Abstract
The simultaneous posterolateral tibial plateau fracture (PLTPF) with anterior cruciate ligament (ACL) injury has posed a great challenge to both orthopedic trauma and sports medicine surgeons. This study investigated the biomechanical mechanism of simultaneous PLTPF with ACL injury and demonstrated the consistency with anterolateral rotatory instability (ALRI) of the knee. A healthy male volunteer’s right knee CT and MRI images were imported into Mimics software to reconstruct a three-dimensional geometric model of bone, ligament, meniscus and cartilage. The PLTPF were simulated at posterior half of the lateral tibial plateau (LTP) and lateral meniscus posterior horn (LMPH). Three PLTPF depression angles were set at 5°, 10° and 15°. Finite element analysis (FEA) was conducted to observe the displacement of bone and meniscus, ACL strain and LTP stress at 0°and 30° knee flexion with axial and tibial internal rotation loading, in ACL intact and deficient knee. For ACL intact knee, FEA showed axial loading at 0° knee flexion led to abnormal displacements of lateral femoral condyle and LMPH. At 30° flexion, axial 10Nm tibia internal rotation loading resulted in more LTP anterior displacement and ACL strains. The stress of LTP concentrated abnormally on anterolateral part at 0° flexion and posterolateral LTP at 30° flexion. All above parameters tended to increase with the enlargement of depression area and depression angle. In ACL deficient knee, axial 10Nm tibia internal rotation loading led to even more LTP anterior displacement and LTP articular stress at 30° flexion than ACL intact knee, with a tendency of aggravating with increasing depression area and angle. Simultaneous PLTPF with ACL injury has a common flexion valgus and tibial internal rotation injury mechanism with ALRI and should be treated as a special pattern of ALRI. Clinically, high grade PLTPF associated with ACL injury should be addressed by concomitant PLTPF reduction and ACL reconstruction to fully restore LTP articular congruence and knee stability.
Similar content being viewed by others
Introduction
The tibial plateau fractures account for 1% of all adult fractures1. Posterolateral tibial plateau fractures (PLTPF) constitute 15% of all tibial plateau fractures and are among the most challenging fracture types in practice due to the high association with ligament and meniscus injury2,3. Research on tibial plateau fractures from trauma surgeons reported the incidence of anterior cruciate ligament (ACL) injury was 83.2%4. However, clinical study on 825 primary arthroscopic ACL reconstruction (ACLR) cases showed that 49.3% had concomitant PLTPF5. This discrepancy in prevalence primarily stems from the differing patient populations studied by the two disciplines: those with PLTPF fractures and those undergoing ACL reconstruction, but it also necessitates interdisciplinary collaboration to better understand this complex injury pattern. These indicate that simultaneous PLTPF and ACL injury are not uncommon and should be paid more attention.
The treatment strategy on simultaneous PLTPF with ACL injury remains controversial. Clinical studies from trauma perspective mostly focused on the surgical approaches and various fixation methods, leaving ACL injury to staged management6. Whereas research from sports medicine perspective suggested ACLR alone was enough and PLTPF could be left alone without any compromise of knee stability7. A third approach proposed arthroscopic ACLR should be performed concomitantly with PLTPF reduction and fixation8,9,10, to achieve improved IKDC score and radiological Rasmussen score9. This diversity in treatment strategy might derive from lack of biomechanical study in this field.
Therefore, a finite element analysis (FEA) was designed to investigate the setting of PLTPF (with various depression area and depression angle), the displacements of bone and lateral meniscus, ACL tensile stress and the stress of lateral tibial plateau (LTP) articular surface in ACL intact and ACL deficient knee. The hypothesis of this study is that simultaneous PLTPF with ACL injury results from a flexion-valgus biomechanical mechanism with tibial internal rotation which is analogous to that of anterolateral rotatory instability (ALRI) of the knee joint. The potential contributions of both fracture and ACL injury to knee instability make meticulous attention to the management of both during surgery necessary. Intraoperative assessment of knee stability after one injury, thereby guiding decisions regarding the necessity of additional surgical intervention for the other, may be a good strategy.
Materials and methods
Ethics statement
This study was approved by the Ethics Committee of the Shandong Second Medical University Affiliated Qingdao Eighth People’s Hospital (Approval No. QBYLL-KY-2024-042). The research involving human subjects complied with all relevant national regulations and institutional policies and was conducted in accordance with the tenets of the 1964 Helsinki Declaration.
