factors for those visiting high-risk departments. When compared with provincial hospitals, city-level hospitals were a risk factor.
ARIMA product seasonal prediction model
Sequence stabilization
Figure 3 A shows that the positive rate of HIV had an epidemic trend and a seasonal epidemic pattern, with the annual epidemic cycle and the peak of the epidemic in the autumn of each year. From 2009 to 2016, the positive rate showed an overall upward trend, and since 2017, it has slightly decreased. The ACF attenuated slowly and PACF had no obvious truncation, which indicated that it was not a stationary time series and needed to be stabilized through logarithmic transformation and differencing (Fig. 3B and C). After natural logarithm conversion, non-seasonal differencing, and seasonal differencing, the new sequence was relatively stationary, the long-term trend and seasonal trend basically disappeared, and the values fluctuated randomly around 0 (Fig. 3D). The ACF was approximately attenuated in a sinusoidal fashion, PACF truncated at time point 4, and ADF test resulted in P < 0·05, which indicated that the new sequence was a stationary time series (Fig. 3E and F).
Sequence stabilization (A) Change in trend of HIV positive rate in 2009–2018. (B) ACF diagram of HIV positive rate series in 2009–2018. (C) PACF diagram of HIV positive rate series in 2009–2018. (D) Time series diagram after logarithmic transformation and differencing. (E) ACF diagram after logarithmic transformation and differencing. (F) PACF diagram after logarithmic transformation and differencing.
Model identification and parameter Estimation
According to the ACF and PACF analyses, P = 2 and Q = 3 were obtained. At this time, the AIC value was the minimum, at 0·654. A continuous ARIMA (2,1,3) model was developed. For seasonal ARIMA (P,1,Q)4 models, it was rare for P and Q values to exceed order 2. Supplement Table 1 showed that ARIMA(2,1,3)(1,1,2)4 had the smallest AIC and the largest R2, which indicated that the fitting value of this model had the smallest difference from the actual value and the best goodness of fit, so it was determined to be the optimal model.Among all tested seasonal ARIMA models, ARIMA(2,1,3)(1,1,2)₄ was chosen because it minimized AIC, which balances model fit and complexity, while maximizing R² to ensure the best data representation.
Model test
The residual sequence fluctuated around a small range of 0 and basically satisfied the normal distribution (Figs. 4A-C). Both ACF and PACF were within the confidence range, and the residual randomness test showed no statistical significance (P > 0·05), indicating that the residuals were randomly distributed, the sequence was uncorrelated, and the sequence was a white noise. Figure 4D showed that the trends of the two were basically consistent, which indicated that the model had a high degree of fit and predictive value.
Model test. (A) Residual diagram of the multiple seasonal ARIMA model (2,1,3)(1,1,2)4. (B) Residual ACF diagram of the multiple seasonal ARIMA model (2,1,3)(1,1,2)4. (C) Residual PACF diagram of the multiple seasonal ARIMA model (2,1,3)(1,1,2)4. (D) Actual and fitted values of HIV positive rate series in 2009–2018.
Prediction
The prediction results of the ARIMA (2,1,3) (1,1,2)4 product model for HIV positive rate in four seasons were the lowest in winter from 2020 to 2023 and highest in summer from 2021 to 2023 (Supplement Table 2).
Discussion
The CNHS on the surgical patient population is the first national epidemiological investigation of preoperative HIV positive rate ever conducted in this population. In the CNHS, the positive rates of HIV in the surgical patient population are calculated directly and more accurately, rather than calculated based on data obtained from the high-risk groups in the traditional Chinese surveys. HIV-positive patients in the CNHS were accidentally found passively during the preoperative screening, rather than actively targeted among high-risk groups. Therefore, the present study demonstrates the actual HIV epidemiology among surgical patients in China. We found that the preoperative HIV positive rate increased from 19·5 to 74·3 per 100,000 population from 2009 to 2018 in the surgical patient population, which implies that HIV infection is a major public health burden in China.
