Abstract
Diabetes mellitus is a common metabolic disorder resulting from either insulin deficiency or ineffectiveness. Hyperglycemic Emergency are the major serious acute complications of diabetes mellitus. Even though; there is an increasing impact of hyperglycemic emergency among adult diabetic patients, its incidence and predictors have not been well studied particularly in Ethiopia. Hence, this study aimed to assess the time to hyperglycemic emergency and its predictors among adult diabetic patients in the follow-up treatment of public hospitals in Hadiya Zone, Central Ethiopia. An institutional-based retrospective follow-up study was conducted from September 1/2019 to August 30/2022. A total of 455 samples were selected using a systematic random sampling technique. Data was collected using a prepared checklist extraction from patients’ charts. The data were entered into epi-data version 4.6 software and then exported to STATA version 14.0 for analysis. Kaplan- Marie survival function and Log-rank test were computed. The assumption was checked by using the Schoenfeld residual test. All variables in bivariate analysis, p-value < 0.20 were entered into a multivariate Cox regression model. Adjusted hazard ratio with 95% Confidence interval was reported to declare the strength of association between independent variables and outcome variable and statistically significant at p-value < 0.05. Model fitness was checked by using the Cox-Snell residual. Finally, data was presented in text, table and graph. The proportion of hyperglycemic emergency among diabetes patients was 56%, with a median time to develop hyperglycemic emergency is 14.3 months. The incidence rate of hyperglycemic emergency among diabetes mellitus patients was 44.1 (95% CI: 39.0, 49.8) per 1000 person month of observation. The study also found that diabetic patients with age of under 40(AHR = 2.1; 95% CI: 1.44, 3.09), had no health insurance AHR = 1.5; 95%CI: 1.11, 1.89), had comorbidities (AHR = 1.6; 95% CI: 1.22, 2.06), missed medication histories before the occurrence of HGEs (AHR = 1.8; 95% CI: 1.41, 2.40), and had poor glycemic control (AHR = 1.5; 95% CI: 1.09, 1.99) were significant predictors of hyperglycemic emergency. The study found that hyperglycemic emergency was a major public health among the diabetic population. The study also found significant predictors for developing hyperglycemic Emergency among diabetic patients including those under 40 years of age, comorbidity, having no health insurance, missing prescribed medication, and poor glycemic control. This study recommends that healthcare providers, policymakers, and community organizations work together to reduce the incidence of hyperglycemic Emergency among diabetic patients, ultimately improving health outcomes and quality of life for this vulnerable population.
Similar content being viewed by others
Introduction
Diabetes mellitus is a serious, long-term condition that occurs when the blood glucose level is > 250 mg/dl. This is because the body cannot produce enough insulin or effectively use the insulin it produces. Commonly, there are 2 types of Diabetes mellitus: type 1 Diabetes mellitus, which occurs when the body does not produce sufficient insulin, and type 2 Diabetes mellitus, which occurs because of ineffective use of insulin11,2,3. A hyperglycemic emergency is a metabolic emergency associated with uncontrolled diabetic mellitus, which includes diabetic ketoacidosis and hyperglycemic hyperosmolar state3,4.
Diabetic ketoacidosis (DKA) is common in type 1 Diabetes mellitus and is characterized by hyperglycemia, ketosis, and acidosis5,6. Hyperosmolar hyperglycemic state (HHS) is a markedly raised blood glucose level and hyperosmolarity with little or absent ketosis. HHS is common in type 2 diabetes mellitus7,8,9,10. HGEs have a common clinical manifestation of polyuria, polydipsia, polyphagia, weight loss, tachycardia, hypotension, electrolyte disturbance, and confusion11,12.
According to the Canadian consensus statement on Diabetes mellitus, the incidence of DKA with type 1 Diabetes mellitus was found to be between 0.32 and 2.0 per 1,000 patient–years13. In Western countries, the annual incidence of DKA was about 4.6 to 8 episodes per 1, 000 diabetic patients4. In Lagos, south-west Nigeria, the prevalence of Hyperglycemic Emergency was 85% for DKA and 15% for HHS14. In a hospital-based prospective observational study in Ethiopia, the prevalence of HGEs was 38.210.
