Abstract
Inflammatory responses are crucial for repairing radiation-induced tissue damage. Excessive tissue remodeling in response to severe tissue injury causes chronic inflammation associated with various diseases including cardiovascular disease and cancer. Fibroblasts are major components of the stroma and play key roles in tissue remodeling. However, causes of inflammatory response activation remain unclear. This study focused on cytosolic mitochondrial DNA (mtDNA) release and its role in inflammation following irradiation. Cytosolic mtDNA leakage increased 3 h after irradiation of normal human fibroblasts and persisted for at least 7 days. H2O2 treatment of fibroblasts increased reactive oxygen species (ROS) levels, the number of cytosolic DNA per cell, and the number of senescent cells, indicating that ROS trigger cytosolic DNA release in association with cellular senescence. The cytosolic mtDNA was then recognized by the DNA sensor cyclic GMP–AMP synthase (cGAS), activating the cGAS/stimulator of interferon genes (STING) signaling pathway. DNA-PK and AMPK inhibitors prevented cytosolic mtDNA release and its colocalization with cGAS following irradiation. Cytosolic and extracellular mtDNA release was also induced in mouse upon whole-body irradiation. Our results demonstrated that mitochondrial damage signals spread throughout the body via exosomes or as cell-free DNA. Released mtDNA act as danger signals that trigger inflammation.
Similar content being viewed by others
Introduction
Inflammation plays a crucial role in maintaining tissue homeostasis as a defense mechanism against tissue damage and foreign pathogens. Inflammatory responses facilitate tissue repair and adaptation to stress conditions by eliminating debris and dead cells1. Fibroblasts are major components of the stroma and play key roles in tissue homeostasis2. They are dormant under physiological conditions and are activated in response to tissue damage3. Upon activation, fibroblasts release inflammatory mediators, such as cytokines, chemokines, and growth factors4,5, to recruit immune cells to the affected site to facilitate tissue remodeling and wound healing. These immune cells associate with fibroblasts to maintain their activation5. When the healing process is completed, the inflammatory responses cease6.
Radiation-induced carcinogenesis is triggered by the accumulation of genetic changes following DNA damage from the initial radiation exposure, which induces mutations7. Mutations in epithelial cells can also arise from mitochondrial dysfunction induced by oxidative stress, thereby making these cells cancerous8. Radiation also alters multicellular interactions, contributing to establishment of the tumor microenvironment among tumor-associated stromal cells9. They play a significant role in the development of the tumor microenvironment. For instance, mitochondrial reactive oxygen species (ROS)-mediated activation of fibroblasts in tumors can transform these fibroblasts into cancer-associated fibroblasts (CAFs), which regulate tumor growth and progression4,5,10. Radiation-induced DNA damage activates multiple signaling pathways for DNA damage responses (DDR). In addition, the immune response is activated to eliminate the damaged cells. If damage signals persist in the case of severe injury, the inflammatory response shifts to excessive extracellular matrix deposition and fibrosis, leading to chronic inflammation11, which is associated with several diseases, including diabetes, cardiovascular disease, and cancer12. Therefore, mitochondrial dysfunction and subsequent chronic inflammatory responses play a role in tumor development. According to the bioinformatics based analyses, the interaction between DDR, inflammation and immunity is well discussed in another paper13. Several molecules have been identified as mediators of radiation-induced immune and/or inflammatory responses14. However, the causes of chronic inflammation activation remain unclear.
Ionizing radiation activates mitochondria to provide energy for the DNA damage response15, resulting in the generation of ROS, a byproduct of oxidative phosphorylation, in mitochondria. Excessive ROS generation due to the indirect effects of radiation can promote oxidative mitochondrial damage and are deleterious to cells16,17. ROS-induced mitochondrial damage was evident by Parkin-positive staining in irradiated cells18. The glutathione peroxidase (GPx) activator melatonin and mitoEbselen-2 scavenge ROS and prevent mitochondrial damage following radiation19. These results strongly suggest that irradiation-induced ROS generation causes mitochondrial damage. The effects of ROS-induced mitochondrial damage are not limited to mitochondria because of the release of mitochondrial contents into the cytoplasm20. Therefore, mitochondria, which are assumed to be sites of stress response initiation, maintain communication with the rest of the cell21. Ariyoshi et al. reported that x-rays induce exosome-like vesicles containing mitochondrial DNA (mtDNA)22. Thus, these vesicles facilitate the release of mtDNA from x-ray irradiated human cells into culture medium or mouse plasma from whole body irradiated mice. However, in this study, our focus was on the intracellular responses following mitochondrial damage. Damaged mtDNA leaks into the cytoplasm through mitochondrial membrane pores. The voltage-dependent anion channel (VDAC) in the outer mitochondrial membrane is a potential candidate for regulating mtDNA release. Damaged mtDNA, which is negatively charged, associates with the positively charged amino residues of VDAC, thereby facilitating mitochondrial pore opening via VDAC oligomerization23. In response to mtDNA release into the cytoplasm, cyclic GMP–AMP synthase (cGAS), a cytosolic DNA sensor, stimulates inflammatory responses via the second messenger cGAMP and the adaptor stimulator of interferon genes (STING)24. Activation of STING is under the control of its phosphorylation25. Furthermore, mtDNA serves as a damage-associated molecular pattern when released into circulation26. Therefore, the cytosolic release of mtDNA activates the innate immune system27.
This study aimed to assess the occurrence of mtDNA release and its role in response to post-radiation inflammation. We used several inhibitors of DNA damage responses to study the molecules associated with mtDNA release. Mice were used as animal models to study the in vivo effects of radiation.
