Abstract
This study leveraged machine learning (ML) models to explore the relationship between three-dimensional (3D) spinal alignment parameters and clinical outcomes in patients suffering from fibromyalgia syndrome (FMS). A cohort of 303 FMS patients, diagnosed according to the 2016 American College of Rheumatology criteria, underwent comprehensive assessments of sagittal imbalance, coronal imbalance, vertebral rotation, pelvic obliquity, pelvic torsion, and pelvic rotation using a validated 3D imaging system. Clinical outcomes, included the fibromyalgia impact questionnaire (FIQ), pain catastrophizing scale (PCS), Pittsburgh sleep quality index (PSQI), and algometric pain scores. Five ML models were employed: Fast Kolmogorov-Arnold Networks with Bee Colony Optimization (FastKAN-BCO), FastKAN with LBFGS, Multilayer Perceptron with LBFGS (MLP-LBFGS), Multilayer Perceptron with ADAM (MLP-ADAM), and linear regression. Among the models tested, FastKAN-BCO demonstrated the highest R-squared value (0.95) for algometric pain, while the MLP-LBFGS model achieved superior performance for PCS (R2 = 0.94), FIQ (R2 = 0.88), and PSQI (R2 = 0.97) predictions. Sagittal imbalance and pelvic obliquity were identified as key predictors of symptom severity. Stratification revealed that individuals with more pronounced pelvic asymmetry and vertebral rotation exceeding 10° experienced increased symptom intensity. The contribution of vertebral rotation was nonlinear, indicating a threshold-dependent impact. This study illustrates the potential of ML techniques to uncover complex associations between 3D spinal alignment and FMS outcomes, offering a foundation for personalized diagnostic and therapeutic approaches. The results emphasize the critical role of postural dysfunction in FMS and highlight the potential of advanced ML models.
Similar content being viewed by others
Introduction
Fibromyalgia syndrome (FMS) is a chronic and debilitating disorder defined by pervasive musculoskeletal pain, persistent fatigue, sleep disturbances, cognitive dysfunction, and a marked reduction in quality of life1. Global prevalence estimates range from 2 to 4%, with a disproportionately higher incidence observed in women2. Despite substantial research efforts, the pathophysiology of FMS remains incompletely understood, presenting significant challenges in both its diagnosis and management3. The existing diagnostic criteria, including the 2016 American College of Rheumatology (ACR) guidelines4, continue to evolve in response to emerging evidence; however, these criteria often suffer from a lack of specificity, contributing to frequent underdiagnosis and suboptimal treatment. Moreover, the effectiveness of current therapeutic strategies remains limited, as conventional interventions fail to comprehensively address the multifactorial and heterogeneous nature of the disorder4,5,6.
Despite the growing body of research into FMS, its pathophysiology remains elusive, with various theories suggesting a complex interplay of genetic, environmental, and neurobiological factors7,8. Dysregulation of the central nervous system, particularly aberrant pain processing and hypersensitivity to stimuli, is thought to play a pivotal role in the manifestation of FMS symptoms9. Moreover, autonomic dysfunction, disturbances in the hypothalamic–pituitary–adrenal axis, and altered inflammatory pathways have been proposed as contributing factors, though their precise involvement remains unclear. As our understanding of FMS evolves, it is becoming increasingly evident that the syndrome represents a multifactorial condition with significant heterogeneity among individuals, complicating both diagnosis and the development of effective treatments7,10.
Recent studies have highlighted a potential association between abnormal postural alignment and the clinical manifestations of FMS. Postural abnormalities, including sagittal imbalance, coronal imbalance, vertebral rotation, and pelvic asymmetry, are linked to altered sensorimotor integration, heightened pain sensitivity, and increased mechanical stress on the musculoskeletal system. These factors may contribute significantly to the chronicity and severity of symptoms in FMS patients6,11,12,13. For example, sagittal imbalance has been shown to increase the likelihood of FMS, with greater deviations correlating with more severe symptomatology12,14. Additionally, vertebral rotation and pelvic asymmetries further amplify mechanical inefficiencies, exacerbating the overall impact of the syndrome6,14.
The convergence of postural dysregulation and central sensitization underscores the necessity for targeted interventions aimed at restoring biomechanical equilibrium. Preliminary evidence suggests that rectifying postural deviations may enhance sensorimotor integration, modulate neurophysiological pain mechanisms, and mitigate the severity of FMS manifestations. However, further rigorous investigations are warranted to elucidate the mechanistic pathways underpinning these associations6,11,12,13,14,15.
Machine learning (ML) has emerged as a transformative paradigm in biomedical research, facilitating the extraction of meaningful patterns from complex, multidimensional datasets. In the context of FMS, ML offers a powerful framework for uncovering latent relationships between three-dimensional (3D) posture parameters and clinical outcomes insights that may elude conventional statistical approaches. By integrating high-dimensional biomechanical and clinical data, ML-driven models can enhance our understanding of the predictive role of posture in FMS, ultimately contributing to the development of more precise diagnostic tools and personalized therapeutic strategies16,17,18. This study aims to harness ML models to elucidate the relationship between key 3D posture parameters and FMS severity indicators. By integrating advanced computational approaches with clinical and biomechanical data, this study presents a novel framework for enhancing the understanding, diagnosis, and management of FMS. It is hypothesized that deviated postures will predict worse scores on the selected outcome questionnaires.
Methods
Design
This study was designed as a cross-sectional predictive analysis utilizing ML techniques to investigate the relationship between 3D postural parameters and FMS severity indicators. A critical aspect of this study involved leveraging data mining from our previously published research, which extensively explored the connection between cervical alignment, postural dynamics, and FMS severity indicators. By integrating data from these earlier investigations, the study ensured a robust and comprehensive foundation for the machine learning analysis, allowing for the identification of complex patterns and predictive relationships within the dataset5,6,19.
-
1.
Participants and Cohorts:
-
2.
Data Harmonization:
-
A standardized data extraction template was created, focusing exclusively on variables that were:
-
Collected using the same measurement instruments (e.g., Formetric 3D system for posture, validated questionnaires for outcomes).
-
Assessed under identical conditions and protocols, ensuring measurement equivalence across studies.
-
Variables included: sagittal imbalance, coronal imbalance, vertebral rotation, pelvic obliquity, pelvic torsion, pelvic rotation, and outcome scores the various questionnaires described below.
-
Variables were harmonized through rescaling and normalization as described in the “Model Training” section of the manuscript.