Diabetes is a major driver of mortality and morbidity worldwide, especially in developing countries, which cannot cover their medical costs. Globally, 6.7 million adults died due to Diabetes mellitus or its complications in 2021report15. According to the National Diabetes Surveillance Program of the Centers for Disease Control (CDC), the overall mortality rate of HGEs was 5–20% for HHS and < 5% for DKA16. In Africa, the mortality rate of HGEs was 7.5% and 34% in South Africa17 and Nigeria18, respectively.
HGEs are diagnosed and treated immediately to decrease morbidity and mortality rates. Fluid, insulin, and electrolyte replacement are vital management methods of HGEs to decrease mortality regarding them19,20. Delayed and improper management of HGEs results in cerebral oedema, pulmonary oedema, hypoglycemia, thromboembolism, hypokalaemia, and renal failure8. Its management costs are markedly higher and even impossible to maintain in developing countries19,21. According to a study in the USA, DKA is responsible for more than 500,000 hospital days per year at an estimated annual direct medical expense and indirect cost of 2.4 billion USD22,23. Since the prevalence of Diabetes mellitus has increased in Ethiopia over the last two to three decades, it is becoming a major economic burden due to the cost of medication and hospitalization24,25.
Despite the different risk factors presented, such as the rise in the incidence of HGEs, poor self-glycaemic control, and interruption of therapy for many social and economic reasons24,25, patient comorbidities16,26, depression and alcohol or substance abuse appear to play strong roles in the increasing incidence of HGEs16. In addition, a study conducted in Ethiopia showed that types of Diabetes mellitus, diabetic durations and patients without community health insurance were found to be significant predictors of hyperglycemic Emergency27.
Diabetes is a growing global burden, but there is limited data on the incidence of hyperglycemic Emergency among diabetic patients, especially in Africa. Due to the severe complications associated with this disease, individuals with diabetes mellitus often make frequent visits to healthcare facilities, which can lead to undesirable economic and social problems. Henceforth, this study aimed to assess the incidence rate, time to hyperglycemic Emergency and its predictors among adult diabetic patients.
Methods
Study area
The study was conducted in Hadiya Zone four public hospitals in the Central Ethiopia Region. Hosanna, the capital town of the Central Ethiopia region, is located 232 km away from Addis Ababa. There are four public hospitals in the Hadiya zone. Wachemo University Comprehensive Specialized Hospital, Shone General Hospital, Homecho Primary Hospital, and Gimbichu Primary Hospital were included in the study. There are diabetes mellitus follow-up clinics in all hospitals in the zone. These hospitals provide inpatient and outpatient services for more than eight million people.
Study design and period
An institutional-based retrospective follow-up study was conducted from September 1, 2019, to August 31, 2022, and the actual data collection period was June 1–30, 2023.
Source of population
All adult diabetic mellitus patients who had a follow-up treatment in the chronic clinic of Hadiya Zone public hospitals.
Study population
All adults diagnosed with diabetes mellitus had follow-up treatment from September 1, 2019, to August 31, 2022, in the four public hospitals in the Hadiya zone.
Eligibility criteria
All diabetes mellitus patients with an age ≥ 18 years old registered in adult diabetes mellitus follow-up clinics from September 1, 2019, to August 31, 2022, were included in the study. However, individuals who developed DKA and HHS at the first diagnosis of diabetes mellitus, patient charts that were not available during data collection, and charts whose records were incomplete for important variables were excluded from the study.
Sample size determination and sampling procedure
For the first objective, a single population proportion formula will be used to calculate the sample size by considering the following statistical assumptions.
-
P = Proportion of HGEs among adults with diabetes mellitus, 38.2% from the previous study in Ethiopia28.
-
q = 1- p.
-
\(\:{Z}_{\alpha\:/2}\)= The corresponding Z score at a 95% confidence level
-
\(\:d\) = Margin of error (5%)
-
\(\:N=\) minimum sample size
N= \(\:\frac{\left(1.96\right)2\:\times\:\:0.382\times\:\:0.618}{\left(0.05\right)2\:}\) = 362.763∼362.8, the after adding a 10% incomplete data rate the sample size is 400.
For the second objective, the sample size will be determined by using the Stat Calc function of Epi Info software version 7 by Appling Cohort sample size calculation technique and taking common predictor variables for HGEs with 95% confidence interval, 80% power, and 1:1 ratio of unexposed to exposed patients. Then the maximum sample size of the variables was taken (Table 1).