Data collection and geometric model establishment
A 42-year-old health male volunteer, with a height of 170 cm and weight of 75 kg and no history of knee trauma, was informed about the study contents and signed a consent form. The right knee was scanned by CT (SOMATOM Force, SIEMENS) and MRI (MAGNETOM Skyra 3.0T, SIEMENS) in full extension within a range 15 cm above and below the knee. The CT slice thickness was 0.5 mm and MRI 0.8 mm. Images were saved in DICOM format and imported into Materialism Mimics 26.0 (Leuven, Belgium) for 3D reconstruction. The bone, cartilage, menisci, and ligaments were manually segmented to create a detailed geometric model of the knee. The knee model was then imported into 3-Matic Medical software, where smoothing operations were applied to refine the geometry. Separate models were created for the femur, tibia, meniscus, cartilage, and ligaments- anterior & posterior cruciate ligaments and lateral & medial collateral ligament.
Boundary conditions and mesh generation
The geometric models were imported into ABAQUS 2018 (Dassault Systemes, France) for FEA. The interface between bone and cartilage, as well as the ligament insertions were set as binding constraint. The anterior and posterior horns of the menisci were simulated to be fixed at their respective attachment sites on the tibial plateau. Contact interfaces between cartilage-menisci, cartilage-cartilage were set as frictional contact, with a friction coefficient of 0.0111. Meshing of the geometric models was performed with the mesh size of the soft tissues being four times smaller than bone12 and mesh refinement was performed at contact areas. After mesh convergence study, the final number of elements was determined to be 23,840 for bone, 16,135 for ligaments, 112,027 for cartilage, and 105,723 for menisci, totaling 257,725 elements (Fig. 1).
Finite element mesh generation. The mesh generation was performed on the geometric model in ABAQUS software. The mesh size for soft tissues is four times smaller than that for bones, with additional refinement applied in areas of contact. Based on a mesh convergence study, the final number of mesh elements was determined as follows: 23,840 elements for bone, 16,135 elements for ligaments, 112,027 elements for cartilage, and 105,723 elements for the menisci, totaling 257,725 elements.
Material properties
Although the cartilage and meniscus are viscoelastic tissues, both were simplified into single-phase linear isotropic materials in this study because of the short loading and the large viscoelastic time constant. The elastic modulus of cartilage was set at 15 MPa, with a Poisson’s ratio of 0.47513,14. Similarly, the meniscus was modeled with an elastic modulus of 59 MPa and a Poisson’s ratio of 0.4915. The ligaments were treated as linear isotropic materials, with an elastic modulus of 300 MPa and a Poisson’s ratio of 0.45. Given that the significantly higher stiffness of bone compared to soft tissues, the bone was modeled as a rigid body16.
Establishment of the injury model
In the reconstructed model, the femur was rotated backward to simulate 30° knee flexion while keeping the ACL intact, as this angle is deemed most suitable for assessing the rotatory and anterior laxity17. The spatial positions of all ligaments were finely adjusted to achieve better spatial alignment and the areas of stress concentration that might interfere with subsequent calculations were modified. Likewise, models of the ACL deficient knee were created at both 0° and 30° to evaluate the biomechanical effects of ACL injury.
The PLTPF model was established using the cutting function of SolidWorks. First, drawing line a from the anterior to the posterior edge of the LTP articular cartilage at the 50% medial-lateral width of LTP. Then, taking the perpendicular bisector of line a as line b, which was defined as posterior half of LTP. Afterwards, drawing line c parallelling to line b, at the midpoint of LMPH, line c was defined as the posterior half of LMPH (Fig. 2A)18. Starting from lines b and c, depression fracture model was created at angles of 5°, 10°, and 15° posteriorly to simulate various degrees of depression in PLTPF (Fig. 2B). The angle setup primarily references the seminal study conducted by Lobenhoffer et al., which investigated the impact of posterolateral slope variation on anterior tibial translation19. These models allowed for the systematic investigation of different fracture severities and their biomechanical implications.
The establishment of PLTPF model: The line a and b bisect the medial–lateral and anterior–posterior dimensions of the lateral tibial plateau, respectively, while line c bisects the anterior–posterior dimension of the posterior horn of the lateral meniscus, with the posterior portion occupying approximately a quarter of the anterior–posterior diameter of the tibial plateau (A). Based on this definition, when the regions posterior to lines b and c experience varying degrees of posterolateral slope increase (5°, 10°, 15°), we will analyze and compare the differences in biomechanical performance of the models (B).
Loading conditions
Condition 1
Axial loading at 0° knee flexion.