Results
Radiation-induced release of MtDNA into the cytosol
Human fibroblast TIG-3 cells were irradiated at the indicated doses, and DNA was extracted from the cytosolic fraction after 24 h. mtDNA present in the cytosolic fraction was detected using quantitative PCR (qPCR) with primers for the mitochondrial genes ND1 and ND5. Radiation exposure increased the amount of mtDNA in the cytosol fraction compared to that of nonirradiated controls (Fig. 1a). Cytosolic DNA can be visualized via immunofluorescence using anti-double-stranded DNA (dsDNA) antibodies after treatment with plasma membrane permeabilization buffer28. Moreover, SYBR Gold nucleic acid stain dye at low concentrations preferentially labels mtDNA29. To detect cytosolic dsDNA of mitochondrial origin, we performed immunofluorescence staining using antibodies against DNA in conjunction with SYBR Gold. We detected the presence of cytosolic DNA in the irradiated cells, as evidenced by the SYBR Gold staining results (Fig. 1b, arrow). Moreover, we found an increase in the amount of cytosolic mtDNA upon radiation exposure, as demonstrated by the double-positive results for dsDNA antibodies and SYBR Gold staining (Fig. 1c). In irradiated cells, mtDNA accounted for approximately half of the cytosolic DNA, whereas the nonirradiated controls were negative for SYBR Gold staining (Fig. 1d).
mtDNA release in the cytoplasm following irradiation. (a) Cytosolic mtDNA levels were measured via qPCR using primers for mitochondrial genes (ND1 and ND5). DNA was isolated from the cytosolic fraction of cells 24 h after irradiation. The asterisk indicates a significant increase in the amount of cytosolic mtDNA compared with that of nonirradiated control cells. (b) Images of cytosolic DNA staining (red), SYBR Gold staining (green), and nuclear staining (blue) of nonirradiated control and irradiated (1 Gy) TIG-3 cells. The arrow indicates the colocalization of cytosolic DNA with SYBR Gold. Scale bar is 50 μm. (c) The amount of cytosolic DNA stained with SYBR Gold per cell is shown. The asterisk indicates a significant difference from that of nonirradiated control cells (*p < 0.05, **p < 0.01). (d) The ratio of SYBR Gold-stained cytosolic DNA to total cytosolic DNA is shown. The asterisk indicates a significant difference from nonirradiated control cells (*p < 0.05, **p < 0.01).
Dose response and persistence of cytosolic DNA after irradiation
To determine the timing of cytosolic DNA appearance, cytosolic DNA from TIG-3 and MRC-5 cells was detected using dsDNA antibodies at time points up to 24 h following irradiation. Cytosolic DNA was detectable at 3 h after irradiation at levels that were significantly higher levels (p < 0.01) than the control levels. The cytosolic DNA levels continued to increase over 24 h (Fig. 2a). The duration of cytosolic DNA persistence was determined by tracking daily changes in cytosolic DNA levels for 1 week following irradiation. In TIG-3 cells exposed to either 1- or 5-Gy irradiation, cytosolic DNA persisted for at least 7 days post-irradiation (Fig. 2b). We then investigated the relationship between cytosolic DNA release and radiation dose (Fig. 2c). Compared to nonirradiated control cells, the number of cytosolic DNA per cell in irradiated cells peaked at a dose of approximately 1 Gy and then plateaued at doses of > 1 Gy. To determine whether cell proliferation is necessary for cytosolic DNA release, cells were cultured in 0.2% serum to suppress cell proliferation. Radiation did not induce cytosolic DNA release in nonproliferating cells cultured under low serum conditions (Fig. 2d).
Time course and dose response of radiation-induced cytosolic DNA release. (a) The amount of cytosolic DNA per cell at the indicated time after exposure to radiation. (b) Long-term persistence of cytosolic DNA after irradiation. (c) Dose response of cytosolic DNA release 24 h after irradiation. (d) Effects of low serum concentrations on radiation-induced cytoplasmic DNA release. The asterisk indicates a significant change in the amount of cytosolic DNA compared with nonirradiated control cells (*p < 0.05, **p < 0.01).
ROS-mediated induction of cytosolic DNA release
The release of mtDNA into the cytosol is assumed to be caused by mitochondrial-derived ROS, given that ROS at high levels can oxidize mtDNA to produce mtDNA fragments30. To increase ROS levels, cells were treated with H2O2 at the indicated concentrations for 1 h, washed, and then incubated in fresh medium for 2 days. The results of 2′,7′-dichlorofluorescin diacetate (DCFDA) staining, an indicator for ROS showed no significant difference(*p < 0.05, **p < 0.01) in the ROS levels between untreated control cells and cells treated with 10 µM H2O2, indicating that at this concentration of H2O2, cells could recover from oxidative stress. In contrast, the ROS levels of cells treated with > 50 µM H2O2 were significantly higher than those of control cells (Fig. 3a). ROS also have the ability to induce cell senescence. ROS-induced cytosolic DNA release and cellular senescence were assessed via immunofluorescence using anti-dsDNA and β-gal staining in TIG-3 and MRC-5 cells following H2O2 treatment (Fig. 3b). Cells treated with > 50 µM H2O2 exhibited increased cytosolic DNA levels compared with untreated cells (Fig. 3c), indicating that ROS generation is associated with mtDNA release. β-gal staining results revealed that H2O2 treatment led to the senescence of cells harboring cytosolic DNA (Fig. 3d and e). We have previously reported that exposure to ionizing radiation increases ROS levels in TIG-3 cells18,31. Although irradiation induced senescence to a lesser extent than H2O2 treatment (Fig. 3d), it induced cytosolic DNA release in association with cellular senescence (Fig. 3e).