Sampling procedure
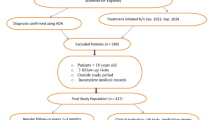
The calculated sample size was proportionally allocated to each hospital based on the number of diabetes mellitus patients on follow-up at the hospitals during the study period. Medical records of adults diagnosed with Diabetic Mellitus were isolated from diabetic follow-up clinics and discharge logbooks (medical, emergency, and Out Patients Department). Then a systematic random sampling method was used to select study charts. The first chart was selected by the lottery method using their order of follow-up entries, and then every second chart was selected for data collection until the total sample size was fulfilled. The subsequent charts were considered if it appeared that any charts had been missed or had incomplete data (Fig. 1).
Operational definition
Hyperglycemic Emergency: are considered based on a clinical diagnosis of DKA, HHS, or mixed diagnosis mentioned in the medical records or when there is a random blood glucose level > 250 mg/dl and urine ketone body > + 2 for DKA and Random blood glucose level > 600 with minimal or absent urine ketone body for HHS32. Survival: time measured between the date of diabetes mellitus diagnosis and the date of developing HGEs or the date of censoring. Censored: adult diagnosed with diabetes mellitus and who did not develop HGEs during follow-up study (transfer-out, died, lost to follow-up, still not develop HGEs because study ends). Controlled blood glucose is defined as a patient whose HgA1c < 7% or average 4-month blood glucose measurement on three consecutive visits is 70–130 mg/dl33. Time to develop HGEs: The time in which the diabetes patient develops HGEs after the diagnosis of diabetes mellitus.
Data collection tools and procedure
Data was collected using a data extraction checklist tool adapted from different literature10,22,34,35. The data were collected from the patient chart in terms of socio-demographic, clinical, treatment-related, and behavioral variables. Charts were retrieved based on their medical registration number in each hospital and were selected by a systematic random sampling method using computer-generated numbers. The extracted data was coded to avoid duplication. Data collection was done by four BSc nurses, and one MSc nurse supervised the data collection process. The data collection was conducted on June 1–30, 2023.
Data quality assurance
A two-day training was provided to data collectors and a supervisor on the data collection process. It focused on introducing the purpose of the study, data collection tools, the initial and end of the data collection period, the correct completion of the checklist, and ethical considerations to standardize the data collection. A preliminary data extraction checklist chart review was conducted at Doctor Bogalech General Hospital to ensure the availability of variables on the patient’s chart. Besides, the data were cross-checked for completeness, clarity, consistency, and accuracy by the supervisor and the principal investigator before data analysis.
Data processing and analysis
Data were entered into Epi-Data version 4.6 and exported to Stata version 14.0 for statistical analysis. Explanatory data analysis was done to determine missing values, normality tests, and the presence of outliers before data analysis. Then the data were described using relative frequency, percent, mean with standard deviation, and median. Incomplete data were managed with the assumption of multiple imputations, after which it was ascertained that the missing data was completely at random and less than 10% of the records. The outcome of each study subject was dichotomized into events and censored. A life table, Kaplan-Meier and log-rank test were computed. The Kaplan-Meier failure curve and the log-rank test were fitted to test the presence of differences between categories of explanatory variables. The Cox proportional hazard regression was used to explore the association between each independent variable and the outcome variable. In bivariable analysis, variables having p-value < 0.20 were candidates for multivariable analysis. The proportional hazard assumption was checked using the Schoenfeld residual test, and it satisfied and global test with a value of p = 0.3437, which was insignificant. Multicollinearity for independent variables was checked by using the variance inflation factor (VIF) and the mean VIF was 1.27. The Cox-Snell residuals were also used to assess the Cox regression model’s fitness for the data. An adjusted hazard ratio (AHR) with a 95% confidence interval was used to explore the strength of the association and variables with p-values less than 0.05 were declared statistically significant with time to hyperglycaemic Emergency. Finally, data was presented using texts, tables and graphs.
Result
Socio-demographicSocio-Demographic characteristic
From the beginning of September 2019 to the end of August 2022, 804 diabetes patients were treated at the chosen public hospitals. A total of 455 charts were reviewed. The participants’ mean age was 45.1 (SD ± 11.3) years. About 29.5% of the research participants were under 40 years of age, with a median age of 46. The majority of individuals (66.6%) were men, with 57% experiencing hyperglycemic crises. Furthermore, 58.9% of the individuals resided in rural settings, with 64.2% experiencing hyperglycemic Emergency. Finally, 40% of the individuals did not have health insurance, and 64% of them experienced hyperglycemic Emergency (Table 2).