Most cases of HIV infection among the general population, particularly in the non-high-risk population, are diagnosed incidentally when they go to the hospital for preoperative screening tests. In this study, the preoperative HIV positive rates in the surgical patient population in 2018 was slightly higher than that reported by the China Centers for Disease Control and Prevention (62·6/100,000)12. The preoperative HIV positive rate in the surgical patient population increased steadily from 19·5 to 74·3 per 100,000, with an annual growth rate of 281% between 2009 and 2018. A study conducted in the Philippines between 2010 and 2018 reported a 203% increase in the incidence of new infections in the general population13 Encouragingly, in some sub-Saharan African countries, the substantial decreases underscore the enormous effort by governments and multilateral organizations to improve HIV infection prevention and provide effective treatment in these countries. For example, the HIV positive rate decreased by 10·2% (95% uncertainty interval [UI] −27·8 to −2·4) in Togo, 11·4% (95% UI −35·9% to 2·5%) in Uganda, and eSwatini reached the highest annual decrease in incidence at 21·8% (95% UI −36·1 to −15·1)14 In our study, the predicted HIV positive rate from 2019 to 2023 showed an overall decreasing trend in the next five years. These predicted results are compatible with the real world data in China that showed that HIV incidence was 5.096/100,000 in 2019, 4.4283/100,000 in 2020, 4.2669/100,000 in 202115,16,17 The Chinese government has put in much effort in HIV prevention and control, including extensive publicity and education, the safe management of blood products, the promotion and application of condoms, free antiviral treatment for HIV patients with financial difficulties, and free HIV antibody screening for all those who volunteer for HIV testing. In addition, free maternal-child blocking drugs are provided to pregnant women infected with HIV. The school fees for orphans of patients with AIDS were waived. HIV patients were provided care, assistance, and anti-discrimination. However, the overall situation of HIV prevention and control in China is still severe, and further efforts should be made to improve the pertinence and effectiveness of prevention and control strategies.
In the past ten years, there have been three major shifts in the route of HIV transmission in China: from high-risk groups to the entire population, from parenteral to sexual, and from predominantly rural areas to both rural and urban areas18 The general population, rather than the traditional high-risk groups (drug users, MSM, and CSWs) have gradually become the source of detected cases, making the control of HIV infection increasingly complex19,20 The present study showed that the annual growth rate of HIV infection among official staff (1508%) is four times higher than the average (382%), and that among unemployed persons (1153%) is three times higher than the average (382%). The average increasing rate of the moderately endemic area (2758%) was faster than that of the traditional highly endemic area (345%), which indicated that the HIV epidemic area in China is changing and more serious. In the present study, both the positive rate and speed of the annual growth rate in males were significantly higher than those in females. Drug use and tainted blood transfusions were the major infection routes early in the epidemic in China; however, over the past decade, the sexual route has become the major mode of transmission19,20,21,22 The official figures from the previous year indicated that 95% of individuals newly diagnosed with HIV infection in China contracted the virus through sexual transmission, with one-quarter occurring among MSM23 Data from the CNHS also demonstrated that both the positive rate and increasing rate in urban areas were higher than those in rural areas, consistent with previous studies18.
With an aging population, HIV infection also appears to be a trend of “aging”. The spread of HIV infection to people over 50 years of age constitutes a new epidemic trend24The CNHS showed that the development speed in the 50-years-and-over age group was higher than that in the 15-to-49-year age group, is primarily attributed to the prevalence of high-risk sexual behaviors, weak protective awareness, inadequate detection and diagnosis, and the combined effects of population aging and antiretroviral therapy extending the survival of infected persons25,26,27.
The CNHS revealed that the positive rates in city and county hospitals were higher than those in provincial hospitals; however, the annual growth rates of city-level and county-level hospitals were lower than that of the provincial hospitals. Both the positive rate and development speed in high-positive rate hospital departments were higher than in general hospital departments. These findings are consistent with the epidemiological characteristics of urban and sexual transmission.