ROS-mediated cytosolic DNA release and cellular senescence. (a) ROS levels were measured by DCFDA staining of cells treated with H2O2 at the indicated concentrations. The fluorescence intensities of DCFDA were normalized to the control values. The asterisk indicates a significant increase in ROS levels compared with nonirradiated control cells(*p < 0.05, **p < 0.01). (b) Images of β-gal staining (green), cytosolic DNA staining (red) and nuclear staining (blue) following H2O2 treatment or 1-Gy-irradiation of TIG-3 cells. Scale bar is 50 μm. (c) Induction of cytosolic DNA release following H2O2 treatment. The asterisk indicates a significant increase in the amount of cytosolic DNA compared with nonirradiated control cells (*p < 0.05, **p < 0.01). (d) Induction of cellular senescence by H2O2 treatment and X-ray irradiation. The asterisk indicates a significant increase in the percentage of senescent cells compared with nonirradiated control cells. (e) Association between cytosolic DNA and cellular senescence. The asterisk indicates a significant increase in the number of senescent cells harboring cytosolic DNA compared with nonirradiated control cells (*p < 0.05, **p < 0.01).
cGAS and phosphorylated STING colocalize with cytosolic DNA
mtDNA located outside the mitochondria is identified as bacterial DNA due to its distinct structural features compared to that of nuclear DNA32. cGAS is a DNA sensor that recognizes cytoplasmic mtDNA and triggers an inflammatory response33. The cellular localization of cGAS was investigated by immunostaining irradiated cells with antibodies against cGAS and dsDNA. cGAS was accumulated around some of the cytosolic DNA in irradiated TIG-3 and MRC-5 cells (Fig. 4a, arrowhead). Phosphorylated STING, assayed via immunostaining, was also accumulated around some of the cytosolic DNA in irradiated cells (Fig. 4b, arrowhead). In cells irradiated with 0.1–0.5 Gy of X-rays, no accumulation of cGAS or phosphorylated STING was detected around cytosolic DNA. However, colocalization of cytosolic DNA with cGAS and phosphorylated STING was observed in both TIG-3 and MRC-5 cells exposed to doses of ≥ 1 Gy (Fig. 4a and b right graph).
Activation of cGAS/STING signaling by radiation-induced cytosolic DNA. (a) Images of cytosolic DNA (red), cGAS (green), and nuclear (blue) staining of nonirradiated control and 1-Gy-irradiated TIG-3 cells. The arrow and arrowhead indicate cGAS-negative and cGAS-positive cytosolic DNA, respectively. Scale bar is 50 μm. (b) Images of cytosolic DNA (red) and phosphorylated STING (green) staining of nonirradiated control and 1-Gy-irradiated TIG-3 cells. The arrow and arrowhead indicate phosphorylated-STING-negative and phosphorylated-STING-potitive cytosolic DNA, respectively. Scale bar is 50 μm. The number of cells positive for both cytosolic DNA and cGAS or for both cytosolic DNA and phosphorylated STING is shown in the right graphs. The asterisk indicates a significant difference between nonirradiated and irradiated cells in each inhibitor group (*p < 0.05, **p < 0.01).
Mitochondrial transcription factor A (TFAM) is known to bind tightly to mtDNA34. Therefore, it is likely that cGAS allows cytosolic mtDNA associated with TFAM to be distinguished from other releases such as nuclear DNA. Double immunostaining with cGAS and TFAM antibodies in Fig. 5 shows the co-localization of cGAS and TFAM in 5 Gy-irradiated cells (Fig. 5a). After irradiation, the number of TFAM-positive cGAS was 2.5 times higher than the number of TFAM-negative cGAS, suggesting that cytosolic mtDNA may be associated with activation of the cGAS pathway (Fig. 5b). Therefore, cytoplasmic DNA positive for cGAS or phosphorylated STING may be of mitochondrial origin.
Co-localization of TFAM and cGAS in irradiated cells. (a) Images of TFAM (red), cGAS (green), and nuclear (blue) staining of nonirradiated control and 5-Gy-irradiated TIG-3 cells. The arrow and arrowhead indicate TFAM-negative and TFAM-positive cGAS, respectively. Scale bar is 50 μm. (b) The number of cells positive for both TFAM and cGAS is shown in the right graphs. The asterisk indicates a significant increase in in the number o cGAS in irradiated cells compared to nonirradiated cells (*p < 0.05, **p < 0.01).
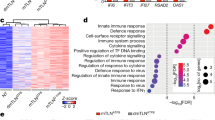
Loss of radiation-induced cytosolic DNA release by inhibiting DNA-PK or AMPK
To explore the underlying mechanism of radiation-induced cytosolic DNA release in cGAS-positive cells, several inhibitors were used to inactivate DNA damage responses (Fig. 6a). Ataxia telangiectasia-mutated (ATM) functions as a master transducer of DNA damage signals to relevant effectors. Protein kinase B (PKB)/Akt regulates cell survival in response to severe radiation-induced DNA damage. The inhibitors of Akt and ATM both enhanced the accumulation of cytosolic DNA following irradiation (Fig. 6b). Colocalization of cGAS with dsDNA was observed in cells exposed to radiation alone, radiation plus ATM inhibitor, and radiation plus Akt inhibitor (Fig. 6c). DNA-PK is a DNA repair protein that regulates non-homologous end joining. AMPK acts as a cellular energy sensor and is believed to transmit DNA damage signals to the mitochondria. The inhibitors of DNA-PK and AMPK both prevented an increase in cytosolic DNA levels following irradiation (Fig. 6b). Pre-irradiation treatment with DNA-PK or AMPK inhibitors did not result in the colocalization of cGAS with cytosolic DNA (Fig. 6c).