Clinical and treatment-related characteristics
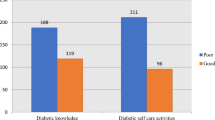
Nearly 39% of the study participants were type 1 diabetic mellitus patients, and more than three-fourths (78.8%) of them had hyperglycemic Emergency (HGEs). Half (50%) of the study participants received lentil insulin (NPH), of which 72% developed HGEs. More than half (51% of study participants) had a history of missing drugs before incidents of hyperglycemic Emergency, and 69% of them developed hyperglycemic Emergency. Regarding the presence of acute illness, 38% of the study participants had acute illness, of which 60.6% developed the HGEs. Nearly half (49.2%) of the participants had at least one comorbidity. Hypertension was the most frequent comorbidity, accounting for 40% of cases. About 12% of the participants suffered from a chronic complication. Of the total diabetic mellitus patients, 62.6% of them had poor glycemic control, and 67% of them developed HGEs. Finally, 48.6% of the study participants missed their follow-up appointment, of which 61% developed HGEs (Table 3).
Incidence density of hyperglycemic emergency among diabetic mellitus patients
This study found that the overall hyperglycemic Emergency among diabetic patients was 56%, with a median time to develop hyperglycemic Emergency of 14.3 months (95% CI: 13.2, 15.3). The total person-time observation was 5781.4 months. The incident rate of hyperglycemic Emergency among diabetic mellitus patients was 44.1 (95% CI: 39.0, 49.8) per 1000 person month of observation. The cumulative probability of failure at the end of 6, 12, 18, 24, and 36 months were 0.2203, 0.3621, 0.6116, 0.6747, 0.7429, and 1.000, respectively (Table 4).
Survival status using the Kaplan-Meier curve
Survival status using Kaplan-Meir curve
The median time was 14.3 months. We notice from the Kaplan-Meir graph that the probability of experiencing hyperglycemic Emergency (HGEs) was lower at the time of diagnosis, but increased as follow-up time (Fig. 2).
Survival function and comparison of survivorship function for different categories
The Kaplan-Meier estimator survival curve provides an estimate of survivor function among different groups, allowing for group comparisons. A survival function line that is above another indicates that the groups indicated by the upper line curve have a higher survival rate than other group line curves within the category. To determine the equivalence of survival curves, the log-rank test was used. The test results derived from the log rank revealed that there is a statistical difference to test the null hypothesis, indicating a difference in the distribution of survival times across categorical variables using the chi-square (Table 5).
In this study, diabetic patients who had no health insurance had a low survival time with a median day of 12.2 months (95% CI: 11.6, 13.2) as compared to patients who had health insurance with 16.3 (95% CI: 14.7, 19.5). The difference was statistically significant with a p-value of 0.0000 (Fig. 3).
This study showed that diabetic mellitus patients who had comorbidities had a higher probability of developing hyperglycemic Emergency, with a survival median of 13.1 months (95% CI: 12.3, 14.2) as compared to patients who had no comorbidities, with a median time of 18.1 months (95% CI: 14.9, 24.0). The difference was statistically significant with a p-value of 0.0000 (Fig. 4).
Study participants whose ages ranged from 18 to 39 years had a lower survival median time with median months of 11.7 (95% CI: 8.5, 12.2) as compared to those of greater age. The difference was statistically significant with a p-value of 0.0000 (Fig. 5).
In this study, diabetic patients who had a history of missing drugs before the incidence of hyperglycemic Emergency had a higher probability of developing hyperglycemic Emergency, with a median of 11.7 months (95% CI). The difference was statistically significant with a p-value of 0.0000 (Fig. 6).
This study also demonstrated that diabetic mellitus patients who had poor glycemic control had a higher probability of developing hyperglycemic Emergency with a median time of 14.2 months (95% CI: 12.6, 15.0) as compared to patients who had good glycemic control with a median time of 19.5 months (95% CI: 14.4, 23.1). The difference was statistically significant with a p-value of 0.0002 (Fig. 7).
Model fitness
Model fitness was checked graphically in this study using the Cox-Snell residuals plot to assess model fitness. As demonstrated in the Cox-Snell residuals graph model, it fits. For the residuals test, the hazard function follows close to the baseline hazard, which indicates that the model was well-fitted. Hence, the final multivariate analysis has been accepted and reported accordingly (Fig. 8).