At full extension (0° flexion), the tibia was constrained in all six degrees of freedom. An axial load of 1150 N was applied to the femur to simulate the maximum compressive force experienced during gait cycles. This condition allowed for the observation of bone and LMPH displacements, as well as stress distribution on the chondral surface.
Condition 2
Combined axial and rotational loading at 30° knee flexion.
At 30° knee flexion, two sequential analysis steps were performed:
-
1.
With the tibia being fully constrained at 6 degrees of freedom, the femur was externally rotated to simulate axial tibial internal rotation.
-
2.
A combined load consisting of an axial load of 750 N and a rotational torque of 10Nm was applied to replicate the biomechanical conditions during jumping and landing activities.
This condition enabled the measurement of anterior angular displacement of LTP, ACL strain and the stress distribution on the chondral surface.
Condition 3
ACL deficient knee under combined loading.
To simulate an ACL deficient knee, the ACL was suppressed and the same loading conditions as in Condition 2 were applied. This allowed for the analysis of the tibial anterior angular displacement and stress distribution on the chondral surface in the absence of ACL support.
Key parameters investigated
For both ACL intact and deficient knees, the following parameters were evaluated across all three loading conditions while ACL strain was only evaluated in ACL intact knees:
-
1.
Displacements of the bone and LMPH.
-
2.
Anterior angular displacement of LTP.
-
3.
Stress distribution on the tibial plateau articular surface.
These parameters were assessed for three PLTPF depression angles (5°, 10°, 15°), two depression areas (posterolateral quadrant and posterior to PHLM) and two knee positions (0° and 30° flexion) to determine the impact of varying fracture severity and its interaction with ACL injury.
All original graphs were created using ABAQUS 2018 and GraphPad Prism 10 software.
Results
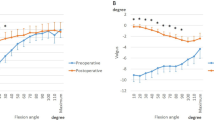
The effect of PLTPF on the displacement of LMPH and femur
In ACL intact knee with concomitant PLTPF, applying an axial load at 0° knee flexion resulted in abnormal posterior extrusion of the LMPH (Fig. 3A). Concurrently, the lateral femoral condyle exhibited significantly greater distal displacement compared to the medial side (Fig. 3B). These displacements increased with the larger of the depression areas and steeper depression angles (Fig. 3C).PLTPF From 0° to 30° knee flexion, the stress concentration area shifted from anterolateral at 0° flexion to the posterolateral region at 30° flexion (Fig. 4A, B). Additionally, applying a 10Nm axial tibial internal rotation load to the flexed knee further increased ACL tensile (Fig. 5A). This effect became more pronounced as the PLTPF depression area and angles of PLTPF increased, with greater depression angles leading to higher ACL strain (Fig. 5B).
The displacements underaxial loading at 0° knee flexion in the FEA model with PLTPF. (A) Displacement cloud diagram for LMPH. (B) Displacement cloud diagram for the lateral femoral condyle. (C) Quantitative comparison of LMPH displacement, showing an increase with larger depression areas and steeper depression angles. LMPH lateral meniscus posterior horn, L lateral side, M Medial side.
Stress distribution on the LTP articular surface in ACL intact knee model with PLTPF: (A) At 0° knee flexion, stress concentrated abnormally on the anterolateral area of the LTP. (B) At 30° knee flexion, stress shifted to posterolateral quadrant of LTP, near the LMPH. LMPH lateral meniscus posterior horn, L lateral side, M Medial side.
Tensile stress in the ACL under 10 Nm axial tibial internal rotation loading at 30° knee in the FEA model with PLTPF: (A) Cloud diagram show changes in ACL tensile stress. (B) Quantitative comparison of ACL tensile stress, demonstrating an increase with larger depression areas and depression angle. LMPH lateral meniscus posterior horn.
The effect of PLTPF on LTP angular displacement
In ACL intact knee at 0° flexion, a 10Nm axial tibial internal rotation load caused a significant increase in anterior angular displacement of the LTP. This displacement was further exacerbated by larger PLTPF depression area and steeper depression angle (Fig. 6A, C). Whereas in ACL deficient knees under the same loading conditions, the magnitude of LTP anterior angular displacement was even greater than that of ACL intact knees, with a similar of worsening as the severity of the PLTPF increased (Fig. 6B, C).