-
-
3.
Measurement Consistency:
-
All studies used the Formetric system for 3D spinal assessment and followed the same calibration and posture acquisition protocols.
-
Questionnaires were administered under similar conditions by trained researchers, ensuring consistent data quality.
-
Participants
Three-hundred and three participants were recruited from outpatient clinics and advertisements placed in community centres and on social media platforms. Eligibility criteria included adults aged 18 years or older with a confirmed diagnosis of FMS based on the 2016 ACR diagnostic criteria4. Participants were required to have chronic symptoms lasting for at least 12 months and no prior history of spinal surgery, significant scoliosis, or severe comorbidities, such as uncontrolled cardiopulmonary disease or neurological disorders. Exclusion criteria also included conditions that could interfere with posture assessments, such as acute musculoskeletal injuries or infections13,16,17 A total of 710 individuals were initially screened across three previously published prospective studies5,6,19 and one additional recruitment cohort. Of these, 303 patients met all eligibility criteria, provided informed consent, and had complete data sets for the outcome measures and 3D posture parameters. Reasons for exclusion included failure to meet diagnostic or procedural criteria (n = 405) and participant withdrawal or refusal (n = 46), primarily due to time constraints, anxiety regarding spinal imaging or manipulation, or logistical challenges. A CONSORT-style flow diagram (Fig. 1) is included to enhance transparency.
The majority of the data used in this study was derived from previously published, ethically approved randomized controlled trials and observational studies involving patients with fibromyalgia syndrome (FMS)5,6,19. As such, participants were not newly recruited for this investigation, and no additional interventions were administered during this secondary data analysis. In the original studies, participants had received structured multimodal programs that typically included pharmacological treatments, cognitive behavioural therapy, supervised exercise, and educational sessions. Moreover, some subgroups received cervical extension traction or cervical manipulative therapy as part of their original study allocation. Detailed protocols of these interventions are reported in Moustafa et al., Moustafa et al., and Ahbouch et al.5,6,19. Therefore, while these previous interventions could have influenced postural outcomes, no new treatments were introduced during the course of this machine learning–based analysis. Ethical approval from the University of Sharjah Research Ethics Committee (approval number: REC-24-06-25-01). The study protocols adhered to the Declaration of Helsinki, and all participants provided written informed consent.
Data collection
Postural parameters were measured using the Formetric software system (DIERS Medical Systems, Chicago, IL, USA), a validated 3D imaging system that provides detailed analysis of postural alignment in three planes (sagittal, frontal/coronal and transverse plane)20,21. The system employs surface topography to capture detailed 3D spinal curvature and pelvic positioning. Data acquisition followed standardized procedures, including calibration of the device and positioning of participants in a natural upright stance with bare feet and minimal clothing to ensure accuracy and repeatability of measurements6,21. The following parameters were recorded as shown in Supplementary Fig. 1:
-
Sagittal imbalance (mm) Vertical deviation of C7 from the sacral midpoint in the sagittal plane.
-
Coronal imbalance (mm) Horizontal deviation of C7 from the sacral midpoint in the frontal plane.
-
Vertebral rotation rms (°) Quantified as the root mean square (RMS) of rotational deviations along the spinal midline in the transverse plane. Clinical significance is often considered at values > 8°–10°, although this relationship may vary depending on coexisting postural factors.
-
Pelvic obliquity (pelvic tilt) (mm) Vertical misalignment between the left and right iliac crests.
-
Pelvic torsion (DL-DR ratio) Relative rotation between the left and right pelvic bones.
-
Pelvis rotation (°) Angular twisting of the pelvis about the vertical axis in the transverse plane.
Reliability of formetric system and clinical instruments
To ensure methodological rigor, all postural measurements were acquired using the Formetric 3D rasterstereographic system (DIERS International GmbH), which has been extensively validated and shown to have high test–retest reliability (ICC > 0.91) and strong correlation with radiographic measurements for sagittal alignment, trunk inclination, and surface rotation5,6,21. The system overestimates radiographic kyphosis and lordosis by a mean of 7°–8°, yet this difference is systematic and predictable, with correlation coefficients ranging from r = 0.79 to 0.87 depending on the specific variable measured.
Additionally, internal test–retest reliability was assessed in our study on a randomly selected subsample (n = 20) for posture variables. Intraclass correlation coefficients (ICCs) exceeded 0.90 for trunk inclination, thoracic kyphosis, and lumbar lordosis. For vertebral rotation and pelvic tilt, ICCs ranged from 0.88 to 0.93 Fig. 2.
Several clinical outcome questionnaires were used in this study: (1) Fibromyalgia Impact Questionnaire (FIQ)22, (2) Pain Catastrophizing Scale (PCS)23, (3) Beck Anxiety Inventory (BAI)24, (4) Beck Depression Inventory (BDI)25, and (5) the Pittsburgh Sleep Quality Index (PSQI)26. These questionnaires have been internationally validated and previously tested in FMS populations with high internal consistency (Cronbach’s α > 0.80)22,23,24,25,26.
Clinical outcomes were assessed using validated questionnaires and tools administered by trained researchers. These included:
-
Fibromyalgia Impact Questionnaire (FIQ) A validated patient questionnaire to assess the impact of FMS on daily life, including physical functioning, work status, pain levels, and psychological well-being5,12. It has a score range from 0 to 100 with higher scores reflecting more impairment27.
-
Pain Catastrophizing Scale (PCS) A measure of cognitive and emotional responses to pain, encompassing rumination, magnification, and helplessness6,15. It is composed of a 5-point Likert scale with greater scores indicating greater levels of catastrophizing pain28.
-
Pittsburgh Sleep Quality Index (PSQI) A questionnaire evaluating sleep quality over a one-month interval, addressing domains such as sleep latency, duration, and disturbances to differentiate poor and good sleepers14,29.
-
Algometric pain (AP) score Pain threshold was measured at 18 standardized tender points using a calibrated handheld digital algometer (kg/cm2). Each site was assessed three times, and the mean value per point was recorded. The final AP score represents the summed pressure-pain thresholds across all 18 sites (kg/cm2), reflecting overall mechanical pain sensitivity. This approach is aligned with established protocols in fibromyalgia research18.
Although the Formetric system and clinical questionnaires used in this study are validated tools, inherent measurement errors must be acknowledged. Surface topography assessments can be influenced by soft tissue variability and operator positioning, while clinical questionnaires and algometry are subject to participant self-report bias and procedural variability. Triplicate measures and standardized protocols were employed to minimize these effects.