Therefore, the fast-growing population infected by HIV, such as those older than 50 years, official staff, unemployed, living in an urban area, moderately endemic area, and visiting a high-risk hospital department. These rapidly growing population groups should have access to rational propaganda in a timely manner, popularize the basic knowledge of HIV infection prevention, and improve prevention awareness and ability among these people. New electronic technology is more involved in human life. Making friends on software makes people’s contact more convenient, which also provides a more hidden and convenient way for commercial transactions. Therefore, it is necessary to increase the number of preventive and control personnel.
Although the CNHS represents the first preoperative positive rate study of HIV infection conducted on the surgical patient population in China, there are some potential limitations that should be considered. First, hospitals rather than individuals were randomly selected using the sampling method, as selecting individuals randomly in each administrative village or neighborhood community directly using this method would not have been practical in China. Second, this study only used enzyme - linked immunosorbent assay (ELISA) for preoperative screening and did not perform PCR confirmation for all positive results. Therefore, there may have been missed infections in the window period, which is one of the limitations of this study. Future studies could incorporate PCR testing to improve accuracy.Third, some of the HIV infection case sample sizes were rather small due to the limited number of participants in some groups. For example, there were only three confirmed HIV infection cases among female medical workers. This resulted in a large random error in the estimated positive rate. Fourth, this study design is cross-sectional at the time of surgery, and no attempts at estimating the time of potential infection in HIV-positive subjects were made. Fifth, known HIV-infected people might not be referred for surgery for several reasons, thus representing a selection bias that was not addressed or acknowledged.
In conclusion, the CNHS represents the first national survey of preoperative HIV positive rate across the surgical patient population in China. The present study provides detailed information on the national preoperative HIV positive rates and growth speed in the last decades for both surgical patient populations and subgroups by factor of interest, which can now be used as an up-to-date database for national health care planning and preventive efforts in China.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization. Key facts and latest estimates on the global HIV epidemic [EB/OL]. [2021-09-30]. http://www.Who.int/hiv/data/en/
Mao, Y. et al. Development of a unified web-based National HIV/AIDS information system in China. Int. J. Epidemiol. 39(Suppl 2), ii79–ii89 (2010).
Wang, L. & Wang, N. HIV/AIDS epidemic and the development of comprehensive surveillance system in China with challenges. Chin. Med. J. (Engl). 123(23), 3495–3500 (2010).
Zhang, L., Chow, E. P., Zhang, J., Jing, J. & Wilson, D. P. Describing the Chinese HIV surveillance system and the influences of political structures and social stigma. Open. AIDS J. 6, 163–168 (2012).
Poon, A. N., Li, Z., Wang, N. & Hong, Y. Review of HIV and other sexually transmitted infections among female sex workers in China. AIDS Care. 23(Suppl 1), 5–25 (2011).
Sun, J. et al. Contributions of international Cooperation projects to the HIV/AIDS response in China. Int. J. Epidemiol. 39(suppl 2), 14–20 (2010).
Qian, H. Z., Vermund, S. H. & Wang, N. Risk of HIV/AIDS in China: subpopulations of special importance. Sex. Transm Infect. 81, 442–447 (2005).
Ministry of Health of the People’s Republic of China. China AIDS Response Progress Report. Beijing: Chinese Ministry of Health, 2012. (2012). http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_CN_Narrative_Report[1].pdf (accessed Sept 9, 2013).
Yu, E. S. et al. HIV infection and AIDS in China, 1985 through 1994. Am. J. Public. Health. 86(8), 1116–1122 (1996).
Jia, Y. et al. Estimates of HIV positive rate in a highly endemic area of China: Dehong Prefecture, Yunnan Province. Int. J. Epidemiol. 37(6), 1287–1296 (2008).
Reich, J., Yates, W. & Woolson, R. Kish method for mail survey respondent selection. Am. J. Public. Health. 76(2), 206 (1986).