Anterior angular displacements of the LTP under 10 Nm axial tibial internal rotation loading at 30° knee flexion in the FEA model with PLTPF. (A) Displacement in ACL intact knee. (B) Displacement in ACL deficient knee. (C) Comparison of anterior angular displacement between ACL intact and ACL deficient knee. Showing greater displacement in ACL-deficient knees and a trend of worsening with increasing fracture severity. LMPH lateral meniscus posterior horn, ACL anterior cruciate ligament, L lateral side, M Medial side.
Stress distribution on the LTP
In ACL intact knees, axial loading at 0° flexion caused stress concentrate abnormally on the anterolateral LTP. For PLTPF involving the posterior half of LTP, the stress levels were higher compared to those involving the LMPH. The magnitude of stress increased with the steeper depression angles (Fig. 4A). At 30° flexion, the stress concentration area shifted to the posterolateral region of the tibial plateau, near the LMPH. The stress levels continued to rise with increasing depression area and angle (Fig. 4B).
In ACL deficient knees, applying 10Nm tibial internal rotation loading at 30° flexion resulted in even greater stress concentration on the posterolateral quadrant of the LTP (Fig. 7A). Compared to ACL intact knees, the stress levels were significantly higher, particularly for PLTPF involving the posterior half of the LTP (Fig. 7B). The magnitude of stress also increased with steeper depression angle, indicating that both the severity of the fracture and the absence of ACL support contribute to elevated articular stress.
Stress distribution on the LTP articular surface under 10 Nm axial tibial internal rotation loading at 30° knee flexion in the FEA model with ACL deficient knee with PLTPF: (A) Stress cloud diagram for ACL deficient knee, showing concentration in the posterolateral quadrant of the LTP. (B) Comparison of peak stress between ACL intact knee in Fig. 4 and ACL deficient knee, demonstrating higher stress levels in ACL-deficient knees, particularly with increasing depression severity. LMPH lateral meniscus posterior horn, L lateral side, M Medial side.
Discussion
The most important finding of this study is that a complex interplay between PLTPF and ACL injury, emphasizing the need for a holistic approach to understanding and managing these injuries. Firstly, bony contour of a joint itself contributes to highly significant stability over and above the ligaments. Therefore, any obvious intra- and juxta-articular fracture may easily contribute to instability by itself. PLTPF could result in the increase of lateral tibia plateau slope (LTPS) and decrease of anteroposterior length of LTP, which have been proved as risk factors for ALRI of the knee18,19. Secondly, ACL injury resulting from flexion valgus mechanism with tibial internal rotation could aggravate anterior displacement of LTP and lead to more stress on the PLTPF articular surface. This vicious circle should be addressed in the treatment of PLTPF with ACL injury. This FEA study found abnormal displacement of lateral femoral condyle and LMPH, leading to valgus instability. Besides, the LTP stress concentrated anterolaterally at 0° flexion and shifted to posterolateral quadrant of LTP at 30° flexion, resulting in pathological anterior displacement or even subluxation of LTP in ACL deficient knees. This suggests that simultaneous PLTPF with ACL injury could be attributed to flexion-valgus-tibial internal rotation mechanism biomechanically, which is in accordance with the injury mechanism of ALRI20,21,22. This interplay has been observed in previous cadaveric experiments. Lobenhoffer et al. found that the anterior displacement of the tibia constrained by the ACL increases with the slope of the posterolateral tibial plateau19. However, their study did not limit the modeling of tibial depression area to the specific posterolateral region, making their conclusions less applicable to this specific type of injury. Milinkovic et al.23 proposed from biomechanical studies that a reduction in the anteroposterior length of the LTP could exacerbate anterior and internal rotational instability of the knee, analogous to the effect of the reduced glenoid diameter on recurrent anterior shoulder dislocation and named this scenario as a “Bankart knee”. Multiple clinical studies have reported that patients with simultaneous PLTPF with ACL injury exhibited characteristic lesions of ALRI, like lateral femoral condyle bone contusions and soft tissue injuries of the anterolateral capsule-ligament and LMPH24,25. Bernholt et al.5,26 found that under the same injury mechanism of knee flexion and valgus with tibial internal rotation, young or male patients with relatively good bone quality were more likely to suffer from ACL injury combined with soft tissue injuries like medial meniscus (MM) ramp’s lesion, LM posterior root injury or lateral femoral condylar notch bone contusion, which could lead to ALRI. Whereas for elderly or female patients with relatively poor bone quality, simultaneous ACL injury with high-grade PLTPF occurred more commonly5. Therefore, it is reasonable to deduce that high-grade PLTPF combined with ACL injury is a special pattern of ALRI of the knee joint.