Machine learning model inputs and outputs
The study utilizes advanced machine learning models to analyze the relationship between 3D spinal alignment and fibromyalgia severity. Six key postural parameters were used as input variables: sagittal imbalance (mm), coronal imbalance (mm), vertebral rotation (°), pelvic obliquity (pelvic tilt, mm), pelvic torsion (DL-DR), and pelvis rotation (°)21 which were used to assess the clinical outcomes or output variables of AP, FIQ, PCS, and PSQI. See Supplementary Table 1.
Model training
To develop and evaluate the predictive models, all variables included in the analysis were complete, with no missing values identified. Therefore, no imputation techniques were applied. The analysis proceeded with the original dataset, which included only fully observed cases. Five models were assessed: Fast Kolmogorov–Arnold Networks with Bee Colony Optimization (FastKAN-BCO), Fast Kolmogorov–Arnold Networks with LBFGS (FastKAN-LBFGS), Linear Regression, Multilayer Perceptron with LBFGS (MLP-LBFGS), and Multilayer Perceptron with ADAM optimizer (MLP-ADAM). The ML models are provided in Supplementary Data S1 with schematics of models in Supplementary figures S2 and S3.
Hyperparameter optimization was conducted using tenfold cross-validation exclusively within the training set to prevent data leakage. For MLP models, a grid search explored variations in the number of hidden layers, neurons per layer, activation functions, regularization strengths, and learning rates. For FastKAN-BCO models, hyperparameter optimization was performed using a Bee Colony Optimization (BCO) metaheuristic, adjusting architecture parameters such as node count, sparsity penalty, and learning rates. The final models were selected based on cross-validated R2 performance on the training set and subsequently evaluated on the independent test set.
FastKAN and MLP architectures were selected based on their proven capacity to model complex nonlinear relationships while maintaining clinical interpretability. FastKAN-BCO offered an adaptive, efficient structure refined through Bee Colony Optimization. MLPs, configured with two hidden layers (64 and 32 neurons) using ReLU activation and He initialization, provided a versatile framework for function approximation. Models were optimized via LBFGS or ADAM optimizers, and regularization techniques were employed to prevent overfitting. Tree-based models and SVMs were considered but not prioritized due to their limitations in capturing smooth, continuous postural effects in moderate-sized clinical datasets.
Hyperparameter optimization was conducted using tenfold cross-validation exclusively within the training set to prevent data leakage. For MLP models, a grid search explored variations in the number of hidden layers, neurons per layer, activation functions, regularization strengths, and learning rates. For FastKAN-BCO models, hyperparameter optimization was performed using a Bee Colony Optimization (BCO) metaheuristic, adjusting architecture parameters such as node count, sparsity penalty, and learning rates. The final models were selected based on cross-validated R2 performance on the training set and subsequently evaluated on the independent test set.
The dataset was split into 80% for training and 20% for testing. To ensure reliability and generalizability of the models, tenfold cross-validation was used on the training dataset for model evaluation and hyperparameter tuning. Reported performance metrics (Table 3) reflect results on the independent test set. Hyperparameter optimization was performed using grid search for linear and neural models, and Bee Colony Optimization for the FastKAN-BCO model.
Sample size estimation
The sample size for this study was determined based on the complexity of the machine learning (ML) models, the number of input features, and the need for sufficient data to ensure model generalization. Given that the study involved predicting four clinical outcomes AP, FIQ, PCS and PSQI using six input features (sagittal imbalance, coronal imbalance, vertebral rotation, pelvic obliquity, pelvic torsion, and pelvic rotation), an appropriate number of samples was required to balance model performance and computational feasibility. To estimate the required sample size, a learning curve analysis was performed by training the models on progressively larger subsets of data and evaluating their performance in terms of mean squared error (MSE) and R-squared (R2) values. This helped identify the point at which adding more data resulted in diminishing returns in predictive accuracy. Additionally, cross-validation techniques (k-fold cross-validation) were used to assess the stability of model predictions and prevent overfitting. Bootstrapping was also applied to estimate variability in model performance and determine whether additional data would significantly improve predictive power.
Statistical analysis
All analyses were performed in Python 3.9.16, using Statsmodels 0.13.5, Scikit-Learn 1.2.2, TensorFlow 2.11.0, PyTorch 1.13.1 + cpu, and SHAP 0.41.0. SPSS Version 26 was used for preliminary descriptive analyses. A fixed random seed of 42 was applied across all modeling steps to ensure reproducibility. Data preprocessing included mean imputation and MinMax scaling. Hyperparameter tuning utilized tenfold cross-validation exclusively within the training set to prevent data leakage. Full code for preprocessing, model training, and evaluation will be made available upon request. Descriptive statistics, including means and standard deviations (SDs), were used to summarize patient demographics and postural variables. Normality of data distribution was assessed using the Shapiro–Wilk test. To assess the relationship between postural alignment and fibromyalgia severity, we employed multiple regression models with AP, FIQ, PCS and PSQI scores as dependent variables. Predictor variables included sagittal imbalance, coronal imbalance, vertebral rotation, pelvic obliquity, pelvic torsion, and pelvic rotation.
Machine learning models, including Fast Kolmogorov-Arnold Networks with Bee Colony Optimization (FastKAN-BCO), FastKAN, multilayer perceptron (MLP), and linear regression, were trained to predict clinical outcomes based on postural parameters. Model performance was evaluated using mean squared error (MSE), root mean squared error (RMSE), and R-squared (R2) values. Feature importance was assessed using SHapley Additive exPlanations (SHAP) values to determine the contribution of each postural variable to the predicted outcomes. SHAP graphs were analyzed to identify key predictors. Significance was set at p < 0.05 for all statistical tests.
Additional statistical modeling
In addition to the machine learning models, standard multiple linear regression analyses were performed for each clinical outcome (AP, FIQ, PCS, PSQI) using the six postural predictors (sagittal imbalance, coronal imbalance, vertebral rotation, pelvic obliquity, pelvic torsion, and pelvic rotation) to establish baseline predictive performance and allow comparison with the nonlinear ML models. Prior to interpretation, key assumptions of multiple linear regression were carefully assessed for the following: Linearity Confirmed via scatterplots and partial regression plots. Normality of residuals Verified by Shapiro–Wilk tests and histogram/Q-Q plots. Homoscedasticity Examined using residual versus fitted plots. Independence of errors Verified using Durbin-Watson statistics (range 1.74–2.09). Multicollinearity All Variance Inflation Factors (VIFs) were < 2.5, indicating acceptable levels. These diagnostics confirmed that the multiple linear regression models satisfied all critical assumptions and were valid within the constraints of linear modelling.