Predictors of time to hyperglycemic emergency among diabetic mellitus patients
Based on the multivariable Cox proportional hazard regression analysis, patients with an age below 40 who had no health insurance, comorbidity, missed drug history before the event of HGEs, and patients who had poor glycemic control were significant predictors of time to the event of hyperglycemic Emergency.
Keeping other variables constant, diabetic mellitus patients aged less than 40 years had 2.1 times a higher hazard of hyperglycemic Emergency as compared to their counterparts (AHR = 2.1; 95% CI: 1.44, 3.09). The hazard of hyperglycemic Emergency among those who had no health insurance was 1.5 times higher as compared to those who had health insurance (AHR = 1.5; 95%CI: 1.11, 1.89). Moreover, those diabetic patients who had comorbidity were 1.6 times more likely to develop hyperglycemic Emergency as compared to those without comorbidity (AHR = 1.6; 95% CI: 1.22, 2.06). From this study, it was found that diabetic patients who had a history of missing drugs were 1.8 times more likely to develop hyperglycemic Emergency as compared to those who had no missing drug history (AHR = 1.8; 95% CI: 1.41, 2.40). Finally, diabetic mellitus patients who had poor glycemic control before incidents of hyperglycemic Emergency were 1.5 times more likely to develop hyperglycemic Emergency compared to their counterparts (AHR = 1.5; 95% CI: 1.09, 1.99) (Table 6).
Discussion
Diabetes mellitus is a significant public health problem. Its complications, such as hyperglycemic Emergency, is a primary cause of death among diabetes patients. As a result, the purpose of this study was to determine the incidence rate, time to hyperglycemic Emergency, and predictors among adult diabetes patients undergoing follow-up treatment at Hadiya Zone Public Hospitals. According to the current study, the median time for hyperglycemic Emergency among diabetes patients was 14.3 months. Diabetic mellitus patients less than the age of 40, who had comorbidities, no health insurance, a history of missing drugs, and poor glycemic control were significant predictors for experiencing hyperglycemic Emergency.
This study found that the median time for hyperglycemic Emergency of diabetic patients was 14.3 months (95% CI: 13.2, 15.3). This finding is lower than that of a study conducted in Ethiopia, which reported that the median time was 53.8 months27. This discrepancy might be because different time frames can lead to variations in the median time for hyperglycemic Emergency.
In this study, the proportion of HGEs during the study period was 56%. It is higher than studies conducted in, Thailand, 7.46%5, Jimma, 38.210, Hawasa, 40%34 and Bahirdar, 32.4527. This study also showed that the overall incidence density rate of hyperglycemic Emergency among diabetic mellitus was 44.1 (95% CI: 39.0, 49.8) per 1000 person-months of observation. This finding is higher than previous studies conducted in Ethiopia27, Spain, 2.6636, Brazil 8.737 and Korea38. This discrepancy might be due to differences in the study population, lifestyle, level of education, environment, patient awareness of diabetes management, quality of care provided by the hospitals, and diabetic care services and treatment modalities, which all affect glycemic control and diabetic management; consequently, these could affect the incidence of HGEs. However, the finding of this study is lower than a study conducted in Nigeria, 93.6%39. The discrepancy may be because of the differences in the study population, the current was conducted on Type I diabetes mellitus and Type II diabetes mellitus patients who were on follow-up for 3 years, whereas the other study was conducted on only Type I diabetes mellitus patients who were admitted to the emergency department, and the duration of the study was 5 years. These factors highly contribute to the increased incidence of HGEs in the study conducted in Nigeria.
Diabetic patients whose age is less than 40 years were found to be a significant predictor of hyperglycemic Emergency, and had 2 times a higher hazard of experiencing hyperglycemic Emergency compared to their counterparts (AHR = 2.1; 95%CI: 1.44, 3.09). This finding is similar to previous studies3,30. In contrast, other studies revealed that there was no significant difference between age categories for developing HGEs18,27. The Possible justification for the variation might be due to Younger diabetes patients, especially those from lower socioeconomic backgrounds, may face several barriers, such as food insecurity, a lack of access to healthcare, improper management of insulin and inadequate health insurance. These factors can lead to poor diabetes control and an increased risk of hyperglycemic Emergency.