This biomechanical study elucidates how anterior angular displacement of the lateral tibial plateau—key manifestation of ALRI—is influenced by various factors. The results demonstrate that both ACL deficiency and variations in the severity of PLTPF contribute to increased translational and rotational instability, supporting the hypothesis that PLTPF combined with ACL injury may represent a distinct pattern of ALRI. These findings also suggest that the ALRI-related manifestations exacerbated by either PLTPF or ACL deficiency may share a common biomechanical basis, with these two injuries and their associated traumas representing variations of a specific injury force mechanism. Overall, these findings enhance our understanding of the concurrent phenomena observed in ALRI, PLTPF, and ACL injuries in clinical study23 by providing insights into their biomechanical interactions. However, given the dual involvement of bony and soft-tissue injuries, further interdisciplinary clinical research integrating expertise from trauma surgery and sports medicine is essential to refine diagnostic criteria and explore its implications for treatment strategies.
This FEA study provided certain inspiration to the treatment strategy for simultaneous PLTPF with ACL injury, just like the analogy from Sauer and Clatworthy27, “a steep hill and a shallow speed bump are a hazardous combination”. It is becoming widely accepted that the ALRI should be managed by combining ACLR with additional lateral extra-articular tenodesis (LET) procedure, only to reduce the failure rate of ACLR and meniscal repair26. Besides, LM injury should be repaired as much as possible28, to avoid “a shallow speed bumper”. Historically, the long-term follow-up has shown high failure rates with either isolated LET surgery or ACLR alone29. Regarding bony morphology, if the LTPS is greater than 12°, a proximal tibial slope reducing osteotomy or tibial deflexion osteotomy should be considered, “making a less steep hill”, to protect the ACLR in revision surgery30. Likewise, in PLTPF with ACL injury cases, PLTPF could also be divided into low-grade and high-grade. Low grade PLTPF was defined as fracture not influencing the LTPS, LTP length or the LMPH stability20,31. For ACL injury with low-grade PLTPF, the clinical outcomes of isolated ACL reconstruction, not addressing PLTPF, were comparable to those ACL injury alone17,31. However, in the setting of PLTPF with increased LTPS or decreased LTP length which producing “Bankart knee”, or fracture depression larger than 50% of LMPH width which” weakening the speed bump”, these scenarios were defined as high-grade PLTPF17,31. For high-grade PLTPF with ACL injury, the strategy might follow the guidance for ALRI treatment that the ACLR must be performed and PLTPF should be reduced and fixed concomitantly20,28,30. According to this FEA results, reducing PLTPF alone without ACLR might increase the risk of PLTPF reduction loss resulting from increased stress on the posterolateral LTP at 30° knee flexion, whereas ACLR without PLTPF reduction equaled to leaving alone the “Bankart knee” with increased LTPS and decreased LTP length from fracture impaction and increased the failure risk of ACLR.
The biomechanical impacts of PLTPF and ACL injuries on the knee stability and suggest the necessity of a comprehensive approach to their treatment. Currently, divergent opinions exist on the optimal surgical management of such injuries6,7. Although biomechanical studies alone are insufficient to establish definitive surgical indications, the potential contributions of both factors to knee instability suggest that surgeons should consider preparing for both PLTPF fixation and ACLR when faced with cases of uncertainty. This strategy enables intraoperative assessment of knee stability following the treatment of one injury, which could help guide decisions on whether additional surgical intervention is needed for the other. This might be an effective strategy to ensure no residual knee instability.
Additionally, the findings of this study, which indicate that the stress on the tibial plateau is predominantly distributed posteriorly at 30° of knee flexion and anteriorly at 0° of knee flexion, suggest that malunion of posterolateral tibial plateau depression fractures may not immediately result in significant abnormalities during knee extension, but instead manifest symptoms during knee flexion. This observation is consistent with recent clinical studies identifying isolated posterolateral fractures as a cause of knee instability and “giving-way” during weight-bearing activities in the flexed knee, such as stair climbing24. Therefore, when analyzing the causes of such symptoms, clinicians should carefully consider the influence of fracture morphology.
Furthermore, this study provides biomechanical evidence relevant to the treatment of posterolateral marginal fractures, also referred to as “apple bite fractures,” which have gained increasing attention in recent years18. Despite their relatively small depression area, these fractures result in greater lateral meniscal extrusion, potentially posing a greater risk to knee stability and function.