Correlation analysis
To assess potential multicollinearity among input features, Pearson correlation coefficients were computed between all six postural parameters. None of the correlations exceeded 0.7, suggesting low-to-moderate interdependence between predictors.
Results
Three-hundred and three patients aged 51.1 (± 8.1) years diagnosed with FMS based on the 2016 ACR criteria were included in this dataset. The clinical characteristics of the sample are shown in Table 1. Compared to established normative data for healthy adults assessed with the Formetric system, participants in this study demonstrated elevated postural deviations across all measured parameters. Specifically, sagittal imbalance (mean = 9.8 mm), coronal imbalance (11.5 mm), vertebral rotation (10.8°), and pelvic obliquity (12.0 mm) were markedly higher than normative ranges reported in the literature (sagittal imbalance ≤ 5 mm, coronal imbalance ≤ 5–7 mm, vertebral rotation ≤ 5°, pelvic obliquity ≤ 3–4 mm)20,21. These findings highlight the significant degree of postural dysfunction present among the fibromyalgia cohort. Table 2 presents the computed Pearson correlation matrix for all six postural input features used in the models.
Table 3 shows the models (Fast KAN-BCO, Fast KAN, linear regression, MLP-LGBFS and MLP-ADAM) performances for the prediction of the four clinical outcomes of AP, FIQ, PCS and PSQI for both the training and testing. The MSE is the averaged squared difference between a predicted and actual value, thus, a lower MSE is indicative of a higher precision model. The RMSE is the square root of the MSE and provides a standardized measure of prediction accuracy. The R-square represents the explained variation in a linear regression model, the higher the value is to 1, the higher the explained variation. As shown, the MLP-LGBFS model demonstrated the highest R2 during testing for the FIQ (R2 = 0.876), PCS (R2 = 0.938) and PSQI (R2 = 0.965). For the AP, the Fast-KAN-BCO model showed the highest explained variance during testing (R2 = 0.952). In addition to Mean Squared Error (MSE) and Root Mean Squared Error (RMSE), Mean Absolute Error (MAE) was calculated for each model to further validate the robustness of predictions. Table 4 summarizes the performance metrics including MAE across all outcomes.
Validation and stability analyses
Final model evaluation reported in Table 3 was based on a single 80/20 train-test split to preserve strict independence of evaluation data. To assess the stability of model performance, additional analyses using five random splits and bootstrapping were performed. Mean and standard deviation of R2 and RMSE metrics across splits confirmed robustness (e.g., R2 for FastKAN-BCO predicting AP: 0.946 ± 0.0041). Bootstrapped confidence intervals for the best models’ R2 were narrow (e.g., 95% CI [0.937, 0.953]). SHAP analyses repeated across splits demonstrated consistent feature importance rankings, with sagittal imbalance and pelvic obliquity persistently identified as the dominant predictors. This highlights the reproducibility and stability of both model predictions and interpretability outputs. Supplementary Table 2 shows the key summary of findings.
Linear regression model results
For comparison with machine learning approaches, the performance of standard multiple linear regression models is summarized below in Table 5.
These results show that the linear regression models demonstrated reasonably strong explanatory power, particularly for PCS and PSQI. However, the nonlinear ML models (such as FastKAN-BCO and MLP-LBFGS) consistently outperformed linear regression, especially for complex outcome variables like FIQ and AP, capturing threshold-dependent and nonlinear relationships more effectively.
Figures 3, 4, 5, and 6 demonstrates the scatterplots of the predicted versus the actual results for each of the five models for the predicted clinical outcomes of AP, FIQ, PCS and PSQI.
Threshold effects identified via SHAP dependence plots were initially detected visually and then quantitatively confirmed by binning postural parameters into clinically relevant intervals and analysing mean SHAP value shifts. Final thresholds, such as vertebral rotation > 10° and sagittal imbalance > 5 mm, were supported by observable non-linear changes in SHAP contributions. All SHAP dependence plots have been updated to include original units for the x-axes (e.g., mm, degrees) to enhance interpretability.
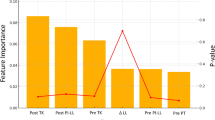
In addition to model performance evaluation, explainability analysis using SHAP (SHapley Additive exPlanations) plots provided critical insights into the underlying feature contributions to model predictions. The SHAP summary plot (Fig. 7) for the prediction of Algometric Pain (AP) revealed that sagittal imbalance and pelvic obliquity (tilt) were consistently the most influential postural predictors across the different machine learning models. Higher sagittal imbalance and pelvic tilt were associated with increased predicted pain severity, as indicated by the positive SHAP values and the predominance of red (high-value) markers. In contrast, features such as coronal imbalance and pelvic rotation showed relatively lower importance for AP prediction.
Furthermore, dependence analysis revealed non-linear feature effects, with notable threshold behaviours. A key dependence plot (Fig. 8) demonstrated a non-linear relationship between vertebral rotation and algometric pain (AP) scores. Specifically, vertebral rotations between 5° and 10° had minimal influence on predicted pain levels. However, vertebral rotations exceeding approximately 10° exhibited a sharp and consistent rise in SHAP values, indicating a threshold beyond which spinal misalignment significantly exacerbates pain severity. This threshold effect appeared more pronounced when accompanied by greater sagittal imbalance, as shown by the color gradient in the plot. These findings underscore the value of SHAP-based interpretation in uncovering complex, nonlinear biomechanical relationships that would be difficult to detect using traditional regression techniques.
Supplementary Figures S4-7 demonstrates SHAP value plots for each of the five ML models for each of the four predicted clinical outcomes of AP, FIQ, PCS and PSQI. SHAP values help interpret machine learning models by showing: (1) the feature importance or which variables impact the prediction most, (2) the direction of impact indicating whether increasing a variable raises or lowers the predicted outcome, and (3) individual contributions of how each variable affects specific predictions. In order to interpret these results, it is important to be knowledgeable about SHAP plot components, which include:
-
1.
Summary plot (Bee swarm plot):
-
Each dot represents a data point.
-
Color: Red = higher value of the variable, Blue = lower value.
-
Color: Red = higher value of the variable, Blue = lower value.
-
X-axis: SHAP value (effect on prediction).
-
-
2.