Suppression of radiation-induced colocalization of cytosolic DNA with cGAS by inhibiting DNA-PK or AMPK. (a) Images of cytosolic DNA (red), cGAS (green) and nuclear (blue) staining in the indicated TIG-3 cell samples. Cells were treated with the indicated inhibitors for 2 h before irradiation. Scale bar is 50 μm. (b) The amount of cytosolic DNA per cell is shown in the graph. The asterisk indicates a significant difference between nonirradiated and irradiated cells in each inhibitor group (*p < 0.05, **p < 0.01). (c) The number of cells positive for both cytosolic DNA and cGAS is shown in the graph. The asterisk indicates a significant difference between nonirradiated and irradiated cells in each inhibitor group (*p < 0.05, **p < 0.01).
Induction of cytosolic DNA release by radiation in vivo
The in vivo effects of radiation were studied in mice exposed to whole-body X-ray radiation. To examine dose- and time-dependent cellular responses in vivo, we preferred to test lymphocytes, which can be immediately harvested by blood collection. Blood mononuclear cells were isolated from mouse whole blood at 1, 3, and 7 days following irradiation and subjected to fluorescence immunostaining using antibodies against dsDNA. Cytosolic DNA staining was observed in the cytoplasm of mouse lymphocytes around the nuclei (Fig. 7a). The fluorescence intensity of cytosolic DNA, as determined by selecting the area stained with anti-dsDNA, increased in cells exposed to > 1 Gy radiation compared with that of nonirradiated control cells (Fig. 7b). Radiation-induced cytosolic DNA accumulation was observed in mouse lymphocytes for up to 3 days following 1-Gy irradiation but returned to control levels by day 7. Induction of cytosolic DNA release was more pronounced in 5-Gy-irradiated mouse lymphocytes than in 1-Gy-irradiated mouse lymphocytes. The increased cytosolic DNA levels persisted for at least 7 days in mouse lymphocytes after 5-Gy irradiation (Fig. 7c). Therefore, radiation-induced cytoplasmic mtDNA leakage was also detected in mouse blood cells in vivo. However, further studies are necessary to clarify the in vivo data with the use of fibroblasts instead of lymphocytes.
Induction of cytosolic DNA release in mice. (a) Images of cytosolic DNA staining (red) in mouse lymphocytes. Scale bar is 50 μm. (b) Fluorescence intensity of cytosolic DNA staining 1 day following irradiation at the indicated doses. (c) Fluorescence intensity of cytosolic DNA staining at 1, 3, and 7 days post-irradiation. The asterisk indicates a significant increase in the fluorescence intensity of irradiated cells compared with that of nonirradiated control cells (*p < 0.05, **p < 0.01). Exosome mtDNA levels (d) and cell-free mtDNA levels (e) were measured via qPCR using primers for mitochondrial genes (ND1 and ND5). DNA was isolated from non-irradiated and irradiated mouse plasma on day 1 and day 7. The asterisk indicates a significant increase in the amount of exosomal mtDNA or cell-free mtDNA compared with that of nonirradiated control cells.
To determine whether mtDNA is released extracellularly, exosome DNA and cell-free DNA were isolated from non-irradiated and irradiated mouse plasma using a commercially available XCF™ complete exosome and cDNA isolation kit. The relative levels of the mitochondrial genes ND1 and ND5 were determined using SYBR Green-based qPCR. Compared to nonirradiated controls, radiation increased plasma extracellular mtDNA levels both in exosomes and as cell-free DNA, which persisted for at least for 7 days after irradiation (Fig. 7d and e).
Methods
Cell culture and irradiation
Normal diploid human fetal lung-derived fibroblasts TIG-3 and MRC-5 were obtained from the Human Science Foundation for Reconstruction and RIKEN Cell Bank (Tsukuba, Japan), respectively, and cultured in alpha-MEM supplemented with 10% fetal bovine serum and penicillin/streptomycin.
The cells were exposed to 150-kVp X-rays, filtered through 0.5-mm Cu and 0.1-mm Al filters, at a dose rate of 0.8 Gy/min using an X-ray irradiator (Akro-Bio; AB-160). Inhibitors of ATM (1 µM KU55933) and DNA-PK (10 µM NU7016) were purchased from Sigma (San Diego, CA, USA). AKT inhibitor (20 µM API-2) and AMPK inhibitor (5 µM dorsomorphin) were purchased from Millipore and MedChemExpress, respectively. These inhibitors were dissolved in dimethyl sulfoxide (DMSO) and added to the media 2 h before irradiation at the indicated doses.
Real-time PCR
The cytosolic fraction was separated by Mitochondria isolation kit for cultured cells (Thermo Fisher). We previously reported successful cytosolic and mitochondrial fractionation using this commercially available kit18. Subsequently, cytosolic DNA was isolated from the cytosolic fraction using a QIAquick Nucleotide Removal Kit (Qiagen, Hilden, Germany), and 50 ng of DNA was amplified. The relative levels of the mitochondrial genes ND1 and ND5 were determined using SYBR Green-based qPCR with a human mtDNA monitoring primer set (Takara Bio Inc.) according to the manufacturer’s instructions (Biorad, CFX Connect Real Time System). The comparative cycle threshold (2−ΔΔCt) method was used to calculate relative gene expression. Since the cytosolic DNA was not amplified with the human nuclear DNA primers SERPINA1 and SLCO2B1, the relative gene expression as shown by compared with the non-irradiated control samples as 1.
SYBR gold staining
SYBR Gold™ was diluted 1:10,000 in DMSO to prepare a stock solution, which was further diluted to 1:1,000 in the culture medium. Cells were incubated with the dye for 30 min at 37 °C, washed with phosphate-buffered saline (PBS) (-), and fixed with 2% paraformaldehyde for 10 min. The colocalization of SYBR Gold with cytosolic DNA was examined via immunofluorescence staining as described below.