Regarding the contributions of bony structures versus soft-tissue structures to knee joint stability, our study, as illustrated in Fig. 6C, reveals the impact of ACL deficiency, steeper posterolateral tibial slope, and larger depression areas on the anterior angular displacement of the lateral tibial plateau. Within the tested ranges, these factors appear to exert comparable effects on knee joint stability, although statistical significance was not assessed due to the study’s focus on qualitative trends. This finding does not contradict the common clinical assertion that fractures generally have a greater impact on knee stability than soft tissue injuries32. Clinical studies often evaluate knee stability comprehensively, incorporating factors such as varus and valgus stresses, which may amplify the perceived contribution of bony injuries. Moreover, the fracture patterns modeled in this study primarily represent low- to moderate-energy trauma and do not fully replicate the compromised bone biomechanics associated with high-energy fractures commonly seen in clinical practice. Nevertheless, these biomechanical insights emphasize the importance of considering both the severity of the fracture and the integrity of soft tissue structures when managing the types of injuries studied here. However, the surgical reduction and fixation methods are controversial. For cases with intact posterolateral cortex and only articular surface depression exceeding 2 mm or larger than 50% LMPH width, arthroscopic-assisted reduction and percutaneous screw fixation with concomitant ACLR showed satisfactory clinical results8,9,10. Another way to address this scenario with comparable clinical results was to combine ACLR with LET26,28. However, for high-grade PLTPF involving posterolateral cortical damage like shear fragment and large displaced osteochondral fracture, open reduction and rigid internal fixation might be the only solution6,18.
Limitations
The FEA method in this study has followed the guidance proposed by Scott et al.33. However, there are still several limitations. First, all soft tissues were defined as isotropic single-phase homogeneous materials. Although this simplification method is widely used to analyze changes in stress, displacement, and other parameters under different loading conditions, the calculated specific values may deviate to a certain extent from the real physiological state in vivo. Therefore, future study should consider incorporating the anisotropy of soft tissues and fluid lubrication into the analysis. Second, this study only involved modeling and analysis of one volunteer, so the data volume is insufficient for statistical processing, allowing only preliminary analysis of trends.
Conclusions
This study demonstrates that simultaneous PLTPF and ACL injury exhibit biomechanical characteristics consistent with anterolateral rotatory instability and may represent variations of a specific injury mechanism. It also highlights the effect on stress distribution, ACL strain, and displacement of femoral condyle and meniscus under different loading conditions in both ACL-intact and ACL-deficient knees. These results underscore the need for comprehensive management addressing both fracture and soft-tissue injury.
Data availability
All data generated or analyzed during this study are included in this published article. Further inquiries can be directed to the corresponding author on reasonable request.
Abbreviations
- PLTPF:
-
Posterolateral tibial plateau fracture
- ACL:
-
Anterior cruciate ligament
- ALRI:
-
Anterolateral rotatory instability
- ACLR:
-
Anterior cruciate ligament reconstruction
- LMPH:
-
Lateral meniscus posterior horn
- LTP:
-
Lateral tibial plateau
- LTPS:
-
Lateral tibia plateau slope
- FEA:
-
Finite element analysis
- HGPS:
-
High-grade pivot shift
- LET:
-
Lateral extra-articular tenodesis
References
Court-Brown, C. M. & Caesar, B. Epidemiology of adult fractures: a review. Injury 37, 691–697. https://doi.org/10.1016/j.injury.2006.04.130 (2006).
Xiang, G., Zhi-Jun, P., Qiang, Z. & Hang, L. Morphological characteristics of posterolateral articular fragments in tibial plateau fractures. Orthopedics 36 (10), e1256–e1261. https://doi.org/10.3928/01477447-20130920-16 (2013).
Wang, Y., Cao, F., Liu, M., Wang, J. & Jia, S. Incidence of soft-tissue injuries in patients with posterolateral tibial plateau fractures: a retrospective review from 2009 to 2014. J. Knee Surg. 29 (6), 451–457. https://doi.org/10.1055/s-0036-1581132 (2016).
Wang, B. et al. Incidence and characteristics of knee ligament and meniscal injuries in patients with posterolateral tibial plateau fractures. Orthop. J. Sports Med. 12 (4), 23259671241238023. https://doi.org/10.1177/23259671241238023 (2024).
Bernholt, D. L. et al. Incidence of displaced posterolateral tibial plateau and lateral femoral condyle impaction fractures in the setting of primary anterior cruciate ligament tear. Am. J. Sports Med. 48 (3), 545–553. https://doi.org/10.1177/0363546519895239 (2020).