In this study, it was found that health insurance was a significant predictor of experiencing hyperglycemic Emergency among diabetic patients. For diabetes, patients who had no health insurance were 1.5 times more likely to develop hyperglycemic Emergency as compared to those who had health insurance (AHR = 1.5; 95% CI: 1.11, 1.89). This finding is in line with previous findings in Ethiopia27. The possible reason could be that diabetic individuals without health insurance frequently lack access to routine preventive healthcare services and delay medical attention due to financial issues. This can lead to poorly controlled diabetes, which increases the risk of hyperglycemic Emergency. Furthermore, without insurance, diabetes medications and equipment like insulin and glucose monitoring devices can be prohibitively expensive. Previous reports have provided scientific data to support this. This is supported by previous scientific reports40.
Moreover, those diabetic patients who had comorbidity were 1.6 times a higher to develop hyperglycemic Emergency as compared to those without comorbidity (AHR = 1.6; 95%CI: 1.22, 2.06). This finding was supported by previous studies10,27,34. The explanation might be that comorbidities hamper diabetes medical treatment, resulting in poor blood sugar control and an increased risk of hyperglycemic Emergency. Comorbidities can further worsen the severity of hyperglycemic Emergency and lead to poor treatment outcomes. In addition, comorbidity may have an impact negatively on medication adherence to diabetes treatment regimens. This is also supported by previous literature40,41.
From this study, it was found that diabetic patients who had a history of missing drugs were 1.8 times more likely to develop hyperglycemic Emergency as compared to those who had no missing drug history (AHR = 1.8; 95% CI: 1.41, 2.40). This finding was in line with a study conducted in Ethiopia27. Another study also indicated that diabetic patients who do not take their prescribed medication properly might be hospitalized, commonly due to elevating their blood glucose level42. However, we found a scarcity of studies on the association between missing medication and the development of hyperglycemic Emergency.
Finally, diabetic mellitus patients who had poor glycemic control before incidents of hyperglycemic Emergency were 1.5 times more likely to develop hyperglycemic Emergency compared to their counterparts (AHR = 1.5; 95% CI: 1.09, 1.99). The current finding is in line with a previous study conducted in Ethiopia27. This is also comparable with studies conducted in the USA43, and Australia44. A possible justification could be that diabetic patients who do not regularly monitor their blood sugar and engage in unhealthy behaviors are more prone to hyperglycemic Emergency.
Limitations of this study
This study was subject to some limitations, including the retrospective nature of the study, certain essential variables such as occupation, educational level, Body mass index, and history of substance abuse were overlooked, which might have a major influence on the incidence of HGEs.
Conclusion
The study found that hyperglycemic Emergency were a major public health among the diabetic population, and 56% of the participants developed hyperglycemic Emergency. The study also found significant predictors for developing hyperglycemic Emergency among diabetic patients including those under 40 years of age, comorbidity, having no health insurance, missing prescribed medication, and poor glycemic control. This study recommends that healthcare providers, policymakers, and community organizations work together to reduce the incidence of hyperglycemic Emergency among diabetic patients, ultimately improving health outcomes and quality of life for this vulnerable population.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hinkle, J. L. & Cheever, K. H. Brunner and Suddarth’s Textbook of medical-surgical Nursing (Wolters kluwer india Pvt Ltd., 2018).
Sun, H. et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109–119 (2022).
Desai, R. et al. Temporal trends in the prevalence of diabetes decompensation (diabetic ketoacidosis and hyperosmolar hyperglycemic state) among adult patients hospitalized with diabetes mellitus: a nationwide analysis stratified by age, gender, and race. Cureus, 11(4). (2019).
Fayfman, M., Pasquel, F. J. & Umpierrez, G. E. Management of hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Med. Clin. 101 (3), 587–606 (2017).
Jervis, A. et al. Prevalence of diabetes ketoacidosis rises and still no strict treatment adherence. Curr. Diabetes. Rev. 9 (1), 54–61 (2013).
Ae, K. Hyperglycemic crisis in adult patients with diabetes. Diabetes Care. 29, 2739–2748 (2006).
Stoner, G. D. Hyperosmolar hyperglycemic state. Am. Family Phys. 96 (11), 729–736 (2017).
Anthanont, P., Khawcharoenporn, T. & Tharavanij, T. Incidences and outcomes of hyperglycemic crises: a 5-year study in a tertiary care center in Thailand. J. Med. Assoc. Thai. 95 (8), 995 (2012).
Corwell, B. et al. Current diagnosis and treatment of hyperglycemic emergency. Emerg. Med. Clin. 32 (2), 437–452 (2014).