Immunofluoresence
Cells (1.0 × 105) were seeded in 35-mm dishes with cover glasses and incubated overnight. After X-ray irradiation, cells were fixed using 4% paraformaldehyde (Nakalai Tesque) for 10 min at room temperature, washed with PBS (-) (Nakalai Tesque), and treated with 0.01% Tween for 10 min at room temperature to permeabilize the membranes. The blocking step was performed for 1 h at room temperature using 1% fetal bovine albumin dissolved in PBS (-). The cells were then incubated overnight with the primary antibody in a humid environment, following by incubation with the secondary antibody for 1 h at room temperature. Primary antibodies against dsDNA (ab27156; Abcam), cGAS (79978; Cell Signaling), and phosphorylated STING (19781; Cell Signaling), and secondary antibodies conjugated to Alexa Fluor 488 (A11034; Molecular Probes, Eugene, OR, USA) or Alexa Fluor 647 (A21236; Molecular Probes) were used. Subsequently, the cell nuclei were stained with 4 µg/ml Hoechst. Fluorescence images were acquired using a Keyence BZ-X810 fluorescence microscope (Keyence Corporation, Osaka, Japan). At least 100 cells were counted for each slide. Image analysis was performed using the Hybrid Cell Count software (BZ-II Analyzer; Keyence Corporation).
H2O2 treatment
Cells were treated with H2O2 for 1 h at the indicated dose, washed with PBS (-), and then cultured for 2 days.
ROS measurements
Cells (2.0 × 105) were seeded in a flask and cultured overnight, following which, they were stained with 5 µM DCFDA (Sigma) for 30 min. The fluorescence intensities of DCFDA were measured using a FACScan automated flow cytometer (Becton, Dickinson and Company, Franklin Lakes, NJ, USA). The fluorescence intensity was normalized to that of control cells.
β-gal staining
Cells (1.0 × 105) were seeded in 35-mm dishes with cover glasses and incubated overnight, following which they were washed with PBS (-) and fixed with 4% paraformaldehyde at room temperature for 3 min. β-Gal staining was then performed using a cell senescence detection kit as per the manufacturer’s instructions (SG03; Dojindo).
Animal experiments
All animal experiments were approved by the Animal Ethical Committee of the National Institute of Public Health (NIPH31-008) and performed in accordance with the ARRIVE guidelines and regulations of the Japan National Institute of Public Health. Five-week-old, C57BL/6NCrSlc male mice were obtained from Japan SLC (Shizuoka, Japan) and housed in an experimental animal laboratory under controlled temperature and pathogen-free conditions. They were provided with ad libitum access to standard laboratory food and water. The mice were divided into nine groups including non-treated control (n = 14), 0.1 (n = 8), 0.5 (n = 8), 1 (n = 12), and 5 Gy (n = 7) on day 1, and 1 Gy on days 3 (n = 6) and 7 (n = 6), and 5 Gy on days 3 (n = 5) and 7 (n = 6). Mice exhibiting a decline of at least 20% of their initial body weight were sacrificed, and the experiment was terminated. Euthanasia was performed using carbon dioxide. No mice died before the completion of the experiment. The mice were anesthetized with an intraperitoneal injection of ketamine (100 mg/kg) and xylazine (10 mg/kg) reconstituted in PBS. Heparinized blood samples were collected from the hearts of mice via cardiac puncture on days 1, 3, and 7 after irradiation. The mice were then sacrificed by cervical dislocation.
Exosome DNA and cell-free DNA isolation from mouse plasma
Heparinized blood samples were obtained from the nonirradiated control (n = 6) and irradiated groups (each n = 4) as described before. Blood cells were removed by the centrifugation at 3000 g for 15 min and obtained mouse plasma. The XCF™ complete exosome and cDNA isolation kit (System Biosciences) was used to separate exosome DNA from cell-free DNA. Subsequently, cell-free DNA was isolated using a QIAquick Nucleotide Removal Kit (Qiagen, Hilden, Germany) and 2.5 ng of DNA was amplified.
Statistical analyses
Error bars represent standard deviation (SD) obtained from at least three independent experiments involving cultures that were seeded and treated separately and mice treated individually. Differences among three or more groups were assessed using analysis of variance (ANOVA), with subsequent pairwise comparisons made via post hoc Dunnett’s tests. All statistical analyses were performed using Microsoft Excel. Statistical significance is indicated in the figures by an asterisk as follows: *p < 0.05, **p < 0.01.