Dependence plot:
-
Shows how one feature’s value correlates with SHAP values.
-
Helps detect threshold effects or nonlinear relationships.
-
In general, the results from the SHAP analysis strongly supports the role of posture in FMS severity. Further, sagittal imbalance and pelvic obliquity consistently emerged as key risk factors. Finally, the Fast KAN-BCO provided the best feature interpretations. Details of each of the SHAP figures for each clinical outcome follow (Supplementary figures. S4-7).
The SHAP for AP is shown in Figure S4. The key findings from this SHAP summary plot indicate that sagittal imbalance and pelvic obliquity (tilt) are the most influential variables. Pelvic rotation has moderate impact, but coronal imbalance has low influence. A greater sagittal imbalance is associated with increased pain (positive SHAP values). Vertebral rotation showed a nonlinear contribution. While moderate rotation (e.g., 4°–6°) sometimes correlated with reduced symptoms, possibly due to compensatory mechanisms, larger amounts (> 10°) were associated with worsened clinical outcomes. These effects were particularly evident when vertebral rotation coincided with sagittal imbalance or pelvic obliquity. Dependence plot observations indicate that sagittal imbalance > 5 mm leads to a sharp increase in predicted pain and that pelvic obliquity (tilt) > 3 mm also significantly increases pain scores.
The SHAP for the FIQ is shown in Figure S5. The fey findings indicate that pelvic obliquity (tilt) has the strongest impact. Sagittal imbalance and vertebral rotation also influence FIQ scores. Pelvic rotation has a weaker but still notable effect. Greater pelvic tilt is associated with higher FIQ (worse impact of FMS). Vertebral rotation displayed a nonlinear relationship with FIQ; while moderate rotation values (around 5°) appeared to correspond with slightly improved FIQ scores, pronounced rotations (> 10°) consistently predicted worse outcomes, highlighting a possible threshold effect. Dependence plot observations demonstrate that pelvic obliquity (tilt) > 4 mm shows a sharp increase in FIQ scores. For vertebral rotation, a dip in the SHAP values was noted around 5°, indicating that moderate vertebral rotation might correspond to slightly improved FIQ scores, possibly due to biomechanical compensation or measurement noise. However, greater rotation (> 10°) was generally associated with an increased FIQ.
The SHAP for the PCS is shown in Figure S6. The key findings identified pelvic obliquity and sagittal imbalance as the most predictive. Specifically, greater pelvic tilt was associated with higher PCS scores (greater emotional distress related to pain). Coronal imbalance was found to have a weak effect while pelvic rotation affects PCS in a non-linearly fashion. The dependence plot observations indicated that pelvic tilt > 3 mm leads to increased PCS scores. While vertebral rotation influenced PCS scores in interaction with sagittal imbalance and pelvic tilt. The SHAP dependence plots showed minimal impact at moderate vertebral rotation but a positive trend when combined with severe sagittal deviations (> 12 mm), highlighting the importance of considering compound or multiple postural components.
The SHAP for the PSQI is shown in figure S7. The key finding indicated that sagittal imbalance is the dominant factor in poor sleep quality whereas pelvic rotation and vertebral rotation show smaller effects. Greater sagittal imbalance was associated with worse sleep (higher PSQI score). Similarly, greater pelvic tilt was associated with slightly worse sleep. The Dependence plot observations identified that sagittal imbalance > 6 mm sharply increased the PSQI scores while pelvic rotation had inconsistent effects.
Finally, in order to ensure the validity of the multiple linear regression models used in this study, we systematically evaluated the assumptions of linearity, independence of errors, homoscedasticity, normality of residuals, and multicollinearity. These analytical results are shown in Supplementary figures S8 and S9, and in supplementary Table 3.
Discussion
To explore the relationship between 3D spinal alignment and FMS outcomes, we employed five machine learning models FastKAN-BCO, FastKAN with LBGFS, linear regression, MLP with LBGFS, and MLP with ADAM. These models were utilized to analyze six critical postural inputs: sagittal imbalance, coronal imbalance, vertebral rotation, pelvic obliquity, pelvic torsion, and pelvic rotation. The goal was to predict four clinical outcomes: AP, FIQ, PCS, and PSQI. In general, the results support our study hypothesis as the SHAP analysis strongly supports the role of 3D posture displacements in FMS severity, where specifically sagittal imbalance and pelvic obliquity emerged as key risk factors. The magnitude of postural deviations observed in our FMS cohort exceeded normative values reported for healthy populations. Elevated sagittal imbalance, vertebral rotation, and pelvic asymmetries likely contribute to biomechanical inefficiencies and nociceptive signaling, providing a plausible link to the heightened symptom burden observed20,21. These deviation magnitudes not only reinforce the role of postural dysfunction in the pathophysiology of FMS but also support the validity of using postural parameters as key predictors in our ML models.
The MLP-LGBFS model consistently demonstrated superior performance compared to other models for predicting the FIQ, PCS and PSQI clinical outcome scores; in fact, the lowest MSE and RMSE corresponding with highest R2 value (0.97) was shown for predicting PSQI. Importantly, except for predicting the AP, the MLP-LGBFS model consistently outperformed the MLP-ADAM model demonstrating its ability to approximate intricate patterns in the data, underscoring the critical role of selecting appropriate optimization methods. Regarding the prediction of the AP, the FastKAN and FastKAN-BCO outperformed the other models; the FastKAN-BCO showed an R2 of 0.95 and the lowest MSE and RMSE values. The FastKAN-BCO performed slightly better than the FastKAN indicating BCO’s ability to iteratively refine hyperparameters, optimizing the model’s structure and weights to better capture the nonlinear relationships between inputs and outputs. It is worth noting that the RMSE obtained for PSQI prediction (~ 1 point after denormalization) corresponds to less than 5% of the total PSQI scale range (0–21). This suggests that the model’s prediction error is relatively small and likely to be clinically negligible, supporting the model’s potential reliability for estimating sleep quality in fibromyalgia patients.