Desse, T. A., Eshetie, T. C. & Gudina, E. K. Predictors and treatment outcome of hyperglycemic emergency at Jimma university specialized hospital, Southwest Ethiopia. BMC Res. Notes. 8, 1–8 (2015).
Kitabchi, A. E. et al. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 32 (7), 1335 (2009).
Puttanna, A. & Padinjakara, R. Diabetic ketoacidosis in type 2 diabetes mellitus. Practical Diabetes. 31 (4), 155–158 (2014).
Butalia, S. et al. Clinical and socio-demographic factors associated with diabetic ketoacidosis hospitalization in adults with type 1 diabetes. Diabet. Med. 30 (5), 567–573 (2013).
Olugbemide, O. et al. Clinical profile and outcome of hyperglycaemic emergency at a rural hospital in Southern Nigeria. Afr. J. Diabetes Med., 25(2). (2017).
Sun, H. et al. Erratum to IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045[Diabetes Res. Clin. Pract. 183 (2022) 109119]. Diabetes research and clinical practice, 204: p. 110945. (2023).
Liu, C. C. et al. Trends in hospitalization for diabetic ketoacidosis in diabetic patients in taiwan: analysis of National claims data, 1997–2005. J. Formos. Med. Assoc. 109 (10), 725–734 (2010).
Pepper, D. et al. Hyperglycaemic emergency admissions to a secondary-level hospital—an unnecessary financial burden. J. Endocrinol. Metabolism Diabetes South. Afr. 12 (2), 56–60 (2007).
Ogbera, A. O. et al. Clinical features, predictive factors and outcome of hyperglycaemic emergency in a developing country. BMC Endocr. Disorders. 9, 1–5 (2009).
Goguen, J., Gilbert, J., C.D.A.C.P.G, E. & Committee Hyperglycemic emergency in adults. Can. J. Diabetes. 37, S72–S76 (2013).
Nigatu, T. Epidemiology, complications and management of diabetes in ethiopia: a systematic review. J. Diabetes. 4 (2), 174–180 (2012).
Wang, Z., Kihl-Selstam, E. & Eriksson, J. W. Ketoacidosis occurs in both type 1 and type 2 diabetes—a population‐based study from Northern Sweden. Diabet. Med. 25 (7), 867–870 (2008).
Bradford, A. L. et al. Predictors of recurrent hospital admission for patients presenting with diabetic ketoacidosis and hyperglycemic hyperosmolar state. J. Clin. Med. Res. 9 (1), 35 (2017).
Control, C. D. & Prevention Estimates of Diabetes and its Burden in the United States. National Diabetes Statistics Report (US Department of Health and Human Services, 2014).
Feleke, Y. & Enquselassie, F. An assessment of the health care system for diabetes in addis ababa, Ethiopia. Ethiop. J. Health Dev. 19 (3), 203–210 (2005).
Lester, F. T. The clinical pattern of diabetes mellitus in Ethiopians. Diabetes Care. 7 (1), 6–11 (1984).
Nyenwe, E. et al. Admissions for diabetic ketoacidosis in ethnic minority groups in a City hospital. Metabolism 56 (2), 172–178 (2007).
Abate, M. D. et al. Incidence and predictors of hyperglycemic emergency among adult diabetic patients in Bahir Dar City public hospitals, Northwest ethiopia, 2021: A multicenter retrospective follow-up study. Front. Public. Health. 11, 1116713 (2023).
Desse, T. A., Eshetie, T. C. & Gudina, E. K. Predictors and treatment outcome of hyperglycemic emergency at Jimma university specialized hospital, Southwest Ethiopia. BMC Res. Notes. 8 (1), 1–8 (2015).
Negera, G. Z., Weldegebriel, B. & Fekadu, G. Acute Complications of Diabetes and its Predictors among Adult Diabetic Patients at Jimma Medical Center, Southwest Ethiopiap. 1237–1242 (Diabetes, 2020).
Mansour, A. & Abdu-Alla, M. Predictors of diabetic ketoacidosis among patients with type 1 diabetes mellitus seen in the emergency unit. Br. J. Med. Med. Res. 11 (10), 1–12 (2016).
Getie, A. et al. Determinants of diabetes ketoacidosis among diabetes mellitus patients at North Wollo and Waghimra zone public hospitals, Amhara region, Northern Ethiopia. BMC Endocr. Disorders. 21, 1–9 (2021).