Discussion
ROS are generated as part of the host defense response and serve as both signaling molecules and mediators of inflammation35. However, ROS also exhibit harmful effects due to oxidative stress. In contrast to the nuclear genome, the mitochondrial genome is too small to be directly damaged by radiation. Mitochondria are vulnerable to damage by ROS because they are primarily generated in mitochondria during oxidative phosphorylation36. ROS-mediated damage to mtDNA occurs as an indirect and delayed effect of ionizing radiation, resulting in the degradation of mtDNA, which is then released into the cytoplasm as an mtDNA damage signal37. Our qPCR analysis using primers specific for mitochondrial genes revealed the presence of mtDNA in the cytosolic fraction outside the mitochondria after irradiation. In addition, double staining with anti-dsDNA and SYBR Gold revealed that approximately half of the radiation-induced cytosolic DNA was mtDNA. Cytosolic DNA release was induced within the first 24 h following irradiation at > 1 Gy and persisted for at least 1 week. Radiation-induced cytosolic DNA release was also observed in mouse lymphocytes for several days following whole-body irradiation of mice. High radiation doses are expected to lead to higher ROS generation and mtDNA damage than low doses38. However, the dose response of cytosolic DNA release to radiation exhibited a nonlinear response, peaking at approximately 1 Gy, with no further increase in cytosolic DNA levels at doses above 1 Gy. This radiation dose-independent phenomenon may be caused by mitochondrial quality control mechanisms that play a role in eliminating dysfunctional mitochondria. We previously reported that high-dose radiation markedly induces Parkin-mediated mitophagy38. The resultant degradation of dysfunctional mitochondria may prevent mtDNA release39. For in vitro experiments, cells are generally allowed to grow exponentially by culturing in 10% serum. In vivo, fibroblasts are in a quiescent state; hence, we investigated the radiation response under conditions that limit cell proliferation by culturing cells in medium containing low serum (0.2%). We found that radiation did not induce cytosolic DNA release in nonproliferating cells cultured under low serum conditions. Therefore, cell growth suppression affects the release of mtDNA into the cytoplasm. In addition, high-dose radiation severely suppressed cell proliferation and delayed recovery. These results indicate that cytosolic DNA release is associated with cell regrowth.
High levels of ROS generated by 1 h H2O2 treatment led to increased cytosolic DNA levels in human fibroblasts. H2O2 treatment also induced cellular senescence, as evidenced by the presence of β-gal-positive cells, which contained cytosolic DNA. Cytosolic DNA accumulation is associated with cellular senescence40. Our results indicate that ROS are associated with the leakage of large amounts of DNA into the cytosol and induction of cellular senescence.
Unresponsiveness to DNA damage upon treatment with ATM or Akt inhibitors before irradiation can result in increased mtDNA damage in irradiated cells. Inhibition of ATM triggers mtDNA leakage into the cytosol and activates cGAS/STING signaling in cancer cells41. Furthermore, treatment with inhibitors of the PI3K/Akt pathway prevents Nrf2-dependent antioxidant gene expression42. The cytosolic DNA levels increased in response to pre-radiation treatment with these inhibitors compared to that observed with irradiation alone. In contrast, DNA-PK and AMPK inhibitors prevented the increase in cytosolic DNA levels following irradiation. The DNA-PK catalytic subunit (DNA-PKcs) forms a complex with adenine nucleotide translocase 2 (ANT2) and voltage-dependent anion channel 2 (VDAC2) for maintaining the mitochondrial membrane potential (MMP) necessary for oxidative phosphorylation. DNA-PKcs phosphorylation in response to oxidative stress leads to disruption of this complex43. AMPK functions as a cellular energy sensor and is a key regulator of mitochondrial damage responses44. Moreover, DNA-PK and AMPK are involved in mitochondrial maintenance. However, further studies are needed to determine the molecular mechanisms underlying the release of mtDNA into the cytoplasm.
mtDNA release into the cytoplasm is assumed to trigger the innate immune system. Radiation induces cytosolic DNA release, which in turn activates the cGAS/STING signaling pathway. DNA-PK phosphorylates cGAS to prevent its DNA sensing activity45. DNA-PK inhibitor prevents the colocalization of cGAS with cytosolic DNA. The transmission of mtDNA-mediated danger signals is not limited to the cell because exosomes can facilitate the removal of mtDNA from cells22. Analysis of the real-time PCR data indicated that mtDNA was extracellularly shed into mouse plasma after irradiation. Both exosomal mtDNA and cell-free mtDNA were increased after irradiation, suggesting their involvement in inflammatory signaling as mitochondrial damage-associated molecular patterns (DAMPs)46,47. Note that radiation increased plasma extracellular mtDNA levels, which persisted for at least for 7 days after irradiation. Radiation-induced mtDNA in the exosomes induces DNA damage in treated cells as part of the radiation-induced bystander effect22. These results suggest that radiation-induced mtDNA release is not only mediated by a direct cellular response to radiation, but also involves systemic mechanisms, including a radiation-induced inflammatory signaling as mitochondrial DAMPs. In addition, elevated levels of blood cell-free mtDNA have been reported to be associated with various diseases and acute psychological stress48,49. Thus, the release of mtDNA is not only a result of radiation exposure.
Mitochondria possess signaling capacity to determine the fate of the cell. Hence, when ionizing radiation mediates mitochondrial damage, the effects are not limited to the mitochondria because of the release of various components from mitochondria. Mitochondrial damage signals spread throughout the body as mitochondrial DAMP. Therefore, mitochondrial dysfunction causes induction of stress responses and the released mtDNA fragments act as danger signals that trigger inflammation.
Data availability
The data presented in this study are available on request to the corresponding author.
References
Chovatiya, R. & Medzhitov, R. Stress, inflammation, and defense of homeostasis. Mol. Cell. 54, 281–288. https://doi.org/10.1016/j.molcel.2014.03.030 (2014).
Darby, I. A., Laverdet, B., Bonté, F. & Desmoulière, A. Fibroblasts and myofibroblasts in wound healing. Clin. Cosmet. Invest. Dermatology. 7, 301–311. https://doi.org/10.2147/ccid.s50046 (2014).
Kalluri, R. The biology and function of fibroblasts in cancer. Nat. Rev. Cancer. 16, 582–598. https://doi.org/10.1038/nrc.2016.73 (2016).
Shimura, T. et al. Radiation-Induced myofibroblasts promote tumor growth via mitochondrial ROS-Activated TGFβ signaling. Mol. cancer Research: MCR. 16, 1676–1686. https://doi.org/10.1158/1541-7786.mcr-18-0321 (2018).
Van Linthout, S., Miteva, K. & Tschöpe, C. Crosstalk between fibroblasts and inflammatory cells. Cardiovascular. Res. 102, 258–269. https://doi.org/10.1093/cvr/cvu062 (2014).