A key aspect of this study was the stratification of patients based on postural metrics, which enabled the identification of those with pronounced vertebral rotation and pelvic obliquity as having a higher likelihood of experiencing severe symptoms, particularly elevated PCS and AP scores. These findings are consistent with the work of Ahbouch et al.6, who found that sagittal imbalance, thoracic kyphotic angle and vertebral rotation were significant contributors to FMS pathophysiology. Similarly30, in a case control design, Sempere-Rubio and colleagues identified that females with FMS had significantly increased thoracic kyphosis, greater shoulder protraction magnitude, and larger forward head posture. Herein, our observed associations between sagittal imbalance and elevated FIQ scores further substantiate the hypothesis that disruptions in spinal alignment exacerbate pain and disability in FMS. This process likely involves the accumulation of mechanical stress on the musculoskeletal system and altered sensory input, which in turn impairs afferent signalling pathways, thus amplifying pain sensitivity, alters postural control, and contributes to the functional limitations commonly observed in FMS patients31,32.
Central sensitization is widely recognized as a hallmark of FMS, where patients experience heightened sensitivity to external stimuli, such as touch, temperature, and pressure, as well as alterations in their pain thresholds33. This phenomenon occurs due to neuroplastic changes within the CNS, leading to an amplification of pain signaling, even in the absence of noxious stimuli. In FMS, this central dysregulation often manifests as widespread, persistent pain, fatigue, and disrupted sleep patterns34. Disturbance of sleep is one of the key disabilities in FMS sufferers and is associated with a strong risk for developing widespread chronic pain. A recent systematic review of forty-seven randomized trials identified that cognitive behavioral therapy showed a statistically significant impact on improvement of sleep quality but had no impact for improvement of pain35. It is interesting to note that two clinical trials on the improvement of spine and postural alignment identified improvement in sleep quality using the PSIQ5,19. Our findings suggest that abnormal spinal posture not only impairs sleep but also may exacerbate the central sensitization that exists in FMS patients by continuously introducing nociceptive input; that is, pain signals generated by mechanical stress or improper alignment of the spine36. These persistent nociceptive signaling can increase the sensitization of neural pathways in the CNS, further heightening pain sensitivity and promoting the chronic nature of FMS symptoms3.
The upper cervical spine is particularly influential in this context, as it is densely populated with mechanoreceptors that contribute to proprioception and postural control. These receptors play a key role in the modulation of pain and the integration of sensory information from the body to the brain. Alterations in cervical spine alignment, such as forward head posture, can disturb normal sensory processing, creating abnormal afferent input that may worsen central sensitization37. Thus, treatments aimed at correcting the cervical alignment, such as the work of Moustafa and Diab5, suggest that this approach may improve FMS outcomes by restoring proper afferent input to the central nervous system (CNS). This, in turn, likely aids in the recalibration of sensory processing and mitigates the amplification of pain signals, balancing the sensory experience, thus alleviating the severity of FMS symptoms and improving the quality of life for affected individuals5,6,19. Additionally, other studies employing cervical extension traction have reported substantial improvements in both postural parameters and fibromyalgia-related disability19, suggesting that altered cervical curvature and posture is a biomechanical contributor to FMS38,39; perhaps due to its effect on spinal cord biomechanics40.
The present study extends current understanding by quantitatively linking 3D postural metrics with clinical outcomes, specifically the PCS and the PSQI. Vertebral rotation showed variable impact that became clinically significant primarily in patients with high deviation (> 10°) or when compounded by other postural abnormalities (sagittal imbalance and pelvic tilt). This suggests a nonlinear, synergistic effect rather than a uniformly direct contribution, emphasizing the need for compound analysis in future work. These results strengthen the hypothesis that postural correction plays a crucial role in restoring sensorimotor integration and alleviating central sensitization37, a fundamental process in FMS pathophysiology33. Integrating ML into routine clinical workflows could assist rehabilitation specialists in prioritizing interventions for patients most likely to experience significant symptom relief through postural corrections. Moreover, the high predictive accuracy of these models reinforces the feasibility of incorporating advanced algorithms into everyday assessments, which could pave the way for more personalized and effective management strategies in fibromyalgia care. Future research should aim to validate these findings in larger and more diverse patient populations, as well as explore the efficacy of postural correction therapies, such as postural traction techniques19,41 and body awareness therapy42, when integrated with multimodal treatment regimens. Longitudinal studies are particularly necessary to determine whether sustained improvements in spinal alignment lead to long-term reductions in the severity of fibromyalgia symptoms.
The reliability of both the clinical outcome measures22,23,24,25,26,27,28 and postural assessments5,6 have been previously investigated. Our use of the Formetric 3D system was based not only on its non-invasive nature but also its proven high reliability in similar populations, with ICCs consistently exceeding 0.90 for sagittal and transverse alignment variables5,6. Furthermore, internal test–retest reliability conducted on a random subsample in our dataset confirmed the reproducibility of these measurements in our study. This enhances the internal validity of the machine learning analysis performed. Similarly, all clinical questionnaires used demonstrated strong psychometric properties in prior trials on fibromyalgia populations, further supporting the reliability of the input features used in model training22,23,24,25,26,27,28.
Limitations
While this study provides novel insights into the role of three-dimensional (3D) spinal alignment in fibromyalgia and introduces the application of advanced machine learning (ML) models, several limitations should be acknowledged to contextualize the findings and guide future research.
-
1.
Cross-Sectional Study Design: This research utilized a cross-sectional design, which inherently limits the ability to infer causality. While associations between postural parameters and fibromyalgia severity were identified, the temporal direction of these relationships remains unclear. Longitudinal studies are needed to confirm whether postural abnormalities precede symptom exacerbation or occur as compensatory mechanisms due to chronic pain and functional limitations.
-
2.
Potential for Unmeasured Confounding Variables: Although several biomechanical and clinical variables were included, there remains the possibility of unmeasured confounding factors influencing the results. These may include psychological stress, hormonal status, physical activity levels, nutritional status, and comorbid pain syndromes—all of which could modulate pain perception and postural adaptations. Future studies should incorporate a broader biopsychosocial framework to control for such multidimensional influences.
-
3.
Generalizability and Population Bias: The study sample, although clinically relevant and well-characterized, consisted exclusively of patients meeting the 2016 ACR diagnostic criteria for fibromyalgia and recruited from outpatient clinics and community settings within a single geographic region. This may limit the generalizability of the findings to broader or more diverse populations. Additional validation in other ethnic, geographic, and clinical populations is warranted to confirm external applicability.
-
4.
Limitations of the 3D Posture Measurement System: Postural data were collected using a non-invasive 3D surface topography system (Formetric), which, while validated, relies on external surface landmarks and may be influenced by soft tissue variability, operator positioning, or lighting conditions. Though standardized procedures were followed to ensure consistency, subtle errors in pelvic or spinal landmark detection may affect accuracy. In addition, deeper structural abnormalities (e.g., vertebral endplate rotation or sacroiliac joint misalignments) could not be visualized using this surface-based technology.