NCAIDS, N. C. S. T. D. & China, C. D. C. Update on the AIDS/STD epidemic in China the third quarter of 2018. China J. AIDS STD. 24(11), 1075 (2018).
Devi, S. Stigma, politics, and an epidemic: HIV in the Philippines. Lancet 394(10215), 2139–2140 (2019).
Global & of, H. I. V. national incidence, positive rate, and mortality 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017.
National Bureau of Statistics of China. China Statistical Yearbook [EB/OL]. http://www.stats.gov.cn/tjsj/ndsj/
Shao, Y. & Jia, Z. Challenges and opportunities for HIV/AIDS control in China. Lancet 379(9818), 804 (2012).
Zhang, L. et al. HIV positive rate in China: integration of surveillance data and a systematic review. LANCET INFECT. DIS. 13(11), 955–963 (2013).
Chen, Y. et al. Changing epidemic of HIV and syphilis among resident and migrant men who have sex with men in Jiangsu, China. Sci. Rep. 7, 9478 (2017).
Li, X. et al. Changing the landscape of the HIV epidemic among MSM in China: results from three consecutive respondent-driven sampling surveys from 2009 to 2011. Biomed Res Int. ; 2014:563517. (2014).
McLaughlin, K. HIV infections are spiking among young gay Chinese. Science 355(6332), 1359 (2017).
Burki, T. HIV in China: a changing epidemic. Lancet Infect. Dis. 18(12), 1311–1312 (2018).
Wang, N. Some new trends of HIV/AIDS epidemic in China. China J. Epidemiol. 31(11), 1205–1209 (2010).
Palella, F. J. Jr et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl. J. Med. 338(6), 853–860 (1998).
Nogueras, M. et al. Epidemiological and clinical features, response to HAART, and survival in HIV infected patients diagnosed at the age of 50 or more. BMC Infect. Dis. 6, 159 (2006).
Greenbaum, A. H. et al. Effect of age and HAART regimen on clinical response in an urban cohort of HIV-infected individual. AIDS 22(17), 2331–2339 (2008).
Lacerda, H. R. & Kitner, D. Mortality of the elderly is still exceedingly high at diagnosis of AIDS despite favorable outcomes after highly active antiretroviral therapy in Recife, Brazil. Int. J. STD AIDS. 19(7), 450–454 (2008).
Wei, Y. B. et al. Pre-exposure prophylaxis for migration-associated HIV in China. Lancet Infect. Dis. 15(1), 18 (2015).
Funding
This study was supported by the Bejing-tianjin-hebei Basic Research Cooperation project (Grant No. J23007), 2025 government-funded clinical medicine talent cultivation project (ZF2025136). The funding source has no role in study design, conduction, data collection or statistical analysis.
Author information
Authors and Affiliations
Contributions
L.H, W.J, C.W, H.Z.Y are responsible for data collection and organization.L.D.Z, J.Y.M, X.X, Z.X.B, Q.J, L.T, Y.X.L are responsible for organizing and collecting information.Y.W.P.Z, L.Y.J, W.Z.H, Z.K, Z.N, S.Y, Y.S.F are responsible for follow-up work.M.L.N, R.Y.T, H.J.L, Z.X.L, W.Y, L.W.J are responsible for writing the main manuscript.Z.Y.Z is the Corresponding author.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board (IRB)(project number: Ke 2019-017-1). Given the retrospective nature of the research and the anonymized characteristics of the data, the IRB waived the requirement for informed consent. All data were de-identified and analyzed in strict compliance with ethical guidelines and data privacy regulations, ensuring patient privacy throughout the study.
Consent for publication
All authors agree to the publication of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lv, H., Wang, J., Zhang, Q. et al. National preoperative HIV prevalence in China: a retrospective analysis of 4,753,874 surgical patients. Sci Rep 15, 19712 (2025). https://doi.org/10.1038/s41598-025-03950-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03950-4