Zhu, B., Chen, J., Zhang, Y., Song, L. & Fang, J. Revisiting the flexion-valgus type unicondylar posterolateral tibial plateau depression fracture pattern: classification and treatment. J. Orthop. Surg. Res. 18 (1), 825. https://doi.org/10.1186/s13018-023-04318-y (2023).
Godshaw, B. M. et al. Posterior tibial plateau impaction fractures are not associated with increased knee instability: a quantitative Pivot shift analysis. Knee Surg. Sports Traumatol. Arthrosc. 31 (7), 2998–3006. https://doi.org/10.1007/s00167-023-07312-3 (2023).
Jiang, L., Wu, H. & Yan, S. Two cases of contact anterior cruciate ligament rupture combined with a posterolateral tibial plateau fracture. Case Rep. Orthop. 2015, 250487. https://doi.org/10.1155/2015/250487 (2015).
Yang, Y. et al. Effectiveness of bone grafting versus cannulated screw fixation in the treatment of posterolateral tibial plateau compression fractures with concomitant ACL injury: a comparative study. J. Orthop. Surg. Res. 19 (1), 75. https://doi.org/10.1186/s13018-023-04516-8 (2024).
Park, J. P. et al. An arthroscopic procedure for restoration of posterolateral tibial plateau slope in tibial plateau fracture associated with anterior cruciate ligament injuries. Arthrosc. Tech. 9 (9), e1249–e1258. https://doi.org/10.1016/j.eats.2020.05.003 (2020).
Yan, M. et al. Model properties and clinical application in the finite element analysis of knee joint: a review. Ortho Surg. 16, 289–302. https://doi.org/10.1111/os.13980 (2024).
Jogi, S. P. et al. Model for in-vivo Estimation of stiffness of tibiofemoral joint using MR imaging and FEM analysis. J. Transl Med. 19 (1), 310. https://doi.org/10.1186/s12967-021-02977-1 (2021).
Haut Donahue, T. L., Hull, M. L., Rashid, M. M. & Jacobs, C. R. A finite element model of the human knee joint for the study of tibio-femoral contact. J. Biomech. Eng. 124, 273. https://doi.org/10.1115/1.1470171 (2002).
Yang, N. H., Canavan, P. K., Nayeb-Hashemi, H., Najafi, B. & Vaziri, A. Protocol for constructing subject-specific Biomechanical models of knee joint. Comput. Methods Biomech. Biomed. Eng. 13 (5), 589–603. https://doi.org/10.1080/10255840903389989 (2010).
Pena, E., Calvo, B., Martinez, M. A. & Doblare, M. A three-dimensional finite element analysis of the combined behavior of ligaments and menisci in the healthy human knee joint. J. Biomech. 39 (9), 1686–1701. https://doi.org/10.1016/j.jbiomech.2005.04.030 (2006).
Steineman, B. D., LaPrade, R. F. & Haut Donahue, T. L. Loosening of posteromedial meniscal root repairs affects knee mechanics: a finite element study. J. Biomech. Eng. 144 (5), 051003. https://doi.org/10.1115/1.4053100 (2022).
Kim, S. H., Park, Y. B., Ham, D. W., Lim, J. W. & Lee, H. J. Stress radiography at 30° of knee flexion is a reliable evaluation tool for high-grade rotatory laxity in complete ACL-injured knees. Knee Surg. Sports Traumatol. Arthrosc. 28 (7), 2233–2244 (2020 ).
Menzdorf, L. et al. Clinical results after surgical treatment of posterolateral tibial plateau fractures (apple bite fracture) in combination with ACL injuries. Eur. J. Trauma. Emerg. Surg. 46 (6), 1239–1248. https://doi.org/10.1007/s00068-020-01509-8 (2020).
Agneskirchner, J. D., Hurschler, C., Stukenborg-Colsman, C., Imhoff, A. B. & Lobenhoffer, P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a Biomechanical study in human cadaveric knees. Winner of the Aga-DonJoy award 2004. Arch. Orthop. Trauma. Surg. 124 (9), 575–584 (2004).
Hughston, J. C. A., James, R., Cross, M. J. & Moschi, A. Classification of knee ligament instabilities. Part II. The lateral compartment. J. Bone Joint Surg. Am. 58, 173–179 (1976).
Tanaka, M. et al. What does it take to have a high-grade Pivot shift? Knee Surg. Sports Traumatol. Arthrosc. 20, 737–742. https://doi.org/10.1007/s00167-011-1866-5 (2012).