-
5.
Machine Learning Model Limitations: While ML models such as FastKAN-BCO and MLP-LBFGS demonstrated high predictive accuracy and the SHAP framework improved model interpretability, several limitations remain. First, despite the use of cross-validation and independent test sets, there is always a risk of overfitting, particularly when using nonlinear models on modest sample sizes. Second, the ML models used are “data hungry” and sensitive to outliers or mislabeled data points. Third, while SHAP values provide insights into feature contributions, they do not necessarily imply clinical causality. Finally, model transparency remains a challenge, and interpretability may vary depending on the complexity of the underlying architecture.
While moderate correlations (ranging 0.3–0.46) were noted between some postural parameters (e.g., pelvic obliquity and coronal imbalance), multicollinearity was not severe (see Supplementary Table 3). SHAP values may distribute attribution among correlated features; however, the consistency of SHAP importance rankings across different model runs suggests that model interpretability was not meaningfully compromised. Clinically, some overlap in postural measures, such as between sagittal imbalance and pelvic obliquity, is biomechanically expected and biologically plausible. Another important limitation to consider is the potential measurement error associated with both the postural parameters and clinical outcome assessments. Minor inaccuracies in surface-based 3D measurements and subjective variability in self-reported outcomes or algometry readings could attenuate the true strength of observed associations, resulting in more conservative estimates of model performance. Nevertheless, the consistently high R2 values across models suggest that the identified relationships are robust and clinically meaningful despite this potential measurement noise. Future studies employing gold-standard imaging techniques or repeated measures designs could further refine the predictive capacity of biomechanical models in fibromyalgia.
-
6.
Treatment heterogeneity: Finally, the heterogeneity of treatment exposure across the datasets analyzed is an important consideration. Since all data were extracted from prior trials and case–control studies involving structured multimodal interventions, participants were not medication-naïve or intervention-free at baseline. For instance, previous studies by Moustafa et al.5,19 involved protocols combining supervised exercise, cognitive behavioral therapy, and either cervical traction or manipulative therapy. Additionally, many participants were concurrently using medications commonly prescribed for FMS, such as low-dose antidepressants and analgesics, as part of standard care. Although these prior interventions were not initiated or controlled during the current analysis, they may have contributed to postural and symptomatic differences observed at baseline or follow-up assessments. This inherent limitation of data reuse introduces a risk of residual confounding, which should be acknowledged when interpreting the model outputs and clinical implications. Future prospective machine learning studies should consider stratifying or controlling for intervention type and treatment dosage to isolate the biomechanical contributions more precisely.
Conclusion
Using advanced machine learning models we identified pivotal relationships between three-dimensional spinal alignment and concomitant fibromyalgia disabilities. Sagittal spinal imbalance, pelvic obliquity, and vertebral rotation exceeding 10° were identified as key predictors of symptom severity. These findings underscore the critical importance of addressing postural dysfunction in the comprehensive management of FMS. By integrating biomechanical insights with clinical practice, this research fosters a deeper understanding of the multifactorial etiology of fibromyalgia and lays the groundwork for the development of more precise, personalized diagnostic and therapeutic approaches.
Data availability
Data is available upon reasonable request from corresponding author (DEH) at drdeed@idealspine.com.
References
Choy, E. Fibromyalgia Syndrome (Oxford University Press, 2015).
Chen, J. L. & Mckenzie-Brown, A. M. The epidemiology and prevalence of fibromyalgia (FMS). In Fibromyalgia: Clinical Guidelines and Treatments 1–21 (Springer, 2015).
Albrecht, P. J. & Rice, F. L. Fibromyalgia syndrome pathology and environmental influences on afflictions with medically unexplained symptoms. Rev. Environ. Health. 31, 281–294 (2016).
Wolfe, F. et al. The American College of rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. (Hoboken) 62, 600–610 (2010).
Moustafa, I. M. & Diab, A. A. The addition of upper cervical manipulative therapy in the treatment of patients with fibromyalgia: A randomized controlled trial. Rheumatol. Int. 35, 1163–1174 (2015).
Ahbouch, A. et al. An investigation of the association between 3D spinal alignment and fibromyalgia. J. Clin. Med. 12, 218 (2022).
Siracusa, R., Di, P. R., Cuzzocrea, S. & Impellizzeri, D. Fibromyalgia: Pathogenesis, mechanisms, diagnosis and treatment options update. Int. J. Mol. Sci. 22, 3891 (2021).
Drozd, M., Marzęda, M., Blicharz, A., Czarnota, J. & Piecewicz-Szczęsna, H. Unclear etiology and current hypotheses of the pathogenesis of fibromyalgia. J. Educ. Health Sport 10, 338–344 (2020).
Gyorfi, M., Rupp, A. & Abd-Elsayed, A. Fibromyalgia pathophysiology. Biomedicines 10, 3070 (2022).
Martínez, M. P. et al. Fibromyalgia as a heterogeneous condition: Subgroups of patients based on physical symptoms and cognitive-affective variables related to pain. Span. J. Psychol. 24, e33 (2021).
Marques, A. P., de do Santo, A. S. E., Berssaneti, A. A., Matsutani, L. A. & Yuan, S. L. K. Prevalence of fibromyalgia: Literature review update. Rev. Bras. Reumatol. 57, 356–363 (2017).
Clauw, D. J. Fibromyalgia: A clinical review. JAMA 311, 1547–1555 (2014).
Toprak Celenay, S., Mete, O., Coban, O., Oskay, D. & Erten, S. Trunk position sense, postural stability, and spine posture in fibromyalgia. Rheumatol. Int. 39, 2087–2094 (2019).
Häuser, W. et al. Fibromyalgia. Nat. Rev. Dis Primers 1, 1–16 (2015).
Yunus, M. B. Central sensitivity syndromes: A unified concept for fibromyalgia and other similar maladies. J. Indian Rheum. Assoc. 8, 27–33 (2000).
Fitzcharles, M.-A. et al. 2012 Canadian guidelines for the diagnosis and management of fibromyalgia syndrome: Executive summary. Pain Res. Manag. 18, 119–126 (2013).
Diers, M. et al. Pain-related multisensory integration: A combined behavioural and fMRI investigation. J. Neurosci. 40, 1130–1140 (2020).
Wolfe, F. et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 33, 160–172 (1990).