Serhan, C. N. & Savill, J. Resolution of inflammation: the beginning programs the end. Nat. Immunol. 6, 1191–1197. https://doi.org/10.1038/ni1276 (2005).
Little, J. B. Radiation carcinogenesis. Carcinogenesis 21, 397–404. https://doi.org/10.1093/carcin/21.3.397 (2000).
Federico, A., Morgillo, F., Tuccillo, C., Ciardiello, F. & Loguercio, C. Chronic inflammation and oxidative stress in human carcinogenesis. Int. J. Cancer. 121, 2381–2386. https://doi.org/10.1002/ijc.23192 (2007).
Barcellos-Hoff, M. H. & Nguyen, D. H. Radiation carcinogenesis in context: how do irradiated tissues become tumors? Health Phys. 97, 446–457. https://doi.org/10.1097/HP.0b013e3181b08a10 (2009).
Caligiuri, G. & Tuveson, D. A. Activated fibroblasts in cancer: perspectives and challenges. Cancer Cell. 41, 434–449. https://doi.org/10.1016/j.ccell.2023.02.015 (2023).
Ueha, S., Shand, F. H. & Matsushima, K. Cellular and molecular mechanisms of chronic inflammation-associated organ fibrosis. Front. Immunol. 3, 71. https://doi.org/10.3389/fimmu.2012.00071 (2012).
Ferrucci, L. & Fabbri, E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 15, 505–522. https://doi.org/10.1038/s41569-018-0064-2 (2018).
Pateras, I. S. et al. The DNA damage response and immune signaling alliance: is it good or bad? Nature decides when and where. Pharmacol. Ther. 154, 36–56. https://doi.org/10.1016/j.pharmthera.2015.06.011 (2015).
Georgakilas, A. G. et al. Emerging molecular networks common in ionizing radiation, immune and inflammatory responses by employing bioinformatics approaches. Cancer Lett. 368, 164–172. https://doi.org/10.1016/j.canlet.2015.03.021 (2015).
Yamamori, T. et al. Ionizing radiation induces mitochondrial reactive oxygen species production accompanied by upregulation of mitochondrial electron transport chain function and mitochondrial content under control of the cell cycle checkpoint. Free Radic. Biol. Med. 53, 260–270. https://doi.org/10.1016/j.freeradbiomed.2012.04.033 (2012).
Murphy, M. P. How mitochondria produce reactive oxygen species. Biochem. J. 417, 1–13. https://doi.org/10.1042/bj20081386 (2009).
Ziech, D., Franco, R., Pappa, A. & Panayiotidis, M. I. Reactive oxygen species (ROS)--induced genetic and epigenetic alterations in human carcinogenesis. Mutat. Res. 711, 167–173. https://doi.org/10.1016/j.mrfmmm.2011.02.015 (2011).
Shimura, T. et al. ATM-mediated mitochondrial damage response triggered by nuclear DNA damage in normal human lung fibroblasts. Cell. Cycle. 16, 2345–2354. https://doi.org/10.1080/15384101.2017.1387697 (2017).
Shimura, T., Shiga, R., Sasatani, M., Kamiya, K. & Ushiyama, A. Melatonin and MitoEbselen-2 are radioprotective agents to mitochondria. Genes 14, 142. https://doi.org/10.3390/genes14010045 (2022).
Shimura, T. Mitochondrial signaling pathways associated with DNA damage responses. Int. J. Mol. Sci. 24, 859. https://doi.org/10.3390/ijms24076128 (2023).
Chandel, N. S. Mitochondria as signaling organelles. BMC Biol. 12, 34. https://doi.org/10.1186/1741-7007-12-34 (2014).
Ariyoshi, K. et al. Radiation-Induced bystander effect is mediated by mitochondrial DNA in Exosome-Like vesicles. Sci. Rep. 9, 9103. https://doi.org/10.1038/s41598-019-45669-z (2019).
Kim, J. et al. VDAC oligomers form mitochondrial pores to release MtDNA fragments and promote lupus-like disease. Sci. (New York N Y). 366, 1531–1536. https://doi.org/10.1126/science.aav4011 (2019).
Chen, Q., Sun, L. & Chen, Z. J. Regulation and function of the cGAS-STING pathway of cytosolic DNA sensing. Nat. Immunol. 17, 1142–1149. https://doi.org/10.1038/ni.3558 (2016).
Zhang, C. et al. Structural basis of STING binding with and phosphorylation by TBK1. Nature 567, 394–398. https://doi.org/10.1038/s41586-019-1000-2 (2019).
Zhang, Q. et al. Circulating mitochondrial damps cause inflammatory responses to injury. Nature 464, 104–107. https://doi.org/10.1038/nature08780 (2010).
Newman, L. E. & Shadel, G. S. Mitochondrial DNA release in innate immune signaling. Annu. Rev. Biochem. 92, 299–332. https://doi.org/10.1146/annurev-biochem-032620-104401 (2023).
Sato, A. et al. Immunofluorescence microscopy-based assessment of cytosolic DNA accumulation in mammalian cells. STAR. Protocols. 2, 100488. https://doi.org/10.1016/j.xpro.2021.100488 (2021).
Jevtic, V., Kindle, P. & Avilov, S. V. SYBR gold dye enables Preferential labelling of mitochondrial nucleoids and their time-lapse imaging by structured illumination microscopy. PloS One. 13, e0203956. https://doi.org/10.1371/journal.pone.0203956 (2018).