Fernandes, M. S. et al. Is femoral lateral condyle’s bone morphology the trochlea of the ACL? Knee Surg. Sports Traumatol. Arthrosc. 25 (1), 207–214. https://doi.org/10.1007/s00167-016-4159-1 (2017).
Milinkovic, D. D. et al. The Bankart knee: high-grade impression fractures of the posterolateral tibial plateau lead to increased translational and anterolateral rotational instability of the ACL-deficient knee. Knee Surg. Sports Traumatol. Arthrosc. 31 (10), 4151–4161. https://doi.org/10.1007/s00167-023-07432-w (2023).
Flury, A. et al. Extent of posterolateral tibial plateau impaction fracture correlates with anterolateral complex injury and has an impact on functional outcome after ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 31 (6), 2266–2273. https://doi.org/10.1007/s00167-022-07282-y (2023).
Korthaus, A. et al. Lateral femoral Notch sign and posterolateral tibial plateau fractures and their associated injuries in the setting of an anterior cruciate ligament rupture. Arch. Orthop. Trauma. Surg. 142 (7), 1605–1612. https://doi.org/10.1007/s00402-021-04105-6 (2022).
Bernholt, D. L. et al. High-grade posterolateral tibial plateau impaction fractures in the setting of a primary anterior cruciate ligament tear are correlated with an increased preoperative Pivot shift and inferior postoperative outcomes after anterior cruciate ligament reconstruction. Am. J. Sports Med. 48 (9), 2185–2194. https://doi.org/10.1177/0363546520932912 (2020).
Sauer, S. & Clatworthy, M. The ratio of tibial slope and meniscal bone angle is a strong predictor for anterior cruciate ligament injury: a steep hill and a shallow speed bump are a hazardous combination. Arthroscopy 37 (5), 1610–1611. https://doi.org/10.1016/j.arthro.2021.02.006 (2021).
Getgood, A. M. J. et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-Year outcomes from the STABILITY study randomized clinical trial. Am. J. Sports Med. 48 (2), 285–297. https://doi.org/10.1177/0363546519896333 (2020).
Hughes, J. D., Rauer, T., Gibbs, C. M. & Musahl, V. Diagnosis and treatment of rotatory knee instability. J. Exp. Orthop. 6 (1), 48. https://doi.org/10.1186/s40634-019-0217-1 (2019).
Guarino, A., Pineda, T., Giovannetti de Sanctis, E. & Dejour, D. The original technique for tibial deflexion osteotomy during revision anterior cruciate ligament reconstruction: surgical technique. Arthrosc. Tech. 13 (1), 102824. https://doi.org/10.1016/j.eats.2023.08.029 (2024).
Bernholt, D. L. et al. Morphologic variants of posterolateral tibial plateau impaction fractures in the setting of primary anterior cruciate ligament tear. Am. J. Sports Med. 48 (2), 318–325. https://doi.org/10.1177/0363546519893709 (2020).
Savarese, E., Bisicchia, S., Romeo, R. & Amendola, A. Role of high tibial osteotomy in chronic injuries of posterior cruciate ligament and posterolateral corner. J. Orthop. Traumatol. 12 (1), 1–17. https://doi.org/10.1007/s10195-010-0120-0 (2011).
Scott, C. E. H., Simpson, A. H. R. W. & Pankaj, P. Distinguishing fact from fiction in finite element analysis. A guide for clinicians. Bone Joint J. 102 (10), 1271–1273. https://doi.org/10.1302/0301-620X.102B10.BJJ-2020-0827.R1 (2020).
Acknowledgements
We thank Drs Yu Zhan and Handong Xu for the guidance and assistance in using Materialise Mimics 26, ABAQUS 2018 software and data processing.
Funding
This study was funded by Qingdao Municipal Health Commission Key Clinical Specialty Funding 2022 (QDMHCKCSF-2022). We declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
QX designed the study. GH and QX were major contributors to write the manuscript. ZZ and YC collected and analyzed the data using Materialise Mimics 26, ABAQUS 2018 software. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of the Shandong Second Medical University Affiliated Qingdao Eighth People’s Hospital (Approval No. QBYLL-KY-2024-042). The research involving human subjects complied with all relevant national regulations and institutional policies and was conducted in accordance with the tenets of the 1964 Helsinki Declaration. The participant signed an informed consent form.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, Q., Han, G., Zhang, Z. et al. Posterolateral tibial plateau fracture with anterior cruciate ligament injury has biomechanical characteristics of anterolateral rotatory instability through finite element analysis. Sci Rep 15, 20482 (2025). https://doi.org/10.1038/s41598-025-05291-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-05291-8