Moustafa, I. M. Does improvement towards a normal cervical sagittal configuration Aid in the management of fibromyalgia: A randomized controlled trial. Bull. Fac. Ph Th Cairo Univ. 18, 29–41 (2013).
Huthwelker, J., Konradi, J., Wolf, C. & Betz, U. Reference values for 3D spinal posture based on videorasterstereographic analyses of healthy adults. Bioengineering 9, 809 (2022).
Krott, N. L., Wild, M. & Betsch, M. Meta-analysis of the validity and reliability of rasterstereographic measurements of spinal posture. Eur. Spine J. 29, 2392–2401 (2020).
Williams, D. A. & Arnold, L. M. Measures applied to the assessment of fibromyalgia: Fibromyalgia Impact Questionnaire (FIQ), Brief Pain Inventory (BPI), the Multidimensional Fatigue Inventory (MFI-20), the MOS sleep scale, and the multiple ability self-report Questionnaire (MASQ; cognitive dysfunction). Arthritis Care Res. (Hoboken) 63, S86 (2011).
Morris, L. D., Grimmer-Somers, K. A., Louw, Q. A. & Sullivan, M. J. Cross-cultural adaptation and validation of the South African pain catastrophizing scale (SA-PCS) among patients with fibromyalgia. Health Qual. Life Outcomes 10, 1–13 (2012).
Ulusoy, M., Sahin, N. H. & Erkmen, H. Turkish version of the beck anxiety inventory: Psychometric properties. J. Cogn. Psychother. 12, 163 (1998).
Hisli, N. A study on validity and reliability test of the beck depression scale. J. Psychol. 6, 118–122 (1988).
Hita-Contreras, F. et al. Reliability and validity of the Spanish version of the Pittsburgh Sleep Quality Index (PSQI) in patients with fibromyalgia. Rheumatol. Int. 34, 929–936 (2014).
El-Naby, M. A., Hefny, M. A., Fahim, A. E. & Awadalla, M. A. Validation of an adapted Arabic version of fibromyalgia syndrome impact questionnaire. Rheumatol. Int. 33, 2561–2567 (2013).
Campbell, C. M. et al. Changes in pain catastrophizing predict later changes in fibromyalgia clinical and experimental pain report: Cross-lagged panel analyses of dispositional and situational catastrophizing. Arthritis Res. Ther. 14, 1–9 (2012).
Mollayeva, T. et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 25, 52–73. https://doi.org/10.1016/j.smrv.2015.01.009 (2016).
Sempere-Rubio, N. et al. Impaired trunk posture in women with fibromyalgia. Spine (Phila Pa 1976) 43, 1536–1542. https://doi.org/10.1097/BRS.0000000000002681 (2018).
Nunez-Fuentes, D. et al. Alteration of postural balance in patients with fibromyalgia syndrome—A systematic review and meta-analysis. Diagnostics 11, 127 (2021).
Pujol, J. et al. Distinctive alterations in the functional anatomy of the cerebral cortex in pain-sensitized osteoarthritis and fibromyalgia patients. Arthritis Res. Ther. 24, 252 (2022).
Desmeules, J. A. et al. Neurophysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum. 48, 1420–1429 (2003).
Sterling, M., Jull, G. & Wright, A. Cervical mobilisation: Concurrent effects on pain, sympathetic nervous system activity and motor activity. Man. Ther. 6, 72–81 (2001).
Pathak, A. et al. Treatments for enhancing sleep quality in fibromyalgia: A systematic review and meta-analysis. Rheumatology https://doi.org/10.1093/rheumatology/keaf147 (2025).
Woolf, C. J. Central sensitization: implications for the diagnosis and treatment of pain. Pain 152, S2–S15 (2011).
Moustafa, I. M., Diab, A. A. M. & Harrison, D. E. Does forward head posture influence somatosensory evoked potentials and somatosensory processing in asymptomatic young adults?. J. Clin. Med. 12, 3217 (2023).
Delen, V. & İlter, S. Loss of cervical lordosis in chronic neck pain patients with fibromyalgia: A cross-sectional study. J. Back Musculoskelet. Rehabil. 36, 1429–1434 (2023).
Katz, R. S., Leavitt, F., Cherny, K., Small, A. K. & Small, B. J. The vast majority of patients with fibromyalgia have a straight neck observed on a lateral view radiograph of the cervical spine: An aid in the diagnosis of fibromyalgia and a possible clue to the etiology. JCR J. Clin. Rheumatol. 29, 91–94 (2023).
Gundamraj, S. et al. Effect of sagittal alignment on spinal cord biomechanics in the stenotic cervical spine during neck flexion and extension. Biomech. Model Mechanobiol. 23, 1757–1764 (2024).
Oakley, P. A., Ehsani, N. N., Moustafa, I. M. & Harrison, D. E. Restoring cervical lordosis by cervical extension traction methods in the treatment of cervical spine disorders: A systematic review of controlled trials. J. Phys. Ther. Sci. 33, 2021–2073. https://doi.org/10.1589/jpts.33.784 (2021).
Tahran, Ö., Ersoz Huseyinsinoglu, B., Yolcu, G., Karadağ Saygı, E. & Yeldan, İ. Comparing face-to-face and internet-based basic body awareness therapy for fibromyalgia: A randomized controlled trial. Disabil. Rehabil. https://doi.org/10.1080/09638288.2025.2465597 (2025).
Funding
Partial funding for this project was received from The NCMIC Foundation and CBP NonProfit for funding of open access fees for publication.
Author information
Authors and Affiliations
Contributions
Authors IMM, IAK, SAMZ, DUO, MTM, PAO., and DEH all participated in the research idea and participated in its design. IMM, IAK, DUO, MTM, and D.E.H. contributed to the statistical analysis. IMM, IAK, SAMZ, DUO, MTM participated in data collection and supervision. IMM, IAK, SAMZ, DUO, MTM, PAO., and DEH all contributed to the interpretation of the results and wrote the drafts. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
PAO is a paid consultant for CBP NonProfit, Inc. DEH teaches rehabilitation methods and is the CEO of a company that distributes spine rehabilitation equipment to physicians in the U.S.A., none of which were used in this manuscript. All the other authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Moustafa, I.M., Khowailed, I.A., Zadeh, S.A.M. et al. Advanced machine learning applications in fibromyalgia to assess the relationship between 3D spinal alignment with clinical outcomes. Sci Rep 15, 22804 (2025). https://doi.org/10.1038/s41598-025-05390-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-05390-6