Shokolenko, I., Venediktova, N., Bochkareva, A., Wilson, G. L. & Alexeyev, M. F. Oxidative stress induces degradation of mitochondrial DNA. Nucleic Acids Res. 37, 2539–2548. https://doi.org/10.1093/nar/gkp100 (2009).
Shimura, T. et al. Mechanism of turnover or persistence of radiation-induced myofibroblast in vitro. Cell. Cycle. 19, 3375–3385. https://doi.org/10.1080/15384101.2020.1848063 (2020).
Boguszewska, K., Szewczuk, M., Kaźmierczak-Barańska, J. & Karwowski, B. T. The similarities between human mitochondria and Bacteria in the context of structure, genome, and base excision repair system. Mol. (Basel Switzerl.) 25, 563. https://doi.org/10.3390/molecules25122857 (2020).
West, A. P. & Shadel, G. S. Mitochondrial DNA in innate immune responses and inflammatory pathology. Nat. Rev. Immunol. 17, 363–375. https://doi.org/10.1038/nri.2017.21 (2017).
Alam, T. I. et al. Human mitochondrial DNA is packaged with TFAM. Nucleic Acids Res. 31, 1640–1645. https://doi.org/10.1093/nar/gkg251 (2003).
Mittal, M., Siddiqui, M. R., Tran, K., Reddy, S. P. & Malik, A. B. Reactive oxygen species in inflammation and tissue injury. Antioxid. Redox. Signal. 20, 1126–1167. https://doi.org/10.1089/ars.2012.5149 (2014).
Kowaltowski, A. J., de Souza-Pinto, N. C., Castilho, R. F. & Vercesi, A. E. Mitochondria and reactive oxygen species. Free Radic. Biol. Med. 47, 333–343. https://doi.org/10.1016/j.freeradbiomed.2009.05.004 (2009).
Riley, J. S. & Tait, S. W. Mitochondrial DNA in inflammation and immunity. EMBO Rep. 21, e49799. https://doi.org/10.15252/embr.201949799 (2020).
Shimura, T. et al. Effects of oxygen on the response of mitochondria to X-irradiation and reactive oxygen species-mediated fibroblast activation. Int. J. Radiat. Biol. 99, 769–778. https://doi.org/10.1080/09553002.2023.2142980 (2023).
Wasner, K. et al. Parkin deficiency impairs mitochondrial DNA dynamics and propagates inflammation. Mov. Disorders: Official J. Mov. Disorder Soc. 37, 1405–1415. https://doi.org/10.1002/mds.29025 (2022).
Takahashi, A. et al. Downregulation of cytoplasmic DNases is implicated in cytoplasmic DNA accumulation and SASP in senescent cells. Nat. Commun. 9, 1249. https://doi.org/10.1038/s41467-018-03555-8 (2018).
Hu, M. et al. ATM Inhibition enhances cancer immunotherapy by promoting MtDNA leakage and cGAS/STING activation. J. Clin. Investig. 131, 369. https://doi.org/10.1172/jci139333 (2021).
Wang, L., Chen, Y., Sternberg, P. & Cai, J. Essential roles of the PI3 kinase/akt pathway in regulating Nrf2-dependent antioxidant functions in the RPE. Investig. Ophthalmol. Vis. Sci. 49, 1671–1678. https://doi.org/10.1167/iovs.07-1099 (2008).
Chen, W. M. et al. DNA-PKcs and ATM modulate mitochondrial ADP-ATP exchange as an oxidative stress checkpoint mechanism. EMBO J. 42, e112094. https://doi.org/10.15252/embj.2022112094 (2023).
Shimura, T. et al. Nuclear DNA damage-triggered ATM-dependent AMPK activation regulates the mitochondrial radiation response. Int. J. Radiat. Biol. 100, 584–594. https://doi.org/10.1080/09553002.2023.2295297 (2024).
Sun, X. et al. DNA-PK deficiency potentiates cGAS-mediated antiviral innate immunity. Nat. Commun. 11, 6182. https://doi.org/10.1038/s41467-020-19941-0 (2020).
Grazioli, S. & Pugin, J. Mitochondrial Damage-Associated molecular patterns: from inflammatory signaling to human diseases. Front. Immunol. 9, 45. https://doi.org/10.3389/fimmu.2018.00832 (2018).
Nakahira, K., Hisata, S. & Choi, A. M. The roles of mitochondrial Damage-Associated molecular patterns in diseases. Antioxid. Redox. Signal. 23, 1329–1350. https://doi.org/10.1089/ars.2015.6407 (2015).
Trumpff, C. et al. Stress and Circulating cell-free mitochondrial DNA: a systematic review of human studies, physiological considerations, and technical recommendations. Mitochondrion 59, 225–245. https://doi.org/10.1016/j.mito.2021.04.002 (2021).
Trumpff, C. et al. Acute psychological stress increases serum Circulating cell-free mitochondrial DNA. Psychoneuroendocrinology 106, 268–276. https://doi.org/10.1016/j.psyneuen.2019.03.026 (2019).
Acknowledgements
We thank Drs. Takashi Sugita and Kenji Hattori for their support on this study.
Author information
Authors and Affiliations
Contributions
T.S. designed the study, performed most of the experiments and wrote the paper. Y.T. C.S. and R.M. performed most of the experiments and helped to analyze the data. M.S., T.K. and A.U. contributed to interpretation of the data and discussion. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shimura, T., Takahashi, Y., Saito, C. et al. Ionizing radiation triggers the release of mitochondrial DNA into the cytosol as a signal of mitochondrial damage. Sci Rep 15, 23191 (2025). https://doi.org/10.1038/s41598-025-04845-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04845-0
Keywords
This article is cited by
-
Ionizing radiation: molecular mechanisms, biological effects, and therapeutic targets
Molecular Biomedicine (2026)