Gebremedhin, G. et al. Hyperglycemic Crisis Characteristics and Outcome of Care in Adult Patients Without and with a History of Diabetes in Tigrai, Ethiopia: Comparative Studyp. 547–556 (Diabetes, Metabolic Syndrome and Obesity, 2021).
Cengiz, E. et al. Severe hypoglycemia and diabetic ketoacidosis among youth with type 1 diabetes in the T1D exchange clinic registry. Pediatr. Diabetes. 14 (6), 447–454 (2013).
Bedaso, A. et al. Diabetic ketoacidosis among adult patients with diabetes mellitus admitted to emergency unit of Hawassa university comprehensive specialized hospital. BMC Res. Notes. 12, 1–5 (2019).
Steenkamp, D. W., Alexanian, S. M. & McDonnell, M. E. Adult hyperglycemic crisis: a review and perspective. Curr. Diab. Rep. 13, 130–137 (2013).
Guisado-Vasco, P. et al. Clinical features, mortality, hospital admission, and length of stay of a cohort of adult patients with diabetic ketoacidosis attending the emergency room of a tertiary hospital in Spain. Endocrinología Y Nutrición (English Edition). 62 (6), 277–284 (2015).
Nunes, R. T. L. et al. Incidence, characteristics and long-term outcomes of patients with diabetic ketoacidosis: a prospective prognosis cohort study in an emergency department. Sao Paulo Med. J. 139 (01), 10–17 (2021).
Son, J. W. Trends in Hyperglycemic Crisis Hospitalizations and in-and out-of-Hospital Mortality in the Last Decade Based on Korean National Health Insurance Claims Data (Endocrinol Metab ; 34: 275–81, Ji Hong You et al.). Endocrinology and Metabolism, 2019. 34(4): pp. 422–423. (2019).
Amadi, C. et al. The Incidence of Diabetic Ketoacidosis and Its Relationship with Residential Areas of Adults with Type 1 Diabetes in Nigeria.
Goguen, J., Gilbert, J., D.C.C.P, G. E. & Committee Hyperglycemic emergency in adults. Can. J. Diabetes. 42, S109–S114 (2018).
Tassew, W. C. et al. Poor treatment outcome and associated factors of hyperglycemic emergency among diabetic patients in ethiopia: A systematic review and meta-analysis. Metab. Open. 21, 100275 (2024).
Yan, J. W. et al. Risk factors for recurrent emergency department visits for hyperglycemia in patients with diabetes mellitus. Int. J. Emerg. Med. 10, 1–8 (2017).
Duca, L. M. et al. Diabetic ketoacidosis at diagnosis of type 1 diabetes predicts poor long-term glycemic control. Diabetes Care. 40 (9), 1249–1255 (2017).
Davis, T. M. & Davis, W. Incidence and associates of diabetic ketoacidosis in a community-based cohort: the Fremantle diabetes study phase II. BMJ Open. Diabetes Res. Care. 8 (1), e000983 (2020).
Acknowledgements
We would like to acknowledge that data collectors, supervisors, staff, and administrators were appreciated for providing the necessary preliminary information. The authors would also like to thank Wachemo University for giving us this chance.
Funding
This research received funds from Addis Ababa University, College of Medicine and Health Science.
Author information
Authors and Affiliations
Contributions
MGA and TMA participated in the study conception and design as well as the interpretation of data. MGA, YDW, GOB, SFS and AGH were advised during proposal development and were involved in the study design and tool preparation, editing the proposal and advised during data analysis. MGA& TMA performed the statistical analysis, as well as drafted and reviewed the manuscript. TMA also edited the manuscript and prepared it for publication. All authors read and approved the final manuscript and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
was obtained from the institutional review board of Wachemo University (protocol number = WCU-IRB 006/23). The Institutional Review Board (IRB) of Wachemo University, College of Medicine and Health Sciences provided the ethical letter and the medical directors of the hospitals where the data was collected provided written approval. Following an explanation of the study’s purpose, potential benefits, and the estimated time required to complete the interview, oral and written informed consent was obtained from each participating epileptic patient before proceeding with the procedure. Every single piece of information taken from the medical records was kept private and utilized just for this purpose. All methods were performed in accordance with the relevant guidelines and regulations in the manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alaro, M.G., Ashine, T.M., Alaro, M.G. et al. Time to hyperglycemic emergency and its predictors among adult diabetic patients on follow-up in four public hospitals, in central Ethiopia. Sci Rep 15, 33844 (2025). https://doi.org/10.1038/s41598-025-06186-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-06186-4